Abstract
Background
Emotion regulation deficits have been consistently linked to psychopathology in cross-sectional studies. However, the direction of the relationship between emotion regulation and psychopathology is unclear. This study examined the longitudinal and reciprocal relationships between emotion regulation deficits and psychopathology in adolescents.
Methods
Emotion dysregulation and symptomatology (depression, anxiety, aggressive behavior, and eating pathology) were assessed in a large, diverse sample of adolescents (N = 1,065) at two time points separated by seven months. Structural equation modeling was used to examine the longitudinal and reciprocal relationships between emotion dysregulation and symptoms of psychopathology.
Results
The three distinct emotion processes examined here (emotional understanding, dysregulated expression of sadness and anger, and ruminative responses to distress) formed a unitary latent emotion dysregulation factor. Emotion dysregulation predicted increases in anxiety symptoms, aggressive behavior, and eating pathology after controlling for baseline symptoms but did not predict depressive symptoms. In contrast, none of the four types of psychopathology predicted increases in emotion dysregulation after controlling for baseline emotion dysregulation.
Conclusions
Emotion dysregulation appears to be an important transdiagnostic factor that increases risk for a wide range of psychopathology outcomes in adolescence. These results suggest targets for preventive interventions during this developmental period of risk.
Keywords: emotion regulation, depression, anxiety, aggression, eating pathology, adolescence
The adaptive management of emotions is critical for social functioning and psychological well-being (Aldao, Nolen-Hoeksema, & Schweizer, 2010; Denham, 1998; Eisenberg, Fabes, Guthrie, & Reiser, 2000; Gross, 1998b). Thompson (1994) defined emotion regulation as: “the extrinsic and intrinsic processes responsible for monitoring, evaluating, and modifying emotional reactions, especially their intensive and temporal features, to accomplish one's goals” (p. 28). Individual differences in the ability to identify and understand one's own emotions, the emotions of others, and the causes and consequences of different emotions, as well as in the types of strategies used to manage and regulate emotions, are evident by early childhood (Cummings, 1987; Denham, 1998; Eisenberg et al., 1993). These differences in emotional understanding and in the acquisition of adaptive strategies for managing emotions have far-reaching implications for social functioning (Denham, 1986; Eisenberg, et al., 1993; Eisenberg, Fabes, et al., 2000; Saarni, 1999). Children and adolescents with better emotion regulation skills are more socially competent, have higher peer status and better quality relationships, and engage in higher levels of prosocial behavior than youth with poor emotion regulation skills (Denham, 1986; Denham et al., 2003; Denham, McKinley, Couchoud, & Holt, 1990; Eisenberg, et al., 1993; Eisenberg et al., 1995; Hubbard & Coie, 1994; Rydell, Berlin, & Bohlin, 2003; Spinard et al., 2006). Children's emotion regulation skills also have been found to predict their social competence at later points in development (Denham, et al., 2003; Rydell, et al., 2003; Spinard, et al., 2006).
Emotion regulation skills also have important implications for mental health (Gross & Muñoz, 1995). Accumulating evidence suggests that emotion regulation is related to the development and maintenance of youth psychopathology. Children with anxiety disorders have been found to have poorer emotional understanding and more difficulty managing negative emotions than non-anxious youth (Southam-Gerow & Kendall, 2000; Suveg & Zeman, 2004). Adolescent depression also has been linked to reductions in the use and quality of strategies to manage negative emotions (Garber, Braafladt, & Weiss, 1995; Silk, Steinberg, & Morris, 2003). Engagement in rumination, an emotion regulation strategy involving passive self-focus on feelings of distress and on their causes and consequences (Nolen-Hoeksema & Morrow, 1991), has been associated consistently with adolescent depression both concurrently (Kuyken, Watkins, Holden, & Cook, 2006; Ziegert & Kistner, 2002) and prospectively (Abela, Brozina, & Haigh, 2002; Broderick & Korteland, 2004; Burwell & Shirk, 2007). Poor emotional understanding and difficulty regulating negative emotions also have been documented among children who engage in high levels of aggressive behavior (Bohnert, Crnic, & Lim, 2003; Cole, Zahn-Waxler, & Smith, 1994; Dearing et al., 2002; Eisenberg et al., 2000; Shields & Cicchetti, 1998) and among adolescent females with eating pathology (Sim & Zeman, 2005, 2006).
Adolescence represents a crucial developmental period in which to study the relationship between emotion regulation skills and psychopathology. A central task of adolescence is to learn to regulate affect in adaptive ways, increasingly without the aid of the adults who provide guidance in childhood (Steinberg & Avenevoli, 2000; Steinberg et al., 2006). Changes in biological, cognitive, and social systems during adolescence present innumerable affectively-laden situations in which emotions must be successfully managed to ensure adaptive functioning (Larson & Richards, 1991; Steinberg, 1987). For instance, increasing independent contact with peers introduces a myriad of challenges that require effective emotional response management (e.g., engagement in romantic relationships and sexual behavior, exposure to substance use). These numerous changes lead to increased perceptions of stress and daily hassles (Larson & Ham, 1993; Seidman, Allen, Aber, Mitchell, & Feiman, 1994; Simmons & Blythe, 1987) as well as increases in the experience of negative affect and emotional instability, and a closer linking of stressful events to the emergence of negative affect (Larson & Ham, 1993; Larson & Lampman-Petraitis, 1989; Larson, Moneta, Richards, & Wilson, 2002). Adolescence also is characterized by high risk for the development of psychopathology (Andersen & Teicher, 2008; Hankin et al., 1998; Lewinsohn, Striegel-Moore, & Seeley, 2000; Twenge & Nolen-Hoeksema, 2002). Individuals who have not developed strategies to adaptively manage negative emotions arising from the many challenges of adolescence may be particularly at risk for adverse mental health outcomes (Silk et al., 2007; Steinberg, et al., 2006).
Despite accumulating evidence suggesting that emotion dysregulation is associated with youth psychopathology, a number of important questions remain unanswered regarding the specific nature of this relationship. First, although poor emotion regulation has been documented among children and adolescents with a variety of diagnoses and associations between emotion regulation and symptoms of psychopathology have been observed in a number of studies, the vast majority of this research has been cross-sectional in nature, with some notable exceptions examining rumination specifically (Abela, et al., 2002; Broderick & Korteland, 2004; Burwell & Shirk, 2007) and problem behaviors in young children (Eisenberg, Guthrie, et al., 2000). Thus, it remains unclear whether emotion dysregulation primarily represents a risk factor for the development of adolescent psychopathology or whether the onset of mental health problems renders adolescents less able to effectively manage their emotions. This distinction has important implications for targeting emotion regulation in treatment versus preventive interventions. If emotion regulation is a risk factor for future psychopathology, techniques targeting emotion regulation skills should be incorporated into both treatment and preventive interventions. Alternatively, if emotion regulation is primarily a consequence of psychopathology or a factor underlying disorder persistence, such techniques would most usefully be included into treatment rather than prevention.
Second, there is a paucity of research on the extent to which emotion dysregulation represents a global risk factor for poor mental health outcomes versus a vulnerability to specific types of psychopathology. Poor emotion regulation has recently been posited to represent a transdiagnostic factor related to multiple types of psychopathology (Ehring & Watkins, 2008; Gross & John, 2003; Harvey, Watkins, Mansell, & Shafran, 2004; Kring & Sloan, 2010; Moses & Barlow, 2006; Watkins, 2008). Significant cross-sectional associations have been documented between emotion dysregulation and symptoms of depression, anxiety, eating pathology, and substance abuse in transdiagnostic studies of adults and in a recent meta-analysis (Aldao & Nolen-Hoeksema, 2010; Aldao, et al., 2010). Prospective data are needed, however, to determine both the direction of effect in the relationship between emotion regulation deficits and psychopathology, and whether emotion dysregulation represent a vulnerability factor for the development of certain types of psychopathology, but not others. Finally, it is unknown whether different aspects of emotion functioning are best represented by a latent factor of emotion regulation or are better characterized as distinct processes in adolescence. Emotion regulation involves a number of component processes, each of which emerge at different points in development (Denham, 1998). Recent evidence from an adult sample indicated that poor understanding of emotions, negative cognitive reactivity to emotional experiences, and maladaptive emotion management (but not emotional intensity) loaded onto a higher-order factor of emotion dysregulation (Mennin, Holaway, Fresco, Moore, & Heimberg, 2007), but it is unknown whether these processes comprise a broad latent factor in adolescents.
The current investigation aimed to address these gaps in the literature by examining the reciprocal relationships among poor emotion regulation skills and various forms of psychopathology in a sample of adolescents followed prospectively. We expected that adolescents who were better able to identify and understand their emotional experiences would also employ more effective strategies for managing their emotions. Specifically, we predicted that emotional understanding, adaptive expression of negative emotions, and cognitive emotion management strategies would best be represented by a higher-order construct of emotion regulation. We selected these specific aspects of emotion regulation in order to capture different stages in the emotion regulation process, each of which has relevance for psychopathology. Awareness and understanding of emotional experience represents an early stage of the emotion regulation process that requires attending to and differentiating interoceptive emotional cues. Emotional awareness has neural correlates that are distinct from emotion expression and regulation (Lane et al., 1998). It has been argued that emotional awareness is necessary to facilitate adaptive emotion regulation (Saarni, 1999), and poor awareness has been linked to a variety of poor mental health outcomes (Mennin, McLaughlin, & Flanagan, 2009; Novick-Kline, Turk, Mennin, Hoyt, & Gallagher, 2005; Southam-Gerow & Kendall, 2000; Suveg & Zeman, 2004). Emotion expression conveys important information about one's emotional experiences to others, and regulation of expression can directly influence the intensity of emotional experience (Gross, 1998a; Gross & John, 2003). Maladaptive or heightened expression of specific emotions—including anger, fear, and sadness—have been linked to internalizing and externalizing problems in adolescents (Keltner, Moffit, & Stouthamer-Loeber, 1995; Zeman, Shipman, & Suveg, 2002). Cognitive emotion regulation strategies—such as rumination— represent a relatively late stage in the emotion regulation process in which an individual engages in specific thoughts or behaviors in response to emotional experiences, often as an attempt to maintain or diminish those experiences. Rumination has been linked to adolescent psychopathology both concurrently and prospectively (Abela, et al., 2002; Burwell & Shirk, 2007). We anticipated that poor emotion regulation skills in each of these areas would predict subsequent increases in adolescent symptoms of depression, anxiety, aggressive behavior, and eating pathology but that baseline symptomatology would not predict changes in emotion regulation.
Methods
Participants
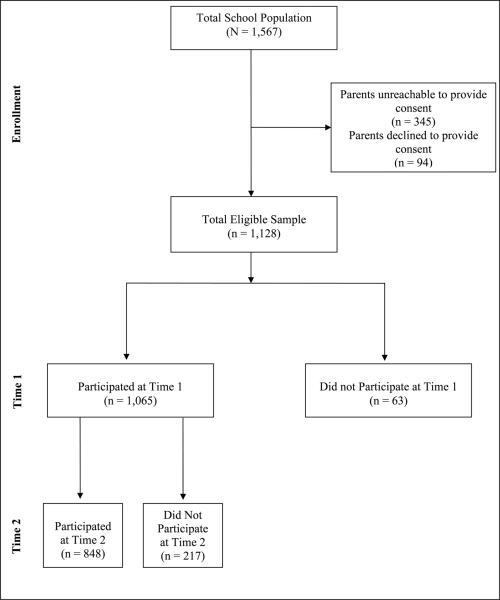
The sample for this study was recruited from the total enrollment of two middle schools (Grades 6-8) from a small urban community (population 71,538) in Connecticut. The parents of all eligible children (N = 1567) in the middle schools were asked to provide active consent for their children to participate. 22% of parents did not return consent forms and could not be reached to obtain consent, and 6% of parents declined to provide consent for their child to participate. The overall cooperation rate in the study at baseline was 72% (see Figure 1). Of the participants who were present at the baseline assessment, 217 (20.4%) did not participate at the Time 2 assessment. This school district population was highly transient; over the four-year period from 2000-2004, 22.7% of students had left the district (Connecticut Department of Education, 2006). We conducted analyses using the sample of 1,065 participants who were present at the baseline assessment, excluding participants who were present at Time 2 but not at Time 1.
Figure 1.
Study flow of participants in the study.
The baseline sample included 51.2% (N = 545) boys and 48.8% (N = 520) girls, resulting in 1065 participants, all of whom provided consent before participating in the study (68% of all eligible students in the schools). Participants (ages 11-14) were evenly distributed across grade level with 31.8% (N = 337) of participants in the sixth, 33.9% (N = 360) in the seventh, and 34.3% (N = 364) in the eighth grade. The race/ethnicity composition of the sample was as follows: 13.2% (N = 141) White, 11.8% (N = 126) Black, 56.9% (N = 610) Hispanic/Latino, 2.2% (N = 24) Asian/Pacific Islander, 0.2% (N = 2) Native American, 0.8% (N = 9) Middle Eastern, 9.3% (N = 100) Biracial/Multiracial, and 4.2% (N = 45) reported being members of other racial/ethnic groups. 1.3% (N = 14) declined to provide this information. 27% (N = 293) of participants reported living in single-parent households. The community in which the participating schools reside is a uniformly lower-SES community, with a per capita income of $18,404 (Connecticut Department of Education, 2006). School records indicated that 62.3% of students qualified for free or reduced lunch in the 2004-2005 school year.
Psychopathology Measures
The Children's Depression Inventory (CDI; Kovacs, 1992) is a widely used self-report measure of depressive symptoms in children and adolescents. The CDI includes 27 items consisting of three statements (e.g., I am sad once in a while, I am sad many times, I am sad all the time) representing different levels of severity of a specific symptom of depression. The CDI has sound psychometric properties, including internal consistency, test-retest reliability, and discriminant validity (Kovacs, 1992; Reynolds, 1994). The item pertaining to suicidal ideation was removed from the measure at the request of school officials and the human subjects committee. The 26 remaining items were summed to create a total score ranging from 0 to 52. The CDI demonstrated good reliability in this sample (Time 1 α = .82, Time 2 α = .89).
Anxiety Symptoms
The Multidimensional Anxiety Scale for Children (MASC; March, Parker, Sullivan, Stallings, & Conners, 1997) is a 39-item widely used measure of anxiety in children. The MASC assesses physical symptoms of anxiety, harm avoidance, social anxiety, and separation anxiety and is appropriate for children ages 8 to 19. Each item presents a symptom of anxiety, and participants indicate how true each item is for them on a four-point Likert scale ranging from never true (0) to very true (3). A total score, ranging from 0 to 117, is generated by summing all items. The MASC has high internal consistency and test-retest reliability across 3-month intervals, and established convergent and divergent validity (Muris, Merckelbach, Ollendick, King, & Bogie, 2002). The MASC demonstrated good reliability in this sample (Time 1 α = 0.88, Time 2 α = .93).
Aggressive Behavior
A revised version of The Revised Peer Experiences Questionnaire (RPEQ; Prinstein, Boergers, & Vernberg, 2001) was used to assess participants’ engagement in aggression toward peers. The RPEQ includes 18 items that assess overt, relational, and reputational aggression toward peers. Participants rate how often they engaged in a specific behavior toward others in the past year (e.g., “I threatened to hurt or beat up another kid”) on a 5-point Likert scale ranging from never (1) to a few times a week (5). The RPEQ has also demonstrated good internal consistency for both versions of the measure (aggressor and victim) as well as for the four subscales, and convergent validity (Prinstein, et al., 2001). The RPEQ demonstrated good internal consistency in this sample (Time 1 α = 0.90, Time 2 α = .91).
Eating pathology
Eating attitudes and behavior were assessed using the Children's Eating Attitudes Test (ChEAT; Maloney, McGuire, & Daniels, 1988). The ChEAT is a 26-item measure that assesses attitudes and behaviors associated with anorexia nervosa and bulimia nervosa. Participants rate how often they engage in specific behaviors or have specific beliefs about food on a 6-point Likert scale ranging from never (1) to always (6). The ChEAT was scored continuously for the current study, yielding a potential range of scores of 0 to 156. This method has been used in other studies (Barr, Petit, Vigna, & Prior, 2001) yielding sound psychometric properties (McVey, Davis, Tweed, & Shaw, 2004). The ChEAT has demonstrated good test-retest reliability and convergent validity (Maloney, et al., 1988; Smolak & Levine, 1994). The continuously scored ChEAT was internally consistent in this sample (Time 1 α = 0.94, Time 2 α = .96).
Emotion Dysregulation Measures
Poor Emotional Understanding
Emotional understanding was assessed using an 8-item subscale from the Emotion Expression Scale for Children (EESC; Penza-Clyve & Zeman, 2002) that provides statements involving lack of emotional awareness and understanding. Children respond to items on a 5-point Likert scale ranging from not at all true (1) to extremely true (5). The 8 items are summed to generate a total score ranging from 8 to 40. Higher scores on this subscale reflect lack of emotional understanding. Representative items from this scale are, “I have feelings that I can’t figure out” and “I often do not know how I am feeling.” The EESC has high internal consistency and moderate test-retest reliability, and the construct validity of the measure has been established (Penza-Clyve & Zeman, 2002). This scale has been used with early adolescents (Sim & Zeman, 2005, 2006). This subscale demonstrated good reliability in this sample (Time 1 α = .82, Time 2 α = .92).
Dysregulated Emotion Expression
The Children's Sadness Management Scale (CSMS) and Anger Management Scale (CAMS) assess both adaptive and maladaptive aspects of emotion expression and regulation for the specific emotions of sadness and anger (Zeman, Shipman, & Penza-Clyve, 2001). We used the Dysregulation subscale of each of these measures, which assesses the extent to which children engage in maladaptive or inappropriate expressions of emotion, such as excessive crying. Higher scores on this scale reflect higher levels of emotion dysregulation. The CSMS contains 12 items, and the CAMS contains 11 items. Children respond on a 3-point Likert scale ranging from hardly ever (1) to often (3). The Dysregulation scale for each measure contains 3 items that are summed to create scores ranging from 3 to 9. The scales have demonstrated adequate reliability, and their construct validity has been established (Zeman, et al., 2001). These scales have been used in prior research with early adolescents (Sim & Zeman, 2005, 2006). Representative items from the dysregulation scale are, “I attack whatever it is that is making me angry,” (CAMS) and “I cry and carry on when I’m sad” (CSMS). The Dysregulation subscale of the CSMS (Time 1 α = 0.61, Time 2 α = .60) and CAMS (Time 1 α =0.56, Time 2 α = .66) each demonstrated adequate reliability.
Rumination
The Children's Response Styles Questionnaire (CRSQ; Abela, et al., 2002) is a 25-item scale that assesses the extent to which children respond to sad feelings with rumination, defined as self-focused thought concerning the causes and consequences of depressed mood, distraction, or problem-solving. The measure is modeled after the Response Styles Questionnaire (Nolen-Hoeksema & Morrow, 1991) that was developed for adults. For each item, youth are asked to rate how often they respond in that way when they feel sad on a 4-point Likert scale ranging from almost never (1) to almost always (4). The rumination subscale includes 13 items that are summed to generate a score ranging from 13 to 42. Sample items include: “Think about a recent situation wishing it had gone better” and “Think why can’t I handle things better?” The reliability and validity of the CRSQ have been demonstrated in samples of early adolescents (Abela, et al., 2002). The CRSQ rumination scale demonstrated good reliability in this study (Time 1 α = 0.86, Time 2 α = .90).
Procedure
Participants completed study questionnaires during their homeroom period. Symptom and emotion regulation measures were each assessed initially at Time 1 and again seven months later at Time 2 . This time frame was chosen to allow the maximum time between assessments while ensuring that all assessments occurred within the same academic year to avoid high attrition. Participants were assured of the confidentiality of their responses and the voluntary nature of their participation. The study was conducted in compliance with the Yale Institutional Review Board.
Data Analysis
Structural equation modeling was used to examine study hypotheses using AMOS 6.0 software (Arbuckle, 2005). Analyses were conducted using the full information maximum likelihood estimation method, which estimates means and intercepts to handle missing data. Both emotion dysregulation and symptoms were modeled as latent variables. We tested two measurement models for emotion dyresgulation. The first included four observed variables representing distinct emotion regulation processes: emotional understanding, dysregulated expression of sadness and of anger, and rumination. The second measurement model included three inter-related latent factors representing each of these emotion regulation processes separately (i.e., emotional understanding, dysregulated expression, and rumination). Each of the four psychopathology outcomes was measured with one scale; as such, latent factors were created using parcels of items from each scale. Parcels were created using the domain representative approach, which accounts for the multidimensionality of each of the psychopathology outcomes (Little, Cunningham, Shahar, & Widaman, 2002). Four parcels were created for each symptom outcome, and each parcel included items from the various subscales of that measure. In structural equation modeling, the use of parcels to model constructs as latent factors, as opposed to using an observed variable representing a total scale score, confers a number of psychometric advantages including greater reliability, reduction of error variance, and increased efficiency (Little, et al., 2002).
We first tested each of the measurement models for emotion dysregulation to determine which model provided the best fit to the data. To test the longitudinal hypotheses, emotion dysregulation at Time 1 was examined as a predictor of Time 2 symptoms, controlling for symptoms at Time 1. This hypothesis was tested by estimating a single model that included all four outcomes of interest (depression, anxiety, aggression, and eating pathology) and allowed us to model the inter-correlations among the four outcomes. Next, we estimated a second model examining each of the four types of symptoms at Time 1 as predictors of emotion dysregulation at Time 2, controlling for emotion dysregulation at Time 1. All analyses controlled for gender and race/ethnicity.
Results
Attrition
Analyses comparing participants who completed both assessments to those who did not revealed that participants who completed the baseline but not the follow-up assessment were more likely to be female, χ2 = 6.85, p < .01, from a single-parent household, χ2 = 8.93, p < .01, and to have lower levels of eating pathology, F(1, 761) = 6.43, p < .05, η2 = 0.01, but did not differ in grade level, race/ethnicity, baseline anxiety, depression, or aggressive behavior, or emotion regulation characteristics (p-values > 0.10). Participants who were present at Time 2 but not Time 1 were not included in analyses.
Descriptive Statistics
Table 1 displays the mean and standard deviation of all measures at each time point and the zero-order correlations among all study measures. The means in this sample are similar to values obtained in other samples of early adolescents (i.e., within 1 standard deviation) (Muris, et al., 2002; Penza-Clyve & Zeman, 2002; Twenge & Nolen-Hoeksema, 2002; Zeman, et al., 2001). Each of the emotion processes were positively inter-correlated, indicating that dysregulation in one of these processes was associated with dysregulation in the others. As expected, emotion dysregulation was positively associated with all four types of symptomatology, which were themselves positively inter-related.
Table 1.
Correlations, means, and standard deviations of Time 1 symptoms and emotion dysregulation.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. CDI T1 | — | |||||||||||||||
| 2. MASC Tl | .28** | — | ||||||||||||||
| 3. RPEQ Tl | .31** | .11** | — | |||||||||||||
| 4. ChEAT Tl | 32** | .17** | .35** | — | ||||||||||||
| 5. EESC Tl | .40** | .42** | .23** | .19** | — | |||||||||||
| 6. CSMS Tl | .21** | .31** | .20** | .22** | .30** | — | ||||||||||
| 7. CAMS TI | .25** | .01 | .26** | .15** | .19** | .20** | — | |||||||||
| 8. CRSQ Tl | .42** | .55** | .16** | .18** | .56** | .35** | .16** | — | ||||||||
| 9. CDI T2 | .54** | .13** | .28** | .24** | .23** | .17** | .24** | .23** | — | |||||||
| 10. MASC T2 | .24** | .53** | .14** | .30** | .31** | .25** | .02 | .35** | .33** | — | ||||||
| ll. RPEQ T2 | .23** | .12** | .38** | .15** | .16** | .08* | .17** | .17** | .27** | .20** | — | |||||
| l2. ChEAT T2 | .21** | .18** | .23** | .18** | .15** | .11** | .06 | .19** | .27** | .22** | .32** | — | ||||
| l3. EESC T2 | .25** | .34** | .15** | .29** | .40** | .20** | .13** | .36** | .33** | .50** | .33** | .18** | — | |||
| l4. CSMS T2 | .11** | .21** | .13** | .12** | .15** | .21** | .05 | .24** | .15** | .34** | .23** | .12** | .33** | — | ||
| l5. CAMS T2 | .18** | .10** | .19** | .13** | .22** | .15** | .30** | .20** | .18** | .17** | .24** | .05 | .32** | .32** | — | |
| l6. CRSQ T2 | .35** | .41** | .17** | .11** | .19** | .27** | .09* | .48** | .44** | .69** | .28** | .23** | .59** | .40** | .24** | — |
| Mean and (SD) | 9.67 (6.44) | 40.20 (15.39) | 5.73 (6.18) | 36.75 (26.26) | 18.67 (7.02) | 4.71 (1.50) | 5.43 (1.63) | 10.84 (7.65) | 10.63 (8.15) | 34.80 (18.05) | 6.69 (6.80) | 38.52 (29.63) | 18.40 (7.47) | 4.79 (1.53) | 5.52 (1.73) | 10.18 (8.07) |
Note: CDI = Children's Depression Inventory; MASC = Multidimensional Anxiety Scale for Children; RPEQ = Revised Peer Experiences Scale (aggressive behavior); ChEAT = Children's Eating Attitudes Test; EESC = Emotion Expression Scale for Children; CSMS = Children's Sadness Management Scale; CRSQ = Children's Response Styles Questionnaire;
p < 0.05
p < 0.01.
Measurement Model of Emotion Dysregulation
The first measurement model of emotion dysregulation was constructed using four indicator variables reflecting distinct types of emotion dysregulation: poor emotional understanding, dysregulated expression of anger and of sadness, and ruminative responses to distress. Hu and Bentler (1999) recommend that values of the comparative fit index (CFI) exceeding .95 indicate adequate fit and that the root-mean-square error of approximation (RMSEA) should be less than 0.06. For the hypothesized model, χ2(2) = 1.21, p = .299, CFI = .99, and RMSEA = .01 (90% CI: .00-.06). Thus, all fit indices indicated that the single-factor measurement model of emotion dysregulation fit the data very well. Because adding more parameters to a model typically improve the fit, the Akaike Information Criteria (AIC) was also used to compare the two measurement models; AIC takes into account both model fit and the number of parameters included in the model (Burnham & Anderson, 2002). Smaller values indicate better fit. For the single factor model, AIC = 26.4.
The second measurement model of emotion dysregulation was constructed using three inter-correlated latent factors representing poor emotional understanding, dysregulated expression (including anger and sadness), and rumination. Latent variables were constructed from parcels of items from each of these scales using the domain representative approach. Although this model also demonstrated adequate fit, it did not fit the data as well as the single-factor model: χ2(32) = 83.0, p < .001, CFI = .98, and RMSEA = .04 (90% CI: .03-.04). The AIC for the three-factor model was considerably higher than for the single factor model (AIC = 149.0). Therefore, we used the single factor model of emotion dysregulation in all subsequent analyses.
Measurement Models of Symptomatology
We next examined the fit of our measurement models for each the four types of psychopathology. Fit indices indicated that each of these models fit the data well: depression, χ2(2) = 1.83, p = .400, CFI = .99, and RMSEA = .01 (90% CI: .00-.05); anxiety, χ2(2) = 9.95, p = .007, CFI = .99, and RMSEA = .06 (90% CI: .02-.09); aggressive behavior, χ2(2) = 2.25, p = .324, CFI = .99, and RMSEA = .01 (90% CI: .00-.06); and eating pathology, χ2(2) = 9.86, p = .007, CFI = .99, and RMSEA = .06 (90% CI: .02-.09).
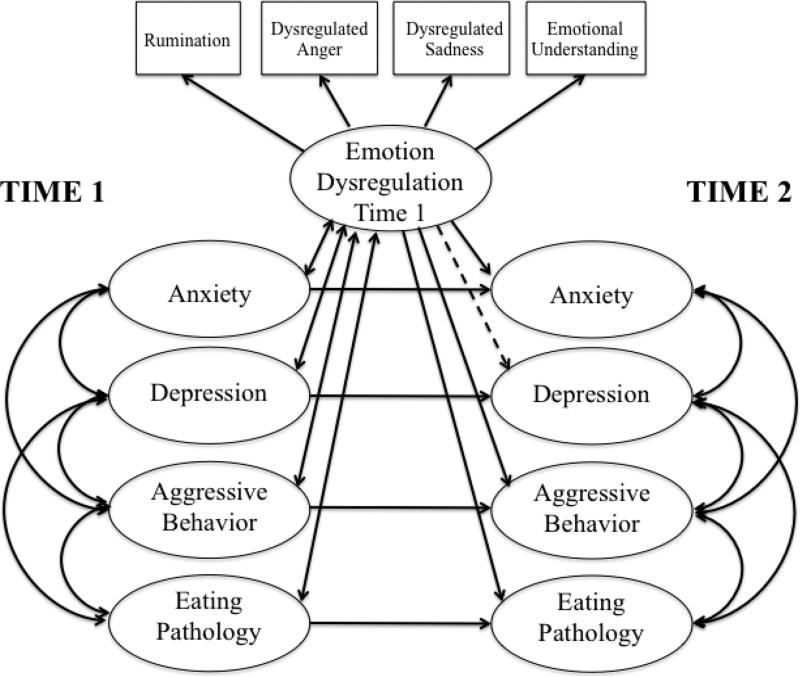
Emotion Dysregulation Predicting Symptoms
We next estimated a model examining the longitudinal association between emotion dysregulation at Time 1 and each of the four types of psychopathology at Time 2, controlling for Time 1 psychopathology. This model was estimated including all four types of psychopathology simultaneously to adjust for the inter-relations between each of the outcomes. The covariance between each type of psychopathology at Time 1 and between emotion dysregulation and each type of psychopathology at Time 1 were also estimated in the model (see Figure 2). In this model, Time 1 emotion dysregulation was significantly associated with Time 2 symptoms of anxiety (β = .19, p < .001), aggression (β = .18, p < .001), and eating pathology (β = .20, p < .001), controlling for Time 1 symptomatology. In contrast, Time 1 emotion dysregulation was not associated with depressive symptoms at Time 2 after adjustment for Time 1 psychopathology, (β = .01, p = .879). The model fit the data well, χ2(641) = 1615.1, p < .001, CFI = .96, RMSEA = .03 (90% CI: .03-.04).
Figure 2.
Note. Figure represents final structural equation model of Time 1 emotion dysregulation predicting Time 2 psychopathology, controlling for psychopathology at Time 1. See Results section for standardized path coefficients (lines drawn with a single-headed arrow). All paths shown are significant (p< .05), except those drawn with broken lines. All constructs were modeled as latent variables. Due to space constraints, indicator variables for psychopathology variables and covariates (sex and race/ethnicity) are not displayed.
Psychopathology Predicting Emotion Dysregulation
To evaluate whether the presence of psychopathology at Time 1 was associated prospectively with emotion dysregulation at Time 2, we estimated a model with each of the four types of psychopathology at Time 1 predicting emotion dysregulation at Time 2, controlling for Time 1 emotion dysregulation. The covariance among the four types of psychopathology was also modeled. Emotion dysregulation at Time 2 was not associated with Time 1 anxiety symptoms (β = .06, p = .351), depressive symptoms (β = .00, p = .973), aggressive behavior (β = .07, p = .131), or eating pathology (β = .03, p = .517), after controlling for Time 1 emotion dysregulation. The model demonstrated good fit to the data, χ2(284) = 832.0, p < .001, CFI = .96, RMSEA = .04 (90% CI: .03-.04).
Discussion
Accumulating evidence suggests that emotion regulation deficits are associated with a wide range of psychopathological outcomes in children and adults (Aldao & Nolen-Hoeksema, 2010; Aldao, et al., 2010; Bohnert, et al., 2003; Silk, et al., 2003; Sim & Zeman, 2006; Zeman, et al., 2002). Because nearly all of this research has been cross-sectional, however, it is unknown whether emotion dysregulation is a risk factor for the development of psychopathology or whether emotion regulation deficits are simply a consequence of having a mental health problem. Clarifying the direction of association between emotion regulation and psychopathology has implications both for theoretical conceptualizations of emotion regulation (Campos, Frankel, & Camras, 2004; Cole, Martin, & Dennis, 2004) and for interventions aimed at preventing and treating adolescent psychopathology. The current study utilized prospective data from a large sample of adolescents that included multiple measures of emotion regulation and symptoms of psychopathology to illuminate this issue. We found that emotion regulation deficits predicted subsequent changes in symptoms of anxiety, aggressive behavior, and eating pathology but not depression. In contrast, psychopathology did not predict subsequent changes in emotion dysregulation. These findings provide perhaps the strongest evidence to date for the role of emotion dysregulation as a risk factor for adolescent psychopathology. Moreover, our results indicate that psychopathology is not associated with increases in emotion dysregulation over time, suggesting that emotion regulation deficits are a predictor and not a consequence of adolescent psychopathology.
Conceptual models of emotion regulation posit that regulation involves processes related to the evaluation and interpretation of emotional information, the modulation of emotional expression, and the management of emotional experiences, responses to emotions, and related thoughts and behaviors (Cole, et al., 2004; Mennin, Heimberg, Turk, & Fresco, 2005; Thompson, 1994). We examined the inter-relations of three of these distinct emotional processes and their associations with adolescent psychopathology. Consistent with prior studies documenting that diverse emotion processes related to emotional awareness and the management of emotional experiences loaded onto a unitary dimension of emotion regulation (Aldao & Nolen-Hoeksema, 2010; Mennin, et al., 2007), we found that emotional understanding, expression of sadness and of anger, and ruminative responses to distress loaded onto a single latent factor of emotion dysregulation. This model provided a better fit to the data than a more differentiated three-factor model. Our finding of a single emotion dysregulation factor suggests that adolescents who are better able to understand their emotional experiences also are more likely to express their emotions and respond to negative affect in adaptive ways. This is not particularly surprising, given that an understanding of one's own emotions is critical for the adaptive expression and management of emotional experiences (Saarni, 1999). Moreover, both emotional understanding and management have been found to be mediated by common neural mechanisms (Lieberman et al., 2007). These findings contrast, however, with some prior work suggesting greater differentiation of emotion regulation processes (Garnefski, Kraaij, & Spinhoven, 2001; Gratz & Roemer, 2004). One explanation for this discrepancy is that these previous studies examined a wider range of emotion regulation facets than we examined in the present study, including acceptance of one's emotions, reactivity to emotional experiences, and ability to engage in goal-directed behavior and refrain from impulsivity (Gratz & Roemer, 2004). Alternatively, it may be that emotion regulation skills become increasingly differentiated across development. The prefrontal cortex undergoes considerable remodeling during adolescence, particularly in regions known to be associated with emotion regulation (e.g., the anterior cingulate cortex) (Cohen, 2006; Giedd, 2004). These developmental changes may be accompanied by greater differentiation of emotion regulation strategies that require cognitive control (e.g., engaging in goal-directed behavior) or higher order reflective processing (e.g., acceptance of emotional experiences). Because prior studies finding greater differentiation of emotion regulation processes have focused on older samples, the different pattern of findings may relate to changes in the structure of emotion regulation across development. Examination of developmental changes in the structure and inter-relatedness of different facets of emotion regulation represents an important area for future research.
Emotion dysregulation predicted the subsequent development of multiple forms of psychopathology, including anxiety, aggression, and eating pathology, and the strength of the prospective association was similar across outcomes. These results suggest that emotion regulation deficits are a fairly global risk factor for adolescent psychopathology, consistent with recent evidence from a cross-sectional study of young adults (Aldao & Nolen-Hoeksema, 2010) and a meta-analysis examining the associations of emotion regulation with depression, anxiety, substance abuse, and disordered eating (Aldao, et al., 2010). The current findings thus bolster recent conceptualizations of emotion dysregulation as a transdiagnostic factor relevant to multiple types of psychopathology (Ehring & Watkins, 2008; Kring & Sloan, 2010; Moses & Barlow, 2006; Watkins, 2008). The significant associations between emotion dysregulation and psychopathology reported here mirror findings from a number of cross-sectional studies documenting emotion regulation deficits in youths with anxiety disorders (Southam-Gerow & Kendall, 2000; Suveg & Zeman, 2004), problematic aggressive behavior (Bohnert, et al., 2003; Cole, et al., 1994; Dearing, et al., 2002; Shields & Cicchetti, 1998), and disordered eating (Sim & Zeman, 2005, 2006). Our findings regarding the prospective association of emotion dysregulation with subsequent symptom development extend this previous work, supporting theoretical conceptualizations of emotion regulation deficits as an important determinant of psychopathology (Gross & Muñoz, 1995; John & Gross, 2004; Mennin, 2004; Mennin, et al., 2005; Moses & Barlow, 2006).
However, emotion dysregulation was not associated with later increases in depressive symptoms. These results contradict somewhat the findings of previous cross-sectional and experience sampling studies documenting associations between emotion regulation deficits and adolescent depressive symptoms (Garber, et al., 1995; Sheeber, Allen, Davis, & Sorensen, 2000; Silk, et al., 2003). These findings were surprising because rumination was included as one indicator of emotion dysregulation, and a robust prospective association between rumination and depressive symptoms has been reported in a wide range of studies (Nolen-Hoeksema & Morrow, 1991), including among children and adolescents (Abela, et al., 2002; Broderick & Korteland, 2004; Burwell & Shirk, 2007). Here, all of the individual emotion regulation measures, including rumination, demonstrated significant cross-sectional relationships with depressive symptoms (see Table 1). Post-hoc linear regression analyses indicated that rumination and dysregulated anger and sadness expression predicted changes in depressive symptoms, but emotional understanding did not. The lack of association between emotional understanding and depression likely contributed to our finding of no prospective relationship between composite emotion dysregulation and depressive symptoms. It may be that adolescents who develop symptoms of depression are not unaware of their emotional experiences; rather, they may be all too aware of their negative emotions. Indeed, the self-focus on one's feelings that defines rumination suggests that adolescents who are at risk for depression may attend to their emotions—particularly negative emotions—too frequently, which contributes to the development of depressive symptoms over time (Nolen-Hoeksema & Morrow, 1991). Given the novelty of this finding, however, the lack of a prospective relationship between emotion dysregulation and depressive symptoms should be interpreted with caution. Future longitudinal studies are needed to determine whether other aspects of emotion dysregulation that were not measured in the current study—such as acceptance of emotions—are associated specifically with risk for adolescent depression.
One of the central unresolved questions in the field of emotion regulation is whether dysregulated emotions are risk factors for, versus sequelae of, psychopathology and negative affect (Campos et al., 2004). The current study provides novel evidence indicating that the presence of psychopathology does not predict subsequent changes in emotion dysregulation over time. Changes in emotion dysregulation were unrelated to baseline symptoms of anxiety, depression, aggressive behavior, or eating pathology. Although these findings suggest that emotion dysregulation is not a consequence of psychopathology, additional research is needed to determine whether the onset of psychiatric disorders predicts changes in emotion regulation and whether these results hold for different periods of developmental risk transitions (e.g., the transition from adolescence to young adulthood).
Our findings have important implications for preventive interventions targeting adolescent mental health problems. Empirically-supported treatments and prevention programs for each of the types of adolescent psychopathology examined here rely heavily on cognitive-behavioral techniques (Clarke, DeBar, & Lewinsohn, 2003; Gillham, Reivich, Jaycox, & Seligman, 1995; Kazdin, 2003; Schmidt et al., 2007; Stice, Shaw, Burton, & Wade, 2006). Such interventions may benefit from the inclusion of techniques targeting emotion regulation processes. Inclusion of techniques specifically aimed at increasing emotional awareness and understanding, effectively managing expressions of sadness and of anger, and reducing engagement in rumination could improve the efficacy of preventive and treatment interventions. Several existing interventions provide a template for how to incorporate such techniques into cognitive-behavioral treatments. For example, a recent treatment specifically designed to reduce ruminative self-focus led to significant reductions in depression and associated comorbidity in a small sample of adults (Watkins et al., 2007). This treatment utilized traditional cognitive-behavioral techniques, including functional analysis, to identify and reduce engagement in rumination and to help individuals adopt thinking styles that promote problem solving and adaptive processing of emotional experiences (Watkins et al. 2007). Mennin (2004, 2006) developed a treatment for anxiety disorders that specifically aims to improve emotional awareness and understanding and decrease engagement in maladaptive emotion regulation strategies. Although both of these interventions warrant further empirical evaluation, the techniques targeting emotion regulation may provide additional clinical benefits if incorporated into existing evidence-based prevention programs for adolescent psychopathology. Kovacs et al. (2006) have developed a particularly promising intervention specifically for children and adolescents targeting self-regulation of distress. The intervention seeks to delineate children's typical responses to distressing situations, identify the contexts that elicit maladaptive management of distress, and replace habitual maladaptive responses to distress with alternative responses from the child's own repertoire of emotion regulation skills to ameliorate negative mood (Kovacs et al., 2006). Several additional treatments that incorporate emotion-focused techniques into cognitive-behavioral therapy for child and adolescent internalizing disorders have been developed and await evaluation in randomized trials (Suveg, Kendall, Comer, & Robin, 2006; Trosper, Buzzella, Bennett, & Ehrenreich, 2009). These treatments each utilize techniques that have direct relevance for preventive interventions targeting emotion dysregulation. Empirical evaluation of preventive interventions that include techniques aimed at promoting adaptive understanding and regulation of emotions represents an important area for future research.
Study findings should be interpreted in light of the following limitations. First, we relied on self-reported symptoms of psychopathology rather than DSM-IV-TR diagnoses based on a structured clinical interview. Although administration of a structured interview to establish diagnoses would represent a methodological improvement, the validity of the self-report measures used in this study is well-established (Timbremont, Braet, & Dreessen, 2004; Wood, Piacentini, Bergman, McCracken, & Barrios, 2002). Nonetheless, future research is needed to examine the association between emotion regulation processes and the development of DSM-IVTR disorders. Our use of self-report measures of emotion regulation is another limitation of the study. Utilization of self-report measures in research examining emotion regulation in youth presents challenges because of the difficulties inherent in disentangling initial emotion activation from emotion regulation (Cole, et al., 2004) and with reporting on one's typical responses to emotional experiences. Biases associated with memories of affective experiences, such as a tendency to remember the most recent experiences or the experiences associated with the most intense emotions (Fredrickson, 2000; Stone et al., 1998), may influence reports of trait emotion regulation. Increasingly, measures that do not rely on self-report, such as psychophysiological and observational measures, are being used to assess emotion and emotion regulation (Chaplin, 2006; Cole, Zahn-Waxler, Fox, Usher, & Welsh, 1996). Such measures are useful in experimental settings to examine state changes in emotion and physiological responses and subsequent regulatory behavior, but they are unfeasible for use with large community samples. Given the size of the sample and the longitudinal nature of the current investigation, utilization of self-report measures presented the only reasonable option for assessing emotion regulation. Moreover, recent evidence suggests good concordance between self-reported and physiologic measures of emotion regulation among youth (Hessler & Katz, 2007), and numerous prior studies examining emotion regulation and youth psychopathology have also relied on self-report measures of emotion regulation (Sim & Zeman, 2005; Southam-Gerow & Kendall, 2000; Zeman, et al., 2002). Fourth, our assessment of emotion regulation was not exhaustive. We focused here on emotional understanding, regulation of sadness and of anger, and rumination but did not measure other aspects of emotion regulation likely to be relevant to risk for psychopathology, including negative reactivity to emotional experiences and management of fear (Mennin, et al., 2005; Mennin, et al., 2007). Examination of the associations of these aspects of emotion regulation with adolescent psychopathology is an important area for future research. Finally, although we believe that the racial/ethnic diversity of our sample represents a strength of the study, the preponderance of adolescents of Hispanic ethnicity in our sample may limit the generalizability of our findings. These findings therefore warrant replication in samples with a more representative ethnic distribution.
We extend the literature linking emotion regulation processes to youth psychopathology by providing, to our knowledge, the first longitudinal evidence documenting the role of emotion dysregulation as a risk factor for the development of adolescent psychopathology. Emotion dysregulation predicted subsequent increases in symptoms of anxiety, aggressive behavior, and disordered eating but not depression. Importantly, the results provided no evidence for an association between psychopathology and subsequent increases in emotion dysregulation, indicating that the presence of psychopathology did not render adolescents less able to effectively manage their emotions. Thus, emotion dysregulation appears to serve as a risk factor for, rather than a consequence of, psychopathology in adolescents. These findings have important implications for preventive interventions targeting adolescents and suggest that techniques that promote emotional understanding and the adaptive expression and modulation of negative emotions should be incorporated into existing interventions.
Highlights.
Emotion dysregulation predicts adolescent anxiety, aggression, and eating pathology.
Emotion dysregulation is not associated with increases in depression.
The presence of psychopathology does not predict increases in emotion dysregulation.
Poor emotional understanding, expressive dysregulation, and rumination forma singlelatent factor.
Emotion dysregulation is a risk factor for adolescent psychopathology.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abela JR, Brozina K, Haigh EP. An examination of the response styles theory of depression in third- and sixth-grade children: a short-term longitudinal study. Journal of Abnormal Child Psychology. 2002;30:515–527. doi: 10.1023/a:1019873015594. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S. Specificity of cognitive emotion regulation strategies: A transdiagnostic examination. Behaviour Research and Therapy. 2010;48:974–983. doi: 10.1016/j.brat.2010.06.002. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Andersen SL, Teicher MH. Stress, sensitive periods and maturational events in adolescent depression. Trends in Neuroscience. 2008;31:183–191. doi: 10.1016/j.tins.2008.01.004. [DOI] [PubMed] [Google Scholar]
- Arbuckle JL. AMOS 6.0 User's Guide. SPSS, Inc.; Chicago: 2005. [Google Scholar]
- Barr SI, Petit MA, Vigna YM, Prior JC. Eating attitudes and habitual calcium intake in peripubertal girls are associated with initial bone mineral content and its change over 2 years. Journal of Bone and Mineral Research. 2001;16:940–947. doi: 10.1359/jbmr.2001.16.5.940. [DOI] [PubMed] [Google Scholar]
- Bohnert AM, Crnic KA, Lim KG. Emotional competence and aggressive behavior in school-age children. Journal of Abnormal Child Psychology. 2003;31:79–91. doi: 10.1023/a:1021725400321. [DOI] [PubMed] [Google Scholar]
- Broderick PC, Korteland C. A prospective study of rumination and depression in early adolescence. Journal of Clinical Child and Adolescent Psychology. 2004;9:383–394. [Google Scholar]
- Burnham KP, Anderson DR. Model selection and multimodel inference: A practical information-theoretic approach. Springer-Verlag; New York, NY: 2002. [Google Scholar]
- Burwell RA, Shirk SR. Subtypes of rumination in adolescence: associations between brooding, reflection, depressive symptoms, and coping. Journal of Clinical Child and Adolescent Psychology. 2007;36:56–65. doi: 10.1080/15374410709336568. [DOI] [PubMed] [Google Scholar]
- Campos JJ, Frankel CB, Camras LA. On the nature of emotion regulation. Child Development. 2004;75:377–394. doi: 10.1111/j.1467-8624.2004.00681.x. [DOI] [PubMed] [Google Scholar]
- Chaplin TM. Anger, happiness, and sadness: Associations with depressive symptoms in late adolescence. Journal of Youth and Adolescence. 2006;35:977–986. [Google Scholar]
- Clarke GN, DeBar LL, Lewinsohn PM. Cognitive-behavioral group treatment for adolescent depression. In: Kazdin AE, Weisz JR, editors. Evidence-based psychotherapies for children and adolescents. Guilford Press; New York: 2003. pp. 120–134. [Google Scholar]
- Cohen RA. Early life stress and morphometry of the adult anterior cingulate cortex and caudate nuclei. Biological Psychiatry. 2006;59:975–982. doi: 10.1016/j.biopsych.2005.12.016. [DOI] [PubMed] [Google Scholar]
- Cole PM, Martin SE, Dennis TA. Emotion regulation as a scientific construct: methodological challenges and directions for child development research. Child Development. 2004;75:317–333. doi: 10.1111/j.1467-8624.2004.00673.x. [DOI] [PubMed] [Google Scholar]
- Cole PM, Zahn-Waxler C, Fox NA, Usher BA, Welsh JD. Individual differences in emotion regulation and behavior problems in preschool children. Journal of Abnormal Psychology. 1996;105:518–529. [PubMed] [Google Scholar]
- Cole PM, Zahn-Waxler C, Smith D. Expressive control during a disappointment: Variations related to preschoolers’ problem behaviors. Developmental Psychology. 1994;30:835–846. [Google Scholar]
- Connecticut Department of Education . Strategic School Profile 2005-2006: New Britain Public Schools. Connecticut Department of Education; Hartford, CT: 2006. [Google Scholar]
- Cummings EM. Coping with background anger in early childhood. Child Development. 1987;58:976–984. doi: 10.1111/j.1467-8624.1987.tb01433.x. [DOI] [PubMed] [Google Scholar]
- Dearing KF, Hubbard JA, Ramsden SR, Parker EH, Relyea N, Smithmyer CM, Flanagan KD. Children's self-reports about anger regulation: Direct and indirect links to social preference and aggression. Merrill-Palmer Quarterly. 2002;48:308–336. [Google Scholar]
- Denham SA. Social cognition, prosocial behavior, and emotion in preschoolers: Contextual validation. Child Development. 1986;57:194–201. [Google Scholar]
- Denham SA. Emotional development in young children. Guilford Press; New York: 1998. [Google Scholar]
- Denham SA, Blair KA, DeMulder E, Levitas J, Sawyer K, Auerbach-Major S, Queenan P. Preschool emotional competence: Pathway to social competence. Child Development. 2003;74:238–256. doi: 10.1111/1467-8624.00533. [DOI] [PubMed] [Google Scholar]
- Denham SA, McKinley M, Couchoud EA, Holt R. Emotional and behavioral predictors of preschool peer ratings. Child Development. 1990;61:1145–1152. [PubMed] [Google Scholar]
- Ehring T, Watkins E. Repetitive negative thinking as a transdiagnostic process. International Journal of Cognitive Therapy. 2008;1:192–205. [Google Scholar]
- Eisenberg N, Fabes RA, Bernzweig J, Karbon M, Poulin R, Hanish L. The relations of emotionality and regulation to preschoolers’ social skills and sociometric status. Child Development. 1993;64:1418–1438. [PubMed] [Google Scholar]
- Eisenberg N, Fabes RA, Guthrie IK, Reiser M. Dispositional emotionality and regulation: Their role in predicting quality of social functioning. Journal of Personality and Social Psychology. 2000;78:136–157. doi: 10.1037//0022-3514.78.1.136. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Fabes RA, Murphy BC, Maszk P, Smith M, Karbon M. The role of emotionality and regulation in children's social functioning: A longitudinal study. Child Development. 1995;66:1360–1384. [PubMed] [Google Scholar]
- Eisenberg N, Guthrie IK, Fabes RA, Shepard SA, Losoya S, Murphy BC, Jones S, Poulin R, Reiser M. Prediction of elementary school children's externalizing problem behaviors from attentional and behavioral regulation and negative emotionality. Child Development. 2000;71:1367–1382. doi: 10.1111/1467-8624.00233. [DOI] [PubMed] [Google Scholar]
- Fredrickson BL. Extracting meaning from past affective experiences: The importance of peaks, ends, and specific emotions. Cognition and Emotion. 2000;14:577–606. [Google Scholar]
- Garber J, Braafladt N, Weiss B. Affect regulation in depressed and nondepressed children and young adolescents. Development and Psychopathology. 1995;7:93–115. [Google Scholar]
- Garnefski N, Kraaij V, Spinhoven P. Negative life events, cognitive emotion regulation and emotional problems. Personality and Individual Differences. 2001;30:1311–1327. [Google Scholar]
- Giedd JN. Structural magnetic resonance imaging of the adolescent brain. Annals of the New York Academy of Sciences. 2004;1021:77–85. doi: 10.1196/annals.1308.009. [DOI] [PubMed] [Google Scholar]
- Gillham JE, Reivich KJ, Jaycox LH, Seligman MEP. Prevention of depressive symptoms in schoolchildren: Two-year follow-up. Psychological Science. 1995;6:343–351. [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and validation of the Difficulties with Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment. 2004;26:41–54. [Google Scholar]
- Gross JJ. Antecedent- and response-focused emotion regulation: Divergent consequences for expression, experience, and physiology. Journal of Personality and Social Psychology. 1998a;24:224–237. doi: 10.1037//0022-3514.74.1.224. [DOI] [PubMed] [Google Scholar]
- Gross JJ. The emerging field of emotion regulation: An integrative review. Review of General Psychology. 1998b;2:271–299. [Google Scholar]
- Gross JJ, John OP. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. Journal of Personality and Social Psychology. 2003;85:348–362. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- Gross JJ, Muñoz RF. Emotion regulation and mental health. Clinical Psychology: Science and Practice. 1995;2:151–164. [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. J Abnorm Psychol. 1998;107(1):128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- Harvey AG, Watkins E, Mansell W, Shafran R. Cognitive behavioural processes across psychological disorders. Oxford University Press; Oxford, United Kingdom: 2004. [Google Scholar]
- Hessler DM, Katz LF. Children's emotion regulation: Self-report and physiological response to peer provocation. Developmental Psychology. 2007;43:27–38. doi: 10.1037/0012-1649.43.1.27. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indices in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Hubbard JA, Coie JD. Emotional correlates of social competence in children's peer relationships. Merrill-Palmer Quarterly. 1994;40:1–20. [Google Scholar]
- John OP, Gross JJ. Healthy and unhealthy emotion regulation: Personality processes, individual differences, and life span development. Journal of Personality. 2004;72:1301–1334. doi: 10.1111/j.1467-6494.2004.00298.x. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Problem-solving skills training and parent management training for conduct disorder. In: Kazdin AE, Weisz JR, editors. Evidence-based psychotherapies for children and adolescents. Guilford Press; New York: 2003. pp. 244–262. [Google Scholar]
- Keltner D, Moffit TE, Stouthamer-Loeber M. Facial expressions of emotion and psychopathology in adolescent boys. Journal of Abnormal Psychology. 1995;104:644–652. doi: 10.1037//0021-843x.104.4.644. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Children's Depression Inventory manual. Multi-Health Systems; North Tonawanda, NY: 1992. [Google Scholar]
- Kovacs M, Sherrill J, George CJ, Pollack M, Tumuluru RV, Ho V. Contextual emotion-regulation therapy for childhood depression: Description and pilot testing of a new intervention. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45:892–903. doi: 10.1097/01.chi.0000222878.74162.5a. [DOI] [PubMed] [Google Scholar]
- Kring AM, Sloan DM. Emotion regulation in psychopathology: A transdiagnostic approach to etiology and treatment. Guilford; New York: 2010. [Google Scholar]
- Kuyken W, Watkins E, Holden E, Cook W. Rumination in adolescents at risk for depression. Journal of Affective Disorders. 2006;96:39–47. doi: 10.1016/j.jad.2006.05.017. [DOI] [PubMed] [Google Scholar]
- Lane RD, Reiman EM, Axelrod B, Yun L-S, Holmes A, Schwartz GE. Neural correlates of levels of emotional awareness: Evidence of an interactioni between emotion and attention in the anterior cingulate cortex. Journal of Cognitive Neuroscience. 1998;10:525–535. doi: 10.1162/089892998562924. [DOI] [PubMed] [Google Scholar]
- Larson R, Ham M. Stress and “storm and stress” in early adolescence: The relationship of negative events with dysphoric affect. Developmental Psychology. 1993;29:130–140. [Google Scholar]
- Larson R, Lampman-Petraitis C. Daily emotional stress as reported by children and adolescents. Child Development. 1989;60:1250–1126. doi: 10.1111/j.1467-8624.1989.tb03555.x. [DOI] [PubMed] [Google Scholar]
- Larson R, Moneta G, Richards MH, Wilson S. Continuity, stability, and change in daily emotional experience across adolescence. Child Development. 2002;73:1151–1165. doi: 10.1111/1467-8624.00464. [DOI] [PubMed] [Google Scholar]
- Larson R, Richards MH. Daily companionship in late childhood and early adolescence: Changing developmental contexts. Child Development. 1991;62:284–300. doi: 10.1111/j.1467-8624.1991.tb01531.x. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Striegel-Moore RH, Seeley JR. Epidemiology and natural course of eating disorders in young women from adolescence to young adulthood. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39(10):1284–1292. doi: 10.1097/00004583-200010000-00016. [DOI] [PubMed] [Google Scholar]
- Little TD, Cunningham WA, Shahar G, Widaman KF. To parcel or not to parcel: Examining the question, weighing the evidence. Structural Equation Modeling. 2002;9:151–173. [Google Scholar]
- Maloney M, McGuire J, Daniels S. Reliability testing of a children's version of the Eating Attitudes Test. Journal of the American Academy of Child & Adolescent Psychiatry. 1988;5:541–543. doi: 10.1097/00004583-198809000-00004. [DOI] [PubMed] [Google Scholar]
- March JS, Parker JDA, Sullivan K, Stallings P, Conners CK. The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability, and validity. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- McVey GL, Davis R, Tweed S, Shaw BF. Evaluation of a school-based program designed to improve body image satisfaction, global self-esteem, and eating Attitudes and behaviors: A replication study. International Journal of Eating Disorders. 2004;36:1–11. doi: 10.1002/eat.20006. [DOI] [PubMed] [Google Scholar]
- Mennin DS. An emotion regulation treatment for generalized anxiety disorder. Clinical Psychology: Science and Practice. 2004;11:17–29. [Google Scholar]
- Mennin DS. Emotion regulation therapy: An integrative approach to treatment-resistant anxiety disorders. Journal of Contemporary Psychotherapy. 2006;36:95–105. [Google Scholar]
- Mennin DS, Heimberg RG, Turk CL, Fresco DM. Preliminary evidence for an emotion dysregulation model of generalized anxiety disorder. Behaviour Research and Therapy. 2005;43:1281–1310. doi: 10.1016/j.brat.2004.08.008. [DOI] [PubMed] [Google Scholar]
- Mennin DS, Holaway RM, Fresco DM, Moore MT, Heimberg RG. Delineating components of emotion and its dysregulation in anxiety and mood pathology. Behavior Therapy. 2007;38:284–302. doi: 10.1016/j.beth.2006.09.001. [DOI] [PubMed] [Google Scholar]
- Mennin DS, McLaughlin KA, Flanagan T. Emotion regulation deficits in generalized anxiety disorder, social phobia, and their co-occurrence. Journal of Anxiety Disorders. 2009;23:866–871. doi: 10.1016/j.janxdis.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moses EB, Barlow DH. A new unified approach for emotional disorders based on emotion science. Current Directions in Psychological Science. 2006;15:146–150. [Google Scholar]
- Muris P, Merckelbach H, Ollendick T, King N, Bogie N. Three traditional and three new childhood anxiety questionnaires: their reliability and validity in a normal adolescent sample. Behaviour Research and Therapy. 2002;40:753–772. doi: 10.1016/s0005-7967(01)00056-0. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The 1989 Loma Prieta earthquake. Journal of Personality and Social Psychology. 1991;61:115–121. doi: 10.1037//0022-3514.61.1.115. [DOI] [PubMed] [Google Scholar]
- Novick-Kline P, Turk CL, Mennin DS, Hoyt EA, Gallagher CL. Level of emotional awareness as a differentiating variable between individuals with and without generalized anxiety disorder. Journal of Anxiety Disorders. 2005;19:557–572. doi: 10.1016/j.janxdis.2004.06.001. [DOI] [PubMed] [Google Scholar]
- Penza-Clyve S, Zeman J. Initial validation of the emotion expression scale for children (EESC). Journal of Clinical Child and Adolescent Psychology. 2002;31:540–547. doi: 10.1207/S15374424JCCP3104_12. [DOI] [PubMed] [Google Scholar]
- Prinstein MJ, Boergers J, Vernberg EM. Overt and relational aggression in adolescents: Social-psychological adjustment of aggressors and victims. Journal of Clinical Child Psychology. 2001;30:479–491. doi: 10.1207/S15374424JCCP3004_05. [DOI] [PubMed] [Google Scholar]
- Reynolds WM. Assessment of depression in children and adolescents by self-report measures. In: Reynolds WM, Johnston HF, editors. Handbook of depression in children and adolescents. Plenum Press; New York: 1994. pp. 209–234. [Google Scholar]
- Rydell A, Berlin L, Bohlin G. Emotionality, emotion regulation, and adaptation among 5- to 8-year-old children. Emotion. 2003;3:30–47. doi: 10.1037/1528-3542.3.1.30. [DOI] [PubMed] [Google Scholar]
- Saarni C. The development of emotional competence. The Guilford Press; New York: 1999. [Google Scholar]
- Schmidt NB, Eggleston AM, Woolaway-Bickel K, Fitzpatrick KK, Vasey MW, Richey JA. Anxiety Sensitivity Amelioration Training (ASAT): A longitudinal primary prevention program targeting cognitive vulnerability. Journal of Anxiety Disorders. 2007;21:302–319. doi: 10.1016/j.janxdis.2006.06.002. [DOI] [PubMed] [Google Scholar]
- Seidman E, Allen L, Aber JL, Mitchell C, Feiman J. The impact of school transitions in early adolescence on the self-system and perceived social context of poor urban youth. Child Development. 1994;65:507–522. [PubMed] [Google Scholar]
- Sheeber L, Allen N, Davis B, Sorensen E. Regulation of negative affect during mother-child problem-solving interactions: adolescent depressive status and family processes. Journal of Abnormal Child Psychology. 2000;28:467–479. doi: 10.1023/a:1005135706799. [DOI] [PubMed] [Google Scholar]
- Shields A, Cicchetti D. Reactive aggression among maltreated children: The contributions of attention and emotion dysregulation. Journal of Clinical Child Psychology. 1998;27:381–395. doi: 10.1207/s15374424jccp2704_2. [DOI] [PubMed] [Google Scholar]
- Silk JS, Steinberg L, Morris AS. Adolescents’ emotion regulation in daily life: Links to depressive symptoms and problem behaviors. Child Development. 2003;74:1869–1880. doi: 10.1046/j.1467-8624.2003.00643.x. [DOI] [PubMed] [Google Scholar]
- Silk JS, Vanderbilt-Adriance E, Shaw DS, Forbes EE, Whalen DJ, Ryan ND, Dahl R. Resilience among children and adolescents at risk for depression: Mediation and moderation across social and neurobiological context. Development and Psychopathology. 2007;19:841–865. doi: 10.1017/S0954579407000417. [DOI] [PubMed] [Google Scholar]
- Sim L, Zeman J. Emotion regulation factors as mediators between body dissatisfaction and bulimic symptoms in early adolescent girls. Journal of Early Adolescence. 2005;25:478–496. [Google Scholar]
- Sim L, Zeman J. The contribution of emotion regulation to body dissatisfaction and disordered eating in early adolescent girls. Journal of Youth and Adolescence. 2006;35:207–216. [Google Scholar]
- Simmons RG, Blythe DA. Moving into adolescence: The impact of pubertal change and school context. Aldine de Gruyter; Hawthorne, NY: 1987. [Google Scholar]
- Smolak L, Levine MP. Psychometric properties of the Children's Eating Attitudes Test. International Journal of Eating Disorders. 1994;16:275–282. doi: 10.1002/1098-108x(199411)16:3<275::aid-eat2260160308>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- Southam-Gerow MA, Kendall PC. A preliminary study of the emotional understanding of youth referred for treatment of anxiety disorders. Journal of Clinical Child Psychology. 2000;29:319–327. doi: 10.1207/S15374424JCCP2903_3. [DOI] [PubMed] [Google Scholar]
- Spinard TL, Eisenberg N, Cumberland A, Fabes RA, Valiente C, Shepard SA, Reiser M, Losoya S, Guthrie IK. Relation of emotion-related regulation to children's social competence: A longitudinal study. Emotion. 2006;6:498–510. doi: 10.1037/1528-3542.6.3.498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L. Impact of puberty on family relations: Effects of pubertal status and pubertal timing. Developmental Psychology. 1987;23:451–460. [Google Scholar]
- Steinberg L, Avenevoli S. The role of context in the development of psychopathology: A conceptual framework and some speculative propositions. Child Development. 2000;71:66–74. doi: 10.1111/1467-8624.00119. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Dahl R, Keating D, Kupfer DJ, Masten A, Pine D. The study of developmental psychopathology in adolescence: Integrating affective neuroscience with the study of context. In: Cicchetti D, Cohen D, editors. Developmental Psychopathology. Vol. 2. Wiley; New York: 2006. pp. 710–741. [Google Scholar]
- Stice E, Shaw H, Burton E, Wade E. Dissonance and healthy weight eating disorder prevention programs: A randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2006;74:263–275. doi: 10.1037/0022-006X.74.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone AA, Schwartz JE, Neale JM, Shiffman S, Marco CA, Hickcox M, Paty J, Porter LS, Cruise LJ. A comparison of coping assessed by ecological momentary assessment and retrospective recall. Journal of Personality and Social Psychology. 1998;74:1670–1680. doi: 10.1037//0022-3514.74.6.1670. [DOI] [PubMed] [Google Scholar]
- Suveg C, Kendall PC, Comer JS, Robin J. Emotion-focused cognitive-behavioral therapy for anxious youth: A multiple-baseline evaluation. Journal of Contemporary Psychotherapy. 2006;36:77–85. [Google Scholar]
- Suveg C, Zeman J. Emotion regulation in children with anxiety disorders. Journal of Clinical Child and Adolescent Psychology. 2004;33:750–759. doi: 10.1207/s15374424jccp3304_10. [DOI] [PubMed] [Google Scholar]
- Thompson RA. Emotion regulation: A theme in search of definition. Monographs for the Society for Research in Child Development. 1994;59:25–52. [PubMed] [Google Scholar]
- Timbremont B, Braet C, Dreessen L. Assessing depression in youth: Relation between the Children's Depression Inventory and a structured interview. Journal of Clinical Child and Adolescent Psychology. 2004;33:149–157. doi: 10.1207/S15374424JCCP3301_14. [DOI] [PubMed] [Google Scholar]
- Trosper SE, Buzzella BA, Bennett SM, Ehrenreich JT. Emotion regulation in youth with emotional disorders: Implications for a unified treatment approach. Clinical Child and Family Psychology Review. 2009;12:234–254. doi: 10.1007/s10567-009-0043-6. [DOI] [PubMed] [Google Scholar]
- Twenge JM, Nolen-Hoeksema S. Age, gender, race, socioeconomic status, and birth cohort differences on the children's depression inventory: a meta-analysis. Journal of Abnormal Psychology. 2002;111(4):578–588. doi: 10.1037//0021-843x.111.4.578. [DOI] [PubMed] [Google Scholar]
- Watkins ER. Constructive and unconstructive repetitive thought. Psychological Bulletin. 2008;134:163–206. doi: 10.1037/0033-2909.134.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins ER, Scott J, Wingrove J, Rimes K, Bathurst N, Steiner H, Kennell-Webb S, Moulds M, Malliaris Y. Rumination-focused cognitive behaviour therapy for residual depression: A case series. Behaviour Research and Therapy. 2007;45:2144–2154. doi: 10.1016/j.brat.2006.09.018. [DOI] [PubMed] [Google Scholar]
- Wood JJ, Piacentini JC, Bergman RL, McCracken J, Barrios V. Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: Child and parent versions. Journal of Child Psychology and Psychiatry. 2002;31:335–342. doi: 10.1207/S15374424JCCP3103_05. [DOI] [PubMed] [Google Scholar]
- Zeman J, Shipman K, Penza-Clyve S. Development and initial validation of the Children's Sadness Management Scale. Journal of Nonverbal Behavior. 2001;25:187–205. [Google Scholar]
- Zeman J, Shipman K, Suveg C. Anger and sadness regulation: Predictions to internalizing and externalizing symptoms in children. Journal of Clinical Child and Adolescent Psychology. 2002;31:393–398. doi: 10.1207/S15374424JCCP3103_11. [DOI] [PubMed] [Google Scholar]
- Ziegert DI, Kistner JA. Response styles theory: Downward extension to children. Journal of Clinical Child and Adolescent Psychology. 2002;31:325–334. doi: 10.1207/S15374424JCCP3103_04. [DOI] [PubMed] [Google Scholar]