Abstract
Petroleum is used widely in health care—primarily as a transport fuel and feedstock for pharmaceuticals, plastics, and medical supplies—and few substitutes for it are available. This dependence theoretically makes health care vulnerable to petroleum supply shifts, but this vulnerability has not been empirically assessed. We quantify key aspects of petroleum use in health care and explore historical associations between petroleum supply shocks and health care prices. These analyses confirm that petroleum products are intrinsic to modern health care and that petroleum supply shifts can affect health care prices. In anticipation of future supply contractions lasting longer than previous shifts and potentially disrupting health care delivery, we propose an adaptive management approach and outline its application to the example of emergency medical services.
Modern medicine relies on petroleum, particularly to transport patients, staff, and supplies, and to manufacture supplies and pharmaceuticals.1,2 This reliance is particularly heavy in the United States, which consumes petroleum disproportionately on a per capita basis compared with other nations. There is increasing consensus that petroleum production has already declined or will soon begin to decline and that constrained supplies will adversely affect most sectors, including health care. (Those unfamiliar with this body of evidence should consult the introductory article in this special issue by Schwartz et al.3) Several authors have highlighted health care's exposure to declines in petroleum production, but the issue has received little attention from economists or policymakers, and little has been done to further assess and manage the potential risk.
In particular, there is no publicly available account of health care's utilization of petroleum-based products, and there have been no econometric studies evaluating historical associations between petroleum production and health care costs. While risk management activities are justified based on the precautionary principle, inattention to this issue has impeded interpretation of and action on the existing preliminary evidence. For instance, a concerned health system administrator who wants to assess a hospital's vulnerability to decreasing petroleum supplies and prioritize risk management strategies has no recommendations to follow.
We attempt to address these concerns within the constraints of a limited evidence base. We first explore evidence of the health care system's vulnerability to petroleum shortages, decomposing vulnerability into exposure, susceptibility, and resilience. We explore exposure by evaluating the magnitude of the US health care system's petroleum dependence, focusing on transport, medical plastics, and pharmaceuticals. We explore susceptibility by analyzing historical associations between the prices of petroleum and of health care goods and services. We explore resilience by assessing system disturbances from historical price shocks.
We then propose an adaptive management framework for engaging the issue. Adaptive management is useful for managing dynamic systems whose complexity complicates linear management decisions. The framework emphasizes stakeholder engagement, modeling, and iterative decision-making, putting a premium on learning about the system being managed and its responses to management decisions. After introducing the framework, we illustrate its application to an emergency medical services (EMS) system as an example of how this approach can be used to manage the health care system's extensive, if latent, risk.
HEALTH CARE'S VULNERABILITY TO PETROLEUM SUPPLY SHIFTS
In risk management frameworks, vulnerability is often broken down into exposure, susceptibility, and resilience.4-7 These components offer a useful starting point for empirically assessing health care's vulnerability to petroleum scarcity.
EXPOSURE
Health care constitutes 16% of the US gross domestic product—the highest such percentage in the Organization of Economic Cooperation and Development, in which the average is 8.9%.8 Given that the United States consumes roughly one quarter of the world's oil production and emits approximately 8% of the world's greenhouse gases,9 it is safe to conclude that health care in the United States consumes a large amount of petroleum and that health care's exposure to petroleum supply shortages is likely significant. Quantifying this exposure is difficult, however. Energy inputs and petroleum-based inputs into health care have not been a topic of investigation in the health or economic literature. Moreover, data on health care transport and medical plastics are scarce; there are few sources of data on the former, and most sources of data on the latter are proprietary. Similarly, very little has been published on petroleum inputs into other medical supplies and pharmaceuticals. Within these constraints, we present the results of a literature review and de novo analysis of available data.
Transport
In 2009, 72% of petroleum consumed in the United States was consumed as transport fuel.10 Transport is also the leading category of petroleum use in the health care sector, which relies on petroleum-based fuels to move staff, patients, and medical supplies.
Transport for health care staff.
Of the three types of health care transport, staff transport accounts for the majority. Health care employed 14.3 million people in 200811 suggesting more than 3.5 billion round-trip work commutes for health care staff, or a total of approximately 7.2 billion staff trips per year.
Health care in the United States is decentralized and is provided in a diverse range of settings; in 2008 there were a total of 595 800 different health care establishments.11 Clinics constituted 83% of all health care sites and employed 43% of health care staff; hospitals constituted 1% of establishments but employed 35% of staff; and nursing and residential care services constituted 11% of establishments and 23% of employment.11 Approximately half of nonhospital health care establishments employed fewer than 5 workers, and more than 70% of hospitals had more than 1000 employees each.11
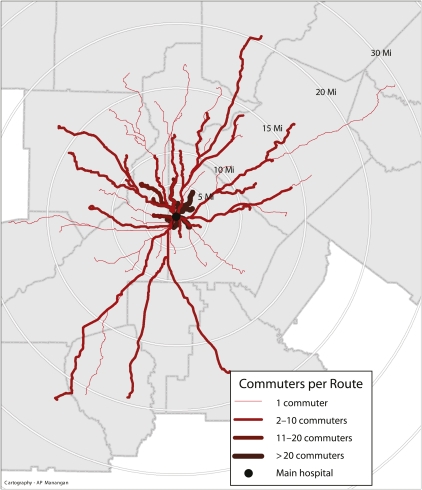
There are no reported figures for commute distance stratified by occupation or industry, so the travel requirements of health care staff are unknown. To begin filling this gap, we analyzed commute distances for employees of a large academic health system in the Southeast that includes 4 inpatient hospitals and a wide range of outpatient facilities. The results of this analysis are presented in the box on this page which includes a map depicting commute patterns for employees commuting to the system's flagship hospital (Figure 1). Our findings reinforce the conclusion that transport requirements for health care staff are significant.
FIGURE 1.
Employee commuting routes to main hospital: Emory HealthCare, Atlanta, GA, 2011.
Transport for health care extenders and patients.
Ancillary services that extend care into patient homes constitute a significant and growing component of the health care system. Home health care employed just less than 1 million people in 2008, for instance, and employment in this sector is projected to expand 46% from 2008 to 2018.11 Other services in this category include home hospice, EMS, and other transport services. In 2006, 12 million patients were served with 428 million home visits.13,14 The National Association for Home Care & Hospice estimated that home health and hospice providers drove 4.8 billion miles in 2006, not including staff commutes to and from work.13,15 EMS provided 18.4 million ambulance transports to hospital emergency departments in 2007.16 Although distances traveled and fuel used are not routinely tracked, these transport services are fuel intensive.
We know relatively little about patient transport, but we do know that patients tend to travel farther for specialist care and that primary care utilization is inversely related to distance.17 Also, distance is inversely related to access for utilization18 and screening,19,20 and distance factors into treatment decisions for therapies with significant transport costs (e.g., whether to pursue breast-conserving surgery or mastectomy with postoperative radiation therapy).21 However, there are no published summaries of patient transport requirements overall.
Estimates of trips made by patients are lower than are those for staff but are still large. Estimates vary significantly by source.
The National Center for Health Statistics (NCHS) reported that in 2006 there were 1.1 billion ambulatory health care visits, which accounted for 97% of all provider encounters, including outpatient visits, home health and hospice visits, and hospital admissions.22 Each of these visits presumably generated 1 round trip. Thus, on the basis of the NCHS statistics, we estimate that there were at least 1.1 billion round trips, or a total of 2.2 billion trips, for ambulatory health care in 2006.
The US Department of Transportation's National Household Travel Survey (NHTS) provides detailed household travel information for a nationally representative sample stratified by trip purpose.22 In 2009, 3.8 billion trips were made to access health care and dental services—1.6% of all household travel—for a total distance of 38.3 billion miles. Only 3 million of these trips (0.08%) involved public transit. The average travel distance to access health care services was 10.3 miles.
The NHTS estimate of 3.8 billion trips to access health care services is 75% larger than the NCHS estimate noted above (2.2 billion). Differences in sampling and definitions (e.g., including dental care) are likely the cause: the NCHS estimate is based on samples from health care sites, whereas the NHTS estimate is based on self-reporting in household surveys, which likely encompasses a wider range of health-care related activity.
In sum, there are extensive transport requirements for staff and patients in the health care sector. Transport requirements are significantly greater for staff than they are for patients. In our analysis of staff transport in a large academic health care system, presented in the box on this page approximately 11 750 staff traveled approximately 78.6 million miles annually, reinforcing this conclusion. Assuming an average automobile gas mileage of 22.6 miles per gallon,23 this health care system alone required 3.8 million gallons of fuel for staff transport for 1 year. The overall estimate of transport needs would of course increase further if supply transport were included.
Plastics and Pharmaceuticals
Plastics and pharmaceuticals are primarily derived from petrochemicals, and there are relatively few substitutes for petroleum inputs into these products.24 Health care's reliance on petroleum for plastics and pharmaceuticals is a longstanding concern, first discussed widely after the 1973 oil embargo.25 As with transport, there is little literature on the volume of petrochemical inputs into plastics and pharmaceuticals used for health care. In contrast with transport, however, there are no publicly available data to analyze. Thus, we explore the existing literature and attempt to generate broad estimates of petroleum usage in these categories.
Plastics.
Plastics are central to the antiseptic model of modern health care and are used in a wide range of medical devices, supplies, and packaging. Most plastics are derived from petroleum, although the proportion of all petroleum used for plastics is relatively small. In the 1970s approximately 5% of petroleum was used for plastics manufacture,26 a proportion that has remained relatively stable.10 In the 1970s 4% of all plastics were used in the health care sector,27 and an estimated 0.2% of petroleum used in the United States was for medical plastics.25 We have found no estimates more recent than these.
The oil embargo of the 1970s caused inflation in the price of plastic feedstocks, delays in their delivery to factories, and subsequent delays in finished product delivery to health care facilities in the United States25 and Britain.28,29 This level of exposure remains essentially unchanged. Although no current figures are available, Schlechter estimated that health care in the United States will use more than 3.4 billion pounds of plastics in 2010.30 Using a recent estimate of 104 billion pounds of plastics resin consumption in 2008 as a denominator,31 it would seem that the market share of medical plastics is comparable to that of the 1970s.
A smattering of articles have discussed medical plastics over the last several decades,32–37 including concerns over supply shortages,38,39 but there have been no recent contributions to this literature. Neither are there data on the distribution of plastic use in the health care system. Presumably, plastic use is heaviest in procedurally intensive health care environments (e.g., hospitals and surgical facilities). In 2006 there were 34.9 million hospital discharges, approximately 3% of total health care visits,40 but these visits likely account for a disproportionate share of plastic medical supply use.
No literature directly addresses the possibilities for plastic substitution, but such options appear to be rare. Alternative feedstocks are in development and might be brought into production if necessary, albeit with significant infrastructure costs.41
Pharmaceuticals.
Pharmaceuticals are vital to health care but represent a relatively small proportion of total petroleum usage. Just less than half of all Americans take prescription medications at any point in time, and approximately 2.3 billion medication orders or prescriptions were written in 2006.42 Approximately 75% of ambulatory visits involve medication administration or prescription.42 Analgesics, antidepressants, antihyperlipidemics, antidiabetic agents, antiemetics, and antihistamines are the leading medications prescribed.42 Again, there are no systematic reviews on petrochemical inputs into commonly prescribed medications. Approximately 3% of petroleum production is used for pharmaceutical manufacture, but nearly 99% of pharmaceutical feedstocks and reagents are derived from petrochemicals (oral communication, Joyce Easter, PhD, Virginia Wesleyan College, December 2010). Petrochemical feedstock costs are likely a relatively small share of total pharmaceutical costs, however, which are dominated by marketing, research, and development.
Summary of Exposure
These analyses suggest that most health system components are heavily reliant on petroleum and are thus significantly exposed to petroleum supply shifts. How this exposure will manifest depends on several factors, including the timing of peak petroleum production, the shape of the production curve's apogee (e.g., whether it will have a single peak, be shaped like a plateau, or undulate before dropping), the rate of production decline, the extent to which producing nations retain their domestic production, and shifts in how petroleum is allocated among various economic sectors. Expert consensus is agnostic on the shape of the production curve at the time of the peak, but holds that peak production will occur within a decade (if it has not occurred already) and that depletion rates will be on the order of 4% to 6% per year.43,44 The availability of substituting technologies such as electric vehicles, biofuels, and cellulosic polymers at the scale required for widespread substitution is far from certain.45–48 Some argue that innovation and substitution will be inadequate even over the long term.49 Absent aggressive efforts to scale up production of product substitutes, exposure probability for health care is high.
SUSCEPTIBILITY AND RESILIENCE
Susceptibility is a measure of exposure impact, and resilience is a measure of the degree to which a system retains its function in the face of shocks to its organization and function. Historical evidence would be helpful for exploring health care's susceptibility and resilience to petroleum supply shifts. However, very little of this historical evidence has been assembled. The oil embargo of the 1970s increased medical plastic costs, but the impact of oil supply shifts on health care prices has not been evaluated. An examination of the dependence of health care price on petroleum supply would show whether the system has historically demonstrated susceptibility. This is an important determination to make, although the impact of transient supply shifts is only a fair proxy for the potential impact of a prolonged supply contraction.
We can deduce many aspects of the relationship between short-term supply contraction and health sector impacts. Historical shortages have unfolded over months to years, so any consequent impacts should be similarly short term. There are substantial supply-chain reserves that take months to deplete, and pricing contracts delay price shifts, so delayed impacts seem likely. Also, petroleum is only one of several production factors, so the impacts of supply shortages would probably be dampened.
To evaluate for historical impacts we use 2 parallel approaches: we look at historic price shocks (which correlate with supply contractions), and we examine a time series of petroleum and health care prices from 1970 to 2010.
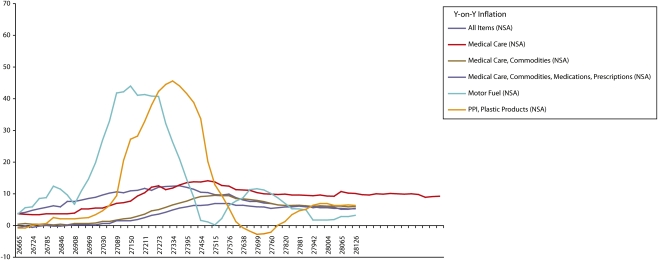
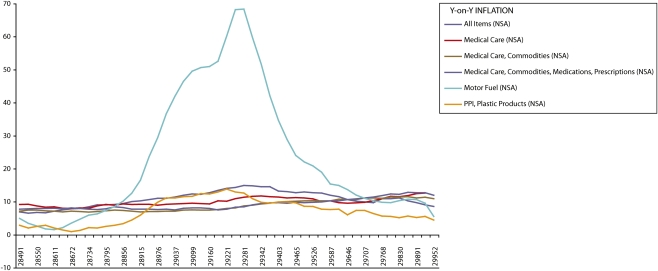
Health Care Price Inflation After Petroleum Supply Shocks
We graphed the trajectories of year-on-year inflation in several nonseasonally adjusted price variables: motor fuel, health care, health care services, health care commodities, prescription medications, plastics, and the consumer price index. All variables were indexed to a 1982–1984 base. We obtained consumer price index data from the US Bureau of Labor Statistics (available at: http://www.bls.gov/cpi/data.htm) and graphed them using Excel. We examined 5 periods corresponding with historical supply shocks: 1973–1974; 1978–1980; 1990–1991; 1999–2001; and 2006–2008. Results for the first 2 periods are presented in Figures 2 and 3. Figures depicting the results for the last 3 shocks, which are characterized by greater variability and declining associations between oil and health care prices, are depicted in Figures S1, S2, and S3 (available as supplements to the online version of this article at http://www.ajph.org).
FIGURE 2.
Year-on-year inflation for selected consumer price index variables: United States, 1973–1977.
Note. NSA = nonseasonally adjusted; PPI = producer price index. To help depict trends, the figure presents additional years before and after the price-shock period.
FIGURE 3.
Year-on-year inflation for selected consumer price index variables: United States, 1978–1982.
Note. To help depict trends, the figure presents additional years before and after the price-shock period.
As expected, there often appears to be an association between decreased petroleum supply (indicated by a rise in inflation in motor fuel prices, which covary closely with petroleum supply), a rise in the price of plastics, and, lagged by several months, the prices of health care commodities and health care as a whole. The consumer price index, by comparison, serves as a control and generally shows less sensitivity. As expected, the increase in health care inflation is blunted compared with the rise in the price of plastics. These patterns are most evident in the first oil price shock in the 1970s, and they diminish over time. As the latter figures illustrate, over time there is increasing volatility in oil price inflation that makes it difficult to discern a clear pattern in later shocks.
There is little likelihood that reverse causation is driving these observations because health care delivery consumes a relatively small proportion of total petroleum output and does not set demand for petroleum-based products. Moreover, oil supply shifts are unrelated to health care delivery, so there is little likelihood that this association is significantly confounded by an unexamined factor. The most likely reasons for the observed association are that health care delivery is petroleum dependent and that its cost is sensitive to shifts in petroleum supply.
The apparent decline in the magnitude of effect is important to note, however. This is likely because of the decreasing contribution of both transport and supply costs to overall health care costs. Health care is a service industry, and labor costs are increasingly dominant in its price structure, as shown by the petroleum–health care price ratio presented in Table 1. Overall, the analysis suggests an association between petroleum supply and health care prices that is inconstant over time because the costs of other health care components have risen disproportionately.
TABLE 1.
Key Drivers of the Relationship Between Petroleum Supply and Health Care Price: United States, 1973–2008
| Shock Period | Shock Duration, Months | 6-Month Average Annual Inflation Rate for Health Care Prices Before Shock, % | Ratio of Petroleum Price to Health Care Price 6 Months Before Shock | Maximum 1-Month Annual Inflation Rate for Petroleum Prices During Shock, % | Month of Shock in Which Maximum 1-Month Petroleum Price Inflation Occurred | Maximum 1-Month Annual Inflation Rate for Health Care Prices During or After Shock, % | Month in Which Maximum 1-Month Health Care Price Inflation Occurred | Delay Between Maximum 1-Month Inflation in Petroleum Price and Maximum Health Care Price, Months |
| 1973–1974 | 37 | 5.8 | 0.15 | 354.9 | June 1974 | 13.9 | April 1975 | 12 |
| 1978–1980 | 22 | 9.0 | 0.35 | 78.6 | February 1980 | 12.5 | December 1981 | 22 |
| 1990–1991 | 23 | 7.4 | 0.10 | 69.1 | December 1990 | 9.7 | January 1991 | 1 |
| 1999–2001 | 20 | 3.5 | 0.03 | 156.7 | February 2000 | 4.8 | November 2001 | 21 |
| 2006–2008 | 12 | 4.1 | 0.08 | 85.1 | June 2008 | 3.7 | March 2010 | 21 |
Note. Shock periods begin in a month in which the 1-mo annual inflation rate for petroleum increased more than 20%. Shock periods end when prices started a steady decline.
Time-Series Analysis of Petroleum Supply and Health Care Prices
We constructed an autoregressive distributed lag model to evaluate the association between petroleum and medical care prices with time lag. Our independent variable was monthly inflation in the price of nonseasonally adjusted imported crude oil, obtained from the Web site of the US Energy Information Administration (available at: http://www.eia.doe.gov). These data only go back to 1974, so we used the official price of Saudi light crude oil as a proxy for earlier years.50 Our dependent variables were month-to-month inflation in consumer price indices for medical care, calculated using data downloaded from the US Bureau of Labor Statistics. When using a time-series design, all variables should be stationary. To achieve this, we differenced both the dependent variable and the independent variable once, and we confirmed stationarity using the augmented Dickey–Fuller test.
The basic model specification is:
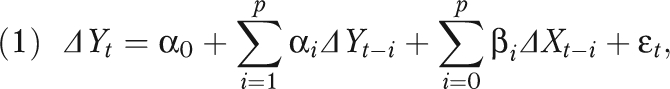 |
where ΔYt is the month-to-month difference in medical care price inflation and ΔXt is the month-to-month difference in oil price inflation. We included lagged values for the independent variables to estimate the effect of oil price variation in previous months on present medical care price inflation. Lagged dependent variables were included to adjust for serial correlation, and we adjusted seasonality by adding monthly dummies.
The analysis revealed that from 1972 to 1980, a 1% increase in monthly oil price inflation resulted in a 0.03% increase in monthly medical care prices at 8 months' lag, with an elevation sustained through 20 months. Full results are shown in Table S1 (available as a supplement to the online version of this article at http://www.ajph.org). The coefficients in Table S1 represent the magnitude of the association between a 1% increase (decrease) in monthly oil price inflation and the resulting percentage increase (decrease) in the dependent variables. The monthly lag structure for the relationship between oil price inflation and medical care price inflation from 1972 to 1980 is illustrated in Figure S4 (available as a supplement to the online version of this article at http://www.ajph.org).
The principal findings of this analysis support our hypothesis: oil price inflation had a modest impact on health care price inflation, with some time lags. Also, the impact on medical commodity prices started later than did the impact on other medical care prices. Finally, both the magnitude and statistical significance of the impact were much larger in the 1970s than after the 1980s, when we observed no effect.
Susceptibility and Resilience, Short Term vs Long Term
Our analyses suggest that, historically, health care shows moderate susceptibility to petroleum supply shifts but also resilience: when petroleum supply declined over the short term, health care prices were affected, but the system was not significantly disrupted. Impacts might be more marked if some of the costs sensitive to petroleum supply, such as transport for health care personnel and patients, were internalized in the metrics of health care price.
Care should be taken in extending these results to long-term petroleum supply contraction, which likely is a categorically different exposure. Factors that affect susceptibility to long-term shifts include exclusive dependence on petroleum inputs, the potential for supply chain localization, and the potential for product substitution. Other susceptibility factors derive from contextual and cultural issues that drive system behavior at larger geographic and time scales. For instance, overall susceptibility is likely increased by an emphasis on fee-for-service care, which is associated with excess health care use,51 and an emphasis on secondary and tertiary interventions over primary care, which drives use of several different categories of costly and often petroleum-intensive resources.51,52
Just as the health care system may be more susceptible in the long term, it may also be less resilient. Factors that drive short-term resilience, such as supply reserves, will be overwhelmed by longer-term shocks. In the case of longer-term contraction, redundancies within the system and the capacity to localize production factors will be more important. System coordination and flexibility can also facilitate product substitutions. For instance, the capacity to substitute telemedicine visits for some face-to-face care would enhance resilience to petroleum supply shocks. Localization of resources, such as reliance on nearby primary care over distant specialty services, could reduce transport costs. Other examples of factors that could enhance long-term resilience include localization of food supplies and human capital resources for hospitals and health care systems.
Enhancing resilience may be slow and laborious. Take, as 2 interrelated examples, the challenges of creating a resilient supply of medical plastics and pharmaceutical feedstocks. Biodegradable feedstocks for plastics are increasingly available.53 Biodegradable items such as gloves, tubing, gowns, implants, drug delivery devices, and hernia repair materials are in development,54 as are bioplastics, whose components are not petroleum based and are derived from renewable raw materials.55 There is great potential for these innovations56; however, none of these technologies are in wide use in health care yet. According to one source,
Cost concerns, regulatory wariness, minimal selection, and a lack of strong demand from end-users have deterred medical device manufacturers from pursuing the use of more environmentally friendly plastics.53
Although sustainability is an acknowledged goal of the chemical and pharmaceutical industries,57 few pharmaceutical companies have adopted green chemistry principles or renewable feedstocks on a large scale.58
Summary of Health Care's Vulnerability
All told, the health care system exhibits high exposure, moderate susceptibility, and high resilience to short-term supply shocks; long-term shocks likely pose a more difficult challenge. The uncertainties associated with the problem, and the possibility that longer-term supply contraction may overwhelm short-term resilience, lead us to suggest the use of an adaptive management framework to engage the issue.
ADAPTIVE MANAGEMENT OF HEALTH CARE'S PETROLEUM USE
All modern health care is complex; the US health care system, with its structural diversity, numerous payers, and extensive bureaucracy, is even more complex than are others in the developed world. As Sterman and others have noted, complexity bedevils evidence-based policymaking by slowing evidence accumulation, evidence interpretation, and evidence translation.59 These complications have been termed “policy resistance” (i.e., “the tendency for interventions to be delayed, diluted, or defeated by the response of the system to the intervention itself”).60 Health care has areas of significant potential policy resistance that are important to consider.
Some of the system's most significant structural aspects were unintended. The current employer-based insurance system was a consequence not of intentional policy but of World War II wage controls that led Henry Kaiser and other employers to lure workers with health insurance.61 This arrangement has endured despite perverse incentives that limit coverage for sick patients. The system has since integrated other powerful incentives, such as fee-for-service pay schedules, that reinforce its interventional orientation, raising long-term costs.62 These features of the system promote inefficiency and may amplify vulnerability to petroleum supply contraction.
Policy resistance is an issue for managing vulnerability to petroleum supply shifts. Consider the policy proposals issued by the National Association for Home Care & Hospice in response to rising fuel costs in 2008. The association called for preservation of annual inflation updates for home health and hospice as provided for under Medicare, reinstatement of a rural add-on for home health services provided to rural patients, exemption from federal gasoline taxes, recognition of telehealth visits as equivalent to in-home visits, and retraction of Medicare regulatory reimbursement cuts for home health providers.63 Some of these policies would reduce vulnerability in the short term but would exacerbate long-run vulnerability by insulating providers from innovation pressures. Others, such as the telehealth emphasis64 and partnership with a fleet management service,65 would enhance resilience.
In complex systems with significant potential for policy resistance, adaptive management has emerged as a viable management strategy. Adaptive management is a framework for managing systems that are difficult to manage in a linear fashion. Such systems have complex dynamics that are difficult for managers to intuit, and they tend to have many different stakeholders with varying perspectives and priorities66; these characteristics interact dynamically to affect management outcomes.67 Adaptive management originated in the natural resources sector68 as an iterative process that acknowledged complexity and uncertainty, emphasized ongoing learning, and allowed for continuous stakeholder input.69 It has enjoyed considerable success, although some problems have resulted from implementation in inappropriate contexts.70
Dynamic models have been used to facilitate adaptive management in health systems,71–73 but petroleum supply issues have not been incorporated into these models. Apart from a handful of examples, the framework is relatively unfamiliar to public health, though its components are staples of public health practice.67,69,74–76
The Adaptive Management Framework
The National Research Council emphasizes 6 primary elements of adaptive management77:
management objectives that are regularly revisited and accordingly revised;
a model of the system(s) being managed;
a range of management choices;
monitoring and evaluation of outcomes;
a mechanism (or mechanisms) for incorporating learning into future decisions;
a collaborative structure for stakeholder participation and learning.
Similarly, there are 6 steps in the process, diagrammed in Figure S5 (available as a supplement to the online version of this article at http://www.ajph.org):
assessment;
planning;
implementation;
monitoring;
evaluation;
adjustment.
The process tailors strategies to particular systems and situations.78 Because of the resources required to assemble system models, it is particularly suited to managing larger systems. Stakeholder engagement is pivotal to its success. A wide range of producers and a diverse range of personnel are integral to the process of providing health care, and all need to be included to make adaptive management of the process a success. Those who manage health care policy and shape the health care system over time, ranging from academics to third-party payers, also need to be included.
Stakeholders are likely to approach the issue from a wide range of perspectives. Health care personnel, particularly those whose commuting costs consume a larger proportion of their income, will have different priorities from facility managers. Health care extenders may lobby for increased reimbursement of travel expenditures, whereas third-party payers are likely to advocate for incentives to increase efficiency in petroleum-intensive activities such as home health services and emergency medical transport of patients. Inclusion of a wide variety of stakeholders and identification of a common set of principles and goals among them is key.
HYPOTHETICAL APPLICATION OF THE ADAPTIVE MANAGEMENT FRAMEWORK
The application of the adaptive management framework is perhaps best conveyed by example. We use a hypothetical EMS system to illustrate how the process might be applied.
First, all the relevant stakeholders for the system should be engaged. In the EMS example, this includes the various organizations responsible for emergency response, e.g., the local fire department, EMS organizations, and EMS medical directors. Depending on how the system is organized (i.e., whether it is administered and funded by a municipality, county, or other entity), the agencies responsible for funding and oversight should also be included, as should EMS personnel. Finally, local residents and the local health department should give input. Depending on how the EMS organizations secure their fuel supplies, vendors and vehicle service facility representatives should also be present.
Assessment
The assessment phase is primarily concerned with generating consensus on management goals, exploring system vulnerabilities, and feeding this information into a model to facilitate management activities.
Management goals.
In the case of EMS, the primary system goal is the prompt field stabilization of acutely ill and injured patients and their safe transport to a facility where they can receive definitive care. Stakeholders are likely to state a number of other priorities, including preservation of existing networks and responsibilities (fire departments, for example, often focus on medical response and may be reluctant to relinquish that responsibility). The ultimate goal of the adaptive management process might be a hybrid of increasing operational efficiency and increasing system resilience while operating within existing infrastructural constraints.
Exploring system vulnerabilities.
Nearly all transport activities in EMS systems as currently configured are dependent on petroleum-based fuel, making EMS systems highly vulnerable health system components. An estimate of fuel use is important to assessing exposure. Here we use national-level data to outline how this might be done. This process requires some assumptions because there are no comprehensive data.
In 2006 there were 18.4 million ambulance transports to emergency departments.15 Estimates in the literature for patient transport from scene to hospital range from 4 to 8 miles; studies suggest that the distance from deployment to scene is half the transport distance.79,80 Assuming a 3-mile deployment, a 6-mile transport, and a 3-mile return to base, and assuming gas mileage of 6 miles per gallon for EMS response in an urban environment,81 we derive an estimate of 36 800 000 gallons of fuel annually for patient transport. This is a significant underestimate of total fuel use given that many systems employ multiple vehicles per call and that staff and supply transport are not included; but this estimate gives a general sense of EMS's dependence on fuel for patient transports. Moreover, in rural counties or urban environments with high levels of health care utilization but relatively few providers, ambulance transport distances are much higher, by as much as a factor of 4.82
As for other susceptibility factors, the fuel supply chain is quite long, stored supply is minimal, and local production is unlikely, though local biodiesel supplies could be harnessed. Product substitution in the form of improved fuel efficiency or alternative fuels is possible but would require significant capital outlays. Some large EMS organizations have improved fuel efficiency in response to fuel price increases,83 but published information on other innovations is rare.
Modeling.
Model construction should begin during the assessment phase. Models can vary widely, from simple diagrams and mental models to complex system dynamics models parameterized from experience and expert knowledge. The requirement of using a model to facilitate system management should not deter system managers from engaging the adaptive management process, because the primary goal is to bring together stakeholders to make collective decisions in an iterative process, not to generate a system model. That said, it is important to revisit and revise the model with successive iterations of the process because the better the model characterizes the system and its behavior—including its responses to management decisions—the more helpful the model will be in guiding management decisions.
Planning
The planning stage is primarily concerned with identifying management options and specific points of leverage and choosing specific management options to pursue.
Identifying management options and specific points of leverage.
Management options for an EMS system include interventions at the level of individual EMS vehicles and interventions in overall system organization.
Interventions at the vehicle level include purchasing vehicles with increased fuel efficiency or hybrid liquid fuel–electric drive vehicles, switching to alternative fuels such as liquid petroleum gas or biodiesel,84 and switching to different vehicle types (e.g., motorcycles for first response). Other substitutions, such as conversion to hybrid or plug-in electric vehicles, are potentially feasible but would require large capital outlays and other system features to maintain performance standards. These substitutions are also subject to limitations in the supply of nonrenewable fossil fuels used to generate electricity in many locales.
Interventions at the system level might include changes in deployment strategy (e.g., from dynamic deployment, in which ambulances roam according to demand, to fixed deployment, in which they are stationed at posts) and strategies to reduce fuel usage while dynamically deployed. Other interventions might include decreasing the number of vehicles deployed in response to an EMS call and development of a system of nonurgent medical transport (which is typically more fuel-efficient) to focus EMS resources primarily on truly urgent needs. Increasing the use of telemedicine is another possible intervention that has the potential to reduce demand for EMS transports, particularly from nursing homes to emergency departments85; reducing rates of patient transport by air is another, although for severely ill and injured patients, indications must trump fuel-use concerns.86
In all of these cases, identifying points of leverage is important, which will depend on the particular system being managed. For instance, in many EMS systems ambulance mileage could be improved relatively easily. Another point of leverage may involve focusing services on truly urgent needs and shifting remaining demand to more fuel-efficient nonurgent transport.
Choosing specific management options to pursue.
The choice of management options should be based on the needs and priorities of system managers and stakeholders. In this process it is important to consider ancillary costs and benefits of the various management options in an effort to perform a more comprehensive cost-benefit calculation. For instance, increasing ambulance fuel efficiency reduces EMS vulnerability to rising fuel prices and cuts operating costs. Replacing some first-responder vehicles with motorcycles can improve response time87,88 but must be balanced against the safety of EMS personnel.89 Another important consideration is the life-cycle energy cost associated with replacing a vehicle fleet and making other significant infrastructure changes. Throughout the process, it is important to note that adaptive management is an iterative process, and more ambitious management options can be deferred if appropriate.
Implementation, Monitoring, Evaluation, and Adjustment
There is no predefined time period for implementation, but typically management options will be implemented over a course of months to years. Implementation is primarily the responsibility of system managers, but it is important to maintain close contact with stakeholders during implementation. It is also important to consider how evaluation will take place and to institute monitoring and evaluation strategies while interventions are being rolled out.
As noted, the outcomes to be monitored should be outlined in the assessment phase. Methods for conducting monitoring should be addressed in the planning phase, and monitoring systems should be put in place during implementation. The monitoring phase thus primarily consists of collection of data that will be used during evaluation. Data to be monitored will likely include process indicators to determine the success of the planning and implementation phases, and outcomes related to management goals. Monitoring should track data on system performance and vulnerability to petroleum scarcity. For instance, in a system that replaces its fleet with more fuel-efficient vehicles, it would be important to track impacts on fuel efficiency, maintenance costs, operational safety, and reliability. In another example, if a policy is put in place to reduce the time ambulances spend idling while deployed in the field, it might be important to monitor EMS staff comfort while deployed and staff behavioral adaptations to new policies (e.g., parking their vehicles and seeking climate-controlled environments, which may affect their response time). Importantly, the data collected during the monitoring phase should facilitate learning about the system and its responses, to facilitate future decision-making.90
Evaluation for adaptive management is no different from traditional program evaluation, except that it should address the range of concerns that stakeholders identify as priorities. In certain adaptive management approaches that use complex modeling and multicriteria decision analysis,91 more complex evaluation methods that use Bayesian statistics are often employed,75,92,93 but this need not be the case for more relatively straightforward management processes.
Adjustment, a key phase, is the point in the cycle when evaluation results are collated and presented to stakeholders, and the next phase of the cycle is engaged. In this phase learning is consolidated, and new questions and management goals are generated. Additional relevant information external to the system being managed—such as updated petroleum supply projections, alternative fuel options, novel telemedicine methods, and other developments that could affect the system's structure and performance—should be integrated into the process during adjustment and the cycle's next assessment phase.
Modeling Considerations
As noted previously, adaptive management is typically facilitated by models that are adjusted continuously during the process. These models can be simple or quite complex. For more complex modeling efforts focused on the health care system as a whole, a system dynamics model would be most effective.59 Such approaches have been applied to the petroleum industry,94 various public health71,72 and medical problems,95 and health reform strategies,73 but not to petroleum use in health care. A dynamic model could help identify the potential reverberations and unintended consequences of proposed interventions, provide a more solid footing for risk evaluation,96 and allow policymakers to anticipate and minimize resistance to evidence-based policymaking.97,98
CONCLUSIONS
The health care system is vulnerable to petroleum supply shifts as a result of its widespread exposure and significant susceptibility. Historically, health care has been resilient to short-term supply shifts, but this resilience may deteriorate with longer-term supply contraction. In such an event, impacts will be felt on local, regional, and national scales, and the system's organizational structure may be challenged.
The adaptive management framework presented here may be useful for engaging these concerns, but health care is limited in its ability to promote wider systemic change. Health care is deeply entwined with other economic sectors, and the peaking of conventional petroleum production is likely to have profound economic, policy, and geopolitical ramifications that extend well beyond health care's relatively small orbit. Many structural factors exacerbate the US health care system's vulnerability to petroleum scarcity, from reliance on employer-based insurance to a procedurally oriented third-party-payer system. The effect of petroleum scarcity on health systems, and their response to those effects, will ultimately take place within this broader context. Here we have discussed health care largely as if it were an isolated entity, and this is a valid approach at a certain level of analysis. But health care is obviously a piece of a much larger puzzle, and changes to petroleum consumption within health care will not happen in isolation from larger social and political commitments (or the lack thereof).
Managing these issues within the health sector is likely to be difficult, given health care's size, decentralization, multiple stakeholders, and complexity; but it is nevertheless imperative. With visionary, activist leadership and support from outside the health sector, the necessary transformation could already be under way when petroleum production begins to decline, allowing the health care system to remain resilient. The longer it takes for adaptation efforts to begin, however, the more the response will be shaped by exigency, and the more likely it is that policy resistance will undermine management efforts, potentially compromising the system's capacity to maintain population health.
Acknowledgments
The authors would like to acknowledge Arie Manangan for his assistance with cartography. We would also like to acknowledge Ned Becker, Howie Frumkin, David Galbraith, Cindy Parker, Brian Schwartz, and 5 anonymous reviewers for their helpful review comments.
Human Participant Protection
With the exception of the analysis of commuter patterns, the analyses presented here were secondary data analyses using deidentified data and were therefore exempt from protocol approval. The commuter travel analysis used deidentified data aggregated to the zip code level, and the Emory University institutional review board exempted the commuter travel analysis from protocol approval.
References
- 1.Frumkin H, Hess J, Vindigni S. Peak petroleum and public health. JAMA. 2007;298(14):1688–1690 [DOI] [PubMed] [Google Scholar]
- 2.Frumkin H, Hess J, Vindigni S. Energy and public health: the challenge of peak petroleum. Public Health Rep. 2009;124(1):5–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schwartz BS, Parker CL, Hess J, Frumkin H. Public health and medicine in an age of energy scarcity: the case of petroleum. Am J Public Health. 2011:101(9):1560–1567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.United Nations Disaster Relief Organization Mitigating natural disasters: phenomena, effects, and options. : Manual for Policy Makers and Planners. Geneva, Switzerland: United Nations; 1991:11–14 [Google Scholar]
- 5.de Boer J, Dubouloz M. Handbook of Disaster Medicine. Utrecht, the Netherlands: International Society of Disaster Medicine; 2000 [Google Scholar]
- 6.Keim M. Building human resilience: the role of public health preparedness and response as an adaptation to climate change. Am J Prev Med. 2008;35(5):508–516 [DOI] [PubMed] [Google Scholar]
- 7.El Moriani Zel A, Ebener S, Boos J, Abdel Ghaffar E, Musani A. Modelling the spatial distribution of five natural hazards in the context of the WHO/EMRO Atlas of Disaster Risk as a step towards the reduction of the health impact related to disasters. Int J Health Geogr. 2007;6:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Organization for Economic Cooperation and Development OECD Health Data. Paris, France: Organization for Economic Cooperation and Development; 2009 [Google Scholar]
- 9.Chung JW, Meltzer DO. Estimate of the carbon footprint of the US health care sector. JAMA. 2009;302(18):1970–1972 [DOI] [PubMed] [Google Scholar]
- 10.US Energy Information Administration Frequently asked questions: crude oil. Available at: http://www.eia.doe.gov/ask/crudeoil_faqs.asp#products_and_uses. Accessed January 11, 2011
- 11.US Bureau of Labor Statistics Career guide to industries, 2010–11 edition. Available at: http://www.bls.gov/oco/cg/cgs035.htm. Accessed January 9, 2011
- 12.US Department of Transportation National Household Travel Survey. Publications: 2009 NHTS documentation. Available at: http://nhts.ornl.gov/publications.shtml#2009. Accessed January 9, 2011
- 13.National Association for Home Care & Hospice Study shows home health care workers drive nearly five billion miles to serve elderly and disabled patients. Available at: http://www.nahc.org/facts/homecareStudy.html. Accessed February 22, 2010
- 14.National Hospice and Palliative Care Association NHPCO Facts and Figures: Hospice Care in America. Alexandria, VA: National Hospice and Palliative Care Association; 2009 [Google Scholar]
- 15.Escalating energy costs threaten health care for critically ill and homebound seniors: home care nurses, aides and therapists drive 4.8 billion miles per year to reach shut-in patients. Caring. 2008;27(8):44–47 [PubMed] [Google Scholar]
- 16.Pitts SR, Niska RW, Xu J, et al. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. Natl Health Stat Rep. 2008(7):1–38 [PubMed] [Google Scholar]
- 17.Kleinman JC, Makuc D. Travel for ambulatory medical care. Med Care. 1983;21(5):543–557 [DOI] [PubMed] [Google Scholar]
- 18.Billi JE, Pai CW, Spahlinger DA. The effect of distance to primary care physician on health care utilization and disease burden. Health Care Manage Rev. 2007;32(1):22–29 [DOI] [PubMed] [Google Scholar]
- 19.Clarke PM. Cost-benefit analysis and mammographic screening: a travel cost approach. J Health Econ. 1998;17(6):767–787 [DOI] [PubMed] [Google Scholar]
- 20.Oleson JJ, Breheny PJ, Pendergast JF, et al. Impact of travel distance on WISEWOMAN Intervention attendance for a rural population. Prev Med. 2008;47(5):565–569 [DOI] [PubMed] [Google Scholar]
- 21.Celaya MO, Rees JR, Gibson JJ, Riddle BL, Greenberg ER. Travel distance and season of diagnosis affect treatment choices for women with early-stage breast cancer in a predominantly rural population (United States). Cancer Causes Control. 2006;17(6):851–856 [DOI] [PubMed] [Google Scholar]
- 22.Schappert SM, Rechtsteiner EA. Ambulatory medical care utilization estimates for 2006. Natl Health Stat Rep. 2008;(8):1–29 [PubMed] [Google Scholar]
- 23.US Bureau of Transportation Statistics Table 4–23: average fuel efficiency of US passenger cars and light trucks. Available at: http://www.bts.gov/publications/national_transportation_statistics/html/table_04_23.html. Accessed January 9, 2011
- 24.Weissermel K, Arpe H- J. Industrial Organic Chemistry. 4th ed Weinheim, Germany: Wiley-VCH; 2003 [Google Scholar]
- 25.Clark GB, Kline B. Impact of oil shortage on plastic medical supplies. Public Health Rep. 1981;96(2):111–115 [PMC free article] [PubMed] [Google Scholar]
- 26.US Energy Research and Development Administration Project Independence: A Summary. Washington, DC: US Energy Research and Development Administration; 1977 [Google Scholar]
- 27.Little A. Dependence of the US on Essential Imported Materials, Year 2000. Alexandria, VA: Defense Documentation Center, Defense Supply Agency; 1974 [Google Scholar]
- 28.Crawford JS. Recycling disposables. Lancet. 1974;303(7848):136. [DOI] [PubMed] [Google Scholar]
- 29.Berton AL. Disposable syringe and needle supplies [letter]. Lancet. 1974;303(7852):317. [DOI] [PubMed] [Google Scholar]
- 30.Schlechter M. Plastics for Health Care Packaging. Wellesley, MA: BCC Research; 2010 [Google Scholar]
- 31.American Chemistry Council Plastic Resins Industry Hit Hard by Global Economic Recession. Washington, DC: American Chemistry Council; 2008 [Google Scholar]
- 32.Plastics in medicine [letter]. Br Med J. 1951;2(4722):46–47 [Google Scholar]
- 33.Plastics in surgery [letter]. Br Med J. 1952;1(4761):750–752 [PMC free article] [PubMed] [Google Scholar]
- 34.Melson H. Plastics in medicine. Lancet. 1971;1(7689):87. [DOI] [PubMed] [Google Scholar]
- 35.Courtney JM. Meeting report: plastics in medicine and surgery. Biomed Eng. 1975;10(12):456–457 [PubMed] [Google Scholar]
- 36.Burch GE. Of plastic materials in clinical medicine. Am Heart J. 1978;95(1):127. [DOI] [PubMed] [Google Scholar]
- 37.Bruck SD. The need for better plastic materials for disposable medical applications: public health benefits and industrial developments. Int J Artif Organs. 1982;5(2):85–86 [PubMed] [Google Scholar]
- 38.Hart C. Shortage of plastics [letter]. BMJ. 1973;4(5894):741 [Google Scholar]
- 39.Kline AB., Jr Will shortages of raw materials and rising prices hurt our chances for better health care? Public Health Rep. 1975;90(1):3–9 [PMC free article] [PubMed] [Google Scholar]
- 40.DeFrances C, Lucas C, Buie V, Golosinkiy A. 2006 National Hospital Discharge Survey. Natl Health Stat Rep. 2008;(5):1–20 [PubMed] [Google Scholar]
- 41.Bozell JJ. Connecting biomass and petroleum processing with a chemical bridge. Science. 2010;329(5991):522–523 [DOI] [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention Therapeutic drug use. Available at: http://www.cdc.gov/nchs/fastats/drugs.htm. Accessed April 26, 2010
- 43.Aleklett K, Höök M, Jakobsson K, Lardelli M, Snowden S, Söderbergh B. The peak of the oil age—analyzing the world oil production Reference Scenario in World Energy Outlook 2008. Energy Policy. 2010;38(3):1398–1414 [Google Scholar]
- 44.Connor S. Warning: oil supplies are running out fast. The Independent. August 3, 2009. Available at: http://www.independent.co.uk/news/science/warning-oil-supplies-are-running-out-fast-1766585.html. Accessed June 9, 2011
- 45.Pearce D. Substitution and sustainability: some reflections on Georgescu-Roegen. Ecol Econ. 1997;22(3):295–297 [Google Scholar]
- 46.Bretschger L. Economics of technological change and the natural environment: how effective are innovations as a remedy for resource scarcity? Ecol Econ. 2005;54(2–3):148–163 [Google Scholar]
- 47.Kaufmann R, Schiers L. Alternatives to conventional crude oil: when, how quickly, and market driven? Ecol Econ. 2008;67(3):405–411 [Google Scholar]
- 48.Hirsch R, Bezdek R, Wendling R. Peaking of World Oil Production: Impacts, Mitigation, & Risk Management. Washington, DC: National Energy Technology Laboratory, US Department of Energy; 2005 [Google Scholar]
- 49.Ayres R. On the practical limits to substitution. Ecol Econ. 2007;61(1):115–128 [Google Scholar]
- 50.US Energy Information Administration Saudi Arabia country analysis brief. Chart 1: nominal dollars per barrel. Available at: http://www.eia.doe.gov/emeu/cabs/AOMC/images/chron_apr2007.xls. Accessed May 31, 2011
- 51.Bentley TG, Effros RM, Palar K, et al. Waste in the US health care system: a conceptual framework. Milbank Q. 2008;86(4):629–659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bush RW. Reducing waste in US health care systems. JAMA. 2007;297(8):871–874 [DOI] [PubMed] [Google Scholar]
- 53.Leonard S. Suppliers aim to renew OEMs' interest in eco-friendly plastics. Med Prod Manufacturing News. 2010;26(2). Available at: http://www.qmed.com/mpmn/article/16869/suppliers-aim-renew-oems-interest-eco-friendly-plastics. Accessed May 31, 2011 [Google Scholar]
- 54.Plastemart.com New applications of biodegradable plastics in medical sector gain acceptance. Available at: http://www.plastemart.com/upload/Literature/New-applications-biodegradable-plastics-medical-sector-Hernia-repair-drug-delivery-medical-implants.asp. Accessed April 14, 2010
- 55.Stevens E. Green Plastics: An Introduction to the New Science of Biodegradable Plastics. Princeton, NJ: Princeton University Press; 2002 [Google Scholar]
- 56.Prieto MA. From oil to bioplastics, a dream come true? J Bacteriol. 2007;189(2):289–290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Committee on Grand Challenges for Sustainability in the Chemical Industry; National Research Council Sustainability in the Chemical Industry: Grand Challenges and Research Needs - A Workshop Report. Washington, DC: National Academies Press; 2005 [Google Scholar]
- 58.Cue B. Green chemistry in the pharmaceutical industry: a model for sustainability. Paper presented at: Rachel Carson Legacy Conference; September 20, 2008; Pittsburgh, PA [Google Scholar]
- 59.Sterman JD. Learning from evidence in a complex world. Am J Public Health. 2006;96(3):505–514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Meadows D. Whole earth models and systems. Coevol Q. 1982;(Summer):98–108 [Google Scholar]
- 61.Scofea L. The development and growth of employer-provided health insurance. Mon Labor Rev. 1994;117(3):3–10 [PubMed] [Google Scholar]
- 62.Fisher ES, Bynum JP, Skinner JS. Slowing the growth of health care costs—lessons from regional variation. N Engl J Med. 2009;360(9):849–852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.National Association for Home Care & Hospice Escalating energy costs threaten health care for critically ill and homebound seniors: home care nurses, aides and therapists drive 4.8 billion miles per year to reach shut-in patients [press release]. Available at: http://www.nahc.org/Media/mediaPR_062508.html. Published June 25, 2008. Accessed February 22, 2010 [PubMed]
- 64.National Association for Home Care & Hospice 2009 NAHC, Cerner BeyondNow “Excellence in Innovation” award goes to Suncoast Hospice [press release]. Available at: http://www.nahc.org/Media/mediaPR_101109.html. Published October 11, 2009. Accessed February 22, 2010
- 65.National Association for Home Care & Hospice NAHC partners with enterprise fleet management to reduce members' transportation costs, boost employee recruitment and retention [press release]. Available at: http://www.nahc.org/Media/mediaPR_083009.html. Published August 30, 2009. Accessed February 22, 2010
- 66.Linkov I, Satterstrom FK, Kiker G, Batchelor C, Bridges T, Ferguson E. From comparative risk assessment to multi-criteria decision analysis and adaptive management: recent developments and applications. Environ Int. 2006;32(8):1072–1093 [DOI] [PubMed] [Google Scholar]
- 67.Henriksen HJ, Barlebo HC. Reflections on the use of Bayesian belief networks for adaptive management. J Environ Manage. 2008;88(4):1025–1036 [DOI] [PubMed] [Google Scholar]
- 68.Holling C. Adaptive Environmental Assessment and Management. New York, NY: Wiley; 1978 [Google Scholar]
- 69.Whicker JJ, Janecky DR, Doerr TB. Adaptive management: a paradigm for remediation of public facilities following a terrorist attack. Risk Anal. 2008;28(5):1445–1456 [DOI] [PubMed] [Google Scholar]
- 70.Gregory R, Ohlson D, Arvai J. Deconstructing adaptive management: criteria for applications to environmental management. Ecol Appl. 2006;16(6):2411–2425 [DOI] [PubMed] [Google Scholar]
- 71.Homer JB, Hirsch GB. System dynamics modeling for public health: background and opportunities. Am J Public Health. 2006;96(3):452–458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Thompson KM, Tebbens RJD. Using system dynamics to develop policies that matter: global management of poliomyelitis and beyond. Syst Dyn Rev. 2008;24(4):433–449 [Google Scholar]
- 73.Milstein B, Homer J, Hirsch G. Analyzing national health reform strategies with a dynamic simulation model. Am J Public Health. 2010;100(5):811–819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bryan BA, Kandulu J, Deere DA, White M, Frizenschaf J, Crossman ND. Adaptive management for mitigating Cryptosporidium risk in source water: a case study in an agricultural catchment in South Australia. J Environ Manage. 2009;90(10):3122–3134 [DOI] [PubMed] [Google Scholar]
- 75.Merl D, Johnson LR, Gramacy RB, Mangel M. A statistical framework for the adaptive management of epidemiological interventions. PLoS ONE. 2009;4(6):e5807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Stubbs M, Lemon M. Learning to network and networking to learn: facilitating the process of adaptive management in a local response to the UK's National Air Quality Strategy. Environ Manage. 2001;27(3):321–334 [DOI] [PubMed] [Google Scholar]
- 77.National Research Council Adaptive Management for Water Resources Project Planning. Washington, DC: National Academies Press; 2004 [Google Scholar]
- 78.Murray C, Marmorek D. Adaptive management and ecological restoration. : Freiderici P, Ecological Restoration of Southwestern Ponderosa Pine Forests. Washington, DC: Island Press; 2003:417–428 [Google Scholar]
- 79.O'Brien DJ, Price TG, Adams P. The effectiveness of lights and siren use during ambulance transport by paramedics. Prehosp Emerg Care. 1999;3(2):127–130 [DOI] [PubMed] [Google Scholar]
- 80.Concannon TW, Griffith JL, Kent DM, et al. Elapsed time in emergency medical services for patients with cardiac complaints: are some patients at greater risk for delay? Circ Cardiovasc Qual Outcomes. 2009;2(1):9–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hess J, Greenberg L. Fuel use in a large, hospital-based, dynamically deployed emergency medical service. Prehosp Disaster Med. In press [DOI] [PubMed] [Google Scholar]
- 82.Patterson PD, Probst JC, Moore CG. Expected annual emergency miles per ambulance: an indicator for measuring availability of emergency medical services resources. J Rural Health. 2006;22(2):102–111 [DOI] [PubMed] [Google Scholar]
- 83.Meaux L. Acadian Ambulance unveils new, fuel-efficient emergency vehicle. Acadiana Gazette. October 29, 2008:3B [Google Scholar]
- 84.Williamson JH, Knapp PE, Hubbard G, Gilbey DJ. Transport fleet costs cut—experience with LPG. Hosp Eng. 1984;38(1):9–13 [PubMed] [Google Scholar]
- 85.Shah MN, Bazarian JJ, Lerner EB, et al. The epidemiology of emergency medical services use by older adults: an analysis of the National Hospital Ambulatory Medical Care Survey. Acad Emerg Med. 2007;14(5):441–447 [DOI] [PubMed] [Google Scholar]
- 86.Blanchard I, Brown L. Carbon footprinting of North American emergency medical services systems. Prehosp Emerg Care. 2011;15(1):23–29 [DOI] [PubMed] [Google Scholar]
- 87.Lin CS, Chang H, Shyu KG, et al. A method to reduce response times in prehospital care: the motorcycle experience. Am J Emerg Med. 1998;16(7):711–713 [DOI] [PubMed] [Google Scholar]
- 88.Soares-Oliveira M, Egipto P, Costa I, Cunha-Ribeiro LM. Emergency motorcycle: has it a place in a medical emergency system? Am J Emerg Med. 2007;25(6):620–622 [DOI] [PubMed] [Google Scholar]
- 89.Kiefe CC, Soares-Oliveira M. Medical emergency motorcycles: are they safe? Eur J Emerg Med. 2008;15(1):40–42 [DOI] [PubMed] [Google Scholar]
- 90.Cundill G, Fabricius C. Monitoring in adaptive co-management: toward a learning based approach. J Environ Manage. 2009;90(11):3205–3211 [DOI] [PubMed] [Google Scholar]
- 91.Satterstrom FK, Linkov I, Kiker G, Bridges T, Greenberg M. Adaptive management: a review and framework for integration with multi-criteria decision analysis. : Macey J, Cannon J, Reclaiming the Land: Rethinking Superfund Institutions, Methods and Practices. New York, NY: Springer; 2007:89–128 [Google Scholar]
- 92.Aven T. An integrated framework for decision support on risk and uncertainty. Risk Manag. 2010;12(4):285–300 [Google Scholar]
- 93.Li L, Wang J, Leung H, Jiang C. Assessment of catastrophic risk using bayesian network constructed from domain knowledge and spatial data. Risk Anal. 2010;30(7):1157–1175 [DOI] [PubMed] [Google Scholar]
- 94.Davidsen PI, Sterman JD, Richardson GP. A petroleum life cycle model for the United States with endogenous technology, exploration, recovery, and demand. Syst Dyn Rev. 1990;6(1):66–93 [Google Scholar]
- 95.Homer J, Hirsch G, Milstein B. Chronic illness in a complex health economy: the perils and promises of downstream and upstream reforms. Syst Dyn Rev. 2007;23(2–3):313–343 [Google Scholar]
- 96.Lardelli M. Scientists need to confront economists about peak oil. Nature. 2007;446(7133):257. [DOI] [PubMed] [Google Scholar]
- 97.Harich J. Change resistance as the crux of the environmental sustainability problem. Syst Dyn Rev. 2010;26(1):35–72 [Google Scholar]
- 98.Sterman JD. Risk communication on climate: mental models and mass balance. Science. 2008;322(5901):532–533 [DOI] [PubMed] [Google Scholar]