Abstract
Depressive syndromes represent a disabling comorbidity for many children with autism spectrum disorders (ASD), however the ascertainment of depression can be complicated by phenotypic overlap between the two conditions, by ways in which autistic symptomatology can mask cardinal features of depression, and by atypical manifestations of depression in children with ASD. These issues have contributed to wide variation in the estimation of prevalence rates of depression in individuals with ASD, and invoke the need for new approaches to the specific detection of depression and other neuropsychiatric comorbidities that aggregate in children affected by ASD. We review the scientific literature relevant to the occurrence of depression in ASD, and consider important parameters of risk, including psychosocial factors such as insight into affectation status, as well as biological factors such as the aggregation of depressive syndromes in certain families affected by autism, which has suggested possible overlap in genetic influences underlying the two conditions. Variability in the manifestations of depression across environmental contexts provides important clues to intervention, and underscores the potential importance of involving multiple informants in ascertaining depression in children and adolescents with ASD. A practical strategy for evaluating the presence of depression in youth with ASD is synthesized from the available data and discussed.
Keywords: Comorbidity, Internalizing Disorders, Pervasive Developmental Disorder, Asperger Syndrome, Major Depressive Disorder
Introduction
Due in part to its chronic nature, the World Health Organization has recognized depression as the single disease imposing the largest public health burden in the United States and the third largest public health burden in the world.1 Depression not only affects the mental health of individuals, but also imposes effects on physical health, which may further contribute to the maintenance of depression.2 Major Depressive Disorder in adolescents is associated with decreased functioning in adulthood, recurrence and an increased risk of death due to suicide.3, 4 Due both to the high burden of disease and the treatable nature of depression, the US Preventive Services Task Force (USPSTF) has recommended screening all adolescents for depression, provided that a framework for accurate diagnosis, treatment and follow-up is in place.3 Although it might be assumed that children and adolescents with autism spectrum disorders (ASD) might be relatively protected from the development of depressive syndromes, there is accumulating evidence that this is not the case. Given the seriousness of depression and inherent difficulties in ascertaining its presence in children with autism spectrum disorders, a high degree of vigilance is warranted in the care of children and adolescents with ASD, a population that is now believed to carry a significantly heightened predisposition, not only to depression but to an array of other comorbid neuropsychiatric conditions.5-8
Autism spectrum disorders often impose severe limitations on capacity for managing activities of daily living,9 and quality of life has been shown to be significantly compromised for many children and families affected by ASD.10 Prevalence rates have been increasing, and have most recently been reported to be 1 in 91 children between the ages of 3 to 17 years as estimated by the 2007 National Survey of Children's Health.11 Equally concerning is that autism spectrum disorders are very frequently associated with a multitude of medical and psychiatric comorbidities at rates higher than those of typically developing children.12 These comorbidities range from gastrointestinal, neurologic, and endocrine abnormalities12, 13 to psychiatric comorbidities such as mood disorders, anxiety, and ADHD.12, 14
As is true for youth unaffected by ASD, the occurrence of depression has specific, and at times profound impact on functioning, however, in the context of ASD, it is not fully known how to identify when a depressive syndrome is present.15 Identification of depressive states has traditionally capitalized on subjective self-report information, which is difficult for many children with ASD to provide.16, 17 Traditional measures of diagnosis have generally not been tested for validity and reliability in ASD populations.18 Moreover, the presentation of depression in children with ASD is often atypical, or at the least complicated by the social, cognitive, and communicative impairments that characterize autism.7 Prevalence rates for depression in ASD vary widely because of phenotypic overlap between the two conditions, the tendency for autistic symptomatology to mask cardinal features of depression, and the fact that symptoms of depression in children with ASD may be atypical.15, 19 Insight into one's own level of impairment is known to be associated with depressive symptomatology,20, 21 but it is not clear if lack of insight in severely affected children confers protection from depressive states, making it all the more critical to develop better methods to ascertain depressive states in non-verbal autistic children.
There has been only modest systematic evaluation of interventions for depression in children with autism spectrum disorders, but enough to conclude that treatment may be effective when the condition is identified. 5, 7, 8, 22, 23 The aggregation of depressive syndromes in certain families affected by autism has suggested possible overlap in genetic influences underlying the two conditions,24-27 but there is also evidence for substantial independence of their respective genetic origins.28, 29
The goal of this review is to summarize pertinent information regarding the presentation and identification of depressive states in ASD, and to consider important parameters of risk derived from the existing data, including psychosocial factors such as insight into affectation status, as well as biological factors such as inherited liability. For this review, we searched the National Library of Medicine Pub Med database for all studies involving “depression” and either “autism spectrum disorders” or “pervasive developmental disorder.”10, 18, 19, 21-23, 30-48 We synthesized the results of these studies with literature on the development and diagnostic assessment of each respective condition.
Presentation of Depression in Autism Spectrum Disorders
Manifestations of depressive symptoms vary as a function of age and therefore general level of developmental maturation, 49 however commonalities across the life course include diminished interest in activities, feelings of worthlessness or guilt, diminished ability to concentrate or make decisions and recurrent thoughts of death.9 An allowance made by the DSM-IV-TR is the substitution of irritability for depressed mood if necessary in diagnosing Major Depressive Disorder in children.9, 49 A study of typically developing preschool-aged children found that while irritability and sadness were the most sensitive predictors of depression (identified in 98% of preschoolers), anhedonia was the most specific, apparent only in the depressed group.50 Younger children may present with somatic complaints and behavior problems and may demonstrate a persistent engagement in activities or play with themes of death or suicide.50 Observation of activities is critical in the assessment of depression in very young children due to limited verbal ability and tendency to express such thoughts through play, although even very young children demonstrate neurovegetative signs and lack of brightening similar to depressed adults.50 Adolescents more commonly display hypersomnia and have an increased risk for suicide in comparison to preadolescents. In general, females more typically display changes in appetite or weight, increased frequency of crying, and feelings of guilt or low self-esteem, while males are more likely to endorse anhedonia, social withdrawal, and variation in mood or energy.49
Given that many individuals with autism spectrum conditions have significant impairments in communication, subjective states of sadness, hopelessness, or disinterest may be extremely difficult to express. In such cases, identification and diagnosis of depression has largely relied on outward behaviors or changes in mental state inferred from parent or caregiver observations. Observable behaviors reported by caregivers and documented in the literature include an increase in sadness, tearfulness, apathy, or an increasingly negative affect.5, 7, 15, 22, 34, 51 Additionally, anhedonia, vegetative signs such as sleep and weight disturbances, or decline in performance / regression of skills have been noted in youth with autism.15, 34, 38 Catatonic behavior has also been reported.23
‘Theory of mind’ deficits associated with ASD can further complicate self-report of depressive syndromes.18 Decreased ability or incapacity of innate self-reflection invoke reliance on alternate signs or symptoms such as a decrease in self-care or an increase in self-injurious behavior (SIB) as manifestations of an increasingly negative self-view.7, 46 SIB in the form of head banging or self-hitting has been reported in children with autism. Theories of its causes include the need for sensory stimulation or a response to stress, discomfort, or frustration.52 Preoccupation with themes of death have also been noted in youth with ASD during periods of depression,8, 22, 53 and case reports illustrate resolution of SIB after treatment of depression in individuals with autism spectrum disorders.8, 34 In support of the theory that increasingly frequent SIB can be a proxy for negative self-view when combined with other depressive signs or symptoms, SIB has also been significantly associated with depression in persons with profound intellectual disabilities.51, 54
Atypical affective changes, such as increased aggression, irritability, agitation, and labile moods may also be present in depressive states.15, 22, 34, 46 Overlap in symptomatology between depression and autism spectrum disorders may challenge the clinician's ability to elicit whether classic signs of depression are due to the primary diagnosis of ASD or to an actual comorbid psychiatric condition.5, 7, 18 For instance, case reports and prospective studies discuss children with ASD and depression demonstrating exacerbated compulsiveness or increased stereotypic behavior.7, 15, 22, 46 Both intensification of and decrease in autistic symptomatology have been reported with the onset of depression. Intensification of autistic traits includes increases in ritualistic behavior or obsessions, often coupled with irritability and hyperactivity. Less frequently associated with depression but reported through anecdotal reports or case studies is the loss of interest in repetitive behaviors and autistic preoccupations accompanying more social withdrawal and decreased adaptive functioning.5, 7 No studies identified have specifically investigated the manner in which autistic traits fluctuate with episodes of depression; however, many studies in the literature demonstrate that deviation of autistic symptoms from baseline may indicate a depressive episode.5, 18, 34, 51 Clinically, a change in behavior from baseline is an easily elicited piece of information that can be of tremendous help in screening children with ASD for affective disorders. A summary of traditional and ASD-specific signs and symptoms that may signify depression in ASD-affected youth can be found in Table 1.
Table 1.
The left column lists characteristics of depression seen in both children and adults. The asterisks (*) indicate qualities that are unique to or more commonly observed in childhood depression. The presentation of depression in children with autism spectrum disorders can be more challenging to characterize and recognize. The right column lists additional characteristics that have been described in ASD-affected children presumed to be affected by depression or depressive symptomatology (ASD-affected children have been observed to exhibit signs or symptoms from both the left and right columns).
| Traditional signs and symptoms of depression including characteristics that may be seen in childhood depression include: | Additional signs and symptoms that may be present in ASD-affected children who are experiencing depression |
|---|---|
|
|
Identifying Depression in ASD and Current Prevalence
To aid clinicians in determining the likelihood of depression in children with ASD, researchers have attempted to estimate co-occurrence of the two conditions in the population. This has proved to be a monumental challenge. Given the long list of complicating factors in identifying a depressive episode, it is not surprising that while many studies have reported increased risk of depression in children with ASD in comparison with typically developing children,5, 7, 12 prevalence rates of depression in autism have varied from 1.4%19 to 38%.15 A major obstacle has been the lack of a gold standard assessment and measurement tool of psychiatric comorbidities designed specifically for those with Autism Spectrum Disorders.7, 14, 15, 18 In lieu of such a tool, clinicians have utilized semi-structured interviews and a variety of measures designed for either the general or learning-disabled population.7, 15, 18
In an effort to address this issue, Leyfer and colleagues18 developed the Autism Comorbidity Interview – Present and Lifetime Version (ACI-PL), a variation of the Kiddie Schedule for Affective Disorders and Schizophrenia specifically modified for children with ASD. The investigators studied 109 high functioning children and adolescents (5-17 years old) with ASD. The mean IQ was 82.5 and the information was obtained via parent report. Validation consisted of an analysis of diagnostic accuracy against community diagnosis of comorbid depression for which the children actually had received clinical treatment; this revealed a sensitivity of 100% and specificity of 83% - 93.7%. A critical aspect of this measurement system is that it specifically seeks to establish the child's “best baseline” for qualitative and quantitative comparison to presenting symptoms5, 7, 18, 53
Simonoff and colleagues19 conducted a standardized assessment of a population-based sample of British children with ASD. DSM-IV diagnoses were made using the Child and Adolescent Psychiatric Assessment – Parent Version (CAPA), a widely used measure, but one that has not been modified specially for youth with ASD. They studied 112 children and adolescents (10 – 14 years old) with autism. The mean IQ was 72.7 and the information obtained via parent report.
The prevalence rate for major depressive episodes varied from 1.5% (Simonoff et al.) to 10% (Leyfer et al.) in these studies, but both reported high rates of subsyndromal depressive symptomatology (10.4% in the Simonoff et al. study and 14% in Leyfer et al.).
Across these studies, the disparity in prevalence was much more pronounced for depressive symptomatology (1.5% - 10%) than for other comorbid psychiatric disorders.18, 19 Variation in verbal ability or intellectual functioning in the respective samples could be responsible for this specific discrepancy in depressive comorbidity, as could specific adaptation of the Leyfer interview for ASD, operating to identify a higher number of cases in that study. This suggests that a scale modified specifically for children with ASD, such as that designed by Leyfer and colleagues, might more completely ascertain internalizing symptoms which are best elicited by self-report in typically developing children.7, 14, 15, 18
Unfortunately, neither of these studies and no studies identified have sought to systematically determine the prevalence of depression or sub-syndromic depression in lower functioning autistic children with an IQ less than 70. Methods validated for this population would be especially useful given the unique challenges that the symptoms of non-verbal ASD impose on derivation of a diagnosis of depression.
Relationships Between Severity of ASD, Insight, Age, and IQ to Depression in Youth with ASD
It has long been postulated that higher-functioning and more socially adjusted children with ASD develop insight into their differences by virtue of their cognitive abilities, leading to more negative self-perception and lower self-worth.5, 20 In support of this, Vickerstaff and colleagues21 found that higher cognitive abilities and greater insight into one's condition leads to a lower self-perceived social competence and subsequently higher rates of depression. Similarly, Sterling and colleagues found that depression in adults with autism spectrum disorders was associated with higher cognitive ability, less social impairment, and older age.32 Taylor and Seltzer recently showed that young adults with ASD without an intellectual disability were three times more likely to have “no daytime activities” compared to adults with ASD who had an intellectual disability, suggesting that inadequacy of current service systems to meet the needs of higher-functioning youth might compound risk for the development of depressive syndromes.55 Finally, Mazurek and Kanne found that youth with lower IQ and increased severity of ASD had fewer symptoms of depression than did higher functioning youth with ASD. It is unknown to what extent verbal ability, a characteristic generally associated with higher functioning youth with ASD, influenced these disparities.47 Preliminary evidence has shown that the prevalence of comorbid psychiatric problems was not a reflection of verbal ability when scored via parental reports.47
Data regarding a significant relationship between age and depression has been less conclusive. It is well known that in typically developing children the incidence of depression increases in adolescence, and this has been postulated to occur in youth with autism spectrum disorders as well.27 No study has directly compared rates of depression between children and adolescents controlling for ASD severity, but several have suggested a lack of association between prevalence and age,21, 43, 48 Vickerstaff et al. postulated that emotional age likely has more influence than chronological age on the development of depression.21
While increased capacity for adaptive functioning has been associated with higher rates of depression, it has also been theorized that increased severity of autism spectrum disorders may itself be associated with greater vulnerability to stressors and thus psychopathology.37, 53, 56 Pearson et al. 37 found that children with autism had more severe symptoms of depression, social withdraw and atypical behaviors than did children with Pervasive Developmental Disorder – Not Otherwise Specified (PDD-NOS), although both groups had elevated rates of clinically significant depressive syndromes. Interestingly, these results were unchanged when intelligence was controlled for, leading the authors to suggest that diagnostic subgroups on the autism spectrum might independently predict differing risks for the development of depression and other psychiatric comorbidities.
It is unknown how constructs such as insight or self-awareness are best measured in children with ASD. It is clinically observed that recognition of the condition and its social repercussions has the potential to be depressogenic in and of itself.21, 41 It is unknown, however, whether those who appear to lack such insight are protected from the development of depression.
Relationships Between Environment, Peer Relations, and Self-Perception to Depression in Youth with ASD
Peers and the environment fundamentally shape an adolescent's self-perception and understanding of the impact of ASD on day-to-day life.30 Many children and adolescents with ASD recognize differences between themselves and their peers, and this recognition has been correlated with higher levels of depressive symptoms.40 Youth with Asperger Syndrome who perceived that they had the lowest group membership and social integration have been reported to have elevated levels of depressive symptoms.31 It has been postulated that high-functioning youth with ASD, in contrast to lower functioning youth with ASD, may be especially vulnerable to depression due to their greater social and self-awareness and heightened interest in social relationships.43, 57 Higher functioning adults with autism spectrum disorders who have been shown to be more socially adept than their lower functioning peers also show an increased incidence of depression.32 In a comprehensive, multi-rater study, Vickerstaff and colleagues21 examined variation in depressive symptomatology in autism as a function of self-perception, insight, intelligence and age. In measurements of social competency, while the children overall were rated by parents and teachers as less socially competent than their peers, it was only the child's self-perceived social competence that was significantly associated with depressive symptoms. Williamson and colleagues found that adolescents with Asperger Syndrome perceived themselves to be less socially competent and to receive less peer approval. In this study of adolescents, peer approval was predictive of depression, and both peer approval and social competency were predictive of global self-worth scores.39
Abnormalities in emotion regulation have been postulated to have a substantial impact on mood in autism spectrum disorders.56 While even commonplace life events can elicit intense affective responses in youth with ASD,27 high-stress situations can be overtly overwhelming.30 Anxiety has been shown to predispose typically developing individuals to depression, and its effects are compounded in those who have difficulties in emotion regulation. 7, 56 For instance, in a recent study one student with autism described a perceived-chaotic classroom environment as a place in which “I'm upset every second, every second I've got tears in my eyes” (p. 38).30 Children and adolescents with ASD also experience loneliness, and may be taught or advised that the acquisition of friendships will assuage such feelings, but may be disinterested in peers or unable to initiate or sustain friendships.58 In typically-developing children, loneliness is associated with low self-esteem, higher levels of anxiety and can predispose to the development of depression.59 Whitehouse et al. studied the relationship between negative affect and quality of friendships in adolescents with Asperger syndrome. In that study, adolescents with Asperger syndrome had greater levels of loneliness and depressive symptomatology relative to their typically-developing peers.33 A significant predictor of depression in this study was conflict and betrayal within friendship. Mazurek and colleagues also studied the relationship between friendship and depression. Analysis of the results revealed that ASD-affected children with more friendships of poorer quality had the highest levels of anxiety and depression.41
Negative peer interactions have been shown to exert independent adverse effects on children with high-functioning ASD who are very commonly bullied, teased or ostracized in educational settings.30, 60, 61 Peer victimization and depressive symptomatology have been correlated, 42 and observational reports document both social isolation and distress as direct consequences of being bullied in the school environment.30 Interpersonal conflict with family members has also been strongly associated with depressive symptomatology.43, 44 Both in family and educational environments, assumptions about the cause of a child's deviant social behaviors (i.e. the premise under which parents, educators, siblings, and peers are operating when interpreting those behaviors) are critical in either buffering or intensifying the response of the environment to those behaviors. There are remarkable anecdotes of positive change in interpersonal relationships and behavior, for example, when the social network surrounding a child with ASD shifts from viewing his/her behaviors as fundamentally “antisocial” in nature to fundamentally “asocial”. This is particularly relevant for children with higher-functioning autistic syndromes who have never been diagnosed, and for whom the assumption of caregivers over years of time has been that the child is engaging in willful violations of social norms.62
Integrating multiple variables previously discussed, Barnhill described how higher functioning children with ASD with higher IQ and increased level of functioning were more likely to attribute social failure to lack of ability instead of chance. This perception resulted in an increase in depressive symptoms.45 Such findings invoke the construct of learned helplessness as a factor in the development of depression in this population. While no studies identified have empirically assessed learned helplessness and depression in children with autism, case reports of depressive symptomatology in conjunction with learned helplessness in persons with ASD have been reported. As an adult female with Asperger syndrome reported: “When I am able to get people to understand me, my view of life is positive, but when I am battling against the prejudice I feel very low. This feeling comes from the powerlessness to change my situation in which I find myself. … In formal situations this is not a major problem, but in informal ones it is a crushing one” (p 233).56
Research has demonstrated that higher levels of autistic traits in college students are associated with a more external locus of control, which contributes to the perception of helplessness.63 In contrast when chances for success are maximized, increases in motivation and appropriate social interactions are observed.64
Context-Specific Variation in Depressive Symptomatology in ASD
Recent research has sought to evaluate autistic and depressive symptomatology in a variety of environments with multiple informants to aid clinicians in diagnosing depression and to elucidate other environmental factors that contribute to depression in ASD. As discussed above, the diagnosis of depression is often complicated by its atypical presentation in youth with ASD. For that reason, assessing rates and symptoms of depression in multiple environments can help to clarify the presentation of depression and may reveal environments especially problematic for a child. Other benefits of cross-context variation assessed via multiple raters include a more accurate inference of the emotional state,65 a greater likelihood for diagnostic accuracy,66 and the potential identification of a serious and stable problem.67 Furthermore, expanding on parental report by drawing on the unique expertise and vantage point of teachers confers the advantage of assimilating into the assessment process information from children in their natural social environments and incorporating repeated observations over time from disparate observers.66
Despite these many benefits, a review of the recently published literature finds only a few studies that have successfully used multi-rater assessment to determine how prevalence of depression in ASD varies with the environment and rater. Vickerstaff et al.21 found the mean parental rating of children's depressive symptomatology to be within the “clinically significant” range (via the Behavior Assessment Scale for Children), but reported teachers' mean rating to be only in the “at-risk” range. Similarly, Kanne and colleagues65 found that a higher percentage of parents reported their children as having clinical level depressive symptomatology (26%) than did their teachers (6%) when using the Achenbach System of Empirically Based Assessment.
Hurtig and colleagues recently expanded such multi-informant approaches by including input from youth themselves, utilizing the Youth Self-Report; it is widely recognized from studies of typically-developing youth that self-report is the most sensitive of all ascertainment strategies for adolescent depression. Hurtig et al. found strong agreement between adolescents, teachers, and parents on social problem scales, indicating awareness among all informants of such difficulties. However, parents reported fewer problems in the internalizing problems subscale than did both adolescents and their teachers. 68 Overall, results suggest that psychiatric symptoms in youth with ASD may have distinct presentations across varying environments, and therefore interpretations based upon a single source or environment may be incomplete, leading to inaccurate diagnoses.65 This has clear implications for any strategy to screen for or diagnose depression in ASD-affected youth.
Genetic Contributions to Depression in ASD
Autism Spectrum Disorders are heavily influenced by genetic factors 69 and there is accumulating evidence that genetic influence on ASD may overlap with that for other neuropsychiatric conditions, including learning disorders, schizophrenia, epilepsy, ADHD, language disorders, and tic disorders.69 The potential for genetic overlap between autism and depression has been explored and is relevant to the ascertainment and identification of depression in this population.69
Depression and anxiety are observed commonly in family members of children affected by autism; studies have found the rates of such conditions to be appreciably higher than the national average.70 There is often a significant history of familial depression in children with ASD who are diagnosed with depression,27, 71 as well as a higher prevalence of familial depression in individuals with ASD compared to controls.72 In a large population-based case-control study, a positive association was found between maternal depression and childhood autism.26
In an attempt to elucidate the possible nature of genetic overlap, twin studies have been conducted. The possibility of genetic overlap between autistic traits and affective disorder traits has been explored in at least four twin studies.28, 29, 73, 74 In a study by Constantino and colleagues28 sub-threshold autistic symptomatology as measured by the Social Responsiveness Scale was largely attributable to unique genetic factors, and these factors were significantly independent of the genetic influences on anxious/depressed symptomatology measured by the Child Behavioral Checklist (CBCL); only social and attention problems as measured by the CBCL had significant associations with autistic traits.
In a study of adolescent twins via self-report, Hoekstra and colleagues reported that social problems related to depression and anxiety overlap with those observed in children with elevated autistic traits. Their multivariate analysis also showed that approximately half of the genetic variance in scores for autistic traits overlapped with those conferring susceptibility to other behavioral problems.74 Autistic traits are known to be continuously distributed in the population,72, 75 but it is important to note that it remains unknown whether the genetic influences on sub-threshold or autistic-like traits are the same as the factors that cause ASD.75
In a multi-rater, population based twin study of 8 – 9 year old children, Hallett et al.29 found a significant phenotypic association between autistic-like and internalizing traits such as depressive symptoms, but only a modest level of genetic overlap. Non-shared environmental influences were generally trait specific, while shared environmental influences contributed to both autistic-like and internalizing traits, suggesting that co-occurrence may also be a consequence of environmental factors.29 A follow-up longitudinal study by Hallett et al.73 supported this view, and demonstrated substantial reciprocal influence between autistic-like and internalizing traits, implying that early autistic-like difficulties may have a pronounced impact on later depression or anxiety, via the effects of stressful environments on individuals with autism-related vulnerabilities.29, 73 In order to fully resolve the question of genetic overlap between depression and autism spectrum disorders, studies in genetically-informative clinical populations will be needed.72, 75
Synthesizing the Current State of Knowledge: a Testable Strategy for Identifying Depression in Youth with ASD
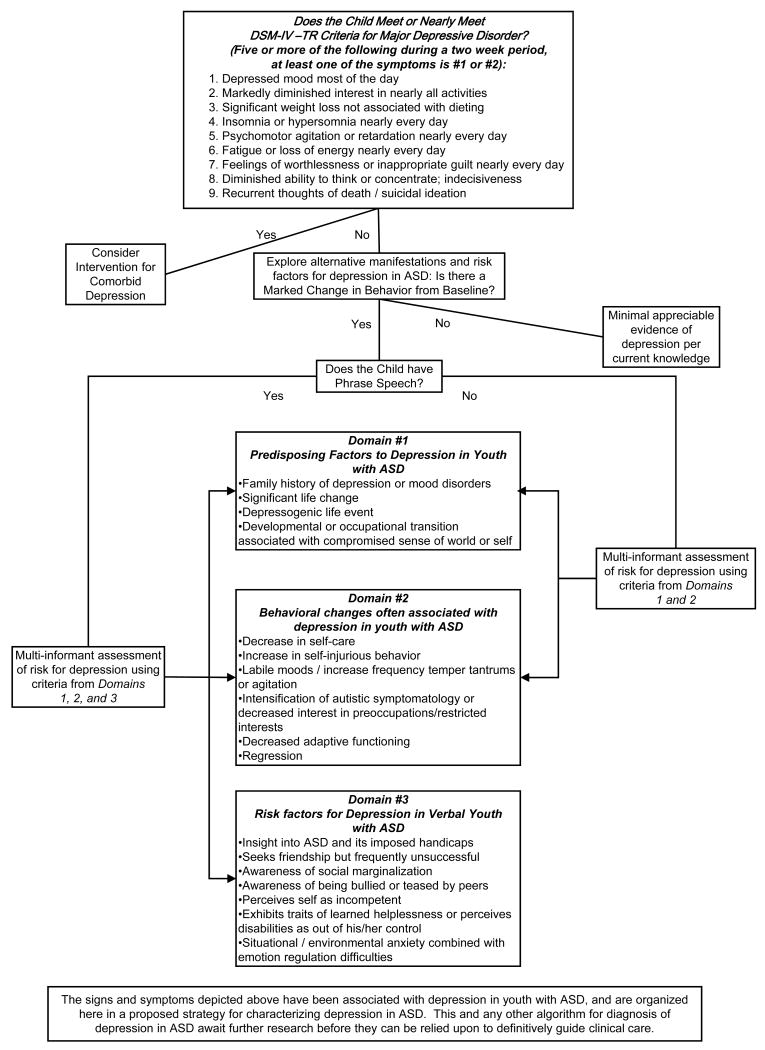
Despite many unanswered questions regarding the interface between depression and ASD, enough is now known to advance a more systematic approach to identification of ASD-affected youth with or at risk for depressive syndromes. Figure 1 synthesizes the findings summarized in this review into a model approach to diagnosis. The model considers both higher functioning children with phrase speech and lower functioning children without verbal language. In an attempt to address the unique signs and symptoms that a child on the autism spectrum may present with, the model incorporates both classic features of depression and the atypical signs and behavior changes indicative of depression in children with ASD that have been reported in the scientific literature. It considers specific moderators and vulnerability factors as well as the unique circumstances that may make insightful children with ASD especially vulnerable to the negative consequences of stressful life events.
Figure 1.
A proposed strategy for ascertainment and characterization of depressive syndromes in youth with ASD. Such an algorithm is testable, and if proven, has the potential to be utilized at routine well-child care visits or specialist visits.
Future Research
The complexities of identifying and characterizing depression in children with autism spectrum disorders invoke the need for ongoing research. Emphasis should continue to be placed on specifying the presentation of depression in autism. It will be necessary to further document the atypical signs and symptoms of depression in this population, and it would be particularly useful to identify how the pathognomonic behaviors of autistic syndromes may fluctuate with the onset of a depressive episode. It will be important to clarify under what circumstances insight is depressogenic in ASD and how risk for depression might be averted by timely implementation of cognitive therapy over the course of development. Continued investigation into peer relations, social awareness, and self-perception among youth with ASD will help identify interventions that will assist such children with social skills, provide meaningful opportunities to learn and contribute to the world around them, and help them construct and sustain a positive self-concept.
To these ends, use and further validation of the Autism Comorbidity Interview – Present and Lifetime Version18 may facilitate progress, given that it was derived from an instrument specifically designed to measure affective signs and symptoms of psychiatric comorbidities. Utilizing such tools in a variety of environments with multiple raters will advance understanding of the presentation of depression in ASD and help refine ascertainment strategies as presented in Figure 1.
Finally, continued investigation into the overlap of causal influences on ASD and depression is warranted. Prospective clinical studies examining pathways by which early autistic symptomatology predicts depression later in life29 would be especially informative. Ultimately, clearer characterization of depressive syndromes in autism will lead to better understanding of their ontogeny, and will facilitate appropriate implementation of effective medical and psychosocial interventions as early as possible in the course of their development.
Acknowledgments
This work was supported, in part, by a grant to Dr. Constantino from the National Institute of Child Health and Human Development (HD-42541)
Contributor Information
Katherine M. Magnuson, Saint Louis University School of Medicine, St. Louis MO
John N. Constantino, Departments of Psychiatry and Pediatrics, Washington University School of Medicine, St. Louis MO
Works Cited
- 1.Boerma J, Fat DM, Mathers C, Organization WH. The global burden of disease: 2004 Update. Geneva: World Health Organization; 2008. [Google Scholar]
- 2.Keenan-Miller D, Hammen CL, Brennan PA. Health outcomes related to early adolescent depression. J Adolesc Health. 2007 Sep;41(3):256–262. doi: 10.1016/j.jadohealth.2007.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Screening and treatment for major depressive disorder in children and adolescents: US Preventive Services Task Force Recommendation Statement. Pediatrics. 2009 Apr;123(4):1223–1228. doi: 10.1542/peds.2008-2381. [DOI] [PubMed] [Google Scholar]
- 4.Williams SB, O'Connor EA, Eder M, Whitlock EP. Screening for child and adolescent depression in primary care settings: a systematic evidence review for the US Preventive Services Task Force. Pediatrics. 2009 Apr;123(4):e716–735. doi: 10.1542/peds.2008-2415. [DOI] [PubMed] [Google Scholar]
- 5.Ghaziuddin M, Ghaziuddin N, Greden J. Depression in persons with autism: implications for research and clinical care. J Autism Dev Disord. 2002 Aug;32(4):299–306. doi: 10.1023/a:1016330802348. [DOI] [PubMed] [Google Scholar]
- 6.Howlin P. Psychiatric disturbances in adulthood. In: Howlin P, editor. Autism: Preparing for Adulthood. London and New York: Routledge; 1997. pp. 229–235. [Google Scholar]
- 7.Stewart ME, Barnard L, Pearson J, Hasan R, O'Brien G. Presentation of depression in autism and Asperger syndrome: a review. Autism. 2006 Jan;10(1):103–116. doi: 10.1177/1362361306062013. [DOI] [PubMed] [Google Scholar]
- 8.Wachtel LE, Griffin M, Reti IM. Electroconvulsive therapy in a man with autism experiencing severe depression, catatonia, and self-injury. J ECT. 2010 Mar;26(1):70–73. doi: 10.1097/YCT.0b013e3181a744ec. [DOI] [PubMed] [Google Scholar]
- 9.Association AP. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 10.Lee LC, Harrington RA, Louie BB, Newschaffer CJ. Children with autism: quality of life and parental concerns. J Autism Dev Disord. 2008 Jul;38(6):1147–1160. doi: 10.1007/s10803-007-0491-0. [DOI] [PubMed] [Google Scholar]
- 11.Kogan MD, Blumberg SJ, Schieve LA, et al. Prevalence of parent-reported diagnosis of autism spectrum disorder among children in the US, 2007. Pediatrics. 2009 Nov;124(5):1395–1403. doi: 10.1542/peds.2009-1522. [DOI] [PubMed] [Google Scholar]
- 12.Gurney J, McPheeters M, Davis M. Parental report of health conditions and health care use among children with and without autism: National survey of children's health. Arch Pediat Adolesc Med. 2006 Aug;160(8):825–830. doi: 10.1001/archpedi.160.8.825. [DOI] [PubMed] [Google Scholar]
- 13.Chen CY, Chen KH, Liu CY, Huang SL, Lin KM. Increased risks of congenital, neurologic, and endocrine disorders associated with autism in preschool children: cognitive ability differences. J Pediatr. 2009 Mar;154(3):345–350. 350 e341. doi: 10.1016/j.jpeds.2008.09.043. [DOI] [PubMed] [Google Scholar]
- 14.Matson JL, Nebel-Schwalm MS. Comorbid psychopathology with autism spectrum disorder in children: an overview. Res Dev Disabil. 2007 Jul-Sep;28(4):341–352. doi: 10.1016/j.ridd.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 15.Lainhart JE, Folstein SE. Affective disorders in people with autism: a review of published cases. J Autism Dev Disord. 1994 Oct;24(5):587–601. doi: 10.1007/BF02172140. [DOI] [PubMed] [Google Scholar]
- 16.Baron-Cohen S, Leslie AM, Frith U. Does the autistic child have a “theory of mind”? Cognition. 1985 Oct;21(1):37–46. doi: 10.1016/0010-0277(85)90022-8. [DOI] [PubMed] [Google Scholar]
- 17.Tager-Flusberg H. Autistic children's talk about psychological states: deficits in the early acquisition of a theory of mind. Child Dev. 1992 Feb;63(1):161–172. [PubMed] [Google Scholar]
- 18.Leyfer OT, Folstein SE, Bacalman S, et al. Comorbid psychiatric disorders in children with autism: interview development and rates of disorders. J Autism Dev Disord. 2006 Oct;36(7):849–861. doi: 10.1007/s10803-006-0123-0. [DOI] [PubMed] [Google Scholar]
- 19.Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008 Aug;47(8):921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- 20.Capps L, Sigman M, Yirmiya N. Self-competence and emotional understanding in high-functioning children with autism. Dev Psychopathol. 1995 Dec;7(1):137–149. [Google Scholar]
- 21.Vickerstaff S, Heriot S, Wong M, Lopes A, Dossetor D. Intellectual ability, self-perceived social competence, and depressive symptomatology in children with high-functioning autistic spectrum disorders. J Autism Dev Disord. 2007 Oct;37(9):1647–1664. doi: 10.1007/s10803-006-0292-x. [DOI] [PubMed] [Google Scholar]
- 22.Perry DW, Marston GM, Hinder SA, Munden AC, Roy A. The phenomenology of depressive illness in people with a learning disability and autism. Autism. 2001 Sep;5(3):265–275. doi: 10.1177/1362361301005003004. [DOI] [PubMed] [Google Scholar]
- 23.Takaoka K, Takata T. Catatonia in high-functioning autism spectrum disorders: case report and review of literature. Psychol Rep. 2007 Dec;101(3 Pt 1):961–969. doi: 10.2466/pr0.101.3.961-969. [DOI] [PubMed] [Google Scholar]
- 24.Bailey A, LeCouteur A, II G, et al. Autism as a strongly genetic disorder: evidence from a British twin study. Psychol Med. 1995 Jan;25(1):63–77. doi: 10.1017/s0033291700028099. [DOI] [PubMed] [Google Scholar]
- 25.Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: review and meta-analysis. Am J Psychiatry. 2000 Oct;157(10):1552–1562. doi: 10.1176/appi.ajp.157.10.1552. [DOI] [PubMed] [Google Scholar]
- 26.Daniels JL, Forssen U, Hultman CM, et al. Parental psychiatric disorders associated with autism spectrum disorders in the offspring. Pediatrics. 2008 May;121(5):e1357–1362. doi: 10.1542/peds.2007-2296. [DOI] [PubMed] [Google Scholar]
- 27.Ghaziuddin M, Greden J. Depression in children with autism/pervasive developmental disorders: a case-control family history study. J Autism Dev Disord. 1998 Apr;28(2):111–115. doi: 10.1023/a:1026036514719. [DOI] [PubMed] [Google Scholar]
- 28.Constantino JN, Hudziak JJ, Todd RD. Deficits in reciprocal social behavior in male twins: evidence for a genetically independent domain of psychopathology. J Am Acad Child Adolesc Psychiatry. 2003 Apr;42(4):458–467. doi: 10.1097/01.CHI.0000046811.95464.21. [DOI] [PubMed] [Google Scholar]
- 29.Hallett V, Ronald A, Happe F. Investigating the association between autistic-like and internalizing traits in a community-based twin sample. J Am Acad Child Adolesc Psychiatry. 2009 Jun;48(6):618–627. doi: 10.1097/CHI.0b013e31819f7116. [DOI] [PubMed] [Google Scholar]
- 30.Humphrey N, Lewis S. ‘Make me normal’: the views and experiences of pupils on the autistic spectrum in mainstream secondary schools. Autism. 2008 Jan;12(1):23–46. doi: 10.1177/1362361307085267. [DOI] [PubMed] [Google Scholar]
- 31.Hedley D, Young R. Social comparison processes and depressive symptoms in children and adolescents with Asperger syndrome. Autism. 2006 Mar;10(2):139–153. doi: 10.1177/1362361306062020. [DOI] [PubMed] [Google Scholar]
- 32.Sterling L, Dawson G, Estes A, Greenson J. Characteristics associated with presence of depressive symptoms in adults with autism spectrum disorder. J Autism Dev Disord. 2008 Jul;38(6):1011–1018. doi: 10.1007/s10803-007-0477-y. [DOI] [PubMed] [Google Scholar]
- 33.Whitehouse AJ, Durkin K, Jaquet E, Ziatas K. Friendship, loneliness and depression in adolescents with Asperger's Syndrome. J Adolesc. 2009 Apr;32(2):309–322. doi: 10.1016/j.adolescence.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 34.Pollard AJ, Prendergast M. Depressive pseudodementia in a child with autism. Dev Med Child Neurol. 2004 Jul;46(7):485–489. doi: 10.1017/s0012162204000805. [DOI] [PubMed] [Google Scholar]
- 35.Meyer JA, Mundy PC, Van Hecke AV, Durocher JS. Social attribution processes and comorbid psychiatric symptoms in children with Asperger syndrome. Autism. 2006 Jul;10(4):383–402. doi: 10.1177/1362361306064435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tsuji H, Miyawaki D, Kawaguchi T, et al. Relationship of hypersensitivity to anxiety and depression in children with high-functioning pervasive developmental disorders. Psychiatry Clin Neurosci. 2009 Apr;63(2):195–201. doi: 10.1111/j.1440-1819.2008.01916.x. [DOI] [PubMed] [Google Scholar]
- 37.Pearson DA, Loveland KA, Lachar D, et al. A comparison of behavioral and emotional functioning in children and adolescents with Autistic Disorder and PDD-NOS. Child Neuropsychol. 2006 Aug;12(4-5):321–333. doi: 10.1080/09297040600646847. [DOI] [PubMed] [Google Scholar]
- 38.Dominick KC, Davis NO, Lainhart J, Tager-Flusberg H, Folstein S. Atypical behaviors in children with autism and children with a history of language impairment. Res Dev Disabil. 2007 Mar-Apr;28(2):145–162. doi: 10.1016/j.ridd.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 39.Williamson S, Craig J, Slinger R. Exploring the relationship between measures of self-esteem and psychological adjustment among adolescents with Asperger syndrome. Autism. 2008 Jul;12(4):391–402. doi: 10.1177/1362361308091652. [DOI] [PubMed] [Google Scholar]
- 40.Butzer B, Konstantareas M. Depression, temperament and their relationship to other characteristics in children with Asperger's disorder. J Dev Disabil. 2003;10(1):67–72. [Google Scholar]
- 41.Mazurek MO, Kanne SM. Friendship and Internalizing Symptoms Among Children and Adolescents with ASD. J Autism Dev Disord. 2010 Apr 20; doi: 10.1007/s10803-010-1014-y. [DOI] [PubMed] [Google Scholar]
- 42.Shtayermman O. Peer victimization in adolescents and young adults diagnosed with Asperger's Syndrome: a link to depressive symptomatology, anxiety symptomatology and suicidal ideation. Issues Compr Pediatr Nurs. 2007 Jul-Sep;30(3):87–107. doi: 10.1080/01460860701525089. [DOI] [PubMed] [Google Scholar]
- 43.Lopata C, Toomey JA, Fox JD, et al. Anxiety and depression in children with HFASDs: symptom levels and source differences. J Abnorm Child Psychol. 2010 Aug;38(6):765–776. doi: 10.1007/s10802-010-9406-1. [DOI] [PubMed] [Google Scholar]
- 44.Kelly AB, Garnett MS, Attwood T, Peterson C. Autism spectrum symptomatology in children: the impact of family and peer relationships. J Abnorm Child Psychol. 2008 Oct;36(7):1069–1081. doi: 10.1007/s10802-008-9234-8. [DOI] [PubMed] [Google Scholar]
- 45.Barnhill GP. Social Attributions and Depression in Adolescents with Asperger Syndrome. Focus on Autism and Other Developmental Disabilities. 2001;16(1):46–53. [Google Scholar]
- 46.Skinner SR, Ng C, McDonald A, Walters T. A patient with autism and severe depression: medical and ethical challenges for an adolescent medicine unit. Med J Aust. 2005 Oct 17;183(8):422–424. doi: 10.5694/j.1326-5377.2005.tb07108.x. [DOI] [PubMed] [Google Scholar]
- 47.Kim J, Szatmari P, Bryson S, Streiner D, Wilson F. The prevalence of anxiety and mood problems among children with autism and Asperger syndrome. Autism. 2000 Jun;4(2):117–132. [Google Scholar]
- 48.Gadow KD, Devincent C, Schneider J. Predictors of psychiatric symptoms in children with an autism spectrum disorder. J Autism Dev Disord. 2008 Oct;38(9):1710–1720. doi: 10.1007/s10803-008-0556-8. [DOI] [PubMed] [Google Scholar]
- 49.Rao U, Chen LA. Characteristics, correlates, and outcomes of childhood and adolescent depressive disorders. Dialogues Clin Neurosci. 2009;11(1):45–62. doi: 10.31887/DCNS.2009.11.1/urao. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tandon M, Cardeli E, Luby J. Internalizing disorders in early childhood: a review of depressive and anxiety disorders. Child Adolesc Psychiatr Clin N Am. 2009 Jul;18(3):593–610. doi: 10.1016/j.chc.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Janowsky DS, Davis JM. Diagnosis and treatment of depression in patients with mental retardation. Curr Psychiatry Rep. 2005 Dec;7(6):421–428. doi: 10.1007/s11920-005-0062-z. [DOI] [PubMed] [Google Scholar]
- 52.Minshawi NF. Behavioral assessment and treatment of self-injurious behavior in autism. Child Adolesc Psychiatr Clin N Am. 2008 Oct;17(4):875–886. x. doi: 10.1016/j.chc.2008.06.012. [DOI] [PubMed] [Google Scholar]
- 53.Ghaziuddin M, Alessi N, Greden JF. Life events and depression in children with pervasive developmental disorders. J Autism Dev Disord. 1995 Oct;25(5):495–502. doi: 10.1007/BF02178296. [DOI] [PubMed] [Google Scholar]
- 54.Matson JL, Rush KS, Hamilton M, et al. Characteristics of depression as assessed by the Diagnostic Assessment for the Severely Handicapped-II (DASH-II) Res Dev Disabil. 1999 Jul-Aug;20(4):305–313. doi: 10.1016/s0891-4222(99)00012-8. [DOI] [PubMed] [Google Scholar]
- 55.Taylor JL, Seltzer MM. Employment and Post-Secondary Educational Activities for Young Adults with Autism Spectrum Disorders During the Transition to Adulthood. J Autism Dev Disord. 2010 Jul 17; doi: 10.1007/s10803-010-1070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hill E, Berthoz S, Frith U. Brief report: cognitive processing of own emotions in individuals with autistic spectrum disorder and in their relatives. J Autism Dev Disord. 2004 Apr;34(2):229–235. doi: 10.1023/b:jadd.0000022613.41399.14. [DOI] [PubMed] [Google Scholar]
- 57.Solomon M, Goodlin-Jones BL, Anders TF. A social adjustment enhancement intervention for high functioning autism, Asperger's syndrome, and pervasive developmental disorder NOS. J Autism Dev Disord. 2004 Dec;34(6):649–668. doi: 10.1007/s10803-004-5286-y. [DOI] [PubMed] [Google Scholar]
- 58.Bauminger N, Shulman C, Agam G. Peer interaction and loneliness in high-functioning children with autism. J Autism Dev Disord. 2003 Oct;33(5):489–507. doi: 10.1023/a:1025827427901. [DOI] [PubMed] [Google Scholar]
- 59.Heinrich LM, Gullone E. The clinical significance of loneliness: a literature review. Clin Psychol Rev. 2006 Oct;26(6):695–718. doi: 10.1016/j.cpr.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 60.Little L. Middle-class mothers' perceptions of peer and sibling victimization among children with Asperger's syndrome and nonverbal learning disorders. Issues Compr Pediatr Nurs. 2002 Jan-Mar;25(1):43–57. doi: 10.1080/014608602753504847. [DOI] [PubMed] [Google Scholar]
- 61.Brunstein Klomek A, Marrocco F, Kleinman M, Schonfeld IS, Gould MS. Bullying, depression, and suicidality in adolescents. J Am Acad Child Adolesc Psychiatry. 2007 Jan;46(1):40–49. doi: 10.1097/01.chi.0000242237.84925.18. [DOI] [PubMed] [Google Scholar]
- 62.Constantino JN. Social Impairment. In: Hollander K, Coyle, editors. Textbook of Autism Spectrum Disorders. Arlington, VA: American Psychiatric Publishing, Inc.; 2010. [Google Scholar]
- 63.Kanne SM, Christ SE, Reiersen AM. Psychiatric symptoms and psychosocial difficulties in young adults with autistic traits. J Autism Dev Disord. 2009 Jun;39(6):827–833. doi: 10.1007/s10803-008-0688-x. [DOI] [PubMed] [Google Scholar]
- 64.Koegel RL, Mentis M. Motivation in childhood autism: can they or won't they? J Child Psychol Psychiatry. 1985 Mar;26(2):185–191. doi: 10.1111/j.1469-7610.1985.tb02259.x. [DOI] [PubMed] [Google Scholar]
- 65.Kanne SM, Abbacchi AM, Constantino JN. Multi-informant ratings of psychiatric symptom severity in children with autism spectrum disorders: the importance of environmental context. J Autism Dev Disord. 2009 Jun;39(6):856–864. doi: 10.1007/s10803-009-0694-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Constantino JN, Lavesser PD, Zhang Y, Abbacchi AM, Gray T, Todd RD. Rapid quantitative assessment of autistic social impairment by classroom teachers. J Am Acad Child Adolesc Psychiatry. 2007 Dec;46(12):1668–1676. doi: 10.1097/chi.0b013e318157cb23. [DOI] [PubMed] [Google Scholar]
- 67.Kerr DC, Lunkenheimer ES, Olson SL. Assessment of child problem behaviors by multiple informants: a longitudinal study from preschool to school entry. J Child Psychol Psychiatry. 2007 Oct;48(10):967–975. doi: 10.1111/j.1469-7610.2007.01776.x. [DOI] [PubMed] [Google Scholar]
- 68.Hurtig T, Kuusikko S, Mattila ML, et al. Multi-informant reports of psychiatric symptoms among high-functioning adolescents with Asperger syndrome or autism. Autism. 2009 Nov;13(6):583–598. doi: 10.1177/1362361309335719. [DOI] [PubMed] [Google Scholar]
- 69.Lichtenstein P, Carlstrom E, Rastam M, Gillberg C, Anckarsater H. The Genetics of Autism Spectrum Disorders and Related Neuropsychiatric Disorders in Childhood. Am J Psychiatry. 2010 Aug 4; doi: 10.1176/appi.ajp.2010.10020223. [DOI] [PubMed] [Google Scholar]
- 70.Brimacombe M, Xue M, Parikh A. Familial risk factors in autism. J Child Neurol. 2007 May;22(5):593–597. doi: 10.1177/0883073807302609. [DOI] [PubMed] [Google Scholar]
- 71.Mazefsky CA, Folstein SE, Lainhart JE. Overrepresentation of mood and anxiety disorders in adults with autism and their first-degree relatives: what does it mean? Autism Res. 2008 Jun;1(3):193–197. doi: 10.1002/aur.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Piven J, Palmer P. Psychiatric disorder and the broad autism phenotype: evidence from a family study of multiple-incidence autism families. Am J Psychiatry. 1999 Apr;156(4):557–563. doi: 10.1176/ajp.156.4.557. [DOI] [PubMed] [Google Scholar]
- 73.Hallett V, Ronald A, Rijsdijk F, Happe F. Association of autistic-like and internalizing traits during childhood: a longitudinal twin study. Am J Psychiatry. 2010 Jul;167(7):809–817. doi: 10.1176/appi.ajp.2009.09070990. [DOI] [PubMed] [Google Scholar]
- 74.Hoekstra RA, Bartels M, Hudziak JJ, Van Beijsterveldt TC, Boomsma DI. Genetic and environmental covariation between autistic traits and behavioral problems. Twin Res Hum Genet. 2007 Dec;10(6):853–860. doi: 10.1375/twin.10.6.853. [DOI] [PubMed] [Google Scholar]
- 75.Constantino JN, Todd RD. Autistic traits in the general population: a twin study. Arch Gen Psychiatry. 2003 May;60(5):524–530. doi: 10.1001/archpsyc.60.5.524. [DOI] [PubMed] [Google Scholar]