Abstract
Research on the conceptualization of adherence to treatment has not addressed a key question: Is adherence best defined as being a uni-dimensional or multi-dimensional behavioral construct? The primary aim of this study was to test which of these conceptual models best described adherence to a weight management program. This ancillary study was conducted as a part of the POUNDS LOST trial that tested the efficacy of four dietary macro-nutrient compositions for promoting weight loss. A sample of 811 overweight/obese adults was recruited across two clinical sites, and each participant was randomly assigned to one of four macronutrient prescriptions: (1) Low fat (20% of energy), average protein (15% of energy); (2) High fat (40%), average protein (15%); (3) Low fat (20%), high protein (25%); (4) High fat (40%), high protein (25%). Throughout the first 6 months of the study, a computer tracking system collected data on eight indicators of adherence. Computer tracking data from the initial 6 months of the intervention were analyzed using exploratory and confirmatory analyses. Two factors (accounting for 66% of the variance) were identified and confirmed: (1) behavioral adherence and (2) dietary adherence. Behavioral adherence did not differ across the four interventions, but prescription of a high fat diet (vs. a low fat diet) was found to be associated with higher levels of dietary adherence. The findings of this study indicated that adherence to a weight management program was best conceptualized as being multi-dimensional, with two dimensions: behavioral and dietary adherence.
Keywords: Adherence, Overweight, Obesity, Randomized controlled trial, Lifestyle behavior modification
Introduction
Adherence to medical procedures is recognized as very important for achieving successful health outcomes (Levensky and O’Donohue 2006). Adherence refers to the “extent to which patients follow the instructions that are given to them for prescribed treatments” (Haynes et al. 2002, p. 2). Research on adherence to medical prescriptions has studied a range of behaviors, from pill-taking to following a prescribed diet (Levensky and O’Donohue 2006). Adherence to prescribed medical procedures (e.g., medication regimens, dietary prescriptions, and metabolic controls for diabetes), is considered to be very important for successful medical management of disease states. Rates of adherence to medical instructions vary widely; typically about 33% for acute conditions and 50–55% for chronic medical conditions (Shearer and Evans 2001). A common clinical observation from earlier papers is that individuals requiring medical attention can be described as either “generally compliant” or “generally non-compliant” (Leventhal 1993), a statement which implies that adherence (often called compliance in the early behavioral literature1) is a uni-dimensional construct. Recently, the theory that people are adherent across a variety of behavioral domains (e.g., obese individuals who adhere to a prescribed diet will also adhere to an exercise prescription) has been questioned (Levensky and O’Donohue 2006; Shearer and Evans 2001). Therefore, one very important question related to behavioral theories of adherence is the extent to which there is strong co-variation among all behavioral indicators of adherence. In other words, should adherence be conceptualized as a uni-dimensional or multi-dimensional construct?
The importance of conceptualizing psychological or behavioral constructs in terms of behavioral co-variation has been a focus of debate for more than 20 years (Evans 1986; Nelson and Hayes 1986). Stemming from this debate, many investigations of health-related behavior have tested whether various health behaviors (ranging from dietary habits to substance abuse) tend to co-vary (Hays et al. 1984; Neumark-Sztainer et al. 1997; Rosenberg et al. 2007). The results of these studies have been mixed, but in general, they have reported that there are multiple classes of behavior which are more or less uncorrelated (e.g., adherence to smoking and exercise prescriptions; Persky et al. 2005), but that behavior does co-vary within classes (Neumark-Sztainer et al. 1997; Rosenberg et al. 2007; Terre et al. 1990). These studies tested for co-variation among a variety of health behaviors (e.g., cigarette smoking, drug use, and exercise patterns), but none of these studies addressed the question of whether behavioral indicators of adherence generally co-vary or whether adherence is best conceptualized as being a multi-dimensional construct.
Adherence is very relevant to behavioral research on weight management since most lifestyle behavior modification programs involve the modification of both dietary and physical activity behaviors (Williamson et al. 2006). Furthermore, adherence related to long-term weight management encompasses an even broader array of behaviors since research findings suggest that it is important for the obese person to attend counseling sessions, to self-monitor food intake and physical activity, and to complete homework assignments (The Look AHEAD Research Group 2006). Thus, successful weight management appears to require adherence across a wide variety of behaviors. Defining adherence poses a significant measurement problem. A variety of methods have been employed across studies and these methods vary from measurement of objective, observable behavior to self-report of the patient; most experts prefer objective behavioral measures to subjective self-report measures (Riekert 2006).
The Prevention of Obesity Using Novel Dietary Strategies (POUNDS) LOST trial (Sacks et al. 2009) provided a unique opportunity to test for co-variation in multi-behavioral indicators of adherence to dietary goals and other behaviors that were hypothesized to be associated with long-term weight management.2 The primary aim of the study was to test the efficacy of four macronutrient diets for weight loss over a 2-year period. The primary results of the study have been recently reported (Sacks et al. 2009). The study found that changes in weight, waist circumference, and other health outcomes did not differ as a function of macronutrient diet assignment with only two exceptions (HDL and LDL cholesterol). Generally, the study found that all four diets resulted in improved health over a 2-year period of intervention. One unique feature of the study was that a computer tracking system was developed to objectively measure behavioral indicators of adherence during the 2-year randomized controlled trial. This feature of the study allowed for a rigorous test of co-variation among eight indicators of adherence in four different diet programs. This ancillary study utilized data collected during the first 6 months of the 2-year POUNDS LOST trial.
The primary aim of this study was to test for the presence of one or more behavioral dimensions that could be used to define adherence in adults who were enrolled in the weight loss study. A secondary aim of the study was to test for differences in adherence associated with the four dietary interventions that prescribed four different patterns of macronutrient intake.
Participants
The POUNDS LOST trial (Sacks et al. 2009) was conducted at two clinical research sites: Boston, MA and Baton Rouge, LA. The study plan (determined by statistical power analysis) called for recruiting 400 participants at each site for a total of 800 volunteers. The inclusion and exclusion criteria for the POUNDS LOST study are summarized in Table 1. The age criteria for this study (i.e., 30–70 years of age) were adopted because we wanted to recruit a sample that was likely to be relatively stable for the duration of the 2 years study. We concluded that people below the age of 30 years were likely to be more mobile due to educational responsibilities and early career changes.
Table 1.
Inclusion and exclusion criteria of the POUNDS LOST trial
| Inclusion criteria |
| Men and women, age 30–70 years |
| Body mass index ≥25 and ≤40 kg/m2 |
| Exclusion criteria |
| Unwilling to participate in the assessment visits or intervention sessions |
| Unwilling to modify diet according to intervention instructions |
| Unable to complete satisfactorily the 5-day diet record at SV2 |
| Unlikely to adhere to the intervention based on a low score in the barriers to effective treatment or psych/eating pathology form |
| Vegan or other unusual diet that would be an obstacle to following any one of the diets |
| Intervention diets contraindicated by a medical condition |
| Anticipated move out of the region during the course of the study |
| Enrolled in another clinical trial related to weight loss or any other purpose or disease |
| History of stomach or gastrointestinal conditions (Inflammatory Bowel disease, Crohn’s disease, malabsorption, colostomy, bowel resection, gastric bypass surgery, etc.) |
| Diabetes mellitus, treated with hypoglycemic oral medicines or insulin which cause weight gain. |
| Current diagnosis of psychosis or bipolar disorder, diagnosis of depression within 6 months of study start (these criteria may be waived at site PI’s judgment) |
| Report of alcohol or substance abuse within 6 months or consumption of >14 alcohol drinks/week |
| History of treatment for eating disorder (this criterion may be waived at the site PI’s judgment) |
| Unstable or recent onset of cardiovascular disease within 6 months or presence of congestive heart failure |
| Diagnosis of cancer within 5 years, except non-melanoma skin cancer (this criterion may be waived at the site PI’s judgment) |
| Illness that might be associated with weight change, such as asthma (because of treatment with corticosteroids), psychosis, inflammatory bowel disease (PI to use clinical judgment, and discuss exceptions with recruitment or steering committee) |
| Use of medications that might cause weight change such as systemic corticosteroids, antipsychotics, anti-depressants, anti-epileptics, weight loss medications (including herbal preparations) (PI to use clinical judgment) |
| Unstable weight with loss or gain of ≥5% in the preceding 3 months |
| Hypothyroidism defined by elevated TSH |
| History of kidney failure, kidney transplant, or dialysis |
| Urinary microalbumin excretion, >100 mg/g creatinine, confirmed by 24-h urine |
| Unstable dose of medication for hyperlipidemia, hypertension, or depression/anxiety or hormone replacement therapy, unless criteria waived by site PI |
| Pregnancy or nursing, or plans to become pregnant during the study |
| History of HIV or active Hepatitis |
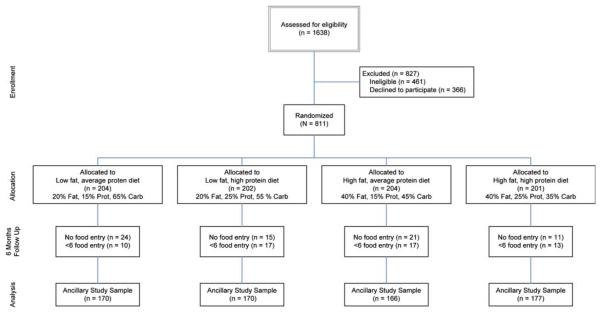
In addition to these criteria, participants were required to record at least six dietary records in the computer tracking system to be included in the analysis for this paper. The recruitment and enrollment of participants into the study are summarized in Fig. 1. The characteristics of the participants at baseline are described in Table 2.
Fig. 1.
CONSORT flow chart that describes the recruitment of participants and development of the study sample for this ancillary study from the parent project called POUNDS LOST. The term “ancillary study sample” refers to the participants (N = 683) who met the criteria for inclusion in the ancillary study, i.e., had entered at least six food entry records
Table 2.
Characteristics of the sample at baseline
| Low fat, average protein |
Low fat, high protein |
High fat, average protein |
High fat, high protein |
Total sample | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | 204 | 202 | 204 | 201 | 811 | |||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||||
| Age | 51 (9) | 50 (10) | 52 (9) | 51 (9) | 51 (9) | |||||
| n | % | n | % | N | % | n | % | n | % | |
| Gender | ||||||||||
| Female | 126 | 62 | 135 | 67 | 125 | 61 | 129 | 64 | 515 | 64 |
| Male | 78 | 38 | 67 | 33 | 79 | 39 | 72 | 36 | 296 | 36 |
| Race | ||||||||||
| White | 159 | 78 | 158 | 78 | 165 | 81 | 161 | 80 | 643 | 79 |
| Black/African American | 33 | 16 | 33 | 16 | 28 | 14 | 33 | 16 | 127 | 16 |
| Asian | 1 | 0 | 1 | 0 | 1 | 0 | 2 | 1 | 5 | 1 |
| Hispanic | 8 | 4 | 7 | 3 | 9 | 4 | 5 | 2 | 29 | 4 |
| Other | 3 | 1 | 3 | 1 | 1 | 0 | NA | NA | 7 | 1 |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||||
| BMI (kg/m2) | 33 (4) | 33 (4) | 32 (4) | 33 (4) | 33 (4) | |||||
| n | % | n | % | N | % | n | % | n | % | |
| BMI categories (kg/m2) | ||||||||||
| 25–29.9 | 51 | 25 | 54 | 27 | 60 | 29 | 58 | 29 | 223 | 27 |
| ≥30 | 153 | 75 | 148 | 73 | 144 | 71 | 143 | 71 | 588 | 73 |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||||
| Education | ||||||||||
| ≤high school | 23 | 11 | 15 | 7 | 19 | 9 | 19 | 9 | 76 | 9 |
| Some college | 47 | 23 | 47 | 23 | 45 | 22 | 41 | 20 | 180 | 22 |
| ≥college grad | 134 | 66 | 140 | 69 | 140 | 69 | 141 | 70 | 555 | 68 |
| Marital status | ||||||||||
| Married | 132 | 65 | 146 | 72 | 144 | 71 | 143 | 71 | 565 | 70 |
| Divorced/separated | 36 | 18 | 24 | 12 | 33 | 16 | 29 | 14 | 122 | 15 |
| Widowed | 8 | 4 | 4 | 2 | 4 | 2 | 2 | 1 | 18 | 2 |
| Never married | 28 | 14 | 28 | 14 | 23 | 11 | 27 | 13 | 106 | 13 |
| Household income | ||||||||||
| <50 K | 56 | 27 | 45 | 22 | 48 | 24 | 46 | 23 | 195 | 24 |
| 50–100 K | 79 | 39 | 82 | 41 | 78 | 38 | 84 | 42 | 323 | 40 |
| 100–150 K | 46 | 23 | 43 | 21 | 43 | 21 | 32 | 16 | 164 | 20 |
| >150 K | 21 | 10 | 30 | 15 | 33 | 16 | 36 | 18 | 120 | 15 |
| Refused | 2 | 1 | 2 | 1 | 2 | 1 | 3 | 1 | 9 | 1 |
The baseline characteristics of this table represent all of the participants who enrolled in the study and do not reflect the “ancillary study sample” that is represented in Fig. 1
Method
Study design
The POUNDS LOST trial was designed to test the efficacy of four macronutrient diets for weight and fat reduction and improvement of health parameters during a 2-year randomized controlled trial. The dietary goals for each of the four dietary interventions: (1) Low fat (20% of energy), average protein (15% of energy); (2) High fat (40%), average protein (15%); (3) Low fat (20%), high protein (25%); (4) High fat (40%), high protein (25%). All four dietary approaches were low in saturated fat and reduced in total energy intake based on the individual’s dietary prescription. A behavioral program of similar programmatic content and intensity across the four dietary interventions was included. The dietary and behavioral components of the program were standardized using written treatment manuals so that the same intervention was administered across the two clinical centers, across intervention staff, and across different cohorts of participants. The duration of the study was 2 years. For the purposes of this study, we only tested data obtained in the first 6 months of this clinical trial. Participants were randomly assigned to the four treatment arms (macro-nutrient diets), stratified by gender. Randomization by computer occurred after the collection of baseline data and was managed by the study statistician. The time-frame for the study was October 2004 to December 2007.
Assessment of adherence using a computer tracking system
A computer tracking system was developed specifically for use in this study. One of the functions of the tracking system was to measure behavioral indicators related to adherence to the four dietary interventions. The computer tracking system was designed to record attendance at group and individual counseling sessions, for self-monitoring of behaviors and providing feedback to participants and researchers. Dietitians and other study staff members entered data into the computer tracking system via a web-based application each time contact was made with a participant (individual or group sessions, or via telephone, email, or mail). The counselor also entered objective data consisting of body weight (measured at an intervention session), attendance, and intervention make-up sessions. Participants also used the computer tracking system to enter their self-reported food intake from diet records. The computer tracking system calculated kcal from fat, protein, carbohydrate, as well as total kcal using nutrient data from the U.S. Department of Agriculture database (1994–1996) that was current during the study period. Therefore, participants did not have to calculate absolute (or percent kcal) calories from fat, protein, or carbohydrate, or total daily caloric intake. Participants also entered data related to number of minutes of physical activity per day and number of days of physical activity per week. The selection of these indicator variables (see Table 3 for a summary) was based upon a need to carefully track a selection of adherence variables that were relevant to the POUNDS LOST study. Therefore, this set of indicator variables is unique to the POUNDS LOST study.
Table 3.
Description and definitions of the eight indicators of adherence
| Behavioral variable | Maximum frequency during 6 months intervals |
Formula for expressing the behavioral variable |
|---|---|---|
| 1. Attendance to individual sessions | 3 individual sessions to be Scheduled | % = # attended/3 sessions |
| 2. Attendance to group sessions | 18 group sessions scheduled (Months 1–6) | % = # attended/18 sessions |
| 3. Number of daily food intake self-monitoring entries |
178 days | % = # entries/178 days |
| 4. Number of daily physical activity self-monitoring entries |
178 days | % = # entries/178 days |
| 5. Mean discrepancy from kcal goal using absolute values |
Variable as a function of number of daily entries |
M = sum of kcal discrepancy scores/# daily entries (from behavioral variable 3) |
| 6. Mean discrepancy from protein goal using absolute values |
Variable as a function of number of daily entries |
M = sum of protein discrepancy scores/# daily entries (from behavioral variable 3) |
| 7. Mean discrepancy from fat goal using absolute values |
Variable as a function of number of daily entries |
M = sum of fat discrepancy scores/# daily entries (from behavioral variable 3) |
| 8. Mean discrepancy from carbohydrate goal using absolute values |
Variable as a function of number of daily entries |
M = sum of carbohydrate discrepancy scores/# daily entries (from behavioral variable 3) |
While participants were able to enter data from any computer, each clinic had dedicated computers for those participants who did not have access to the Internet. Most participants (>99%) had access to the Internet at home and/or work, and the few who did not have this access were provided regular opportunities to use computers at the two clinical sites.
The formula used to calculate percent deviation from macronutrient and calorie goals was: [(Actual value − Prescribed value)/Prescribed value] × 100. Deviation scores for fat, carbohydrate, and protein were calculated using percent of calories. This procedure was designed to evaluate adherence to each diet intervention for each participant based upon his or her unique caloric and macro-nutrient goals. It should be noted, that since adherence to dietary goals was based upon absolute deviations from prescribed values (not percentages) the macronutrient and caloric deviation scores were mathematically independent.
Feedback related to meeting the daily kcal and macro-nutrient goals for each individual was provided at the end of each day of self-monitoring via the computer tracking system. As noted above, participants entered their food intake each day, and they were required to confirm that the information provided was their total food intake for that day. When this confirmation was made, the data entry for that day was “locked,” and the computer tracking system calculated deviations from the kcal and macronutrient goals for that individual using a “thermometer” that indicated the extent to which the participant’s intake exceeded or failed to meet the goals for total kcal, fat, protein, and carbohydrate. We elected to analyze the adherence data from only the first 6 months for two reasons: (1) the feedback provisions of the computer tracking system were changed mid-way through the study (after all participants had at least 6 months in the study) to allow immediate feedback after each food intake entry (versus each complete food record) at one of the two sites, and (2) utilization of the computer tracking system diminished steadily over the course of the 24 months study, such that information from the computer tracking system during Months 7–24, is likely from a non-representative sample.
Dietary treatment interventions
General implementation strategy
Prior to dietary intervention, estimated energy needs were calculated using indirect calorimetry to determine resting energy expenditure. Estimated total energy was calculated by multiplying resting energy expenditure by an activity factor (Baecke et al. 1982). For the weight loss phase of the study, the participant’s diet prescription represented an approximate 750 kcal/day deficit from his/her estimated energy intake. The 750 calorie deficit was then rounded to the nearest 200 to give 1,200, 1,400, 1,600, 1,800, 2,000, 2,200, 2,400, 2,600, 2,800, 3,000, and 3,200 calorie diet prescriptions. This 750 kcal/day deficit was intended to promote a weight loss rate of approximately 1.5 pounds per week (0.7 kg/week). Sacks et al. (2009) reported data that suggest that during the first 6 months of the study, average caloric reduction was approximately 225 kcal/day, and that the treatment arms did not differ in terms of average caloric restriction. It is noteworthy, however, that the participants did not meet the caloric restriction goals and that this “non-adherence” was equivalent across the four macronutrient diets.
When a cohort of approximately 48–80 participants was recruited, the four interventions were initiated with 12–20 participants per group by randomly assigning participants to one of the four diet interventions. During the intense weight loss phase (Weeks 1–26), participants were offered group sessions 3 out of 4 weeks, whereas during the weight maintenance phase (Weeks 27–104), participants were offered group sessions 2 out of 4 weeks. During the entire 2-year program, participants scheduled individual one-on-one visits with a dietitian every 8 weeks. The one-on-one counseling session, lasting 30 min, was used to review adherence to the assigned diet prescription, solve problems that were identified as barriers to success, and develop strategies to maximize adherence. The group sessions, lasting 1 h, provided nutrition education, included behavioral methods to reinforce dietary and behavioral goals, and also provided social support. During the intense weight loss phase, the focus of the group sessions was on nutrition education with some counseling to ensure comprehension of and adherence to the assigned macronutrient diet. Beginning in Week 13, the sessions were structured to support continued adherence to the assigned diet. The goal for structured exercise was 30 min per day on 3 days per week. Counselors had access to the computer tracking system records of dietary intake of the participants, and they reviewed these records in the context of the individual’s goals for total kcal/day and intake of fat, protein, and carbohydrate. The counselors also addressed adherence to other treatment goals, such as self-monitoring and group attendance, during individual sessions. Therefore, the intervention was designed to enhance adherence to the dietary prescriptions and other behavioral changes related to treatment goals. Throughout the 2-year program, the intervention team members set positive dietary goals, praised participants for success, and used behavioral strategies (e.g., goal setting, problem solving) to enhance adherence and improve retention.
Weight loss phase (Weeks 0–26)
Following randomization to one of the four diets, each participant met one-on-one with a registered dietitian, who instructed the participant on following his/her specific macronutrient diet prescription. To aid participants in achieving the goals of their assigned dietary regimen, 14 days of menus were developed for each of the four diet treatment arms and at various calorie levels, as described previously.
While the structured menus were well accepted, there was a need for alternate strategies for adherence to the diets. The exchange system for weight management was the subject of one of the group sessions and participants were provided with the American Dietetic Association/American Diabetes Association booklets on this topic. The structured menus were also revised to show the appropriate exchange for each food, further enabling their use but allowing substitutions, and therefore another educational piece. Tip sheets were developed to assist the participants in following the diet prescription. These included general shopping and food preparation strategies that either lowered or increased fat and protein intakes to better achieve the targeted nutrient variables.
At the first group counseling session, the participants received a shopping list, which was designed for their assigned diet to support efforts in purchasing appropriate foods. Each participant was counseled to use the computer tracking system to monitor food and drink consumed each day, as well as minutes of physical activity. Body weight was measured at each intervention visit.
Description of behavioral methods
A number of behavioral methods were incorporated into the group and individual sessions over the course of the study. The primary components of the behavior modification program included: stimulus control procedures, self-monitoring, goal setting, behavioral contracting, problem solving, social support, procedures aimed at preventing emotional eating and binge eating, assertiveness training, and relapse prevention. Participants received training in all of these skills to facilitate their ability to follow their prescribed dietary plan. The components of the behavioral program were held constant across the four treatment arms and were designed to promote the intervention by enhancing adherence to the dietary plans.
Enhancement of adherence and retention
Incentives were used to promote adherence and retention. Incentives (e.g., gift cards, stress balls, measuring cups and spoons), were provided for attending individual and group sessions, for adhering to their prescribed dietary and behavioral programs when participants demonstrated consistently good adherence, and made significant improvements in following their assigned diet. For those participants who experienced difficulty adhering to their dietary program, additional motivational strategies were employed. For example, when a participant was identified as having sub-optimal adherence, he or she was scheduled for an extra meeting with their counselor to discuss potential barriers to adherence. During this meeting, the counselor worked with the participant to develop strategies to remove or minimize specific barriers to adherence.
Procedures
The computer tracking system recorded data related to adherence for each participant over the course of the study. For the purposes of this study, eight behavioral indicators of adherence to the prescribed interventions were measured. These eight variables are described in Table 3. Attendance to individual and group counseling sessions was defined as observation of the participant at a regularly scheduled session by the counselor, who then entered this observation in the computer tracking system. Attendance to extra meetings3 was not counted toward attendance. Submission of self-monitoring records for food intake and physical activity was defined as daily recording of these behaviors and confirmation that a full day of recording had occurred. Total daily caloric intake and consumption of fat, protein, and carbohydrate were calculated by the computer tracking system using information from the 1994–1996 U.S. Department of Agriculture nutrient database. Each of these variables was summarized over the first 6 months of this 2-year study in terms of an average (e.g., mean discrepancy from a dietary prescription) or a percentage (e.g., percent of groups attended).
Statistical methods
Figure 1 shows that, of the 811 participants enrolled in the study, 740 participants had at least one food intake entry across the first 6 months, and 683 participants had six or more food intake entries across the initial 6 months. This study used data from the 683 participants with at least six food intake entries. This criterion (at least 6 days of food entry out of a possible 178 days) was necessary because the assessment of dietary adherence required at least a few days of recording, at a minimum. The selection of a minimum of 6 days was derived by a consensus of the investigators. This consensus was based upon defining a sample with a wide range of adherence scores for all eight indicator variables. As shown in Fig. 1, there were similar numbers of participants in each of the four treatment arms (range = 166–177 participants per arm) that met this criterion.
As a first data analytic step, we computed factor analyses using the eight indicators of adherence for each of the four treatment arms (diets) to determine if the factor structure was similar across treatment arms. We found that the factor structure was very similar, with two factors emerging for each treatment with identical indicators for each diet type. Therefore, we concluded that the factor structure was stable across treatment arms, which provided justification for the adherence data to be analyzed as one large sample, as opposed to by treatment arm. As a second step, we randomly selected half the participants (stratified by treatment arm) to compute an exploratory factor analysis of the eight indicators of adherence (described in Table 3). Following principal components analysis, an orthogonal (varimax) rotation was performed to create independent factors. The number of factors to be considered for interpretation was evaluated using the eigenvalue >1.0 rule. The third data analytic step used the remaining half of the sample to conduct a confirmatory factor analysis of the behavioral indicators during the first 6 months to test for stability of the factor structure identified in Step 2. Confirmation of the factor structure identified by exploratory factor analysis was interpreted using five common fit indices: Goodness-of-Fit Index, Adjusted Goodness-of-Fit-Index, Root Mean Square Error of Approximation, Comparative Fit Index, and Non-normed Fit Index. In Step 4, we calculated factor scores for each dietary intervention and tested for differential adherence as a function of treatment arm. All statistical analyses were performed using SAS 9.1.
Results
Description of the indicators of adherence
Before performing exploratory and confirmatory factor analyses, we tested for differences across treatment arms, using ANOVAs, among the eight indicators of adherence (Table 4). Effect sizes were reported as the eta squared statistic (, Cohen 1977). These tests were conducted to test for treatment arm differences if the eight indicator variables were conceptualized as eight independent measures of adherence. The strategy of treating each indicator as an independent measure of adherence has been a common practice in previous research (e.g., Sacks et al. 2009; Alhassan et al. 2008). Also, this analysis provided a general description of adherence. Attendance to individual counseling sessions (64.3%) was slightly higher than attendance to group sessions (53.8%). Also, electronic submission of food records was more frequent (57.8%) than submission of exercise records (28.8%). Deviations from caloric and macronutrient goals indicated that participants were reporting nutrient intakes that approximated the study goals.
Table 4.
Means (SDs) of behavioral indicators of adherence derived from the computer tracking system
| Behavioral variable | Overall | Low fat, avg protein |
Low fat, high protein |
High fat, avg protein |
High fat, high protein |
Sig. effect |
|---|---|---|---|---|---|---|
| % Individual sessions attended | 64.3(30.8) [0–100] |
61.6(31.2) [0–100] |
60.4(30.6) [0–100] |
65.5(30.0) [0–100] |
69.5(30.7) [0–100] |
Fata |
| % Group sessions attended | 53.8(20.7) [0–91] |
55.2(21.8) [5–91] |
53.1(20.6) [0–86] |
51.6(20.4) [0–81] |
55.3(20.0) [0–86] |
None |
| % of days with completed food entriesc | 57.8(32.9) [4–100] |
56.7(34.2) [4–100] |
57.2(32.1) [4. 100] |
57.0(33.5) [4–100] |
60.1(31.9) [4–100] |
None |
| % of days with PA entriesc | 28.8(23.0) [0–100] |
27.9(23.1) [0–100] |
30.5(24.6) [0–100] |
27.0(22.0) [0–99] |
29.8(22.4) [0–100] |
None |
| Mean % discrepancy (kcal goal)d | −10.9(12.0) [−73 to 32] |
−13.3(13.1) [−62 to 21] |
−11.6(11.9) [−65 to 13] |
−9.4(11.3) [−59 to 32] |
−9.5(11.4) [−73 to 16] |
Fata |
| Mean % discrepancy (protein goal)d | −8.9(15.5) [−72 to 41] |
−3.1(14.9) [−53 to 41] |
−16.7(14.2) [−69 to 12] |
−0.7(13.3) [−52 to 40] |
−14.5(13.2) [−72 to 10] |
Proteinb |
| Mean % discrepancy (fat goal)d | −5.6(21.7) [−81 to 119] |
0.4 (26.3) [−69 to 119] |
4.8(22.0) [−72 to 67] |
−13.6(15.1) [−74 to 42] |
−13.8(14.8) [−81 to 25] |
Fatb |
| Mean % discrepancy (carbohydrate goal)d | −11.2(15.2) [−70 to 31] |
−19.9(14.5) [−70 to 5] |
−14.9(13.8) [−59 to 17] |
−8.8(12.5) [−49 to 24] |
−1.4(13.2) [−63 to 31] |
Fatb, Proteinb |
Statistical values are means and standard deviations (shown in parentheses) and ranges [shown in Brackets]
p < 0.01 level
p < 0.0001 level
Total possible days = 178
Dietary discrepancy scores were defined by the following formula: [(Actual value − Prescribed value)/Prescribed value] × 100
To test for treatment arm differences, each of the indicator variables was subjected to a two-way ANOVA having two levels of fat (high, low) and two levels of protein (average, high). No significant main effect attributable to the fat or protein prescriptions were detected for attendance at group sessions, electronic submissions of food records, or electronic submissions of exercise records. For attendance at individual sessions, a main effect associated with the fat prescription was observed, F (1, 679) = 7.7, p < 0.01, . Participants assigned to the two treatment arms that prescribed high fat consumption attended individual sessions more frequently than those participants assigned to the two low fat diets. No interaction effects were observed for these indicator variables.
The next set of analyses tested for treatment arm differences among the four measures of adherence to the four assigned diets (see Table 4). Main effects for fat and/or protein were observed for all four dietary indicators of adherence. For caloric intake, a main effect associated with the fat prescription was observed, F (1, 679) = 10.8, p < 0.01, . Participants assigned to treatment arms that prescribed high fat consumption reported slightly exceeding caloric intake goals in comparison to participants assigned to the low fat diets. Participants assigned to the high protein diets reported eating less protein than prescribed, while participants assigned to consume average amounts of protein consumed the prescribed amounts, F (1, 679) = 167.2, p < 0.0001, . Assignment to the low fat diets was associated with consuming more fat than prescribed, and assignment to the high fat diets was associated with consuming less fat than prescribed (F (1, 679) = 111.5, p < 0.0001, ). Treatment effects associated with diets varying in fat and protein were detected for adherence to carbohydrate target goals. Participants assigned to the high fat diets were more adherent to carbohydrate goals in comparison to participants assigned to low fat diets, F (1, 679) = 142.0, p < 0.0001, . Participants assigned to the high protein diets were more adherent to carbohydrate goals in comparison to participants assigned to the average protein diets, F (1, 679) = 35.6, p < 0.0001, . No significant interactions between fat and protein prescriptions were observed for any of the four indicators of dietary adherence. It is noteworthy that when each indicator variable was analyzed in isolation of the other indicators, the findings suggested widely different conclusions concerning which macronutrient diet was associated with the “best adherence.”
Factor analytic results
Results of exploratory factor analysis
Strictly speaking, deviation from the target dietary goal was an indication of poor adherence. Based upon this premise, absolute values4 were calculated for the dietary adherence variables before conducting factor analyses. Two factors were identified and this factor structure is summarized in Table 5. The total variance accounted for by these two factors was 66%. Factor loadings for each of the eight indicators of adherence indicated that two factors described the dataset (each factor had four indicator variables). The first factor was defined by caloric or macro-nutrient intake relative to goals. This factor was labeled “dietary adherence” because it was derived from self-reported intake and converted into deviations from caloric or macronutrient goals. The second factor was defined by objective behavioral variables. These variables were entered into the computer tracking system by the counselors (frequency of attendance to individual and group counseling sessions) or were entered by the participants (frequency of entry of food or exercise records). This factor was labeled “behavioral adherence” because it was derived from objectively defined behavioral indicators of adherence.5 Internal consistency of both factors was evaluated using alpha = 0.70 as a cut-off (Nunnally and Bernstein 1994). Cronbach’s alpha was satisfactory for both factors (0.86 for dietary adherence and 0.77 for behavioral adherence).
Table 5.
Factor structure and item loadings from the exploratory factor analysis
| Item | Factor 1 | Factor 2 |
|---|---|---|
| Factor 1: dietary adherence | ||
| Mean discrepancy from kcal goal | 0.91* | −0.19 |
| Mean discrepancy from protein goal | 0.83* | −0.14 |
| Mean discrepancy from fat goal | 0.67* | −0.19 |
| Mean discrepancy from carbohydrate goal | 0.85* | −0.16 |
| Factor 2: behavioral adherence | ||
| Attendance to individual sessions | −0.02 | 0.57* |
| Attendance to group sessions | −0.18 | 0.82* |
| No. of daily food intake entries | −0.32 | 0.82* |
| No. of daily physical activity entries | −0.23 | 0.78* |
| Mean | 55.1 | 204.7 |
| Standard deviation | 42.0 | 81.2 |
| Cronbach’s alpha | 0.86 | 0.77 |
Signifies a factor loading greater than 0.50 and based only on items with factor loadings >0.50
Confirmatory factor analysis
A test of the stability of the two-factor structure identified by exploratory factor analysis was confirmed in a randomly selected sample of 50% of the participants using the maximum likelihood method. The fit of the two-factor structure was determined to be acceptable (Goodness-of-Fit Index = 0.97, Adjusted Goodness-of-Fit-Index = 0.94, Root Mean Square Error of Approximation = 0.06, Comparative Fit Index = 0.98, Non-normed Fit Index = 0.97). It is noteworthy that these same two factors emerged (with identical indicators for each factor) when the factor analyses were performed by treatment arm (i.e., four diet types).
Test of adherence to the four dietary interventions
In order to derive total scores for each of the two factors, equivalent factor loadings (1.0) were assigned to each of the indicator variables associated with the two factors. The total scores (using absolute values) of the behavioral adherence and the dietary adherence factors were calculated and subjected to a two-way analysis of variance to test for differences as a function of the treatment arms, i.e., diets varying in amounts of fat and protein. For the behavioral adherence factor, main effects associated with different levels of fat, F (1, 679) = 1.1, p = 0.29, , and protein, F (1, 679) = 1.2, p = 0.28, , were not statistically significant. The interaction of diet types was also nonsignificant, F (1, 679) = 1.3, p = 0.26, , for the behavioral adherence factor.
For the dietary adherence factor, a main effect associated with the different levels of fat prescriptions was detected, F (1, 679) = 19.5, p < 0.0001, , indicating that the mean dietary adherence total score was significantly greater among participants assigned to a low fat diet (M = 62.1 ± 2.2) in comparison to participants assigned to a high fat diet (M = 48.1 ± 2.2). Since a lower dietary adherence score indicated smaller discrepancy from dietary goals, this pattern of data indicated that participants prescribed the high fat diets reported overall dietary adherence that was significantly better than that of participants prescribed the low fat diets. The main effect associated with different levels of protein was not statistically significant, F (1, 679) = 0.04, p = 0.84, , nor was the interaction of fat and protein, F (1, 679) = 0.4, p = 0.54, .
Discussion
The results of this study were consistent with the conceptualization of adherence to a dietary weight management program as a multi-dimensional construct. Specifically, two dimensions of adherence were identified: behavioral adherence and dietary adherence. Thus, adherence of individuals in the POUNDS LOST trial varied along two dimensions. One dimension was defined by objective behaviors: attendance to individual and group counseling sessions and electronic entry of food records or exercise records. The strong co-variation of these behaviors suggests that during the first 6 months of the intervention, if a participant was likely to attend individual sessions, he or she was also likely to attend group sessions and to submit self-monitoring records related to food intake and exercise. The second dimension was defined by self-monitoring data related to deviation from caloric and macronutrient goals. The co-variation among these intake data indicate that if a participant tended to report good adherence to the caloric goal, he or she was also likely to report good adherence to all three macronutrient goals. This finding is significant for several reasons: (1) the strong behavioral co-variation indicates that adherence to macronutrient diets tends to vary regardless of the specific composition of the diet, (2) participants apparently did not sacrifice the caloric goal to meet macronutrient goals, or vice versa, and (3) dietary adherence to macronutrient goals is a single construct that is not uniquely related to either caloric goals or specific macronutrient goals. The finding that there were two factors that accounted for a majority (66%) of the variance in adherence measures is also significant. The identification of two independent factors suggests that participants can, in principle, adhere to behavioral components of the study (e.g., high rates of attendance and self-monitoring), but not follow the guidelines for caloric or macronutrient goals. Or, conversely, an individual might adhere to dietary goals, but not follow behavioral guidelines (e.g., attend sessions or submit self-monitoring records). Of course, it is also possible that the person might have satisfactory behavioral and dietary adherence or have sub-optimal performance related to both types of adherence.
These findings are consistent with behavioral theories that recognize co-variation among behaviors as a means for objectively defining psychological or behavioral constructs (Evans 1986; Nelson and Hayes 1986). The results suggest that adherence in this weight management study was best conceptualized as being multi-dimensional. These findings were quite robust and applicable to all four diets to which participants were randomly assigned. We suspect that if other behavioral requirements were added to a treatment intervention (e.g., taking medications or following exercise prescriptions), it is likely that additional dimensions of adherence would be required to more completely define the adherence construct. An issue of considerable importance, however, is whether future studies investigating this topic also identify multiple dimensions of adherence.
Results related to adherence to assigned caloric and macronutrient goals are summarized in Table 4. It is noteworthy, that participants reported, on average, relatively small deviations from the caloric and macronutrient goals across the four dietary interventions. In general, the data summarized in Table 4 show that adherence deviated toward the sample average prescriptive values, i.e., provision of higher macronutrient goals was associated with slightly lower levels of consumption and provision of lower macronutrient goals was associated with slightly higher levels of consumption. This finding was consistent across caloric goals and all three macronutrient goals. A noteworthy observation is that the dietary intake data provided in Table 4 appear to reflect a higher degree of dietary adherence to the individually prescribed diets relative to the dietary intake information provided by Sacks et al. (2009), which was based on information obtained from dietary recall and diet records.
The treatment arm comparisons derived from a conceptualization of adherence in terms of eight independent indicator variables (see Table 4) yielded very different results when compared to results that conceptualized adherence as two independent dimensions, i.e., behavioral and dietary adherence. Examination of Table 4 shows that whichever indicator is selected as the “best” indicator of adherence determines the conclusion of which diets were associated with the highest levels of adherence. It is noteworthy that in the recent paper describing the primary findings of the POUNDS LOST trial, Sacks et al. (2009) reported that attendance to group sessions was similar across the four diet interventions, but was strongly associated with weight loss such that more frequent attendance to group sessions was associated with greater weight loss. In this secondary paper, when adherence was conceptualized as a two-dimensional construct, comparable levels of behavioral and dietary adherence were found across the high versus average protein diets but overall dietary adherence was higher among participants prescribed the two high fat diets in comparison to those prescribed low fat diets.
The study design called for consistent behavioral components across the four dietary intervention arms so that the study varied the prescription of dietary goals, not the intensity of the behavioral intervention. The finding that scores for the behavioral adherence factor did not differ as a function of type of dietary intervention suggests that the effort to equate the behavioral components was successful.
The findings of the study are limited by a variety of factors: (1) the study focused exclusively upon adherence to a weight management program with four different types of macronutrient diets, (2) a limited number (eight) of indicators of adherence were selected for study, (3) the self-reported caloric intakes may have been underestimated, (4) the study sample was highly selected and recruited at two clinical research sites and cannot be regarded as a representative sample of adults or even overweight/obese adults in the United States (e.g., the study sample had a majority of women and Caucasian participants), (5) physical activity was not adequately studied due to the design of the parent study that intentionally de-emphasized changes in physical activity and emphasized adherence to the four macronutrient diets that provided very specific dietary prescriptions, (6) the four dietary interventions of this study were, by definition, designed to enhance adherence to all aspects of the intervention, (7) one consequence of the decision to recruit participants with ages 30–70 years was that the POUNDS LOST study sample was slightly older than other recent weight management studies that recruited relatively healthy overweight or obese adults (e.g., Alhassan et al. 2008; Persky et al. 2005; Warziski et al. 2008), and (8) the examination of indicators of adherence in this study was limited to the first 6 months of the intervention.
It is, therefore, unknown whether the same factor structure would have emerged in a less structured medical, dietary, or behavioral regimen (e.g., only providing brief counseling to change diet and exercise). Therefore, it will be necessary for these findings to be replicated in other health behavior change trials and clinical settings that focus on other health concerns and employ different interventions and study different indicators of adherence. Based upon these preliminary results from the POUNDS LOST study, we conclude that adherence was best conceptualized as a multi-dimensional behavioral construct, and we encourage investigators to test this hypothesis in new studies that require adherence to a variety of medical procedures and include other behavioral prescriptions (e.g., explicit instructions to increase physical activity and/or improve physical fitness) and different methods for measuring behavioral indicators of adherence.
Acknowledgments
Supported by a cooperative agreement award HL073286 from National Heart, Lung, and Blood Institute, National Institutes of Health; and NIH General Clinical Research Center grant RR-02635. This study was approved by the appropriate ethics committees and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. All persons gave their informed consent prior to their inclusion in the study.
Footnotes
Most contemporary authors have preferred the term “adherence” over the term “compliance,” since the former term connotes behavior of the patient/participant related to following a medical prescription whereas the latter term connotes following a dictum from a higher authority. We concur with this contemporary preference for the term adherence and that will be our choice of wording throughout the paper.
The primary aim of the POUNDS LOST trial was to test the efficacy of four different macronutrient prescriptions for weight loss and health outcomes. The study design intentionally de-emphasized changes in physical activity and exercise so that diet effects on weight and health changes would not be overshadowed by changes in physical activity. Using this rationale, physical activity goals were set quite low, i.e., only 90 min per week of exercise via walking, and explicit instructions to promote physical activity, exercise, or fitness were deliberately avoided throughout the intervention. The study design called for equivalent levels of physical activity and other behavioral changes (e.g., self-monitoring and attendance to sessions, across the four treatment arms). As noted by Sacks et al. (2009), these objectives were met. One consequence of this decision for this ancillary study was that data collection related to adherence to physical activity prescriptions was not a part of the study design. As noted later in the paper, one effect of a lack of focus on physical activity was that participants did not report minutes of exercise nearly as often as they reported food intake (see Table 4).
The average number of extra sessions during the first 6 months of the study was 0.16 sessions. Participants assigned to the moderate fat/high protein diet attended more extra sessions (M = 0.31 vs. means ranging from 0.06 to 0.15 for the other treatment arms). This difference (p < 0.02) did not influence the findings since extra sessions were not counted toward adherence to attendance goals.
The use of absolute values based upon actual (not percent) deviations from caloric and macronutrient goals had the effect of creating dietary adherence variables that were not dependent upon one another, which would occur if percentages or raw (positive and negative deviations) values were used in the factor analyses.
We were concerned that these two factors may have emerged because of difference in variance that could be attributed to different methods. For example, the dietary factor was derived from indicators that were calculated by the computer tracking system and the behavioral factor included data that had been entered by counselors (for attendance) and self-monitoring by the participants. We converted the data for all eight variables to standardized scores and obtained identical findings. This statistical control may not entirely rule out this possible explanation of the factor structure; therefore, we believe that it will be important for future studies to evaluate the dimensionality of adherence to using entirely different methods for data collection and summary.
Contributor Information
Donald A. Williamson, Pennington Biomedical Research Center, LSU System, 6400 Perkins Rd., Baton Rouge, LA, USA
Stephen D. Anton, Pennington Biomedical Research Center, LSU System, 6400 Perkins Rd., Baton Rouge, LA, USA
Hongmei Han, Pennington Biomedical Research Center, LSU System, 6400 Perkins Rd., Baton Rouge, LA, USA.
Catherine M. Champagne, Pennington Biomedical Research Center, LSU System, 6400 Perkins Rd., Baton Rouge, LA, USA
Ray Allen, Pennington Biomedical Research Center, LSU System, 6400 Perkins Rd., Baton Rouge, LA, USA.
Eric LeBlanc, Pennington Biomedical Research Center, LSU System, 6400 Perkins Rd., Baton Rouge, LA, USA.
Donna H. Ryan, Pennington Biomedical Research Center, LSU System, 6400 Perkins Rd., Baton Rouge, LA, USA
Katherine McManus, Department of Nutrition, Harvard School of Public Health, Boston, MA, USA.
Nancy Laranjo, Department of Nutrition, Harvard School of Public Health, Boston, MA, USA.
Vincent J. Carey, Department of Nutrition, Harvard School of Public Health, Boston, MA, USA
Catherine M. Loria, National Heart, Lung, and Blood Institute, Bethesda, MD, USA
George A. Bray, Pennington Biomedical Research Center, LSU System, 6400 Perkins Rd., Baton Rouge, LA, USA
Frank M. Sacks, Department of Nutrition, Harvard School of Public Health, Boston, MA, USA
References
- Alhassan S, Kim S, Bersamin A, King AC, Gardner CD. Dietary adherence and weight loss success among overweight women: Results from the A TO Z weight loss study. International Journal of Obesity (London) 2008;32(6):985–991. doi: 10.1038/ijo.2008.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. American Journal of Clinical Nutrition. 1982;36(5):936–942. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associates, Inc.; Hillsdale, NJ: 1977. [Google Scholar]
- Evans IM. Response structure and the triple-response-mode concept. In: Nelson RO, Hayes SC, editors. Conceptual foundations of behavioral assessment. The Guilford Press; New York: 1986. pp. 131–155. [Google Scholar]
- Haynes RB, McDonald H, Garg AX, Montague P. Interventions for helping patients to follow prescriptions for medications. The Cochrane Database of Systematic Reviews. 2002;(2) doi: 10.1002/14651858.CD000011. doi:10.1002/14651858.CD000011. [DOI] [PubMed] [Google Scholar]
- Hays R, Stacy AW, DiMatteo MR. Covariation among health-related behaviors. Addictive Behaviors. 1984;9(3):315–318. doi: 10.1016/0306-4603(84)90028-5. [DOI] [PubMed] [Google Scholar]
- Levensky ER, O’Donohue WT. Patient adherence and nonadherence to treatments. In: O’Donohue WT, Levensky ER, editors. Promoting treatment adherence: A practical handbook for health care providers. Sage Publications Inc.; Thousand Oaks, CA: 2006. pp. 1–14. [Google Scholar]
- Leventhal H. Theories of compliance, and turning necessities into preferences: Application to adolescent health action. In: Krasnegor NA, Epstein LH, Johnson SB, Yaffe SJ, editors. Developmental aspects of health compliance behavior. Lawrence Erlbaum Associates Inc.; Hillsdale, NJ: 1993. pp. 91–124. [Google Scholar]
- Nelson RO, Hayes SC. Conceptual foundations of behavioral assessment. The Guilford Press; New York: 1986. [Google Scholar]
- Neumark-Sztainer D, Story M, Toporoff E, Himes JH, Resnick MD, Blum RW. Covariations of eating behaviors with other health-related behaviors among adolescents. The Journal of Adolescent Health. 1997;20(6):450–458. doi: 10.1016/S1054-139X(96)00279-0. [DOI] [PubMed] [Google Scholar]
- Nunnally JC, Bernstein IH. Psychometric theory. 3rd ed McGraw-Hill, Inc.; New York: 1994. [Google Scholar]
- Persky I, Spring B, Vander Wal JS, Pagoto S, Hedeker D. Adherence across behavioral domains in treatment promoting smoking cessation plus weight control. Health Psychology. 2005;24(2):153–160. doi: 10.1037/0278-6133.24.2.153. [DOI] [PubMed] [Google Scholar]
- Riekert KA. Integrating regimen adherence assessment into clinical practice. In: O’Donohue WT, Levensky ER, editors. Promoting treatment adherence. Sage Publications, Inc.; Thousand Oaks, CA: 2006. pp. 17–34. [Google Scholar]
- Rosenberg DE, Norman GJ, Sallis JF, Calfas KJ, Patrick K. Covariation of adolescent physical activity and dietary behaviors over 12 months. The Journal of Adolescent Health. 2007;41(5):472–478. doi: 10.1016/j.jadohealth.2007.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. New England Journal of Medicine. 2009;360(9):859–873. doi: 10.1056/NEJMoa0804748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shearer HM, Evans DR. Adherence to health care. In: Kazarian SS, Evans DR, editors. Handbook of cultural health psychology. Academic Press; San Diego, CA: 2001. pp. 113–138. [Google Scholar]
- Terre L, Drabman RS, Meydrech EF. Relationships among children’s health-related behaviors: A multivariate, developmental perspective. Preventive Medicine. 1990;19(2):134–146. doi: 10.1016/0091-7435(90)90015-c. [DOI] [PubMed] [Google Scholar]
- The Look AHEAD Research Group The Look AHEAD study: A description of the lifestyle intervention and the evidence supporting it. Obesity. 2006;14(5):737–775. doi: 10.1038/oby.2006.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Agriculture . Agricultural Research Service. Beltsville Human Nutrition Research Center, Food Surveys Research Group; Beltsville, MD: 1994–1996. Continuing survey of food intakes by individuals. [Google Scholar]
- Warziski MT, Sereika SM, Styn MA, Music E, Burke LE. Changes in self-efficacy and dietary adherence: The impact on the weight loss in the PREFER study. Journal of Behavioral Medicine. 2008;31:81–82. doi: 10.1007/s10865-007-9135-2. [DOI] [PubMed] [Google Scholar]
- Williamson DA, Martin CK, Stewart TM. Behavioral strategies for controlling obesity. In: Bray GA, Ryan DH, editors. Overweight and the metabolic syndrome: From bench to bedside. Springer; New York: 2006. pp. 219–232. [Google Scholar]