Abstract
Objective
The aim of this study was to investigate the effectiveness of a qigong training program in reducing stress in hospital staff.
Methods
Subjects were randomly assigned to a 6-week intervention of either qigong practice (n = 16) or a waiting list (n = 21). The primary measure of stress was the Perceived Stress Scale. Secondary measures included the Short Form 36 (SF-36) quality-of-life measure and a 100-mm analog pain scale.
Results
The qigong group demonstrated a statistically significant reduction of perceived stress compared to the control group (p = 0.02). On the Social Interaction subscale of the SF-36, the qigong group demonstrated greater improvement compared to controls (p = 0.04). Within-groups analyses demonstrated that the qigong group (p = 0.03), but not the control group, experienced a significant reduction of pain intensity. A regression analysis demonstrated an association between higher baseline stress levels and greater improvement within the qigong group (R2 = 0.34; p = 0.02).
Conclusions
These results suggest that short-term exposure to qigong was effective in reducing stress in hospital staff. Further studies are needed to evaluate the possible effectiveness of qigong in reducing pain and in improving quality of life.
Introduction
Excessive stress adversely impacts health and is associated with an increased incidence of anxiety and mood disorders and impairments of functioning in every organ system of the body.1–5 Ultimately, the deleterious effects of stress generalize to the workplace, leading to professional burnout with attendant declines in job productivity and increased absenteeism.6
Among hospital staff in particular, there is evidence of elevated rates of psychologic stress and stress-related disorders. For example, medical and social work staff have greater levels of mood disorders and other stress-related illness compared to employees in other fields.7 Even when psychiatric vulnerability and outside-of-work social stress were accounted for, work-related stress was demonstrated to be a contributor to anxiety and depressive disorders in health care professionals and hospital staff.8 Another recent report noted an increasing prevalence of emotional exhaustion and psychiatric disorders in physicians.9
One novel approach that may prove useful in mitigating stress in the workplace is medical qigong, an exercise technique that originated in China more than 3000 years ago.10 This practice synchronizes precise physical movements with specific breathing techniques to enhance health. Initial trials have suggested that qigong is effective in reducing perceived stress11,12 and blood pressure.13,14 Given these reports, there is an ongoing need for further studies to extend these findings to evaluate the effectiveness of qigong in specific treatment groups. In addition, since there are over 1000 forms of qigong extant, it is important to determine whether some types of qigong are more effective than others in reducing stress.
The purpose of this study was to evaluate the effectiveness and feasibility of utilizing “The Basic Eight©” qigong set to reduce stress in hospital staff, a group known to have elevated rates of stress.7 Providing qigong in such a high-intensity workplace potentially offers a number of unique challenges, as hospital staff generally have irregular schedules frequently interrupted by urgent, job-related matters.15 Thus, the 2 questions addressed by this study were as follows: (1) Will qigong prove effective in reducing stress in hospital staff? and (2) Is an onsite qigong intervention a feasible approach for hospital staff?
Methods
Subjects and recruitment
Subjects were employees of the Denver Veterans Affairs Medical Center. Recruitment fliers were posted on both hospital grounds and were sent to employees' work e-mail addresses. It was made clear that this study was voluntary and would not affect employment status in any way. Potential study subjects were screened to ensure that they did not have medical problems that would limit their ability to perform exercise of mild-to-moderate intensity. Subjects were excluded if they used another mind–body practice (for example, yoga or meditation) more frequently than once per week. The study was approved by the University of Colorado Institutional Review Board and by the Denver Veterans Affairs Research Committee as safe and appropriate for human subjects.
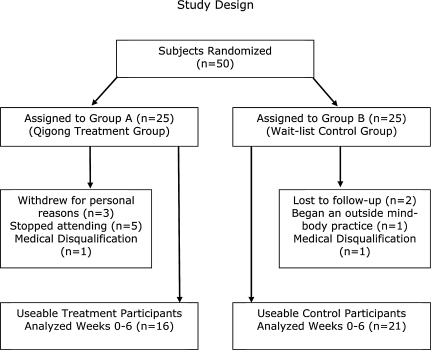
Fifty (50) subjects, 39 females and 11 males, were matched for gender and then randomized (25 in each treatment group) through the use of computer-generated numbers (SYSTAT 12.0 for Windows, Cranes Software, 2007, Bangalore, India). Thirteen (13) subjects (9 from the qigong group and 4 from the control group) did not complete the study (Fig. 1). Five (5) participants from group A (qigong group) withdrew for unknown reasons and 3 withdrew for personal reasons (death in the family). Two (2) subjects from group B (waiting-list group) were lost to follow-up. There were no significant differences in numbers of withdrawals between study groups. There were no adverse events related to the study.
FIG. 1.
Study design.
Study design
This was a randomized, waiting-list controlled, 6-week clinical trial of the effectiveness and feasibility of a qigong intervention designed to reduce perceived stress and improve quality of life in hospital staff (Fig. 1). Measures were obtained during the week prior to the initiation of the study and 6 weeks after the beginning of the study. The primary measure was the Perceived Stress Scale,16 a 10-item measure with 5-point Likert scales with a maximum stress score of 40. Secondary measures were the Health Status Survey Short Form (SF-36) quality-of-life measure,17 body weight, blood pressure, heart rate, and quality of sleep and intensity of pain over the previous week measures recorded by 100-mm visual analog scales. Subjects in the qigong exercise group recorded the number of minutes they practiced each day in an exercise diary.
Study interventions
Subjects assigned to the exercise group attended a 1-hour, noon qigong class twice weekly and were asked to practice independently for 30 minutes on nonclass days with the aid of a DVD demonstrating the instructor performing the exercises. Classes were taught by a senior apprentice in qigong with over 17 years' experience in qigong (J.G.). In addition, subjects were provided a manual that outlined the acupuncture meridians and the rationale for the exercises.
Qigong exercises
The qigong exercises employed were The Basic Eight©, a medical qigong set consisting of 8 exercises designed by qigong grandmaster Hong Liu to activate 14 of the meridians commonly employed by acupuncturists: the lung, large intestine, stomach, spleen, heart, small intestine, urinary bladder, kidney, heart governor, triple heater, gallbladder, liver, and conception and governing vessels. It should be noted that when Chinese Medicine began over 3000 years ago, physicians lacked the modern anatomical and physiologic methods currently employed to describe medical processes. Thus, much of the terminology used in Chinese Medicine is metaphorical. Even so, many acupuncture points lie at the intersection of nerves, blood vessels, and fascial tissue planes.18,19 The Basic Eight© qigong set uses specific movements postulated to physically stimulate key acupuncture points of meridians, which, from a classical qigong perspective, promotes the flow of qi (vital energy) through these meridians.10 During class sessions, subjects practiced movements until they experienced a sensation of stretching or pressure in the targeted acupuncture points (see Appendix). The qigong movements were synchronized with specific breathing patterns, and subjects were instructed to inhale and exhale fully at a comfortable rate, with a target respiratory rate of 6 breaths or fewer per minute.
Statistical analyses
Between-group comparisons of demographic characteristics, baseline measures, and changes in measures from baseline to study completion were analyzed by preplanned t tests. Regression analyses were used to evaluate the impact of practice duration and initial Perceived Stress Scale (PSS) scores on changes in PSS scores. All analyses were conducted with SYSTAT 12.0 for Windows.
Results
Subject characteristics
Based upon t tests, there were no significant differences in baseline demographic or clinical characteristics between groups A and B (Table 1).Similarly, there were no significant differences in baseline scores on the PSS, SF-36, and sleep and pain analog scales. Based upon t tests, there were no statistically significant differences between groups in changes of weight, blood pressure, pain, or sleep measures (Table 2).
Table 1.
Subject Demographics and Baseline Measures
| Group A | Group B | |
|---|---|---|
| Male/female subjects | 4/12 | 5/17 |
| Age (SD) | 52 (9) | 50 (10) |
| Weight (SD) | 163 (25) | 179 (46) |
| Height (SD) | 66 (4) | 70 (4) |
| BP: systolic (SD) | 127 (14) | 124 (15) |
| BP: diastolic (SD) | 80 (8) | 73 (10) |
| Pulse (SD) | 72 (10) | 69 (10) |
BP, blood pressure; SD, standard deviation.
Table 2.
Change in Measures from Baseline
| |
Active |
Waiting list |
Diff. between groups |
||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | t | p | df | |
| PSS | −4.5 | 6.6 | 0.4 | 4.9 | −2.458 | 0.02 | 35 |
| SF-36 Physical Functioning | 3.4 | 14.2 | 1.7 | 7.5 | 0.453 | 0.66 | 35 |
| SF-36 Role-Physical | 3.1 | 35.2 | 14.3 | 35.0 | −0.958 | 0.35 | 35 |
| SF-36 Bodily Pain | 8.3 | 24.1 | 4.8 | 14.6 | 0.512 | 0.61 | 35 |
| SF-36 General Health | 1.9 | 18.4 | 3.6 | 15.8 | −0.295 | 0.77 | 35 |
| SF-36 Vitality | 11.3 | 19.2 | 3.8 | 14.9 | 1.284 | 0.21 | 35 |
| SF-36 Social Functioning | 17.3 | 24.5 | 2.4 | 16.7 | 2.035 | 0.05 | 35 |
| SF-36 Role-Emotional | 14.6 | 24.1 | 19.1 | 34.3 | −0.471 | 0.64 | 35 |
| SF-36 Mental Health | 73.3 | 17.3 | 69.1 | 24.5 | 0.597 | 0.55 | 35 |
| Sleep | 10.0 | 17.7 | 7.0 | 28.9 | 0.389 | 0.70 | 35 |
| Pain | −5.6 | 10.7 | −0.3 | 18.4 | −1.097 | 0.28 | 26 |
Statistically significant differences are highlighted in bold. PSS, Perceived Stress Scale; SF-36, Health Status Survey Short Form.
Based on PSS scores, group A had significant reductions in perceived stress compared to group B (Table 2).Members of group A also exhibited significant increases on the SF-36 Social Functioning subscale in comparison to group B. However, groups A and B did not demonstrated significantly different changes in Physical Function, Role Function, Bodily Pain, General Health, Vitality, Role-Emotional, or Mental Health subscales. Table 2 reports the results of the t tests that were done to compare the changes in outcome scores of groups A and B.
Pain analyses
A subanalysis was conducted in subjects who experienced pain (11 subjects from group A and 16 subjects from group B), using within-groups t tests to further analyze for changes in pain intensity during the course of the study. In this analysis, group A demonstrated a significant reduction of pain (t = 2.15, df = 35, p = 0.02) but group B did not.
Regression analyses
Because PSS scores indicated that the treatment group experienced a significant reduction in stress, a regression analysis was performed to look for a dose effect of qigong practice time. The results of a linear regression indicated that change in PSS score was not a linear function of total exercise time (R2 = 0.000; p = 0.984). In an effort to explore the possible explanations for the change in PSS scores, a linear regression was run to examine whether change in PSS score was a function of baseline PSS score (Table 3).Regression results indicated that baseline PSS score was a strong predictor of change in PSS score only in the qigong group (R2 = 0.345; p = 0.02). To look for an interaction effect between baseline PSS score and total exercise time, a third linear regression examined change in PSS score as a function of baseline PSS score and total exercise time in the qigong group. The resulting equation was not a significantly better fit than the model that examined only baseline PSS scores and change in PSS scores.
Table 3.
Regression Analyses of Perceived Stress Scale (PSS) Scores
|
Active | |||
|---|---|---|---|
| Dependent variable | Independent variables | R2 | p |
| PSS score change | Exercise time | 0 | 0.98 |
| PSS score change | PSS baseline score | 0.34 | 0.02 |
| PSS score change | Exercise time + PSS baseline score | 0.36 | 0.02 (PSS_BL); |
| 0.61 (exercise time) | |||
|
Waiting list | |||
|---|---|---|---|
| Dependent variable | Independent variables | R2 | p |
| PSS score change | PSS baseline score | 0.14 | 0.09 |
Statistically significant results are depicted in bold. BL, baseline.
The fact that change in PSS scores were strongly related to baseline PSS score in the qigong group could indicate that the changes in PSS score experienced by the active group were a function of regression to the mean. Therefore, we performed a similar regression analysis examining PSS score change as a function of the baseline PSS score among the waiting-list group. For the control group, changes in PSS scores were not significantly related to baseline PSS scores (R2 = 0.142; p = 0.09), indicating that qigong was the active mediator.
Discussion
This investigation found medical qigong effective in reducing stress in hospital staff over the course of a 6-week trial. As this medical qigong course was taught during work hours, with subjects utilizing their lunch times to participate, class participation was subject to the usual interruptions associated with working in a hospital environment. Thus, the study results suggest that medical qigong can be effective in reducing perceived stress under typical hospital work conditions.
The results of the regression analysis did not indicate a dosage effect for qigong treatment. However, the fact that changes in PSS score were not significantly related to baseline PSS scores in the control group indicates that the changes in PSS scores among the active group cannot simply be attributed to regression toward the mean. Rather, the results indicate that the effects of qigong may be more dichotomous, such that practicing at or above a critical amount will produce a relatively consistent positive effect, while practicing below that critical amount will produce little or no effect. Once the critical amount of activity is achieved, the benefits become a function of how distressed the patient feels.
The basis of qigong's impact on stress reduction likely involves multiple mechanisms. Exercise is known to reduce stress, and the particular set of medical qigong employed in this study provides exercise of moderate intensity.20 Concentration meditation, a component of qigong practice, also decreases stress.21,22 The practice of slow, deep breathing patterns similar to those employed in this qigong set have been demonstrated effective in reducing blood pressure in both mild hypertensive and normotensive subjects, through a mechanism thought to be related to decreased sympathetic activity.23 Finally, stress-related endogenous chemicals, including norepinephrine11 and cortisol,24 were reported to be reduced by qigong.
There are many different forms of qigong exercise, and in this study we use the general term qigong to include t'ai chi, a standard practice in many qigong traditions. The medical qigong set utilized in this study emphasizes precise movements intended to create a sensation of pressure or stretching of muscle and/or connective tissue at targeted acupuncture points. Although the long-term impact of medical qigong designed to stimulate specific acupuncture points is yet to be studied, reports from the acupuncture literature suggest that stimulation of acupuncture points can generate effects unique to that point. For example, acupuncture stimulation at heart governor 6 has consistently been demonstrated to be antiemetic.25 Furthermore, a recent report on the effects of capsaicin plaster stimulation at stomach 36 found it superior to placebo plaster and capsaicin plaster stimulation at a nonacupuncture point in reducing quantities of morphine required for postoperative pain.26 Thus, further inquiry is needed to determine whether qigong practices such as The Basic Eight©, which provide specific acupuncture point stimulation, provide unique therapeutic effects that distinguish it from different qigong forms and other mind–body methods.
In addition to demonstrating a reduction of perceived stress, those with pain in the qigong group had a significant reduction of pain intensity. The failure to find a significant difference in pain reduction between groups may have been related to the small sample size evaluated, and requires further studies designed to specifically address pain. One recent qigong study reported that elderly patients who practiced qigong reported significant reductions of pain and had significant improvements of cell-mediated immunity.27
The social function subscale of the SF-36 was significantly improved in qigong practitioners. Previous studies have analyzed the impact of qigong on social function and also reported that qigong improved this parameter.12,28 On other SF-36 quality-of-life subscales, as well as sleep and vital sign measurements, there were no significant changes between groups over the course of the study. Other investigations have reported that qigong practice decreased blood pressure and pulse rate.13,14,29
Limitations of this study include the relatively small size of the sample, which may have generated a type II error in quality of life and vital sign measures. In addition, a lengthier exposure to qigong may have produced additional differences between the qigong and control groups; however, the majority of qigong studies on stress and stress-related disorders have been 6–8 weeks in duration. Given that a growing literature is now demonstrating qigong to be effective in reducing stress, future evaluations of qigong will benefit by head-to-head comparisons with other mind–body techniques to determine which approaches are most effective for given populations and treatment settings.
In summary, a randomized, waiting-list controlled, 6-week trial of medical qigong demonstrated a significant reduction in perceived stress in hospital staff. Teaching this technique appears to be feasible even in a high-intensity hospital setting.
Appendix
| Exercise | Acupuncture points of focus | |
|---|---|---|
| #1 | Lung: 1, 2, 7 & Shu points | Large intestine: 4 & Shu points |
| Lung and large intestine | Inhale, raising hands in an arc in front of the body to above the head. Exhale, lowering arms to sides. Inhale, raising hands behind back and attempt to touch elbows. Exhale, extending upward palms in front of body. Inhale, forming a broad tiger claw hand position. Keeping the back straight and upright, squat so that thighs are parallel to the floor. Exhale as you release the tiger claw and return to standing position. Repeat squatting movements twice. | |
| #2 | Stomach: 8, 25 & 36 | Spleen: 3, 4, & 21 |
| Stomach and Spleen | Step back at a 45 degree angle and form a solid stance with 90% of weight on bent rear leg. Inhaling, draw the archerís bow. Exhaling, return to starting position, dragging the large toe along the floor. Repeat this process for opposite side. | |
| #3 | Heart: 1, 2, & 7 | Small Intestine: 4 & 9–17 |
| Heart and Small Intestine | Starting position: Hold tiger claw hand position in front of torso. Inhaling, first raise the shoulders, then elbows and hands along the front of the body. When you can no longer maintain the forearm position parallel to the floor, release the hands and arms straight upward. Exhaling, lower the arms in an arc out to your sides as you rotate your feet at a 45 degree angle and squat downward until the thighs are parallel to the floor, while keeping your back straight. | |
| #4 | Bladder: 9–24 & 59–64 | Kidney: 1–8 |
| Bladder and Kidney | Starting position: Palms facing forward in front of body with elbows straight. Inhaling, first raise the shoulders as high as possible and then the hands along the front of the body. Then, rotate the shoulders so that the fingers point to sides. Simultaneously rotate your feet so toes point outward at a 180 degree angle, keeping your knees straight. Holding your breath, extend your arms then rotate the palms forward. Exhaling, lower your arms in an arc as you squat down until the thighs are parallel to the floor, keeping the back straight. | |
| #5 | Pericardium: 4–7 | Triple Heater: 4–8 |
| Pericardium and Triple Heater | Starting position: Stand upright with palms facing up at side of chest. Step out with your right foot, transferring the majority of your weight to this foot as you bend the right knee and straighten the left knee, simultaneously rotate palms to face toward sides. Inhaling, look at your left middle finger as your press your arms outward from your sides. Exhaling, return to the starting position. Repeat to your left side. | |
| #6 | Gallbladder: 6–11 & Shu point | Liver: Shu point |
| Gallbladder and Liver | Inhaling, raise your arms upward with the elbows straight. Bring the palms toward your eyes, right eye to right palm and left eye to left palm. Rub thumbs in an arc around the ears and then extend the hands straight out, left eye to back of left hand and right eye to back right hand. Exhaling, bend over and stretch the spine at the lower thoracic area. | |
| #7 | Conception Vessel: All points along the conception vessel | |
| Conception Vessel | Starting position: Stand on your right foot with your left off the floor, left knee flexed at a 90 degree angle. Left hand points downward and right hand is positioned as if holding onto a support. Inhaling, simultaneously lean forward as your extend the left hand forward and the left foot behind you, bring the right hand to the midthoracic area. Exhale and repeat at the other side. | |
| #8 | Governing Vessel: All points along the governing vessel | |
| Governing Vessel | Starting position: Feet are ∼2 shoulder widths apart. Bend over and with hands positioned as if holding a ball. Neck is relaxed and head is hanging down. Inhaling, rotate to your left so that you carry the “ball” as far to your left side as possible, keeping the back straight. Exhaling, repeat the process to your right side. | |
Acknowledgment
The authors wish to acknowledge Pamela Staves, C.N.S., N.P. for her assistance with study logistics. This research was supported by the Department of Veterans Affairs VISN 19 MIRECC and by the following grants to Dr. Adler: National Institutes of Mental Health 5RO1 MH050787-10 and Department of Defense DAMD 17-01-1-0760. There are no conflicts of interest to report.
Author Disclosure Statement
Hong Liu holds a copyright to The Basic Eight© qigong set.
References
- 1.Selye H. A syndrome produced by diverse nocuous agents. Nature. 1936;138:32. doi: 10.1176/jnp.10.2.230a. [DOI] [PubMed] [Google Scholar]
- 2.Zubin J. Bonnie S. Vulnerability: A new view of schizophrenia. J Abnorm Psychol. 1977;86:103–126. doi: 10.1037//0021-843x.86.2.103. [DOI] [PubMed] [Google Scholar]
- 3.Melamed S. Ugarten U. Shirom A, et al. Chronic burnout, somatic arousal and elevated salivary cortisol Levels. J Psychosom Res. 1999;46:591–598. doi: 10.1016/s0022-3999(99)00007-0. [DOI] [PubMed] [Google Scholar]
- 4.Luine VN. Beck KD. Bowman RE, et al. Chronic stress and neural function: Accounting for sex and age. J Neuroendocrinol. 2007;19:743–751. doi: 10.1111/j.1365-2826.2007.01594.x. [DOI] [PubMed] [Google Scholar]
- 5.Chow YWY. Tsang HWH. Biopsychosocial effects of qigong as a mindful exercise for people with anxiety disorders: A speculative review. J Altern Complement Med. 2007;13:831–839. doi: 10.1089/acm.2007.7166. [DOI] [PubMed] [Google Scholar]
- 6.Melamed S. Shirom A. Toker S, et al. Burnout and risk of cardiovascular disease: Evidence, possible causal paths, and promising research directions. Psychol Bull. 2006;132:327–353. doi: 10.1037/0033-2909.132.3.327. [DOI] [PubMed] [Google Scholar]
- 7.Wieclaw J. Agerbo E. Mortensen PB. Bonde JP. Risk of affective and stress related disorders among employees in human service professions. Occup Environ Med. 2006;63:314–319. doi: 10.1136/oem.2004.019398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weinberg A. Creed F. Stress and psychiatric disorder in healthcare professionals and hospital staff. Lancet. 2000;355:533–537. doi: 10.1016/S0140-6736(99)07366-3. [DOI] [PubMed] [Google Scholar]
- 9.Taylor C. Graham J. Potts HWW, et al. Changes in mental health of UK hospital consultants since the mid-1990s. Lancet. 2005;366:742–744. doi: 10.1016/S0140-6736(05)67178-4. [DOI] [PubMed] [Google Scholar]
- 10.Liu H. The Healing Art of Qigong. New York: Warner Books; 1999. p. 293. [Google Scholar]
- 11.Skoglund L. Jansson E. Qigong reduces stress in computer operators. Complement Ther Clin Pract. 2007;13:78–84. doi: 10.1016/j.ctcp.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 12.Taylor-Piliae RE. Haskell WL. Waters CM, et al. Change in perceived psychosocial status following a 12-week t'ai chi exercise programme. J Adv Nurs. 2006;54:313–329. doi: 10.1111/j.1365-2648.2006.03809.x. [DOI] [PubMed] [Google Scholar]
- 13.Lee MS. Lee MS. Kim HJ. Qigong reduced blood pressure and catecholamine levels of patients with essential hypertension. Int J Neurosci. 2003;113:1691–1701. doi: 10.1080/00207450390245306. [DOI] [PubMed] [Google Scholar]
- 14.Cheung BMY. Lo JLF. Fong DYT, et al. Randomised controlled trial of qigong in the treatment of mild essential hypertension. J Hum Hypertens. 2005;19:697–704. doi: 10.1038/sj.jhh.1001884. [DOI] [PubMed] [Google Scholar]
- 15.Milliken TF. Clements PT. Tillman HJ. The impact of stress management on nurse productivity and retention. Nurs Econ. 2007;25:203–210. [PubMed] [Google Scholar]
- 16.Cohen S. Kamarck T. Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 17.Ware JE. Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 18.Helms JM. Acupuncture Energetics: A Clinical Approach for Physicians. 1st. Berkeley, CA: Medical Acupuncture Publishers; 2007. p. 757. [Google Scholar]
- 19.Langevin HM. Konofagou EE. Badger GJ, et al. Tissue displacements during acupuncture using ultrasound elastography techniques. Ultrasound Med Biol. 2004;30:1173–1183. doi: 10.1016/j.ultrasmedbio.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 20.Berger BG. Owen DR. Stress reduction and mood enhancement in four exercise modes: Swimming, body conditioning, hatha yoga, and fencing. Res Q Exerc Sport. 1988;59:148–159. [Google Scholar]
- 21.Lee MS. Ryu H. Chung HT. Stress management by psychosomatic training: Effects of ChunDoSunBup qi-training on symptoms of stress. A cross sectional study. Stress Med. 2000;16:161–166. [Google Scholar]
- 22.Lane JD. Seskevich JE. Pieper CE. Brief meditation training can improve perceived stress and negative mood. Altern Ther. 2007;13:38–44. [PubMed] [Google Scholar]
- 23.Joseph CN. Porta C. Casucci G, et al. Slow breathing improves arterial baroreflex sensitivity and decreases blood pressure in essential hypertension. Hypertension. 2005. www.hypertensionaha.org. [May 24;2007 ]. www.hypertensionaha.org [DOI] [PubMed]
- 24.Lee MS. Kang CW. Lim HJ. Lee MS. Effects of qi-training on anxiety and plasma concentrations of cortisol, ACTH, and aldosterone: A randomized placebo-controlled pilot study. Stress Health. 2004;20:243–248. [Google Scholar]
- 25.Dundee JW. Ghaly RG. Fitzpatrick KTJ. Acupuncture prophylaxis of cancer chemotherapy-induced sickness. J R Soc Med. 1989;82:268–271. doi: 10.1177/014107688908200508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim KS. Nam YM. The analgesic effects of capsicum plaster at the Zusanli point after abdominal hysterectomy. Int Anesth Res Soc. 2006;103:709–713. doi: 10.1213/01.ane.0000228864.74691.9f. [DOI] [PubMed] [Google Scholar]
- 27.Irwin M. Olmstead R. Oxman M. Augmenting immune responses to varicella zoster virus in older adults: A randomized, controlled trail of t'ai chi. Am Geriatr Soc. 2007;55:511–517. doi: 10.1111/j.1532-5415.2007.01109.x. [DOI] [PubMed] [Google Scholar]
- 28.Tsang HWH. Cheung L. Lak DCC. Qigong as a psychosocial intervention for depressed elderly with chronic physical illnesses. Int J Geriatr Psychiatry. 2002;17:1146–1154. doi: 10.1002/gps.739. [DOI] [PubMed] [Google Scholar]
- 29.Tsai JC. Wang WH. Chan P, et al. The beneficial effects of t'ai chi chuan on blood pressure and lipid profile and anxiety status in a randomized controlled trial. J Altern Complement Med. 2003;9:747–754. doi: 10.1089/107555303322524599. [DOI] [PubMed] [Google Scholar]