Abstract
Objective
To study the relationship of waist circumference (WC) and bioelectrical impedance analysis (BIA) and degree of agreement between anthropometric index (AI) and BIA, using BIA as a reference or ‘gold standard’. The second objective is to study the relationship between body mass index (BMI) and BIA in subjects with spinal cord injury (SCI).
Study design
Comparative cross-sectional study.
Setting
Convenience sample at outpatient clinic of spinal cord center.
Outcome measures
Estimation of obesity was made in 23 men with motor complete paraplegia (>1 year post-injury). Bland and Altman statistics were used to define level of agreement between AI and BIA, Pearson's r to describe correlation between WC and BIA and BMI and BIA.
Results
Good agreement between BIA and AI with a small systematic difference in fat mass (FM) (mean difference: −0.28%, Pearson's r: 0.91) was found. The correlation between WC and the BIA (% FM) was very high (Pearson's r: 0.83). The correlation between WC and BMI (% FM) was just over moderate (Pearson's r: 0.51).
Conclusion
AI seems to be a valid proxy measure to estimate obesity in males living with SCI. Measurement of obesity in persons with SCI based on WC is promising. BMI showed not to be valid to estimate obesity in persons with SCI.
Keywords: Spinal cord injuries, Obesity, Anthropometrics, Body mass index, Bioelectrical impedance analysis
Introduction
Obesity has become a major health problem in the last decades, reaching epidemic proportions.1,2 It is associated with a higher prevalence of a wide range of co-morbidities3 such as cardiovascular disease (CVD), hypertension, type 2 diabetes mellitus, dyslipidemia, certain forms of cancer, sleep apnoea, and osteoarthritis and is associated with a higher risk of mortality. Central obesity in particular is a strong risk factor of metabolic complications for instance hyperinsulinemia and dyslipidemia.4,5 Besides these medical complications, associations between obesity and reduced quality of life, low self-esteem, and poor life satisfaction have been observed.6,7
The epidemic proportions of obesity has affected not only the able-bodied population, but also persons with disabilities,8 including those with a spinal cord injury (SCI). In studies in persons with SCI, prevalence of obesity varies from 40 to 66%.9–11
After SCI, changes in body composition (reduction in muscle mass), changes in metabolic rate, and limited mobility might lead to an increased prevalence of obesity in this population.10 Reported medical consequences of obesity in persons with SCI include, for example, pulmonary embolism,12 metabolic syndrome,13 and CVD.14,15 The prevalence of CVD in the SCI population has surpassed the prevalence rates of the able-bodied population.16
Due to the many deleterious effects of obesity on health, an adequate monitoring and management of obesity in persons with SCI is of utmost importance.
Good management of obesity starts with a reliable and valid assessment with a practical and feasible measurement in day-to-day practice. In persons with SCI, this is a major challenge. Existing valid methods to estimate obesity in subjects with SCI are neither practical nor feasible for day-to-day measurement. Examples of such methods are dual-energy X-ray absorptiometry17 and hydrostatic weighting,18 both being expensive, in most clinics not available and placing a high burden on personnel and patients. The World Health Organization (WHO) advocates use of the body mass index (BMI = kg/m2) which is the most useful population-level indicator of obesity for able-bodied persons. Although BMI is not a direct measure of body fat, it is a more accurate indicator of overweight and obesity than relying on weight alone. In the able-bodied population, overweight is defined as a BMI of 25–29.9 kg/m2 and obesity as a BMI of ≥30.0 kg/m2. On the one hand, the use of the BMI in persons with SCI has been found to underestimate obesity15,19–21 and therefore, may fail to identify truly obese persons in this specific population. On the other hand, lowering the BMI cut-offs has shown to better identify obese persons with SCI21 and advocated as a screening method. However, another problem in using BMI in the SCI population is the feasibility of measuring weight and height which require special equipment and high-level skills. For example, a special wheelchair scale is needed to assess the weight of wheelchair-dependent persons. For the measurement of height, an accurate and reliable measurement is still lacking. Height can be measured in supine with the legs straight, feet placed in dorsal flexion and head in Frankfurt plane. However, in many persons with SCI this may be difficult because of existing joint contractures or spasticity. Thus, although the BMI appears to be an attractive approach, it seems that it is a suboptimal assessment to screen for obesity in the SCI population. Nevertheless, due to a lack of other alternative measures, BMI is still applied in clinical management and research in persons with SCI.22
A method, advocated to be feasible and valid to asses obesity in persons with SCI in day-to-day practice is bioelectrical impedance analysis (BIA).23 BIA measures the resistance of body tissues to an electric current. The resistance between the conductors provides a measure of body fat since the resistance to electricity varies between adipose, muscular, and skeletal tissue. Women with >40% and men with >27% body fat are considered obese (example for the age group of 41–60 years). It has been shown that BIA underestimates fat mass in persons with SCI.23 After adding a prediction equation including age, sex, height, and weight to the BIA data, the method has shown to be valid for defining fat mass in persons with SCI and therefore, can be used as reference method or so called ‘gold standard’.19 However, although advocated as a bedside method and requiring minimal technical expertise, this method uses special equipment; patients need to avoid exercise, caffeine, and alcohol for 24 hours and fast 12 hours before measurement, which makes the method less suited for daily practice.
An easier way to estimate obesity is the measurement of waist circumference (WC). WC is measured in centimeters and was shown to be accurate to predict obesity in the able-bodied population. Persons with a WC >35 inches/88 cm for women and >40 inches/102 cm for men are defined as obese by the National Institutes of Health (http://www.nhlbi.nih.gov). In the SCI population, the measurement of WC to determine obesity has been rarely used.15,24–26 A study on the use of WC as a marker for obesity by Buchholz and Bugaresti.15 in 2005 showed that WC has not been validated as a surrogate measure of visceral adipose tissue. Edwards et al.25 used WC to match participants in a study on 31 persons (15 with SCI) to compare different outcomes on adipose tissue and studied the reproducibility of measuring WC. WC was measured in supine after normal expiration at three locations: immediately below the lowest rib, immediately above the iliac crest, and midpoint between the lowest rib and the iliac crest. Measurements were taken twice and if necessary a third measurement was obtained. Reproducibility of WC measurements was very high. The intraclass correlation coefficient was r = 0.999 (95% CI 0.998:0.999) for all three locations.25
Another possibly useful method for day-to-day practice to estimate obesity in persons with SCI was described in the study of Bulbulian et al.27 In their study, the use of an anthropometric index (AI) was studied in 22 men with paraplegia.27 The AI is based on the estimation of body density (Db) using chest diameter, sub-scapular skin fold, and waist and calf circumference based on the following equation: (Db = 1.09092 + 0.00296 chest diameter – 0.72 sub scapular skin fold – 0.00182 waist circumference + 0.00124 calf circumference). Using a SIRI-equation, fat mass can be estimated (Fat (%) = 4.95/Db-4.5)28 Bulbulian et al.27 found that a paraplegic-specific equation was at that time best suited for predicting Db. We did not find any further studies on the validation of this method.
Therefore, our study has two objectives. The first objective of this paper is to study the relationship of WC and BIA and the degree of agreement between AI and BIA, using BIA as a reference or ‘gold standard’. The second objective is to study the relationship between BMI and BIA in subjects with SCI.
Methods
Participants
Men with SCI were recruited from the community. All subjects included had motor complete SCI (AIS scale A or B) according to the International Standards for Neurological and Functional Classification of Spinal Cord Injury29 below the first thoracic level (T1) and were at least one year post-injury. All subjects were investigated at the Swiss Paraplegic Center in Nottwil, Switzerland, a specialized SCI rehabilitation center. The rationale for including only men was two-fold. First, to our clinical expertise, it is the group in which obesity is most prevalent and the need for simple assessment the biggest. Second, for research reasons the choice for this group was to create homogeneity.
All subjects gave their written informed consent prior to study participation. The study was approved by the local ethics committee. This certifies that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Measurements
All subjects were informed about the preparations for the measurements (not exercising for 12 hours prior to measurement, omit consuming alcohol or caffeine 24 hours before examination, omit energy-rich nutrition 4–5 hours before measurement, retain of body lotion, and empty the bladder directly before measurement).
Body weight
Body weight of the subjects was measured in kg on an electronic wheelchair scale with an accuracy of 0.01 kg (Busch 535, Busch Werke AG, Trimmis, Switzerland). Total mass from the subjects with clothing and the wheelchair was determined first and after transferring the subject from the wheelchair, the wheelchair and clothes were weighted separately again. Body weight of the subject was determined by subtracting the weight of the wheelchair and clothes from total mass.
Stature
Body height was determined in cm with the subject in a 30° supine position, the head in Frankfurt plane, legs stretched, feet in dorsal flexion, and holding a full breath, using a sliding anthropometer (accuracy ± 0.5 mm, designed for the study). The 30° supine position was chosen to mimic standing as much as possible.
Waist circumference
WC was measured with a constant tension, flexible measuring tape (accuracy ± 1.0 mm, Ganzoni Sigvaris 3Q system, Memmingen, Germany) at minimal waist after normal expiration. The participant was placed lying in a 30° supine position.
Calf circumference
With the subject in a supine position, the heels placed on a knee roll, maximal circumference of the calf was measured using a constant tension, flexible measuring tape (accuracy ± 1.0 mm, Ganzoni Sigvaris 3Q system).
Sub-scapular skin fold
Right sub-scapular skin fold was measured with a slim guide skin fold calliper (GPM ±0.2 mm, DKSH Switzerland Ltd., Zurich, Switzerland). The subject was placed in a lying position on his left side, the right arm resting on the right hip.
Chest diameter
Chest diameter was measured with sliding anthropometer (accuracy ± 0.5 mm) designed for our study. The subject was placed in a supine position and chest diameter was measured at nipple level, at mid-expiration30
Body tissue resistance
Using the Bodystat® quad scan 4000 whole-body bioelectrical impedance measures were taken using gel electrodes at a 50-Hz frequency (Bodystat Ltd, Douglas Isle of Man, British Isles). Further instructions from the instruction manual were followed. At start of the measurement subjects were at least for 4 minutes in a supine position (www.bodystat.com).
Statistical analysis
To study the agreement between BIA and AI, we used Bland and Altman statistics and plots (difference plots).31 Bland Altman plot is a method of data plotting used in analyzing the agreement between two different measures with the same outcome variable. Further, it can be used to compare a new measurement technique with a ‘gold standard’. The x-axis shows the mean of the results of the two methods ([A + B]/2), whereas the y-axis represents the absolute difference between the two methods ([B − A]). In our study, the differences between the measurements with BIA and AI were plotted against the mean of both measurements. As the true percentages of fat mass are not known, the mean between both methods is regarded as the best estimate of the true fat mass. Limits of agreement were calculated as the mean difference ± 1.96 standard deviations of the difference. According to the limits of agreement method, it was decided prior to the conduction of the study that the maximally acceptable absolute difference between BIA and AI could be 3%. A power analysis was performed with statistical software package nQuery Advisor 7.0 (Statistical Solutions Ltd, Cork, Ireland). A power analysis, based on a 5% significance level and two-sided testing, indicated that in our study with 23 participants, the power would be >99% with a standard deviation (SD) of 1.56 and a mean of 0.28 for the differences.32
To examine the association between BIA and WC and the association between BIA and BMI, we calculated Pearson's correlation coefficient, presented in scatter plots. We considered a Pearson's correlation of >0.8 as clinically meaningful.
Results
Table 1 shows the characteristics of the study participants. Of the 23 participants, 22 were classified as AIS A, 1 AIS B. Lesion level ranged between Th2 and L1.
Table 1.
Characteristics of participants (n = 23)
| Mean | SD | Range | |
|---|---|---|---|
| Age (years) | 43.3 | 12.0 | 25.5–65.2 |
| Duration of injury (years) | 14.6 | 13.3 | 1.0–43.0 |
| Body weight (kg) | 74.8 | 11.8 | 56.0–95.8 |
| Body height (cm) | 177 | 7.5 | 166–197 |
| BMI | 24.9 | 3.5 | 18–31.5 |
| BIA | 24.3 | 6.0 | 12.7–39.1 |
| WC | 92.4 | 9.8 | 74.4–112.0 |
| AI | 25.1 | 6.6 | 14.2–42.1 |
n, number of participants; SD, standard deviation; kg, kilogram; cm, centimetres; BMI, body mass index; BIA, bioelectrical impedance analysis; WC, waist circumference; AI, anthropometric index.
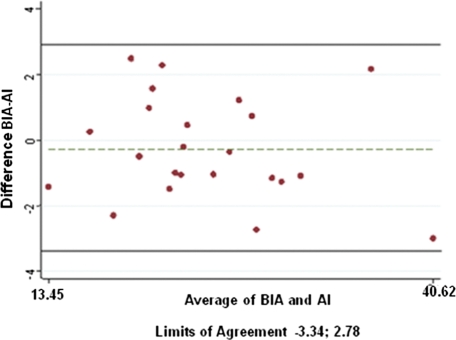
Fig. 1 shows the difference of measurement of percentage body fat with BIA + equation and with the AI versus the average of values measured by both methods. The dotted line shows that there is only a very small systematic difference between the two methods (mean difference: −0.28%). All our subjects are within the 95% confidence level, indicating that we can be confident at a 95% level that the difference is not only due to measurement error. The correlation (Pearson's r) between the AI and the BIA was 0.91.
Figure 1.
Measured percentage body fat: difference of the measurement for spinal cord-injured population-adjusted bioelectrical impedance analysis (BIA), and an anthropometric index (AI) versus the average of values measured by both methods. An absolute difference of 3% reflects the 95% limits of agreement: –3.34 to 2.78.
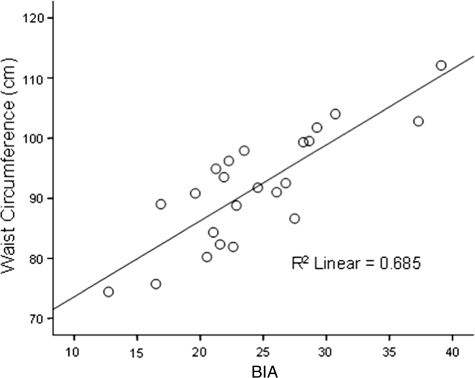
Fig. 2 shows a scatter plot of the WC versus the BIA with a regression line. The correlation (Pearson's r) between the WC and the BIA was 0.83.
Figure 2.
Scatter plot of BIA versus waist circumference. A regression line is drawn. The coefficient of determination (r2) was 0.685.
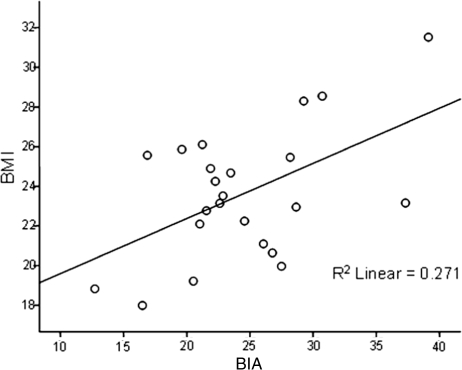
Fig. 3 shows a scatter plot of the BMI versus the BIA with a regression line. The correlation (Pearson's r) between the BMI and the BIA was 0.51.
Figure 3.
Scatter plot of body mass index (BMI) versus bioelectrical impedance analysis (BIA). A regression line is drawn. The coefficient of determination (r2) was 0.271.
Discussion
This study contributes to the search for a valid measure to identify obese persons with SCI that may be more practical to implement in clinical practice. We have examined WC measurement and AI measurement to measure obesity in the SCI population using BIA as a reference or ‘gold standard’. We found that the use of an AI has a very small systematic difference with BIA and is therefore, a reasonable proxy measure to identify obesity in men with motor complete SCI. WC was found to have a good correlation with BIA and can be seen as a valid proxy measure to identify obese persons with SCI. BMI was found to have only a moderate correlation with BIA, which makes the BMI relatively less suited for research and clinical use.
Anthropometric index
AI showed to be a reasonable proxy measure to identify obese men with complete SCI. This is in concordance with the study performed by Bulbulian et al.27 In this study of Bulbulian et al., body composition in 22 male athletes with paraplegia was measured with different techniques. The method used in our study, existing of a combined equation was found being best in the study of Bulbulian et al.27 Our current study included athletes as well as non-athletes; it has been observed that the AI might serve as a proxy method in this population too.
Waist circumference
The finding that the measurement of WC is a valid method to identify obese persons with SCI is consistent with the results of Edwards et al.25 In their study, the relation between WC and visceral adipose tissue in 31 subjects (15 SCI, 16 controls) was estimated, showing that WC may be a valid surrogate measure in SCI. Our study confirms the potential use of WC to estimate obesity in persons with SCI. What remains a challenge is finding the most appropriate method for the measurement of WC. Buchholz and Bugaresti.15 described potential problems in the appropriateness of using WC in the SCI population. Edwards et al.25 measured their subjects in supine and measured using three localizations and found a very high reproducibility of WC measurement. In our study, we placed the participants in a 30° supine position, because it mirrors the method used in standing able-bodied persons. In day-to-day practice, it would be preferred to measure WC in a sitting position. The simplicity of measuring WC and the promising results suggest further research on the standardization of the method.
Both AI and WC show potential value as a screening tool for obesity in persons with SCI. The use of the AI and WC measurement should be seen as possible methods to identify those persons at risk of obesity. This proposition, however, needs further and more specific testing. The AI is constructed of chest diameter, sub-scapular skin fold, and waist and calf circumference, combining measurement sites below and above the level of SCI, which gives a total picture of fat mass composition in persons with SCI.
Body mass index
The second objective of our study was to evaluate the validity of BMI for subjects with SCI. BMI is calculated using height and weight of a person. After SCI, major changes in body composition take place. Loss of muscle below the level of injury might be the main reasons for underestimating obesity in persons with SCI. In our study, we also showed a moderate correlation of BMI with BIA. This is consistent with the literature on the use of BMI in subjects with SCI.10,11,33 This again shows that BMI is an invalid method to estimate obesity in persons with SCI and therefore, should not be advocated as an outcome to estimate obesity in clinical practice and research.
Clinical relevance
Identifying those persons with obesity has clinical implications. Because of the associated risk for a person's health, managing obesity in SCI is a difficult but necessary challenge. Clinical implications that follow from detecting obesity in persons with SCI are dietary management and promotion of physical activity. Health interventions in the SCI population have been scarcely studied. Recently, Chen et al.34 published a study on the effects of weight loss interventions for persons with SCI showing that a 12-week dietary program leaded to considerable weight loss, but also a significant reduction in total fat mass, and an improvement in metabolic profile. It is know that persons with SCI show low levels of physical activity.35,36 There are currently no guidelines for duration, type, and level of exercise intensity for health promotion and weight loss in persons with SCI36 but the overview of Jacobs et al.37 provides recommendations for exercise specifically for persons with SCI.
Research implications
Until now, little is known on the magnitude of obesity on co-morbidities in an SCI population. The recently published paper of Edwards et al.25 showing that high levels of visceral adipose tissue exists in young people with SCI, who classify themselves as active and healthy, and findings by Laughton et al.21 ask for more and longitudinal research on this topic. The reference values of WC for obesity in persons with SCI are not known yet. Currently, the values of the able-bodied population are also used for persons with SCI, which might be not correct. Another issue raised is whether in persons with SCI total body adiposity or visceral adiposity is related to health outcomes, like in the case of cardiovascular diseases. Longitudinal studies in persons with SCI addressing the association between obesity and cardiovascular diseases and metabolic syndrome are of major relevance in the identification of persons at risk.
We encourage clinicians and researchers to further investigate the validity as well as the reliability and feasibility of the AI and different WC measures for weight management in persons with SCI.
Limitations of the study
Our study included a sample of 23 men with paraplegia. The rationale for this choice was that in this group, to our experience, obesity is the most prevalent problem and to create homogeneity in our study population. Before advocating one of the methods to be useful for all persons with SCI in clinical practice, both AI and WC should be evaluated in more diverse groups (including women, persons with incomplete lesion, and persons with tetraplegia), and in subjects with more extreme body tissue composition (underweight and overweight). However, our study shows the potential clinical and research relevance of the measures AI and WC to identify obese SCI subjects.
Conclusion
AI is a valid proxy measure to identify obese men with motor complete SCI. WC seems promising as a method to identify obese men with motor complete SCI, but further validation studies in larger and more heterogeneous populations should be performed. BMI shows only a moderate correlation with BIA and should therefore not be advocated as a method to identify obesity in persons with SCI.
References
- 1.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA 2002;288(14):1723–7 [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 2006;295(13):1549–55 [DOI] [PubMed] [Google Scholar]
- 3.Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA 1999;282(16):1523–9 [DOI] [PubMed] [Google Scholar]
- 4.Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr 2004;79(3):379–84 [DOI] [PubMed] [Google Scholar]
- 5.Snijder MB, Dekker JM, Visser M, Bouter LM, Stehouwer CD, Kostense PJ, et al. Associations of hip and thigh circumferences independent of waist circumference with the incidence of type 2 diabetes: the Hoorn Study. Am J Clin Nutr 2003;77(5):1192–7 [DOI] [PubMed] [Google Scholar]
- 6.Sullivan M, Karlsson J, Sjostrom L, Backman L, Bengtsson C, Bouchard C, et al. Swedish obese subjects (SOS) – an intervention study of obesity. Baseline evaluation of health and psychosocial functioning in the first 1743 subjects examined. Int J Obes Relat Metab Disord 1993;17(9):503–12 [PubMed] [Google Scholar]
- 7.Yancy WS, Jr, Olsen MK, Westman EC, Bosworth HB, Edelman D. Relationship between obesity and health-related quality of life in men. Obes Res 2002;10(10):1057–64 [DOI] [PubMed] [Google Scholar]
- 8.Weil E, Wachterman M, McCarthy EP, Davis RB, O'Day B, Iezzoni LI, et al. Obesity among adults with disabling conditions. JAMA 2002;288(10):1265–8 [DOI] [PubMed] [Google Scholar]
- 9.Anson CA, Shepherd C. Incidence of secondary complications in spinal cord injury. Int J Rehabil Res 1996;19(1):55–66 [DOI] [PubMed] [Google Scholar]
- 10.Chen YM, Ho SC, Lam SS, Chan SS. Validity of body mass index and waist circumference in the classification of obesity as compared to percent body fat in Chinese middle-aged women. Int J Obes (Lond) 2006;30(6):918–25 [DOI] [PubMed] [Google Scholar]
- 11.Liang H, Chen D, Wang Y, Rimmer JH, Braunschweig CL. Different risk factor patterns for metabolic syndrome in men with spinal cord injury compared with able-bodied men despite similar prevalence rates. Arch Phys Med Rehabil 2007;88(9):1198–204 [DOI] [PubMed] [Google Scholar]
- 12.Green D, Twardowski P, Wei R, Rademaker AW. Fatal pulmonary embolism in spinal cord injury. Chest. 1994;105(3):853–5 [DOI] [PubMed] [Google Scholar]
- 13.Maruyama Y, Mizuguchi M, Yaginuma T, Kusaka M, Yoshida H, Yokoyama K, et al. Serum leptin, abdominal obesity and the metabolic syndrome in individuals with chronic spinal cord injury. Spinal Cord 2008;46(7):494–9 [DOI] [PubMed] [Google Scholar]
- 14.Baumann W, Spungen A. Coronary heart disease in individuals with spinal cord injury: assessment of risk factors. Spinal Cord 2008;46:466–76 [DOI] [PubMed] [Google Scholar]
- 15.Buchholz AC, Bugaresti JM. A review of body mass index and waist circumference as markers of obesity and coronary heart disease risk in persons with chronic spinal cord injury. Spinal Cord 2005;43(9):513–8 [DOI] [PubMed] [Google Scholar]
- 16.Garshick E, Kelley A, Cohen SA, Garrison A, Tun CG, Gagnon D, et al. A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord 2005;43(7):408–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jones LM, Goulding A, Gerrard DF. DEXA: a practical and accurate tool to demonstrate total and regional bone loss, lean tissue loss and fat mass gain in paraplegia. Spinal Cord 1998;36(9):637–40 [DOI] [PubMed] [Google Scholar]
- 18.Sedlock DA, Laventure SJ. Body composition and resting energy expenditure in long term spinal cord injury. Paraplegia 1990;28(7):448–54 [DOI] [PubMed] [Google Scholar]
- 19.Buchholz AC, McGillivray CF, Pencharz PB. The use of bioelectric impedance analysis to measure fluid compartments in subjects with chronic paraplegia. Arch Phys Med Rehabil 2003;84(6):854–61 [DOI] [PubMed] [Google Scholar]
- 20.Jones LM, Legge M, Goulding A. Healthy body mass index values often underestimate body fat in men with spinal cord injury. Arch Phys Med Rehabil 2003;84(7):1068–71 [DOI] [PubMed] [Google Scholar]
- 21.Laughton GE, Buchholz AC, Martin Ginis KA, Goy RE. Lowering body mass index cutoffs better identifies obese persons with spinal cord injury. Spinal Cord 2009;47(10):757–62 [DOI] [PubMed] [Google Scholar]
- 22.de Groot S, Post MW, Postma K, Sluis TA, van der Woude LH. Prospective analysis of body mass index during and up to 5 years after discharge from inpatient spinal cord injury rehabilitation. J Rehabil Med 2010;42(10):922–8 [DOI] [PubMed] [Google Scholar]
- 23.Spungen AM, Bauman WA, Wang J, Pierson RN., Jr Measurement of body fat in individuals with tetraplegia: a comparison of eight clinical methods. Paraplegia 1995;33(7):402–8 [DOI] [PubMed] [Google Scholar]
- 24.Demirel S, Demirel G, Tukek T, Erk O, Yilmaz H. Risk factors for coronary heart disease in patients with spinal cord injury in Turkey. Spinal Cord 2001;39(3):134–8 [DOI] [PubMed] [Google Scholar]
- 25.Edwards LA, Bugaresti JM, Buchholz AC. Visceral adipose tissue and the ratio of visceral to subcutaneous adipose tissue are greater in adults with than in those without spinal cord injury, despite matching waist circumferences. Am J Clin Nutri 2008;87(3):600–7 [DOI] [PubMed] [Google Scholar]
- 26.Maki KC, Briones ER, Langbein WE, Inman-Felton A, Nemchausky B, Welch M, et al. Associations between serum lipids and indicators of adiposity in men with spinal cord injury. Paraplegia 1995;33(2):102–9 [DOI] [PubMed] [Google Scholar]
- 27.Bulbulian R, Johnson RE, Gruber JJ, Darabos B. Body composition in paraplegic male athletes. Med Sci Sports Exerc 1987;19(3):195–201 [PubMed] [Google Scholar]
- 28.Siri WE. Body composition from fluid space and density. In: Brozek J, Hanschel A. (eds.) Techniques for measuring body composition. Washington, DC: National Academy of Science; 1961. pp. 223–44 [Google Scholar]
- 29.Maynard FM, Jr, Bracken MB, Creasey G, Ditunno JF, Jr, Donovan WH, Ducker TB, et al. International standards for neurological and functional classification of spinal cord injury. American Spinal Injury Association. Spinal Cord 1997;35(5):266–74 [DOI] [PubMed] [Google Scholar]
- 30.Wilmore JH, Behnke AR. An anthropometric estimation of body density and lean body weight in young men. J Appl Physiol 1969;27(1):25–31 [DOI] [PubMed] [Google Scholar]
- 31.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8:135. [DOI] [PubMed] [Google Scholar]
- 32.Machin D, Campbell MJ. Statistical tables for design of clinical trials. Oxford: Blackwell Scientific Publications; 1987 [Google Scholar]
- 33.Gupta N, White KT, Sandford PR. Body mass index in spinal cord injury – a retrospective study. Spinal Cord 2006;44(2):92–4 [DOI] [PubMed] [Google Scholar]
- 34.Chen Y, Henson S, Jackson AB, Richards JS. Obesity intervention in persons with spinal cord injury. Spinal Cord 2006;44(2):82–91 [DOI] [PubMed] [Google Scholar]
- 35.Buchholz AC, McGillivray CF, Pencharz PB. Differences in resting metabolic rate between paraplegic and able-bodied subjects are explained by differences in body composition. Am J Clin Nutr 2003;77(2):371–8 [DOI] [PubMed] [Google Scholar]
- 36.Duran FS, Lugo L, Ramirez L, Eusse E. Effects of an exercise program on the rehabilitation of patients with spinal cord injury. Arch Phys Med Rehabil 2001;82(10):1349–54 [DOI] [PubMed] [Google Scholar]
- 37.Jacobs PL, Nash MS. Exercise recommendations for individuals with spinal cord injury. Sports Med 2004;34(11):727–51 [DOI] [PubMed] [Google Scholar]