Abstract
Objectives. We evaluated the effectiveness of a community-based participatory research–grounded intervention among women receiving Temporary Assistance for Needy Families (TANF) with chronic health conditions in increasing (1) health care visits, (2) Medicaid knowledge and skills, and (3) health and functional status.
Methods. We used a randomized controlled trial design to assign 432 women to a public health nurse case management plus Medicaid intervention or a wait-control group. We assessed Medicaid outcomes pre- and posttraining; other outcomes were assessed at 3, 6, and 9 months.
Results. Medicaid knowledge and skills improved (P < .001 for both). Intervention group participants were more likely to have a new mental health visit (odds ratio [OR] = 1.92; P = .007), and this likelihood increased in higher-risk subgroups (OR = 2.03 and 2.83; P = .04 and .006, respectively). Depression and functional status improved in the intervention group over time (P = .016 for both). No differences were found in routine or preventive care, or general health.
Conclusions. Health outcomes among women receiving TANF can be improved with public health interventions. Additional strategies are needed to further reduce health disparities in this population.
In 1996, welfare reform legislation ushered in a new era of the US welfare system by creating the Temporary Assistance for Needy Families (TANF) program. Major changes in the new program included (1) work requirements and (2) consecutive months and lifetime time limits to benefit receipt.1
At the time TANF was implemented, the concept of health disparities was just emerging as a focal area for research and gaining recognition as a nationwide problem.2 Numerous studies had examined earnings and employment after a welfare exit3–7 and the effects of welfare receipt on the health and development of children8,9; however, little was known about the health of the women receiving welfare.10 Given the increased attention on health disparities11 and findings demonstrating that the majority of women who left welfare for employment remained in poverty,12–14 the new TANF regulations generated a swift increase in research. Notably, these studies began to examine how the health of the TANF population (96% of whom are single mothers and children) may be affected given the clear work mandates, time limits, and high prevalence of health problems in this group.15–17
Early postreform descriptive studies found that 25% to 42% of women receiving TANF had been diagnosed with major depressive disorder compared with 12% of women in the general population, and 9% were suffering from posttraumatic stress disorder.18 Rates of substance abuse (21%) and domestic violence (14.9%) were also reported to be significantly higher in the TANF population than they were in the general population (13% and 3.4%, respectively),18 as were rates of poor physical and general health based on the Short Form Health Survey (SF-12).19 Moreover, 48% of those with a work barrier identified a health problem as the primary limitation to working,20 and women with health problems that did leave TANF for employment had a 5.4-month shorter job tenure than did those without health problems.21 Therefore, health-related barriers were threatening—and continue to threaten—the ability of women leaving welfare for work to move toward economic self-sufficiency, and have impeded TANF program progress in meeting this goal.
Between 1996 and 2001, more than 5 million persons—predominantly women and children—left TANF (a 57% caseload reduction),22 with studies indicating that women with health problems14 and those from racial minority groups23 were becoming more concentrated in TANF programs. Taken together, these findings suggested that a work-first TANF approach that does not take into account the health needs of this population is unlikely to yield long-term gains in either self-sufficiency or health-related outcomes.
Despite this greater concentration, with few recent exceptions24–27 attempts to address health problems among women receiving TANF have relied nearly exclusively on descriptive reports of best practices16,28,29 or project evaluations that lack valid and reliable measures,29 rather than on well-designed intervention studies. Across states, programs to address health needs in this group have largely focused on screening for drug use (64% of states), domestic violence (50%), and mental health problems (45%)30; however, practices vary widely within and across states, and there is a lack of clarity around outcomes. Findings from our preliminary studies indicated that women disliked the health screening process and questionnaires used in an existing Welfare Transition Program (or a WTP, which encompasses the mandatory work-focused activities of TANF), raising questions about the effectiveness of approaches not grounded in their specific needs, perspectives, or life context.31
This study fills a large gap in the existing intervention-based evidence that is needed to address the health problems among women receiving welfare. Over the past decade, administrators responsible for TANF implementation at the federal, state, and local levels have raised concerns about how to effectively handle the mental and physical health-related needs of the population they serve,16 but intervention research in this area has not kept pace with the needs.
This study was guided by Milio's ecological framework32 for improving health, which conceptualizes policy factors operating in the macrolevel environment as the most significant determinants of health. As such, it assumes individual or behavioral-focused interventions—although necessary—are insufficient for improving population health. Although we focused on ways to improve women's health through TANF-related system (and policy) enhancements, our research also builds on the literature documenting the effectiveness of public health nursing (PHN) case management with similar populations of low-income, at-risk single mothers,33,34 the importance of tailoring intervention materials to specific groups,35,36 the difficulties low-income patients have in understanding Medicaid benefits, and the application of patient-centered interventions for improving health outcomes.36,37 Specifically, we report the outcomes from a randomized controlled trial that had the following aim: to test the efficacy of a PHN case management and Medicaid knowledge and skills training program for women enrolled in WTPs in (1) increasing rates of health care visits for mental health and chronic health conditions, (2) increasing the ability to navigate the Medicaid system, and (3) improving functional and health status over time among women with chronic health conditions by using a community-based participatory research (CBPR) methodology. To the best of our knowledge, no previous study has tested a similar intervention with this population.
METHODS
We used a CBPR approach to design and conduct this study. Although no uniform approach exists, CBPR should generally encompass (1) genuine partnerships with the community, (2) shared decision-making, (3) capacity building, and (4) benefiting all partners.38–40 Before this study, the principal investigator had a 5-year history of building positive, trusting relationships with administrative members and attendees of the local WTP, the African American community, and local public health and health care providers as a researcher and clinician who provided care to underserved populations.
Preliminary studies provided the groundwork for developing major components of the intervention that were of most importance to women in the WTP, insured the intervention was participant-focused, and made recommendations for how to best engage members of the community while conducting the randomized, controlled trial. Details of the participatory processes related to study development are described elsewhere.41 A Community Advisory Group comprising 17 diverse academic researchers, agency representatives, and lay community members provided guidance to the study team; its vote on key issues was required before the principal investigator could proceed with study enrollment. In addition, 3 women who had been recent WTP participants were hired full-time onto the study team: 2 as community research assistants and 1 as the study coordinator. All 3 women hired onto the study engaged in both personal and community capacity building by (1) developing a set of research-related employment skills that would be sought after in the university-centered geographical area in which they lived; (2) providing factual information about research processes, involvement, and benefits in their (predominantly) minority communities; (3) applying their knowledge of research to address other problems relevant to the community through grant writing efforts; and, (4) serving as role models for other women struggling to leave welfare for work. Members of the Community Advisory Group, WTP partners, and participants from the trial assisted in interpretation of findings. These findings have contributed to local capacity-building efforts within the WTP to make programmatic improvements and better meet the health needs of the TANF population. Additional analyses and dissemination efforts with community partners are ongoing.
Setting and Sample
We recruited a convenience sample from 1 WTP serving 1 urban and 1 rural county in north-central Florida between 2007 and 2009. Recruitment, consent, follow-up, and the intervention delivery were conducted on-site in the local WTP offices in each county, which housed a number of independent agencies contracted to provide employment-related services; however, the individual spaces provided for study purposes insured participants’ privacy. Only women were eligible for study participation, as more than 90% of persons receiving TANF are women. Enrollment criteria required women to be receiving TANF, to not yet be employed, to be between the ages of 18 and 60 years, to have at least 1 chronic health condition, and to speak English. Women who were pregnant or receiving disability income were excluded, and those who became pregnant or moved during the study were withdrawn. Recruitment was conducted in the WTP offices by the community research assistants, generally during WTP orientation sessions, and flyers were posted in targeted community areas.
Institutional review board approval was granted at the university where the study was conducted. We screened interested participants to determine whether they met the initial eligibility criteria. Afterward, they underwent 2 informed consent processes: the first to complete a health screening questionnaire and interview by a PHN to ensure a chronic health condition was present, and the second for enrollment, if eligible. We adopted the definition of a chronic health condition used by the National Health Interview Survey of “conditions that are generally not cured, once acquired” for this study.42(p29) We applied this broadly, to also include conditions for which single, episodic treatment and cure are possible, but in which relapse or recurrence rates are very high—such as with depression.43 An additional requirement was that the condition had to have a reasonable potential for interfering with functional status and, by extension, employment performance and absenteeism. So, for example, conditions such as migraine headaches, asthma, and arthritis would qualify for inclusion, whereas high cholesterol or obesity (alone) would not.
The chronic health condition criterion was met by either self-report of a condition diagnosed by a health provider, or findings from the PHN health screening, which could include a positive screen for depression (≥ 17 on the Beck Depression Inventory-II44 [BDI-II] confirmed by the Structured Clinical Interview for DSM Disorders Axis I, Nonpatient45 [SCID-I/NP]—Major Depressive Episode/Disorder), anxiety (≥ 16 on the Beck Anxiety Inventory46 [BAI] confirmed by the SCID-I/NP—Generalized Anxiety Disorder), or posttraumatic stress disorder (PTSD; based on the SCID-I/NP—PTSD) as a chronic health condition.47 Thus, a wide range of conditions met this criterion. Randomization and allocation processes followed CONSORT guidelines,48 with a computer-generated random number sequence used to randomize participants to group, and sequentially numbered envelopes concealed group status until allocation was complete.
After enrollment and at each follow-up, participants received a $50.00 gift certificate. In addition, a $5.00 gift certificate with a thank-you card was mailed to participants each month.
Intervention
The primary intervention component included 9 months of case management by a PHN on-site at the WTP. All PHNs had a minimum of a baccalaureate of science in nursing degree and experience working with disadvantaged women.49 Building trust with the PHN was identified as a crucial feature by this population when we were designing the intervention41; therefore, the intervention group participants received care by the same PHN from initial screening to the 9-month follow-up. Case management emphasized health care access or entry into primary care for newly identified symptoms; care coordination; health education; health and social service referrals; obtaining preventive services, screening, and routine care; and assistance in meeting health goals participants had set for themselves.
The PHNs were instructed to approach their case-management interventions in a manner that generally reflected the Stages of Change approach used in the health screening questionnaire developed by women in the TANF program.50 As an example, some of the more sensitive questions in the screening questionnaire asked participants if they would like additional information, a referral, or other form of intervention in various health areas, with the options of answering “yes,” “no,” or “maybe, but later.”41 This meant that participants were not pushed into interventions in which they were not ready to engage. Instead, PHNs worked with participants over time in building trust, providing support, and slowly helping them move toward engagement and taking action.51 In addition, PHNs intervened with WTP case workers and employers when warranted to insure health-related needs were met—and only when intervention group participants gave permission to intervene. Case management was individualized, and PHNs had a minimum of 4 typically 1-hour meetings with intervention group participants. The majority of visits were conducted at the WTP site; however, a small number of home visits were conducted when deemed necessary by the PHN or to complete a follow-up visit.
In addition to case management, a 1-time, 2-hour training session was provided by a community research assistant to enhance intervention group participants’ knowledge and skills to use their Medicaid coverage most effectively. This component was also identified as a need by WTP participants in preliminary studies, as several indicated they were frustrated with navigating the complexity of the Medicaid and health care systems, and would be unable to successfully have their health care needs met if they could not optimally use their Medicaid benefits. Building on these preliminary data, the knowledge-building portion of the training was based on factual Medicaid benefit information. The skills-building portion was grounded within the Transactional Model of Stress and Coping52 and employed cognitive behavioral stress management therapy techniques that have been demonstrated to improve stress, coping, and clinical outcomes in similar populations.53 Specifically, it was geared toward helping participants (1) identify aspects of navigating Medicaid services (“events”) that are stressful; (2) identify how perceptions of these events impact mood, behavior, and physical symptoms; (3) label uncontrollable and controllable aspects of these events; and (4) engage in adaptive, emotion-based, or problem-based coping strategies to manage these events. Brief didactic training about how to engage in this stress appraisal and coping process was provided and then participants practiced their knowledge and skills by role-playing responses to standardized scenarios commonly experienced as stressful by Medicaid recipients.
Across all aspects of the intervention, training was provided to research staff for their respective roles and fidelity was insured by monitoring and observing intervention delivery by the study principal investigator. Control group participants were wait-listed—meaning they were offered a reduced form of the intervention when they completed the study (i.e., at the end of their 9-month follow-up). The wait-list session included a 1-time appointment with the PHN to provide whatever case-management services could be completed in a single appointment (without time constraints), along with the Medicaid training, and was incorporated as part of the study design based on recommendations from our community partners.
Data Collection and Outcome Measures
Recruitment and all follow-up took place from February 2007 to April 2010. We collected data at baseline, 3 months, 6 months, and 9 months by primarily self-report questionnaires. Intervention group participants brought completed questionnaires to their PHN visit, and control group participants submitted completed questionnaires to the community research assistant assigned as their data collector.
To improve self-report accuracy for health care visits, we employed an approach that links visit recall to personally meaningful events on a calendar.54 For mental health visits, we compared whether women who were not receiving treatment at enrollment made a new visit during the study. For chronic health conditions, we focused on visits to primary care providers that were made for routine management of existing conditions or preventive care, rather than care for acute illness reasons. We used dichotomous variables indicating whether participants reported a visit for a new mental health visit and a primary care routine or preventive visit at any time during the study period as outcome measures. In Florida, Medicaid benefits typically continue for the first few months after TANF receipt; thus, at least initially, health care access was generally uniform across participants.
We assessed knowledge of Medicaid benefits with a 20-item questionnaire developed by the research team. We established content validity through a review of the questions by the community research assistants, staff in the local Medicaid office, and comparison of the questions to the regional Medicaid guidelines. The possible range of scores was 0 to 20. We assessed Medicaid skills competence with standard approaches recognized by behavioral health care agencies55 and created a rating tool that assessed the degree to which participants’ behaviors indicated effective coping skills during standardized role play. Behavioral performance was rated on 5 dimensions: confidence to engage in role play, emotional responses, content accuracy of responses (i.e., Do participants’ ask specific, appropriate questions?), incorporation of behavioral skills, and interpersonal communication. These dimensions, ratings, and behavioral benchmarks were developed by members of the research team with expertise in stress management, cognitive behavioral therapy, and skills competency evaluation. The rating tool had a possible range of zero to 15 points, with a higher score indicating greater skills competence. The Medicaid knowledge questionnaire and skills competence evaluations were administered and coded before and after the teaching session by a consistent community research assistant throughout the study period.
Our main health outcomes included depression (the BDI-II), general health (from the SF-12 version 2 [SF-12v2]), and a composite measure of functional status derived from 4 dimensions within the SF-12v2. The BDI-II and the SF-12v2 health dimension measures have established validity and reliability in this population.44,56,57 Four of the SF-12v2 dimensions directly relate to whether health has limited carrying out expected roles (role–emotional and role–physical), or has limited routine physical or social activities (physical functioning and social functioning).57 We used a composite of mean role–emotional, role–physical, physical functioning, and social functioning scores as a measure of functional status. In our sample, the BDI-II and the SF-12v2 functional status composite had a Cronbach's α of 0.93 and 0.86, respectively. No internal consistency reliability data are reported for the SF-12v2 General Health dimension, as it is comprised of a single item.
Finally, we calculated intervention “nurse dose” by having PHNs document the number of minutes spent with intervention group participants. This included measures of indirect dose (i.e., telephone or text messages), direct phone dose (i.e., phone conversation), direct in-person (i.e., face-to-face time), and a total, or combined, dose of these.
Sample Size and Statistical Analyses
The original power analysis for this study called for a sample of 312 women. At roughly midpoint during the study we performed an internal pilot interim power analysis revision based on accepted approaches in the literature to correct for (1) an initial sample calculation that did not fully account for the longitudinal nature of the data, and (2) the substitution of the SF-12v2 composite functional status measure to be used in place of the Sickness Impact Profile (because of data collection and scoring problems with the Sickness Impact Profile that arose during the study).58–62 A final sample size of 432 insured at least 0.80 power for the Treatment effect of 5 points in general health and the Treatment and Treatment × Time effects of 15 points for functional status. This revision accounted for up to a 20% attrition rate in the study. We deemed the sample size to be adequate for examining changes in depression based on information from earlier studies.63,64 Missing data were minimal, with less than 10% missing on outcomes of interest among those who completed follow-up at each time point.
We examined intervention effects on health care visit rates by using logistic regression. In addition to determining group effects in the full sample, we wanted to examine whether the odds of visits increased as the need for referral and health care visits increased. Therefore, logistic regression models with “new mental health visit” as the outcome were tested in the full sample, in participants reporting a history of depression, and in participants whose BDI-II scores reflected moderate or severe depressive symptoms. Similarly, participants with a higher number of chronic health conditions would be more likely to need a routine or preventive care visit for adequate management; thus, we examined whether the odds of a routine or preventive care visit differed by group in the full sample and a subsample with 3 or more chronic health conditions.
We assessed changes in Medicaid knowledge and skills scores by using the Wilcoxon matched-pairs signed ranks test, because they were not normally distributed (Shapiro–Wilk test; P < .001 for all).
We performed repeated measures longitudinal analysis with SAS version 9.2 (SAS Institute, Cary, NC). Because of randomization, there were no between-treatment-group differences at baseline on sociodemographic or other health-related variables of interest. We compared parametric models for each outcome by using likelihood ratio tests to determine the best fitting parametric curve among cubic (saturated), quadratic, or linear. The main tests of interest were the Treatment × Time effects on the outcome measures for general health, functional status, and depression over the 9 months of follow-up. We followed a significant Treatment × Time test at α = 0.05 by testing for differences at each follow-up time point. If the Treatment × Time test was nonsignificant, we assessed an exploratory time averaged Treatment difference over the follow-up periods.
RESULTS
Figure A (available as a supplement to the online version of this article at http://www.ajph.org) depicts the flow of participants through the study. During recruitment, we screened 589 women to determine whether they met the initial inclusion criteria. Of those, we had a final sample of 432 (73% of those who completed initial screening). Fifty-nine participants (13.7%) had to be withdrawn (Figure A). Of the 373 eligible to complete the study, 76% (n = 285) completed the 9-month follow-up. Sample demographics and health-related characteristics are detailed in Table 1. The sample included women who were primarily Black (56.3%), unmarried (88.4%), and had a mean age of 29.8 years (SD = 8.2). Nearly 53% screened positive for possible depression according to the BDI-II at baseline. The chronic health conditions most prevalent in the sample included headaches (53%), back pain (50%), depression (40%), and seasonal allergies (38%). There were no differences in sociodemographic or health characteristics at baseline (Table 1) or in retention status between groups. The mean nurse dose (in minutes of PHN contact) was as follows: direct phone (mean = 57; SD = 50), direct in-person (mean = 157; SD = 72), indirect (mean = 47; SD = 22), and combined (mean = 261; SD = 112).
TABLE 1.
Baseline Sociodemographic and Select Health Sample Characteristics: Women Receiving Temporary Assistance for Needy Families, Florida, 2007–2009
| Characteristic | Intervention (n = 214), % or Mean (SD) | Control (n = 218), % or Mean (SD) | Total (n = 432), % or Mean (SD) |
| Age | 28.8 (7.3) | 30.8 (8.9) | 29.8 (8.2) |
| Race | |||
| Black | 61.2 | 51.4 | 56.3 |
| White | 35.5 | 43.1 | 39.4 |
| Other | 3.3 | 5.5 | 4.4 |
| Ethnicity: Hispanic | 4.2 | 5.1 | 4.6 |
| Education level | |||
| < 12th grade | 32.2 | 32.6 | 32.4 |
| High-school diploma or GED | 29.0 | 26.6 | 27.8 |
| Some college or technical training | 37.4 | 38.5 | 38.0 |
| College degree (≥ associate degree) | 1.4 | 2.3 | 1.8 |
| County | |||
| Urban | 78.5 | 82.1 | 80.3 |
| Rural | 21.5 | 17.9 | 19.7 |
| No. of times received TANF previously | |||
| 0–1 | 51.4 | 53.7 | 52.6 |
| 2–3 | 31.8 | 27.5 | 29.6 |
| ≥4 | 16.8 | 18.8 | 17.8 |
| No. of jobs held in past y | |||
| 0 | 17.3 | 21.6 | 19.4 |
| 1–2 | 64.5 | 59.2 | 61.8 |
| 3–4 | 12.2 | 15.1 | 13.7 |
| ≥5 | 6.1 | 4.1 | 5.1 |
| No. of jobs left in past y because of health problems | |||
| 0 | 66.8 | 74.8 | 70.8 |
| ≥1 | 33.2 | 25.2 | 29.2 |
| No. of children | 2.5 (1.3) | 2.5 (1.2) | 2.5 (1.3) |
| Mean age of children | 6.6 (5.0) | 7.5 (6.0) | 7.1 (5.6) |
| Marital status: single or unmarried | 89.3 | 87.6 | 88.4 |
| Total household income,a $ | 687.5 (427.8) | 626.2 (440.3) | 656.6 (434.4) |
| Number of chronic health conditions | 3.7 (2.1) | 3.8 (2.5) | 3.8 (2.3) |
| Number of generalized symptomsb | 8.3 (6.4) | 7.9 (6.9) | 8.1 (6.6) |
| BDI-II depressive symptom category | |||
| Minimal symptoms | 36.7 | 32.2 | 34.4 |
| Mild symptoms | 22.0 | 23.6 | 22.8 |
| Moderate symptoms | 16.8 | 21.1 | 19.0 |
| Severe symptoms | 24.5 | 23.1 | 23.8 |
| BDI-II cutoff for depression screening | |||
| Positive (BDI-II score ≥ 17) | 52.5 | 47.2 | 52.7 |
| Negative (BDI-II score < 17) | 47.5 | 52.8 | 47.3 |
Notes. BDI = Beck Depression Inventory; GED = general equivalency diploma TANF = Temporary Assistance for Needy Families.
Total household income includes income per month from food stamps, TANF, work-related income, and income received from others (e.g., family, friends, or partners) on a regular basis.
Number of reported symptoms based on routine review of systems.
Findings for health care visits are detailed in Table 2. Intervention group participants were nearly twice as likely to have made a new mental health visit during the study period (OR = 1.92; P = .007). To determine whether subgroups of participants more at risk for needing health care visits were more likely to have received them, we conducted a narrowly defined set of subgroup analyses posthoc, mindful of the exploratory nature of and standards for examining subgroups.65 Intervention group participants with a history of depression had twice the odds of a new mental health visit (OR = 2.03; P = .04), and those with moderate or severe depressive symptoms were nearly 3 times as likely to enter mental health care (OR = 2.83; P = .006). Similar increases were not observed for routine or preventive care visits—even in the subgroup with 3 or more chronic health conditions (P > .05). There were statistically significant increases in both Medicaid knowledge and skills competence following training (P < .001 for each); however, the actual increases in scores were minimal (median increases from 14–15, and 15–16, respectively).
TABLE 2.
Odds of a Health Care Visit for Select Chronic Health Conditions: Women Receiving Temporary Assistance for Needy Families, Florida, 2007–2009
| Outcome Variable | Intervention, % (No.) | Control, % (No.) | OR (95% CI) | P |
| New mental health visit madea | ||||
| Full sample: all participants (n = 358) | 33 (58) | 20 (37) | 1.92 (1.19, 3.11) | .007 |
| Subgroup 1: history of self-reported depression (n = 147) | 49 (38) | 32 (22) | 2.03 (1.04, 3.98) | .04 |
| Subgroup 2: BDI-II scores = moderate or severe (n = 133) | 45 (28) | 23 (16) | 2.83 (1.34, 5.98) | .006 |
| Preventive or routine care visit madeb | ||||
| Full sample: all participants (n = 346) | 88 (189) | 87 (189) | 1.50 (0.92, 2.46) | .11 |
| Subgroup 1: participants with ≥ 3 chronic health conditions (n = 228) | 81 (91) | 71 (82) | 1.66 (0.90, 3.08) | .11 |
Notes. BDI-II = Beck Depression Inventory-II; CI = confidence interval; OR = odds ratio.
Includes any new mental health visits made over the 9-mo study period among participants who were not already receiving mental health services at baseline and had completed at least 1 follow-up; subgroup 1 with “history of depression” compares only participants who self-reported history of depression at baseline. BDI-II scores reflect severity at baseline or study enrollment, and compare only those categorized as moderate or severe by group.
Refers to any visit to primary care provider for preventive or routine care made over the 9-mo study period; subgroup 1 refers to participants with ≥ 3 chronic health conditions at baseline or study enrollment.
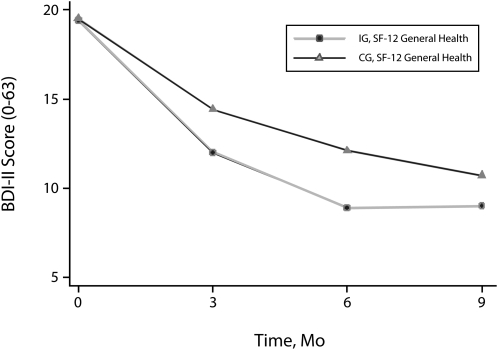
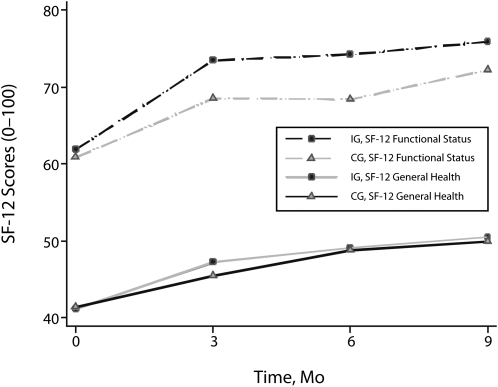
Descriptive statistics for health outcomes are presented in Table A (available as a supplement to the online version of this article at http://www.ajph.org). Depressive symptoms decreased in both groups, with the intervention group having a significantly greater rate of reduction over the 9-month period than did the control group (Treatment × Time P = .016). As shown in Figure 1, the most dramatic decrease in depressive symptoms occurred between 0 and 6 months. Both the rate of decrease within group and the rate of difference between groups diminished from 6 to 9 months. Follow-up tests confirmed significant Treatment differences at 3 and 6 months (both with P < .01) with less evidence at 9 months (P = .08). Despite trends toward improvement in general health, no group differences were observed (P = .72). Functional status had overall improving trends as well as an observed but nonsignificant Treatment × Time effect (P = .09) over the 9 months of follow-up. The time-averaged Treatment test on follow-up time points for functional status was significant (P = .016) with an estimated mean functional score for the intervention group 4.7 points higher than that for the control group across the study follow-up time points (Figure 2).
FIGURE 1.
Depressive symptom severity (BDI-II) by group and time: women receiving Temporary Assistance for Needy Families, Florida, 2007–2009.
Note. BDI = Beck Depression Inventory.
FIGURE 2.
Functional status (SF-12v2) and general health (SF-12v2) by group and time: women receiving Temporary Assistance for Needy Families, Florida, 2007–2009.
Note. SF-12v2 = Short Form 12 version 2.
DISCUSSION
The main group-effect findings from this randomized, controlled trial suggest that a PHN case-management intervention combined with Medicaid training is effective in improving health care visit rates for mental health, reducing depressive symptoms, and improving functional status among women in a WTP. Medicaid knowledge and skills competence increases were relatively small given the potential range of scores; however, based on responses to a single question asked at the 9-month follow-up, 34% of intervention group participants indicated that they applied what they learned in a real-life Medicaid use encounter by the end of the study. No significant group differences in general health were observed during the study period, although there was improvement from baseline to the 3-month follow-up visit in both groups.
Findings from the study related to mental health visits and routine or preventive health care visits may have mediated findings with respect to mental and physical health. That is, the higher number of mental health visits in the intervention group may have facilitated a decrease in depressive symptoms and improvements in functional status, which has been reported in similar studies.66 By contrast, no group differences in routine or preventive health care visits may mean physical health needs were met to a lesser extent, and may in part explain the lack of an intervention effect on general health. Moreover, ceiling effects at baseline for having had a routine or preventive health care visit in the previous 12 months (> 86%, across groups) reduced the ability to detect group differences.
Notably, both groups improved over time on depressive symptoms, functional status, and in general health—particularly between baseline and the 3-month follow-up. Why this finding occurred in the control group to the extent that it did is uncertain; however, anecdotally, women in the trial indicated they were at an extreme low point in their lives when baseline measures were taken (i.e., for most, having just applied for TANF or welfare benefits), and that moving into employment or becoming independent of the WTP made a major improvement in their overall well-being—prompting what may be a regression to the mean—or a trend of health-related scores returning to their prewelfare level. In addition, control group participants commented that the health screening questionnaire (developed specifically for women in the WTP41) challenged them to think more seriously about their health needs (and in some cases act on those needs). Finally, additional anecdotal reports from study participants suggest the community research assistants collecting data from the control group may have served as a form of an attention control—even though no intentional social support or intervention was delivered. Given the potential relevance of similar effects across an array of CBPR-grounded studies, we are formally examining these influences in a follow-up, qualitative study with women who were participants in the trial.
Our health-related findings show interesting parallels to and differences from other recent trials with similar populations. Using intensive case management delivered in local TANF offices, Morgenstern et al. demonstrated that substance-abuse treatment and 24-month abstinence rates among substance-abusing women in a WTP were nearly twice as high in the intervention group.24,27 Miranda et al.66 found that women with major depressive disorder who completed clinical guideline-driven treatment (either medication management or cognitive behavioral therapy) exhibited improvement in depressive symptoms, social functioning, and instrumental functioning over a 1-year period. In the study by Miranda et al.,66 these improvements occurred on a magnitude of roughly 15% to 18%, 22% to 23%, and 26% to 33%, respectively (in the 2 treatment groups), and in our study, depressive symptoms and functional status improved on the order of 15% and 14%, respectively (in the intervention group). Although these studies differ in terms of the measures used and end follow-up period, the reduction in depressive symptoms was similar, although the magnitude of functional status improvement in our study was not as robust. Moreover, although the average functional status difference between groups was statistically significant in our study, it did appear there was a trend toward convergence at the 9-month follow-up, whereas in the study by Miranda et al.66 functional status improvement was maintained through the 12-month follow-up for those completing medication treatment. A potentially key difference that may account for this divergence in functional status findings was the referral of our intervention group to community mental health care, whereas community mental health care served as the control condition in the study by Miranda et al. It is plausible that ensuring the delivery of medication or cognitive behavioral therapy guideline-based interventions in the future with women in WTPs may increase both the magnitude and duration of functional status improvement because studies have demonstrated long-term improvements in social functioning and employment outcomes from medication or cognitive behavioral therapy.67,68 On a final note, although functional status is an important component of quality of life for all populations, improving functioning in the WTP population of women is particularly salient because of the policy changes with welfare reform and the emphasis on rapid entry into—and the need to maintain—employment.
Strengths and Limitations
The methodological strengths of this study included the randomized, controlled trial design, sample size, retention, and use of the CBPR process. Providing services on-site in local WTP offices, using lay community personnel to deliver Medicaid training, and basing the intervention largely on PHN competencies are features that facilitate transfer into practice. Moreover, consistent with other findings in the literature,69 we believe the CBPR approach used to tailor the intervention to the expressed needs of women in the WTP, and the CBPR components incorporated in conducting the trial were instrumental in overcoming the recruitment and retention difficulties that commonly occur in randomized, controlled trials with low-income and minority populations. The findings are limited in that they do not generalize beyond White or Black women, are limited to relatively short-term outcomes, and were dependent on a composite measure of functional status that has not had rigorous psychometric evaluation.
Conclusions
Taken together, findings from this and other studies suggest that on-site PHN case management can improve outcomes for women in TANF programs. Our findings are directly relevant for future welfare policy development, as they provide some initial evidence of how to structure health-related services within TANF programs to serve a broad array of health needs. However, as with all attempts to move evidence into practice, any uptake of this intervention into the TANF arena requires careful adherence to retain the major components and their fidelity—including, but not limited to, use of a culturally sensitive, acceptable screening tool; PHNs with similar educational levels, experience, and training; and integrating community members as program personnel in a manner similar to that used here. Concerns WTP or TANF administrators may have about implementation can be readily addressed by partnering with nurse administrators at local health departments, who either have the knowledge and skill required to appropriately implement the evidence into practice or can collaborate with colleagues who do.
Despite this contribution to the literature, questions remain. For example, whether referral to the community mental health standard of care for the TANF population is sufficient to expect optimal mental health and functional status outcomes is an issue with which local public health professionals and those involved in welfare policy decision-making will need to grapple. Future findings from this study may further inform policy and practice. Analyses of the effects of race, nurse dose, and other factors as mediators or moderators of outcomes from the study are ongoing and may further inform policy and practice. Perhaps what is most certain is what remains to be done on policy, practice, and research fronts. Given the complexity of the social, health, and other needs of this population, and the complexity of the systems from which we try to address them, additional research to improve long-term health outcomes of women in WTPs is necessary to meet the nation's challenge of eliminating health disparities.
Acknowledgments
The project was supported by the National Institutes of Health/National Institute of Nursing Research (NIH/NINR, grant 5R01NR009406).
We thank those who have engaged in the community-based participatory research (CBPR) process with us, who enrolled in the study as research participants, and who have remained steadfast in their desire to improve the lives and health of other women in similar life circumstances. We are also grateful to our community partners and research team, including the public health nurses, research assistants, and students; staff at the Florida Works program in Alachua and Bradford counties; Eastside Community Practice; the Alachua County Health Department; and the Alachua County Department of Children and Families Medicaid office. Finally, we are especially proud of the achievements made by the CBPR research assistants and study coordinator—Deidra Means, Cynthia Allen, and Toni Watson—both during the study and since its completion in improving their lives, the lives of others, and working to improve the health of their communities.
Note. The article contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH or NINR.
Human Participant Protection
We received approval from the University of Florida institutional review board before conducting the study. Participants received written informed consent before both health screenings to determine eligibility and enrollment.
References
- 1.Personal Responsibility and Work Opportunity Reconciliation Act of 1996, §401 et seq. (1996). [Google Scholar]
- 2.James SA. Epidemiologic research on health disparities: some thoughts on history and current developments. Epidemiol Rev. 2009;31:1–6 [DOI] [PubMed] [Google Scholar]
- 3.Harris KM. Life after welfare: women, work, and repeat dependency. Am Sociol Rev. 1996;61:407–426 [Google Scholar]
- 4.Cao J. Welfare Recipiency and Welfare Recidivism: An Analysis of the NLSY Data. Madison, WI: Institute for Research on Poverty; 1996:1081–1096 [Google Scholar]
- 5.Bane MJ, Ellwood DT. Welfare Realities: From Rhetoric to Reform. Cambridge, MA: Harvard University Press; 1994 [Google Scholar]
- 6.Pavetti LA. The Dynamics of Welfare and Work: Exploring the Process by Which Women Work Their Way off Welfare [PhD dissertation] Cambridge, MA: Kennedy School of Government, Harvard University; 1993 [Google Scholar]
- 7.Meyer DR, Cancian M. Life After Welfare: The Economic Well-Being of Women and Children Following an Exit From AFDC. Madison, WI: Institute for Research on Poverty; 1996. Discussion paper no 1101–96 [Google Scholar]
- 8.Currie J, Cole N. Welfare and child health: the link between AFDC participation and birth weight. Am Econ Rev. 1993;83(4):971–985 [Google Scholar]
- 9.Moore KA, Zaslow MJ, Coiro MJ, Miller SM. How Well Are They Faring? AFDC Families With Preschool-Aged Children in Atlanta at the Outset of the JOBS Evaluation. Oakland, CA: Manpower Demonstration Research Corporation; 1995 [Google Scholar]
- 10.Kneipp S. Economic self-sufficiency: an insufficient indicator of how women fare following welfare reform. Policy Polit Nurs Pract. 2000;1(4):256–266 [Google Scholar]
- 11.Wilkinson R. Unhealthy Societies: The Afflictions of Inequality. New York, NY: Routledge; 1996 [Google Scholar]
- 12.Cancian M, Haveman R, Meyer DR, Wolfe B. Before and After TANF: The Economic Well-Being of Women Leaving Welfare. Madison, WI: Institute for Research on Poverty; 2000. Special report no. 77 [Google Scholar]
- 13.Loprest P. Families Who Left Welfare: Who Are They and How Are They Doing? Washington, DC: The Urban Institute; 1999 [Google Scholar]
- 14.Loprest P. How Are Families That Left Welfare Doing? A Comparison of Early and Recent Welfare Leavers. Washington, DC: The Urban Institute; 2001. Series B, No. B-36 [Google Scholar]
- 15.Coiro MJ. Depressive symptoms among women receiving welfare. Women Health. 2001;32(1-2):1–23 [DOI] [PubMed] [Google Scholar]
- 16.Fagnoni C. Opportunities Exist to Help People With Impairments Become More Self-Sufficient: TANF and SSI. Washington, DC: US Government Accountability Office; 2004:32 [Google Scholar]
- 17.Kaplan GA, Siefert K, Ranjit N, et al. The health of poor women under welfare reform. Am J Public Health. 2005;95(7):1252–1258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Danziger S, Corcoran M, Danziger S, et al. Barriers to the Employment of Welfare Recipients. Madison, WI: Institute for Research on Poverty; 1999. No. 1193–99 [Google Scholar]
- 19.Polit DF, London AS, Martinez JM. The Health of Poor Urban Women: Findings from the Project on Devolution and Urban Change: New York, NY: Manpower Demonstration Research Corporation; 2001 [Google Scholar]
- 20.Zedlewski SR. Work Activity and Obstacles to Work Among TANF Recipients. Washington, DC: The Urban Institute; 1999. Series B, No. B-2 [Google Scholar]
- 21.Corcoran M, Danziger S, Tolman R. Long term employment of African-American and White welfare recipients and the role of persistent health and mental health problems. Women Health. 2004;39(4):21–40 [DOI] [PubMed] [Google Scholar]
- 22.US Department of Health and Human Services Percent change in AFDC/TANF families and recipients, August 1996-September 2001. Available at: http://www.acf.hhs.gov/programs/ofa/data-reports/index.htm. Accessed May 19, 2011
- 23.US Department of Health and Human Services Temporary Assistance for Needy Families (TANF) Fifth Annual Report to Congress. Washington, DC: Administration for Children and Families; 2003 [Google Scholar]
- 24.Morgenstern J, Blanchard KA, McCrady BS, McVeigh KH, Morgan TJ, Pandina RJ. Effectiveness of intensive case management for substance-dependent women receiving temporary assistance for needy families. Am J Public Health. 2006;96(11):2016–2023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morgenstern J, Hogue A, Dauber S, Dasaro C, McKay JR. Does coordinated care management improve employment for substance-using welfare recipients? J Stud Alcohol Drugs. 2009;70(6):955–963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morgenstern J, Nakashian M, Woolis DD, Gibson FM, Bloom NL, Kaulback BG. CASAWORKS for Families. A new treatment model for substance-abusing parenting women on welfare. Eval Rev. 2003;27(6):583–596 [DOI] [PubMed] [Google Scholar]
- 27.Morgenstern J, Neighbors CJ, Kuerbis A, et al. Improving 24-month abstinence and employment outcomes for substance-dependent women receiving Temporary Assistance for Needy Families with intensive case management. Am J Public Health. 2009;99(2):328–333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hoffman L. State Strategies for Improving the Employment Outcomes of TANF and Low-Income Families Washington, DC: National Governor's Association Center for Best Practices; 2007 [Google Scholar]
- 29.Huston AC, Miller C, Richburg-Hayes L, et al. New Hope for Families and Children: Five-Year Results of a Program to Reduce Poverty and Reform Welfare. New York, NY: Manpower Demonstration Research Corporation; 2003 [Google Scholar]
- 30.Smith LR, O'Campo P, Grason H. Welfare Reform and Women's Health: Opportunities to Advance the Public Response to the Health Needs of Women on Welfare Through Collaboration. Baltimore, MD: The Women's and Children's Health Policy Center, Johns Hopkins University School of Public Health; 2001 [Google Scholar]
- 31.Kneipp S. Integrating nursing services into welfare-to-work transition programs: negotiating the terrain between patient advocacy and political complicity. Paper presented at: American Public Health Association 130th Annual Meeting; November 9–13, 2002; Philadelphia, PA [Google Scholar]
- 32.Milio N. Promoting Health Through Public Policy. Philadelphia, PA: F.A. Davis; 1981 [Google Scholar]
- 33.Olds DL, Eckenrode J, Henderson CR, Jr, et al. Long-term effects of home visitation on maternal life course and child abuse and neglect. Fifteen-year follow-up of a randomized trial. JAMA. 1997;278(8):637–643 [PubMed] [Google Scholar]
- 34.Olds DL, Henderson CR, Jr, Tatelbaum R, Chamberlin R. Improving the life-course development of socially disadvantaged mothers: a randomized trial of nurse home visitation. Am J Public Health. 1988;78(11):1436–1445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kreuter MW, Wray RJ. Tailored and targeted health communication: strategies for enhancing information relevance. Am J Health Behav. 2003;27(Suppl 3):S227–S232 [DOI] [PubMed] [Google Scholar]
- 36.Ryan P, Lauver DR. The efficacy of tailored interventions. J Nurs Scholarsh. 2002;34(4):331–337 [DOI] [PubMed] [Google Scholar]
- 37.Lauver DR, Ward SE, Heidrich SM, et al. Patient-centered interventions. Res Nurs Health. 2002;25(4):246–255 [DOI] [PubMed] [Google Scholar]
- 38.Israel BA, Eng E, Schulz AJ, Parker EA, Methods in Community-Based Participatory Research for Health. San Francisco, CA: Jossey-Bass; 2005 [Google Scholar]
- 39.Wallerstein N, Duran B. The conceptual, historical, and practice roots of community based participatory research and related participatory traditions. : Minkler M, Wallerstein N, Community-Based Participatory Research for Health. San Francisco, CA: Jossey-Bass; 2003:27–52 [Google Scholar]
- 40.Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract. 2006;7(3):312–323 [DOI] [PubMed] [Google Scholar]
- 41.Lutz BJ, Kneipp S, Means D. Developing a health screening questionnaire for women in welfare transition programs in the United States. Qual Health Res. 2009;19(1):105–115 [DOI] [PubMed] [Google Scholar]
- 42.National Center for Health Statistics Division of Health Interview Statistics 2002 National Health Interview Survey (NHIS) public use data release survey description. Hyattsville, MD: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2003 [Google Scholar]
- 43.Lenze SN, Cyranowski JM, Thompson WK, Anderson B, Frank E. The cumulative impact of nonsevere life events predicts depression recurrence during maintenance treatment with Interpersonal Psychotherapy (IPT-M). J Clin Psychol. 2008;76(6):979–987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Beck AT, Steer RA, Brown GK. Beck Depression Inventory-II Manual San Antonio: The Psychological Corporation. San Antonio, TX: Harcourt Brace and Company; 1996:38 [Google Scholar]
- 45.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition. New York, NY: Biometrics Research, New York State Psychiatric Institute; 2002 [Google Scholar]
- 46.Beck AT, Steer RA. Beck Anxiety Inventory Manual. San Antonio, TX: The Psychological Corporation, Harcourt Brace and Company; 1990:23 [Google Scholar]
- 47.Shear MK, Greeno C, Kang J, et al. Diagnosis of nonpsychotic patients in community clinics. Am J Psychiatry. 2000;157(4):581–587 [DOI] [PubMed] [Google Scholar]
- 48.Schulz KF, Altman DG, Moher DCONSORT. 2010 Statement: updated guidelines for reporting parallel group randomised trials. Trials. 2010;11(32):1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.American Public Health Association Public Health Nursing Section The definition and role of public health nursing in the delivery of health care: a statement of the public health nursing section. 1996. Available at: http://www.apha.org/membergroups/sections/aphasections/phn/about/defbackground.htm. Accessed August 25, 1999
- 50.Zimmerman GL, Olsen CG, Bosworth MFA. “Stages of Change” approach to helping patients change behavior. Am Fam Physician. 2000;61(5):1409–1422 [PubMed] [Google Scholar]
- 51.Perz CA, DiClemente CC, Carbonari JP. Doing the right thing at the right time? The interaction of stages and processes of change in successful smoking cessation. Health Psychol. 1996;15(6):462–468 [DOI] [PubMed] [Google Scholar]
- 52.Lazarus R, Folkman S. Stress, Appraisal, and Coping. New York, NY: Springer Publishing Company; 1984 [Google Scholar]
- 53.Antoni MH, Pereira DB, Marion I, et al. Stress management effects on perceived stress and cervical neoplasia in low-income HIV-infected women. J Psychosom Res. 2008;65(4):389–401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Means B, Nigam A, Zarrow M. Autobiographical memory for health-related events. Series 6: Cognition and Survey Measurement, No. 2. Vital Health Stat 6. 1989;6(2):1–37 [Google Scholar]
- 55.Meeting the Competency Challenge in Behavioral Healthcare: The Resource Tool for Behavioral Healthcare Human Resource Professionals Who Must Meet the Rigorous Requirements of JCAHO. Washington, DC: Joint Commission on Accreditation of Healthcare Organizations; 2000 [Google Scholar]
- 56.Kneipp SM, Kairalla JA, Stacciarini J, Pereira D. The Beck Depression Inventory II factor structure among low-income women. Nurs Res. 2009;58(6):400–409 [DOI] [PubMed] [Google Scholar]
- 57.Ware JE, Kosinski M, Turner-Bowker DM, Gandek B. How to Score Version 2 of the SF-12 Health Survey. Lincoln, RI: Quality Metric Incorporated; 2005 [Google Scholar]
- 58.Coffey CS, Kairalla JA. Adaptive clinical trials: progress and challenges. Drugs R D. 2008;9(4):229–242 [DOI] [PubMed] [Google Scholar]
- 59.Coffey CS, Kairalla JA, Muller KE. Practical methods for bounding type I error rate with an internal pilot design. Comm Statist Theory Methods. 2007;36(11):2143–2158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Coffey CS, Muller KE. Exact test size and power of a Gaussian error linear model for an internal pilot study. Stat Med. 1999;18(10):1199–1214 [DOI] [PubMed] [Google Scholar]
- 61.Coffey CS, Muller KE. Properties of internal pilots with the univariate approach to repeated measures. Stat Med. 2003;22(15):2469–2485 [DOI] [PubMed] [Google Scholar]
- 62.Wittes J, Brittain E. The role of internal pilot studies in increasing the efficiency of clinical trials. Stat Med. 1990;9(1-2):65–72 [DOI] [PubMed] [Google Scholar]
- 63.Davidson KW, Rieckmann N, Clemow L, et al. Enhanced depression care for patients with acute coronary syndrome and persistent depressive symptoms: Coronary Psychosocial Evaluation Studies Randomized Controlled Trial. Arch Intern Med. 2010;170(7):600–608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Perini S, Titov N, Andrews G. Clinician-assisted Internet-based treatment is effective for depression: randomized controlled trial. Aust N Z J Psychiatry. 2009;43(6):571–578 [DOI] [PubMed] [Google Scholar]
- 65.Assmann SF, Pocock SJ, Enos LE, Kasten LE. Subgroup analysis and other (mis)uses of baseline data in clinical trials. Lancet. 2000;355(9209):1064–1069 [DOI] [PubMed] [Google Scholar]
- 66.Miranda J, Green BL, Krupnick JL, et al. One-year outcomes of a randomized clinical trial treating depression in low-income minority women. J Consult Clin Psychol. 2006;74(1):99–111 [DOI] [PubMed] [Google Scholar]
- 67.Practice Guideline for the Treatment of Patients With Major Depressive Disorder. Washington, DC: American Psychiatric Association; 2000 [PubMed] [Google Scholar]
- 68.Lexis MA, Jansen NW, Huibers MJ, et al. Prevention of long-term sickness absence and major depression in high-risk employees: a randomised controlled trial. Occup Environ Med. 2010. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 69.Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health. 2006;27:1–28 [DOI] [PubMed] [Google Scholar]