1 Introduction
Human filariasis is mainly caused by the parasites, Wuchereria bancrofti and Brugia malayi, whose adults live in the lymphatic vessels of humans. In Japan, bancroftian filariasis was once endemic, but has been completely eradicated from the country. Although imported cases of filariasis are occasionally reported [1, 2, 3], no autochthonous case has been identified in recent years. By contrast, more than 10 cases of filariasis of animal origin are diagnosed annually in Japan. The most important parasite responsible for zoonotic filariasis in Japan is Dirofilaria immitis, the canine heartworm. The adult worms reside in the pulmonary arteries and the right ventricle, resulting in severe heart failure, which may cause sudden death of the affected dog. Humans can also be infected with D. immitis by a mosquito bite, but the larvae are unable to reach maturity in humans or primates, which are unsuitable hosts. Infected people present either pulmonary infarct or a subcutaneous nodule. The parasite is also occasionally observed in a deep inner organ. Hence, it is frequently confused with malignant tumor.
Human dirofilariasis, therefore, can be categorized into two groups: pulmonary and extra-pulmonary dirofilariasis. Extra-pulmonary dirofilariasis is classified further into four groups: cardiovascular, subcutaneous, visceral, and ophthalmic dirofilariasis. In this article, we focus on the studies of zoonotic filariasis that have been carried out by Japanese researchers in Japan.
2 Case reports of dirofilariasis since 1964 in Japan
2.1 Cardiovascular dirofilariasis
The filarial parasite of animal origin was first found in the left ventricle of a Brazilian boy (Magelhaes, 1887). Later, the worms were identified as adult male and female worms of D. immitis by Faust et al. [4]. This was a very unusual case in which the invading worm survived and grew into maturity in a human, just as it would do in the definitive host, Canidae. To date, only four cases of cardiovascular dirofilariasis have been reported worldwide; one of these was in Japan. Takeuchi et al. [5] found two slender nematodes in the heart and inferior vena cava of a 36-year-old Japanese male who died of liver cirrhosis. The worms were incidentally found through an administrative autopsy, and there was no evidence that the worms were involved as a cause of death. Both worms were identified as non-gravid adults females of D. immitis. The other two cases, a 73- and a 40-year-old women, were reported in New Orleans in the United States.
2.2 Pulmonary dirofilariasis
In Japan, pulmonary dirofilariasis, the most common type of human dirofilariasis, was first found in Kanazawa city in 1968 [6]. The patient was a 42-year-old male high school teacher. He was admitted to the hospital because of loss of consciousness for 20 minutes following his morning stretching routine. Chest X-ray examination revealed a coin lesion in his left lower lobe. Under the diagnosis of tuberculosis or lung cancer, a thoracotomy was carried out. Histopathological examination showed a pulmonary infraction caused by a premature female of D. immitis. Six years later two additional cases of pulmonary dirofilariasis were independently reported by Fuse et al. [7] and Otsuru et al. [8].
Thereafter, many clinical cases were noticed every year. Makiya et al. [9] reviewed the clinical cases published from 1964 to 1986. A total of 41 cases of pulmonary dirofilariasis were reported in this period. The coin lesions were mostly located in the right lower lobe of the affected lungs. They also observed that the most of the patients resided in the southwestern part of Japan but a few were in the northern part of Japan. They suggested that the geographical difference was attributable to the lower prevalence of microfilaremia in dogs with D. immitis infection in the northeastern part of Japan relative to the southwestern part, since the cumulative temperature in the northeastern part was insufficient to develop the same number of vector mosquitoes. For this reason, no cases have been reported in Hokkaido thus far, which is located in the northernmost part of Japan and has a far-colder climate than Tokyo.
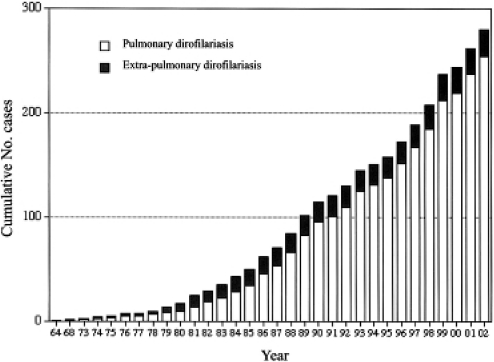
The overall incidence as compiled from published cases from 1964 to 1995 was recorded by Kagei [10]. According to his report, 103 additional cases of pulmonary dirofilariasis were counted from 1986 to 1995 in Japan. These figures indicated that the patients drastically increased in number more than doubled in 10 years. Figure 1 shows the cumulative cases of pulmonary dirofilariasis as of the end of 2002, in which the data from 1964 to 1986 and from 1986 to 1995 were quoted from Makiya et al. [9] and Kagei [10], respectively. The number of cases continues to increase, and since the study by Kagei [10], a total of 117 cases of pulmonary dirofilariasis have been cited in the database of Japana Centra Revuo Medicina over the last 7 years. In addition, three cases appeared in the Japanese Journal of Clinical Parasitology [11, 12] and four more cases were referred to us (Dr. I. Sato, Department of Pathology, Miyagi Prefectural Hosphal, personal communication). Consequently, 254 cases of pulmonary dirofilariasis have been recorded as of the end of 2002 (Fig. 1).
Fig. 1.
Cumulative number of cases of human dirofilariasis in Japan from 1964 to 2002.
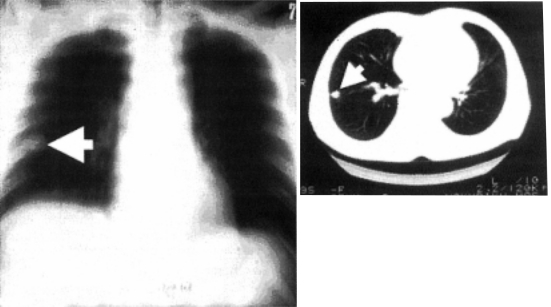
Kobayashi et al. [13] noted that the maximum diameter of the pulmonary lesions induced by the infarct of the worm was less than 3 cm. Therefore, a coin lesion of more than 3 cm in diameter on a chest X-ray examination should be excluded from the diagnosis of pulmonary dirofilariasis (Fig. 2). Thoracotomy, which is a high-risk procedure, used to be the only option for making a clear diagnosis prior to the 1990’s. Fortunately, thoracoscopic surgery introduced in the early 1990’s has been adapted to resect the parasitic nodule provoked by Diroflaria infection. Miura et al. [14] performed a thoracoscopic lung biopsy and observed an immature worm of D. immitis in the necrotic tissue of a peripheral pulmonary artery of a removed nodule. The patient, a 50-year-old male, was discharged 7 days after the medical treatment from Oita Medical University Hospital without any complications. This technique is now widely accepted as a less-invasive medical procedure and for diagnosing pulmonary dirofilariasis.
Fig. 2.
Chest X-ray (left) and CT (right) appearance of a patient with pulmonary dirofilariasis. A solitary nodule called “coin lesion” is adjacent to the pleural membrane (arrow).
2.3 Cutaneous dirofilariasis
Nishimura et al. [15] reported the first case of cutaneous dirofilariasis in Japan. The patient, a 52-year-old female living in Ibaragi city of Osaka prefecture, was admitted to a hospital with a chief complaint of a left breast nodule of 4 days’ duration. A surgical resection of the nodule was performed on 19 January 1961. A thread-like nematode of 50 mm in length and 0.21 mm in width was found in the removed tissue. From the morphological characteristics, they concluded that the worm was identical to a male D. immitis. Ten years later, an additional case of cutaneous dirofilariasis was reported by Otsuru et al. [8]. The patient, a 68-year-old male, was admitted to the Hospital of Okayama University because of a subcutaneous nodule on his right abdominal wall. Pathological specimens revealed several transverse sections of an immature female worm of D. immitis. Since then, 12 cases of cutaneous dirofilariasis have been reported between 1964 and 1986 [9], and nine additional cases were published between 1987 and 2002.
The parasites responsible for cutaneous nodules are thought to be D. immitis, except for the case described by MacLean et al. [16]. The patient, a 67-year-old male, living in Okinawa prefecture, which is in the southernmost part of Japan, presented with 2 cm (diameter) subcutaneous nodule which had appeared on his left anterior chest wall. The nodule was surgically removed, and pathological examination revealed several transverse sections of a worm, which was identified as Dirofilaria repens based on its morphological characteristics.
2.4 Visceral diroflariasis
A developing immature D. immitis worm is occasionally found in deep inner organs, such as the liver, uterus, and abdominal cavity. Tada et al. [17] reported a case of visceral dirofilariasis following a death due to bleeding in the abdominal cavity resulting from liver cirrhosis. A tumor-like mass was found embedded in the adipose tissue of the mesentery. At the central region of the nodule, they found several fragments of a female worm of Dirofilaria sp., probably D. immitis. In 1980, an additional case of extrapulmonary dirofilariasis was found in a 74-year-old female, residing in Toyama city, in Toyama prefecture [18]. She was admitted to the Toyama Medical and Pharmaceutical University Hospital because of uterine bleeding over the past 1 year. A hysterectomy was performed and an endometrial polyp measuring 2.0 x 1.5 x 1.0 cm was seen in the rear right wall of her uterus, in which a nematode parasite was revealed by a histopathological examination. The parasite, measuring 150 to 160 µm in diameter showed the typical appearance of a male D. immitis. Miyakawa et al. [19] reported a case of accidental identification of several transverse or oblique sections of Dirofilaria sp. in the liver of a 58-year-old female with colon cancer.
2.5 Ophthalmic dirofilariasis
The Dirofilaria worm has also been implicated in certain ophthalmic infections. According to the review of Kagei [10], six cases of ophthalmic dirofilariasis have been reported so far: two cases of orbital tumor, two of neuroretinitis, one of peripheral proliferative vasculitis of the fundus, and one of an eyelid legion. However, the last case did not precisely constitute ophthalmic dirofilariasis since the parasite was recovered from subcutaneous tissue from the eyelid. Moreover, there is no apparent evidence that the Dirofilaria worm is responsible for the eye pathologies in the remaining cases. The patients were suspected of having the parasitic infection based not on the pathological findings but on the clinical and serological examinations; otherwise, the authors only stated that the patient had a parasite without any evidential presentation of photographs. Therefore, it is uncertain whether these patients were frank cases of ophthalmic dirofilariasis in Japan, despite a number of cases that have appeared in the foreign literature [20, 21]. In conclusion, the number of extra-pulmonary dirofilariasis cases in Japan was estimated to be 26 as of the end of 2002 (Fig. 1).
3 Diagnostics
3.1 Diagnostic morphology of zoonotic filariasis
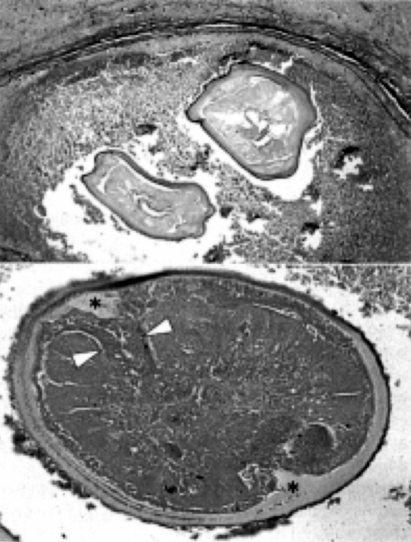
Gutierrez [22] described the diagnostic features of zoonotic filariae in tissue sections. A review article written by Chitwood and Lichtenfels [23] also mentioned the morphological characteristics of Filaridae. Both reviews are useful for pathologists to distinguish each filarial worm from the others in pathological specimens. In Japan, Uni et al. [24] studied the comparative morphology of D. urusi and D. immitis in cross-sections. Yoshimura and Akao [25] investigated the cross-sectional morphology of human and zoonotic filarial worms that were found in human tissues (Figs. 3 and 4). These studies have contributed to the identification of filarial infections, including an imported case of onchocerciasis and a case of zoonotic onchocerciasis, among the Japanese [1, 26].
Fig. 3.
Histopathologic findings of the nodule. Two transverse sections of an immature worm of D. immtis are seen in a small pulmonary artery (upper, Elastica van Gieson stain), and a transverse section of an immature adult worm showing large lateral chords (arrow head) with internal longitudinal ridges (*) and multilayered cuticle (bottom, HE stain).
Fig. 4.

Low-power view of a pulmonary infarct containing a transverse section and a longitudinal section of a mature male D. immitis (upper). Two spicules are clearly observable (bottom).
Nagano et al. [27] attempted to detect the genomic DNA of D. immitis by polymerase chain reaction (PCR). This is a promising tool for identifying necrotizing parasites that do not show normal structures.
3.2 Serological investigations
Serology is an alternative method of diagnosing parasitic infections because the invading parasite cannot always be identified by pathologyical examination of resected tissues. Therefore, many attempts have been made to detect a specific antibody against filarial proteins. At first, filarial antigen derived from D. immitis was studied to diagnose bancroftian filariasis in Japan. Ishizaki et al. [28] prepared a defatted somatic antigen of adult D. immitis and adapted it to the epidemiological survey of bancroftian filariasis in an endemic area of Ehime prefecture as an intradermal test. Of 54 patients with microfilaremia, 44 showed a positive reaction and the remainder were negative, indicating that the sensitivity was unsatisfactory for a field survey. Tada and Kawashima [29] demonstrated the usefulness of a purified antigen derived from adult D. immitis for an intradermal skin test against bancroftian filariasis. This antigen showed extremely low cross-reactivity against the sera from eight other parasitic infections and did not show nonspecific reaction in patients with allergic diseases. Sawada and his colleagues studied the antigenic nature of a purified D. immitis antigen, FST, and its derivatives [30-32]. Although all these antigens were prepared for use in an intradermal test of bancroftian filariasis, they had a potential diagnostic benefit for human dirofilariasis.
The first step in making a serodiagnosis of human dirofilariasis in Japan was achieved by Tamaoki et al. [33], who performed several immunological tests, intradermal skin test, agar-gel diffusion, and immunoelectrophoretic analysis, that lead to a preoperative diagnosis. Sato et al. [34] introduced an enzyme-linked immunosorbent assay (ELISA) for the diagnosis and follow-up study of dirofilariasis. The antigen they used included a veronal-buffered saline extract of adult worms of D. immitis to detect specific IgG antibody. The antibody was demonstrated in the patient’s serum preoperatively, but the serum also reacted with the antigen derived from adult worms of Ascaris suum. After operation, the IgG responses to both antigens decreased gradually, with more prominent reduction of Ascaris antibody. The ELISA could be useful for the post-operative follow-up in human dirofilariasis. Around the same time in the United States, Glickrnan et al. [35] demonstrated that an antibody to somatic antigen of adult D. immitis was detectable by indirect hemagglutination test and ELISA in eight patients with radiologically evident pulmonary nodules in whom the final diagnosis was confirmed pathologically as Dirofilaria sp. infection. A mixed passive hemagglutination test was also attempted to detect the IgG antibody [36].
Akao et al. [37] demonstrated that the excretorysecretory (ES) products of female worms of D. immitis provided a more sensitive antigen than the adult somatic antigen by using an immunoblot analysis. They also suggested that a low molecular component of ES products strongly cross-reacted with the sera from non-filarial patients, and that adult somatic antigen shared this antigenic component. Nakagaki et al. [38] observed that, using an ELISA, the sensitivity of ES antigen was less than 50%, but periodate-treated ES (PI) antigen was superior to that of ES antigen. They also noted that not only phosphate buffer extracted antigen but also ES and PI antigens highly cross-reacted to the sera of patients with loasis, tropical eosinophila and gnathostomiasis, suggesting that it was extremely difficult to diagnose human pulmonary dirofilariasis by ELISA. Sun and Sugane [39] isolated an immunodominant antigen of D. immitis from genomic DNA and established a recombinant DNA-derived fusion protein for ELISA. However, there is no report on the practical application of this antigen for human dirofilariasis to date. In conclusion, the reliability of serological tests is still questionable and further investigations are needed to identify a more specific antigen suitable for immunodiagnosis.
4 Animal models for human dirofilariasis
To understand the pathophysiology and to improve the serodiagnosis of dirofilariasis in humans, several animal models have been investigated. Experimental infections with fifth-stage larvae molting in the dog were successful in rabbits, rats, and guinea pigs, while infections with third-stage larvae molting in vector mosquitoes were only successful in dogs and ferrets [40, 41]. Nakagaki et al. [42] observed that the subcutaneous transplantation of these juvenile D. immitis migrated into lung arteries, resulting in pulmonary hemorrhagic infarction. They noticed that the pathological findings of the lung closely resembled the lesions of human pulmonary dirofilariasis. They are also studying the immune response of experimentally infected rabbits to develop a more precise diagnosis of human dirofilariasis (Dr. K. Nakagaki, personal communication).
5 Investigations of vector mosquitoes
In Japan, at least 16 species of mosquitoes are thought to play a role as a vector of D immitis. Of these, Culex pipiens pallens and Cx. tritaeniorhynchus are the major species and are distributed nationwide. A detailed distribution of these vector mosquitoes and the prevalence of the infection in dogs have been described in a review article by Kagei [10].
Acknowledgements
The author sincerely thanks Drs Kunioki Araki and Kazuhide Nakagaki for their valuable advices. This paper is revised from Asian Parasitology Vol.3 Filariasis in Asia and Western Pacific Islands, 145-152 by The Federation of Asian Parasitologists in 2004.
References
- 1.Yoshimura H, Kondo K, Akao N, Ohnishi Y, Tsubota N, lkado S, Miyawaki H. Case report of onchocercomata surgically removed from a Japanese probably infected in Africa. Clin Surgery (Rin-sho Geka) 1983; 38: 1679-1681 (in Japanese). [Google Scholar]
- 2.Sugiyama E, Shinonaga S, Tsukidate S, Ftijita K, Nawada H, Sazaki N, Kamikawadoko S, Ohtaki N, Oka K. A case of Loiasis. J Jpn Assoc Infec Dis 1988; 62: 490-494 (in Japanese). [DOI] [PubMed] [Google Scholar]
- 3.Yoshida Y, Shiota K, Yamada M. The first imported case report with Mansonella perstains. Jpn Med J 1982; (3047): 43-47 (in Japanese). [Google Scholar]
- 4.Faust EC, Thomas ER, Jones J. Discovery of human heartworm infection in New Orleans. J Parasitol 1941; 27: 115-122 [Google Scholar]
- 5.Takeuchi T, Asami K, Kobayashi S, Masuda M, Tanabe M, Miura S, Asakawa M. Diroflaria immitis infection in man: Report of a case of the infection in heart and inferior vena cava from Japan. J Parasitol 1981; 30: 966-969 [DOI] [PubMed] [Google Scholar]
- 6.Yoshimura H, Yokogawa M, Monma R, Yamato K, Takekawa A. A case of pulmonary dirofilariasis causing acute infatct of the lung. Jpn Med J 1968; (2344): 26-29 (in Japanese). [Google Scholar]
- 7.Fuse K, Yoshimura K, Kofujida K. A case of human dirofilariasis showing abnormal pulmonary shadow. Surgery (Geka) 1974; 36: 737-740 (in Japanese). [Google Scholar]
- 8.Otsuru M, Shirakawa T, Kenmotsu M. Some cases of larval or adult nematode migration in the human tissue. Jpn J Parasitol 1974; 23: 106-115 (in Japanese). [Google Scholar]
- 9.Makiya K, Tsukamoto M, Kagei N. A comprehensive list of human dirofilariasis in Japan. J Univ Occu Env Health 1987; 9: 233-242 (in Japanese). [DOI] [PubMed] [Google Scholar]
- 10.Kagei N. Dirofilariasis. In: Otsuru M., Kamegai S., Hayashi S. editors. Progress of Medical Parasitology in Japan. Vol. 8. Tokyo: Meguro Parasitology Museum, 2003: 521-556.
- 11.Takao Y, Fukuma T, Morishita M, Tanaka H, Shimamatsu K. Three parasitic cases diagnosed by examination of extirpated speciemens (sparganosis mansoni, human dirofilariasis, anisakiasis). J CIin Parasitol 2001; 12: 35-39 (in Japanese). [Google Scholar]
- 12.Ohashi R, Suginuma H, Kino H, Terada M, Kobayashi H, Ogawa H, Masago S, Tamada T, Niwa H. Efficacy of intraoperative frozen-section examination for dirofilariasis immitis, report of two cases. J Clin Parasitol 2002; 13: 92-94 (in Japanese). [Google Scholar]
- 13.Kobayashi H, Kusajima Y, Mori K, Nakamura T, Shima Y, Konishi K, Hirono T, Nakamura H, Mizukami H, Takayanagi K, Yagi M, Konishi Z, Miyazaki I, Yoshimura H, Asaji H. A case of human pulmonary dirofilariasis. Jpn J CIin Surg 1989; 50: 531-536 (in Japanese). [Google Scholar]
- 14.Miura T, Tanaka K, Uchida Y, Kawano Y, Tamai H, Hadama T, Takaoka H, Asou S. A case of pulmonary dirofilariasis diagnosed through thoracoscopic lung biopsy. J CIin Surg 1996; 49: 187-189 (in Japanese). [PubMed] [Google Scholar]
- 15.Nishimura T, Kondo K, Shoho C. Human infection with a subcutaneous Dirofilaria immitis. Biken J 1964; 7: 1-8 [PubMed] [Google Scholar]
- 16.MacLean JD, Beaver PC, Michalek H. Subcutaneous dirofilariasis in Okinawa Japan. Am J Trop Med Hyg 1979; 28: 45-48 [DOI] [PubMed] [Google Scholar]
- 17.Tada I, Sakaguchi Y, Eto K. Dirofilaria in the abdominal cavity of a man in Japan. Am J Trop Med Hyg 1979; 28: 988-990 [DOI] [PubMed] [Google Scholar]
- 18.Yoshimura H, Akao N, Kondo K, Ohishi Y, Kitagawa M, Kamimura K. Human dirofilariasis in Japan; Case report and review of literature. Int J Zoonosis 1980; 7: 107-114 [PubMed] [Google Scholar]
- 19.Miyagawa Y, Harada H, Nishimaki K, Kaneko T, Ozawa J, Komatsubara A, Kondo K, Akao N, Uchikawa K. A case of hepatic dirofilariasis found at operation of colon cancer. J CIin Parasitol 1998; 9: 27-29 (in Japanese). [Google Scholar]
- 20.Arvanitis PG, Vakalis NC, Damanakis AG, Theodossiadis GP. Ophthalmic dirofilariasis. Am J Ophthalmol 1997; 123: 689-691 [DOI] [PubMed] [Google Scholar]
- 21.Stringfellow GJ, Francis IC, Coroneo MT, Walker J. Orbital dirofilariasis. Clin Exp Ophthalmol 2002; 30: 378-380 [DOI] [PubMed] [Google Scholar]
- 22.Gutierrez Y. Diagnostic features of zoonotic filariae in tissue sections. Human Pathol 1984; 15: 514-525 [DOI] [PubMed] [Google Scholar]
- 23.Chitwood M, Lichtenfels JR. Identification of parasitic metazoa in tissue sections. Exp Parasitol 1972; 32: 407-519 [DOI] [PubMed] [Google Scholar]
- 24.Uni S, Kimata I, Takada S. Cross-section morphology of Dirofilaria ursi in comparison with D. immitis. Jpn J Parasitol 1980; 29: 489-497 [Google Scholar]
- 25.Yoshimura H, Akao N. Clinicopathology of human Diroflaria infection and histological identification of the parasite in the involved tissues. Saishin-Igaku. 1982; 37: 959-964 [Google Scholar]
- 26.Hashimoto H, Murakami I, Fujiwara S, Takayasu S, Takaoka H, Uga S, Akao N, Kondo K, Yoshimura H. A human case of zoonotic onchocerciasis in Japan. J Dermatol 1990; 17: 52-55 [DOI] [PubMed] [Google Scholar]
- 27.Nagano I, Zhiliang W, Nakayama M, Takahashi Y. A simple method to design PCR primer to detect genomic DNA of parasites and its application to Diroflaria immitis. Mol Cellular Probes 1996; 10: 423-425 [DOI] [PubMed] [Google Scholar]
- 28.Ishizaki T, Kutsumi H, Kumada M, Muranaka M, Miyamoto T, Makino S, Nagai R. Studies on the intradermal reaction by the antigen of Diroflaria immitis. 1. Determination of the new criterion for positive skin reaction and factors related to or affecting the skin reaction. Jpn J Parasitol 1964; 13: 43-50 (in Japanese). [Google Scholar]
- 29.Tada I, Kawashima K. Studies on the skin reaction in human filariasis with a purified antigen from Diroflaria immitis. Jpn J Parasitol 1964; 13: 427-434 (in Japanese). [Google Scholar]
- 30.Sawada T, Kono M, Sato S, Yamamoto I, Takei K. Immunological studies on filariasis. (2) Intradermal test with purified antigen in canine and human filariasis. Gunma J Med 1962; 11: 16-24 (in Japanese). [Google Scholar]
- 31.Sato S, Takei K, Matsuyama S. The practical use of skin test with antigen FST (FSCD1) for epidemiological survey of filariasis. Jpn J Parasitol 1969; 18: 21-27 (in Japanese). [Google Scholar]
- 32.Sato K. Studies on the skin test antigen FST for the iimnunodiagnosis of filariasis. The electropholetic analysis and separation of antigen FST. Jpn J Parasitol 1969; 18: 166-173 (in Japanese). [Google Scholar]
- 33.Tamaki J, Ono E, Naruse K, Tanaka K, Fujiwara T, Kawakami M, Konno K, Takizawa T, Kimie O, Kimura T, Orihira H, Hayashi S, Asahi H, Hosaka Y, Koyama T. A case of pulmonary dirofilariasis presenting pulmonary infarction caused by Dirofilaria immitis. Jpn J Thorac Dis 1978; 16: 865-870 (in Japanese). [PubMed] [Google Scholar]
- 34.Sato M, Koyama A, Iwai K, Kawabata Y, Kojima S. Human pulmonary dirofilariasis with special reference to the ELISA for the diagnosis and follow-up study. Z Parasitenkd 1985; 71: 561-563 [DOI] [PubMed] [Google Scholar]
- 35.Glickman LT, Grive RB, Schantz PM. Serologic diagnosis of zoonotic pulmonary dirofilariasis. Am J Med 1986; 80: 161-164 [DOI] [PubMed] [Google Scholar]
- 36.Ohnishi Y, Yoshimura H, Ohyama T, Tokairin M, Nagakura M. An attempt of immunodiagnosis by means of mixed passive hemagglutination (MPHA) test for human pulmonary dirofilariasis. Parasitol Res 1988; 74: 177-280 [DOI] [PubMed] [Google Scholar]
- 37.Akao N, Kondo K, Fojita K. Immunoblot analysis of Dirofilaria immitis recognized by infected humans. Ann Trop Med Parasitol 1991; 85: 455-460 [DOI] [PubMed] [Google Scholar]
- 38.Nakagaki K, Araki K, Nogami S, Maeda R, Carlow CK-S. Comparison of various antigens for diagnosis of human pulmonary dirofilariasis. San Antonio, Texas: American Heartworm Society 2001: 225-229.
- 39.Sun S, Sugane K. Complete structure of the gene encoding an immunodominant antigen of Diroflaria immitis and larva-specific synthesis of primary transcript. J Helminthol 1994; 68: 259-264 [DOI] [PubMed] [Google Scholar]
- 40.Kume S, Itagaki S. A preliminary report of experimental infection with fifth-stage larvae of Diroflaria immitis to rabbits, rats and guinea pigs. Jpn J Vet Sci 1947; 9: 106 (in Japanese). [Google Scholar]
- 41.Blair LS, Williams E, Ewanciw DV. Efficacy of ivermectin against third-stage Dirofilaria immitis larvae in ferrets and dogs. Res Vet Sci 1982; 33: 386-387 [PubMed] [Google Scholar]
- 42.Nakagaki K, Nogami S, Araki K, Tagawa M, Maeda R. Dirofilaria immitis: Experimental infection of rabbits with immature fifth-stage worms. Am J Trop Med Hyg 1997; 57: 667-671 [DOI] [PubMed] [Google Scholar]