Abstract
This paper describes the use of Group Schema Therapy for Eating Disorders (ST-E-g) in a case series of eight participants with chronic eating disorders and high levels of co-morbidity. Treatment was comprised of 20 sessions which included cognitive, experiential, and interpersonal strategies, with an emphasis on behavioral change. Specific schema-based strategies focused on bodily felt-sense and body-image, as well as emotional regulation skills. Six attended until end of treatment, two dropped-out at mid-treatment. Eating disorder severity, global schema severity, shame, and anxiety levels were reduced between pre- and post-therapy, with a large effect size at follow-up. Clinically significant improvement in eating severity was found in four out of six completers. Group completers showed a mean reduction in schema severity of 43% at post-treatment, and 59% at follow-up. By follow-up, all completers had achieved over 60% improvement in schema severity. Self-report feedback suggests that group factors may catalyze the change process in schema therapy by increasing perceptions of support and encouragement to take risks and try out new behaviors, whilst providing a de-stigmatizing and de-shaming therapeutic experience.
Keywords: eating disorder, chronicity, co-morbidity, schema therapy, group, case series
Introduction
Eating disorders are amongst the most difficult psychopathologies to treat, with only a relatively limited proportion responding to standard cognitive behavioral therapy (CBT). Indeed, less than half of those with bulimia nervosa (BN) are abstinent at follow-up (Fairburn et al., 1995; Fairburn and Harrison, 2003) with a typical drop-out rate of about 25% (Shapiro et al., 2007). Evidence supporting CBT for anorexia nervosa (AN) is weak, with no clear evidence of improvement in the underweight population (Bulik et al., 2007). There appears to be a significant group of sufferers whose symptoms become chronic (e.g., Herzog et al., 1999; Keller et al., 2006). Although the recent transdiagnostic model of eating disorders (Fairburn et al., 2003) has led to some improvement in outcome over the original model, particularly for those with atypical disorders and/or additional psychopathology, approximately 50% of patients remained highly symptomatic at 60-week follow-up (Fairburn et al., 2009). There may be several factors that conspire to make this patient group particularly treatment resistant, most notably the ambivalence regarding change (especially in AN) (Vitousek et al., 1998), ingrained and entrenched thinking patterns (Leung et al., 2000; Mountford and Waller, 2006) and high levels of shame (Burney and Irwin, 2000; Goss and Gilbert, 2002). In addition, eating disorders are often accompanied by pathology which is difficult to treat, including dissociation, perfectionism, compulsive pathology, and rigid personality traits (Waller, 1997; Fairburn et al., 2003; Lawson et al., 2007; Waller et al., 2007).
There is a high level of co-morbidity in the eating disorder population (Blinder, 2006). The presence of rigid personality features can increase the complexity of eating disorder presentations and is associated with poor outcome (Giles et al., 1985; Keel and Mitchell, 1997; Thompson-Brenner et al., 2008). Up to 69% of eating disorder sufferers may meet DSM IV (APA, 1994), diagnostic criteria for an Axis II disorder, and of these, 93% may have concurrent Axis I co-morbidity (especially affective disorders, anxiety disorders and substance misuse) (Braun et al., 1994). Certain personality traits have been linked to different diagnostic groups: patients with BN are most often found to be emotionally unstable, extroverted and histrionic, whereas patients with AN are more likely to be perfectionistic, shy and compliant (Vitousek and Manke, 1994; Cassin and von Ranson, 2005). In particular, poor treatment outcome and chronicity of eating disorder symptoms has been linked to avoidant-insecure personality pathology (Grilo et al., 2007; Thompson-Brenner et al., 2008). The nature of this co-morbidity is complex, with factors such as malnourishment and unreliability of self-report in this population having a confounding effect on the accuracy of measurement of personality (Vitousek and Stumpf, 2005). Eating disorders have also been linked to a range of trauma-related risk factors, including childhood abuse and neglect, which may also be mediated by personality disorder (Brewerton, 2007).
Given the high levels of co-morbidity and prevalence of particular personality traits in this population, it is important to consider the deeper-level belief systems which underlie this pathology. It seems clear that those sufferers with chronic and rigid schema-level beliefs tend not to respond to the standard CBT model and may require treatment which specifically addresses these in a more focused and intensive way (Leung et al., 2000; Waller et al., 2000). The “transdiagnostic model” (Fairburn et al., 2003) begins to address more rigid belief systems, however, this model is also restricted to maintenance factors, with minimal attention paid to early origins of underlying schema-level representations and behaviors. In order to adequately address the features of eating disorders which are not amenable to the here-and-now CBT model, a more sophisticated model is required which specifically addresses the role of early experience in the development of “core” schema-level beliefs, as well as the coping mechanisms which maintain these underlying structures (Waller, 1997; Waller and Kennerley, 2003).
The schema therapy eating disorder group (ST-E-g) was developed to specifically address the schema-level beliefs which underpin chronic and persistent pathology in treatment-resistant eating disorders. Schema therapy was initially developed to deal with personality pathology and resistant clinical problems by Young (1990-1999). It is an integrative approach which draws on CBT, gestalt, psychodynamic and interpersonal therapeutic models, which places significant emphasis on the therapeutic relationship, emotional experience, and early life experiences. Early maladaptive schemas (EMS) which are made up of emotions, bodily responses and the deepest level of cognition are defined as “Extremely stable and enduring themes that develop during childhood and are elaborated upon throughout an individual's lifetime…[and] serve as templates for the processing of later experience” (Young, 1990-1999, p. 9). They develop through unhealthy experiences with parents, peers or significant others, mostly in the form of unmet needs and repeated patterns (e.g., a child who is repeatedly criticized or humiliated may develop the defectiveness/shame schema and learn to think of themselves as inferior or unlovable/unattractive). Schemas function as rigid unconditional beliefs about oneself, others and the world. They are destructive and lead to recurring dysfunction and distress within relationships with others and directly in relation to the self. When triggered they lead to high levels of affective arousal (Young et al., 2003). Schemas are perpetuated through three main schema processes: surrender, avoidance and compensation, all of which function as strategies to prevent the affect associated with schema triggering, but which in fact ultimately reinforce the schemas. For example, someone with a failure schema may avoid applying for a better job due to a fear that they will fail at interview, thus reinforcing their ongoing sense of failure by having to stay in a job with no prospects. They may surrender to self-deprecatory thoughts about themselves as “hopeless” and “incompetent.” They may compensate by trying too hard to be successful in other areas of their life (e.g., body shape/eating), such as through restricting or over-exercising.
These schema processes provide a rationale for the development of both restrictive/compulsive and bulimic/restrictive phenomena in eating disorders alongside other co-morbid behaviors and cognitions (Waller et al., 2007). Although treatment is based on individualized formulations, evidence suggests that maladaptive schemas are more strongly held by anorexics and bulimics than by normal controls (Leung, 1999). There appears to be little difference between the strength of schemas held by anorexics and bulimics, but there may be different patterns of association between schemas and eating attitudes in these two groups. Preliminary data (Mountford et al., 2004; Luck et al., 2005) supports the notion that it is the schema processes that are engaged in an attempt to avoid intolerable emotional states associated with these schemas that in fact determine whether an individual will manifest restrictive or bulimic pathology. Whereas restrictive pathology may be a compulsive behavior developed to prevent schemas being triggered at all (schema compensation), bulimic pathology may function alongside other impulsive behaviors as a method of escaping schema-related affect once schemas have already been triggered (schema avoidance) (Mountford et al., 2004; Luck et al., 2005).
The schema model also incorporates the concept of “modes,” which is particularly useful for patients with high levels of complexity and co-morbidity and who may therefore have several schemas active at any one time. Modes differ from schemas in that they refer to an individual's state rather than a trait, and represent a broader concept than schemas. Modes reflect whatever combination of schemas and coping strategies (thoughts, emotions, bodily sensations, and behavior) are active for an individual at any point in time and are therefore able to account for rapid changes in emotional state and behavior linked to emotional instability (Young et al., 2003; Lobbestael et al., 2007). Ten central modes have been identified (Young et al., 2003), although since then several additional “sub-modes” have been listed, some of which are linked to specific disorders (Lobbestael et al., 2007, 2010).
A randomized controlled trial of schema therapy in the treatment of borderline personality disorder (BPD) over a 3-year period found it to be superior to transference-focused psychotherapy in terms of recovery from BPD, severity of BPD symptoms, quality of life, and a composite index of general psychopathology and personality features (Giesen-Bloo et al., 2006). Moreover, over the 3 years of treatment, ST had significantly fewer drop-outs from treatment than the transference-focused psychotherapy condition (26.7% vs. 52.4%). The reduction of BPD-related costs for society was also larger in the schema therapy condition (Van Asselt et al., 2008). A second Dutch study demonstrated that ST can be successfully implemented in regular health care, and found even larger positive treatment effects than in the original trial (Nadort et al., 2009).
Group schema therapy has also shown promising results with BPD. A recent study (Farrell et al., 2009) found that compared to treatment as usual, group schema therapy had shorter duration, required less therapist time, had fewer drop-outs, and significantly larger treatment effects. The authors suggest that schema therapy may be more powerful when delivered in a group modality because specific group factors seem to facilitate the activation of schema therapy techniques, and have significant remediating effects on core symptoms of BPD psychopathology such as abandonment, emptiness, and stormy relationships. Similar results were found in a recent Dutch study of short-term (18 session) group schema therapy, which led to significant reductions in schema severity and symptomatology (van Vreeswijk et al., unpublished manuscript). Larger-scale randomized controlled trials evaluating group schema therapy for BPD are currently in progress (e.g., Fosse, 2008; Arntz and Farrell, 2010).
Although this preliminary evidence supports the use of the schema model in group treatment of patients with complex and chronic problems, it has not yet been tested on an eating disordered population. This paper describes a pilot study with a schema therapy group specifically adapted for the eating disordered population (by S. Simpson). It is hypothesized that group treatment lends itself to the schema therapy model, by providing in vivo exposure to situations which trigger schemas and modes (especially in terms of interacting and forming close bonds with others). It is proposed that this allows members to work with schema processes as they arise, rather than talking “about” these in a once-removed way such as may be required in individual work, thus giving members the benefit of linking early experiences with here-and-now schema processes in the supportive context of a group. Group members become therapists to each other, thereby increasing opportunities for both evidence-based and vicarious learning, taking risks with new behavior, and experiences of self-efficacy.
Materials and Methods
Participants
This naturalistic study was an evaluation of everyday clinical practice. Informed consent was obtained from all participants, but research-based ethical approval was not required, as the group (and evaluation) reflected usual clinical practice within the service. Participants were recruited from the waiting list of the Eating Disorders Service in Aberdeen, Scotland. The aim was to recruit eight clients for the group. Suitable candidates were selected by scrutinizing case notes and referral letters for evidence of previous unsuccessful treatment, alongside entrenched problems, co-morbidity, and personality-related difficulties. Approximately 40 referral letters from the waiting list were scrutinized and from these, 10 potential candidates were identified as being suitable for the group based on the limited information available at pre-assessment. Those with a low BMI were not excluded unless they were actively losing weight or more suitable for a different treatment on offer in the department. For example, those participants who were pre-contemplative about change were not considered suitable due to the fact that they were not ready to work actively on making changes. Two of the 10 candidates were found not to be eligible for the group due to the clear presence of personality traits (i.e., high levels of narcissism with entitlement) which would have made it difficult for them to work in a group context. Of those who were invited to the group, two participants had attended previous CBT sessions, but this had not led to any significant clinical improvement. All participants were initially seen by a psychiatrist who diagnosed their eating disorder according to DSM-IV criteria. This was followed by a screening interview with two group leaders (doctoral-level clinical psychologists) where their eating disorder was assessed alongside other ongoing Axis I and Axis II difficulties. Eight participants, all of European descent, were included in the study. Of these, four met DSM-IV criteria (APA, 1994) for a bulimic disorder: bulimia nervosa (BN) or eating disorders not otherwise specified (EDNOS) (including binge-eating disorder or “atypical” bulimia nervosa) and four met criteria for atypical AN (also classified under EDNOS). As can be seen in Table 1, participants’ body mass index (BMI) ranged between 17.9 and 37.9, indicating that one was in the underweight category, five were within the normal range, one was overweight and one was in the obese category (WHO, 2006). Depression levels were in the severe category for two, and mild range for five participants as rated on the hospital anxiety and depression scale (HADS, Zigmond and Snaith, 1983). Five participants (2, 3, 4, 5, and 7) were taking anti-depressant medication at the start of treatment. Anxiety levels were rated as severe by two participants, moderate for three participants, and mild for three participants. Sociodemographic data indicated that four of the group had a higher level qualification, and four had completed their standard grade at secondary school. This group was characterized by chronic problems and strong avoidant personality traits, as shown by relatively high ratings of the “detached protector” mode on the Young-Atkinson mode inventory (YAMI) (Young et al., 2005) scale. The “demanding parent” and “compliant surrenderer” modes were also high for almost all participants. This indicated a strong internalized voice which pushed them to reach ever higher standards whilst avoiding mistakes at all costs, and a tendency to cope through serving others and prioritizing their needs and feelings at their own cost.
Table 1.
Sociodemographic data for eight group participants.
| DSM-IV diagnosis | Chronicity of eating disorder (years) | Medication (Y/N) | BMI | Age | Occupation | Educational level | Marital status | Sessions attended | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | BN | 20 | N | 25.2 | 32 | Bookseller | HND (diploma) | Single | 20 |
| 2 | EDNOS (BED) | 8 | Y | 37.9 | 39 | Solicitor | Postgrad. Diploma | Married | 20 |
| 3 | EDNOS | 7 | Y | 23.9 | 35 | Project Manager | Honors degree | De-facto | 20 |
| 4 | AN (B/P) | 15 | Y | 17.9 | 28 | Care Assistant | Bachelor degree | De-facto | 20 |
| 5 | EDNOS | 5+ | Y | 20.2 | 37 | Housekeeping | Standard grade | Single | 20 |
| 6 | EDNOS | 2 | N | 21.8 | 30 | Housekeeping | Standard grade | Married | 20 |
| 7 | EDNOS | 3+ | Y | 19.2 | 30 | Community Living Assistant | Standard grade | Married | 9 discontin. |
| 8 | EDNOS | 5+ | N | 21.3 | 30 | Administrator | Standard grade | De-facto | 8 discontin. |
*BN, bulimia nervosa; AN, anorexia nervosa; AN (B/P), anorexia nervosa, binge-eating and purging sub-type;
EDNOS, eating disorder not otherwise specified; BED, binge-eating disorder.
There were no significant differences between those in the group who had undertaken higher education and those who had not on YSI-L2 (t(4) = 0.76, p = 0.49) or EDEQ change scores (t(4) = −1.66, p = 0.17). Furthermore, two participants (5 and 8) initially rated their HADs depression in the severe category, but there were no significant differences between those patients and the others in terms of outcome (t(4) = −0.45, p = 0.67).
Two patients dropped-out at session 10. Participant 7 felt she was no longer able to commit to attend regular sessions or to watch the DVD between sessions due to other demands on her time (including a child with a chronic illness). Participant 8 terminated her treatment due to difficulty tolerating the distress associated with talking about schemas whilst managing a responsible job and being a single mother. Table 1 gives basic demographic details of the eight participants and the number of sessions attended.
There were no significant differences between the participants who dropped-out (7 and 8) and the others in terms of initial severity of ratings across all six questionnaire measures (YSI-L2: t(6) = −1.16, p = 0.29; depression: t(6) = −1.64, p = 0.15; anxiety: t(6) = −1.45, p = 0.197; shame: t(6) = 1.36, p = 0.22; EQVAS: t(5) = 0.33, p = 0.75; EDE-Q: t(6) = 0.45, p = 0.67).
Outcome measures
Diagnostic status was ascertained initially through interview with a psychiatrist and then verified through use of the eating disorders examination questionnaire (EDE-Q, Fairburn and Beglin, 1994). The EDE-Q is a self-report questionnaire designed to assess eating disorders in accordance with DSM-IV criteria (APA, 1994).
The Young schema inventory (YSI-L2; Young and Brown, 1990) has good psychometric properties for eating disorders (Waller et al., 2001) and was used to measure change in strength of schemas through treatment.
Hospital anxiety and depression scale (Zigmond and Snaith, 1983) is a self-report questionnaire designed to measure anxiety and depression states. On each subscale (depression and anxiety), higher scores indicate a greater number of symptoms and a greater severity of the emotional state.
The EQ5-D (EuroQol Group, 1990) is a standardized instrument which measures health-related quality of life. It consists of two parts: the Health Questionnaire and the euroqol visual analog scale (EQVAS) on which participants rate how “good” or “bad” they perceive their health to be. In this study we have used the EQVAS as a measure of quality of life.
The experience of shame scale (Andrews et al., 2002) is a 25 item questionnaire which assesses four areas of characterological shame: (1) shame of personal habits, (2) manner with others, (3) sort of person you are, (4) personal ability; three areas of behavioral shame (5) shame about doing something wrong, (6) saying something stupid, (7) failure in competitive situations and bodily shame (8) feeling ashamed of (your) body or any part of it. For each of these shame areas there are three items addressing the experiential, behavioral and cognitive components of shame.
Treatment
The treatment was adapted from the schema-focused treatment programme: “Schema Focused Therapy in a Group Setting” (Van Vreeswijk and Broersen, 2006). The original programme consisted of eighteen 90-min sessions with two follow-up sessions. All participants are provided with a patient-version workbook which corresponds with the treatment manual (Broersen and van Vreeswijk, 2006). The first part of the group focuses on schema-focused cognitive behavioral strategies which help participants to identify and start challenging their schemas, whilst working on behavioral change both within and outside the group. This model assists participants to develop an individualized formulation of their own difficulties using a schema therapy framework. The highest three schemas and modes are identified for each patient on the basis of their scores on the YSI-L2 and the YAMI and participants are required to rate the severity of these each week, with a view to working on reducing their severity over the course of the group. Therapists take on the role of “limited reparenting” for the whole group, with a view to sharing this parenting role with group participants as the group progresses. The main aim of this reparenting role is to act as an antidote to participants’ schemas and to provide a stable nurturing role in order to meet their emotional needs within the limits of group therapy. The second part of the group is increasingly focused on behavioral change, using a range of techniques (e.g., cost–benefit analysis, pie charts, evaluating schemas using continua (Padesky, 1994), role plays with healthy adult versus schemas).
This group was adapted for the treatment of chronic eating disorders. Sessions lasted 2 h and were run once a week, except for the final two sessions which took place fortnightly. Each session was recorded and whenever group members missed a session for any reason they were strongly encouraged to come in to watch this. This ensured that they did not miss any educational material, and allayed anxieties that group might talk “about’ them in their absence. Particular emphasis was placed on linking eating behaviors to the schema modes, so that participants were able to learn about the origins and coping functions associated with their own pattern of symptoms. High levels of avoidant coping and intellectualizing was prevalent in the group, and this was addressed frequently by labeling the “Detached Protector” mode when it was identified either by group leaders or by other participants (i.e., both in the context of the group and when talking about eating behavior which took place between sessions). Use of over-compensatory behaviors to avoid emotions was also identified and group members were encouraged to point this out to each other empathically as the group progressed. Due to the lack of emotional awareness and emotional tolerance within the group, participants were encouraged to learn to express empathy and to ask for their emotional needs to be met within the context of the group, rather than detaching from emotional needs through eating behaviors. Mindfulness meditation (Kristeller et al., 2006; Van Vreeswijk et al., 2009), was incorporated to increase awareness of urges to carry out eating disordered behaviors and associated triggers and to facilitate emotional regulation.
Participants were helped to identify the origins of their negative body-image, and to link these to the development of particular modes (e.g. through a Historical Role-play exercise (Young, 1984), whereby group members played out the early experience and then re-played it after restructuring the meaning). Body-image restructuring work involved participants learning to recognize the way in which their perception and visceral sense of their bodies differed from the perspective of their most prominent modes, and developing a compassionate “Healthy Adult” mode which was accepting and nurturing toward the body. Mode dialogues were used to enable group members to repeatedly coach each other to send the “Critical” mode away when it expressed negative assertions about the body (e.g. “You are ugly, fat, and nobody really likes you”). This gave group participants the opportunity to practice being in Healthy Adult mode firstly for others and then for themselves. Flashcards were used to reinforce what was learned in sessions and to help them to challenge modes and resist eating disordered behavior between sessions.
Participants attended sessions at the Eating Disorder Service in Aberdeen, Scotland. Participants repeated questionnaires at session 10 and session 20 and then at 6-month follow-up. Each participant attended a mid- and post-treatment 30-min appointment with the group-therapy leaders in order to discuss progress to date and agree on targets for change in the future. Letters were sent to participants at both time-points to summarize both the results from these meetings and changes in questionnaire scores since pre-treatment. The therapists were doctoral-level trained clinical psychologists, one of whom is an accredited schema therapist. Treatment fidelity was ensured through regular schema therapy supervision by Skype with the original author of the treatment programme (van Vreeswijk), and detailed notes were kept on the content of all clinical sessions. As this was an evaluation of usual service delivery, research ethical permission unnecessary.
Design
A simple one-group pre-/post-test case series design was used in order to evaluate the outcome of a clinical service. This naturalistic design was chosen to facilitate the examination of the process of group schema therapy as a new and innovative form of treatment and to identify whether there was any gross effect of this type of intervention. This was chosen as a precursor to a more sophisticated interrupted time-series design. This methodology facilitates the examination of the specific elements of change at different points in the therapy process, and allows more detailed exploration of this process through a focus on individual participants. The measurement of eating symptoms on the EDE-Q and general distress as rated on the HADs were the main measures of change. Schema severity (YSI-L2) was also considered important, as this is hypothesized to be an important factor underlying resistance to change in eating behavior.
Data analysis
Data were initially analyzed using two strategies: visual analysis of graphically presented self-monitoring data and statistical analysis using repeated measures analysis of variance (ANOVA). To further the understanding of the data, and to avoid the well documented confounds related to small sample sizes for ANOVA, a measure of effect size (Cohen's d) was also employed. Effect size estimates the size of change of the overall group for each questionnaire measure. The Effect Size Generator computer software was used (ClinTools Software, 2008). Due to the single group design of the study, the program calculates the effect size of each measure by considering the correlation coefficient for the sample at time 1 and time 2, the t-test statistic for the sample at time 1 and time 2, and also the number of participants at each trial.
Reliable change and clinical significance was calculated on standardized measures (EDE-Q and HADS). Percentage reduction in YSI-L2 scores were described, as the global reliability coefficient required for calculating reliable change was unavailable. In addition, clinically important changes and observations made by participants are reported.
Results
Visual inspection of the data
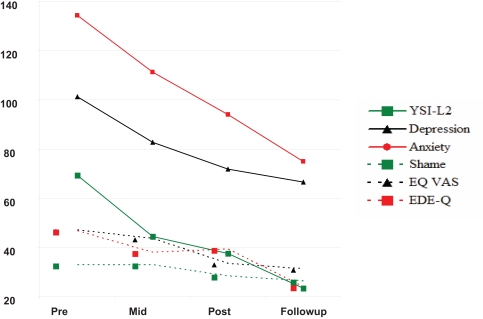
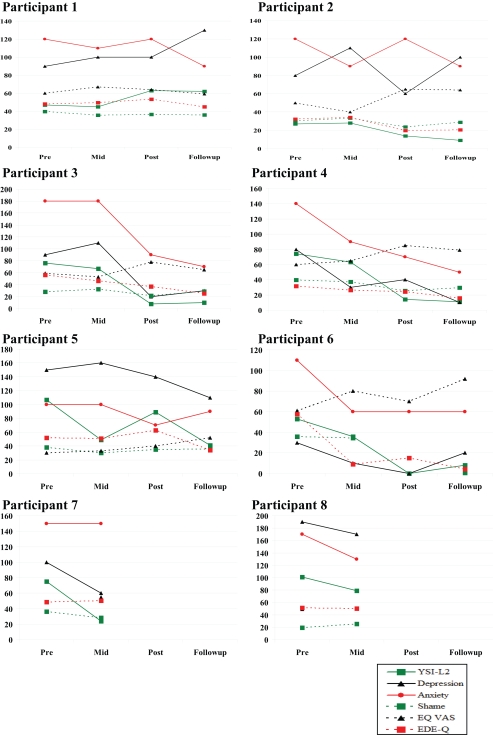
Visual inspection of the group mean scores indicates a trend for scores to consistently improve over the four trial periods across all six questionnaire measures (see Figure 1). To note, the global scores of the depression, anxiety, shame and EDE-Q measures were multiplied by 10 in order to illustrate the patterns effectively. This pattern is also evident through visual inspection of scores for individual participants who completed the group (see Figure 2).
Figure 1.
Group mean scores on YSI-L2, depression (HADS), anxiety (HADS), Shame, EQ-VAS, EDE-Q from pre-treatment through mid, post, and follow-up.
Figure 2.
Global scores on YSI-L2, Depression (HADS), Anxiety (HADS), Shame, EQ VAS, EDE-Q from pre-treatment through mid-, post-, and follow-up.
Statistical tests of outcome data
A number of statistical methods were employed in order to establish whether the seemingly persuasive group pattern of scores across trials were statistically convincing. First of all, an ANOVA was conducted on the six questionnaire measures across the four trial periods (pre, mid, post, and follow-up). On the basis of Mauchly's test of sphericity, the sphericity of the group was assumed, and the results of the test are shown in Table 2. As this study aims to investigate the changes in the maladaptive schemas of the participants, the results of the repeated measures ANOVA for the YSI-L2 indicated a significant time effect: F(3,15) = 4.40; p = 0.02.
Table 2.
Means, standard deviations, F statistics and the p value of the six questionnaire measures as a result of the repeated measures ANOVA.
| Measure | Pre (SD) | Mid (SD) | Post (SD) | Follow-up (SD) | Total (SD) | F (p value) |
|---|---|---|---|---|---|---|
| YSI-L2 | 69.29 (29.0) | 44.57 (16.50) | 37.60 (36.32) | 23.50 (22.71) | 45.04 (30.08) | 4.40 (0.02*) |
| Depression | 10.14 (5.24) | 8.29 (5.22) | 7.2 (4.82) | 6.67 (5.24) | 8.2 (5.02) | 1.82 (1.19) |
| Anxiety | 13.43 (3.05) | 11.14 (4.06) | 9.4 (2.51) | 7.5 (1.76) | 10.56 (3.64) | 5.21 (0.04*) |
| Shame | 3.30 (0.74) | 3.31 (0.31) | 2.85 (0.68) | 2.66 (1.31) | 3.06 (0.82) | 3.26 (0.06) |
| EQ VAS | 52.71 (11.19) | 56.14 (16.19) | 66.40 (17.21) | 68.50 (14.54) | 60.20 (15.38) | 3.91 (0.03*) |
| EQE-Q | 4.69 (1.07) | 3.82 (1.59) | 3.94 (1.84) | 2.42 (1.42) | 3.75 (1.62) | 4.52 (0.02*) |
*Indicates significance to the 0.05 level.
Therefore, on the basis of the repeated measures ANOVA, the findings suggest that the group's scores as a whole significantly improved for four of six of the questionnaire measures (the YSI-L2, the HADS anxiety subscale, the EQ VAS and the EDE-Q). The group scores of the shame scale showed a positive trend, though not statistically significant. The group scores from the depression component of the HADS did not demonstrate a statistically significant change.
The results of the effect size calculations for both “pre to post” and “pre to follow-up” trials are shown in Table 3. There were no outliers at pre-therapy for any of the questionnaires. According to guidelines for grouping the scores into either small, medium, or large effects (Kinnear and Gray, 2008), all the d scores other than depression at the pre to follow-up trials were either medium or large. The majority of the d scores showed large effect sizes.
Table 3.
Effect size (d) scores for all six questionnaire measures, showing both pre to post effects and pre to follow-up effects.
| Treatment period | YSI-L2 (d) | Depression (d) | Anxiety (d) | Shame (d) | EQ -VAS (d) | EDE-Q (d) |
|---|---|---|---|---|---|---|
| Pre to Post | 1.00 | 0.52 | 1.45 | 0.97 | 0.89 | 0.75 |
| Pre to Follow-up | 1.59 | 0.39 | 1.53 | 0.91 | 1.00 | 1.70 |
| Post to Follow-up | 0.08 | 0.16 | 0.05 | 0.005 | 0.14 | 0.02 |
Clinical significance of changes on standardized measures
Reliable change and clinical significance were calculated using criteria suggested by Jacobsen et al. (1984). Clinical significance was calculated only if reliable change was established, using recommendations by Jacobsen and Truax (1991). For the EDE-Q and HADS, norms were available and the distributions of the clinical and non-clinical populations were overlapping. Clinical significance was therefore calculated on the basis that the post-therapy score ended up closer to the mean of the non-clinical than the clinical population.
Changes in EDE-Q, depression and anxiety are shown in Table 4. Calculations showed that there was reliable change on eating symptoms (EDE-Q) from pre- to post-therapy and pre to follow-up for four participants. This was clinically significant for two participants at post-therapy and for four participants by follow-up.
Table 4.
Reliable change (RC) and clinical significance (CS) pre-to-post and pre-to-follow-up for treatment completers.
| ID | Depression (HADS) Pre–post | Anxiety (HADS) Pre–post | EDE-Q Pre–post | Depression (HADS) Pre- to follow-up | Anxiety ( HADS) Pre- to follow-up | EDE-Q Pre-follow-up | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RC | CS | RC | CS | RC | CS | RC | CS | RC | CS | RC | CS | |
| 1 | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | (sig.) | n.s. | n.s. | n.s. | n.s. | n.s. |
| 2 | sig. | sig. | sig. | n.s. | sig. | n.s. | sig. | sig. | sig. | n.s. | sig. | sig. |
| 3 | sig. | sig. | sig. | n.s. | sig. | n.s. | sig. | sig. | sig. | sig. | sig. | sig. |
| 4 | n.s. | n.s. | n.s. | n.s. | sig. | sig. | n.s. | n.s. | n.s. | n.s. | sig. | sig. |
| 5 | n.s. | n.s. | n.s. | n.s. | sig. | n.s. | sig. | n.s. | n.s. | n.s. | sig. | n.s. |
| 6 | n.s. | n.s. | sig. | sig. | sig. | sig. | n.s. | n.s. | sig. | sig. | sig. | sig. |
| 7* | sig. | n.s. | n.s. | n.s. | n.s. | n.s. | ||||||
| 8* | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | ||||||
Use of brackets ( ) denotes that the change demonstrated moved in the opposite direction from what would be clinically desirable (i.e., the individual's score worsened over time). *Mid-therapy scores were used as final outcome data for participants 7 and 8, due to drop-out.
Guideline cut-off scores for the magnitude of effect size: 0.2–0.5 = small; 0.5–0.8 = medium; 0.8 < = large.
Percentage change in schema severity
Changes in YSI-L2 scores between pre- and post-therapy indicated a 43% improvement in the completers between pre and post, which increased to 59% at follow-up. The two participants (7 and 8) who dropped-out showed a 68% and 22% reduction in schema severity respectively by mid-therapy. By follow-up, all completers had achieved over 60% improvement in schema severity, except Participant 1, whose global score had increased. In spite of this, her scores showed a trend of improvement on two out of three of her highest scoring schemas.
Self-report evaluations
It is beyond the scope of this article to present this feedback in detail. However, written self-report data at post-therapy indicated that the most significant changes experienced since taking part in the group were the development of increased understanding about factors that had caused and maintained their difficulties. This enabled participants to develop some self-compassion and to reduce self-critical thinking associated with previous difficulties and behaviors. The group was experienced as de-shaming and de-stigmatizing, especially for those who had kept their eating disorder and other maladaptive coping strategies (e.g., self-harm) hidden from others for several years. Participants indicated that the group had increased awareness about the nature of their relationships with others and their own role in perpetuating negative patterns. The importance of mindfulness practice was highlighted as an important tool for identifying understanding and changing schema-driven patterns of behavior. Many group members also began to conceptualize their own individual identities as distinct from the roles and coping strategies that they had previously used to define themselves. This was linked to reduced anxiety levels and self-blame, as well as increased self-acceptance, especially of bodily imperfections. Several participants commented that they perceived increased support by being in a group setting which gave them the impetus to try new behaviors and take risks.
Discussion
Important clinical improvements were found following schema group therapy in a small pilot sample. A large effect size was found for the group between pre-therapy and follow-up for all measures except depression. These results suggest that participants derived ongoing benefits from the group in terms of improvement in eating disordered symptoms, as well as schema severity, shame, anxiety, and quality of life even after treatment ended. Clinically significant change of eating disorder severity at follow-up was also shown for the majority of completers. The above findings are consistent with self-report evaluations.
The results show a surprisingly large improvement in the strength of maladaptive schemas over the course of the group through to follow-up, given the relatively short-term nature of this treatment for a patient group with characteristically chronic and entrenched difficulties. In contrast, eating disordered symptoms did not change at the same rate for all participants. Visual inspection of the data shows that change in eating disordered symptoms was strongest for participants 2, 3, 4, and 6. For participants 1 and 5 change was slower, despite there being no statistically significant difference between these two and the other participants on other measures that could explain this difference. It is of interest to note that Participant 1 had the highest chronicity of eating disorder symptoms in the group, although evidence to date has not consistently supported this as a prognostic factor for bulimic disorders (Steinhausen and Weber, 2009). Her schema severity increased at post-therapy, although this may be due to an increased awareness of the presence of schemas that she had been unaware of prior to the group. In addition, her depression levels increased at follow-up. Self-report suggest that this may have been linked to her house being broken into, which she experienced as highly traumatic.
The two participants who dropped-out at mid-treatment showed no change in eating behaviors but there was a reduction in schema severity scores. It seems plausible that participants were only able to start changing eating behaviors (alongside other schema-driven behaviors), once they had begun the main task of the group which was on challenging and healing the underlying schemas. Although participants were actively working on changing their coping strategies, it was clear that most had relied on eating behaviors as a familiar “back-up” coping mechanism for many years. Participants indicated that the “Detached Self-Soother” mode (manifested by binging, vomiting, self-harm, over-exercise) was an automatic and reliable way of escaping distressing emotions, particularly shame. They also acknowledged the struggle involved in changing these behaviors, due to the strength of associated compulsive (and/or impulsive) urges. Through consistent practice of mindfulness meditation, several participants began to develop the awareness and self-control necessary to recognize mode “flipping” and to resist the urge to self-soothe with their eating behaviors. Written feedback indicated that a number of participants recognized the importance of continuing to work on changing entrenched eating disordered behaviors after the group was concluded.
These early findings suggest that schema therapy conducted in a group setting may hold promise for eating disordered patients with high levels of chronicity and co-morbidity and it will be important to follow-up these findings in future studies. It is hypothesized that there may be particular factors operating in group schema therapy that challenge schemas at a group-process level. Whereas in individual therapy patients are reliant to a large degree on feedback and challenges that come from their therapist (who is paid to treat them), in group-therapy members challenge and encourage each other, which may in fact be more credible and therefore have more impact in undermining long-held schemas. It was clear from the written feedback following the group that group members felt less isolated and shamed about their experience of having an eating disorder, alongside other difficulties such as self-harm and depression, as a result of working with others with similar problems. The group had a de-stigmatizing effect, but also allowed group members to identify with others’ successes and set-backs, and to encourage each other to move forward and take risks. It seems that the social support derived from the group was enough to overcome any initial anxieties that group members identified, which were mostly associated with feeling overwhelmed by emotions associated with schemas being triggered by group discussion and exercises. The group functioned as a safe arena in which participants could start to experiment with testing negative predictions linked to maladaptive schemas and trying new behaviors. Even attending the group was a major hurdle for those with strong longstanding social isolation schemas and avoidant coping styles. Participant 5 attended the group regularly despite high anxiety levels, and although she was silent for the first four sessions, she managed to start taking an active role and verbalizing her own feelings and needs thereafter. She indicated that the group enabled her to feel sufficiently safe and accepted to take these steps.
It may be worth exploring whether future groups would benefit from increasing the mindfulness-based-schema-therapy component with a view to improving participants’ emotional regulation skills whilst increasing their awareness of “mode-flipping.” It may also be worth exploring whether the incorporation of additional behavioral skills training sessions, targeting longstanding schema-driven eating habits and associated urges would lead to improved outcome on eating disorder measures. Group members indicated that they would have preferred the group to be longer, or to have the option of moving on to an “advanced” schema group. We do not have long-term follow-up results from this group, but given the longstanding and entrenched nature of participants’ presenting problems, it may be that a longer group would allow further opportunity to establish new behavioral patterns and reduce the likelihood of relapse.
In future, any additional benefits provided by group processes could be explored further by comparing group with individual schema therapy and identifying whether outcome varies in terms of rate and extent of change. It would also be of interest to see whether incorporating a “combination” (of both group and individual therapy) treatment condition would improve outcome by drawing on the particular advantages associated with each modality.
The use of a single case design allowed for the examination of both the factors which were critical to outcome for each individual and the interaction of individual circumstances and preferences with response to video therapy. However, this design also limited the generalizability of findings due to the small sample size and lack of a control group. By incorporating both a control group and a pre-therapy assessment period, future studies will be able to examine whether or not these findings reflect true treatment effects.
Conclusion
This case series aimed to evaluate the effectiveness of group schema therapy with a sample of eight participants with an eating disorder. Although there is some initial evidence to support the use of the schema model in groups, it has not yet been tested on an eating disorder population. This pilot study examined a schema therapy group specifically adapted for the eating disordered population. Findings suggested that most participants made clinically important improvements in terms of severity of schemas, eating disorder symptoms, anxiety levels, and quality of life. However, results must be treated with caution, due to the small sample size, and lack of longer-term follow-up. Unfortunately, due to the practical constraints of this time-limited pilot study, it was not feasible to include a comparative face-to-face control group. It is therefore not possible to determine to what degree these findings are due to participants’ response to therapy in general, or to group schema therapy in particular, or indeed to other factors. However, initial results suggest that group schema therapy may benefit eating disordered clients.
This exploratory research trial represents an improvement on previous research in this area. It is methodologically robust as a case series, using standardized measures to assess eating disordered symptoms. These initial findings are likely to prove particularly useful in planning the logistics of setting up a randomized controlled trial, testing the efficacy of group schema therapy for eating disorders.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank Kim Robertson for assisting with the preparation of the final manuscript.
References
- American Psychiatric Association (APA) (1994). Diagnostic and Statistical Manual of Mental Disorders, 4th Edn. Washington, DC: American Psychiatric Association [Google Scholar]
- Andrews B., Qian M., Valentine J. D. (2002). Predicting depressive symptoms with a new measure of shame: The experience of shame scale. Br. J. Clin. Psychol. 41, 29–42 [DOI] [PubMed] [Google Scholar]
- Arntz A., Farrell J. (2010). Advanced Training Course in Group Schema Therapy for international multicenter study on Group Schema Therapy. Maastricht, The Netherlands [Google Scholar]
- Blinder B. J., Cumella E. J., Sanathara V. A. (2006). Psychiatric comorbidities of female inpatients with eating disorders. Psychosom. Med. 68, 454–462 [DOI] [PubMed] [Google Scholar]
- Broersen J., van Vreeswijk M. (2006). Schema Focused Therapy in a Group Setting: Schemagerichte therapie in groepen: Werkboek voor patienten. Houten, The Netherlands: Bohn Stafleu van Loghum [Google Scholar]
- Braun D. L., Sunday S. R., Halmi K. A. (1994). Psychiatric comorbidity in patients with eating disorders. Psychol. Med. 24, 859–867 [DOI] [PubMed] [Google Scholar]
- Brewerton T. D. (2007). Eating disorders, trauma and comorbidity: focus on PTSD. Eat. Disord. 15, 285–304 [DOI] [PubMed] [Google Scholar]
- Bulik C., Berkman N., Brownley K., Sedway J., Lohr K. (2007). Anorexia nervosa treatment: a systematic review of randomized controlled trials. Int. J. Eat. Disord. 40, 310–320 [DOI] [PubMed] [Google Scholar]
- Burney J., Irwin H. J. (2000). Shame and guilt in women with eating-disorder symptomatology. J. Clin. Psychol. 56, 51–61 [DOI] [PubMed] [Google Scholar]
- Cassin S. E., von Ranson K. M. (2005). Personality and eating disorders: a decade in review. Clin. Psychol. Rev. 25, 895–916 [DOI] [PubMed] [Google Scholar]
- ClinTools Software. (2008). ClinTools Downloads: http://clintools.com/download/download.html Accessed February 26, 2010.18342996
- EuroQol Group. (1990). EuroQol – a new facility for the measurement of health-related quality of life. Health Pol. 16, 199–208 10.1016/0168-8510(90)90421-9 [DOI] [PubMed] [Google Scholar]
- Fairburn C. G., Beglin S. J. (1994). Assessment of eating disorders: interview or self-report questionnaire? Int. J. Eat. Disord. 16, 363–370 [PubMed] [Google Scholar]
- Fairburn C. G., Cooper Z., Doll H. A., O'Connor M. E., Kristin Bohn B. A., Hawker D. M., Wales J. A., Palmer R. L. (2009). Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: a two-site trial with 60-week follow-up. Am. J. Psychiatry 166, 311–319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn C. G., Cooper Z., Shafran R. (2003). Cognitive behavior therapy for eating disorders: a “transdiagnostic” theory and treatment. Behav. Res. Ther. 41, 509–528 [DOI] [PubMed] [Google Scholar]
- Fairburn C. G., Harrison P. J. (2003). Eating disorders. Lancet 361, 407–416 10.1016/S0140-6736(03)12378-1 [DOI] [PubMed] [Google Scholar]
- Fairburn C. G., Norman P. A., Welch S. L., O'Connor M. E., Doll H. A., Peveler R. C. (1995). A prospective study of outcome in bulimia nervosa and the long-term effects of three psychological treatments. Arch. Gen. Psychiatry 52, 304–312 [DOI] [PubMed] [Google Scholar]
- Farrell J. M., Shaw I. A., Webber M. A. (2009). Schema-focused approach to group psychotherapy for outpatients with borderline personality disorder: a randomized controlled trial. J. Behav. Ther. Exp. Psychiatry 40, 317–328 [DOI] [PubMed] [Google Scholar]
- Fosse G. (2008). Paper presented at the 3rd Conference of the International Society of Schema Therapy. Coimbra October, 2008 [Google Scholar]
- Giesen-Bloo J., van Dyck R., Spinhoven P., van Tilburg W., Dirksen C., van Asselt T., Kremers I., Nadort M., Arntz A. (2006). Outpatient psychotherapy for borderline personality disorder. Randomized trial of schema-focused therapy versus transference-focused psychotherapy. Arch. Gen. Psychiatry 63, 649–658 [DOI] [PubMed] [Google Scholar]
- Giles T. R., Young R. R., Young D. E. (1985). Case studies and clinical replication series: behavioral treatment of severe bulimia. Behav. Ther. 16, 393–405 [Google Scholar]
- Goss K., Gilbert P. (2002). “Eating disorders, shame and pride: A cognitive-behavioural functional analysis,” in Body Shame: Conceptualisation, research and treatment, eds Gilbert P., Miles J. (Hove and New York: Brunner-Routledge; ), 219–255 [Google Scholar]
- Grilo C. M., Pagano M. E., Skodol A. E., Sanislow C. A., McGlashan T. H., Gunderson J. G., Stout R. L. (2007). Natural course of bulimia nervosa and of eating disorder not otherwise specified: 5-year prospective study of remissions, relapses, and the effects of personality disorder psychopathology. J. Clin. Psychiatry 68, 738–746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herzog D. B., Dorer D. J., Keel P. K., Selwyn S. E., Ekeblad E. R., Flores A., Greenwood D. N., Burwell R. A., Keller M. B. (1999). Recovery and relapse in anorexia and bulimia nervosa: a 7.5-year follow-up study. J. Am. Acad. Child Adolesc. Psychiatry 38, 829–837 [DOI] [PubMed] [Google Scholar]
- Jacobsen N. S., Follette W. C., Revenstorf D. (1984). Psychotherapy outcome research: methods for reporting variability and evaluating clinical significance. Behav. Ther. 15, 336–352 [Google Scholar]
- Jacobsen N. S., Truax P. (1991). Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J. Consult. Clin. Psychol. 59, 12–19 [DOI] [PubMed] [Google Scholar]
- Keel P. K., Mitchell J. E. (1997). Outcome in bulimia nervosa. Am. J. Psychiatry 154, 313–321 [DOI] [PubMed] [Google Scholar]
- Kinnear P. R., Gray C. D. (2008). SPSS 15 Made Simple. Hove and New York: Psychology Press [Google Scholar]
- Kristeller J., Baer R., Quillian-Wolever R. (2006). “Mindfulness-based approaches to eating disorders,” In Mindfulness-Based Treatment Approaches, ed Baer R. A. (San Diego: Elsevier; ), 75–91 10.1016/B978-012088519-0/50005-8 [DOI] [Google Scholar]
- Keller M. B., Herzog D. B., Lavori P. W., Bradburn I. S., Mahoney E. S. (2006). A naturalistic history of bulimia nervosa: extraordinarily high rates of chronicity, relapse, recurrence, and psychosocial morbidity. Int. J. Eat. Disord. 12, 1–9 [Google Scholar]
- Lawson R., Waller G., Lockwood R. (2007). Cognitive content and process in eating-disordered patients with obsessive-compulsive features. Eat. Behav. 8, 305–310 [DOI] [PubMed] [Google Scholar]
- Leung N. M. (1999). Core beliefs in anorexic and bulimic women. J. Nerv. Ment. Dis. 187, 736–741 [DOI] [PubMed] [Google Scholar]
- Leung N., Waller G., Thomas G. (2000). Outcome of group cognitive-behaviour therapy for bulimia nervosa: the role of core beliefs. Behav. Res. Ther. 38, 145–156 [DOI] [PubMed] [Google Scholar]
- Lobbestael J., van Vreeswijk M. F., Arntz A. (2007). Shedding light on schema modes: a clarification of the mode concept and its current research status. Netherlands J. Psychol. 63, 69–78 [Google Scholar]
- Lobbestael J., van Vreeswijk M. F., Spinhoven P., Schouten E., Arntz A. (2010). The reliability and validity of the schema mode inventory (SMI). Cogn. Behav. Psychother. 38, 437–458 [DOI] [PubMed] [Google Scholar]
- Luck A., Waller G., Meyer C., Ussher M., Lacey H. (2005). The role of schema processes in the eating disorders. Cogn. Ther. Res. 29, 717–732 [Google Scholar]
- Mountford V., Waller G. (2006). Using imagery in cognitive-behavioral treatment for eating disorders: tackling the restrictive mode. Int. J. Eat. Disord. 39, 533–543 [DOI] [PubMed] [Google Scholar]
- Mountford V., Waller G., Watson D., Scragg P. (2004). An experimental analysis of the role of schema compensation in anorexia nervosa. Eat. Behav. 5, 223–230 [DOI] [PubMed] [Google Scholar]
- Nadort M., Arntz A., Smit J., Giesen-Bloo J., Eikelenbooma M., Spinhoven P., van Asselt T., Wensing M., vanDyck R. (2009). Implementation of outpatient schema therapy for borderline personality disorder with versus without crisis support by the therapist outside office hours: a randomized trial. Behav. Res. Ther. 47, 961–973 [DOI] [PubMed] [Google Scholar]
- Padesky C. A. (1994). Schema change processes in cognitive therapy. Clin. Psychol. Psychother. 1, 267–278 [Google Scholar]
- Shapiro J. R., Berkman N. D., Brownley K. A., Sedway J. A., Lohr K. N., Bulik M. (2007). Bulimia nervosa treatment: a systematic review of randomized controlled trials. Int. J. Eat. Disord. 40, 321–336 [DOI] [PubMed] [Google Scholar]
- Steinhausen H. C., Weber S. (2009). The outcome of bulimia nervosa: findings from one-quarter century of research. Am. J. Psychiatry 166, 1331–1341 [DOI] [PubMed] [Google Scholar]
- Thompson-Brenner H., Eddy K. T., Franko D. L., Dorer D. J., Vashchenko M., Kass A. E., Herzog D. B. (2008). A personality classification system for eating disorders: a longitudital study. Compr. Psychiatry 49, 551–560 [DOI] [PubMed] [Google Scholar]
- Van Asselt A. D. I., Dirksen C. D., Arntz A., Giesen-Bloo J. H., van Dyck R., Spinhoven P., Van Tilburg W., Kremers I. P., Nadort M., Severens J. L. (2008). Outpatient psychotherapy for borderline personality disorder: cost effectiveness of schema-focused therapy versus transference focused psychotherapy. Br. J. Psychiatry 192, 450–457 [DOI] [PubMed] [Google Scholar]
- Van Vreeswijk M., Broersen J. (2006). Schemagerichte Therapie in Groepen: Handleiding Voor Therapeuten. Houten, The Netherlands: Bohn Stafleu van Loghum [Google Scholar]
- Van Vreeswijk M. F., Broersen J., Schunk G. (2009). Mindfulness en Schematherapie: Praktische Training bij Persoonlijkheidsproblematiek. Houten, The Netherlands: Bohn Stafleu van Loghum; 10.1007/978-90-313-7587-5_2 [DOI] [Google Scholar]
- Vitousek K., Manke F. (1994). Personality variables and disorders in anorexia nervosa and bulimia nervosa [Special Issue: Personality and Psychopathology]. J. Abnorm. Psychol. 103, 137–147 [DOI] [PubMed] [Google Scholar]
- Vitousek K. M., Stumpf R. E. (2005). Difficulties in the assessment of personality traits and disorders in eating-disordered individuals. Eat. Disord. 13, 37–60 [DOI] [PubMed] [Google Scholar]
- Vitousek K. M., Watson S., Wilson G. T. (1998). Enhancing motivation for change in treatment-resistant eating disorders. Clin. Psychol. Rev. 18, 391–420 [DOI] [PubMed] [Google Scholar]
- Waller G. (1997). Drop-out and failure to engage in individual outpatient cognitive behavior therapy for bulimic disorders. Int. J. Eat. Disord. 22, 35–41 [DOI] [PubMed] [Google Scholar]
- Waller G., Kennerley H. (2003). “Cognitive-behavioral treatments,” in Handbook of Eating Disorders, eds Treasure J., Schmidt U., Furth E. (Chichester, England: Wiley; ), 233–252 10.1002/0470013443.ch1414756179 [DOI] [Google Scholar]
- Waller G., Kennerley H., Ohanian V. (2007). “Schema-focused cognitive behaviour therapy with eating disorders,” In Cognitive Schemas and Core Beliefs in Psychiatric Disorders: A Scientist Practitioners’ Guide, eds Riso L. P., du Toit P. T., Young J. E. (American Psychiatric Association; New York: ), 139–175 10.1037/11561-007 [DOI] [Google Scholar]
- Waller G., Meyer C., Ohanian V. (2001). Psychometric properties of the long and short versions of the young schema questionnaire: core beliefs among bulimic and comparison women. Cognit. Ther. Res. 25, 137–147 [Google Scholar]
- Waller G., Ohanian V., Meyer C., Osman S. (2000). Cognitive content among bulimic women: the role of core beliefs. Int. J. Eat. Disord. 28, 235–241 [DOI] [PubMed] [Google Scholar]
- World Health Organisation. (2006). Global Database on Body Mass Index. http://apps.who.int/bmi/index.jsp?introPage=intro_1.html Accessed 20, April 2010.
- Young J. (1984). Cognitive Therapy With Difficult Patients. Workshop presented at the meeting of the Association for Advancement of Behavior Therapy, Philadelphia, PA [Google Scholar]
- Young J., Atkinson T., Arntz A., Weishaar E., Weishaar M. (2005). Young-Atkinson Mode Inventory (YAMI-PM). New York, NY 10036: Schema Therapy Institute, 36 West 44th St, Suite 1007 [Google Scholar]
- Young J., Brown G. (1990). The Young Schema Questionnaire- Long Version (YSI-L2). New York, NY: Cognitive Therapy Center of New York. 130 West 42nd St., Suite 501 [Google Scholar]
- Young J. E. (1990-1999). Cognitive Therapy for Personality Disorders: A Schema-Focused Approach (revised edition). Sarasota, FL: Professional Resource Press [Google Scholar]
- Young J. E., Klosko J., Weishaar M. E. (2003). Schema Therapy: A Practitioners Guide. New York: Guilford [Google Scholar]
- Zigmond A. S., Snaith R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatr. Scand. 67, 361–370 [DOI] [PubMed] [Google Scholar]