Abstract
Purpose
This study aims to examine the subjective functional outcomes of patients 70 years or older who sustained distal radius fractures through the use of the Disability of the Arm, Shoulder, and Hand (DASH) and Short Form-8 Health (SF-8) surveys.
Methods
Patients at least 70 years old with a distal radius fracture between 2000 and 2004 were identified and their charts reviewed. They were contacted to answer the DASH and SF-8 surveys. The radiographic injury parameters examined were articular stepoff greater than 2 mm, dorsal tilt on the lateral radiograph, ulnar variance, and presence of an ulnar styloid fracture.
Results
Fifty-eight patients answered the DASH and SF-8 surveys. The mean age at the time of injury in the survey group was 78 years old (range 70–94 years). Mean follow-up period was 33 months (range 13–65 months). Average DASH and SF-8 scores were 22.3 (SD 22.4) and 31.5 (SD 6.9), respectively. DASH scores were inversely correlated with SF-8 scores (R = −0.65, p < 0.01). Patients who sustained an associated ulnar styloid fracture demonstrated worse DASH scores than those without an ulnar styloid fracture (presence of ulnar styloid fracture: mean DASH 26.2, no ulnar styloid fracture: mean DASH 12.9, p = 0.04). There were no significant differences in functional outcome for any other radiographic parameters assessed. Males had statistically better DASH scores than the females (males: mean DASH 6.9, females: mean DASH 24.4, p = 0.003). No difference was found in functional outcome scores among different treatment groups.
Conclusion
In elderly patients with distal radius fractures, the only radiographic parameter we found that affects functional outcome is an associated ulnar styloid fracture. Additionally, females had worse functional outcomes than males.
Keywords: Functional outcomes, Elderly, Distal radius fractures
Introduction
Elderly patients represent a growing population segment. Distal radius fractures are the most common upper extremity fracture in individuals aged 65 years and older with 15% of Caucasian women fracturing their distal radius after age 50 [8].
Elderly patients exhibit lower bone mineral density which may predispose them to fracture following low energy trauma while mandating longer healing times during which displacement may occur [17]. This fracture instability has been shown to result in a 30–50% likelihood of secondary displacement after closed reduction efforts [3, 26, 30, 31]. Cumulative risk factors for a loss of reduction are (1) age over 60, (2) greater than 20° of dorsal angulation, (3) 5 mm of radial shortening, (4) dorsal comminution, (5) ulna fracture, or (6) intraarticular radiocarpal involvement [25].
Prior studies have shown radiographic parameters do not correlate with self-reported disability [1, 2, 15, 20, 21, 32, 43]. However, other studies have shown radiographic parameters predict functional outcome [4, 12, 19, 29, 40].
While previous studies have examined the outcomes of distal radius fractures in elderly patients, it remains unclear what risk factors are for poor outcomes in this group [7, 9, 14, 33]. This is evidenced by the 2010 American Academy of Orthopaedic Surgery Clinical Practice Guideline Summary of Treatment of Distal Radius Fractures where the expert panel was unable to come to a consensus on treatment of distal radius fractures in elderly patients [27]. The frequency of distal radius fractures in elderly patients and the lack of consensus regarding management led us to perform a retrospective review of patients older than 70 years who sustained a distal radius fracture. Our objective was to examine the subjective functional outcomes of patients 70 years or older who sustained distal radius fractures through the use of the Disability of the Arm, Shoulder, and Hand (DASH) and Short Form-8 Health (SF-8) surveys. Our hypotheses were that the following factors would be associated with poor outcome in this elderly group: female gender, increasing age, AO type C fractures, articular stepoff greater than 2 mm, associated ulnar styloid fracture, and other radiographic parameters.
Materials and Methods
Institutional Review Board approval was obtained prior to initiating this study. Inclusion criteria were patients aged 70 years or older for whom initial injury films were available, definitive treatment was known, and who were still alive at the time of survey follow-up. There were 198 patients aged 70 years or older treated for a distal radius fracture at our hospital between January 2000 and December 2004. We identified 107 patients for which initial injury films were available and definitive treatment was known. Of the 107 patients, 20 (20 of 107 = 18.7%) were confirmed to be deceased. This left a possible 87 patients who could potentially perform follow-up questionnaires. Twenty-one of 87 patients (24.1%) could not be reached and were considered lost to follow-up. Of the remaining 66 people, 58 agreed to answer the survey questionnaires (66.7% follow-up rate). The mean age at the time of injury in the survey group was 78 years old (range 70–94 years). Mean follow-up period in the survey group was 33 months (range 13–65 months).
The patients’ demographic data was recorded. We reviewed all initial injury radiographs of patients who fit the inclusion criteria for the study. The senior authors recorded the AO Fracture Classification based on initial injury radiographs into groups A, B, and C [24]. The senior authors used initial injury films to record standard radiographic parameters. The radiographic parameters used were amount of articular stepoff on the anterior–posterior view, ulnar variance on the anterior–posterior view, dorsal tilt on the lateral view, and presence of ulnar styloid fracture on the anterior–posterior view. All radiographs and measurements were reviewed digitally and were agreed upon by both senior authors.
Additionally, treatment was broadly classified into nonoperative, closed reduction and percutaneous pinning (CRPP) with pins and casting, closed reduction and external fixation (Ex Fix), or open reduction and internal fixation (ORIF).
The functional outcome data was obtained via telephone interviews. We attempted to account for and contact all patients who met the inclusion criteria for the study. We called these patients and performed the DASH and SF-8 surveys by telephone. DASH is a previously validated 30 question survey used for patients with upper extremity conditions with lesser scores having better function [16]. The Short Form-8 is an eight-question survey designed to measure overall health status with higher scores having better health.
Treatment Types
Of survey respondents, 22 were treated nonoperatively, two were treated by closed reduction and percutaneous pinning, 18 were treated with external fixation, and 16 were treated by open reduction and internal fixation. Of the 16 patients who underwent ORIF, one patient had a dorsal non-locking plate, two patients had a dorsal locking plate, one patient had a volar non-locking plate, and the remaining 12 patients had a volar locking plate. Distal radio-ulnar joint stability was addressed during surgery and in four cases was deemed unstable. These unstable joints were associated with a Fernandez type 3 ulnar styloid fracture [11]. ORIF and pinning of the distal radioulnar joint was performed in these four patients.
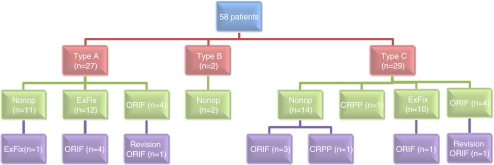
Of the 27 type A fractures, initial treatment was closed reduction in 11 cases, external fixation in 12 cases, and ORIF in four cases. For the 11 type A fractures that were initially treated nonoperatively by closed reduction, one went on to undergo open reduction and internal fixation. Of the 12 type A cases that initially underwent external fixation, four had to be revised. One of the 4 type A cases that underwent ORIF eventually had to be revised (Fig. 1).
Fig. 1.
Group of patients divided into their AO classifications followed by primary treatment and any secondary procedures performed. Type A, B, C: AO Classification. Nonop nonoperative treatment with either sugar tong splint or fiberglass cast; ExFix closed reduction and external fixation, ORIF open reduction and internal fixation, CRPP closed reduction and percutaneous pinning with casting
Both type B fractures were initially treated nonoperatively and did not require any future operative procedure.
Of the 29 type C fractures, initial treatment was nonoperative in 14 cases, closed reduction and percutaneous pinning in one case, external fixation in 10 cases, and open reduction and internal fixation in four cases. Four of the 14 (28.5%) type C cases initially treated nonoperatively went on to undergo open reduction and internal fixation. One of the 10 type C cases that initially underwent external fixation eventually underwent ORIF. One of the four type C cases that initially underwent ORIF eventually underwent a revision procedure.
Complications
Major complications were recorded for the different treatments. Of the 27 nonoperatively treated patients, four went on to collapse and one went on to nonunion. Of the 22 patients initially treated by external fixation, three experienced significant pin site infection requiring hardware removal, two collapsed, and three experienced a nonunion. Of the eight patients initially treated with ORIF, one had a malunion, and another had a nonunion.
Associated Injuries
Other than the concurrent ulnar styloid fractures, other injuries were recorded. Five patients concomitantly suffered ipsilateral hip fractures, two suffered ipsilateral proximal humerus fractures, one an ipsilateral distal humerus fracture, one an ipsilateral olecranon fracture, one an ipsilateral scaphoid fracture, one an ipsilateral radial shaft fracture, one a contralateral humeral shaft fracture and distal femur fracture, two a contralateral patella fracture, and one a facial fracture.
Statistical Analysis
An a priori power analysis was performed to determine the minimum number of patients needed to detect a significant difference in DASH scores between groups. Previous literature has estimated a 10-point difference in the DASH score to be clinically meaningful [13, 18]. Recent studies administering the DASH to patients with distal radius fractures have shown that a standard deviation of DASH scores ranging from 5 to 10 points allowed for an accurate power analysis [6, 34, 37, 42]. Using these parameters in the literature—a mean difference of 10 points, and a standard deviation of 10—we determined with an alpha of 0.05 a minimum of 17 patients per group were required to detect a significant difference with a two-tailed independent samples t test between groups. These groups included male versus female gender, AO type A versus type C fractures, articular stepoff greater than 2 mm versus less than 2 mm, associated ulnar styloid fractures, ulnar neutral or negative versus positive, dorsal angulation less than 20° versus greater than or equal to 20°, operative versus nonoperative treatment, and closed versus open fractures. Statistical analyses were performed using independent samples t tests to determine differences in mean DASH and SF-8 scores between different groups. Pearson’s correlation analyses were used to determine correlations between two continuous variables, including between DASH and SF-8 scores as well as between age and functional outcome scores. The level of significance for all statistical tests was p < 0.05. All tests were two-tailed. We used SPSS version 14.0 to perform statistical analysis.
Results
Functional Outcome Scores
Average DASH and SF-8 scores in the survey group were 22.3 (SD 22.4) and 31.5 (SD 6.9), respectively. Mean follow-up period in the survey group was 33 months (range 13–65 months). DASH and SF-8 scores did have an inverse correlation to each other, with R = −0.65, p < 0.01.
Radiographic Parameters
Articular stepoff on initial injury radiographs was recorded into stepoff less than 2 mm and stepoff of 2 mm or greater. Two millimeters was used as a cutoff based on prior studies that have shown this to be a clinically significant amount [23]. Nine patients had stepoff of 2 mm or more; 49 had less than 2 mm. Using an independent samples t test, we found no significance between the groups based on DASH or SF-8 scores (Tables 1 and 2).
Table 1.
DASH scores
| Mean DASH (SD) | p Value | |
|---|---|---|
| Articular stepoff | ||
| <2 mm (n = 49) | 22.3 (22.4) | 0.99 |
| ≥2 mm (n = 9) | 22.2 (23.6) | |
| Ulnar variance | ||
| Ulnar neutral or negative (n = 28) | 23.6 (22.4) | 0.67 |
| Ulnar positive (n = 30) | 21.1 (22.7) | |
| Dorsal tilt | ||
| <20° (n = 49) | 21.8 (21.6) | 0.72 |
| ≥20° (n = 9) | 24.8 (27.7) | |
| Ulnar styloid fracture | ||
| Ulnar styloid fracture present (n = 41) | 26.2 (23.0) | 0.04a |
| No ulnar styloid fracture (n = 17) | 12.9 (18.2) | |
| AO fracture classification | ||
| Type A (n = 27) | 24.4 (26.2) | 0.68 |
| Type C (n = 29) | 21.8 (18.6) | |
| Gender | ||
| Females (n = 51) | 24.4 (22.8) | 0.003a |
| Males (n = 7) | 6.9 (10.3) | |
| Treatment | ||
| Nonoperative (n = 22) | 20.2 (24.4) | 0.59 |
| Operative (n = 36) | 23.6 (21.3) | |
| Open versus closed injury | ||
| Closed injury (n = 52) | 20.6 (21.8) | 0.09 |
| Open injury (n = 6) | 37.1 (24.0) | |
aSignificance (p value of 0.05 or less)
Table 2.
SF-8 scores
| Mean SF-8 (SD) | P value | |
|---|---|---|
| Articular stepoff | ||
| <2 mm (n = 49) | 32.0 (6.3) | 0.14 |
| ≥2 mm (n = 9) | 28.3 (9.4) | |
| Ulnar variance | ||
| Ulnar neutral or negative (n = 28) | 31.1 (6.9) | 0.75 |
| Ulnar positive (n = 30) | 31.7 (6.9) | |
| Dorsal tilt | ||
| <20° (n = 49) | 31.3 (6.5) | 0.68 |
| ≥20° (n = 9) | 32.3 (8.9) | |
| Ulnar styloid fracture | ||
| Ulnar styloid fracture present (n = 41) | 30.6 (6.7) | 0.15 |
| No ulnar styloid fracture (n = 17) | 33.5 (6.9) | |
| AO fracture classification | ||
| Type A (n = 27) | 31.6 (6.8) | 0.67 |
| Type C (n = 29) | 30.8 (6.9) | |
| Gender | ||
| Females (n = 51) | 31.0 (6.8) | 0.22 |
| Males (n = 7) | 34.4 (7.0) | |
| Treatment | ||
| Nonoperative (n = 22) | 32.2 (7.7) | 0.55 |
| Operative (36) | 31.0 (6.4) | |
| Open versus closed injury | ||
| Closed injury (n = 52) | 31.5 (7.2) | 0.92 |
| Open injury (n = 6) | 31.2 (3.9) | |
aSignificance (p value of 0.05 or less)
Ulnar variance on initial injury radiographs was recorded. Twenty-eight patients were either ulnar neutral or negative, while 30 patients were ulnar positive. Using an independent samples t test, we found no significance between the groups based on DASH or SF-8 scores (Tables 1 and 2).
Dorsal tilt on initial injury radiographs was recorded. Using 20° as a cutoff for amount of initial dorsal angulation based on the criteria of Lafontaine, 49 patients had less than 20° of dorsal angulation while nine patients had 20° or more [25]. Using an independent samples t test, we found no difference between the groups based on DASH or SF-8 scores (Tables 1 and 2).
Forty-one of 58 patients had an ulnar styloid fracture (71%). Using an independent samples t test, we found there to be a significant difference between groups based on DASH, with those patients who had an ulnar styloid fracture doing worse (Table 1). However, there was no difference in SF-8 scores between the groups (Table 2). Given the association of ulnar styloid with poorer DASH scores, and given the likelihood that more fractures with ulnar styloid fractures may have received operative intervention, we performed a secondary analysis to determine if patients with ulnar styloid fractures did better with operative intervention versus nonoperative treatment. Comparing those patients who received operative intervention (n = 23) to those patients who received nonoperative treatment (n = 18), we found no difference in mean DASH scores (mean DASH 26.7 ± SD 22.7 in operative group; mean DASH 25.5 ± SD 24.0 in nonoperative group, p = 0.87). We also found no difference in SF-8 scores between patients treated operatively versus nonoperatively (mean SF-8 31.4 ± SD 7.2 in operative group; mean SF-8 30.0 ± 6.5 in the nonoperative group, p = 0.50).
AO Fracture Classification
Of survey respondents, there were 27 type A fractures (46.6%), two type B fractures (3.4%), and 29 type C fractures (50%). Given that there were only two patients with type B fractures, we excluded them from statistical analysis and compared DASH and SF-8 scores between patients with type A fractures and those with type C fractures. Using an independent samples t-test, we found no difference between type A and C fracture groups in terms of DASH scores or SF-8 scores (Tables 1 and 2).
Gender
Seven males and 51 females answered the questionnaires. We found the DASH scores in the male group to be statistically better than females (Table 1). Females had mean DASH of 24.4 at follow-up whereas males had mean DASH of 6.9. However, there was no significant difference in SF-8 scores between the sexes (Table 2).
Age
A Pearson correlation was performed to determine whether age correlated with either DASH score or SF-8 scores in the group of 58 patients who answered questionnaires. A weak correlation was found between age at time of injury and DASH score, with increasing age being correlated with worsening DASH score (R = 0.27, p < 0.05). No correlation was found between age and SF-8 score (R = −0.138, p = 0.30).
Treatment
We broadly compared nonoperative versus operative treatment in the cohort. Nonoperative treatment consisted of anyone who had a final treatment of nonoperative treatment, whereas operative treatment consisted of all patients with a final treatment of operative treatment, which included Ex Fix, CRPP, and ORIF. We found no difference in DASH or SF-8 scores between patients treated operatively and nonoperatively (Tables 1 and 2). Further ANOVA testing comparing groups of functional outcome scores among nonoperative, external fixation, and ORIF revealed no difference in DASH or SF-8 scores among the groups (DASH p = 0.26; SF-8 p = 0.80).
Open Versus Closed Fracture
There was a 10.3% incidence (6/58) of open fractures in this study population, of which five were treated by irrigation and debridement with external fixation and one was treated by irrigation and debridement and ORIF with a volar plate. We found no difference in functional outcomes between those patients with and without open fractures by either DASH or SF-8 scores (Tables 1 and 2). This is consistent with prior studies which have shown that patients with open distal radius fractures have similar outcomes and DASH scores as those with a closed injury [35].
Discussion
Fracture management of this common injury has received significant attention in the literature yet remains without consensus opinion. Even the concept of the “elderly patient” leads to confusion and is not necessarily defined by physiological criteria such as bone density or functional lifestyle but rather societal customs and legal definitions of retirement age. The geriatric literature, although lacking objective criteria, seems to accept age 65 as a cut-off point [5]. In order to clearly position ourselves into a patient group that would likely exhibit decreased bone mineral density, we chose 70 years of age as our cutoff for this review.
Overall, we found that patients 70 years of age or older with distal radius fractures have functional outcomes with notable deficits when compared to previously published literature of outcomes in younger patients. Our average DASH scores were 22.3 in patients with a mean age of 78 years of age at nearly 3 years of follow-up, which is slightly poorer than previously published literature in younger populations [39, 42]. We also found a weak correlation between age and functional outcome, further supporting that with increasing age patients with distal radius fractures have worse outcome.
Prior studies have examined the correlation of radiographs to functional outcome scores in older patient populations. Jaremko et al. found in a cohort of 74 patients who suffered distal radius fractures with a mean age of 68.5 years that standard radiographic parameters had no effect on DASH or SF-12 scores [20]. Most recently, Synn et al. found no correlation of radiographic fracture pattern to functional outcome in a group of patients older than age 55 years [39]. Our study found similar results although the two studies cannot be compared as Synn et al.’s group of 53 patients had an average age of 69 years and our study group of 58 patients had an average of 78 years, a full 9-year difference in age, which is likely to affect outcome data.
Elderly patients with distal radius fractures remain a controversial group in terms of treatment, and previous literature has demonstrated since the year 2000 an increasing trend to treat distal radius fractures in the elderly with open reduction and internal fixation, despite a lack of a significant body of evidence supporting superior outcomes with internal fixation over closed treatment [7, 10]. Our results demonstrate that there was no difference in functional outcomes between patients treated nonoperatively versus patients treated operatively. This study confirms recent studies that have shown operatively treated distal radius fractures in elderly patients have no better functional outcomes than nonoperatively treated patients [9].
We did not find the fracture severity based on the AO classification to correlate with final functional outcome either. Again, prior studies have shown this to be the case in elderly populations. However, of the 14 type C fractures initially treated with closed reduction and splinting, 28.6% (four of 14) of these were revised because of fracture collapse to either closed reduction and percutaneous pinning or open reduction and internal fixation. Other authors have found that there is a higher rate of secondary displacement of distal radius fractures treated with closed reduction as patients’ age and have recommended considering early operative treatment to prevent this [28]. Our findings support this consideration in the case of type C fractures.
We found that the DASH and SF-8 inversely correlated with each other, which to our knowledge has not been shown before. This suggests that elderly patients who sustain distal radius fractures not only suffer upper extremity dysfunction but also have worse global health related quality of life.
The female patients who had functional outcome scores did worse in terms of the DASH scores than their male counterparts. The results suggest that elderly males have perhaps better healing potential or have differences in the perception of outcome and disability and may be able to compensate better for their injuries than elderly women. That being said, there was no difference in SF-8 scores between males and females, suggesting that there was no difference in overall health related quality of life between males and females.
Among the radiographic parameters we tested, the only factor we found that had any effect on functional outcome in this group of patients was the presence of an ulnar styloid fracture. Patients who sustained an associated ulnar styloid fracture did functionally worse on their DASH scores than patients without an ulnar styloid fracture. There are many recent studies which have shown that ulnar styoid fractures do not have an effect on functional outcome as long as the distal radius fracture is treated with internal fixation [22, 36, 38, 44]. The results of our study suggest that in elderly patients the presence of an ulnar styloid fracture prognosticates poorer functional outcome contrary to the data for younger patients. However, those patients with an associated ulnar styloid fracture who received operative treatment fared no better functionally than those treated nonoperatively.
There were several limitations to this study. It was a retrospective review and lacked complete radiographic or survey follow-up on all patients. Nonetheless, there may have been a selection bias in that patients who did worse were either deceased or otherwise excluded from the study. While our follow-up rate of 66.7% is considered low, given the fact that this was an elderly patient population, many of the patients lost to follow-up may in fact be deceased or incapable of answering questionnaires. Furthermore, multiple surgeons treated these injuries with each one employing his particular treatment algorithm, which introduced treatment bias. While we did find a significant difference in DASH scores in patients with and without an ulnar styloid fracture and between males and females, we did not detect a significant difference in DASH or SF-8 scores in those patients with articular stepoff greater than 2 mm, dorsal tilt greater than 20°, or open versus closed injuries. Our a priori power analysis indicated that these particular subgroups were above our threshold for standard deviation, thus underpowering these specific analyses.
Another limitation to this study is that we used only initial injury radiographs to measure radiographic parameters and did not use post-treatment or final radiographic follow-up films for measurements of radiographic outcome. The goal of surgery was to restore the anatomy to an acceptable level. In all operatively treated cases, the patients’ fractures were restored to at least 10° of neutral alignment and 2 mm of ulnar positive variance. In most cases, the alignment was restored to neutral or even volar alignment. The reason for not adding the ultimate follow-up radiographs to the analysis was that the length of radiographic follow-up varied widely in this study, and some patients had subsequent care at an outside institution as they lived a great distance from our hospital. The true collapse, therefore, is not known.
Based on this study, a few statements can be made with reasonable certainty. The goal of treatment is to restore an upper extremity with both acceptable mobility and durability. An important initial determination should be the patient’s physiologic age and level of functioning. One may surmise that as patients age they tend to place fewer demands on their upper extremities and are, therefore, in lesser need of full restoration of their pre-injury anatomy. Although activities will eventually decrease with advancing age, today’s elderly patients are increasingly remaining more active and minimizing bone loss through medical intervention [14]. The elderly patients’ physiologic and actual age may vary greatly and be perhaps even unrelated to their perceived youth. This potential separation between actual, physiologic, and perceived age needs to be considered when managing distal radius fractures in the elderly. Lending objective findings through the use of the “Physical Activity Scale of the Elderly” may be of value [41]. If they are perhaps lower demand and sedentary, nonoperative management with avoidance of finger stiffness is appropriate. The realization that outcomes are quite good in lower functioning patients makes cost effective nonoperative management worthwhile. If nonoperative treatment is chosen, cast disease, namely atrophy and joint stiffness must be avoided. The acceptance of significant fracture malalignment may not benefit the elderly patient who is more active and places greater functional demands on their upper extremity. One may suggest that in this group radiographic appearance such as articular stepoff and radial shortening do play a significant role in determining the patient’s functional outcome.
For patients that fall between lower and higher functioning groups, a decision based on surgeon philosophy, skill set, and patient expectations can be made. The realization that functional outcomes are, at best, poorly associated with fracture alignment should comfort the surgeon if nonoperative management is chosen. Although multiple studies have aimed to shed light on this subject, the surgeon still faces a dilemma when deciding between operative and nonoperative treatment. Although traditionally immobilized with a cast, this management is being revisited as patients are living longer and more active lives.
Footnotes
Investigation performed at the University of Pittsburgh Medical Center, Pittsburgh, PA, USA.
References
- 1.Anzarut A, Johnson JA, Rowe BH, Lambert RG, Blitz S, Majumdar SR. Radiologic and patient-reported functional outcomes in an elderly cohort with conservatively treated distal radius fractures. J Hand Surg Am. 2004;29:1121–1127. doi: 10.1016/j.jhsa.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 2.Azzopardi T, Ehrendorfer S, Coulton T, Abela M. Unstable extra-articular fractures of the distal radius: a prospective, randomised study of immobilisation in a cast versus supplementary percutaneous pinning. J Bone Joint Surg Br. 2005;87:837–840. doi: 10.1302/0301-620X.87B6.15608. [DOI] [PubMed] [Google Scholar]
- 3.Beumer A, McQueen MM. Fractures of the distal radius in low-demand elderly patients: closed reduction of no value in 53 of 60 wrists. Acta Orthop Scand. 2003;74:98–100. doi: 10.1080/00016470310014283. [DOI] [PubMed] [Google Scholar]
- 4.Board T, Kocialkowski A, Andrew G. Does Kapandji wiring help in older patients? A retrospective comparative review of displaced intra-articular distal radial fractures in patients over 55 years. Injury. 1999;30:663–669. doi: 10.1016/S0020-1383(99)00167-9. [DOI] [PubMed] [Google Scholar]
- 5.Brenner H, Arndt V. Epidemiology in aging research. Exp Gerontol. 2004;39:679–686. doi: 10.1016/j.exger.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 6.Brogren E, Petranek M, Atroshi I. Incidence and characteristics of distal radius fractures in a southern Swedish region. BMC Musculoskelet Disord. 2007;8:48. doi: 10.1186/1471-2474-8-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 2009;91:1868–1873. doi: 10.2106/JBJS.H.01297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cummings SR, Black DM, Rubin SM. Lifetime risks of hip, Colles’, or vertebral fracture and coronary heart disease among white postmenopausal women. Arch Intern Med. 1989;149:2445–2448. doi: 10.1001/archinte.149.11.2445. [DOI] [PubMed] [Google Scholar]
- 9.Egol KA, Walsh M, Romo-Cardoso S, Dorsky S, Paksima N. Distal radial fractures in the elderly: operative compared with nonoperative treatment. J Bone Joint Surg Am. 2010;92:1851–1857. doi: 10.2106/JBJS.I.00968. [DOI] [PubMed] [Google Scholar]
- 10.Fanuele J, Koval KJ, Lurie J, Zhou W, Tosteson A, Ring D. Distal radial fracture treatment: what you get may depend on your age and address. J Bone Joint Surg Am. 2009;91:1313–1319. doi: 10.2106/JBJS.H.00448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fernandez DL. Distal radius fracture: the rationale of a classification. Chir Main. 2001;20:411–425. doi: 10.1016/S1297-3203(01)00067-1. [DOI] [PubMed] [Google Scholar]
- 12.Fujii K, Henmi T, Kanematsu Y, Mishiro T, Sakai T, Terai T. Fractures of the distal end of radius in elderly patients: a comparative study of anatomical and functional results. J Orthop Surg Hong Kong. 2002;10:9–15. doi: 10.1177/230949900201000103. [DOI] [PubMed] [Google Scholar]
- 13.Gummesson C, Atroshi I, Ekdahl C. The Disabilities of the Arm, Shoulder and Hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord. 2003;4:11. doi: 10.1186/1471-2474-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hegeman JH, Oskam J, Palen J, Duis HJ, Vierhout PA. The distal radial fracture in elderly women and the bone mineral density of the lumbar spine and hip. J Hand Surg. 2004;29B:473–476. doi: 10.1016/j.jhsb.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 15.Hegeman JH, Oskam J, Vierhout PA, Duis HJ. External fixation for unstable intra-articular distal radial fractures in women older than 55 years. Acceptable functional end results in the majority of the patients despite significant secondary displacement. Injury. 2005;36:339–344. doi: 10.1016/j.injury.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 16.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (Disabilities of the Arm, Shoulder and Hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29:602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 17.Hung LK, Wu HT, Leung PC, Qin L. Low BMD is a risk factor for low-energy Colles’ fractures in women before and after menopause. Clin Orthop Relat Res. 2005;435:219–225. doi: 10.1097/01.blo.0000155345.04782.14. [DOI] [PubMed] [Google Scholar]
- 18.Hunsaker FG, Cioffi DA, Amadio PC, Wright JG, Caughlin B. The American academy of orthopaedic surgeons outcomes instruments: normative values from the general population. J Bone Joint Surg Am. 2002;84-A:208–215. doi: 10.2106/00004623-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Jakob M, Mielke S, Keller H, Metzger U. Results of therapy after primary conservative management of distal radius fractures in patients over 65 years of age. Handchir Mikrochir Plast Chir. 1999;31:241–247. doi: 10.1055/s-1999-13532. [DOI] [PubMed] [Google Scholar]
- 20.Jaremko JL, Lambert RG, Rowe BH, Johnson JA, Majumdar SR. Do radiographic indices of distal radius fracture reduction predict outcomes in older adults receiving conservative treatment? Clin Radiol. 2007;62:65–72. doi: 10.1016/j.crad.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 21.Kelly AJ, Warwick D, Crichlow TP, Bannister GC. Is manipulation of moderately displaced Colles’ fracture worthwhile? A prospective randomized trial. Injury. 1997;28:283–287. doi: 10.1016/S0020-1383(96)00204-5. [DOI] [PubMed] [Google Scholar]
- 22.Kim JK, Koh YD, Do NH. Should an ulnar styloid fracture be fixed following volar plate fixation of a distal radial fracture? J Bone Joint Surg Am. 2010;92:1–6. doi: 10.2106/JBJS.H.01738. [DOI] [PubMed] [Google Scholar]
- 23.Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986;68:647–659. [PubMed] [Google Scholar]
- 24.Kreder HJ, Hanel DP, McKee M, Jupiter J, McGillivary G, Swiontkowski MF. Consistency of AO fracture classification for the distal radius. J Bone Joint Surg Br. 1996;78:726–731. [PubMed] [Google Scholar]
- 25.Lafontaine M, Delince P, Hardy D, Simons M. Instability of fractures of the lower end of the radius: apropos of a series of 167 cases. Acta Orthop Belg. 1989;55:203–216. [PubMed] [Google Scholar]
- 26.Leone J, Bhandari M, Adili A, McKenzie S, Moro JK, Dunlop RB. Predictors of early and late instability following conservative treatment of extra-articular distal radius fractures. Arch Orthop Trauma Surg. 2004;124:38–41. doi: 10.1007/s00402-003-0597-6. [DOI] [PubMed] [Google Scholar]
- 27.Lichtman DM, Bindra RR, Boyer MI, et al. Treatment of distal radius fractures. J Am Acad Orthop Surg. 2010;18:180–189. doi: 10.5435/00124635-201003000-00007. [DOI] [PubMed] [Google Scholar]
- 28.Makhni EC, Ewald TJ, Kelly S, Day CS. Effect of patient age on the radiographic outcomes of distal radius fractures subject to nonoperative treatment. J Hand Surg Am. 2008;33:1301–1308. doi: 10.1016/j.jhsa.2008.04.031. [DOI] [PubMed] [Google Scholar]
- 29.McQueen M, Caspers J. Colles fracture: does the anatomical result affect the final function? J Bone Joint Surg. 1988;70B:649–651. doi: 10.1302/0301-620X.70B4.3403617. [DOI] [PubMed] [Google Scholar]
- 30.Nesbitt KS, Failla JM, Les C. Assessment of instability factors in adult distal radius fractures. J Hand Surg. 2004;29A:1128–1138. doi: 10.1016/j.jhsa.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 31.Porter M, Stockley I. Fractures of the distal radius. Intermediate and end results in relation to radiologic parameters. Clin Orthop Relat Res. 1987;220:241–252. [PubMed] [Google Scholar]
- 32.Roumen RM, Hesp WL, Bruggink ED. Unstable Colles’ fractures in elderly patients. A randomised trial of external fixation for redisplacement. J Bone Joint Surg. 1991;73B:307–311. doi: 10.1302/0301-620X.73B2.2005162. [DOI] [PubMed] [Google Scholar]
- 33.Roumen RM, Hesp WL, Bruggink ED. Unstable Colles’ fractures in elderly patients. A randomised trial of external fixation for redisplacement. J Bone Joint Surg Br. 1991;73:307–311. doi: 10.1302/0301-620X.73B2.2005162. [DOI] [PubMed] [Google Scholar]
- 34.Ruch DS, Papadonikolakis A. Volar versus dorsal plating in the management of intra-articular distal radius fractures. J Hand Surg Am. 2006;31:9–16. doi: 10.1016/j.jhsa.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 35.Ruchelsman DE MB, Bechtel C, Walsh MG, Paksima N, Egol K. Outcomes following open fractures of the distal radius. In: Orthopaedic Trauma Association Annual Meeting; 2009; San Diego, CA; 2009.
- 36.Sammer DM, Shah HM, Shauver MJ, Chung KC. The effect of ulnar styloid fractures on patient-rated outcomes after volar locking plating of distal radius fractures. J Hand Surg Am. 2009;34:1595–1602. doi: 10.1016/j.jhsa.2009.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schmelzer-Schmied N, Wieloch P, Martini AK, Daecke W. Comparison of external fixation, locking and non-locking palmar plating for unstable distal radius fractures in the elderly. Int Orthop. 2009;33:773–778. doi: 10.1007/s00264-007-0504-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Souer JS, Ring D, Matschke S, Audige L, Marent-Huber M, Jupiter JB. Effect of an unrepaired fracture of the ulnar styloid base on outcome after plate-and-screw fixation of a distal radial fracture. J Bone Joint Surg Am. 2009;91:830–838. doi: 10.2106/JBJS.H.00345. [DOI] [PubMed] [Google Scholar]
- 39.Synn AJ, Makhni EC, Makhni MC, Rozental TD, Day CS. Distal radius fractures in older patients: is anatomic reduction necessary? Clin Orthop Relat Res. 2009;467:1612–1620. doi: 10.1007/s11999-008-0660-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vogt MT, Cauley JA, Tomaino MM, Stone K, Williams JR, Herndon JH. Distal radius fractures in older women: a 10-year follow-up study of descriptive characteristics and risk factors. The study of osteoporotic fractures. J Am Geriatr Soc. 2002;50:97–103. doi: 10.1046/j.1532-5415.2002.50014.x. [DOI] [PubMed] [Google Scholar]
- 41.Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol. 1999;52:643–651. doi: 10.1016/S0895-4356(99)00049-9. [DOI] [PubMed] [Google Scholar]
- 42.Wei DH, Raizman NM, Bottino CJ, Jobin CM, Strauch RJ, Rosenwasser MP. Unstable distal radial fractures treated with external fixation, a radial column plate, or a volar plate. A prospective randomized trial. J Bone Joint Surg Am. 2009;91:1568–1577. doi: 10.2106/JBJS.H.00722. [DOI] [PubMed] [Google Scholar]
- 43.Young BT, Rayan GM. Outcome following nonoperative treatment of displaced distal radius fractures in low-demand patients older than 60 years. J Hand Surg Am. 2000;25:19–28. doi: 10.1053/jhsu.2000.jhsu025a0019. [DOI] [PubMed] [Google Scholar]
- 44.Zenke Y, Sakai A, Oshige T, Moritani S, Nakamura T. The effect of an associated ulnar styloid fracture on the outcome after fixation of a fracture of the distal radius. J Bone Joint Surg Br. 2009;91:102–107. doi: 10.1302/0301-620X.91B1.21026. [DOI] [PubMed] [Google Scholar]