Abstract
Anopheles gambiae s.s., Anopheles arabiensis, and Anopheles funestus s.s. are the most important species for malaria transmission. Pyrethroid resistance of these vector mosquitoes is one of the main obstacles against effective vector control. The objective of the present study was to monitor the pyrethroid susceptibility in the 3 major malaria vectors in a highly malaria endemic area in western Kenya and to elucidate the mechanisms of pyrethroid resistance in these species. Gembe East and West, Mbita Division, and 4 main western islands in the Suba district of the Nyanza province in western Kenya were used as the study area. Larval and adult collection and bioassay were conducted, as well as the detection of point mutation in the voltage-gated sodium channel (1014L) by using direct DNA sequencing. A high level of pyrethroid resistance caused by the high frequency of point mutations (L1014S) was detected in An. gambiae s.s. In contrast, P450-related pyrethroid resistance seemed to be widespread in both An. arabiensis and An. funestus s.s. Not a single L1014S mutation was detected in these 2 species. A lack of cross-resistance between DDT and permethrin was also found in An. arabiensis and An. funestus s.s., while An. gambiae s.s. was resistant to both insecticides. It is noteworthy that the above species in the same area are found to be resistant to pyrethroids by their unique resistance mechanisms. Furthermore, it is interesting that 2 different resistance mechanisms have developed in the 2 sibling species in the same area individually. The cross resistance between permethrin and DDT in An. gambiae s.s. may be attributed to the high frequency of kdr mutation, which might be selected by the frequent exposure to ITNs. Similarly, the metabolic pyrethroid resistance in An. arabiensis and An. funestus s.s. is thought to develop without strong selection by DDT.
Introduction
The most exciting event in the history of mosquito control was the invention of dichloro-diphenyl-trichloroethane (DDT). The long persistence, excellent killing efficacy, and strong repellency of DDT are responsible for its considerable success in malaria control after the Second World War. Nevertheless, the first DDT resistance case in Anopheles mosquitoes was detected several years later. Furthermore, DDT resistance was responsible for the increase in the incidence of malaria in the 1960s. The number of reported malaria cases throughout the world had increased in 1977 by 2.5 times in comparison with 1973. The development of DDT resistance was one of the main factors caused the above increase [1]. Due to the failure of the malaria eradication program, the World Health Organization (WHO) has altered their policy from eradication to control. Since WHO announced the Roll Back Malaria (RBM) movement in 1998 [2], insecticide-treated nets (ITNs) have become a major tool in the RBM. In Kenya, ITNs have been mainly distributed to pregnant women and children under five years old through programs of the Kenya Ministry of Health and nongovernmental organizations (NGOs) [3], [4]. Consequently, ITN coverage for children under five years old has increased rapidly from 7% in 2004 to 67% in 2006; this increase has been associated with a 44% reduction in malaria deaths [5].
Pyrethroid is the general term for a group of synthetic chemicals that are structurally modified from natural pyrethrins derived from Chrysanthemum flowers. Most of the pyrethroids are nontoxic to mammals as compared to the insecticide groups and possess high knockdown activity against insects. Nowadays, pyrethroids are emerging as the predominant insecticides for vector control. They are used in various formulations such as long lasting insecticide-treated nets (LLIN) for the long-time prevention of mosquito bites in malaria endemic areas, indoor residual spray, and ultra-low volume (ULV) sprays for emergency control of dengue vectors. In fact, pyrethroids comprise 40% of the insecticides used annually on a global level for indoor residual spraying against malaria vectors and 100% of the WHO-recommended insecticides for the treatment of mosquito nets [6].
The resistance of vector mosquitoes is one of the main obstacles against effective vector control. Pyrethroid resistance is predicted to be a major problem for the vector control program since at present there are no suitable chemical substitutes for pyrethroids. In order to effectively manage pyrethroid resistance, the establishment of a feasible insecticide management system and a regular monitoring system of insecticide susceptibility will be essential. More than 90% of the current annual malaria incidence is found in Africa where the major vectors are Anopheles gambiae Giles s.l. that breeds in both temporal stagnant and permanent water pools. Two point mutations at the voltage-gated sodium channel have been found to be associated with knockdown resistance (kdr) to DDT and pyrethroids in An. gambiae. One mutation involves a leucine (TTA)-phenylalanine (TTT) transversion at residue 1014 of the gene (L1014F), and the other mutation involves a leucine (TTA)-serine (TCA) transition in the same residue (L1014S) [7]. The L1014F mutation is only present at west of 10°W latitude in Africa, while L1014S is found in areas both west and east of 10°W, including Kenya [7].
Recently, a causal relationship between the high coverage of ITNs due to mass campaigns and the increase in the kdr frequency in An. gambiae s.s. has been reported [8], [9], [10]. The two point mutations are, therefore, important as indices of knockdown resistance in An. gambiae s.s., and periodical analyses of these mutations are essential for monitoring the development of pyrethroid resistance. Anopheles arabiensis Patton and Anopheles funestus Giles s.s., the former breeds in the same habitat as An. gambiae s.s. and the latter prefers to breed in permanent fresh waters with water weeds, are the second most common malaria vectors in Africa. The above point mutations, however, have been reported to be rare in An. arabiensis [8], [11], [12], [13], [14], [15] with the exception of 1 Ethiopian case [16], [17], and no such kdr mutation has been reported in An. funestus s.s. [18], [19], [20], [21]. On the contrary, evidence of metabolic resistance caused by the enhancement of P450 or glutathione S-transferase activity in these species has been reported [12], [20], [21].
The objective of the present study was to monitor the pyrethroid susceptibility in 3 major malaria vectors, An. gambiae s.s., An. arabiensis, and An. funestus, in a highly malaria endemic area in western Kenya and to elucidate the mechanisms of pyrethroid resistance in these species.
Materials and Methods
Study area
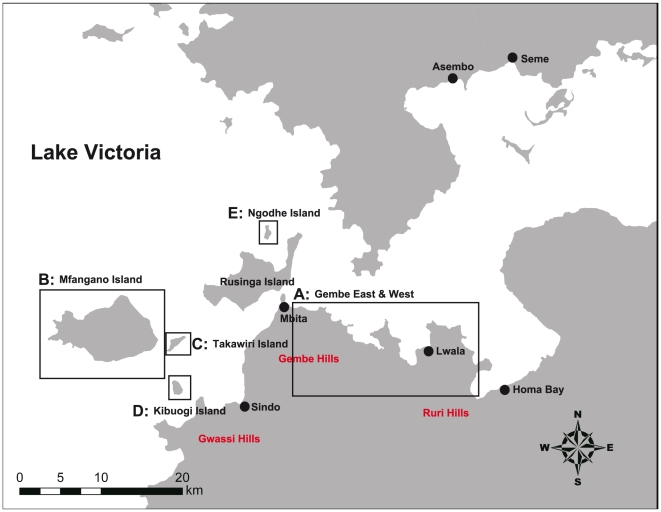
Gembe East and West, Mbita Division, and 4 main western islands, Mfangano, Takawiri, Kibuogi, and Ngodhe, in the Suba district of the Nyanza province in western Kenya were used as study area (Figure 1). The Suba district has a population of 214,463 and an area of 1,063 km2 (2010). The district has 2 rainy seasons and is drier in the eastern part towards the Usao and Waondo locations and wetter towards the higher altitudes in the western parts of Gwassi hill and Mfangano Island. In the highlands, the rainfall ranges between 800–1900 mm per annum, while the lower area receives 800–1200 mm. The rainfall pattern in the area is bimodal, with the long rainy season occurring from March through May, and the short rainy season occurring in November and December. Malaria infection peaks briefly in June, following the long rains and more steadily between September and February [22]. The mean temperature is 25°C while the maximum temperature is 30°C, and humidity is relatively high.
Figure 1. Map of study area (A, Gembe East & West; B, C, D, E, western islands).
The Suba district is one of the focal points identified as a high vector transmission area in Kenya, and more than 50% of the population is exposed to ≥40% PfPR2–10 (Plasmodium falciparum parasite rate corrected to a standard age-range of 2 to less than 10 years old) [23]. A renewed effort to increase the coverage of effective preventative measures such as ITNs and combined vector control approaches have been adopted in this area. The Akado Medical Centre Project Mosquito Net and Power of Love Foundation in partnership with World Swim Against Malaria distributed 6,000 ITNs to children under five and pregnant women in the Gembe area. This increased the number of mosquito nets at least 3 fold, from 17% to 52% ITN coverage.
Larval collection
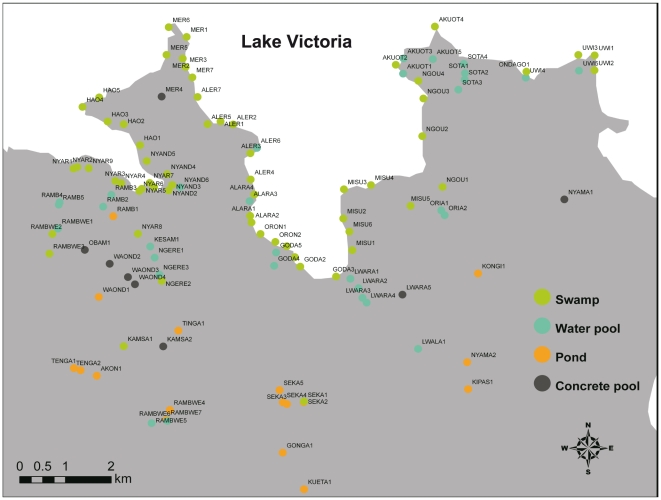
The typical breeding habitats of mosquitoes, such as small temporal pools, ponds, swamps, concrete pools, etc., in the Gembe East area were surveyed (Figure 2). Larvae were collected by dipping at each breeding site and brought to the laboratory for rearing and/or susceptibility testing. The geographical information, such as longitude, latitude, and elevation at each breeding site were recorded using a GPS unit. Larval collection was performed from May 5 to July 15, 2009.
Figure 2. Mosquito breeding sites in Gembe East where larval collections were performed.
Adult collection and rearing of F1 progenies
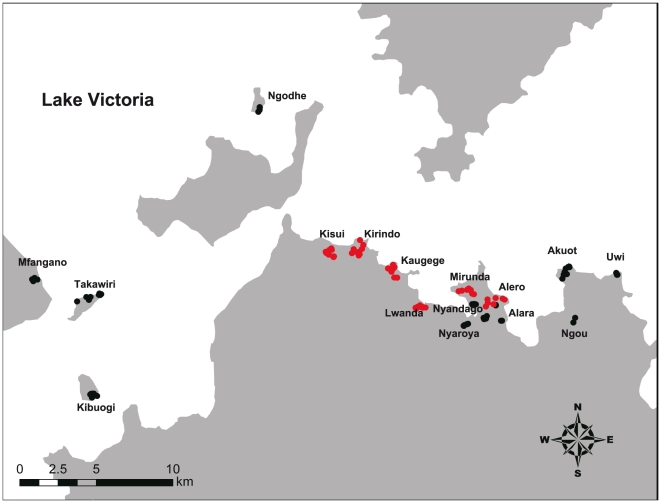
Indoor mosquito collection was performed in the morning (7:00–10:00) by 2 conventional methods, namely, the pyrethrum spray sheet collection method (PSC) [24] (Gembe West and East area) and the aspiration with the battery-powered aspirator method (Cat. No. 2809C; BioQuip Products; Rancho Dominguez, CA, USA) (Gembe East and western islands area, Figure 3). After collection by aspiration, live blood-fed or gravid females were individually confined into a 20 ml glass vial with 2 ml of water and a strip of filter paper (ca 3×4 cm) was placed on the side of the vial to collect the eggs. Hatched larvae were reared with the lake water to obtain F1 larvae and adults for susceptibility testing. Larvae were fed with a mixture of powdered animal food (CE-2; Clea Tokyo, Japan, Inc.) and dried yeast (Ebios®; Mitsubishi Tanabe Pharma, Tokyo, Japan). Water cabbage (Pistia stratiotes L.) was added to the water for rearing An. funestus larvae. Adult collection was performed from October 1 to December 9, 2009 (Gembe East area), from February 1 to March 8, 2010 (Gembe East and western islands area), from April 19 to July 3, 2010 (Gembe East and West and western islands area), from September 13 to November 4, 2010 (Gembe East and West and western islands area), and from February 4 to March 5, 2011 (western islands area).
Figure 3. Adult collection sites.
Black and red circles indicate aspirator and pyrethrum spray sheet collection sites, respectively.
Simplified knockdown bioassay using the mosquito larvae
The bioassay for the assessment of knockdown susceptibility was carried out on the day of collection by using the mosquito larvae obtained from the collection sites from which we could procure an adequate number of insects according to the simplified method previously described by Kawada et al. [25]. D-T80-allethrin was used for the test, since this chemical is one of the most conventional pyrethroid used for mosquito control and its high knock down activity is highly useful to the knock down bioassay. The larvae collected from each collection site were briefly identified on the day of collection, and fourth instar larvae of An. gambiae s.l., which occasionally might comprise a mixed population of An. gambiae s.s. and An. arabiensis individuals, were used for the susceptibility test. Each larva was individually placed in a glass vial with 20 ml of water. An emulsifiable concentrate of 90% d-T80-allethrin was diluted with water to obtain a 250-ppm solution. After releasing the larva, 32 or 8 µl of the solution was added in each vial to obtain a concentration of 0.4 and 0.1 ppm, respectively. At most, 20 larvae from each site were used for each concentration regime. Knockdown of the larvae was observed for 30 min. Larvae that sank to the bottom of the glass vial and could not swim, float, or were paralyzed were judged as knocked down larvae; the time to knockdown was recorded for each larva. After the test, each larva was placed in a 1.5-ml plastic vial containing ethanol solution for identification at a later time. The median knockdown times (KT50s), i.e., the time required for 50% knockdown, were scored according to the following 6 categories: 1, <5 min; 2, 5–10 min; 3, 10–15 min; 4, 15–20 min; 5, 20–30 min; and 6, >30 min. The susceptibility index was calculated as the product of the scores at 0.1 and 0.4 ppm. Thus, mosquito colonies with susceptibility index of 1 were considered to be the most susceptible, and those with susceptibility index of 36 were considered to be the least susceptible to d-allethrin. The larval bioassay was also performed for the larvae of F1 progeny to investigate the correlation in pyrethroid susceptibility between larvae and adults.
Insecticide susceptibility test for adults
1. Susceptibility test with WHO test tubes
Insecticide impregnated papers were prepared and adult susceptibility tests using WHO test tube kits were performed according to the WHO instructions (WHO/CDS/CPC/MAL/98.12). Insecticide impregnated papers, 0.75% permethrin (0.027 mg/cm2), 0.75% permethrin+0.75% piperonyl butoxide (PBO) (0.027 mg+0.027 mg/cm2), and 4% DDT (0.144 mg/cm2), were used for the tests. Female mosquitoes (1- to 3-day-old unfed F1 adults reared from the eggs of field collected females) were released in the WHO test tubes in order to expose them to the surface of an insecticide-impregnated paper for 1 hr; meanwhile, the time for knockdown was recorded. After exposure, the insects were transferred to the clean tube, fed with cotton soaked with 5% glucose solution, and mortality was recorded after 1 day. KT50 and average mortality for the mosquito colony were calculated. After the test, the insects were individually reserved in a 1.5-ml plastic vial with silica gel granules until detection of the kdr mutation.
2. Susceptibility test by topical application
Technical grades of permethrin and PBO were used for the study. Female mosquitoes (1- to 3-day-old unfed F1 adults reared from the eggs of field collected females) were anesthetized briefly with carbon dioxide and were put on the metal cooling plate (Cool Plate NCP-2215; Nissin Scientific Corp, Tokyo, Japan), the surface temperature of which was maintained 4°C to maintain the anesthesia. A 0.25-µl acetone solution of the test chemical was topically applied to the dorsal mesothorax of 1- to 3-day-old female adults by using a Hand Microapplicator (Burkard Manufacturing Co., Ltd, Rickmansworth, UK). Treated insects were kept in a plastic cup, the bottom of which was lined with a filter paper, and fed with 5% glucose solution. Mortality was observed 24 h after treatment and LD50 (median lethal dosage) was calculated.
Species identification
Mosquito larvae and collected adults were examined microscopically to distinguish An. gambiae s.l. and An. funestus s.l. from the other anophelines on the basis of the identification keys of Gillies and Coetzee [26]. Individual species within An. gambiae s.l. and An. funestus s.l. were identified using the multiplex polymerase chain reaction (PCR) method described by Scott et al. [27] and Koekemoer et al. [28].
Detection of point mutations in the voltage-gated sodium channel
In order to verify the presence of point mutations at L1014 in An. gambiae s.s., An. arabiensis, and An. funestus s.s., PCR and direct DNA sequencing was conducted. The whole body of a larva or 2 to 3 legs of an adult were placed in a 1.5-ml PCR reaction tube. The sample was homogenized in a mixed solution of extraction solution (20 µl)+tissue preparation solution (5 µl) (REDExtract-N-AmpTM Tissue PCR Kit; SIGMA, St. Louis, MO, USA) for extraction of DNA. The solution was heated at 95°C for 3 min and neutralized. Initial fragment amplification was carried out using primers AGKF1(CATGATCTGCCAAGATGGAA) and AGKR1 (GTTGGTGCAGACAAGGATGA) for An. gambiae s.l.; and AFF1 (ACCAAGATCTGCCAAGATGG) and AFR1 (TGGTGCAGACAAGGATGAAG) for An. funestus s.s., respectively. The PCR mixture contained 4 µl of REDExtract-N-AmpTM ReadyMix (SIGMA), 0.5 µM of each primer, and 1 µl of the DNA template in a total volume of 10 µl. PCR was performed under the following conditions: 94°C for 3 min and 35 cycles of 94°C for 15 s, 55°C for 30 s, 72°C for 30 s, and 72°C for 10 min (for An. gambiae s.l.) or 94°C for 3 min and 35 cycles of 94°C for 15 s, 45°C for 30 s, 72°C for 30 s, and 72°C for 10 min (for An. funestus s.s.). The amplified fragments of the expected size were purified using ExoSAP-IT (USB Corporation, Cleveland, OH, USA) at a temperature of 37°C for 30 min and then 80°C for 15 min. DNA sequencing was carried out using primers Dg1 (TGGATHGARWSHATGTGGGAYTG) for An. gambiae s.l. and Dg3 (TGGATCGAATCCATGTGGGACTG) for An. funestus s.s., respectively. A BigDye Terminator v. 3.1 Cycle Sequencing Kit (Applied Biosystems Japan Ltd., Tokyo, Japan) was used for DNA sequencing according to the manufacturer's instructions. Direct DNA sequencing was performed by using the 3730 DNA Analyzer (Applied Biosystems). The electropherogram of the targeted amino acid replacement was analyzed by MEGA 4.0 public domain software (http://www.megasoftware.net/). All new data were deposited in GenBank (AB627099–AB627102).
Statistical analysis
A digital map in shapefile format (Kenya-Boundaries, FAO Africover, http://www.africover.org/index.htm) was used for mapping of the collection sites. The geographical positions and the susceptibility index of larvae were plotted on the map by using ArcGIS 9.3 (ESRI Japan Corp, Tokyo, Japan.). Median knockdown times (KT50s) and lethal dosages (LD50s) were calculated by using the Bliss' probit method [29].
Results
Larval susceptibility against d-allethrin by simplified knockdown bioassay
Larvae of An. gambiae s.l. and An. funestus s.l. were collected from 82 breeding sites among the 117 sites surveyed. Larvae of An. arabiensis, which were collected in 74 sites, were common and dominant in the Gembe East area. The number of breeding sites where An. gambiae s.s. and An. funestus s.l. were collected, 4 and 4 sites respectively, were significantly fewer than those of An. arabiensis. Concrete pools, normally located in large permanent building site such as schools, seemed to be good breeding places for An. arabiensis larvae as well as the other culicine larvae (Table 1). A large number of An. pharoensis Theobald and a small number of An. coustani Laveran s.l. larvae were also collected at several sites as non-target species. Although quantitative sampling was not conducted and the sampling was mainly concentrated on the collection of late instar larvae for bioassay purposes, An. arabiensis larvae occupied 99% in the total number of collected larvae (1194), while the numbers of An. gambiae s.s. and An. funestus s.l. larvae were few (Table 2). The larval bioassay was, therefore, carried out solely using An. arabiensis larvae.
Table 1. Allelic frequency of L1014S mutations in Anopheline mosquito larvae collected in Gembe East, Mbita, Kenya.
| Location | Breeding Place1) | Species - Allelic frequency of L1014S (AF %) and % of homozygous of L1014S (RR %) | |||||||||||
| An. gambiae s.s. | An. arabiensis | An. funestus s.s. | An. rivulorum | ||||||||||
| N | AF % | RR % | N | AF % | RR % | N | AF % | RR % | N | AF % | RR % | ||
| Nyaroya | SW, WP | - | - | - | 124 | 0 | 0 | - | - | - | - | - | - |
| Nyandago | SW, WP | - | - | - | 78 | 0 | 0 | - | - | - | 1 | 0 | 0 |
| Mirunda | SWL, CP | 2 | 50 | 50 | 70 | 0 | 0 | - | - | - | - | - | - |
| Hao | SWL | - | - | - | 18 | 0 | 0 | 2 | 0 | 0 | 5 | 0 | 0 |
| Alero | SW, SWL | - | - | - | 75 | 0 | 0 | - | - | - | - | - | - |
| Alara | SWL, WP | - | - | - | 83 | 0 | 0 | - | - | - | - | - | - |
| Orongo | SW, SWL | - | - | - | 25 | 0 | 0 | - | - | - | - | - | - |
| Godariyo | SW, SWL, WP | - | - | - | 71 | 0 | 0 | - | - | - | - | - | - |
| Misuri | SW, SWL | - | - | - | 38 | 0 | 0 | - | - | - | - | - | - |
| Ngau | SWL | - | - | - | 26 | 0 | 0 | - | - | - | - | - | - |
| Akuot | SWL, WP | - | - | - | 59 | 0 | 0 | - | - | - | - | - | - |
| Uwi | SWL, WP | - | - | - | 69 | 0 | 0 | - | - | - | - | - | - |
| Lambwe | SW, WP, PD | - | - | - | 97 | 0 | 0 | - | - | - | - | - | - |
| Kisamba | WP | 1 | 100 | 100 | 17 | 0 | 0 | - | - | - | - | - | - |
| Obambo | CP | 1 | 100 | 100 | 14 | 0 | 0 | - | - | - | - | - | - |
| Waondo | PD, CP | - | - | - | 29 | 0 | 0 | - | - | - | - | - | - |
| Kamsama | SW | - | - | - | 20 | 0 | 0 | - | - | - | - | - | - |
| Akonya | PD | - | - | - | 18 | 0 | 0 | - | - | - | - | - | - |
| Ngere | SW, WP | - | - | - | 25 | 0 | 0 | - | - | - | - | - | - |
| Tinga | WP, PD | - | - | - | 20 | 0 | 0 | - | - | - | - | - | - |
| Lwara | WP, CP | - | - | - | 80 | 0 | 0 | - | - | - | - | - | - |
| Oria | WP | - | - | - | 16 | 0 | 0 | - | - | - | - | - | - |
| Sota | WP | - | - | - | 60 | 0 | 0 | - | - | - | - | - | - |
| Rambwe | PD, WP | - | - | - | 20 | 0 | 0 | - | - | - | - | - | - |
| Nyamaji | CP | - | - | - | 20 | 0 | 0 | - | - | - | - | - | - |
SW, swamp; SWL, swamp near lake shore; WP, small water pool; PD, pond; CP, concrete pool.
Table 2. Collection Data of Anopheline mosquitoes in Gembe East, Gembe West, and western islands, Kenya.
| Sampling Method | Collection Place | Date of Collection | Test Performed (generation used) | Collected species (figures in parenthesis are No. of females oviposited) | |||||
| An. arabiensis | An. gambiae s.s. | An. funestus s.s. | |||||||
| F | M | F | M | F | M | ||||
| Larval Collection (Dipping) | Gembe East | May 5–July 15, 2009 | Simplified Knockdown Assay (F0) Detection of kdr (F0) | 1182 | 4 | 2 | |||
| ( - ) | ( - ) | ( - ) | |||||||
| Adult Collection (Aspiration) | Gembe East | Oct 1–Dec 9, 2009 | WHO Tube Test for Permethrin and DDT (F1) Detection of kdr (F0 & F1) | 67 | 34 | 1 | 0 | 14 | 0 |
| (40) | (0) | (10) | |||||||
| Western islands | Sept 13–Nov 4, 2010 Feb 4–Mar 5, 2011 | 0 | 0 | 4 | 0 | 0 | 0 | ||
| ( - ) | (3) | ( - ) | |||||||
| Adult Collection (Aspiration) | Gembe East | Feb 1–Mar 8, 2010 | WHO Tube Test for Permethrin and PBO (F1) Detection of kdr (F0 & F1) | 30 | 7 | 1 | 0 | 74 | 11 |
| (17) | (0) | (32) | |||||||
| Western islands | 4 | 1 | 28 | 15 | 1 | 0 | |||
| (1) | (5) | (0) | |||||||
| Adult Collection (Aspiration) Larval Collection (Dipping) | Gembe East | Apr 19–July 3, 2010 | Topical Application for Permethrin and PBO (F1) Detection of kdr (F0 & F1) | 671) | 141) | 8 | 3 | 686 | 241 |
| (35) | (1) | (137) | |||||||
| Western islands | 6 | 0 | 81 | 12 | 3 | 0 | |||
| (4) | (33) | (0) | |||||||
| Adult Collection (Pyrethrum Spray Sheet) | Gembe East | Apr 19–July 3, 2010 Sept 13–Nov 4, 2010 | Detection of kdr (F0) | 0 | - | 0 | - | 1922) | - |
| ( - ) | ( - ) | ( - ) | |||||||
| Gembe West | 165 | - | 4 | - | 2632) | - | |||
| ( - ) | ( - ) | ( - ) | |||||||
Additionally, larvae were collected in Nyaroya and emerged 189 female adults were used for topical application test.,
Additionary, 59 females and 16 males, and 7 females of An. rivurolum were collected in Gembe East and Gembe West, respectively.
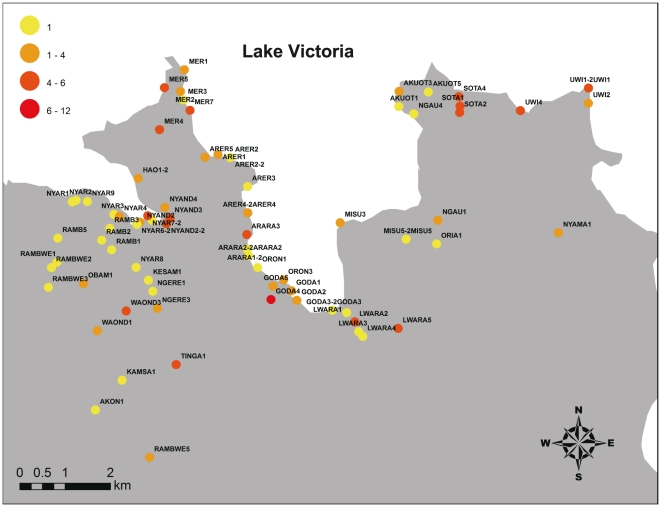
Figure 4 shows the distribution of the susceptibility index in field-collected An. arabiensis larvae against d-allethrin in Gembe East area. Almost all the larval colonies of An. arabiensis showed low susceptibility indices (<6) except for 1 colony collected in Godariyo (Site ID GODA4) of which the index was 12. Furthermore, not a single point mutation at L1014 was observed in all larval colonies of An. arabiensis (Table 1). On the other hand, however, among the 4 An. gambiae s.s. larvae collected at Mirunda, Kisamba, and Obambo, 3 larvae had homozygous L1014S mutations.
Figure 4. Distribution of larval susceptibility index for An. arabiensis collected in Gembe East area.
Adult susceptibility against permethrin and DDT by WHO tube test
F1 progenies of mosquitoes collected from October 1 to December 8, 2009 in the Gembe East area and those collected from September 13 to November 4, 2010 and February 4 to March 5, 2011 in the western islands were used for the test (Table 2). F1 progenies from 22 female An. arabiensis collected in 9 different houses, 4 female An. gambiae s.s. collected in different houses, and 7 female An. funestus s.s. collected in 5 different houses were tested. The data for F1 progenies of females collected from the same house were mixed for the calculation of KT50 and mortality. Additionally, one laboratory colony of An. gambiae s.s. collected in Lwanda, Mbita in 2002 that has been maintained in the Thomas Odhiambo campus of the International Center of Insect Physiology and Ecology (ICIPE) was also used as a reference. The allelic frequency and the rate of homozygous L1014S point mutations in this colony were relatively low (6.3% and 0%). Table 3 shows the insecticide susceptibility of F1 larvae and female adults by the simplified larval knockdown assay and WHO tube test. Not a single point mutation at L1014 was observed in all F1 colonies of An. arabiensis and An. funestus s.s. Adult susceptibility of both species against DDT seemed to be high, showing a >80% mortality and a KT50 of <60 min. On the other hand, the susceptibilities against permethrin were relatively low in both species. In total, 7 (77.8%) and 3 (60%) colonies showed KT50s of >60 min and all colonies showed mortalities of <80% in An. arabiensis and An. funestus, respectively. Larval susceptibility indices were low (<12) in almost all colonies except for 1 colony in An. funestus s.s. Although the sample sizes were small, there seemed to be no correlation between the larval susceptibility indices and adult mortality against permethrin in An. arabiensis. On the other hand, An. gambiae s.s. colonies, except for laboratory colony (ICIPE) and one colony with no homozygous L1014S collected in Nyandago (NYAND 8), showed low mortality and a KT50s of >60 min against both permethrin and DDT, indicating that the positive correlation with larval susceptibility for these colonies (susceptibility indices were >30).
Table 3. Susceptibility against permethrin and DDT of F1 larvae and female adults produced by individual blood-fed females collected in houses in Gembe East, Mbita and western islands, Kenya.
| Species | House ID2) , 3) | F1 larvae | F1 adults (WHO Tube Test) | |||||||
| N | Susceptibility Index (d-allethrin) | Permethrin 0.75% | DDT 4% | RR %1) | ||||||
| N | KT50 (min.) | % Mortality | N | KT50 (min.) | % Mortality | |||||
| An. arabiensis | NYAND 6 | 24 | 6 | 20 | 45–60 | 75.0 | 10 | 20–30 | 100 | 0 |
| NYAND 8 | 26 | 6 | 26 | >60 | 48.0 | 17 | 29.1 | 100 | 0 | |
| NYAND 11 | 30 | 6 | 30 | >60 | 30.0 | 25 | 34.2 | 100 | 0 | |
| NYAND 13 | 10 | 6 | 4 | >60 | 75.0 | - | - | - | 0 | |
| NYAR 1 | - | - | 13 | >60 | 23.1 | 12 | 30–45 | 100 | 0 | |
| NYAR 3 | 10 | 6 | 13 | 47.5 | 76.9 | 10 | 28.1 | 100 | 0 | |
| NYAR 5 | 74 | 12 | 45 | >60 | 64.4 | 33 | 41.0 | 100 | 0 | |
| NYAR 6 | 14 | 6 | 10 | >60 | 50.0 | 10 | 30–45 | 100 | 0 | |
| NYAR 8 | 10 | 12 | 10 | >60 | 44.4 | 10 | 27.3 | 100 | 0 | |
| An. gambiae s.s. | ICIPE4) | 40 | 2 | 26 | 38.1 | 100 | 21 | 30.2 | 100 | 0 |
| NYAND 8 | - | - | 3 | >60 | 33.3 | 3 | 45–60 | 100 | 0 | |
| MFA 1 | 20 | 36 | 32 | >60 | 50.0 | 25 | >60 | 56.0 | 100 | |
| MFA 6 | 14 | 36 | 27 | >60 | 0 | 28 | >60 | 13.8 | 100 | |
| TAKA 4 | 8 | 30 | 15 | >60 | 14.3 | 15 | >60 | 60.0 | 100 | |
| An. funestus s.s | NYAND 11 | - | - | 2 | 30–45 | 50.0 | - | - | - | 0 |
| NYAR 1 | 10 | 6 | 16 | >60 | 26.7 | 12 | 32.6 | 83.3 | 0 | |
| NYAR 3 | - | - | 12 | >60 | 54.5 | 1- | 30–45 | 100 | 0 | |
| NYAR 7 | 20 | 36 | 8 | 30.6 | 62.5 | 4 | 20.8 | 100 | 0 | |
| NYAR 8 | - | - | 1 | >60 | 0 | - | - | - | 0 | |
% of homozygous L1014S mutation,
Collection site - House No.,
NYAND, Nyandago; NYAR, Nyaroya; MFA, Mfangano; TAKA, Takawiri,
Laboratory colony reared in ICIPE since the collection at Lwanda, Mbita in 2002.
Synergism of permethrin and PBO by WHO tube test
F1 progenies of mosquitoes collected from February 1 to March 8, 2010 in the Gembe East area and western islands were used for the test (Table 2). F1 progenies from 18 female An. arabiensis collected in 12 different houses, 5 female An. gambiae s.s. collected in 4 different houses, and 4 female An. funestus s.s. collected in 4 different houses were tested. The data for F1 progenies of females collected from the same house were mixed for the calculation of KT50 and mortality. The results are shown in Table 4. All colonies of the 3 species showed a KT50s of >60 min and 17 (94.4%) colonies of An. arabiensis and all colonies of An. gambiae s.s. and An. funestus s.s. showed mortalities of <80% when they were exposed to permethrin 0.75% impregnated paper, indicating the high resistance of these species to permethrin. On the contrary, faster knockdown and higher mortality were observed in the test when female adults of the same colonies were exposed to permethrin+PBO 0.75/0.75% paper. All colonies and 3 (75%) colonies of An. arabiensis and An. funestus s.s. showed KT50s of <60 min, and 14 (77.8%) colonies of An. arabiensis and 2 (50%) colonies of An. funestus s.s. showed mortalities of >80% in this case, indicating that permethrin+PBO showed high synergism to the above 2 species. The reaction of An. gambiae s.s., on the other hand, was different from those of the other species. Although some improvement in mortality was observed (>80% mortality in 2 of 5 colonies), there was no improvement in knockdown activity by the synergist in this species. Furthermore, An. gambiae s.s. colonies had L1014S point mutations at high frequency, while not a single point mutation at L1014 was observed in all F1 colonies of An. arabiensis and An. funestus s.s.
Table 4. Susceptibility against permethrin and permethrin/PBO of F1 female adults produced by individual blood-fed females collected in houses in Gembe East, Mbita, and western islands, Kenya.
| Species | House ID2) , 3) | WHO Tube Test (F1 adult) | ||||||
| Permethrin 0.75% | Permethrin/PBO 0.75/0.75% | RR %4) | ||||||
| N | KT50 (min.) | % Mortality | N | KT50 (min.) | % Mortality | |||
| An. arabiensis | NYAR 3 | 26 | >60 | 47.6 | 23 | 24.8 | 90.9 | 0 |
| NYAR 5 | 14 | >60 | 25.0 | 15 | 26.0 | 100 | 0 | |
| NYAR 10 | 25 | >60 | 24.0 | 32 | 26.8 | 93.8 | 0 | |
| NYAND 8 | 15 | >60 | 0 | 16 | 18.0 | 100 | 0 | |
| AKU 1 | 12 | >60 | 30.0 | 13 | 16.3 | 100 | 0 | |
| AKU 2 | 14 | >60 | 7.1 | 17 | 42.1 | 70.6 | 0 | |
| AKU 3 | 12 | >60 | 8.3 | 13 | 20.3 | 84.6 | 0 | |
| AKU 4 | 12 | >60 | 0 | 12 | 20.2 | 100 | 0 | |
| NGOU 2 | 3 | >60 | 0 | 3 | 30–45 | 66.7 | 0 | |
| UWI 2 | 12 | >60 | 16.7 | 13 | 31.3 | 76.9 | 0 | |
| TAKA 2 | 2 | >60 | 0 | 3 | 24.5 | 33.3 | 0 | |
| KIBU 1 | 17 | >60 | 55.6 | 18 | 18.2 | 100 | 0 | |
| An. gambiae s.s. | ICIPE1) | 26 | 38.1 | 100 | 20 | 17.0 | 100 | 0 |
| TAKA 1 | 25 | >60 | 8.0 | 28 | >60 | 84.6 | 100 | |
| KIBU 2 | 3 | >60 | 0 | 5 | >60 | 0 | 75 | |
| MFA 3 | 15 | >60 | 46.7 | 12 | >60 | 41.6 | 91.7 | |
| An. funestus s.s. | NYAND 6 | 2 | >60 | 0 | 2 | 15–20 | 100 | 0 |
| NYAR 3 | 11 | >60 | 30.0 | 11 | 28.3 | 54.5 | 0 | |
| NYAR 4 | 1 | >60 | 0 | 2 | >60 | 50.0 | 0 | |
| NYAR 10 | 4 | >60 | 0 | 5 | 36.7 | 100 | 0 | |
Laboratory colony reared in ICIPE since the collection at Lwanda, Mbita in 2002,
Collection site - House No.,
NYAR, Nyaroya; NYAND, Nyandago; AKU, Akuot, TAKA, Takawiri; KIBU, Kibuogi; MFA, Mfangano,
% of homozygous L1014S mutants.
Synergism of permethrin and PBO by topical application
F1 progenies of mosquitoes collected and female adults emerged from the larvae collected in Nyaroya from April 19 to July 3, 2010 in the Gembe East area and western islands were used for the test (Table 2). By aspirator collections of adult mosquitoes in the Gembe East area, An. arabiensis, An. gambiae s.s., and An. funestus s.s. were collected in 22 houses. Finally, An. gambiae s.s. were collected in 22 houses in the 4 western islands, while the other 2 species were few. F1 progenies from the same village were mixed and used for the topical application test. For evaluation of a synergism, a mixed solution of PBO and permethrin, in which the concentration of PBO was fixed (1.25 µg/female), was topically applied to the females of the same colony.
Table 5 shows the LD50s of permethrin for village-based groups of F1 progenies of An. arabiensis, An. gambiae s.s., and An. funestus s.s. Reduction in LD50s by PBO treatment was prominent in An. arabiensis and An. funestus s.s., and the synergic effects (Ratio P/B) for both species were >20. The synergic effect of PBO in An. gambiae s.s., on the other hand, was lower than those in the above 2 species (<10). Anopheles gambiae s.s. colonies had L1014S point mutations at high frequency (70.4–100%), while not a single point mutation at L1014 was observed in all F1 colonies of An. arabiensis and An. funestus s.s.
Table 5. Susceptibility against permethrin and permethrin/PBO of F1 female adults produced by individual blood-fed females collected in houses in Gembe East, Mbita, and western islands, Kenya by topical application.
| Species | Location1) | Permethrin (P) | Permethrin+PBO (1.25 µg) (B) | % RR4) | RatioP/B | ||||||
| LD50 (µg/female) | 95% C.L. | Slope | N | LD50(µg/female) | 95% C.L. | Slope | N | ||||
| An. arabiensis | Nyandago | 0.017 | (0.0097–0.026) | 3.0 | 51 | 0.00039 | - | 1.2 | 30 | 0 | 44 |
| Nyaroya2) | 0.092 | (0.063–0.16) | 2.0 | 99 | 0.0042 | (0.0023–0.012) | 2.3 | 90 | 0 | 22 | |
| Nyaroya | 0.023 | (0.060–0.045) | 1.3 | 67 | 0.00059 | (0.00027–0.00094) | 1.8 | 75 | 0 | 39 | |
| Alero/Alara | 0.024 | (0.0063–0.046) | 2.1 | 36 | 0.00042 | - | 1.1 | 27 | 0 | 57 | |
| Akuot | 0.011 | (0.00041–0.017) | 2.3 | 30 | 0.00032 | (0.000066–0.00075) | 1.1 | 28 | 0 | 34 | |
| Mfangano | 0.020 | - | 2.8 | 35 | 0.00029 | - | 1.7 | 38 | 0 | 69 | |
| An. gambiae s.s. | ICIPE3) | 0.0030 | (0.0023–0.0035) | 2.5 | 182 | 0.00062 | (0.00024–0.00097) | 1.1 | 151 | 0 | 4.8 |
| Ngodhe | 0.036 | (0.022–0.057) | 1.9 | 66 | 0.0047 | (0.0026–0.0088) | 1.4 | 80 | 87.6 | 7.7 | |
| Takawiri | 0.057 | (0.015–0.91) | 0.89 | 36 | 0.015 | (0.0074–0.023) | 4.3 | 41 | 92.5 | 3.8 | |
| Mfangano | 0.15 | - | 1.0 | 54 | 0.020 | - | 3.8 | 62 | 70.4 | 7.5 | |
| Kibuogi | 0.078–0.16 | - | - | 36 | 0.044 | (0.012–0.094) | 2.4 | 40 | 100 | 1.8–3.6 | |
| An. funestus s.s. | Nyandago | 0.018 | - | 3.4 | 31 | 0.00031 | - | 2.3 | 17 | 0 | 58 |
| Nyaroya | 0.012 | (0.0081–0.021) | 3.9 | 33 | 0.00051 | - | 2.3 | 26 | 0 | 24 | |
Location where parental females were collected,
Collected as larvae,
Laboratory colony reared in ICIPE since the collection at Lwanda, Mbita in 2002,
% of homozygous L1014S.
Allelic frequency of L1014S mutations in Anopheline mosquitoes collected in the study area
The allelic frequencies and percentages of homozygous L1014S mutations in An. arabiensis, An. gambiae s.s., An. funestus s.s., and An. rivulorum collected in Gembe East and West and the western islands are shown in Table 6. The West African type mutation, L1014F, was not detected in our study. Not a single L1014S mutation was detected in An. arabiensis (208 females and 77 males) and An. funestus s.s. (613 females and 108 males). Significantly high allelic frequencies (>90%) and percentages of homozygous L1014S mutations (>80%), on the contrary, were detected in An. gambiae s.s. High allelic frequency in the L1014S mutation seemed to be equally detected in An. gambiae s.s. collected in the inland areas as well as those collected in the islands, even though the number of collection was small.
Table 6. Allelic frequency of L1014S mutations in Anopheline mosquito adults collected in Gembe East and Gembe West, Mbita, and western islands, Kenya.
| Species | Location | Female | Male | ||||
| N | AF %1) | RR %2) | N | AF % | RR % | ||
| An. arabiensis | Nyandago | 53 | 0 | 0 | 27 | 0 | 0 |
| Nyaroya3) | 50 | 0 | 0 | 23 | 0 | 0 | |
| Nyaroya | 76 | 0 | 0 | 22 | 0 | 0 | |
| Alero/Alala | 5 | 0 | 0 | 2 | 0 | 0 | |
| Akuot | 12 | 0 | 0 | 1 | 0 | 0 | |
| Ngou | 2 | 0 | 0 | - | - | - | |
| Uwi | 1 | 0 | 0 | 1 | 0 | 0 | |
| Kirindo | 10 | 0 | 0 | - | - | - | |
| Kaugege | 50 | 0 | 0 | - | - | - | |
| Lwanda | 104 | 0 | 0 | - | - | - | |
| Mfangano | 4 | 0 | 0 | 1 | 0 | 0 | |
| Takawiri | 5 | 0 | 0 | - | - | - | |
| An. gambiae s.s. | ICIPE4) | 405) | 6.3 | 0 | - | - | - |
| Nyandago | 2 | 100 | 100 | 1 | 0 | 0 | |
| Nyaroya | 2 | 0 | 0 | - | - | - | |
| Akuot | 6 | 100 | 100 | 2 | 100 | 100 | |
| Kaugege | 1 | 100 | 100 | - | - | - | |
| Lwanda | 2 | 50 | 50 | - | - | - | |
| Takawiri | 40 | 93.8 | 92.5 | 6 | 66.7 | 66.7 | |
| Ngodhe | 35 | 92.9 | 91.4 | 3 | 100 | 100 | |
| Mfangano | 24 | 95.9 | 91.7 | 18 | 91.7 | 83.3 | |
| Kibuogi | 8 | 93.8 | 87.5 | - | - | - | |
| An. funestus s.s. | Nyandago | 221 | 0 | 0 | 93 | 0 | 0 |
| Nyaroya | 164 | 0 | 0 | 12 | 0 | 0 | |
| Mirunda | 95 | 0 | 0 | - | - | - | |
| Akuot | 12 | 0 | 0 | 1 | 0 | 0 | |
| Ngou | 5 | 0 | 0 | - | - | - | |
| Alero/Alala | 117 | 0 | 0 | 3 | 0 | 0 | |
| Kaugege | 105 | 0 | 0 | - | - | - | |
| Lwanda | 144 | 0 | 0 | - | - | - | |
| Kirindo | 10 | 0 | 0 | - | - | - | |
| Kisui | 1 | 0 | 0 | - | - | - | |
| Mfangano | 1 | 0 | 0 | - | - | - | |
| Takawiri | 2 | 0 | 0 | - | - | - | |
| An. rivulorum | Nyandago | 54 | 0 | 0 | 15 | 0 | 0 |
| Nyaroya | 4 | 0 | 0 | 1 | 0 | 0 | |
| Mirunda | 1 | 0 | 0 | - | - | - | |
| Lwanda | 6 | 0 | 0 | - | - | - | |
| Kirindo | 1 | 0 | 0 | - | - | - | |
Allelic frequency of L1014S mutations,
% of homozygous L1014S mutations,
Collected as larvae,
Laboratory colony reared in ICIPE since the collection at Lwanda, Mbita in 2002,
Tested with larvae.
Discussion
By the collection data in the present study, An. gambiae s.s. dominated in the 4 western islands, while An. arabiensis dominated in the inland areas of Gembe East and West. In the study area, however, An. gambiae s.s. had been a dominant species since the end of 20th century [30]. Recently, Bayoh et al. [10] reported the same inequality in the 2 species in western Kenya, finding that the frequency of An. gambiae s.s. varied by site with frequencies of <15% at sites west of Kisumu and along the lakeshore (Asembo and Kisian) but frequencies of >80% at sites further from the lakeshore (Busia, Bungoma, Kakamega, and Malaba). The authors also reported that the frequency of An. gambiae s.s. declined at 2 sites along the lakeshore (Asembo and Kisian) after 1996 in association with the rollout of LLINs. The study area of the present report was located in the south of the above area on the opposite side of Lake Victoria. Similar unknown ecological, meteorological, or artificial factors, therefore, seem to relate to these phenomena. Mathias et al. [9] also stated that the East African kdr allele (L1014S) coincidentally increased in frequency during the past decade in An. gambiae s.s. in western Kenya, most of which are homozygous kdr allele, as household ownership of insecticide-treated bed nets increased regionally. The same correlation between the increase in L1014S frequency and increased use of ITN was reported by Stump et al. [8]. In our study, the allelic frequency of L1014S mutation in the An. gambiae s.s. colony collected in 2002 was found to be low (6.3%), while the recent wild colonies collected in several locations had high frequency (>90%). Our findings not only support the above previous reports concerning the increase in kdr frequency during the past decade, but they also clarify the lower contribution of the P450-related metabolic resistance factors in An. gambiae s.s. since the synergistic effect of PBO was significantly lower in An. gambiae s.s. than the other 2 species (Tables 4 and 5).
In contrast, P450-related pyrethroid resistance was found to be widespread in both An. arabiensis and An. funestus s.s. in the study area. According to the few reports on the evaluation of insecticide efficacy against An. gambiae s.l. by the topical application method, the LD50 of permethrin in susceptible An. gambiae s.s. is thought to be 0.0001 to 0.001 µg/female [31], [32], [33]; that finding corresponds to the LD50s of permethrin in An. arabiensis and An. funestus s.s. in the present report when it was synergized by PBO, indicating that resistance factors in the above 2 species are mainly due to P450-related enhanced metabolism (Table 5). Lack of L1014S mutation in these species also supports the above facts (Table 6). On the contrary, larval susceptibilities to d-allethrin in An. arabiensis and An. funestus s.s. were relatively high and did not correlate to adult susceptibility to permethrin (Table 3), suggesting that different metabolic mechanisms play a role in the larval and adult stages. The correlation between adult and larval susceptibility against pyrethroids seems to be common [31], [34], especially when insects have homozygous kdr mutations at high frequency [25], [35]. This is, however, not always true for all cases, since mosquitoes may develop different resistance mechanisms through different metabolic pathways in the larval and adult stages. A similar case was previously reported regarding the malathion resistance of An. arabiensis in Sudan [36], in which the authors attributed the absence of larval resistance to the house spraying as the major source of selection pressure rather than agricultural spraying. The L1014S or L1014F point mutations have been reported to be rare in An. arabiensis [8], [11], [12], [13], [14], [15] with the exception of one Ethiopian case [16], [17]. Not a single L1014S mutation in An. arabiensis was found in Chad [11], Zimbabwe [13], or Malawi [14]; only 1 heterozygous L1014S mutation was found of 572 samples in Asembo, Kenya [8] and of 54 samples in Ahero, Kenya [12]; and 9 (0.04%) homozygous and 4 (0.02%) heterozygous L1014S mutations were reported in 243 An. arabiensis in Uganda [15]. The pyrethroid resistance in An. arabiensis in Ethiopian cases [16], [17] is unique and exceptional since the West African type L1014F mutations were found at high frequency, whereas East African type mutations (L1014S) were absent. The authors suggested that the high frequency of such kdr mutations might be attributed to the long intensive use of DDT in indoor residual spraying (IRS) for malaria control and/or to the illegal extensive use of DDT for the control of agricultural pests. In contrast, the present study shows a lack of cross-resistance between DDT and permethrin in An. arabiensis (Table 3). In Nyanza province, dieldrin was reported to be administered mainly through aerial spraying especially for tsetse fly control [37], while the organized intensive spray of DDT for mosquito control was not performed in the 1970s and 1980s (Mwatele et al. personal communication), and no IRS has been administered since then. Therefore, it might not be possible to attribute the DDT participation to the causality of metabolic pyrethroid resistance in An. arabiensis in the study area, suggesting that the different selection pressure resulted in a different resistance mechanism from those in the same species in Ethiopian cases. The cross-resistance between permethrin and DDT in An. gambiae s.s. in the study area is thought to be attributed to the high frequency of kdr mutation, which might be selected by the frequent exposure to ITNs.
Recently, high levels of pyrethroid resistance in An. funestus s.s. have been reported in Uganda [18], Ghana [19], and Mozambique [20], [21]. No kdr mutation has been reported in the above reports, while evidence of metabolic resistance caused by the enhancement of P450 or glutathione S-transferase activity in these species has been reported. Morgan et al. [18] stated that their findings on pyrethroid/DDT resistance in An. funestus s.s. in Uganda were the first reports from East Africa, indicating that resistance in An. funestus s.s. might be more widespread in Africa than previously assumed. No pyrethroid resistance in An. funestus s.s. has been reported in Kenya [38], and our study may be the first report in Kenya.
Anopheles gambiae s.s., An. arabiensis, and An. funestus s.s. are the most widely distributed vectors in Kenya [39] and are thought to be the most important species for malaria transmission. It is noteworthy that the above species in the same area are found to be resistant to pyrethroids by their unique resistance mechanisms. Furthermore, it is interesting that 2 different resistance mechanisms have developed in the 2 sibling species in the same area individually, indicating the absence of gene flow between these species. The difference in biological characteristics between the 2 species might be hypothesized to explain the above. The extent of selection pressure might depend on the environmental difference in the major breeding sites treated with agricultural pesticides and on the difference in anthropophily in insecticides for indoor spray or ITN. Anthropophilic An. gambiae s.s. might have a greater chance to be exposed to insecticides for indoor use than An. arabiensis and An. funestus s.s., which are more zoophilic than An. gambiae s.s. [40]. Similarly, Bayoh et al. [10] concluded that the historical decline in An. gambiae s.s. populations associated with intensive distribution of ITNs at sites west of Kisumu and along the lakeshore might partly be attributable to the above difference in the anthropophily of mosquitoes. An. funestus s.s. is more anthropophilic than An. arabiensis [40] and this species might also have experienced the selection by LLITNs than An. arabiensis. Another main difference among three species comes probably from their breeding sites which are more polluted by agricultural pesticides for An. gambiae s.s. and An. arabiensis but less for An. funestus. The present study also suggests that the combinational use of a synergist such as PBO might reduce the resistance levels of An. arabiensis and An. funestus s.s. to their original susceptibility levels. Simplistic and intensive use of such combinations, however, might trigger another resistance mechanism.
Insecticides still provide the most promising countermeasures for controlling malaria as well as other arthropod-borne diseases. At the global level, 547 tons of DDT, 39 tons of organophosphates, 23 tons of carbamates, and 41 tons of pyrethroids are used annually for indoor residual spraying against malaria vectors [6]. The average total amount of pyrethroids used annually between 2003 and 2005 was 161 tons, which is 36% of the total insecticide consumption if the amount of DDT, which is exclusively used in African countries, is excluded. Among pyrethroids that are used for vector control, 98.7% comprise photostable pyrethroids such as μ-cypermethrin, μ-cyhalothrin, cyfluthrin, cypermethrin, deltamethrin (type II), etofenprox, bifenthrin, and permethrin (type I) [6]. Vector resistance against these pyrethroids has been a worldwide concern. It is expected that the use of photo-unstable knockdown agents such as spatial repellents, which effectively interfere with disease transmission without causing any selection pressure to insect populations, will be reconsidered [41]. Additionally, new self-protection measures using exito-repellent type I pyrethroids are of great interest as substitutional or supplemental techniques for bio-rational vector control measures in the future. The most popular and long-standing formulations using pyrethroids are mosquito coils, mosquito mats, and liquid vaporizers. Pyrethroids belonging to the knockdown agent group, such as allethrin, pyrethrin, and prallethrin, are used in these formulations. In particular, d-allethrin still continues to be used in these types of formulations. Further, mosquitoes have developed minimum physiological resistance to these pyrethroids due to the low selection pressure. Pyrethroids belonging to the knockdown agent group have been successfully used worldwide for a long period as a spatial repellent. Spatial repellency will not induce any pyrethroid resistance since it has low lethal activity on the affected insects and causes less selection pressure on insect populations. The discovery of the phenoxybenzyl alcohol moiety accelerated the development of photostable pyrethroids that could be used for outdoor use, including agricultural purposes. These “second generation” pyrethroids have been used worldwide as good vector control agents with various application techniques, such as residual spraying, ULV spraying, and LLIN. However, photostable and highly effective pyrethroids might accelerate the development of pyrethroid resistance in mosquito populations. Photostable pyrethroids consist of 2 structurally different types of chemicals according to the presence of μ-cyano moiety, type I (permethrin, etofenprox, etc.) and type II (deltamethrin, lambda-cyhalothrin, cypermethrin, etc.). Siegert et al. [42] reported that the Olyset® Net, slow-released polyethylene formulation containing 1000 mg of permethrin per m2, fitted over the human hand reduced landing attempts and elevated flight frequency, resulting in little mortality, while mosquito landing attempts on the PermaNet®, containing 55 mg of deltamethrin per m2, under the same conditions were sustained longer and caused greater mortality than the Olyset® Net. The authors concluded that the optimal LLIN formulation should maximize taxis or kinesis (“engagement”) so as to maximize mortality. This appears to be important for an effective control of the mosquito population. The high lethal pyrethroids, however, might accelerate the development of resistance. The exito-repellency of slow-released permethrin, on the contrary, might reduce the human-vector contact and blood feeding success [43]. In fact, there was no difference between Olyset® Net and PermaNet® in the field efficacy as measured by blood feeding rate [44]. The positive use of exito-repellency of slow-released pyrethroids, therefore, might lead bio-rational vector control with the maximum reduction of mosquito biting and minimum risk of resistance.
Acknowledgments
The protocol for this study including field work and sample collection (Case No. 1775) was reviewed and approved by the Scientific Steering Committee (SSC) and National Ethics Review Committee (ERC) of the Kenya Medical Research Institute (KEMRI). We thank all staffs in Thomas Odhiambo campus of the International Center of Insect Physiology and Ecology (ICIPE) for providing facilities and experimental insects. We also thank F. Sonye and G. Juma, Springs of Hope, Mbita, Kenya; Y. Higa, E. Kawashima, C. Tsurukawa, Y. Sonoda, and H. Iwashita, Institute of Tropical Medicine, Nagasaki University, Nagasaki, Japan; and H. Takeshita and N. Nagata, the School of Medicine, Nagasaki University, Nagasaki, Japan, for providing technical support, for rearing and providing the experimental insects, and for assisting with this study.
Footnotes
Competing Interests: Dr. Ohashi is an employee of Sumitomo Chemical Co., Ltd., and works as a researcher, developing insecticides for vector control. The authors have no patent or product in development related to this study. Any of above situation does not alter the authors‚ adherence to all the PLoS ONE policies on sharing data and materials.
Funding: This study was funded by Nagasaki University and Sumitomo Chemical Co., Ltd. for the creation of field and semi-field bioassay systems for insecticide delivering technology. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Bruce-Chwatt LJ. Essential Malariology. New York: John Wiley & Sons, Inc; 1985. 452 [Google Scholar]
- 2.Nabarro DN, Tayler EM. The “roll back malaria” campaign. Science. 1998;280:2067–2068. doi: 10.1126/science.280.5372.2067. [DOI] [PubMed] [Google Scholar]
- 3.Noor AM, Amin AA, Akhwale WS, Snow RW. Increasing coverage and decreasing inequity in insecticide-treated bed net use among rural Kenyan children. PLoS Med. 2007;4:e255. doi: 10.1371/journal.pmed.0040255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wacira DG, Hill J, McCall PJ, Kroeger A. Delivery of insecticide treated net services through employer and community based approaches in Kenya. Trop Med Int Hlth. 2007;12:140–149. doi: 10.1111/j.1365-3156.2006.01759.x. [DOI] [PubMed] [Google Scholar]
- 5.Fegan GW, Noor AM, Akhwale WS, Cousens S, Snow RW. Effect of expanded insecticide-treated bed net coverage on child survival in rural Kenya: a longitudinal study. Lancet. 2007;370:1035–1039. doi: 10.1016/S0140-6736(07)61477-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zaim M, Jambulingam P. Global insecticide use for vector-borne disease control, 3rd ed. World Health Organization; 2007. [Google Scholar]
- 7.Santolamazza F, Calzetta M, Etang J, Barrese E, Dia I, et al. Distribution of knock-down resistance mutations in Anopheles gambiae molecular forms in west and west-central Africa. Malar J. 2008;7:74. doi: 10.1186/1475-2875-7-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stump AD, Atieli FK, Vulule JM, Besansky NJ. Dynamics of the pyrethroid knockdown resistance allele in western Kenyan populations of Anopheles gambiae in response to insecticide-treated bed net trials. Am J Med Trop Hyg. 2004;70:591–596. [PubMed] [Google Scholar]
- 9.Mathias D, Ochomo EO, Atieli F, Ombok M, Bayoh MN, et al. Spatial and temporal variation in the kdr allele L1014S in Anopheles gambiae s.s. and phenotypic variability in susceptibility to insecticides in Western Kenya. Malr J. 2011;10:10. doi: 10.1186/1475-2875-10-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bayoh MN, Mathias DK, Odiere MR, Mutuku FM, Kamau L, et al. Anopheles gambiae: historical population decline associated with regional distribution of insecticide-treated bed nets in western Nyanza Province, Kenya. Mal J. 2010;9:62. doi: 10.1186/1475-2875-9-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kerah-Hinzoumbe C, Peka M, Nwane P, Donan-Gouni I, Etang J, et al. Insecticide resistance in Anopheles gambiae from south-western Chad, Central Africa. Malar J. 2008;7:192. doi: 10.1186/1475-2875-7-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen H, Githeko AK, Githure JI, Mutunga J, Zhou G, et al. Monooxygenase levels and knockdown resistance (kdr) allele frequencies in Anopheles gambiae and Anopheles arabiensis in Kenya. J Med Entomol. 2008;45:242–250. doi: 10.1603/0022-2585(2008)45[242:mlakrk]2.0.co;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Munhenga G, Masendu HT, Brooke BD, Hunt RH, Koekemoer LK. Pyrethroid resistance in the major malaria vector Anopheles arabiensis from Gwave, a malaria-endemic area in Zimbabwe. Malar J. 2008;7:247. doi: 10.1186/1475-2875-7-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mzilahowa T, Ball AJ, Bass C, Morgan JC, Nyoni B, et al. Reduced susceptibility to DDT in field populations of Anopheles quadriannulatus and Anopheles arabiensis in Malawi: evidence for larval selection. Med Vet Entomol. 2008;22:258–263. doi: 10.1111/j.1365-2915.2008.00736.x. [DOI] [PubMed] [Google Scholar]
- 15.Ramphul U, Boase T, Bass C, Okedi LM, Donnelly MJ, et al. Insecticide resistance and its association with target-site mutations in natural populations of Anopheles gambiae from eastern Uganda. Trans R Soc Trop Med Hyg. 2009;103:1121–1126. doi: 10.1016/j.trstmh.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 16.Yewhalaw D, Bortel WV, Denis L, Coosemans M, Duchateau L, et al. First evidence of high knockdown resistance frequency in Anopheles arabiensis (Diptera: Culicidae) from Ethiopia. Am J Trop Med Hyg. 2010;83:122–125. doi: 10.4269/ajtmh.2010.09-0738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Balkew M, Ibrahim M, Koekemoer L, Brooke BD, Engers H, et al. Insecticide resistance in Anopheles arabiensis (Diptera: Culicidae) from villages in central, northern and south west Ethiopia and detection of kdr mutation. Parasites & Vectors. 2010;3:40. doi: 10.1186/1756-3305-3-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morgan JC, Irving H, Okedi LM, Steven A, Wondji CS. Pyrethroid resistance in an Anopheles funestus population from Uganda. PLoS One. 2010;5:e11872. doi: 10.1371/journal.pone.0011872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Okoye PN, Brooke BD, Koekemoer LL, Hunt RH, Coetzee M. Characterization of DDT, pyrethroid and carbamate resistance in Anopheles funestus from Obuasi, Ghana. Trans Roy Soc Trop Med Hyg. 2008;102:591–598. doi: 10.1016/j.trstmh.2008.02.022. [DOI] [PubMed] [Google Scholar]
- 20.Amenya DA, Naguran R, Lo T-CM, Ranson H, Spillings BL, et al. Over expression of a cytochrome P450 (CYP6P9) in a major African malaria vector, Anopheles funestus, resistant to pyrethroids. Insect Mol Biol. 2008;17:19–25. doi: 10.1111/j.1365-2583.2008.00776.x. [DOI] [PubMed] [Google Scholar]
- 21.Cuamba N, Morgan JC, Irving H, Steven A, Wondji CS. High level of pyrethroid resistance in an Anopheles funestus population of the Chokwe district in Mozanbique. PLoS One. 2010;5:e11010. doi: 10.1371/journal.pone.0011010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gouagna LC, Okech BA, Kabiru EW, Killeen GF, Obare P, et al. Infectivity pf Plasmodium falciparum gametocytes in patients attending rural health centers in western Kenya. East Afr med J. 2003;80:627–634. doi: 10.4314/eamj.v80i12.8779. [DOI] [PubMed] [Google Scholar]
- 23.Noor AM, Gething PW, Alegana1 VA, Patil AP, Hay SI, et al. The risks of malaria infection in Kenya in 2009. BMC Infect Dis. 2009;9:180. doi: 10.1186/1471-2334-9-180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Service MW. Sampling the adult resting population. In: Service MW, editor. Mosquito ecology field sampling methods. 2nd edition. Edited by Service MW. London and New York: Elsevier Applied Science; 1993. pp. 210–290. [Google Scholar]
- 25.Kawada H, Higa Y, Nguyen YT, Tran SH, Nguyen HT, et al. Nationwide investigation of the pyrethroid susceptibility of mosquito larvae collected from used tires in Vietnam. PLoS Negl Trop Dis. 2009;3:e0000391. doi: 10.1371/journal.pntd.0000391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gillies MT, Coetzee M. A supplement to the Anophelinae of Africa south of the Sahara (Afrotropical region). 1987. South African Institute for Medical Research No. 55.
- 27.Scott JA, Brogdon WG, Collins FH. Identification of single specimens of the Anopheles gambiae complex by the polymerase chain reaction. Am J Trop Med Hyg. 1993;49:520–529. doi: 10.4269/ajtmh.1993.49.520. [DOI] [PubMed] [Google Scholar]
- 28.Koekemoer LL, Kamau L, Hunt RH, Coetzee M. A cocktail polymerase chain reaction (PCR) assay to identify members of the Anopheles funestus (Diptera: Culicidae) group. Am J Trop Med Hyg. 2002;66:804–811. doi: 10.4269/ajtmh.2002.66.804. [DOI] [PubMed] [Google Scholar]
- 29.Bliss CI. The method of probits. Science. 1934;79:38–39. doi: 10.1126/science.79.2037.38. [DOI] [PubMed] [Google Scholar]
- 30.Futami K. Change in relative abundance of the Anopheles gambiae complex in Suba district in western Kenya. Mal J. 2010 in review. [Google Scholar]
- 31.Kawada H, Shono Y, Itoh T, Abe Y. Laboratory evaluation of an insect growth regulators against several species of Anopheline mosquitoes. Jpn J Sanit Zool. 1993;44:349–353. [Google Scholar]
- 32.Hougard JM, Duchon S, Zaim M, Guillet P. Bifenthrin: a useful pyrethroid insecticide for treatment of mosquito nets. J Med Entomol. 2002;39:526–533. doi: 10.1603/0022-2585-39.3.526. [DOI] [PubMed] [Google Scholar]
- 33.Chandre F, Darriet F, Duchon S, Finot L, Manguin S, et al. Modifications of pyrethroid effects associated with kdr mutation in Anopheles gambiae. Med Vet Entomol. 2000;14:81–88. doi: 10.1046/j.1365-2915.2000.00212.x. [DOI] [PubMed] [Google Scholar]
- 34.Nazni WA, Lee HL, Azahari AH. Adult and larval insecticide susceptibility status of Culex quinquefasciatus (Say) mosquitoes in Kuala Lumpur Malaysia. Trop Biomed. 2005;22:63–68. [PubMed] [Google Scholar]
- 35.Kawada H, Higa Y, Komagata O, Kasai S, Tomita T, et al. Widespread distribution of a newly found point mutation in voltage-gated sodium channel in pyrethroid-resistant Aedes aegypti populations in Vietnam. PLoS Negl Trop Dis. 2009;3:e0000527. doi: 10.1371/journal.pntd.0000527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hemingway J. Biochemical studies on malathion resistance in Anopheles arabiensis from Sudan. Trans R Soc Trop Med Hyg. 1983;77:477–480. doi: 10.1016/0035-9203(83)90118-9. [DOI] [PubMed] [Google Scholar]
- 37.Bertram DS. Tsetse and trypanosomiasis control in Nyanza Province, Kenya. Trans R Soc Trop Med Hyg. 1969;63:125. doi: 10.1016/0035-9203(69)90093-5. [DOI] [PubMed] [Google Scholar]
- 38.Kamau L, Agai D, Matoke D, Wachira L, Gikandi G, et al. Status of insecticide susceptibility in Anopheles gambiae sensu lato and Anopheles funestus mosquitoes from western Kenya. J Insect Sci. 2007;8:11. doi: 10.1673/031.008.1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Okara RM, Sinka ME, Minakawa N, Mbogo, Hay SI, et al. Distribution of the main malaria vectors in Kenya. Malar J. 2010;9:69. doi: 10.1186/1475-2875-9-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Muriu SM, Muturi EJ, Shililu JI, Mbogo CM, Mwangangi JM, et al. Host choice and multiple blood feeding behaviour of malaria vectors and other anophelines in Mwea rice scheme, Kenya. Malar J. 2008;7:43. doi: 10.1186/1475-2875-7-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kawada H. An inconvenient truth of pyrethroid–Does it have a promising future? In: Clark J, Bloomquist JR, Kawada H, editors. Advances in human vector control (ACS Symposium Book 1014) New York: American Chemical Society; 2009. [Google Scholar]
- 42.Siegert PY, Walker E, Miller JR. Differential behavioral responses of Anopheles gambiae (Diptera: Culicidae) modulate mortality caused by pyrethroid-treated bednets. J Econ Entomol. 2009;102:2061–2071. doi: 10.1603/029.102.0607. [DOI] [PubMed] [Google Scholar]
- 43.Mathenge EM, Gimnig JE, Kolczak M, Ombok M, Irungu LW, et al. Effect of permethrin-impregnated nets on exiting behavior, blood feeding success, and time of feeding of malaria mosquitoes (Diptera: Culicidae) in western Kenya. J Med Entomol. 2001;38:531–536. doi: 10.1603/0022-2585-38.4.531. [DOI] [PubMed] [Google Scholar]
- 44.Dabire RK, Diabate A, Baldet T, Pare-Toe L, Guiguemde RT, et al. Personal protection of long lasting insecticide-treated nets in areas of Anopheles gambiae s.s. resistance to pyrethroids. Malar J. 2006;5:12. doi: 10.1186/1475-2875-5-12. [DOI] [PMC free article] [PubMed] [Google Scholar]