Abstract
Background
Very little research has been conducted in the West to evaluate the clinical efficacy of Japanese acupuncture (JA). The characteristics that define and differentiate JA from Chinese acupuncture styles add specific challenges to the operationalization of treatment protocols for use in clinical trials.
Objectives
To develop an ecologically valid and viable multimodal treatment intervention, including active and sham protocols, for use in a pilot randomized sham-controlled trial of a style of JA in treating endometriosis related chronic pelvic pain in adolescents and young women.
Methods
A focus group format was used to systematize the diagnostic framework, operationalize the intake, design the treatment protocols, and develop a viable and effective sham acupuncture intervention using the Streitberger device and sham moxibustion. Implementation of the treatment protocol employed the manualization process to provide flexibility of treatment while assuring replicability and standardization.
Setting
The Japanese Acupuncture Department at the New England School of Acupuncture in Newton, MA.
Results
Completed study visit forms indicated good compliance of study practitioners with active and sham treatment protocols. The specific JA protocols used in our pilot study were well tolerated by the adolescent girls who participated in the trial. No serious adverse events were reported by any participants. Our protocols were successful in maintaining patient blinding and minimizing differences in outcome expectations between treatment groups.
Conclusions
Manualization provided a viable method for conforming to the interactive nature of JA treatments, yet facilitated compliance with a replicable treatment protocol. Sham controls of complex, multicomponent JA interventions pose unique challenges. The modified Streitberger needle in conjunction with sham moxibustion showed promise as a viable control in clinical trails of JA; both components of this sham protocol require further validation.
Introduction
In contrast to Traditional Chinese Medicine (TCM) acupuncture, very little research has been conducted in the West to evaluate the clinical efficacy of Japanese Acupuncture (JA). Several common characteristics define and differentiate JA, which encompasses many different treatment styles. These characteristics add their own set of challenges to the operationalization of treatment protocols for use in clinical trials and include (1) Emphasis on the use of palpation; (2) gentler needling techniques; (3) the use of thinner needles, and milder, shallower stimulation; (4) immediate confirmation of effects of treatment and continuous adjustment based on direct patient feedback; and (5) the use of adjunctive techniques to reinforce the primary treatment.
To evaluate the clinical efficacy of a JA intervention that reflects actual clinical practice, treatments need to be adjusted to the unique clinical configurations of each participant, while providing treatment protocols that can be replicated. Manualization of treatment protocols is one method that has been used extensively in clinical trials of TCM style acupuncture1–3 to accomplish flexibility and standardization; yet no JA studies to date have employed manualization. JA presents specific additional challenges to the manualization process.
Manualization involves the development of a treatment manual to guide the implementation of a protocol in a particular study by providing both the background and rationale for the selection of a clinical framework, and the step-by-step guidelines for its implementation. Manualization allows practitioners to adjust acupuncture treatments to study participants' unique diagnoses, allowing the delivery of ecologically valid treatments within a predefined framework that can be replicated. The treatments are “standardized” not by the selection of fixed point formulae, but by providing an algorithm that can be adapted to each patient.
As part of a pilot, randomized, sham-controlled study to evaluate the potential application of JA in treating endometriosis-related chronic pelvic pain in young women,4 we designed a multimodal intervention based on a style of JA. In addition, we designed a parallel sham control employing the nonpenetrating Streitberger sham needling device5 and sham moxibustion. In this paper, we summarize the rationale and design of the JA and sham acupuncture protocols and the development and use of a JA manualized approach.1 In addition, we present modifications to the use of the Streitberger sham needle device to better comply with the JA treatment framework. Finally, we discuss more general challenges to the design and implementation of a viable control in clinical trials of JA.
Background and Rationale
Several studies have evaluated acupuncture for gynecological conditions including endometriosis and dysmenorrheal,6–9 and a growing body of research suggests that acupuncture is well received by adolescents and their families.10–13 No definitive studies, however, have been conducted in the West evaluating Japanese acupuncture (JA) for pelvic pain, or specifically for chronic pain in adolescents.
The treatment protocols discussed in this paper were developed for a prospective, randomized sham-controlled trial with blinding of patients (n = 18) and outcome assessors. Young women ages 13–22 diagnosed with endometriosis with persisting pelvic pain received 16 acupuncture treatments (JA or sham), twice per week for 8 consecutive weeks. Treatments were administered by 7 licensed acupuncturists with formal training in JA. Further details regarding the study design, outcome measures, and results of the clinical trial are presented elsewhere.4
Manualization of Individually Tailored Acupuncture Treatments
According to JA, for any given biomedical condition (e.g., chronic pelvic pain [CPP]), the clinical presentation is determined by individual patient differences. Consequently, the optimal treatment strategy will also vary from patient to patient, and using 1 fixed treatment protocol for all study participants could underestimate the potential value of acupuncture therapy.3 To allow for flexible, dynamic, individually tailored JA treatments as practiced in a clinical setting, while at the same time assuring replicability and standardization, we developed a treatment approach based on the manualization process.1 We employed manualization in this study not only to conform to the interactive nature of JA treatments, but also to assure compliance with the treatment guidelines, to train and supervise acupuncture providers on implementation of the protocol, and to improve consistency and inter-rater reliability among practitioners.
The protocol was based on the JA curriculum currently taught at New England School of Acupuncture (NESA); it was developed in conjunction with the JA department cochairs (D.I. and J.K.) at NESA, and with 2 other senior acupuncturists from the community, 1 with specific experience of treating CPP in this patient population, and 1 with extensive experience in JA (n = 4). We conducted a series of structured planning meetings using a focus-group format.14 A researcher (R.S.) with expertise in manualization led the overall process. During these meetings, the research and clinical teams discussed the potential effectiveness of JA styles in treating this condition, the systematization of the diagnostic framework, structure of intake, treatment protocols, type of stimulation, and the design of a viable and effective sham acupuncture intervention and sham moxibustion in JA. The information collected in these meetings was organized into a treatment manual. Acupuncturists who subsequently participated in this study were trained with the help of the manual on the implementation of the JA and sham interventions in a controlled research setting.
Japanese Acupuncture Protocol
The style of JA employed in this study derives from classical acupuncture texts and emphasizes a channel-based treatment that incorporates two complementary styles of JA. Primarily, we used an adaptation of Shima's15 treatment of the secondary channels including the use of divergent channels and extra channel polarizations, in combination with a technique developed by Shima himself that integrates the use of auricular points16 with secondary channels. Our approach differs from Shima's by incorporating Manaka's empirical use of abdominal conformations and additional channel combinations17 not included in Shima's protocols. An outline of the key features of the JA and sham protocols employed in our trial is presented in Table 1.
Table 1.
Key Features of the Japanese Acupuncture and Sham Protocols
| Protocol component | Japanese acupuncture protocol | Rationale/reason | Sham protocol |
|---|---|---|---|
| Questioning | short questionnaire and comprehensive patient interview | To ascertain presenting symptoms and to assess the patient's experience of her illness | Short questionnaire and comprehensive patient interview. Identical to JA arm. |
| Diagnosis | |||
| Palpation: | |||
| i. Pulse | Taken at the radial artery in 3 positions on each wrist | Evaluate the state of health of the body. Helps practitioner to assess the state of the qi and blood. Special emphasis placed on determining deficiency or excess of channels. | Pulse not palpated |
| ii. Abdominal | Palpating the condition of the skin, muscles, and subcutaneous tissues. Yoshio Manaka's style emphasizes palpation of specific diagnostic points (Mu points) located on the front of the body. | Helps confirm the Extraordinary Vessels Diagnosis | Abdomen not palpated |
| Testing the jing-well points with the Hibiki-7 device | Hibiki-7: a device to measure electrical impedance on the skin of the jing-well points (located on the fingers and toes). Numerical index is obtained; numerical values are compared between left and right sides of the body, added to obtain TNV for the entire channel. A deviation is obtained by comparing TNVs to the right/left values of other related channels. | Determines the left/right imbalances of acupuncture channels. Used to obtain information about the Channel Divergences, the Extraordinary Vessels, and lateral imbalances (left/right). Modeled after Miki Shima style, Hibiki findings are emphasized and abdominal confirmation and pulses are used to corroborate and complement Hibiki findings. | Testing with the Hibiki is done the same as in the active arm. Identical to JA arm. |
| Treatment | |||
| Jing-well points | Any jing-well points with readings >20 are treated using the Hibiki-7 machine until they register <20 | For Hibiki-7 measurements at jing-well points, any reading between 10 and 20 is normal. Readings >20 or <5 must be treated with the Hibiki-7. | Jing-well points not treated with Hibiki-7 |
| CDsa | The 2 most deficient CDs, as determined from the Hibiki readings, are chosen for treatment using the appropriate polarity (gold needles to tonify; stainless steel needles to disperse). Additional abdominal point located off of an acupuncture meridian selected and cleaned with alcohol. Placebo needle is placed at abdominal point to help maintain blinding. | Divergent Channels act as an axis between the interior and exterior of the body. If a CD is found to be deficient, its job of directing OPIs away from the organs of the body may be disabled and the OPI may penetrate deeper into the body. | Four body points located off acupuncture channels are selected, cleaned and “needled” with Streitberger device to “treat” the EVs and CDs |
| EVsa | The 3 most deficient EVs, as determined from the Hibiki readings and corroborated by the abdominal findings, are chosen for treatment using the appropriate polarity (gold needles to tonify; stainless steel needles to disperse) | According to Manaka, the 8 EVs are thought to supplement the deficiencies of the other channels and distribute the body's qi (essential energy) at deeper levels.17 Hence, treating the EVs supplements the energy of the whole body. | Practitioner does not attach the clip of the Hibiki-7 machine to one of the body needles as in the active protocol. Practitioner holds patient's ear. Hibiki-7 probe is held near the ear, but no ear points are stimulated. Practitioner touches the Hibiki-7 probe to elicit noise. |
| Auricular | Toward the end of the first phase of the treatment, while the CD and EV needles are still in, up to 5 ear points appropriate to the patient's presenting symptoms are stimulated in each ear with the Hibiki-7 machine | Stimulation of auricular points corresponding with a patient's symptoms has been empirically proven to produce pain relief. Shima has used it extensively as an adjunctive treatment to an overall channel divergence strategy.15 | |
| Back shu points | The back shu points corresponding to the channels found to be most deficient (readings >20) in the Hibiki readings are treated on the appropriate side with a form of moxibustion called okyū Three rounds of okyū are done on these points. | Tonifies the qi of the most deficient organs of the body | Shiunko burn cream is applied at 3–5 randomly selected “points” located off any channel on the back. Small threads of moxibustion ōkyu are placed on the cream. The moxa is not lit, but the incensed is waved above it, to provide smell and attention but no or minimal thermal stimulation. Each point on the back is “treated” with 3 okyūs |
| Local treatment (Dr. Hara) | Eight points are palpated along a triangle on the sacrum for pressure pain or indurations and are then marked with shiunko cream (a burn cream). Three okyūs are applied at each point. | Local treatment for pelvic pain due to endometriosis | Shiunko cream is applied at 8 points selected at random without palpation along a triangle on the sacrum. After ōkyu is placed on the shiunko, an incense stick is waved over the ōkyu without lighting it, as described above. Each point is “treated” with 3 okyūs. |
Needles for both the CDs and the EVs are inserted simultaneously and are retained for approximately 15–20 minutes; TNV, total numerical values.
JA, Japanese acupuncture; CD, channel divergences; OPIs, Outside Pathogenic Influences; EV, extraordinary vessels.
The focus of the diagnosis was placed on palpatory findings, especially the abdomen and pulse, as well as an assessment of the flow of the channels by measuring electrical impedance (EI) on the skin at specific acupuncture points (jing-well points). Testing of EI was conducted using a Hibiki-7 device (Asahi Butsuryooki Research Lab; Kita Kyoto, Japan). Treatment focused on addressing the root (underlying predisposition) and the branch (symptomatic presentation). Shallow and light needling stimulation (1–2 mm) using fine needles (0.18–0.16 mm) inserted with the aid of insertion tubes was emphasized. Points were needled at a 10°–20° angle with a 2-hand needling technique, generally in the direction of the flow of the channel. In contrast with TCM style acupuncture, we did not employ vigorous manipulation in order to elicit a strong de qi sensation (defined as a feeling of heaviness around the acupuncture point).18 Practitioners focused instead on feeling the response to stimulation as an “echo” sensation experienced on the receiving hand, while the active hand performed the actual needling. Attention was placed on reactivity or change in diagnostic areas, especially the pulse and abdomen. By carefully assessing changes in palpatory findings, the treatment was adjusted continuously based on the patient's response. Before needling, the “live” points were identified by palpation, that is, subtle changes at the skin level, or upon touch or pressure, for that particular patient; the anatomical location of acupoints was used as a reference to find the “live” points. Rather than based exclusively on point function according to theory, points were selected based on changes elicited during examination.
In addition to needling, moxibustion or thermal stimulation of the acupoints was used forming very fine wool of mugwort (Artemisa vulgaris) into minute, thread-size punks (okyū) and placing them on a thin layer of an herbal cream (shiunko). The moxa was lit with an incense stick and the process was repeated several times until warmth was felt by the patient.
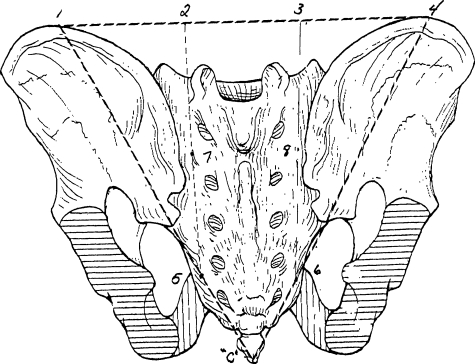
Each treatment consisted of 4 broad steps: (1) treatment of the divergent channels (DC) based on EI findings at jing-well points; (2) treatment of the extraordinary vessels and other extra channel polarizations (i.e., TaiYin, ShaoYin, etc.) based on abdominal conformation and EI findings; (3) treatment of auricular points; and (4) treatment of the symptom (i.e., chronic pelvic pain) by selecting local points (i.e., on the sacrum). In steps 1 and 2, gold (to supplement) and silver needles (to disperse) were used to create a polarity. Needles were retained for 15 minutes and moxa was used to reinforce the treatment strategy. In step 3 (last few minutes of treatment), auricular points with a functional correspondence to pelvic pain (i.e., uterus point) were checked for reactivity with the use of the Hibiki machine; up to 5 auricular points were treated by connecting them to 1 of the points in Step 1 (i.e., the master point of the appropriate DC) and stimulating them with the Hibiki until reactivity was reduced. Step 4 consisted of the application of 3 moxa threads at each of the 8 “Dr. Hara's points” (Fig. 1).
FIG. 1.
The 8 Hara points are located on the sacrum. Four (4) points are located horizontally in line with the fifth lumbar vertebra and 4 points are on 2 parallel lines roughly corresponding to the second and fourth sacral foramina.
Design of the Sham Japanese Acupuncture Control Protocol
Assessment
The control acupuncture protocol aimed to replicate the steps used in the JA treatment (Table 1)while providing not an inert but a minimally active intervention. The diagnosis component of the sham protocol differed from the JA in the lack of palpation of the abdomen and pulse. Measurement of the jing-well points and verbal interaction remained the same between the 2 groups.
Needling
To control for the needling component of the JA protocol, we used the Streitberger sham acupuncture device5 with some significant modifications. The Streitberger device has a retractable, dull needle head. The patient sees and feels the acupuncture needle penetrate their body but instead the needle goes up the needle shaft. A plastic ring is taped over on the acupuncture point to be treated and is used both with sham and JA treatments; this enables the sham needle to stand stationary like a true needle. The real and sham needles look and feel identical: The only difference is that the real needle penetrates the skin while the sham needle does not. We reported no acupuncture-related adverse events with the use of this device.4
The Streitberger device has been previously validated19 but not in JA trials. Since in JA minimal contact of needles with the skin is believed to be therapeutic, we conducted a preliminary evaluation of this device to modify it by eliminating direct skin contact and minimizing stimulation. Our JA experts were blindfolded while exploring a number of modifications to its suggested use. Our team concluded that by placing a fitted circular piece of plastic electric tape at the base of the O-ring (between the needle tip and skin), the pressure provided by the tip of the needle was blunted and dispersed over a larger surface area; the electrical tape barrier seemed to minimize possible therapeutic effects, as assessed by instantaneous feedback of radial pulses. In the JA acupuncture arm, we did not use the Streitberger ring.
Point selection
Specific points used in the control arm were selected to mimic the anatomical distribution and number of points used in the JA arm. All locations selected for application of the sham needle were nonacupuncture points off acupuncture channels. All nonactive points were located 1 cun (width of thumb) proximal or distal, lateral or medial to real points and 0.5–1 cun from any other verum points.
We took additional measures to best control for other non-needling components of treatment. Although the assertion that “nonlive” points are less active has not been tested experimentally, we aimed to minimize any stimulation of the channels: Practitioners were instructed to keep 1 cun away from any active points in all directions, palpation was not used for finding nonactive points, and to avoid inadvertently focusing intention on a specific site that could bring qi to the area, potentially making the point more “active,” specific guidelines on how to find nonactive points were not given to practitioners. Extensive training on the effective and skillful use of the Streitberger needle20 was provided.
Furthermore, to prevent unblinding of the participants by unforeseen communication between patients, all participants including those in the JA arm received 1 sham needle in the abdomen, using the ring and tape; participants with previous acupuncture experience were excluded. Table 2 provides 4 examples of the anatomical relationship between JA and sham points.
Table 2.
A Sample of Location of Nonchannel Points (Sham Points) in Relation to Actual Acupuncture Channel Points
| Actual acupuncture point | Location nonchannel points | Actual acupuncture point | Location nonchannel points |
|---|---|---|---|
| Sp 6 | 5 cun above the medial malleolus, 1 cun medial to the Lv channel | P 6 | 1 cun medial and 1 cun proximal to P 4, about 1 cun lateral to the Heart channel |
| Sp 10 | 4 cun above the superior medial border of the kneecap on top of the thigh. | Sp 4 | 1 cun lateral and 1 cun proximal to the actual point, on top of the head of the first metatarsal bone |
Sham moxibustion
In the control arm, a relatively inert sham moxibustion intervention was accomplished by using an extra layer of protective (shiunko) cream and by waving the incense above the moxa but not lighting it. This method resulted in minimal—if any—thermal stimulation of the body surface, but retained the smell of the incense and moxa, as well as the attention associated with the JA arm. All sham moxibustion was performed outside the patient's field of vision (all moxa points were located on the back).
Sham ear acupuncture
The sham ear acupuncture component of the protocol consisted of holding the Hibiki-7 probe near the ear, without stimulating any ear points, while the practitioner held the patient's ear. To elicit the sound associated with Hibiki stimulation of the ear, the practitioner touched the Hibiki-7 probe to his own hand; the clip of the Hibiki-7 machine was not attached to one of the body needles.
Discussion
While a number of prior clinical trials evaluating TCM acupuncture have used manualized protocols, this is first study we are aware of that manualizes a JA protocol. Our study suggests that manualization of complex, multimodal, interactive treatment interventions such as JA for research purposes is feasible. Completed study visit forms indicated good compliance of study practitioners with JA and sham treatment protocols.
The specific JA protocols used in our pilot study were well tolerated by the adolescent girls who participated in the trial. No serious adverse events were reported by any participants.4 Qualitative interviews with study participants suggest that treatments were comfortable, not painful, and generally enjoyable.* Moreover, once enrolled, 14 of the 18 participants completed the study, per protocol.4 Our protocols were successful in maintaining patient blinding and minimizing differences in outcome expectations between treatment groups; data on blinding have been published elsewhere.4 The results of our pilot study suggest that the JA protocol we developed shows promise for managing endometriosis-related chronic pelvic pain in young women and should be further evaluated.*
Our modifications to the use of the Streitberger sham device warrant specific comment. This and other retractable devices are becoming an increasingly popular choice as sham controls in acupuncture studies. Although they have been validated as controls for certain styles of acupuncture,3,19,21 their use may not be generalizable to all styles. It is still debatable whether the Streitberger needle or other retractable acupuncture devices are in fact inert. It has been argued that by producing an acupressure effect, these devices may compromise the validity of the control, even when used over nonacupuncture points.22 This is a consideration, especially in JA, where very subtle needling techniques are used and the slightest point stimulation is meant to have an effect.22 Another limitation of these retractable devices is that they potentially compromise the ability of the practitioners to provide effective treatment. The use of this device requires that the plastic rings also be used in the acupuncture arm, which limits skillful manipulation of the needles; for this reason we chose against using these rings in the JA arm. Extensive training of the practitioners should be provided for efficient and effective use of this device.
Our modifications in the use of the Streitberger needle (i.e., use of plastic barrier under the O-ring to minimize acupressure effects and elimination of O-rings in JA arm) were necessary to conform to the principles of JA. They allowed practitioners to administer a minimally active, if not inert, sham intervention, and a more ecologically valid JA intervention consistent with real-life practice. Both of these assumptions can and should be further evaluated: the first experimentally and the second using qualitative methods and practitioner interviews.
Our sham moxibustion protocol also warrants comment. Few studies have described the use of a sham moxibustion intervention. To our knowledge, our protocol is the first to develop a sham control for thread moxibustion. As with the adaptations of the Streitberger needle for JA, further testing should be conducted to confirm the validity of this component of the protocol.
Our protocol reflects some important weaknesses. First, the reliability of the Hibiki in measuring EI has not been established. Although we strived to design a minimally active sham intervention, it was not intended to be and cannot be considered a truly inert placebo. While measuring the points, the Hibiki provides significant electrical input even at low settings; therefore, the measurement itself delivers some stimulation. Second, the use of shunkio cream—a therapeutic herbal cream—as part of the sham acupuncture component may have delivered some unexpected therapeutic and thermal effects, even though participants did not report feeling any heat. Some stimulation may have also been provided by the practitioner when applying pressure on his or her own skin to elicit the Hibiki sound, while holding the participant's ear.
One unexpected challenge was the great difficulty and ethical conflict experienced by some of the JA practitioners with respect to providing treatment in a controlled experimental setting. Practitioners often face difficulty and conflict of interest when asked to perform sham procedures.23 Acupuncturists who have participated in other clinical trials of acupuncture involving the administration of sham treatments have reported feeling “uncomfortable,” “deceitful,” “hypocritical,” and significant ethical “tension between their patient-focused training and their roles as scientific investigators.”24 Although acupuncturists in our study received training that included discussion of potential challenges, the successful compliance with treatment protocol required consistent support from the administrative team. Strategies for coping with perceived ethical issues are critical for the successful completion of a sham controlled acupuncture trial.24
Conclusions
Manualization provided a viable method for conforming to the interactive nature of JA treatments, yet facilitated compliance with a replicable treatment protocol. The specific JA protocol employed in this study was well tolerated by adolescent girls and young women, and warrants further research as an intervention for endometriosis-related pelvic pain. Sham controls of complex, multi-component interventions continue to pose unique challenges. The modified Streitberger needle in conjunction with sham moxibustion showed promise as a viable, but not necessarily inert, control in clinical trails of JA; both components of this sham protocol require further validation. Finally, translating acupuncture clinical skills into the research setting requires careful training and supervision of the participating clinicians, and should not be underestimated.
Footnotes
Conboy L, Quilty M, Catherine K, et al. A qualitative analysis of adolescents' experiences of active and sham Japanese-style acupuncture protocols administered in a clinical trial (2008; in press).
Acknowledgments
This project was supported by grant number 5 U19 AT002022 from the National Center for Complementary and Alternative Medicine. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Center for Complementary and Alternative Medicine, or the National Institutes of Health. We thank Bella Rosner and Ellen Highfield for their participation in the development of the protocol and providing treatments; we also thank Kate Billings, Susan Panarese, Rachel Hartstein, and Eileen Power for providing treatments. We also thank Julie Buring, Roger Davis, Ellen Connors, and Andrea Hrbek for their assistance with this project.
References
- 1.Schnyer RN. Allen JJ. Bridging the gap in complementary and alternative medicine research: Manualization as a means of promoting standardization and flexibility of treatment in clinical trials of acupuncture. J Altern Complement Med. 2002;8:623–634. doi: 10.1089/107555302320825147. [DOI] [PubMed] [Google Scholar]
- 2.Schnyer RN. Conboy LA. Jacobson E, et al. Development of a Chinese medicine assessment measure: An interdisciplinary approach using the delphi method. J Altern Complement Med. 2005;11:1005–1013. doi: 10.1089/acm.2005.11.1005. [DOI] [PubMed] [Google Scholar]
- 3.Schnyer RN. Wayne PM. Kaptchuk TJ, et al. Standardization of individualized treatments in a randomized controlled trial of acupuncture for stroke rehabilitation. J Altern Complement Med. 2006;12:106–109. doi: 10.1089/acm.2006.12.106. [DOI] [PubMed] [Google Scholar]
- 4.Wayne P. Kerr C. Schnyer R, et al. Japanese-style acupuncture for endometriosis-related pelvic pain in adolescents and young women: Results of a randomized sham-controlled trial. J Pediatr Adolesc Gynecol. 2008 doi: 10.1016/j.jpag.2007.07.008. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Streitberger K. Kleinhentz J. Introducing a placebo needle into acupuncture research. Lancet. 1998;352:992. doi: 10.1016/S0140-6736(97)10471-8. [DOI] [PubMed] [Google Scholar]
- 6.Helms J. Acupuncture for the management of primary dysmenorrhea. Obstet Gynecol. 1987;69:51–56. [PubMed] [Google Scholar]
- 7.Highfield ES. McLellan MC. Kemper KJ, et al. Integration of complementary and alternative medicine in a major pediatric teaching hospital: An initial overview. J Altern Complement Med. 2005;11:373–380. doi: 10.1089/acm.2005.11.373. [DOI] [PubMed] [Google Scholar]
- 8.Xiang D, YS. Liang X, et al. Ear acupuncture therapy for 37 cases of dysmenorrhea due to endometriosis. J Tradit Chin Med. 2002;22:282–285. [PubMed] [Google Scholar]
- 9.Zhan C. Treatment of 32 cases of dysmenorrhea by puncturing hegu and sanyinjiao acupoints. J Tradit Chin Med. 1990;10:33–35. [PubMed] [Google Scholar]
- 10.Lee AC. Highfield ES. Berde CB. Kemper KJ. Survey of acupuncturists: Practice characteristics and pediatric care. West J Med. 1999;171:153–157. [PMC free article] [PubMed] [Google Scholar]
- 11.Kemper KJ. Sarah R. Silver-Highfield E, et al. On pins and needles? Pediatric pain patients experience with acupuncture. Pediatrics. 2000;105(4 Pt 2):941–947. [PubMed] [Google Scholar]
- 12.Ottolini MC. Hamburger EK. Loprieato JO, et al. Complementary and alternative medicine use among children in the Washington, DC area. Ambul Pediatr. 2001;1:122–125. doi: 10.1367/1539-4409(2001)001<0122:caamua>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 13.Zeltzer LK. Tsao JC. Stelling C, et al. A phase I study on the feasibility and acceptability of an acupuncture/hypnosis intervention for chronic pediatric pain. J Pain Symptom Manage. 2002;24:437–446. doi: 10.1016/s0885-3924(02)00506-7. [DOI] [PubMed] [Google Scholar]
- 14.Powell RA. Single HM. Focus groups. Int J Qual Health Care. 1996;8:499–504. doi: 10.1093/intqhc/8.5.499. [DOI] [PubMed] [Google Scholar]
- 15.Shima M. Chace C. The Channel Divergences: Deeper Pathways of the Web. Boulder: Blue Poppy Press; 2001. [Google Scholar]
- 16.Oleson T. Auriculotherapy Manual: Chinese and Western Systems of Ear Acupuncture. Edinburgh: Churchill Livingstone; 2002. [Google Scholar]
- 17.Manaka Y. Itaya K. Birch S. Chasing the Dragon's Tail: The Theory and Practice of Acupuncture in the Work of Yoshio Manaka. Boston: Paradigm Publications; 1995. [Google Scholar]
- 18.Langevin HM. Churchill DL. Fox JR, et al. Biomechanical response to acupuncture needling in humans. J Appl Physiol. 2001;91:2471–2478. doi: 10.1152/jappl.2001.91.6.2471. [DOI] [PubMed] [Google Scholar]
- 19.Kleinhenz J. Streitberger K. Windeler J, et al. Randomised clinical trial comparing the effects of acupuncture and a newly designed placebo needle in rotator cuff tendinitis. Pain. 1999;83:235–241. doi: 10.1016/s0304-3959(99)00107-4. [DOI] [PubMed] [Google Scholar]
- 20.McManus C. Schnyer R. Kong J, et al. Sham acupuncture devices: Practical advice for researchers. Acupunct Med. 2007;25:36–40. doi: 10.1136/aim.25.1-2.36. [DOI] [PubMed] [Google Scholar]
- 21.Schneider A. Enck P. Streitberger K, et al. Acupuncture treatment in irritable bowel syndrome. Gut. 2006;55:649–654. doi: 10.1136/gut.2005.074518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schnyer R. Chambers AS. Hitt SK, et al. Acupuncture for major depressive disorder: Uncovering evidence for efficacy in one trial highlights the challenge of research designs. J Affect Disord. 2007;68:1617–1618. [Google Scholar]
- 23.Miller FG. Kaptchuk TJ. Sham procedures and the ethics of clinical trials. J R Soc Med. 2004;97:576–578. doi: 10.1258/jrsm.97.12.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McManus C. Kaptchuk T. Schnyer R, et al. Experiences of acupuncturists in a placebo-controlled, randomized clinical trial. J Altern Complement Med. 2007;13:533–538. doi: 10.1089/acm.2007.6309. [DOI] [PubMed] [Google Scholar]