Abstract
We hypothesized that spinal manipulation (SM) would reduce strength imbalances between legs. Using an un-blinded randomized design, 28 males and 21 females (54 ± 19y) with at least a 15% difference in isometric strength between legs for hip flexion, extension, abduction, or knee flexion were randomized to treatment or placebo (mock spinal manipulation). Strength of the stronger and weaker legs for hip flexion, extension, abduction, and/or knee flexion was assessed before and after the intervention. SM reduced the relative strength difference between legs for knee flexion (mean ± SD 57 ± 53 to 5 ± 14%) and hip flexion (24 ± 12 to 11 ± 15%) compared to placebo (34 ± 29 to 24 ± 36%, and 20 ± 18 to 22 ± 26%, respectively) (p = 0.05). SM also improved strength in the weak leg for hip abduction (104 ± 43 to 116 ± 43 Nm) compared to placebo (84 ± 24 to 85 ± 31 Nm) (p = 0.03). This study suggests that spinal manipulation may reduce imbalances in strength between legs for knee and hip flexion.
Keywords: hip, hamstring, flexion, extension, abduction
Abstract
Notre hypothèse est que la manipulation vertébrale (MV) réduirait le déséquilibre entre les jambes. À l’aide d’un essai aléatoire ouvert, 28 hommes et 21 femmes (54 ± 19a) ayant une différence de force isométrique d’au moins 15 % entre les jambes pour la flexion, l’étirement et l’abduction de la hanche, ou la flexion du genou, ont subi de façon aléatoire un traitement réel ou un traitement placebo (manipulation vertébrale simulée). On a alors évalué la force des jambes plus fortes et plus faibles en fonction de la flexion, l’étirement et l’abduction de la hanche, ou la flexion du genou, avant et après l’intervention. La MV a réduit la différence de force entre les jambes quant à la flexion du genou (moyenne ± ET 57 ± 53 à 5 ± 14 %) et la flexion de la hanche (24 ± 12 à 11 ± 15 %) par rapport au traitement placebo (34 ± 29 à 24 ± 36 %, et 20 ± 18 à 22 ± 26 %, respectivement) (p = 0,05). La MV a également amélioré la force de la jambe faible quant à l’abduction de la hanche (104 ± 43 à 116 ± 43 Nm) par rapport au traitement placebo (84 ± 24 à 85 ± 31 Nm) (p = 0,03). Cette étude suggère que la manipulation vertébrale peut réduire le déséquilibre de la force entre les jambes quant à la flexion du genou et de la hanche.
MOTS CLÉS : hanche, tendon du jarret, flexion, étirement, abduction
Introduction
Musculoskeletal injuries may be partly related to strength imbalances between limbs. Strength imbalances between legs may affect performance of activities and result in increased chance of injury occurrence.1–8 Contra-lateral imbalances in strength of hip flexors, hip extensors, and knee flexors in asymptomatic subjects predict future lower extremity injuries such as hamstring strains or single leg overuse injuries1,3,4,6,8 while contra-lateral differences between hip extensors strength in asymptomatic subjects predicts future lower back pain.9 Contra-lateral strength differences have also been observed in injured athletes2,5 or athletes who have a past history of injury.7 In contrast, there are a number of studies indicating no relationship between strength imbalance and injury occurrence.10–12 The objective of this study was to determine whether a single chiropractic spinal manipulation (SM) could improve strength imbalances between legs.
Strength is influenced by both muscle mass and the ability of the nervous system to recruit muscle.13 Unilateral muscle weakness and strength imbalances between the legs may therefore be caused by neural deficits. It has been suggested that spinal manipulation may overcome neural deficits by a number of mechanisms including reduced nerve impingement, altered discharge from muscle spindles, Golgi tendon organs, mechanoreceptors and nociceptors, altered sensory processing in the spinal cord (allowing increased pain tolerance), and altered skeletal muscle reflexes.14 These changes may alter afferent feedback to the spinal cord to cause an increase in motor neuron excitability. Spinal manipulation on one side of the body can reduce inhibition of limb musculature on the same side of the body. For example, spinal manipulation of the sacroiliac joint on the ipsilateral side of an injured knee resulted in reduced motor unit inhibition to the knee extensors of the injured limb, as measured by the interpolated twitch technique.15,16 Manipulation of the lumbar spine also increases motor neuron excitability as measured by transcranial magnetic stimulation.17 Spinal manipulation has a greater effect on the weaker limb – the removal of motor unit inhibition occurred to a greater extent in an injured than non-injured limb.15,16 We therefore hypothesized that spinal manipulation of the lumbar spine would increase strength of the weaker limb; and that this would decrease the imbalance in strength in subjects with an imbalance in strength between legs.
Methods
The study was approved by our university’s ethics review board. Subjects were volunteers from the general community who responded to advertisements posted around a university campus, and at chiropractic clinics. Subjects who responded to the advertisement were contacted initially by a research assistant who explained the nature and purpose of the study. If subjects were still interested in participating an initial appointment was made with the research assistant. At the initial appointment the procedures were fully explained, and subjects gave their informed consent to participate in the study. They then filled out a physical activity readiness questionnaire (PAR-Q). An initial measurement of strength deficits between lower limbs was then performed using an isokinetic dynamometer (Biodex System 3, Biodex Medical Systems Inc., Shirley NY) set in isometric mode. Assessment of isometric hip abduction, hip flexion, hip extension, and knee flexion strength has been described in detail previously.18–20 Three isometric contractions of 5 seconds were performed for each movement with a 30 second rest period between contractions. The highest peak torque obtained was recorded in newton meters (Nm). Knee flexion was tested with the participant in a seated position with the hips at 90° and the knee flexed at 30° (where 0° indicates full extension). Stabilizing straps were applied diagonally across the chest, waist, and just above the knee on the leg not being tested. The dynamometer attachment was adjusted so the pad was placed just proximal to the lateral malleoli of the leg being tested and the knee joint was in line with the axis of rotation of the dynamometer. All hip movements were performed from a standing position, with the hip joint in line with the dynamometer axis of rotation. Participants placed their hands on the machine at waist level for balance and in order to stabilize the standing position. The dynamometer attachment was adjusted so the pad was placed three finger widths above the lateral joint line of the knee for hip abduction, flexion, and extension. Participants were asked to keep their foot just off the ground with knee slightly flexed for abduction and extension. Hip abduction was performed with the leg at an angle of 10° of abduction. For hip extension the contraction was performed from 0° or as close as their hip range would allow. Hip flexion was performed with the leg set at 80° of flexion. All hip joint angles were referenced from thigh to vertical. All measurements were corrected for the effects of gravity on the leg and the dynamometer’s resistance pad. Reproducibility of these strength tests was assessed using the initial test results on day 1 and the first test on the treatment day one week later (i.e. before SM or placebo treatment; i.e. mock SM). Intra-class correlation coefficients for hip abduction, hip flexion, hip extension, and knee flexion strength were 0.91, 0.80, 0.88, and 0.92, respectively.
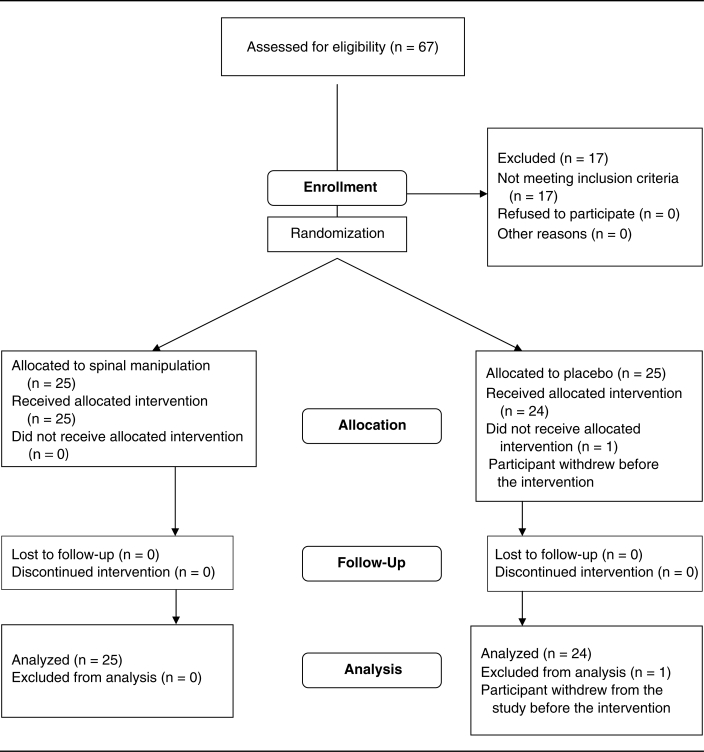
Subjects were considered eligible for the study if they had at least a 15% difference in strength between their legs for hip extension, hip flexion, hip abduction, or knee flexion at the initial testing session. This criterion has previously predicted lower extremity injuries.1 Eligible subjects were invited back to our laboratory at least one week later for an additional session where they were stratified by sex, and randomized to receive either a SM or placebo (i.e. mock adjustment). Randomization was done by a computerized random-number generator and group allocation for each subject was concealed in a sealed envelope and held by an individual who was not involved in any other aspect of the study. Subjects then performed the strength test(s), for which they had greater than or equal to 15% differences between legs on the initial testing day, before and after they received SM or placebo (mock SM). The SM or placebo intervention was given immediately after the strength tests. These strength tests took between 5 to 30 minutes depending on the number of strength tests (i.e. subjects were given 1–4 strength tests depending on which tests they had a 15% or greater difference between their limbs a week earlier). After the intervention was completed, strength tests were repeated. If more than one strength test was done, the order of the tests was randomized before the intervention and the same order of testing was followed after the intervention. At least a 3-minute rest was given between strength tests. Sixty-seven subjects were initially evaluated and 50 met the inclusion criteria. One subject from the placebo (mock SM) group withdrew for personal reasons. The flow of participants through the study is summarized in Figure 1.
Figure 1.
Flow of participants through the study
Subjects and investigators performing the strength measurements were blinded to the treatment groups, while the chiropractor performing the treatment was blinded to the strength results throughout the study.
All spinal manipulations or placebo (mock spinal manipulation) treatment were performed by the same chiropractor. The theoretical rationale for the manipulation was to influence the nerve root that goes to the weak muscle group by delivery of a high velocity, low amplitude thrust to the appropriate area.21 Treatments were as follows:
Left Hip Flexors Weakness Treatment: Hip flexors are mainly innervated by L2–3 spinal nerves.22 If the left hip flexors were weak, this suggested the left L2–3 nerve roots have the neurological deficit. The patients lay on their right side, with the superior leg bent. The lumbar spine was placed into right rotation. The chiropractor’s left hand held back the patient’s left shoulder, and the chiropractor’s right hand contacted the left L3 transverse process. A pre-load torque was applied to the spine through the patient’s shoulder and pelvis and then a high-velocity low amplitude thrust was given at the end range of motion, directed at the level of the L3 transverse process.
Right Hip Flexors Weakness Treatment: The patient received the same treatment as above except on the opposite side.
Left Leg Abduction Weakness Treatment: Abductors are mainly innervated by the L4 spinal nerve.22 If the left leg was weak in abduction this suggested a neurological deficit at the left L4 nerve root. The same manipulative procedure described above was done except the segmental contract point was the left L5 transverse process.
Right Leg Abduction Weakness Treatment: The patient received the same treatment as above except on the opposite side.
Left Hip Extension Weakness Treatment: The major hip extensor [gluteus maximus] is mainly innervated by S1 and S2 spinal nerves.22 If the left hip extensors were weak this suggested a neurological deficit to the S1 nerve root. The same manipulative procedure described above was done except the segmental contact point was the upper left iliac crest.23 With the iliac crest contact one can slightly rotate the ilium on the sacrum to influence the S1 nerve root.
Right Hip Extension Weakness: The patient received the same treatment as above except on the opposite side.
Left Knee Flexion Weakness Treatment: Knee flexors are mainly innervated by L5 spinal nerves.22 If the left knee flexors were weak, this suggested that L5 nerve root on the left side had a neurological deficit. The patients lay on their left side. The lumbar spine was placed into left rotation. The chiropractor’s right hand held the patient’s right shoulder back, and the chiropractor’s left hand contacted the patient’s mid right ilium. A pre-load torque was applied and then a high-velocity low amplitude thrust was given at the end range of motion, rotating the sacrum on the L5 vertebra.
Right Knee Flexion Weakness Treatment: The patient received the same treatment as above except on the opposite side.
All lumbar adjustments were “resisted” adjustments as described by Bergman and Peterson.24 Participants who had more than one strength deficit on initial testing received multiple spinal manipulations (i.e. one for each deficit). There were cavitations during these manipulations. Mock spinal manipulation was done according to the methods of Roy et al.25 For the mock treatment, participants were placed in the exact same position as the SM group. The contact of the hands were the same as above and the patient’s lumbar spine was taken in rotation to the end range of motion and held for three seconds (to match the physical contact time given to the SM group) but there was no high-velocity low amplitude thrust given. There were no cavitations with the mock adjustments.
As a test of our blinding, subjects were asked whether they thought they received the actual SM treatment, the mock placebo treatment, or did not know which treatment they received. This was done by telephone by a research assistant after the intervention.
Statistics
Subjects performed only the strength test(s) for which they had greater than 15% differences between legs on the initial testing day, before and after they received SM or placebo (mock SM). Subjects therefore were tested for between one to four movements (i.e. hip abduction, hip flexion, hip extension, and/or knee flexion) on the day of the intervention. The absolute strength difference between legs was calculated as the strong leg minus the weak leg. To calculate the relative (percent) strength differences between limbs (i.e. to determine how much stronger the strong limb was relative to the weak limb) we subtracted the strength of the weaker limb from the strength of the stronger limb, divided this by the strength of the weaker limb, and multiplied by 100. This was done for comparison to the literature where percent differences of 15% or greater, as calculated by this manner, was determined to predict future injury.1 A Shapiro-Wilk’s test was done on each data set to determine normality. A Mann-Whitney U test (for data that was not normally distributed) or a one-way ANOVA (for normally distributed data) was used to determine differences between the spinal manipulation group and the placebo (mock spinal manipulation) group for changes in the absolute and relative strength differences between legs for each functional movement. For the strong and weak leg for each movement we also performed either a Mann-Whitney U test or one-way ANOVA (depending on whether the data were normally distributed) to determine if the change scores were different between the spinal manipulation and placebo (mock spinal manipulation) groups. The significance level was set at p ≤ 0.05. All data are presented as mean (SD). All data were analyzed using Statistica 6.0 (Stat Soft, Chicago, IL) by PDC.
Results
Baseline data are presented in Table 1. There were no adverse events reported that were related to the treatment. Overall, 42 spinal manipulations were performed (11 for knee flexors imbalance, 10 for hip flexors imbalance, 11 for hip extensors imbalance, and 10 for hip abductors imbalance), and 41 mock (placebo) adjustments were performed (15 for knee flexors imbalance, 11 for hip flexors imbalance, 9 for hip extensors imbalance, and 6 for hip abductors imbalance). Sixty-seven percent of subjects correctly identified which group they were in, while 33% either guessed the incorrect group or stated that they did not know which treatment they received.
Table 1.
Baseline characteristics of the treatment groups
| Spinal Manipulation (15 males, 10 females) | Placebo (mock treatment) (13 males, 11 females) | |
|---|---|---|
| Age (y) | 54.7 (18.7) | 52.7 (20.0) |
| Height (cm) | 171 (9) | 171 (11) |
| Weight (kg) | 78.4 (14.8) | 80.8 (17.7) |
All values are means (SD)
Strength Differences
In general, the participants reproduced the strength difference between limbs of 15% or greater between the first and second visits. The number of participants who had strength differences of at least 15% on both visits corresponded to 22/26, 17/21, 14/20, and 9/16 individuals for knee flexion, hip flexion, hip extension, and hip abduction, respectively. Participants who did not have a strength difference of at least 15% on the second visit were still included in the analyses.
There was a significant decrease in the relative strength difference between limbs during knee and hip flexion in the SM compared to the placebo (mock SM) group (p = 0.05; Table 2). The change in relative strength difference between limbs for hip extension and abduction, and the change in absolute strength differences between limbs for all movements was not different between groups (Table 2). When comparing changes in weak and strong limb strength, spinal manipulation increased weak limb strength during hip abduction compared to the placebo (mock spinal manipulation) (p = 0.03; Table 3) with no other differences between groups.
Table 2.
Mean (SD) absolute and relative strength differences between weak and strong legs for individual movements for spinal manipulation and placebo (mock spinal manipulation) groups
| Absolute strength difference (Nm) before the intervention | Absolute strength difference (Nm) after the intervention | Relative strength difference (%) before the intervention | Relative strength difference (%) after the intervention | |
|---|---|---|---|---|
| Knee Flexors | ||||
| Spinal manipulation (n = 11) | 20 (14) | 4 (8) | 57 (53) | 5 (14)* |
| Placebo (n = 15) | 15 (10) | 9 (15) | 34 (29) | 24 (36) |
| Hip flexors | ||||
| Spinal manipulation (n = 10) | 28 (15) | 16 (22) | 24 (12) | 11 (15)* |
| Placebo (n = 11) | 23 (16) | 26 (33) | 20 (18) | 22 (26) |
| Hip extensors | ||||
| Spinal manipulation (n = 11) | 19 (10) | 14 (13) | 22 (15) | 13 (13) |
| Placebo (n = 9) | 24 (19) | 17 (17) | 22 (16) | 15 (19) |
| Hip abductors | ||||
| Spinal manipulation (n = 10) | 21 (10) | 7 (10) | 25 (18) | 10 (13) |
| Placebo (n = 6) | 9 (7) | 0 (8) | 10 (6) | 2 (9) |
The change in the relative strength difference between limbs was greater in the spinal manipulation group compared to the placebo (mock spinal manipulation) group (p = 0.05)
Table 3.
Baseline and post-intervention means (SD) for strength of individual movements for spinal manipulation and placebo (mock spinal manipulation) groups
| Baseline strength (Nm) | Post-intervention strength (Nm) | P-value for difference in change between groups | |
|---|---|---|---|
| Weak side knee flexors | |||
| Spinal manipulation (n = 11) | 51 (27) | 65 (21) | 0.38 |
| Placebo (n = 15) | 60 (36) | 64 (32) | |
| Strong side knee flexors | |||
| Spinal manipulation (n = 11) | 71 (29) | 68 (21) | 0.89 |
| Placebo (n = 15) | 75 (41) | 73 (35) | |
| Weak side hip flexors | |||
| Spinal manipulation (n = 10) | 118 (40) | 139 (40) | 0.11 |
| Placebo (n = 11) | 118 (39) | 126 (45) | |
| Strong side hip flexors | |||
| Spinal manipulation (n = 10) | 145 (47) | 155 (49) | 0.70 |
| Placebo (n = 11) | 141 (47) | 152 (60) | |
| Weak side hip extensors | |||
| Spinal manipulation (n = 11) | 101 (33) | 115 (35) | 0.17 |
| Placebo (n = 9) | 115 (39) | 121 (39) | |
| Strong side hip extensors | |||
| Spinal manipulation (n = 11) | 120 (35) | 129 (38) | 0.11 |
| Placebo (n = 9) | 139 (45) | 139 (44) | |
| Weak side hip abductors | |||
| Spinal manipulation (n = 10) | 104 (43) | 116 (43) | 0.03 |
| Placebo (n = 6) | 84 (24) | 85 (31) | |
| Strong side hip abductors | |||
| Spinal manipulation (n = 10) | 126 (47) | 122 (39) | 0.49 |
| Placebo (n = 6) | 93 (28) | 85 (25) | |
Discussion
The main results of this research indicate that a spinal manipulation is able to reduce the relative strength difference between the lower limbs for knee and hip flexion in people that had a 15% or greater difference in strength between limbs at baseline (Table 2). Spinal manipulation also increased the strength of the weaker limb in hip abduction compared to placebo (mock spinal manipulation) (Table 3). Spinal manipulation reduced the relative strength differences between limbs from a mean (SD) of 57(53)% to 5(14)% for knee flexion and from 24(12)% to 11(15)% for hip flexion (Table 2). This may have clinical significance. For example, a 15% or greater strength imbalance between limbs for knee flexion is associated with greater development of lower limb injuries in female collegiate athletes.1 Future research should determine whether spinal manipulation can actually reduce the chance of future injury for individuals with lower leg strength imbalances.
The results are in agreement with a number of previous studies that have assessed the effects of spinal manipulation on knee extensor strength,15,16,26 trunk extensor strength,27,28 and elbow flexor strength.29 Our results are unique: While other studies have shown that spine manipulation can increase strength of weakened muscles, our study shows that a strength deficit between limbs may be reduced with a single lumbar spine manipulation. This could have implications for recreational or competitive athletes, or older people with functional impairments who have a large strength difference between limbs. Previous observations have suggested that those with large strength imbalances between limbs have a significantly increased risk of future injury.1,3,4,6,8,9
The mechanism whereby spinal manipulation improves the strength deficit between limbs is unknown in this study. Our study showed an immediate reduction in relative strength differences between limbs with one spinal manipulation. There are a number of studies suggesting enhanced motor unit excitability or reduced motor unit inhibition with spinal manipulation. A recent case series found that the thickness of the contracted transverse abdominus muscle was enhanced after spinal manipulation suggesting enhanced ability to recruit the musculature for contraction.30 Motor neuron excitability, as measured by transcranial magnetic stimulation increased after lumbar spine manipulation.17 Motor neuron inhibition, as measured by the interpolated twitch technique, was reduced in the knee extensors of a limb weakened by injury following manipulation of the sacroiliac joint on the ipsilateral side of the weaken limb.15,16 A number of mechanisms are proposed for the increase in motor neuron excitability or the removal of motor neuron inhibition with spinal manipulation, including altered excitability of mechanoreceptors in paraspinous tissue, altered discharge from muscle spindles or Golgi tendon organs, increased pain tolerance, increased opiate release, and alteration in sympathetic nervous system activity.14 These factors could alter afferent feedback to the spinal cord and ultimately enhance motor unit discharge. Another possibility is that spinal manipulation reduces connective tissue-mediated constriction of either the spinal nerve roots or of the blood vessels supplying the nerve roots,31 thus allowing increased recruitment of alpha motor neurons. Our study cannot determine which mechanism is responsible, but improvements in the weak leg strength of our participants is most likely due to enhanced motor unit excitability (or reduced motor unit inhibition) in these weak muscles.
There are a number of limitations to the current study. Although the reduction for relative (%) strength difference between legs was greater in the SM compared to the placebo (mock SM) group for knee and hip flexion (Table 2), there were no differences between groups for changes in absolute strength differences between legs. Our study was underpowered to detect these changes. For example, for knee flexion, the change for the SM group was about 16 Nm, and the change for the placebo (mock SM) group was 6 Nm (Table 2). The standard deviation for these change scores was about 15 Nm. With our sample size the power for this comparison was 0.36. Put another way, we would require 37 participants per group to achieve statistical significance at an alpha of 0.05 and a power of 0.8. Our study is limited in that power was calculated post-hoc. An additional limitation is that we did not correct our alpha-level for multiple statistical tests. Given that the statistical differences for change scores between groups from Tables 2 and 3 were of borderline significance (i.e. p-values between 0.03 and 0.05), there is a chance of type I statistical error.
It may have been difficult to blind some subjects to the treatment as many were recruited from advertisements in chiropractic clinics and therefore would have been familiar with actual chiropractic manipulation. Two thirds of the participants were able to correctly identify which group they were in and this might introduce bias into our results. Since many of the participants were aware they were receiving SM or placebo (mock SM) our study might more appropriately be described as a comparative study, rather than a placebo study. An innovative technique for blinding involving general anesthesia delivered before SM or placebo has recently been introduced and could be used in future clinical trials.32
Another limitation is that we did not perform long-term follow-up on participants to determine if the spinal manipulation was effective in the long-term. Our results indicate that spinal manipulation can reduce differences in leg strength immediately after spinal manipulation, but we do not know whether such an effect dissipates over time. If the effects of spinal manipulation dissipate over time, then the results of the strength tests after the spinal manipulation may have differed for those who had between-leg differences for multiple functional muscle groups compared to those with differences for only one muscle group (i.e. it would have taken up to 30 minutes to do all the strength testing after spinal manipulation for those with multiple strength tests).
We assumed that adjustment of specific lumbar vertebrae would affect specific nerve roots; however the accuracy of lumbar spine manipulations has been called into question. Ross et al.33 determined that the average error from target for lumbar spine manipulations was at least one vertebra away from the target and only about half of lumbar spine manipulations were deemed accurate. Given this non-specificity of spinal manipulation, the patients that received multiple adjustments (i.e. those who had more than one functional muscle group that showed a 15% strength difference between legs) might have received a higher dose of spinal manipulation compared to other participants.
Other limitations include the heterogeneity of our participant population and the lack of reproducibility of the 15% difference between contra-lateral legs for all functional measurements. Our study included participants of a wide range of ages and fitness levels. Our only inclusion criterion was a significant difference in strength between their weaker and stronger legs. Participants had the strength differences compared between legs and then were invited back into the lab a week later for spinal manipulation or mock placebo treatment if they had a 15% or greater strength difference for one or more functional movements. Between 15% and 44% of participants (depending on the strength test) improved strength on the second visit to an extent that they no longer had the hypothesized clinically important threshold of a 15% strength difference between limbs. These participants were still included in the study.
Conclusion
A single lumbar spinal manipulation may decrease the relative (%) strength difference between limbs for knee and hip flexion in individuals with 15% or greater discrepancy in strength between limbs at baseline. These results could have important implications for recreational and high performance athletes, or older people with functional impairments, as strength deficits between limbs may predict future injury. These conclusions are limited by the fact that 67% of the participants were able to identify whether they received actual spinal manipulation or the placebo (mock spinal manipulation). It is unknown whether the effect of spinal manipulation is transitory in nature because the durability of the effect was not assessed. Further research should evaluate the mechanism whereby the strength deficit between limbs is enhanced following spinal manipulation, and the durability of this effect. The clinical significance of the reduction in strength differences between limbs needs testing in future studies to determine if it actually prevents occurrence of future injury.
Footnotes
Supported by a grant from the Ralston Brothers Medical Research Fund.
References
- 1.Knapik JJ, Bauman CL, Jones BH, Harris JM, Vaughan L. Preseason strength and flexibility imbalances associated with athletic injuries in female collegiate athletes. Am J Sports Med. 1991;19:76–81. doi: 10.1177/036354659101900113. [DOI] [PubMed] [Google Scholar]
- 2.Niemuth PE, Johnson RJ, Myers MJ, Thieman TJ. Hip muscle weakness and overuse injuries in recreational runners. Clin J Sport Med. 2005;15:14–21. doi: 10.1097/00042752-200501000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Yamamoto T. Relationship between hamstring strains and leg muscle strength. A follow-up study of collegiate track and field athletes. J Sports Med Phys Fitness. 1993;33:194–9. [PubMed] [Google Scholar]
- 4.Askling C, Karlsson J, Thorstensson A. Hamstring injury occurrence in elite soccer players after preseason strength training with eccentric overload. Scand J Med Sci Sports. 2003;13:244–50. doi: 10.1034/j.1600-0838.2003.00312.x. [DOI] [PubMed] [Google Scholar]
- 5.Croisier JL, Forthomme B, Namurois MH, Vanderthommen M, Crielaard JM. Hamstring muscle strain recurrence and strength performance disorders. Am J Sports Med. 2002;30:199–203. doi: 10.1177/03635465020300020901. [DOI] [PubMed] [Google Scholar]
- 6.Orchard J, Marsden J, Lord S, Garlick D. Preseason hamstring muscle weakness associated with hamstring muscle injury in Australian footballers. Am J Sports Med. 1997;25:81–5. doi: 10.1177/036354659702500116. [DOI] [PubMed] [Google Scholar]
- 7.Lehance C, Binet J, Bury T, Croisier JL. Muscular strength, functional performances and injury risk in professional and junior elite soccer players. Scand J Med Sci Sports. 2009;19:243–51. doi: 10.1111/j.1600-0838.2008.00780.x. [DOI] [PubMed] [Google Scholar]
- 8.Croisier JL, Ganteaume S, Binet J, Genty M, Ferret JM. Strength imbalances and prevention of hamstring injury in professional soccer players: a prospective study. Am J Sports Med. 2008;36:1469–75. doi: 10.1177/0363546508316764. [DOI] [PubMed] [Google Scholar]
- 9.Nadler SF, Malanga GA, Feinberg JH, Prybicien M, Stitik TP, DePrince M. Relationship between hip muscle imbalance and occurrence of low back pain in collegiate athletes: a prospective study. Am J Phys Med Rehab. 2001;80:572–7. doi: 10.1097/00002060-200108000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Bennell K, Wajswelner H, Lew P, Schall-Riaucour A, Leslie S, Plant D, et al. Isokinetic strength testing does not predict hamstring injury in Australian Rules footballers. Brit J Sports Med. 1998;32:309–14. doi: 10.1136/bjsm.32.4.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brockett CL, Morgan DL, Proske U. Predicting hamstring strain injury in elite athletes. Med Sci Sports Exerc. 2004;36:379–87. doi: 10.1249/01.mss.0000117165.75832.05. [DOI] [PubMed] [Google Scholar]
- 12.Grace TG, Sweetser ER, Nelson MA, Ydens LR, Skipper BJ. Isokinetic muscle imbalance and knee-joint injuries. A prospective blind study. J Bone Joint Surg. 1984;66:734–40. [PubMed] [Google Scholar]
- 13.Chilibeck PD, Calder AW, Sale DG, Webber CE. A comparison of strength and muscle mass increases during resistance training in young women. Eur J Appl Physiol. 1998;77:170–5. doi: 10.1007/s004210050316. [DOI] [PubMed] [Google Scholar]
- 14.Pickar JG. Neurophysiological effects of spinal manipulation. Spine J. 2002;2:357–71. doi: 10.1016/s1529-9430(02)00400-x. [DOI] [PubMed] [Google Scholar]
- 15.Suter E, McMorland G, Herzog W, Bray R. Decrease in quadriceps inhibition after sacroiliac joint manipulation in patients with anterior knee pain. J Manipulative Physiol Ther. 1999;22:149–53. doi: 10.1016/S0161-4754(99)70128-4. [DOI] [PubMed] [Google Scholar]
- 16.Suter E, McMorland G, Herzog W, Bray R. Conservative lower back treatment reduces inhibition in knee-extensor muscles: a randomized controlled trial. J Manipulative Physiol Ther. 2000;23:76–80. [PubMed] [Google Scholar]
- 17.Dishman JD, Ball KA, Burke J. Central motor excitability changes after spinal manipulation: a transcranial magnetic stimulation study. J Manipulative Physiol Ther. 2002;25:1–9. [PubMed] [Google Scholar]
- 18.Cahalan TD, Johnson ME, Liu S, Chao EY. Quantitative measurements of hip strength in different age groups. Clin Orthop Relat Res. 1989;246:136–45. [PubMed] [Google Scholar]
- 19.Knapik JJ, Wright JE, Mawdsley RH, Braun J. Isometric, isotonic, and isokinetic torque variations in four muscle groups through a range of joint motion. Phys Ther. 1983;63:938–47. doi: 10.1093/ptj/63.6.938. [DOI] [PubMed] [Google Scholar]
- 20.Arnold CM, Warkentin KD, Chilibeck PD, Magnus CR. The reliability and validity of handheld dynamometry for the measurement of lower-extremity muscle strength in older adults. J Strength Cond Res. 2010;24:815–24. doi: 10.1519/JSC.0b013e3181aa36b8. [DOI] [PubMed] [Google Scholar]
- 21.Haldeman S. Spinal manipulative therapy; a status report. Clin Orthop. 1983;179:62–70. [PubMed] [Google Scholar]
- 22.Moore KL. Clinically Oriented Anatomy-Third Edition. Baltimore, MD: Williams & Wilkens; 1992. [Google Scholar]
- 23.Sandell J, Palmgren PJ, Björndahl L. Effect of chiropractic treatment on hip extension ability and running velocity among young male running athletes. J Chiropr Med. 2008;7:39–47. doi: 10.1016/j.jcme.2008.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bergman TF, Peterson DH. Chiropractic technique: principles and procedures. 3rd ed. St Louis Mo: Mosby/Elsevier; 2011. pp. 84–144. [Google Scholar]
- 25.Roy RA, Boucher JP, Comtois AS. Paraspinoal cutaneous temperature modification after spinal manipulation at L5. J Manipulative Physiol Ther. 2010;33:308–14. doi: 10.1016/j.jmpt.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 26.Hillermann B, Gomes AN, Korporaal C, Jackson D. A pilot study comparing the effects of spinal manipulative therapy with those of extra-spinal manipulative therapy on quadriceps muscle strength. J Manipulative Physiol Ther. 2006;29:145–9. doi: 10.1016/j.jmpt.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 27.Keller TS, Colloca CJ. Mechanical force spinal manipulation increases trunk muscle strength assessed by electromyography: a comparative clinical trial. J Manipulative Physiol Ther. 2000;23:585–95. doi: 10.1067/mmt.2000.110947. [DOI] [PubMed] [Google Scholar]
- 28.Perle SM. Mechanical force spinal manipulation increases trunk muscle strength assessed by electromyography: a comparative clinical trial. J Manipulative Physiol Ther. 2002;25:345–7. doi: 10.1067/mmt.2002.123179. [DOI] [PubMed] [Google Scholar]
- 29.Suter E, McMorland G. Decrease in elbow flexor inhibition after cervical spine manipulation in patients with chronic neck pain. Clin Biomech. 2002;17:541–4. doi: 10.1016/s0268-0033(02)00025-6. [DOI] [PubMed] [Google Scholar]
- 30.Raney NH, Teyhen DS, Childs JD. Observed changes in lateral abdominal muscle thickness after spinal manipulation: a case series using rehabilitative ultrasound imaging. J Orthop Sports Phys Ther. 2007;37:472–9. doi: 10.2519/jospt.2007.2523. [DOI] [PubMed] [Google Scholar]
- 31.Excoffon SG, Wallace H. Chiropractic and rehabilitative management of a patient with progressive lumbar disk injury, spondylolisthesis, and spondyloptosis. J Manipulative Physiol Ther. 2006;29(1):66–71. doi: 10.1016/j.jmpt.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 32.Kawchuk GN, Haugen R, Fritz J. A true blind for subjects who receive spinal manipulation therapy. Arch Phys Med Rehabil. 2009;90:366–8. doi: 10.1016/j.apmr.2008.08.213. [DOI] [PubMed] [Google Scholar]
- 33.Ross JK, Bereznick DE, McGill SM. Determining cavitation location during lumbar and thoracic spinal manipulation: is a spinal manipulation accurate and specific? Spine. 2004;29:1452–7. doi: 10.1097/01.brs.0000129024.95630.57. [DOI] [PubMed] [Google Scholar]