Abstract
BACKGROUND
Intima–media thickness of the walls of the common carotid artery and internal carotid artery may add to the Framingham risk score for predicting cardiovascular events.
METHODS
We measured the mean intima–media thickness of the common carotid artery and the maximum intima–media thickness of the internal carotid artery in 2965 members of the Framingham Offspring Study cohort. Cardiovascular-disease outcomes were evaluated for an average follow-up of 7.2 years. Multivariable Cox proportional-hazards models were generated for intima–media thickness and risk factors. We evaluated the reclassification of cardiovascular disease on the basis of the 8-year Framingham risk score category (low, intermediate, or high) after adding intima–media thickness values.
RESULTS
A total of 296 participants had a cardiovascular event. The risk factors of the Framingham risk score predicted these events, with a C statistic of 0.748 (95% confidence interval [CI], 0.719 to 0.776). The adjusted hazard ratio for cardiovascular disease with a 1-SD increase in the mean intima–media thickness of the common carotid artery was 1.13 (95% CI, 1.02 to 1.24), with a nonsignificant change in the C statistic of 0.003 (95% CI, 0.000 to 0.007); the corresponding hazard ratio for the maximum intima–media thickness of the internal carotid artery was 1.21 (95% CI, 1.13 to 1.29), with a modest increase in the C statistic of 0.009 (95% CI, 0.003 to 0.016). The net reclassification index increased significantly after addition of intima–media thickness of the internal carotid artery (7.6%, P<0.001) but not intima–media thickness of the common carotid artery (0.0%, P = 0.99). With the presence of plaque, defined as intima–media thickness of the internal carotid artery of more than 1.5 mm, the net reclassification index was 7.3% (P = 0.01), with an increase in the C statistic of 0.014 (95% CI, 0.003 to 0.025).
CONCLUSIONS
The maximum internal and mean common carotid-artery intima–media thicknesses both predict cardiovascular outcomes, but only the maximum intima–media thickness of (and presence of plaque in) the internal carotid artery significantly (albeit modestly) improves the classification of risk of cardiovascular disease in the Framingham Offspring Study cohort. (Funded by the National Heart, Lung, and Blood Institute.)
Carotid-wall intima–media thickness is a surrogate measure of atherosclerosis1 associated with cardiovascular risk factors2 and with cardiovascular outcomes.3–7 The intima–media thickness is the distance from the lumen–intima interface to the media–adventitia interface of the artery wall, as measured on noninvasively acquired ultrasonographic images of the carotid arteries. Increased intima–media thickness of the common carotid artery represents a form of atherosclerosis that is manifested as diffuse arterial-wall thickening,8 whereas increased intima–media thickness of the proximal internal carotid artery is a surrogate for focal atherosclerotic plaque.9 The mean intima–media thickness of the common carotid artery is a more reproducible measure than the intima–media thickness of the internal carotid artery and is believed to be better suited for cardiovascular risk assessment10 and intervention studies.11 Although measurement of intima–media thickness is promoted as a tool for cardiovascular risk assessment12,13 in primary prevention, the incremental predictive value of the intima–media thickness of either the common carotid artery or the internal carotid artery, over and above the value of traditional cardiovascular risk factors, is questionable.14,15
We hypothesized that the intima–media thicknesses of the common carotid artery and internal carotid artery would add to the predictive value of Framingham risk factors regarding new-onset cardiovascular events in a population-based cohort; we tested this hypothesis in the Framingham Offspring Study cohort. We also hypothesized that consideration of the intima–media thickness would improve the classification of patients into Framingham risk score categories.
METHODS
STUDY PARTICIPANTS
The study population consisted of members of the Framingham Offspring Study cohort, composed of non-Hispanic whites, who were undergoing the sixth examination cycle, from February 1995 through September 1998. Of the 3532 persons seen during the clinic visit, 2965 who did not have current disease underwent ultrasonography, of whom 2946 had interpretable images of the internal carotid artery. Missing data were due to scheduling issues or unavailability of the ultrasonographic device. Details of the Framingham Offspring Study design have been published previously.16 All participants in our study provided written informed consent, and the institutional review board at Boston Medical Center approved our study protocol.
ASSESSMENT OF RISK FACTORS
During the clinic visit, a medical history was obtained, and a physical examination was performed. The measured cardiovascular risk factors relevant to our study were systolic blood pressure, cigarette-smoking status, total cholesterol level, high-density lipoprotein (HDL) cholesterol level, and presence or absence of hypertension treatment, diabetes, and a history of cardiovascular disease, including stroke.
The systolic blood pressure was determined from the average of two measurements of resting systolic blood pressure, performed by a physician using a 14-cm–wide blood-pressure cuff on the right arm. Smoking status was ascertained on the basis of the self-reported history of cigarette smoking. The presence of diabetes was based on a history of diabetes, defined as either a current or previous fasting glucose level of 126 mg per deciliter (7 mmol per liter) or higher or current or previous use of antihyperglycemic medication. All lipid analyses were performed at the Framingham Heart Study laboratory according to the Standardization Program of the Centers for Disease Control and Prevention and the Lipid Research Clinics of the National Heart, Lung, and Blood Institute.17,18
ASSESSMENT OF INTIMA–MEDIA THICKNESS
Ultrasonographic images were acquired at end diastole (defined as the R wave of an electrocardiogram) by a sonographer certified by the Registry of Diagnostic Medical Sonographers. Intima–media interface lines were manually traced as continuous lines by a certified reader, and intima–media thickness values were calculated.19 The mean intima–media thickness of the common carotid artery was measured over a segment of the common carotid artery that was 1 cm long, located approximately 0.5 cm below the carotid-artery bulb, and considered not to contain any plaque (i.e., not to have any perceivable protrusion of the artery wall into the lumen).20 The maximum intima–media thickness of the internal carotid artery was defined as the greatest intima–media thickness in either the right or left internal carotid artery extending from the bulb to 1 cm above the carotid sinus, ascertained from a total of four views on each side. Reproducibility was assessed by replicating measurements for 37 participants.19 Pearson’s correlation coefficient for replicate readings was 0.94 for the mean intima–media thickness of the common carotid artery and 0.76 for the maximum intima–media thickness of the internal carotid artery.
INCIDENT CARDIOVASCULAR DISEASE
All cardiovascular events in the Framingham Offspring Study cohort were adjudicated by a panel of three physicians, on the basis of a review of data collected from Framingham clinic visits, inpatient hospitalizations, and office records. For this study, we used the Framingham Heart Study definition of cardiovascular disease: coronary heart disease (i.e., a fatal coronary event, myocardial infarction, coronary insufficiency, or angina), a cerebrovascular event (i.e., ischemic stroke, hemorrhagic stroke, or transient ischemic attack), peripheral arterial disease (i.e., intermittent claudication), or heart failure.21
STATISTICAL ANALYSIS
Multivariable Cox proportional-hazards models were generated, with the following candidate variables: age, sex, systolic blood pressure, total cholesterol level, HDL cholesterol level, presence or absence of diabetes, and smoking status — the original components of the 10-year Framingham risk score for general cardiovascular disease. Presence or absence of hypertensive treatment was added to the models.21
Two separate models were then created by adding the mean intima–media thickness of the common carotid artery and the maximum intima–media thickness of the internal carotid artery as separate predictor variables. Hazard ratios were generated for each independent variable in each of the two models. We evaluated differences between the two models, after confirming the calibration of the original Cox models, by comparing the respective C statistics before and after the addition of the variables for intima–media thickness.22
The incremental effect of adding intima–media thickness to the Framingham risk score for predicting cardiovascular outcomes was evaluated with the use of the net reclassification index.23 First, we stratified participants into one of three risk categories on the basis of their Framingham risk score for general cardiovascular disease (calculated for this study as an 8-year score): low risk (0 to <6%), intermediate risk (6 to 20%), or high risk (>20%). Then, we used the intima–media thickness to reclassify the risk category, specifically to ascertain whether there would be improvement in the net reclassification index — that is, whether reclassification would assign persons in whom cardiovascular disease developed to a higher risk category and those in whom cardiovascular disease did not develop to a lower risk category.23 The net reclassification index also accounts for movement between categories in the opposite direction than predicted and applies different weights to events and nonevents.23 Separate net-reclassification-index values were calculated for men and women as well as for participants who were 60 years of age or younger and participants who were older than 60 years at baseline, on the basis of the probability of a cardiovascular event and the probability of no event, as predicted from pooled models (combining women and men and all ages) with and without inclusion of intima–media thickness of the internal carotid artery.
We also investigated models in which the presence of plaque, defined as an intima–media thickness of more than 1.5 mm, was used as a predictor variable and examined how the presence of plaque affected the prediction of events within the Framingham risk score categories, using log-rank statistics across all strata. All analyses were performed with the use of SAS software (version 9.1), and a two-sided P value of less than 0.05 was considered to indicate statistical significance.
RESULTS
CHARACTERISTICS OF THE PARTICIPANTS
A total of 2965 participants with a mean (±SD) age of 58±10 years and no history of cardiovascular disease, 1629 (55.3%) of whom were women, were followed for an average of 7.2 years. There were 296 first-time cardiovascular events. The baseline characteristics of the participants are shown in Table 1, and a breakdown of types of cardiovascular events is given in the Supplementary Appendix (available with the full text of this article at NEJM.org).
Table 1.
Baseline Characteristics of the 2965 Participants without Evidence of Cardiovascular Disease (CVD) on Ultrasonography, According to CVD Status at Follow-up.*
| Characteristic | No CVD at Follow-up (N = 2669) | CVD at Follow-up (N = 296) |
|---|---|---|
| Duration of follow-up — yr | 7.5±1.7 | 4.6±2.8 |
| Age — yr | 57.3±9.5 | 62.9±9.5 |
| Female sex — no. (%) | 1501 (56.2) | 128 (43.2) |
| Systolic blood pressure — mm Hg | 126.8±18.4 | 136.8±19.2 |
| Treatment for high blood pressure — no. (%) | 598 (22.4) | 126 (42.6) |
| Cholesterol — mg/dl | ||
| Total | 206.1±39.1 | 211.1±41.4 |
| HDL | 52.3±16.3 | 46.2±12.9 |
| Diabetes — no. (%) | 205 (7.7) | 52 (17.6) |
| Cigarette smoking — no. (%) | 377 (14.1) | 64 (21.6) |
| Intima–media thickness† | ||
| Mean CCA thickness — mm | 0.59±0.13 | 0.66±0.15 |
| Maximum ICA thickness — mm | 1.30±0.79 | 1.90±1.00 |
| ICA thickness >1.5 mm, indicating plaque— no. (%) | 727 (27.4) | 177 (59.6) |
Plus–minus values are means ±SD. CCA denotes common carotid artery, HDL high-density lipoprotein, and ICA internal carotid artery. To convert the values for cholesterol to millimoles per liter, multiply by 0.02586.
Data on the maximum intima–media thickness of the ICA were available for 2946 persons.
PREDICTIVE VALUE OF INTIMA–MEDIA THICKNESS
Multivariable Cox proportional-hazards models were constructed to include Framingham risk factors only, risk factors plus the mean intima–media thickness of the common carotid artery (Table 2), and risk factors plus the maximum intima–media thickness of the internal carotid artery (Table 3). The results showed that the Framingham risk factors were all significant predictors of cardiovascular disease. The addition of the mean intima–media thickness for the common carotid artery was significantly associated with the risk of cardiovascular disease (hazard ratio per 1-SD increase in thickness, 1.13; 95% confidence interval [CI], 1.02 to 1.24; P = 0.02). However, the C statistic increased only nonsignificantly, by 0.003 (95% CI, 0.000 to 0.007; P = 0.07), from 0.748 (95% CI, 0.719 to 0.776) to 0.751 (95% CI, 0.723 to 0.779). The maximum intima–media thickness of the internal carotid artery was also significantly associated with the risk of cardiovascular disease (hazard ratio per 1-SD increase in thickness, 1.21; 95% CI, 1.13 to 1.29; P<0.001) in models that included the Framingham risk factors. Moreover, when internal carotid artery intima–media thickness was added to the model, the C statistic increased significantly, by 0.010 (95% CI, 0.003 to 0.016; P = 0.003), from 0.748 (95% CI, 0.719 to 0.776) to 0.758 (95% CI, 0.730 to 0.785).
Table 2.
Hazard Ratios for Cardiovascular Disease, According to Models with and without Common Carotid Artery (CCA) Intima–Media Thickness.*
| Risk Factor | Model with Risk Factors Only | Model with Risk Factors and CCA Intima–Media Thickness | ||
|---|---|---|---|---|
| Hazard Ratio or C Statistic (95% CI) | P Value | Hazard Ratio or C Statistic (95% CI) | P Value | |
| Sex, female vs. male | 0.74 (0.58–0.96) | 0.02 | 0.77 (0.59–0.99) | 0.04 |
|
| ||||
| Age, per increase of 1 yr | 1.05 (1.04–1.07) | <0.001 | 1.05 (1.03–1.06) | <0.001 |
|
| ||||
| Systolic pressure, per increase of 1 mm Hg | 1.01 (1.01–1.02) | <0.001 | 1.01 (1.00–1.02) | 0.001 |
|
| ||||
| Treatment for high blood pressure, yes vs. no | 1.52 (1.18–1.96) | 0.001 | 1.50 (1.17–1.93) | 0.002 |
|
| ||||
| Cholesterol, per increase of 1 mg/dl
| ||||
| Total | 1.00 (1.00–1.01) | 0.02 | 1.00 (1.00–1.01) | 0.02 |
|
| ||||
| HDL | 0.98 (0.97–0.99) | <0.001 | 0.98 (0.97–0.99) | <0.001 |
|
| ||||
| Diabetes, yes vs. no | 1.47 (1.08–2.01) | 0.02 | 1.46 (1.07–1.99) | 0.02 |
|
| ||||
| Cigarette smoking, yes vs. no | 2.25 (1.69–3.00) | <0.001 | 2.16 (1.62–2.90) | <0.001 |
|
| ||||
| CCA intima–media thickness
| ||||
| Per increase of 1 mm | 2.46 (1.18–5.13) | 0.02 | ||
|
| ||||
| Per increase of 1 SD | 1.13 (1.02–1.24) | 0.02 | ||
|
| ||||
| C statistic | 0.748 (0.719–0.776) | 0.751 (0.723–0.779) | ||
The results of Cox proportional-hazards models are shown. HDL denotes high-density lipoprotein.
Table 3.
Hazard Ratios for Cardiovascular Disease, According to Models with and without Internal Carotid Artery (ICA) Intima–Media Thicknesses.*
| Risk Factor | Model with Risk Factors Only | Model with Risk Factors and ICA Intima–Media Thickness | Model with Risk Factors and ICA Intima–Media Thickness >1.5 mm | |||
|---|---|---|---|---|---|---|
| Hazard Ratio or C Statistic (95% CI) | P Value | Hazard Ratio or C Statistic (95% CI) | P Value | Hazard Ratio or C Statistic (95% CI) | P Value | |
| Sex, female vs. male | 0.74 (0.57–0.95) | 0.02 | 0.78 (0.61–1.01) | 0.06 | 0.79 (0.61–1.02) | 0.07 |
|
| ||||||
| Age, per increase of 1 yr | 1.05 (1.04–1.07) | <0.001 | 1.05 (1.03–1.06) | <0.001 | 1.04 (1.03–1.06) | <0.001 |
|
| ||||||
| Systolic pressure, per increase of 1 mm Hg | 1.01 (1.01–1.02) | <0.001 | 1.01 (1.01–1.02) | <0.001 | 1.01 (1.00–1.02) | 0.002 |
|
| ||||||
| Treatment for high blood pressure, yes vs. no | 1.55 (1.21–2.00) | <0.001 | 1.51 (1.18–1.95) | 0.001 | 1.47 (1.14–1.89) | 0.003 |
|
| ||||||
| Cholesterol, per increase of 1 mg/dl
| ||||||
| Total | 1.00 (1.00–1.01) | 0.02 | 1.00 (1.00–1.01) | 0.03 | 1.00 (1.00–1.01) | 0.03 |
|
| ||||||
| HDL | 0.98 (0.97–0.99) | <0.001 | 0.98 (0.97–0.99) | <0.001 | 0.98 (0.97–0.99) | <0.001 |
|
| ||||||
| Diabetes, yes vs. no | 1.44 (1.06–1.97) | 0.02 | 1.41 (1.03–1.92) | 0.03 | 1.38 (1.01–1.88) | 0.04 |
|
| ||||||
| Cigarette smoking, yes vs. no | 2.23 (1.67–2.98) | <0.001 | 2.10 (1.57–2.81) | <0.001 | 1.97 (1.47–2.64) | <0.001 |
|
| ||||||
| ICA intima–media thickness
| ||||||
| Per increase of 1 mm | 1.26 (1.16–1.36) | <0.001 | ||||
|
| ||||||
| Per increase of 1 SD | 1.21 (1.13–1.29) | <0.001 | ||||
|
| ||||||
| Thickness ≥1.5 mm, representing plaque | 1.92 (1.49–2.47) | <0.001 | ||||
|
| ||||||
| C statistic | 0.748 (0.719–0.776) | 0.758 (0.730–0.785) | 0.762 (0.734–0.789) | |||
The results of Cox proportional-hazards models are shown. HDL denotes high-density lipoprotein
NET RECLASSIFICATION INDEX
We treated intima–media thickness variables as continuous and reclassified the original Framingham risk scores for the study participants. The resultant net reclassification index was significant with the inclusion of maximum intima–media thickness of the internal carotid artery (index, 5.8% for participants with cardiovascular events, 1.8% for participants without cardiovascular events, and 7.6% overall; P<0.001) (Table 4) but not for mean intima–media thickness of the common carotid artery (index, 0.4% for events, 0.4% for nonevents, and 0.0% overall; P = 0.99) (Table 3 in the Supplementary Appendix).
Table 4.
Reclassification of Framingham Risk Score Categories after Addition of Intima–Media Thickness of Internal Carotid Artery.*
| Original Risk Category | Reclassification | ||
|---|---|---|---|
| Low Risk | Intermediate Risk | High Risk | |
| number of participants | |||
|
Participants without cardiovascular events
| |||
| Low risk | 1125 | 31 | 0 |
|
| |||
| Intermediate risk | 85 | 1126 | 45 |
|
| |||
| High risk | 0 | 40 | 234 |
|
| |||
|
Participants with cardiovascular events
| |||
| Low risk | 27 | 8 | 0 |
|
| |||
| Intermediate risk | 1 | 112 | 13 |
|
| |||
| High risk | 0 | 5 | 94 |
According to the Framingham score, calculated in this case for an 8-year risk of cardiovascular disease, low risk indicates a risk of less than 6%, intermediate risk a risk of 6 to 20%, and high risk a risk of more than 20%. The net reclassification index was 1.8% (49 of 2686 participants) for participants without events, 5.8% (15 of 260 participants) for those with events, and 7.6% overall.
In pooled analyses, internal carotid artery intima–media thickness significantly increased the net reclassification index for men and women (index, 6.7% and 9.2%, respectively), as well as for persons 60 years of age or younger and those older than 60 years (index, 9.1% and 7.6%, respectively) (P<0.05 for all comparisons).
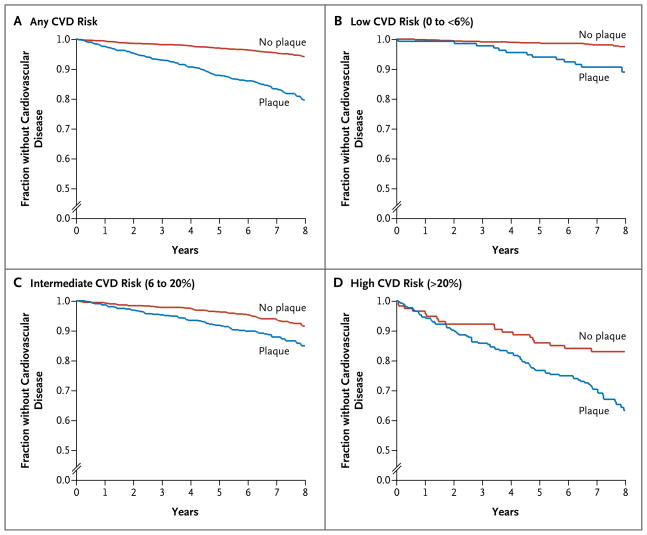
PREDICTIVE VALUE OF PLAQUE
The presence of plaque, defined as a maximum intima–media thickness of greater than 1.5 mm in the internal carotid artery, was a significant independent predictor of cardiovascular events (Table 3), significantly increasing the C statistic from 0.748 to 0.762 (increase of 0.014; 95% CI, 0.003 to 0.025; P=0.02) and a significant (P=0.01) but modest net reclassification index of 7.3% (Table 3 in the Supplementary Appendix). Kaplan–Meier estimates for participants in each risk category confirmed that the presence of plaque significantly improved the prediction of new-onset cardiovascular disease (Fig. 1) across all strata.
Figure 1. Kaplan–Meier Estimates of the Probability of New-Onset Cardiovascular Disease (CVD).
Data are shown for all 2946 participants overall (Panel A) and according to the category of Framingham risk score for CVD: low risk (0 to <6%) (Panel B), intermediate risk (6 to 20%) (Panel C), and high risk (>20%) (Panel D). In the low-risk category, 134 of the 1191 persons had plaque, for a prevalence of 11.3%, and the 8-year rates of cardiovascular disease were 2.5% and 11.0% among persons without plaque and those with plaque, respectively (P<0.001) (Panel B). In the intermediate-risk category, 513 of the 1382 persons had plaque, for a prevalence of 37.1%, and the 8-year rates of cardiovascular disease were 8.5% and 15.1% among persons without plaque and those with plaque, respectively (P<0.001) (Panel C). In the high-risk category, 257 of the 373 persons had plaque, for a prevalence of 68.9%, and the 8-year rates of cardiovascular disease were 17.0% and 36.7% among persons without plaque and those with plaque, respectively (P = 0.004) (Panel D).
DISCUSSION
Carotid-artery intima–media thickness, measured noninvasively with the use of carotid-artery ultrasonography, is an independent predictor of new cardiovascular events in persons without a history of cardiovascular disease. The intima–media thickness of the internal carotid artery, but not of the common carotid artery, significantly improved two metrics used to determine the value of a biomarker for cardiovascular risk prediction: the C statistic, derived from multivariable Cox-proportional-hazards models, and the net reclassification index for Framingham risk score categories. The intima–media thickness of the internal carotid artery also modestly but significantly added predictive value to the Framingham risk score when dichotomized at a threshold used to define plaque (>1.5 mm, vs. ≤1.5 mm for no plaque).
Ultrasonographic measurements of intima–media thickness can be limited to the common carotid artery,5,7 averaged across multiple carotid-artery segments,4,6 or combined as a score.3 A review of eight epidemiologic studies showed that the intima–media thickness of the common carotid artery by itself (in all eight studies) or combined with the intima–media thickness of the internal carotid artery and presented as a score (in one of the eight studies) had independent predictive power with respect to cardiovascular events.24 Three studies with separate measurements for the common and internal carotid arteries showed significant associations of cardiovascular events with intima–media thickness.4,25,26 Our study confirms that intima–media thickness of the common carotid artery and that of the internal carotid artery are independent predictors of cardiovascular outcomes.
It is not clear whether the intima–media thickness incrementally adds value to the Framingham risk factors for cardiovascular-risk prediction. The addition of intima–media thickness measurements slightly increased the predictive power with respect to cardiovascular risk assessment in one study14 and with respect to stroke in another study.27 The presence of plaque (defined as an internal-carotid-artery intima–media thickness ≥1.9 mm) has been shown to be associated with increased event rates.28 Our data clearly show that addition of the intima–media thickness of the internal carotid artery increases the net reclassification index for risk categories based on the Framingham risk factors.
Reclassification is a practical approach to gauging the effects of adding new risk factors to the traditional Framingham risk factors when differences in the C statistic are marginal.23 A recent meta-analysis reviewed studies suggesting that a new risk factor added predictive value to the Framingham risk score.29 We performed our study according to the criteria proposed in the meta-analysis: verification of regression calibration, predictive value of the new risk factor in a multivariable model with the Framingham risk factors, positive change in the C statistic, and an increased net reclassification index. The intima–media thickness of the internal carotid artery satisfied all these metrics, whereas the intima–media thickness of the common carotid artery did not. The Atherosclerosis Risk in Communities study (ARIC; ClinicalTrials.gov number, NCT00005131)4 showed an increase in the area under the curve from 0.742 to 0.755 and an increase in the net reclassification index of 9.9%15 for predicting incident coronary heart disease with the use of the intima–media thickness of the common carotid artery in combination with the presence or absence of plaque, whereas the results with the use of the intima–media thickness of the common carotid artery alone were modest.
Our study differs from the ARIC study in several respects. The mean follow-up period was 7.2 years in our study, as compared with 10 years in the ARIC study; our study was smaller (2946 participants, as compared with 13,145); and we excluded plaques from our measurement of intima–media thickness in the common carotid artery, whereas in the ARIC study, plaques were included.15,30 Plaque in the common carotid artery may account for the weak positive associations between intima–media thickness of the common carotid artery and outcomes in the ARIC study. Further clarification of the predictive power of risk factors and intima–media thickness will most likely require verification in other epidemiologic cohorts and attention to differences in the protocol for measurement of the intima–media thickness.
We chose to assess the net reclassification index for three clinically relevant risk categories.21,23 These categories were intended to reflect clinical practice, in which high risk may suggest the need for treatment, low risk indicates the absence of clinical symptoms of any form of cardiovascular disease, and intermediate risk reflects the state in between. Similar categories are used in widely applied national guidelines for lipid-lowering interventions.31 Splitting the middle category into two would introduce the potential for additional movement between categories that may not have clinical implications unless attention is given to specific risk factors.31 Even within the three Framingham risk categories we used, the presence of plaque, defined as an intima–media thickness of more than 1.5 mm, was a significant predictor of cardiovascular events (Fig. 1), suggesting that further analyses are needed to evaluate the effect of plaque on risk stratification.
A limitation of our study is the white race of our population, such that our results may not be applicable to other races or ethnic groups. However, the Framingham risk factors and the risk score have been successfully applied to various ethnic groups,32,33 and intima–media thickness seems to be similarly applicable.34 Another limitation is our 7.2-year follow-up period, which is shorter than the 10-year period for which the Framingham risk score is calculated.35 This discrepancy may have decreased the overall power of our observations. In addition, we relied on a single experienced and supervised sonographer to obtain high-quality measurements during carotid-artery ultrasonography, but this might affect the implementation of our findings in primary prevention, since we believe that the sonographer’s judgment and experience affect the assessment for plaque in the internal carotid artery.19 One benefit of using the sonographer, however, was that data on intima–media thickness in the internal carotid artery were missing for only 19 of our 2965 participants.
Our results may affect how intima–media thickness is assessed for the primary prevention of cardiovascular disease. The recent American College of Cardiology Foundation–American Heart Association guidelines13 give carotid intima–media thickness a level IIa recommendation for cardiovascular risk evaluation (the same as the recommendation level for the ankle–brachial index and coronary-artery calcium scoring), with an emphasis on an indication of high risk if the common-carotid-artery intima–media thickness is above the 75th percentile.10 The 75th-percentile threshold is also adopted in the report of the Screening for Heart Attack Prevention and Education Task Force,12 and its use is currently reimbursed in one state.36 However, these two guidelines lack quantitative criteria for the intima–media thickness of the internal carotid artery.
Our results show that plaque in the internal carotid artery, either measured as part of the continuous intima–media thickness or assumed to be present if the thickness exceeds a set point of 1.5 mm, offers modest incremental value to the Framingham risk score in predicting cardiovascular events. We believe the intima–media thickness of the internal carotid artery should be measured in addition to the thickness of the common carotid artery for purposes of cardiovascular risk assessment. One limitation, however, may be the method used to measure the intima–media thickness of the internal carotid artery. We used a continuous tracing of the contour of the wall and an automatic algorithm to determine the maximum value.19 The results of these offline measurements may differ from the results of measurements made with the calipers available on an ultrasonographic imaging device.
We conclude that the intima–media thickness of the common carotid artery and the intima–media thickness of the internal carotid artery are independent predictors of cardiovascular events among participants in the Framingham Offspring Study. The maximum intima–media thickness of the internal carotid artery, as either a continuous measurement or a surrogate for the presence of plaque (above a threshold of 1.5 mm), contributed significantly but modestly to the predictive power of the risk factors used in calculating the Framingham risk score and improved risk classification on the basis of the Framingham risk score.
Supplementary Material
Acknowledgments
Supported by grants from the National Heart, Lung, and Blood Institute (R01 HL069003 and HL081352, to Dr. Polak) and its Framingham Heart Study (N01-HC-25195).
We thank Allison Meisner for performing additional verification of the data presented in the manuscript.
Footnotes
Dr. Pencina reports receiving fees for board membership from Abbott. No other potential conflict of interest relevant to this article was reported.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Hodis HN, Mack WJ, LaBree L, et al. Reduction in carotid arterial wall thickness using lovastatin and dietary therapy: a randomized controlled clinical trial. Ann Intern Med. 1996;124:548–56. doi: 10.7326/0003-4819-124-6-199603150-00002. [DOI] [PubMed] [Google Scholar]
- 2.O’Leary DH, Polak JF, Kronmal RA, et al. Thickening of the carotid wall: a marker for atherosclerosis in the elderly? Stroke. 1996;27:224–31. doi: 10.1161/01.str.27.2.224. [DOI] [PubMed] [Google Scholar]
- 3.O’Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK., Jr Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. N Engl J Med. 1999;340:14–22. doi: 10.1056/NEJM199901073400103. [DOI] [PubMed] [Google Scholar]
- 4.Chambless LE, Heiss G, Folsom AR, et al. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study, 1987–1993. Am J Epidemiol. 1997;146:483–94. doi: 10.1093/oxfordjournals.aje.a009302. [DOI] [PubMed] [Google Scholar]
- 5.Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE. Common carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam Study. Circulation. 1997;96:1432–7. doi: 10.1161/01.cir.96.5.1432. [DOI] [PubMed] [Google Scholar]
- 6.Chambless LE, Folsom AR, Clegg LX, et al. Carotid wall thickness is predictive of incident clinical stroke: the Atherosclerosis Risk in Communities (ARIC) study. Am J Epidemiol. 2000;151:478–87. doi: 10.1093/oxfordjournals.aje.a010233. [DOI] [PubMed] [Google Scholar]
- 7.Hodis HN, Mack WJ, LaBree L, et al. The role of carotid arterial intima-media thickness in predicting clinical coronary events. Ann Intern Med. 1998;128:262–9. doi: 10.7326/0003-4819-128-4-199802150-00002. [DOI] [PubMed] [Google Scholar]
- 8.Pignoli P, Tremoli E, Poli A, Oreste P, Paoletti R. Intimal plus medial thickness of the arterial wall: a direct measurement with ultrasound imaging. Circulation. 1986;74:1399–406. doi: 10.1161/01.cir.74.6.1399. [DOI] [PubMed] [Google Scholar]
- 9.Dalager S, Paaske WP, Kristensen IB, Laurberg JM, Falk E. Artery-related differences in atherosclerosis expression: implications for atherogenesis and dynamics in intima-media thickness. Stroke. 2007;38:2698–705. doi: 10.1161/STROKEAHA.107.486480. [DOI] [PubMed] [Google Scholar]
- 10.Stein JH, Korcarz CE, Hurst RT, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force: endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr. 2008;21:93–111. doi: 10.1016/j.echo.2007.11.011. [Erratum, J Am Soc Echocardiogr 2008;21:376.] [DOI] [PubMed] [Google Scholar]
- 11.Touboul PJ, Hennerici MG, Meairs S, et al. Mannheim intima-media thickness consensus. Cerebrovasc Dis. 2004;18:346–9. doi: 10.1159/000081812. [DOI] [PubMed] [Google Scholar]
- 12.Naghavi M, Falk E, Hecht HS, et al. From vulnerable plaque to vulnerable patient — part III: executive summary of the Screening for Heart Attack Prevention and Education (SHAPE) Task Force report. Am J Cardiol. 2006;98:2H–15H. doi: 10.1016/j.amjcard.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 13.Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2010;122:2748–64. doi: 10.1161/CIR.0b013e3182051bab. [DOI] [PubMed] [Google Scholar]
- 14.del Sol AI, Moons KG, Hollander M, et al. Is carotid intima-media thickness useful in cardiovascular disease risk assessment? The Rotterdam Study. Stroke. 2001;32:1532–8. doi: 10.1161/01.str.32.7.1532. [DOI] [PubMed] [Google Scholar]
- 15.Nambi V, Chambless L, Folsom AR, et al. Carotid intima-media thickness and presence or absence of plaque improves prediction of coronary heart disease: the ARIC (Atherosclerosis Risk in Communities) study. J Am Coll Cardiol. 2010;55:1600–7. doi: 10.1016/j.jacc.2009.11.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kannel WB, Feinleib M, McNamara PM, Garrison RJ, Castelli WP. An investigation of coronary heart disease in families: the Framingham Offspring Study. Am J Epidemiol. 1979;110:281–90. doi: 10.1093/oxfordjournals.aje.a112813. [DOI] [PubMed] [Google Scholar]
- 17.McNamara JR, Schaefer EJ. Automated enzymatic standardized lipid analyses for plasma and lipoprotein fractions. Clin Chim Acta. 1987;166:1–8. doi: 10.1016/0009-8981(87)90188-4. [DOI] [PubMed] [Google Scholar]
- 18.Warwick GR, Benderson J, Albers JJ. Dextran sulfate-magnesium precipitation procedure for quantitation of high-density-lipoprotein cholesterol. Clin Chem. 1982;28:1379–88. [PubMed] [Google Scholar]
- 19.Polak JF, Pencina MJ, Meisner A, et al. Associations of carotid artery intima-media thickness (IMT) with risk factors and prevalent cardiovascular disease: comparison of mean common carotid artery IMT with maximum internal carotid artery IMT. J Ultrasound Med. 2010;29:1759–68. doi: 10.7863/jum.2010.29.12.1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Polak JF, O’Leary DH, Kronmal RA, et al. Sonographic evaluation of carotid artery atherosclerosis in the elderly: relationship of disease severity to stroke and transient ischemic attack. Radiology. 1993;188:363–70. doi: 10.1148/radiology.188.2.8327679. [DOI] [PubMed] [Google Scholar]
- 21.D’Agostino RB, Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–53. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 22.Pencina MJ, D’Agostino RB. Overall C as a measure of discrimination in survival analysis: model specific population value and confidence interval estimation. Stat Med. 2004;23:2109–23. doi: 10.1002/sim.1802. [DOI] [PubMed] [Google Scholar]
- 23.Pencina MJ, D’Agostino RB, Sr, D’Agostino RB, Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–72. doi: 10.1002/sim.2929. [DOI] [PubMed] [Google Scholar]
- 24.Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. 2007;115:459–67. doi: 10.1161/CIRCULATIONAHA.106.628875. [DOI] [PubMed] [Google Scholar]
- 25.Lorenz MW, von Kegler S, Steinmetz H, Markus HS, Sitzer M. Carotid intima-media thickening indicates a higher vascular risk across a wide age range: prospective data from the Carotid Atherosclerosis Progression Study (CAPS) Stroke. 2006;37:87–92. doi: 10.1161/01.STR.0000196964.24024.ea. [DOI] [PubMed] [Google Scholar]
- 26.Rosvall M, Janzon L, Berglund G, Engström G, Hedblad B. Incident coronary events and case fatality in relation to common carotid intima-media thickness. J Intern Med. 2005;257:430–7. doi: 10.1111/j.1365-2796.2005.01485.x. [DOI] [PubMed] [Google Scholar]
- 27.Touboul PJ, Labreuche J, Vicaut E, Amarenco P. Carotid intima-media thickness, plaques, and Framingham risk score as independent determinants of stroke risk. Stroke. 2005;36:1741–5. doi: 10.1161/01.STR.0000174490.23495.57. [DOI] [PubMed] [Google Scholar]
- 28.Rundek T, Arif H, Boden-Albala B, El-kind MS, Paik MC, Sacco RL. Carotid plaque, a subclinical precursor of vascular events: the Northern Manhattan Study. Neurology. 2008;70:1200–7. doi: 10.1212/01.wnl.0000303969.63165.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tzoulaki I, Liberopoulos G, Ioannidis JPA. Assessment of claims of improved prediction beyond the Framingham risk score. JAMA. 2009;302:2345–52. doi: 10.1001/jama.2009.1757. [DOI] [PubMed] [Google Scholar]
- 30.Li R, Duncan BB, Metcalf PA, et al. B-mode-detected carotid artery plaque in a general population. Stroke. 1994;25:2377–83. doi: 10.1161/01.str.25.12.2377. [DOI] [PubMed] [Google Scholar]
- 31.Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 32.D’Agostino RB, Sr, Grundy S, Sullivan LM, Wilson P. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA. 2001;286:180–7. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- 33.Liu J, Hong Y, D’Agostino RB, Sr, et al. Predictive value for the Chinese population of the Framingham CHD risk assessment tool compared with the Chinese Multi-Provincial Cohort Study. JAMA. 2004;291:2591–9. doi: 10.1001/jama.291.21.2591. [DOI] [PubMed] [Google Scholar]
- 34.Folsom AR, Kronmal RA, Detrano RC, et al. Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: the Multi-Ethnic Study of Atherosclerosis (MESA) Arch Intern Med. 2008;168:1333–9. doi: 10.1001/archinte.168.12.1333. [Erratum, Arch Intern Med 2008;168:1782.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–47. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 36.Texas State Legislature. H.B. No. 1290: An act relating to health benefit plan coverage for bariatric surgery and for certain tests for the early detection of cardiovascular disease. 2009:1–6. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.