Abstract
OBJECTIVE
To assess contraceptive discontinuation, switching, factors associated with method discontinuation, and pregnancy among women initiating hormonal contraceptives.
METHODS
This was a 12-month longitudinal cohort study of adolescent girls and women (n=1,387) aged 15 to 24 years attending public family planning clinics who did not desire pregnancy for at least 1 year and selected to initiate the patch, ring, depot medroxyprogesterone acetate, or pills. Participants completed follow-up assessments at 3, 6, and 12 months after baseline. Life table analysis was used to estimate survival rates for contraceptive continuation. Cox proportional hazards models were used to estimate factors associated with method discontinuation.
RESULTS
The continuation rate (per 100 person-years) at 12 months was low for all methods; however, it was lowest for patch and depot medroxyprogesterone acetate initiators, 10.9 and 12.1 per 100 person years, respectively (P≤.003); continuation among ring initiators was comparable to pill initiators, 29.4 and 32.7 per 100 person-years, respectively (P=.06). Discontinuation was independently associated with method initiated and younger age. The only factors associated with lower risk of discontinuation were greater intent to use the method and being in school or working. The pregnancy rate (per 100 person-years) was highest for patch and ring initiators (30.1 and 30.5) and comparable for pill and depot medroxyprogesterone acetate initiators (16.5 and 16.1; P<.001).
CONCLUSION
The patch and the ring may not be better options than the pill or depot medroxyprogesterone acetate for women at high risk for unintended pregnancy. This study highlights the need for counseling interventions to improve contraceptive continuation, education about longer-acting methods, and developing new contraceptives that women may be more likely to continue.
Despite advances in the types and increasing variety of hormonal contraceptives that are available for adolescent girls and women, the rate of unintended pregnancy remains unacceptably high. Approximately half of all pregnancies in the United States are unintended, and half of those pregnancies end in abortion.1 Unintended pregnancies have consequences and also are becoming increasingly concentrated among minority and socioeconomically disadvantaged women.1
Use of less effective methods, infrequent use, and method discontinuation have an effect on the rate of unintended pregnancies.2-4 Combination oral contraceptive pills remain the most common method of reversible contraception; however, inconsistent use, gaps in use, switching, and discontinuation are common.5,6 Several studies demonstrate that method continuation with depot medroxyprogesterone acetate (depot medroxyprogesterone acetate) is also problematic.7-9 In addition, data reveal racial and ethnic minorities and women of lower socioeconomic status have higher rates of contraceptive failure compared with whites and women of higher socioeconomic status.10,11
Two relatively new methods for women desiring reversible contraceptive options are the transdermal patch (Ortho Evra) and the vaginal ring (Nuvaring), which offer promise of greater satisfaction and compliance; however, there are limited data on patterns of use of these methods in diverse women at risk for unintended pregnancy.12,13 Clinical trials typically do not include adolescents or large numbers of racial and ethnic minorities and low-income women. A postmarketing trial by Creinin et al14 comparing acceptance and continuation among 500 patch and ring users found 92% and 84% of patch users and ring users, respectively, completed 3 months; however, the study population was primarily white and college-educated and the investigators did not examine long-term use. Postmarketing studies assessing acceptability of the patch in adolescents also have been hampered by small sample size and short follow-up periods.15,16
Information on how individual factors, including views of consequences and beliefs about the newer contraceptives, are associated with contraceptive use patterns is also limited.3 Research is needed to help health care providers understand more about women who present to clinics for contraception and guide the development of interventions to improve contraceptive use. We conducted a 12-month, prospective, longitudinal cohort study of adolescents and women presenting to public family planning clinics who were not desiring pregnancy and initiated the transdermal patch, the vaginal ring, or depot medroxyprogesterone acetate, and we compared them to women who initiated pills. We wanted to gain a better understanding using a behavioral theoretical framework of what happens over time when women who present for birth control with varying degrees of motivation to continue contraception and avoid pregnancy select to initiate a range of reversible hormonal contraceptive methods. Our primary goal was to determine whether contraceptive continuation was better for women selecting the relatively newer methods that offer more convenience (the patch and the ring) compared with the pill and to assess how baseline factors that providers can assess before initiating a birth control method are associated with contraceptive discontinuation. We also wanted to examine unintended pregnancy rates in this population by method selected and pattern of use.
MATERIALS AND METHODS
The study was approved by the Committee on Human Subjects at the University of California, San Francisco. All participants provided written informed consent; because minors can consent to contraceptive services in California and because the study posed minimal risk, parental consent for participation for minors was waived. The study was conducted from September 2005 to July 2008 at four Planned Parenthood clinics in the Northern California: Vallejo, Richmond, East Oakland, and Hayward. We enrolled consecutive women who presented for reproductive health care at the study clinics and selected to initiate a hormonal contraceptive after they received standard clinical care from clinic providers. Women were eligible for inclusion in the study if they were aged 15 to 24, not married, could read English or Spanish, were not pregnant (self-report) or were not desiring pregnancy within the next year, and were able to provide written informed consent and comply with study procedures. Women had to have not used the contraceptive method selected in the past (“initiators”); however, they may have used another hormonal contraceptive.
Research staff collected data from enrolled participants via self-administered electronic questionnaires at baseline and at 3, 6, and 12 months after baseline. Questionnaires were pilot-tested to ensure that the instrument was at an appropriate reading level and understood by respondents. The questionnaires, which were available in English and Spanish, were accessed by web link on laptop computers and were administered either at the clinic site or at a location convenient for the participant or by telephone. Study participants received $30 for completing the baseline and 12-month follow-up questionnaires and $20 for completing the 3- and 6-month follow-up questionnaires.
Sociodemographic and reproductive health measures collected at baseline were from previously validated questionnaires and included income, race and ethnicity, education, and employment status.17-20 Reproductive health measures included information on sexual partners, hormonal contraceptive use, and history of pregnancy.
The selection of other baseline study measures was guided by the theory of reasoned action, which posits that the best predictor of a given behavior is intention to engage in the behavior.21 Intention is influenced by two factors: 1) the individual’s attitudes toward taking the action, which reflects one’s beliefs and values about consequences of engaging in the behavior; and 2) their view of social expectations related to the behavior. Participants were asked the question, “how sure are you that you will use the baseline method selected for 1 year?” to gauge intent to use contraception (answer choices: very sure, sure, somewhat sure, and not at all sure).6 To assess pregnancy desire, participants were asked when they wanted to have a child (answer choices: never, in the next year, in the next 1–2 years, in more than 2 years, and do not know) and how they would feel if they got pregnant in the next 3 months (answer choices: very upset, somewhat upset, I would not care, somewhat pleased, very pleased, and do not know).
To understand consequences related to method use, we explored perceptions of side effects of combined hormonal birth control methods using questions developed from information obtained in focus groups conducted in the formative stages of the study.22,23 Study participants were asked to rank how much they agreed or disagreed with 13 negative statements about attributes of combined hormonal contraceptive methods, such as “it is dirty to put the ring in the vagina.” A Likert scale was used (strongly agree, agree, neither agree nor disagree, disagree, strongly disagree) and a negative attributes scale adding scores from the 13 items was developed, with a higher score indicating more negative perceptions of combined hormonal methods. The score had fair internal consistency (Cronbach α=.62). To assess perceptions of social expectations, participants also were asked questions about how their partners and peers felt about their use of various hormonal contraceptive methods and if they thought their parents would be upset if they knew they used birth control.
The follow up questionnaires focused on the main study outcomes: contraceptive use and pregnancies over the 12-month follow-up period. Participants were asked if they started the method selected, if they were using it currently, and whether they used the method continuously (without breaks). If participants discontinued the method, then they were asked how long they used it, the main reason for discontinuation, subsequent methods used (switching), and birth control method used during last sexual encounter. When use of another method was reported, use of any hormonal method or an intrauterine device was considered use of an effective method. Information on pregnancies was collected via self-report at each follow-up, urine pregnancy tests were performed at 6 and 12 months during in-person follow-up visits, and medical record chart review was performed at the study sites at the end of the 12-month follow-up period.
Using data on contraceptive continuation from the 1995 National Survey of Family Growth and clinical trials of the patch and the ring, anticipated continuation rates were 50% for pill users and 60% for patch, ring, and depot medroxyprogesterone acetate. It was estimated that a sample size of 375 pill, patch, ring, and depot medroxyprogesterone acetate initiators would allow us to detect a significant difference in continuation rates at 12 months with a one-tailed test. Calculations were based on survival analysis with comparison of two groups with α of .05, β of 80%, and 20% attrition rate at 1 year.11-13,24 To allow for adequate comparisons, participants initiating any of the four methods were enrolled until a sample of 400 women initiating pills was reached. Enrollment of pill initiators was then discontinued while continuing to enroll women initiating the other three methods.
Women who completed at least one follow-up are included in the analyses; for those lost to follow-up during the study period, data are included up until the point when they were lost to follow-up (ie, censored). To compare women with no follow-up data to women contributing study data, we completed an attrition analysis. We examined characteristics of the study population by contraceptive method selected at baseline comparing the patch, ring, and depot medroxyprogesterone acetate initiators to pill initiators using χ2 statistics for categorical variables and F tests from one-way analysis of variance for continuous variables. We plotted 12-month contraceptive continuation by method with Kaplan-Meier estimates of the probability of discontinuation. Life table analysis was used to estimate survival rates for contraceptive continuation. The log-rank test was used to compare survival rates for different methods. Comparisons of main reasons reported for contraceptive discontinuation by method were performed using χ2 analysis.
To assess factors associated with method discontinuation, we estimated Cox proportional hazards models with contraceptive method and covariates from the baseline data, including sociodemographic characteristics, reproductive history, pregnancy desire, and attitudes toward contraception.25 For the survival analysis, we estimated time to the event (contraceptive discontinuation or first pregnancy). Each woman contributed observation time to the analysis for the period in which she participated. Individuals were censored when lost to follow-up, when the event occurred, or when they exited the study. Unadjusted and adjusted hazards ratios and 95% confidence intervals were estimated. Likelihood ratio tests were used to estimate the final simplest model. Missing values are not included in the analyses. To check the assumptions of the proportional hazards models, we estimated the Schoenfeld residuals.
Contraceptive use was categorized into one of three patterns over the study year: (1) continuation of the method selected at baseline (with or without breaks); (2) discontinuation of the baseline method followed by switching to another effective method; and (3) discontinuation of the baseline method without subsequent use of another effective method. Time to first pregnancy was estimated using survival analysis, and Cox proportional hazards were estimated to compare pregnancy hazards by baseline method selected and contraceptive use pattern. All analyses were conducted using STATA 11 (Stata Corporation, College Station, TX).
RESULTS
During enrollment, 1,605 women were screened and 1,387 women were enrolled; 187 women declined to participate and 31 women did not meet eligibility criteria. The main reason for ineligibility was previous use of the selected method. Follow-up data on contraceptive use, discontinuation, and pregnancies were available for 1,316 women who completed at least one follow-up questionnaire. Follow-up data were available for 1,237 participants at visit 2, 1,256 at visit 3, and 1,208 at visit 4. Attrition analysis on the women lost to follow-up revealed no significant differences from those who contributed follow-up data by contraceptive method selected at baseline and intention to use the method in the next year, as well as important sociodemographic and reproductive health factors, including age, race or ethnicity, low income, previous use of hormonal contraception, and previous birth or abortion.
Almost two thirds (67%) of the participants were adolescents (Table 1). The sample was racially and ethnically diverse, with more than half of participants being Latina or African American. Approximately half (45%) of the women reported living in low-income neighborhoods, and the majority (78%) had no or public insurance. Ring initiators were more likely to be older and to have used hormonal contraception in the past. Patch initiators were significantly more likely to be African American and live in low-income neighborhoods. Pill initiators were less likely to have used hormonal contraception or to have been pregnant. Pill and depot medroxyprogesterone acetate initiators were more likely to report that they were very sure they would continue their method for 1 year than were patch and ring initiators; however, even for these methods, less than half of women were very sure.
Table 1.
Characteristics of Participants by Contraceptive Method Selected at Baseline
| Total | Pill | Patch | Ring | DMPA | P | |
|---|---|---|---|---|---|---|
| Sociodemographics | 1,387 (100.0) | 31.2 | 28.9 | 18.7 | 21.3 | |
| Mean age (y) | 19.2±2.5 | 18.6 | 19.2 | 20.4 | 18.9 | <.001 |
| Race or ethnicity | <.001 | |||||
| White | 152 (11.0) | 12.3 | 7.0 | 11.2 | 14.5 | |
| Latina | 366 (26.4) | 24.8 | 27.2 | 25.9 | 28.1 | |
| African American | 492 (35.5) | 29.2 | 41.1 | 35.1 | 37.3 | |
| Asian or Pacific Islander | 153 (11.0) | 13.9 | 11.1 | 12.4 | 5.8 | |
| Multiracial or other | 223 (16.1) | 19.7 | 13.7 | 15.4 | 14.6 | |
| Low-income neighborhood* | 610 (44.8) | 41.4 | 50.6 | 47.4 | 39.6 | .010 |
| In school or employed (part-time or full-time) | 1,144 (82.5) | 84.9 | 82.0 | 82.2 | 79.7 | .319 |
| Health insurance | <.001 | |||||
| Private insurance | 117 (8.5) | 10.0 | 6.5 | 10.0 | 7.5 | |
| Medical or Family PACT | 625 (45.2) | 35.2 | 50.2 | 47.9 | 50.7 | |
| None | 462 (33.4) | 38.7 | 29.2 | 18.2 | 32.3 | |
| Do not know | 178 (12.9) | 16.1 | 14.0 | 9.6 | 9.5 | |
| Clinic site | <.001 | |||||
| Oakland | 437 (31.5) | 25.9 | 36.7 | 27.4 | 36.3 | |
| Hayward | 344 (24.8) | 26.6 | 19.2 | 20.5 | 33.6 | |
| Vallejo | 158 (11.4) | 11.1 | 10.7 | 14.7 | 9.8 | |
| Richmond | 448 (32.3) | 36.3 | 33.4 | 37.4 | 20.3 | |
| Contraceptive and reproductive history | ||||||
| Currently has a sex partner | 1,142 (82.9) | 85.5 | 79.6 | 84.5 | 82.0 | .129 |
| Previous use of hormonal method | 655 (47.5) | 28.7 | 43.9 | 77.8 | 53.2 | <.001 |
| Previous pregnancy | 679 (49.1) | 33.3 | 52.0 | 59.7 | 59.0 | <.001 |
| Pregnancy desire | ||||||
| Does not want child in next 2 y or ever | 970 (70.7) | 71.7 | 72.3 | 70.0 | 67.7 | .564 |
| Very upset if became pregnant in next 3 mo | 598 (43.6) | 45.2 | 39.9 | 44.7 | 45.2 | .387 |
| Very sure will continue method for 1 y | 580 (42.2) | 48.1 | 36.6 | 34.1 | 48.1 | <.001 |
| Attitudes toward contraception | ||||||
| Endorsed negative attributes of combined hormonal contraception |
706 (53.0) | 44.9 | 54.3 | 50.6 | 65.3 | <.001 |
| Peers against use of hormonal method | 179 (13.0) | 11.7 | 13.6 | 17.4 | 10.2 | .062 |
| Main partner against use of hormonal method† | 188 (13.5) | 14.6 | 13.5 | 15.8 | 10.2 | .219 |
| Parents would be upset if they knew she used contraception |
276 (20.1) | 24.9 | 22.2 | 13.7 | 16.1 | .001 |
DMPA, depot medroxyprogesterone acetate; PACT, Planning, Access, Care, and Treatment.
Data are n (%), %, or mean±standard deviation unless otherwise specified.
Defined as living in a zip code where the percentage of families living below the federal poverty level is greater than the national average.
Asked only of those with partners.
Contraceptive continuation at 12 months (Fig. 1) was low for all methods, Overall, the 12-month continuation rate was 18.5 women per 100 person-years; however, it was significantly lower for patch and depot medroxyprogesterone acetate initiators than pill initiators (10.9 and 12.1 per 100 person-years compared with 32.7 per 100 person-years, respectively; P≤.003). Continuation among ring initiators was comparable to pill initiators (29.4 compared with 32.7 per 100 person-years; P=.06). The majority of patch and depot medroxyprogesterone acetate initiators discontinued their methods by 4 months. There was a slower drop-off rate for pill and ring initiators, who had a median time of discontinuation of 5 months. Among women who reported continuation of the baseline method, 46.5% reported taking breaks from their method.
Fig. 1.
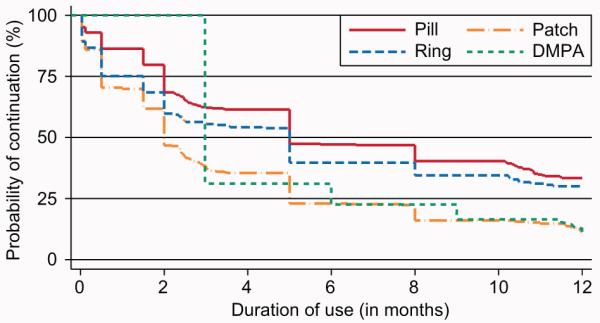
Kaplan-Meier curve for continuation of the method selected at baseline. Pill compared with patch, P<.001; pill compared with ring, P=.06; pill compared with depot medroxyprogesterone acetate, P=.003.
Results from multivariable model of discontinuation (Table 2) show that method selected at baseline was significantly associated with discontinuation, with patch initiators being almost twice as likely as pill initiators to discontinue. Depot medroxyprogesterone acetate initiators were also significantly more likely than pill initiators to discontinue their method. Although several factors were associated with discontinuation in the unadjusted model, only two factors were independently associated with discontinuation in the adjusted model. In addition to method selected, younger age was significantly associated with method discontinuation in the adjusted model. Being very sure about continuing a method for 1 year and being in school or working were the only factors that were associated with lower risk of discontinuation.
Table 2.
Unadjusted and Adjusted Hazard Models Predicting Risk of Discontinuation (n=1,267*)
| Unadjusted Hazard Ratio (95% CI) |
Bivariate P |
Adjusted Hazard Ratio (95% CI) |
Multivariate P† |
|
|---|---|---|---|---|
| Baseline method | ||||
| Pill | 1 (reference) | 1 (reference) | ||
| Patch | 1.99 (1.68–2.34) | <.001 | 1.90 (1.59–2.27) | <.001 |
| Ring | 1.20 (.99–1.46) | .068 | 1.18 (.94–1.46) | .146 |
| DMPA | 1.35 (1.13–1.61) | .001 | 1.24 (1.03–1.51) | .025 |
| Sociodemographic characteristics | ||||
| Age (y) | 0.98 (.96–1.01) | .162 | 0.96 (.93–0.99) | .008 |
| Race or ethnicity | ||||
| White | 1 (reference) | 1 (reference) | ||
| Latina | 1.28 (1.02–1.62) | .036 | 1.10 (.86–1.41) | .455 |
| African American | 1.43 (1.14–1.79) | .002 | 1.22 (.95–1.55) | .114 |
| Asian or Pacific Islander | 1.16 (.88–1.53) | .295 | 1.10 (.82–1.47) | .521 |
| Multiracial or other | 1.27 (.99–1.64) | .062 | 1.22 (.93–1.58) | .147 |
| Neighborhood income‡ | 2.48 (1.04–5.94) | .040 | 0.89 (.31–2.54) | .825 |
| In school or employed | 0.85 (.72–1.00) | .046 | 0.83 (.69–0.98) | .032 |
| Clinic site | ||||
| Oakland | 1 (reference) | 1 (reference) | ||
| Hayward | 0.84 (.71–0.99) | .043 | 0.96 (.78–1.18) | .717 |
| Vallejo | 0.86 (.69–1.06) | .156 | 0.96 (.75–1.22) | .726 |
| Richmond | 0.81 (.69–0.94) | .007 | 0.89 (.75–1.06) | .202 |
| Currently has a sex partner | 0.94 (.79–1.11) | .460 | 1.05 (.88–1.27) | .582 |
| Previous hormonal method use | 0.99 (.87–1.12) | .879 | 0.98 (.86–1.13) | .816 |
| Previous pregnancy | 1.18 (1.04–1.34) | .010 | 1.10 (.95–1.28) | .185 |
| Pregnancy desire | ||||
| Does not want a child in next 2 y or ever | 0.87 (.76–0.99) | .039 | 0.94 (.82–1.09) | .409 |
| Very sure will continue method for 1 y | 0.70 (.61–0.80) | <.001 | 0.73 (.64–0.83) | <.001 |
| Attitudes toward contraception | ||||
| Endorsed negative attributes of combined hormonal contraception |
1.16 (1.02–1.32) | .020 | 1.18 (1.00–1.39) | .055 |
| Peers very against use of hormonal method | 1.01 (.84–1.21) | .940 | 0.90 (.73–1.10) | .307 |
| Partner very against use of hormonal method | 1.20 (1.01–1.44) | .040 | 1.20 (.99–1.47) | .066 |
| Parents would be upset if knew she used contraception | 0.92 (.78–1.07) | .277 | 0.95 (.79–1.13) | .544 |
CI, confidence interval; DMPA, depot medroxyprogesterone acetate.
Excludes 49 women who had missing information on independent variables.
Multivariable model log likelihood ratio c2 (22) = 125.4.
Percentage of families in resident zip code below federal poverty level (continuous measure).
The log likelihood ratio χ2 was 125.4 (22 degrees of freedom). Reduced nested models with fewer degrees of freedom were more significant, but we retained variables from the theoretical framework in the analysis, albeit insignificant, to show the relative importance of the factors tested. A test of the Schoenfeld residuals confirmed the visual examination of the survival curves in Figure 1 that depot medroxyprogesterone acetate has a different shape over time than the other methods; depot medroxyprogesterone acetate can only be discontinued when a re-injection visit is missed, unlike the other methods. We estimated the model, stratified by contraceptive method, and we also estimated the model without depot medroxyprogesterone acetate. In the stratified Cox regression by method the results were consistent, with a lower intent-to-use method as the most significant predictor of subsequent discontinuation. The only difference in the results was that age was no longer significant. However, in the model without depot medroxyprogesterone acetate, age was highly significant. Method had the strongest association with discontinuation, followed by intent-to-use method and being in school or working. In the model without depot medroxyprogesterone acetate, negative attitudes about combined hormonal contraceptives became significantly associated with discontinuation, as did African-American race.
The most common reason for discontinuation was side effects. Women who discontinued depot medroxyprogesterone acetate were most likely to report side effects as the main reason for discontinuation (Table 3). Although women who discontinued depot medroxyprogesterone acetate were the least likely to report discontinuation because of difficulty using the method, and they were the most likely to report discontinuing because of access problems. More than two thirds (74%) of participants who discontinued the baseline method switched to another effective method (Table 4).
Table 3.
Main Reason for Method Discontinuation by Method Selected
| Pill (n=259) | Patch (n=322) | Ring (n=163) | DMPA (n=247) | Total (n=991) | |
|---|---|---|---|---|---|
| Side effects | 33 | 34 | 26 | 46 | 36 |
| Access, supply, or cost barriers | 9 | 8 | 10 | 17 | 11 |
| Not sexually active, perceived need | 15 | 8 | 11 | 10 | 11 |
| Difficulties with use | 20 | 9 | 14 | 1 | 11 |
| Pregnancy-related | 5 | 9 | 8 | 3 | 6 |
| Medical reasons or health concerns | 4 | 6 | 6 | 3 | 4 |
| Wanted to become pregnant | 2 | 1 | 2 | 2 | 2 |
| Other or unknown | 14 | 25 | 25 | 20 | 21 |
DMPA, depot medroxyprogesterone acetate; PACT, Planning, Access, Care, and Treatment.
Data are percentage of women discontinuing method.
Pearson c2 (18)= 97.9.
P≤.001.
Table 4.
Pregnancies (Per 100 Person-Years) by Method Selected and Contraceptive Use Pattern
| Contraceptive Use Pattern |
||||
|---|---|---|---|---|
| Method Selected at Baseline |
Continuation of the Method Selected* (n=325) |
Discontinuation of the Method Selected With Switch to Another Effective Method (n=738) |
Discontinuation of the Method Selected Without Subsequent Use of Another Effective Method (n=253) |
Pregnancy Rate by Method (P<.001) |
| Pill (n=387) | 4.4 | 19.2 | 34.5 | 16.5 |
| Patch (n=370) | 19.6 | 28.8 | 39.1 | 30.1 |
| Ring (n=233) | 12.4 | 34.3 | 52.7 | 30.5 |
| DMPA (n = 279) | 5.7 | 17.1 | 20.4 | 16.1 |
| Pregnancy rate by use pattern (P<.001) |
9.1 | 23.9 | 37.2 | Overall 22.9 |
DMPA, depot medroxyprogesterone acetate.
Of the 144 women in this category, 46.5% reported taking one or more breaks (pill, 46.5%; patch, 56.9%; ring, 51.4%; DMPA, 19.4%; P=.003).
Overall, 22.9 women per 100 person-years became pregnant (Table 4). Pregnancy rates were associated with method selected and pattern of use over the study period. The highest pregnancy rates were among patch initiators and ring initiators. Women switching to another effective method during the study had far higher pregnancy rates than those who continued the same method (P<.001; Table 4). Among women who continued their method, those who reported taking breaks had a pregnancy rate of 11.9 per 100 person-years compared with a rate of 6.1 per 100 person-years for those who did not report breaks, although this difference was not significant (P=.08).
DISCUSSION
In our cohort of adolescents and women at risk for unintended pregnancy who initiated a hormonal contraceptive, very few were still using the method after 1 year. Women initiating the newer methods and those who switched to another hormonal method during the year were also more likely to experience a pregnancy. Method selected was a significant predictor of discontinuation. Despite expectations that the relatively newer combined hormonal contraceptive methods, the patch and the ring, would improve contraceptive compliance, we found that ring initiators were no more likely to continue the method than pill initiators, whose continuation was also low. Patch initiators were almost twice as likely to discontinue as pill initiators. Method continuation in general is better with longer-acting methods such as implants and intrauterine devices that do not rely on user behavior.26
Consistent with our conceptual model, women who were more intent on using the method for 1 year were more likely to continue their method. The theory of reasoned action asserts that contraceptive behavior, like any other human behavior, is planned, that is, if a person intends to do a behavior, then that person is likely to do it. As predicted by theory, intention was guided by attitudes toward contraception, pregnancy desire, and partner’s attitudes. In the bivariate analyses, these factors from the model were significantly associated with discontinuation.21,27 Only intention, however, remained significant in the adjusted model, suggesting its importance in predicting future contraceptive behavior. Thus, it is clear that use of a prospective framework is critical for understanding subsequent contraceptive behavior in young women. Health care providers may be able to utilize relatively simple questions about contraceptive use intention to identify women at risk for contraceptive discontinuation. Our understanding of what we can do in the clinical setting for women who are not very sure or have low intentions to use contraception is extremely limited.28 Research is needed to determine how to accurately assess contraceptive intent in the clinical setting and how to effect it through counseling interventions.
Race, ethnicity, and socioeconomic status were not independently associated with discontinuation; however, younger women were more likely to discontinue their method. Adolescents’ limited cognitive and abstracting abilities may make it difficult for them to plan and commit to behaviors. Women who were in school or working were less likely to discontinue their method, supporting the notion that women have to have a reason not to get pregnant and want to use contraception to be successful. Interventions to improve contraceptive use need to address context and how contraception and pregnancy fit into the lives of young women.
Although side effects were the most common reason reported for method discontinuation, only approximately one third of women reported this as the main reason for discontinuation. In a trial of “quick start” pills, Westhoff et al29 found that women who reported side effects were more likely to discontinue pills by 6 months; however, these women discontinued whether they believed the side effects were caused by the pills. Our findings are consistent with this research and suggest that factors such as side effects, which occur over time, may not be as important for continuation as intention to use the method. Further analyses of our data will explore longitudinal factors, like side effects, and how they may affect women differently.
Even though we used multiple regression analyses, it is possible that the lower continuation rate for patch and depot medroxyprogesterone acetate initiators and the higher pregnancy rate for ring and patch initiators in our study is attributable to unmeasured selection bias. Lack of randomization is a weakness of the study and would have helped reduce such bias. However, the observational design allowed for reflection on the current standard of care in family planning clinics, which is to provide women with information about contraceptive options and to help them to make informed decisions. Women who were destined to have poor compliance may have been less likely to select to initiate the pill, or providers may have been more likely to recommend other methods to them. Patch, ring, and depot medroxyprogesterone acetate initiators were more likely to have used other hormonal methods in the past and patch and ring initiators were more likely to report being less sure about using the method for 1 year. The most likely reason for the comparable pregnancy rate for depot medroxyprogesterone acetate and pill initiators despite the higher discontinuation rate for depot medroxyprogesterone acetate initiators is the delay of return to fertility with depot medroxyprogesterone acetate use; however, it is also possible that this is attributable to selection bias.26 Whether our findings are a result of selection bias, they suggest that among these highly effective hormonal methods the patch and the ring are not better options than the pill or depot medroxyprogesterone acetate for women at high risk.
This study examined racially and ethnically diverse women from public family planning clinics in Northern California. These women had a source of care and essentially no cost barriers because of the availability of contraceptives at low or no cost for low-income women through the public funding (Family PACT [Planning, Access, Care, and Treatment] and Title X).30 Whereas this population represents an important demographic, our study is also limited in that findings may not be generalizable to other women initiating contraceptives. The 1-year pregnancy rates observed in this study were for women who initiated a method, whether they continued the method. Our findings of pregnancy rates that are higher than “typical use” failure rates in the literature are consistent with other studies of young, minority, and low-income women.31 This “real-life” view of what happens to young women initiating highly effective hormonal contraceptive methods, including relatively newer methods such as the patch and the ring, highlights the need for counseling interventions to improve contraceptive continuation, education about longer-acting methods, and the development of new contraceptive methods that women may be more likely to continue.
Acknowledgments
Supported by Eunice Kennedy Shriver National Institute of Child Health and Human Development Grant R01 HD045480.
Footnotes
Results do not necessarily represent the views of Planned Parenthood Federation of America, Inc.
Financial Disclosure
Dr. Raine and Dr. Harper currently receive grant support from Teva Pharmaceutical Industries for research work on Plan B and Plan B One-Step emergency contraception. Dr. Raine has received honoraria from Merck as an Implanon insertion trainer (ended July 2009). The other authors did not report any potential conflicts of interest.
REFERENCES
- 1.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38:90–6. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- 2.Ranjit N, Bankole A, Darroch JE, Singh S. Contraceptive failure in the first two years of use: differences across socioeconomic subgroups. Fam Plann Perspect. 2001;33:19–27. [PubMed] [Google Scholar]
- 3.Frost JJ, Singh S, Finer LB. U.S. women’s one-year contraceptive-use patterns, 2004. Perspect Sex Reprod Health. 2007:38–55. doi: 10.1363/3904807. [DOI] [PubMed] [Google Scholar]
- 4.Glei DA. Measuring contraceptive use patterns among teenage and adult women. Fam Plann Perspect. 1999;31:73–80. [PubMed] [Google Scholar]
- 5.Rosenberg MJ, Burnhill MS, Waugh MS, Grimes DA, Hillard PJ. Compliance and oral contraceptives: a review. Contraception. 1995;52:137–41. doi: 10.1016/0010-7824(95)00161-3. [DOI] [PubMed] [Google Scholar]
- 6.Westhoff C, Heartwell S, Edwards S, Zieman M, Cushman L, Robilotto C, et al. Initiation of oral contraception using quick start compared with a conventional start: a randomized controlled trial. Obstet Gynecol. 2007;109:1270–6. doi: 10.1097/01.AOG.0000264550.41242.f2. [DOI] [PubMed] [Google Scholar]
- 7.Sangi-Haghpeykar H, Poindexter AN, 3rd, Bateman L, Ditmore JR. Experiences of injectable contraceptive users in an urban setting. Obstet Gynecol. 1996;88:227–33. doi: 10.1016/0029-7844(96)00194-9. [DOI] [PubMed] [Google Scholar]
- 8.Westfall JM, Main DS, Barnard L. Continuation rates among injectable contraceptive users. Fam Plann Perspect. 1996;28:275–7. [PubMed] [Google Scholar]
- 9.Polaneczky M, Liblanc M. Long-term depot medroxyprogesterone acetate (Depo-Provera) use in inner-city adolescents. J Adolesc Health. 1998;23:81–8. doi: 10.1016/s1054-139x(98)00014-7. [DOI] [PubMed] [Google Scholar]
- 10.Mosher WD, Martinez GM, Chandra A, Abma JC, Willson SJ. Use of contraception and use of family planning services in the United States: 1982–2002. Adv Data. 2004;350:1–36. [PubMed] [Google Scholar]
- 11.Trussell J, Vaughan B. Contraceptive failure, method related-discontinuation and resumption of use: Results from the 1995 National Survey of Family Growth. Fam Plann Perspect. 1999;31:64–72. [PubMed] [Google Scholar]
- 12.Archer DF, Bigrigg A, Smallwood GH, Shangold GA, Creasy GW, Fisher AC. Assessment of compliance with a weekly contraceptive patch (Ortho Evra/Evra) among North American women. Fertil Steril. 2002;77:S27–31. doi: 10.1016/s0015-0282(01)03263-0. [DOI] [PubMed] [Google Scholar]
- 13.Dieben TO, Roumen FJ, Apter D. Efficacy, cycle control, and user acceptability of a novel combined contraceptive vaginal ring. Obstet Gynecol. 2002;100:585–93. doi: 10.1016/s0029-7844(02)02124-5. [DOI] [PubMed] [Google Scholar]
- 14.Creinin MD, Meyn LA, Borgatta L, Barnhart K, Jensen J, Burke AE, et al. Multicenter comparison of the contraceptive ring and patch: a randomized controlled trial. Obstet Gynecol. 2008;111:267–77. doi: 10.1097/01.AOG.0000298338.58511.d1. [DOI] [PubMed] [Google Scholar]
- 15.Rubinstein ML, Halpern-Felsher BL, Irwin CE., Jr. An evaluation of the use of the transdermal contraceptive patch in adolescents. J Adolesc Health. 2004;34:395–401. doi: 10.1016/j.jadohealth.2003.08.017. [DOI] [PubMed] [Google Scholar]
- 16.Harel Z, Riggs S, Vaz R, Flanagan P, Dunn K, Harel D. Adolescents’ experience with the combined estrogen and progestin transdermal contraceptive method Ortho Evra. Pediatr Adolesc Gynecol. 2005;18:85–90. doi: 10.1016/j.jpag.2004.11.016. [DOI] [PubMed] [Google Scholar]
- 17.Groves RM, Benson G, Mosher WD, Rosenbaum J, Granda P, Axinn W, et al. Plan and operation of cycle 6 of the National Survey of Family Growth. Vital Health Stat. 2005;1:1–86. [PubMed] [Google Scholar]
- 18.California health Interview Surveys. Available at: http://www.chis.ucla.edu/questionnaires.html Retrieved January 6, 2010.
- 19.Behavioral Risk Factor Surveillance system questionnaires. Available at: http://www.cdc.gov/brfss/questionnaires/english.htm Retrieved January 6, 2010.
- 20.Novák A, de la Loge C, Abetz L. Development and validation of an acceptability and satisfaction questionnaire for a contraceptive vaginal ring, NuvaRing. Pharmacoeconomics. 2004;22:245–56. doi: 10.2165/00019053-200422040-00003. [DOI] [PubMed] [Google Scholar]
- 21.Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. Prentice-Hall; Englewood Cliffs (NJ): 1980. [Google Scholar]
- 22.Raine TR, Gard J, Boyer CB, Haider S, Brown BA, Ramirez Hernandez FA, et al. Contraceptive decision-making in sexual relationships: young men’s experiences, attitudes, and values. Culture Health Sex. 2010;12:373–86. doi: 10.1080/13691050903524769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Raine TR, Epstein LB, Harper CC, Brown BA, Boyer CB. Attitudes toward the vaginal ring and transdermal patch among adolescents and young women. J Adol Health. 2009;45:262–7. doi: 10.1016/j.jadohealth.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Collett D. Modelling survival data in medical research. Chapman & Hall; London (UK): 1994. [Google Scholar]
- 25.Cox DR. Regression models and life tables. R Stat Soc. 1972;34:187–220. [Google Scholar]
- 26.Speroff L, Darney PD, editors. A clinical guide for contraception. 4th ed. Lippincott Williams & Wilkins; Philadelphia (PA): 2005. [Google Scholar]
- 27.Moore PJ, Adler NE, Kegeles SM. Adolescents and the contraceptive pill: the impact of beliefs on intentions and use. Obstet Gynecol. 1996;88:48S–56S. doi: 10.1016/0029-7844(96)00244-x. [DOI] [PubMed] [Google Scholar]
- 28.Kirby D. The impact of programs to increase contraceptive use among adult women: a review of experimental and quasi-experimental studies. Perspect Sex Reprod Health. 2008;40:34–41. doi: 10.1363/4003408. [DOI] [PubMed] [Google Scholar]
- 29.Westhoff C, Heartwell S, Edwards S, Zieman M, Stuart G, Cwiak C, et al. Oral contraceptive discontinuation: do side-effects matter? Am J Obstet Gynecol. 2007;196(412):e1–7. doi: 10.1016/j.ajog.2006.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.FamilyPACT web site. Available at: http://familypact.org/en/home.aspx Retrieved January 6, 2010.
- 31.Kost K, Singh S, Vaughan B, Trussell J, Bankole A. Estimates of contraceptive failure from the 2002 National Survey of Family Growth. Contraception. 2008;77:10–21. doi: 10.1016/j.contraception.2007.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]


