Abstract
Context
Acupressure is a non-invasive strategy used to manage various symptoms.
Objectives
The purpose of this paper was to review randomized controlled trials (RCTs) that investigated the efficacy of acupressure for the management of symptoms.
Methods
A literature search was conducted in the Cumulative Index to Nursing and Allied Health Literature (CINAHL), Medline, and PubMed, using the key words acupressure, clinical trial, human, and/or randomized. RCTs published between January 1, 2000 and January 31, 2010, which used acupressure as an intervention for one group, were included when they were written in English and when there were four or more studies of the efficacy of acupressure for that particular symptom.
Results
Forty-three studies were included in this review. Investigators in 16 of 23 studies concluded acupressure was effective, primarily for the management of nausea and vomiting in patients during pregnancy and during chemotherapy. Investigators in nine of ten studies concluded that acupressure was effective for pain in patients with dysmenorrhea, during labor, and after trauma. Investigators of four studies concluded that acupressure was effective in the management of dyspnea and investigators in six studies concluded that acupressure was effective in improving fatigue and reducing insomnia in a variety of populations. However, evaluation of the RCT reports indicated a significant likelihood of bias.
Conclusion
Acupressure may be a useful strategy for the management of multiple symptoms in a variety of patient populations, but rigorous trials are needed. Inclusion of acupressure as an intervention may improve patient outcomes.
Keywords: Acupressure, pain, dyspnea, fatigue, nausea, review
Introduction
Symptoms are the subjective sensations that accompany disease or injury and include nausea, pain, dyspnea, and fatigue. These experiences are ubiquitous; all individuals encounter multiple symptoms during their lifetime. Symptoms may be acute or chronic, isolated or found in clusters, and they are the primary reason individuals seek health care.1,2 Effective management of symptoms is needed to improve individual quality of life and reduce health care costs. For example, chronic pain occurs in 50 million Americans annually and has been found to influence functional status, to reduce quality of life, and to cost an estimated $150 million each year.3 Thus, interventions to effectively manage symptoms like pain are needed. Acupressure may be an effective intervention for a wide variety of symptoms. This intervention is noninvasive, relatively inexpensive, and has been demonstrated to be without adverse effects.4
The use of acupressure is based on meridian theory, which proposes that acupressure stimulates meridians, a network of energy pathways throughout the body, to increase the flow of qi (bio-energy), subsequently altering the symptom experience. 5 Meridians are shown in Fig. 1. Acupressure is applied to specific points by the use of finger, hand, elbow, foot, and/or acupressure band (Sea-Bands®, Leicestershire, UK), an elastic band with a protruding plastic button, for stimulation of these pathways to increase the flow of qi.
Figure 1.
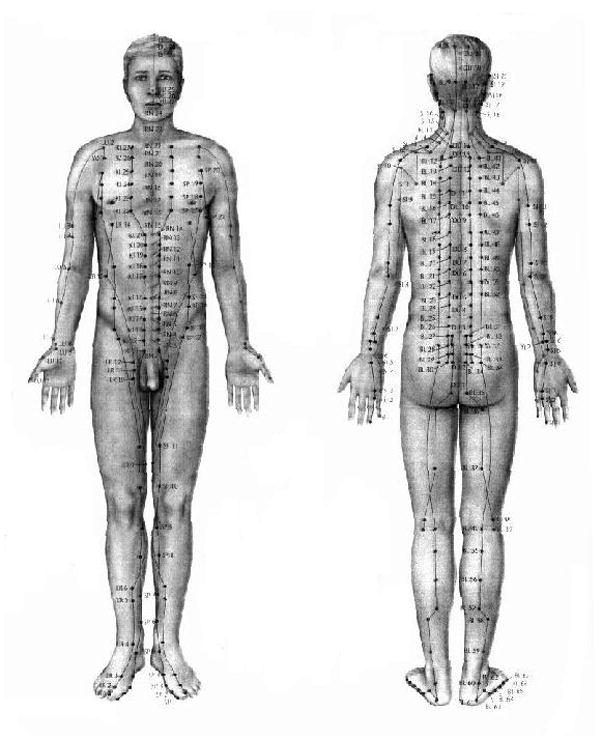
Acupressure meridians
Used with permission. Source: www.theamt.com (2010)
Studies testing the efficacy of acupressure for symptom management have been a focus of research, particularly during the last decade. However, no reviews have been published reporting the efficacy of acupressure for the management of multiple common symptoms. Thus, the purpose of this paper was to review the findings of RCTs that tested the efficacy of acupressure for symptom reduction.
Methods
Studies from this decade were included, as standards for reporting clinical trials were in place and this would provide a synthesis of the most recent findings of rigorous trials related to acupressure and symptom management.6 Reference lists of these articles also were hand searched to find additional pertinent studies. Articles were included in this review if they were written in English and reported randomized controlled trials. Studies were included when acupressure was the sole intervention in at least one of the experimental groups. A review of studies for individual symptoms was included in this review if there were at least four trials for management of a particular symptom. This cut-point was selected to ensure that there were a minimum number of clinical trials focused on a given symptom. Investigations with a sample size of less than 30 individuals were excluded because of a presumptive lack of statistical power (if sample size is 30, α level 0.05, large effect size 0.8, power = 56%). Studies using auricular or hand acupressure, reflexology, shiatsu, and electronic or magnetic devices were excluded because they use a different naming system for the meridians and a different technique from body acupressure. Unpublished studies and abstracts also were excluded.
Meta-analysis was not used in the evaluation of efficacy as the populations and interventions studied were very diverse and not suitable for this technique. Effect size (Hedges’s g) for each trial was calculated using the mean values of the acupressure and control groups when provided.7 Pre-post mean for the acupressure group was used alone when the post-mean of the control group was not available.
Each experimental study was evaluated for quality using the risk of bias tool by the Cochrane group.6 This instrument consists of six domains: sequence generation; allocation concealment; blinding of participants, personnel, and outcomes; incomplete outcome data; selective outcome reporting; and other source of bias. Articles were evaluated for the presence of each domain and one point was assigned for each domain present. Scores range from 0 to 6 and a higher value indicated higher quality and less risk for bias (Table 1). All trials were evaluated by the two authors and the agreement between them was 100%.
Table 1.
Effect Size and Risk of Bias Evaluation for Studies in the Review
| Author | Measure | Quality of Study | Acupressure | Control/Placebo/Post | Effect Size | CI | P | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | n | Mean | SD | n | ||||||
| Norheim (2001) | Duration of nausea | 2 | −2.74 | −0.85 | 0.33–3.45 | < .05 | |||||
| Werntoft (2001) | Severity of nausea (0–10) | 6 | 4.2 | 2.6 | 20 | 6.5 | 2.2 | 20 | 0.96 | 0.28–1.59 | .01 |
| Habek(2004) | Success rate of treatment on nausea | 4 | 0.64 | .14 | 11 | 0.13 | 0.12 | 8 | 0.59 | −0.37–1.49 | <.001 |
| Heazell (2006) | Number of patients required 2nd and 3rd anti-emetics (%) | 4 | 0.73 | .07 | 40 | 0.7 | .07 | 40 | .43 | −0.02–0.87 | NS |
| Shin (2007) | Rhodes Index of Nausea & Vomiting (6–30) | 5 | 17.6 | 1.06 | 23 | 21.6 | 1.06 | 22 | 3.79 | 2.76–4.69 | <.05 |
| Jamigorn (2007) | Rhodes Index of Nausea, Vomiting, Retching (RINVR) (8–40) | 4 | 14.3 Pre | 3.3 | 33 | 33 | 3.3 | <.001 | |||
| Roscoe (2003) | Severity of nausea (1–7) | 2 | 2.6 | 233 | 3 | 232 | < .05 | ||||
| Molassiotis(2007) | Incidence of nausea (%) | 5 | 0.66 | 1.6 | 17 | 2.16 | 2.4 | 19 | 0.73 | 0.04–1.39 | < .05 |
| Dibble (2007) | Rhodes Index of Nausea (age<55) | 4 | 6.5 | 3.3 | <.001 | ||||||
| Roscoe (2009) | Severity of nausea (Pre-post mean difference) | 5 | 0.7 | 0.23 | 59 | 0.1 | 0.27 | 29 | 2.4 | 1.87–3.01 | <.001 |
| Harmon (2000) | Incidence of nausea & vomiting (%) | 4 | 0.36 | .07 | 47 | 0.66 | .07 | 47 | 4.3 | 3.52–4.98 | .007 |
| Agarwal (2000) | Incidence of nausea (%) | 4 | 0.18 | .03 | 100 | 0.2 | .03 | 100 | 0.67 | 0.38–0.95 | NS |
| Alkaissi (2002) | Incidence of nausea & vomiting (%) | 5 | 0.33 | .04 | 135 | 0.46 | .04 | 136 | 3.25 | 2.88–3.6 | <.05 |
| Ming (2002) | RINVR (finger) | 2 | 1.28 | 3.4 | 50 | 6.96 | 5.96 | 50 | 1.2 | 0.74–1.59 | < .01 |
| RINVR (wrist band) | 4.34 | 6.63 | 50 | 6.96 | 5.96 | 50 | 0.41 | 0.01–0.81 | <.05 | ||
| Agarwal (2002) | Incidence of nausea (%) | 4 | 0.06 | .01 | 50 | 0.24 | .06 | 50 | 4.18 | 3.46–4.85 | <.05 |
| Schultz (2003) | Moderate to severe nausea (%) | 5 | 0.64 | .1 | 22 | 0.63 | .1 | 24 | .1 | −0.48–0.68 | NS |
| Samad (2003) | Incidence of nausea (%) | 3 | 0. 36 | 0.1 | 25 | 0.40 | 0.1 | 25 | −0.4 | −0.95–0.17 | NS |
| Klein (2004) | Incidence of nausea (%) | 4 | 0.33 | .05 | 75 | 0.36 | 0.06 | 77 | .5 | 0.22–0.86 | NS |
| Ho (2006) | Incidence of nausea (%) | 5 | 0.64 | .06 | 55 | 0.71 | 0.06 | 55 | 1.2 | 0.75–1.56 | NS |
| Turgut (2007) | Incidence of nausea (%) | 4 | 0.32 | .07 | 50 | 0.64 | 0.07 | 50 | 4.57 | 3.29–5.28 | <.05 |
| Sadighha (2008) | Severity of nausea (0–10) | 2 | 0.14 | 0.05 | 51 | 0 | 0 | 52 | 3.98 | 3.29–4.61 | <.001 |
| Dent (2003) | Incidence of nausea & vomiting | 4 | 0.18 | .04 | 95 | 0.43 | 0.05 | 108 | 5.48 | 4.86–6.06 | <.05 |
| Alkaissi (2005) | Mean time to moderate nausea (second) | 3 | 352 | 93 | 20 | 280 | 119 | 20 | 0.66 | 0.02–1.03 | NS |
| Taylor (2002) | Pain score (0–10) | 4 | 3.9 | 1.5 | 28 | 7.3 | 1.4 | 26 | 2.34 | 1.62–3 | <.001 |
| Pouresmail (2002) | Severity of dysmenorrheal (score 0) | 1 | 0.50 | 0.06 | 72 | 0.18 | 0.05 | 72 | 5.79 | 5.02–6.5 | <.001 |
| Chen (2004) | VAS for pain (0–10) | 4 | 3.9 | 1.8 | 35 | 4.8 | 1.8 | 34 | 0.5 | 0.01–0.97 | <.05 |
| Chung (2003) | VAS for pain (0–10) | 4 | 0.17 | 1.32 | 43 | 0.81 | 1.23 | 42 | 0.5 | 0.07–0.93 | <.05 |
| Lee (2004) | Pain score | 4 | 6.4 | 1.8 | 36 | 7.6 | 1.9 | 39 | .6 | 5.65–6.49 | .012 |
| Hsieh (2004) | Pain score | 5 | 9.29 | 2.6 | 69 | 5.05 | 5.11 | 77 | 1.0 | 0.68–1.37 | .0002 |
| Hsieh (2006) | Roland and Morris Disability Questionnaire | 5 | 5.4 | 5.0 | 64 | 9.2 | 5.8 | 65 | .7 | 6.37–8.24 | < .01 |
| Lang (2007) | VAS for pain (0–100) | 6 | 36.6 | 22.2 | 15 | 56 | 13.3 | 16 | 1.07 | 0.29–1.79 | <.001 |
| Sakurai (2003) | VAS for pain (0–100) | 5 | 29.5 | 13.5 | 23 | 40 | 18 | 30 | 0.65 | 0.08–1.19 | NS |
| Kober (2002) | VAS for pain (0–100) pre-post | 5 | 61.8 | 11.8 | 19 | 34 | 16.9 | 19 | 1.9 | 1.11–2.63 | < .01 |
| Maa (2003) | Saint George Respiratory Questionnaire (%) | 1 | 0.76 | .1 | 17 | 0.38 | .13 | 13 | 3.3 | .98–44 | <.05 |
| Wu (2004) | Pulmonary function, dyspnea questionnaire | 2 | .98 | 1.41 | 22 | 0.41 | .43 | 22 | 0.55 | −0.01–1.14 | <.05 |
| Tsay (2005) | VAS for dyspnea (0–100) pre-post | 3 | 69.4 | 12.0 | 26 | 62.7 | 12.03 | 26 | 0.56 | −0.01–1.10 | <.05 |
| Maa (2007) | St. George’s Respiratory Questionnaire - activity | 3 | 14.8 | 13.2 | 11 | 28.4 | 24.8 | 13 | −0.7 | −1.47–0.18 | .01 |
| Tsay (2003) | Pittsburgh Sleep Quality Index | 3 | 7.1 | 4.15 | 35 | 10.3 | 4.25 | 31 | 0.76 | 0.26–1.26 | <.05 |
| Tsay (2004) | Piper Fatigue Scale | 1 | 4.66 | 1.77 | 35 | 5.71 | 1.82 | 36 | 0.58 | 0.1–1.05 | <.05 |
| Cho(2004) | Piper Fatigue Scale | 2 | 3.4 | 1.5 | 28 | 4.7 | 1.7 | 30 | 0.8 | 0.26–1.3 | <.05 |
| Harris (2005) | Stanford Sleeping Scale | 2 | 0.57 | 21 | 1.13 | 18 | <.001 | ||||
| Molassiotis(2007) | Multidimensional Fatigue Inventory (%) | 3 | 0.19 | 0.1 | 16 | 0.01 | 0.06 | 16 | 2.23 | <.001 | |
| Nordio (2008) | Pittsburgh Sleep Quality Index | 4 | 4.8 | 2.75 | 18 | 1.3 | 2.9 | 15 | 1.27 | 0.4–1.99 | < .05 |
SD = standard deviation; VAS = visual analogue scale.
Results
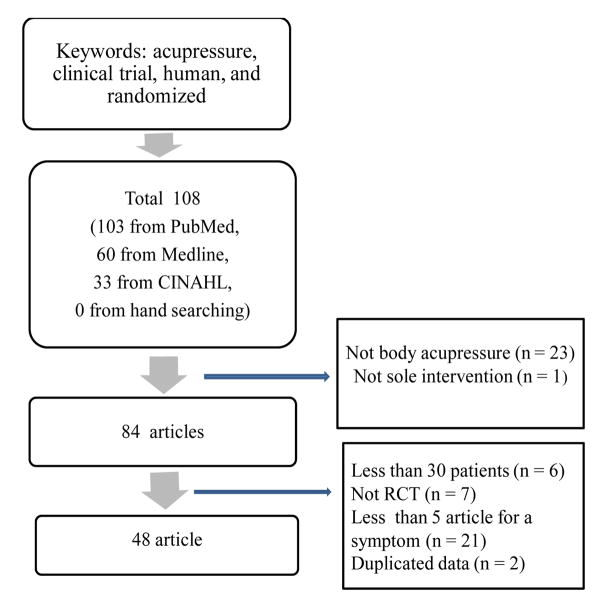
Thirty-three articles were retrieved from CINAHL, 60 from Medline, 103 from Pubmed, and none from hand searching, for a total of 196 articles initially retrieved. Eighty-eight articles were duplicates, which left 108 articles for screening. Four articles were excluded because of duplicate data.8–11 After application of the exclusion criteria, 43 studies remained for inclusion in this review (Fig. 2). Studies were categorized by the symptoms managed, which included nausea and vomiting, pain, dyspnea and fatigue/insomnia. Fatigue and insomnia were grouped together as these investigations typically studied both simultaneously. The characteristics of these studies are summarized in Table 2.
Figure 2.
Flow diagram of study inclusion and exclusion
Table 2.
Acupressure Studies in the Review
| Author | Sample | n | Acupressure Point | Tool | Time Per Day | Day | Measures |
|---|---|---|---|---|---|---|---|
| Nausea | |||||||
| Norheim (2001) | Pregnancy | 97 | PC6 | Sea-Band | 24 h | 4 d | Visual Analogue Scale (VAS), nausea intensity, duration, nature of symptom |
| Werntoft (2001) | Pregnancy | 60 | PC6 | Wrist band | 24h | 14d | VAS for nausea |
| Habek(2004) | Pregnancy | 36 | PC6 | Acupressure | 30min | 7d | Incidence of nausea, vomiting, antiemetic |
| Heazell (2006) | Pregnancy | 80 | PC6 | Sea-Band | 8 h | 3 d | Length of stay, amount of medication and fluid |
| Shin (2007) | Pregnancy | 66 | PC6 | Acupressure | 10 min | 4 d | Rhodes Index of Nausea, Vomiting, and Retching, ketonuria |
| Jamigorn(2007) | Pregnancy | 60 | PC6 | Sea-Band | 24h | 5d | Rhodes Index of Nausea, vomiting |
| Roscoe (2003) | Chemotherapy | 739 | PC6 | Sea-Band | 24h | 5 d | Severity, frequency of nausea & vomiting, expected efficacy of the wrist bands |
| Molassiotis (2007) | Chemotherapy | 36 | PC6 | Sea-Band | 24h | 5 d | Rhodes index of Nausea, Vomiting, and Retching |
| Dibble (2007) | Chemotherapy | 160 | PC6 | Acupressure | 9 min | 21 d | Rhodes Index of Nausea, NRS, State-trait Anxiety Inventory |
| Roscoe (2009) | Radiation | 88 | PC6 | Sea-Band | 24h | 5d | Likert scale for severity of nausea, number of vomiting |
| Harmon (2000) | Surgery | 94 | PC6 | Sea-Band | 6h | once | Incidence or vomiting, VAS for nausea, antiemetic |
| Agarwal (2000) | Surgery | 200 | PC6 | Sea-Band | 6h | once | Incidence of nausea, vomiting |
| Alkaissi (2002) | Surgery | 410 | PC6 | Sea-Band | 24h | 1d | Seven point scale for nausea, vomiting, pain |
| Ming (2002) | Surgery | 150 | PC6, HT7 | Acupressure wrist band | 20 min 24h | once 1 d | Rhodes Index of Nausea, Vomiting, and Retching, State-trait Anxiety Inventory |
| Agarwal (2002) | Surgery | 150 | PC6 | Sea-Band | 6h | once | Incidence of nausea, vomiting |
| Schultz (2003) | Surgery | 103 | PC6 | Sea-Band | 24h | 3d | Four point scale for nausea, incidence of vomiting, retching |
| Samad (2003) | Surgery | 50 | PC6 | Sea-Band | 6h | once | Incidence of nausea, vomiting, antiemetic |
| Klein (2004) | Surgery | 152 | PC6 | Sea-Band | 24h | 1d | Incidence of nausea, vomiting, antiemetic |
| Ho (2006) | Surgery | 110 | PC6 | Sea-Band | 104min | once | Incidence of nausea and vomiting |
| Turgut (2007) | Surgery | 100 | PC6 | Sea-Band | 24h | 1d | Likert scale for nausea and vomiting |
| Sadighha(2008) | Surgery | 156 | PC6 | Wrist band | 24h | 1d | Likert scale for nausea and vomiting |
| Dent (2003) | Acute MI | 301 | PC6 | Wrist band | 24 h | 1 d | Incidence and severity of nausea and vomiting, doses of anti-emetic medication |
| Alkaissi (2005) | Motion sickness | 60 | PC6 | Sea-Band | Likert-type scale for nausea | ||
| Pain | |||||||
| Taylor (2002) | Dysmenorrhea | 58 | Multipoint | Acupressure pad | 24 h | 3 d | Descriptive numeric rating scale of pain intensity, Dysmenorrhea Symptom Intensity & Distress Inventory |
| Pouresmail (2002) | Dysmenorrhea | 216 | Multipoins | Acupressure | 2 min | VAS for pain, multi-dimensional scoring system for the severity of dysmenorrhea | |
| Chen (2004) | Dysmenorrhea | 69 | SP6 | Acupressure | 20 min | 2d | VAS for pain and anxiety, Menstrual Distress Questionnaire, Short-form McGill Pain Questionnaire |
| Chung (2003) | Labor | 127 | LI4, UB67 | Acupressure | 20 min | Once | VAS for pain, external fetal monitor, time of first stage of labor |
| Lee (2004) | Labor | 75 | SP6 | Acupressure | 30 min | Once | VAS for labor pain, duration of labor to delivery |
| Hsieh (2004) | Back pain | 146 | Acupressure | 15 min | 120d | Short-form Pain Questionnaire | |
| Hsieh (2006) | Back pain | 129 | Acupressure | 30d | Roland and Morris Disability Questionnaire, Oswestry Disability Questionnaire, quality of life | ||
| Lang (2007) | Radial fracture | 70 | GV20, LI4 | Acupressure | 6 min | Once | VAS for pain and anxiety |
| Sakurai (2003) | Surgery | 53 | Multipoint | Sphere | VAS for pain, opioid use | ||
| Kober (2002) | Trauma | 60 | Multipoint | Acupressure | 3 min | once | VAS for pain, anxiety |
| Dyspnea | |||||||
| Maa (2003) | Asthma | 41 | Multipoint | Acupressure | 2.5–10min | 56d | VAS for dyspnea, Borg Scale, St. George’s Respiratory Questionnaire, Bronchitis Emphysema Symptom Checklist |
| Wu (2004) | COPD | 44 | Multipoint | Acupressure | 16 min | 28d | Pulmonary functional status, Dyspnea Questionnaire-modified, 6-minute walk distance |
| Tsay (2005) | COPD | 52 | LI4, PC6, H T7 | Acupressure | 12 min | 10 d | Respiratory rate, heart rate, VAS for anxiety and dyspnea |
| Maa (2007) | Bronchiectasis | 35 | Multipoint | Acupressure | 2.5–10min | 56d | Daily sputum amount, 6-minute walk distance, VAS for dyspnea, Saint George Respiratory Questionnaire |
| Fatigue | |||||||
| Tsay (2003) | ERSD | 98 | HT7, KD11 | Acupressure | 9 min | 12d | Pittsburgh Sleep Quality Index, sleep log |
| Tsay (2004) | ESRD | 106 | Multipoint | Acupressure | 12 min | 12d | Piper Fatigue Scale, VAS for fatigue, Pittsburgh Sleep Quality Index |
| Cho (2004) | ESRD | 58 | ST 36, K1 SP6, K13 | Acupressure | 12 min | 12d | Piper Fatigue Scale, Beck Depression Inventory |
| Harris (2005) | Students | 39 | Multipoint | Acupressure | 15 min | 3 d | Stanford Sleeping Scale |
| Molassiotis (2007) | Chemotherapy | 47 | LI4, SP6, ST36 | Acupressure | 3 min | 12d | Multi-dimensional Fatigue Inventory |
| Nordio (2008) | Insomnia | 40 | HT 7 | Acupressure band | 10h | 20d | Pittsburgh Sleep Quality Index, urinary melatonin |
MI = Myocardial infarction; COPD = Chronic obstructive pulmonary disease; ESRD = End-stage renal disease;
Acupressure point: conception vessel (CV), governing vessel (GV), heart (HT), pericardium (PC), lung (LU), spleen (SP), liver (LV/LR), kidney (KD/KI), small intestine (SI), triple heater (TH/TE), large intestine (LI), stomach (ST), gall bladder (GB), and urinary bladder (UB/BL).
Quality of Studies
The average risk of bias score was 3.8 for RCTs focused on nausea/vomiting, 4.8 for studies investigating pain management, 2.3 for studies of efficacy for dyspnea, and 2.5 for those studying the reduction of fatigue/insomnia. Thus, the risk for bias of these studies was moderate to high and only two studies (5%) earned scores of 6, indicating the lowest risk of bias and highest quality RCT. Of 43 RCTs, the randomization strategy was unclear in 14 studies,12–25 16 studies did not use double-blinding,13,14,16,24,26–37 and four of 27 studies that used double blinding 17,38–40 did not describe the method employed. Nine studies did not report the attrition rate and reasons for attrition.12,14,15,29,37,40–43
Another particular issue related to quality was the lack of fidelity evaluation in the 40% (n = 17) of studies that used acupressure administered by the participants. Also, only four of these reported the length of time participants performed acupressure.26,30,34,39 Fidelity to the intervention is an important confounding factor that may have added bias to these studies.
Outcome Measures
To measure the efficacy of acupressure on nausea and vomiting, outcome measures included a visual analogue scale (VAS) for nausea and vomiting,18 the incidence and severity of nausea and vomiting,12 hospital length of stay, dose of medication required and the Rhodes Index of Nausea, Vomiting and Retching.41 To measure the efficacy of acupressure for pain, a VAS for pain35 and the Short-Form McGill Pain Questionnaire13 were primarily used. To measure the efficacy of acupressure for dyspnea, the Saint George Respiratory Questionnaire,44 six-minute walk distance,14 a VAS for dyspnea,44 and the Pulmonary Functional Status and Dyspnea Questionnaire14 were used to evaluate outcomes. To measure the efficacy of acupressure for fatigue and sleep, the Pittsburgh Statistical Quality Index,45 the Piper Fatigue Scale,16 the Stanford Sleeping Scale,37 and a VAS for fatigue16 were employed.
Description of Studies
Acupressure for Nausea and Vomiting
Nausea and vomiting associated with pregnancy
Six RCTs examined the efficacy of acupressure at PC6 in the prevention or management of nausea and vomiting associated with pregnancy.12,18,32,33,38,41 Investigators used nausea self-report and objective measurement of emesis, total dose of anti-emetic medications, and hospital length of stay as indicators of efficacy. Habek and colleagues12 reported that acupressure for 30 minutes daily for seven days significantly improved nausea and vomiting compared to placebo acupressure in patients with hyperemesis gravidarum (n=36). In women with gestational age 8–12 weeks, investigators tested four days of acupressure using Sea-Bands and compared the duration and intensity of nausea and vomiting with a control group who wore wrist bands with a felt patch for the same time period.18 These investigators found that acupressure significantly reduced the duration of nausea and vomiting early in pregnancy, but did not reduce the intensity of nausea when compared with a placebo group. Sixty-three percent of participants in the acupressure group and 90% in the placebo group experienced pain, numbness, soreness and hand-swelling from using wrist bands. Werntoft and Dykes38 found that acupressure using Sea-Bands daily for two weeks (removed only when showering) significantly reduced nausea in healthy pregnant women compared with both control (no antiemetic) and placebo (Sea-Bands at non-meridian) groups (n= 60).
Because prolonged nausea and vomiting produces ketonuria, Shin and colleagues41 used kenonuria as an additional outcome variable. These investigators found that a four-day, daily, 10-minute acupressure treatment significantly reduced nausea, vomiting, and ketonuria in women with hyperemesis gravidarum when compared to placebo (acupressure at inappropriate location) and control groups (standard care) (n= 66). Jemigorn and Phupong 33 also found that acupressure using Sea-Bands for 24 hours a day for five days reduced nausea and vomiting in 60 pregnant women compared to vitamin B6 and placebo wrist bands. Only one patient reported adverse effects from the Sea-Bands. In contrast, Heazell and colleagues 32 found that the use of acupressure bands (Sea-Bands) for an eight-hour period did not affect the length of hospital stay, amount of anti-emetic medication required, and the volume of fluid administered to patients who experienced nausea and vomiting in early pregnancy when compared with a placebo group (Sea-Bands placed in a non-meridian location) (n= 80).
Nausea and vomiting associated with chemotherapy and radiation
Four RCTs examined the efficacy of acupressure at PC6 for nausea and vomiting in cancer patients who were undergoing chemotherapy or radiation.19,30,31,34 Roscoe and colleagues 34 found that acupressure using Sea-Bands continuously for five days significantly reduced nausea and vomiting on the first day of chemotherapy compared to the control group, which received standard care (n = 739). However, there was no significant difference on the second to fifth day of chemotherapy. In another study by Roscoe and colleagues,30 they found that Sea-Bands were effective in reducing nausea and vomiting associated with radiation therapy compared to standard care (n= 94). Molassiotis and colleagues31 found that acupressure using Sea-Bands continuously for five days significantly reduced nausea, vomiting, and retching in patients with breast cancer receiving chemotherapy when compared to a control group receiving standard care (n= 36). However, Dibble and colleagues19 found that a daily nine-minute acupressure treatment given prior to chemotherapy administration on the day of treatment initiation and continuing for 21 days did not reduce acute nausea and vomiting on the day of chemotherapy, but did decrease nausea and vomiting from day 2 to day 11 when compared to the control (standard care) and placebo groups (acupressure in inappropriate locations) (n= 160).
Nausea and vomiting associated with surgical intervention
Eleven studies examined the efficacy of acupressure at PC6/HT 7 for nausea and vomiting in a variety of post-operative patients.20,22,28,29,39,40,42,43,46–48 The majority of these investigations focused on patients following abdominal surgery, particularly obstetric and gynecological surgery or cholecystectomy.
Alkaissi48 reported that acupressure using Sea-Bands for 24 hours significantly improved nausea and vomiting in patients after gynecological surgery compared to standard care (n= 410). These investigators found that Sea-Bands were reported to be uncomfortable and were associated with red indentations, itching, headache and dizziness, pain, swelling, and blistering at the site of the acupressure button. In another investigation, six hours of acupressure significantly reduced nausea and vomiting following Caesarean section compared to placebo bands (n= 94)22 and 24 hours of acupressure significantly improved nausea and vomiting after other gynecological surgery compared to placebo bands (n= 100).28 However, Ho and colleagues40 found that acupressure after Caesarean section did not reduce the incidence of nausea and vomiting when compared to a control group (placebo wrist bands) (n= 110). Schultz 39 also found that acupressure with placebo drugs administered 24 hours a day for three days did not reduce nausea and vomiting in patients after gynecologic surgery compared to placebo drugs with placebo bands (n= 103).
Agarwal and colleagues found that acupressure using Sea-Bands for six hours was as effective as administration of ondansetron in improving nausea and vomiting in patients after cholecystectomy when compared to placebo wrist bands (n= 150),47 but did not improve nausea and vomiting in patients after urological endoscopic surgery compared to placebo wrist bands (n= 200).46 In addition, acupressure using Sea-Bands for six hours did not improve nausea and vomiting compared to the placebo wrist bands in patients after cholecystectomy (n= 50).29 In contrast, Sadighha 43 reported that the use of an acupressure wristband for one day relieved nausea and vomiting in patients after laparoscopic cholecystectomy compared to placebo band and antiemetic groups (n = 156).
Acupressure also has been studied as a management strategy following other surgical procedures. Following functional endoscopic sinus surgery, Ming and colleagues 20 found that one 20-minute acupressure treatment or Sea-Bands for 24 hours were both effective in reducing nausea and vomiting when compared to a control group (standard care) (n= 150). Of the two acupressure strategies used with the sinus surgery patients, acupressure using fingers for 20 minutes was more effective than Sea-Bands. In contrast, Klein and colleagues42 found that acupressure using Sea-Bands for 24 hours did not improve nausea and vomiting compared to the placebo wrist band group in patients following cardiac surgery (n= 152). Thus, overall findings for the postoperative population are equivocal.
Nausea and vomiting associated with acute myocardial infarction (AMI)
Dent and colleagues27 reported that acupressure for 24 hours using Sea-Bands at PC6 was not effective in reducing the incidence and severity of nausea and vomiting after AMI (n =301). Sea-Bands were supposed to be applied when patients were admitted. However, 15% of patients did not receive these until at least two hours after admission. The investigators concluded that failure to apply Sea-Bands during the early onset of AMI might have reduced the effect of the treatment.
Nausea and vomiting associated with motion sickness
Alkaissi and colleagues49 studied women with a history of motion sickness and reported that acupressure using Sea-Bands at PC6 was not effective in reducing nausea related to motion sickness compared to the placebo group (n = 60). The intervention group received acupressure using Sea-Bands, but the time of application and the length of treatment were not described. The placebo group wore Sea-Bands in an inappropriate location, also for an unknown period of time, and the control group received no therapy. Rotation chairs with 60°/second speed were used to induce motion sickness. When participants reported moderate nausea, rotation chairs were stopped. Nausea was measured immediately and 30 minutes later using a 7-point Likert scale and motion sickness was not improved by acupressure in this experiment.
Acupressure for Pain
Dysmenorrhea
Three studies examined the efficacy of acupressure for menstrual pain.13,26,50 Chen and Chen13 studied adolescents with menstrual pain (n= 69) and found that 20 minutes of acupressure at SP6 on the first day of menstruation was effective in reducing dysmenorrhea compared to a control group that received a rest period in the school health center. Taylor and colleagues26 used specialized panties that administered acupressure to multiple points (CV2, 4, SP12, SP13, ST30, KD11, KD13, UB23, UB25, UB27, UB28, and GV4) continuously. These panties were worn for the first three menstrual days and were found to be effective in reducing dysmenorrhea and the number of doses of pain medication daily compared to a control group who received usual care (n= 58). Concurrently, Pouresmail and Ibrahimzadeh50 reported that acupressure were effective in the treatment dysmenorrhea in high school students when compared to a placebo group who received sham acupressure (n= 216).
Labor pain
Two RCTs tested the efficacy of acupressure for the reduction of labor pain.21,35 Chung and colleagues35 found that acupressure at LI4 and UB67 for 20 minutes during the first stage of labor was effective in reducing pain when compared to a placebo group who received effleurage, a light stroking at both upper outer arms, and a control group who received usual care (n= 127). In a similar study, Lee and colleagues21 found that acupressure at SP6 for 30 minutes significantly reduced pain and decreased labor time required for cervical dilation from 3cm to delivery when compared to a placebo group that received only touch at SP6 (n= 75).
Pain related to trauma
Two RCTs examined the efficacy of acupressure for pain related to trauma.51,52 Kober and colleagues51 reported that acupressure at LI4, PC6, PC9, BL60, and GV2 for 3 minutes in patients being transported by ambulance following minor trauma reduced pain, anxiety and heart rate compared to control (standard care) and sham acupressure groups (n= 60). In a similar study, Lang and colleagues52 found that in patients with a radial fracture, 6 minutes of acupressure administered once at GV20 and LI4 during ambulance transport to the hospital significantly reduced pain and anxiety when compared to a placebo group that received acupressure at an inappropriate location (n= 70).
Muscular system
Two RCTs examined the efficacy of acupressure for muscular pain.53,54 Hsieh and colleagues54 found that acupressure treatment six times over a one month period was significantly more effective in reducing chronic low back pain compared to a comparison group that was treated with physical therapy (n=146). The efficacy of the acupressure treatments persisted for six months and pain scores remained significantly lower than the physical therapy group. In a subsequent study, Hsieh and colleagues53 used the same protocol and found that acupressure significantly reduced chronic low back pain when compared to a placebo acupressure group (n= 129). Unfortunately, these two reports provided inadequate details about the acupressure treatment, which precludes replication of the studies.
Pain related to surgery
Sakurai et al.55 compared acupressure with a control condition (standard care) after open abdominal surgery. All patients received intravenous morphine via patient-controlled analgesia. These investigators found that acupressure at PC6, ST36, SP4, and SP6 did not reduce pain scores or total dose of analgesia required when compared the control group (n= 53).
Acupressure for Dyspnea
The authors of four investigations reported that acupressure was effective in reducing dyspnea.14,15,36,44 Dyspnea is the sensation of difficulty breathing or shortness of breath, which may be acute or chronic. Dyspnea is often accompanied by other symptoms, such as anxiety and depression, and signs like tachypnea and reduced functional ability.10,14 Dyspnea is the most common and most debilitating symptom found in chronic lung disease. Thus, studies primarily included patients with some form of chronic lung disease. Wu and colleagues14 found that four weeks of a daily 16-minute acupressure treatment at GV14, CV22, UB13, UB23, and LU10 was effective in improving pulmonary function, oxygen saturation, six-minute walk distance, dyspnea and state-anxiety when compared to a placebo group that received acupressure at an inappropriate location in patients with chronic obstructive pulmonary disease (COPD) (n= 44). In another study of patients with COPD, Tsay and colleagues15 found that 12 minutes of daily acupressure for 10 days at LI4, PC6, and HT7 improved dyspnea, anxiety, blood pressure, heart rate, and respiratory rate when compared to a placebo group that received handholding and massage. Two studies by Maa and colleagues36,44 found that 2.5–10 minutes of daily acupressure for an eight-week period at LU1, LU5, LU10, and ST36, ST40 and standard care significantly improved dyspnea and respiratory health-related quality of life in patients with bronchiectasis and asthma when compared to a standard care group (medication and chest physiotherapy).
Acupressure for Insomnia and Fatigue
Six RCTs were performed to determine the efficacy of acupressure on the reduction of fatigue and improvement of sleep in adults.16,17,24,37,45,56 Authors of all six studies concluded that acupressure was effective in improving fatigue and reducing insomnia. The symptom of fatigue is often associated with poorer sleep quality, so the efficacy of acupressure for fatigue and sleep was investigated both separately and simultaneously in these studies.
Tsay and Chen45 found that the application of nine minutes of acupressure at HT7 and KD11, three times a week for four weeks, improved the sleep quality in patients with end-stage renal disease (ESRD) when compared to standard care (n = 98). However, there was no statistical difference between the acupressure treatment and placebo (acupressure at non-acupressure points) groups. Melatonin and its circadian rhythm have been postulated to have an important role in sleep. In a subsequent study of acupressure and sleep, Nordio and Romanelli 17 studied the efficacy of acupressure on sleep and melatonin changes. These investigators found that the use of an acupressure band at HT7 for 10 hours daily for 20 days significantly improved sleep and melatonin biorhythm compared to a placebo group (wrist band in different meridian) (n= 40).
Other investigators studied the use of acupressure to reduce fatigue and increase alertness. Harris and colleagues37 investigated the efficacy of two sequences of acupressure treatment administered daily for three days using a cross-over design to support relaxation or stimulation in healthy young adults. These investigators found that stimulation acupressure at LI4, ST36, KD1, and UB10 significantly decreased fatigue and improved alertness when compared to placebo acupressure (n= 39). Harris and colleagues37 reported that acupressure was also associated with adverse effects such as muscle cramps, muscle aches, headaches and fatigue when used with healthy college students. Other investigators studied the efficacy of acupressure in patients with a chronic disease. Molassiotis and colleagues56 reported that acupressure for 20 minutes, six times per week for two weeks, reduced fatigue in cancer patients when compared to a sham acupressure group (n= 47).
Because fatigue and insomnia are often accompanied by depressive symptoms, Tsay16 included depressive symptoms as an outcome and found that the application of 12 minutes of acupressure at SP6, GB34, ST36, and KD1 three times a week for four weeks significantly reduced fatigue and depression, and improved sleep quality in patients with ESRD when compared to standard care (n= 106).
Discussion
Forty-three studies examined the efficacy of acupressure for symptom management. A majority of these investigators (84%) concluded that acupressure was effective for symptom management in adults with a variety of disorders and conditions. Unfortunately, the quality ratings using the Cochrane bias instrument did not find that these trials were of sufficient rigor to provide adequate evidence for efficacy of acupressure. Most of these investigators reported that acupressure did not have adverse effects.57 However, in two studies, acupressure was associated with headache and dizziness, as well as skin reactions.33, 37
Symptom management strategies include pharmacological therapy, nutritional therapy,58 exercise,59 cognitive behavioral therapy, relaxation, complementary and alternative therapies,60 meditation,61 music therapy, and guided imagery.62 There are currently few studies that compare the efficacy of acupressure with other symptom management strategies. Thus, there is a dearth of evidence to support the use of acupressure over other management strategies or as an adjunct to other strategies.
The daily dose of acupressure in this review varied from 2.5 minutes to 24 hours. The total intervention time for acupressure varied from 20 minutes to 56 days. The numbers of acupressure points varied from one to twelve. There were no studies that compared equivalent doses of acupressure. Thus, well-designed, rigorous studies are needed to compare equivalent daily doses, intervention times and number of acupressure points.
It is vital that investigators include appropriate measures of outcome for acupressure trials. Nearly one-fourth of the reviewed studies included both subjective measures of symptoms and objective markers of symptom improvement. These included physiological measures like urinalysis for ketonuria, as well as clinical indicators, such as total daily dose of medication for symptom management. Although symptoms are an individual experience, and as such, self-report is the gold standard measure,63 the addition of these types of objective indicators provides additional evidence for efficacy and utility.
Acupressure may be administered using several techniques. Only two of the studies reviewed compared different methods of administration of acupressure.20,34 Ming and colleagues20 reported that manual acupressure and Sea-Bands were equally effective for management of nausea. Other studies used techniques as varied as traditional finger pressure to specialized panties that applied pressure to multiple acupressure sites. Thus, different administration strategies, in addition to variation in the meridians treated, makes comparisons across studies impossible. Consistency in techniques and acupressure sites under study would facilitate comparison of results and provide more rigorous examination of the efficacy of acupressure for symptom management.
In addition to consistency, patient-provider interaction during acupressure therapy may confound outcomes. Most of these studies did not describe patient-practitioner interaction. Only one study by Ming and colleagues20 reported that practitioners stayed with patients in the control group for 20 minutes. The lack of information about the practitioner-patient interaction in both intervention and control groups could introduce a serious confounding variable that has not been considered in these studies.
Patient and health care provider attitudes toward acupressure may be a factor related to its efficacy and use. Roscoe and colleagues34 found that patients who expected acupressure to be effective demonstrated more positive effects than those who thought that acupressure was unlikely to be effective. However, Rosenberg and colleagues64 found that although more than half of their chronic pain patients used some form of complementary or alternative therapy in addition to their traditional treatment, when given the choice between traditional treatment and alternative therapy, the traditional treatment strategy was preferred. Other factors like the degree of individual perceived control and level of depression might also influence the use of acupressure and require investigation.
The effective use of both traditional and complementary and alternative therapies is an attractive strategy for symptom management. A variety of patient populations, including those with chronic diseases and those requiring palliative care, could benefit from a noninvasive, easily performed intervention with few adverse effects. Unfortunately, there are considerable knowledge deficits about acupressure, in spite of a generally positive attitude about its inclusion in a plan of care.65 Because of this, curriculum development and continuing education focused on the inclusion of alternative and complementary strategies is clearly needed should rigorous RCTs demonstrate the efficacy of acupressure for symptom management.
Limitations
Statistical techniques such as meta-analysis for definitive evidence of efficacy were not possible because of the wide variability in participants and the interventions, including fundamental differences in treatment site, treatment frequency, treatment length and number of days of treatment, and the method of application of acupressure. The limitations of this review also include the exclusion criteria, such as sample size, publication years, and language. Excluded studies might have been well designed, but the lack of well-designed studies in those included suggests this would not be the case and studies performed prior to 2000 could have offered more rigorous evidence of efficacy. There is always the possibility that some appropriate studies were missed with our search strategy. However, multiple key words were used and reference lists were hand searched to ensure that all studies that met criteria were included.
Conclusion
Acupressure is commonly used in some cultures and countries to manage symptoms. This technique is noninvasive and may prove to be a useful adjunct in the care of a wide variety of individuals with symptoms. Our review of clinical trials from the past decade did not provide rigorous support for the efficacy of acupressure for symptom management. Well-designed, randomized controlled studies are needed to determine the utility and efficacy of acupressure to manage a variety of symptoms in a number of patient populations.
Acknowledgments
This work was supported in part by a grant to the University of Kentucky, College of Nursing from the National Institutes of Health’s National Institute of Nursing Research (1P20NR010679). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Footnotes
Disclosures
The authors declare no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Leonard R, Kourlas H. Too much of a good thing? Treating the emerging syndrome of opioid-induced hyperalgesia. J Pharm Pract. 2008;21(2):165–168. [Google Scholar]
- 2.Shapiro AP, Teasell RW. Behavioural interventions in the rehabilitation of acute v. chronic non-organic (conversion/factitious) motor disorders. Br J Psychiatry. 2004;185:140–146. doi: 10.1192/bjp.185.2.140. [DOI] [PubMed] [Google Scholar]
- 3.American Pain Society. Pain hurts—individuals, significant others, and society. [Accessed October 10, 2009];APS Bulletin. 2006 16:1. Available from: http://www.ampainsoc.org/pub/bulletin/win06/pres1.htm.
- 4.Jones E, Isom S, Kemper KJ, McLean TW. Acupressure for chemotherapy-associated nausea and vomiting in children. J Soc Integr Oncol. 2008;6(4):141–145. [PubMed] [Google Scholar]
- 5.National Cancer Institute. [Accessed December 18, 2008];Acupuncture. 2007 Available from: http://www.cancer.gov/cancertopics/pdq/cam/acupuncture/HealthProfessional.
- 6.Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. J Am Podiatr Med Assoc. 2001;91(8):437–442. doi: 10.7547/87507315-91-8-437. [DOI] [PubMed] [Google Scholar]
- 7.Durham University. [Accessed October 6, 2010];Effect size caculator. 2010 Available from: http://www.pipsproject.org/RenderPagePrint.asp?linkID=30325017.
- 8.Tsay S, Chen M. Acupressure and quality of sleep in patients with end-stage renal disease -- a randomized controlled trial. Int J Nurs Stud. 2003;40(1):1–7. doi: 10.1016/s0020-7489(02)00019-6. [DOI] [PubMed] [Google Scholar]
- 9.Tsay S, Cho Y, Chen M. Acupressure and transcutaneous electrical acupoint stimulation in improving fatigue, sleep quality and depression in hemodialysis patients. Am J Chin Med. 2004;32(3):407–416. doi: 10.1142/S0192415X04002065. [DOI] [PubMed] [Google Scholar]
- 10.Wu H, Lin L, Wu S, Lin J. The psychological consequences of chronic dyspnea in chronic pulmonary obstruction disease: the effects of acupressure on depression. J Altern Complement Med. 2007;13(2):253–261. doi: 10.1089/acm.2006.5342. [DOI] [PubMed] [Google Scholar]
- 11.Roscoe JA, Jean-Pierre P, Morrow GR, et al. Exploratory analysis of the usefulness of acupressure bands when severe chemotherapy-related nausea is expected. J Soc Integr Oncol. 2006;4(1):16–20. [PubMed] [Google Scholar]
- 12.Habek D, Barbir A, Habek JC, Janculiak D, Bobic-Vukovic M. Success of acupuncture and acupressure of the Pc 6 acupoint in the treatment of hyperemesis gravidarum. Forsch Komplementarmed Klass Naturheilkd. 2004;11(1):20–23. doi: 10.1159/000077192. [DOI] [PubMed] [Google Scholar]
- 13.Chen HM, Chen CH. Effects of acupressure at the Sanyinjiao point on primary dysmenorrhea. J Adv Nurs. 2004;48(4):380–387. doi: 10.1111/j.1365-2648.2004.03236.x. [DOI] [PubMed] [Google Scholar]
- 14.Wu H, Wu S, Lin J, Lin L. Effectiveness of acupressure in improving dyspnoea in chronic obstructive pulmonary disease. J Adv Nurs. 2004;45(3):252–259. doi: 10.1046/j.1365-2648.2003.02886.x. [DOI] [PubMed] [Google Scholar]
- 15.Tsay S, Wang J, Lin K, Chung U. Effects of acupressure therapy for patients having prolonged mechanical ventilation support. J Adv Nurs. 2005;52(2):142–150. doi: 10.1111/j.1365-2648.2005.03576.x. [DOI] [PubMed] [Google Scholar]
- 16.Tsay S. Acupressure and fatigue in patients with end-stage renal disease: a randomized controlled trial. Int J Nurs Stud. 2004;41(1):99–106. doi: 10.1016/s0020-7489(03)00079-8. [DOI] [PubMed] [Google Scholar]
- 17.Nordio M, Romanelli F. Efficacy of wrists overnight compression (HT 7 point) on insomniacs: possible role of melatonin? Minerva Med. 2008;99(6):539–547. [PubMed] [Google Scholar]
- 18.Norheim AJ, Pedersen EJ, Fonnebo V, Berge L. Acupressure treatment of morning sickness in pregnancy: a randomized, double-blind, placebo-controlled study. Scand J Prim Health Care. 2001;19(1):43–47. doi: 10.1080/028134301300034666. [DOI] [PubMed] [Google Scholar]
- 19.Dibble SL, Chapman J, Mack KA, Shih A. Acupressure for nausea: results of a pilot study. Oncol Nurs Forum. 2000;27(1):41–47. [PubMed] [Google Scholar]
- 20.Ming JL, Kuo BI, Lin JG, Lin LC. The efficacy of acupressure to prevent nausea and vomiting in post-operative patients. J Adv Nurs. 2002;39(4):343–351. doi: 10.1046/j.1365-2648.2002.02295.x. [DOI] [PubMed] [Google Scholar]
- 21.Lee MK, Chang SB, Kang D. Effects of SP6 acupressure on labor pain and length of delivery time in women during labor. J Altern Complement Med. 2004;10(6):959–965. doi: 10.1089/acm.2004.10.959. [DOI] [PubMed] [Google Scholar]
- 22.Harmon D, Ryan M, Kelly A, Bowen M. Acupressure and prevention of nausea and vomiting during and after spinal anaesthesia for caesarean section. Br J Anaesth. 2000;84(4):463–467. doi: 10.1093/oxfordjournals.bja.a013471. [DOI] [PubMed] [Google Scholar]
- 23.Shin B, Lee MS. Effects of aromatherapy acupressure on hemiplegic shoulder pain and motor power in stroke patients: a pilot study. J Altern Complement Med. 2007;13(2):247–251. doi: 10.1089/acm.2006.6189. [DOI] [PubMed] [Google Scholar]
- 24.Cho YC, Tsay SL. The effect of acupressure with massage on fatigue and depression in patients with end-stage renal disease. J Nurs Res. 2004;12(1):51–59. doi: 10.1097/01.jnr.0000387488.63438.9a. [DOI] [PubMed] [Google Scholar]
- 25.Tsay S, Rong J, Lin P. Acupoints massage in improving the quality of sleep and quality of life in patients with end-stage renal disease. J Adv Nurs. 2003;42(2):134–142. doi: 10.1046/j.1365-2648.2003.02596.x. [DOI] [PubMed] [Google Scholar]
- 26.Taylor D, Miaskowski C, Kohn J. A randomized clinical trial of the effectiveness of an acupressure device (relief brief) for managing symptoms of dysmenorrhea. J Altern Complement Med. 2002;8(3):357–370. doi: 10.1089/10755530260128050. [DOI] [PubMed] [Google Scholar]
- 27.Dent HE, Dewhurst NG, Mills SY, Willoughby M. Continuous PC6 wristband acupressure for relief of nausea and vomiting associated with acute myocardial infarction: a partially randomised, placebo-controlled trial. Complement Ther Med. 2003;11(2):72–77. doi: 10.1016/s0965-2299(03)00058-x. [DOI] [PubMed] [Google Scholar]
- 28.Turgut S, Ozalp G, Dikmen S, et al. Acupressure for postoperative nausea and vomiting in gynaecological patients receiving patient-controlled analgesia. Eur J Anaesthesiol. 2007;24(1):87–91. doi: 10.1017/S0265021506001190. [DOI] [PubMed] [Google Scholar]
- 29.Samad K, Afshan G, Kamal R. Effect of acupressure on postoperative nausea and vomiting in laparoscopic cholecystectomy. J Pak Med Assoc. 2003;53(2):68–72. [PubMed] [Google Scholar]
- 30.Roscoe JA, Bushunow P, Jean-Pierre P, et al. Acupressure bands are effective in reducing radiation therapy-related nausea. J Pain Symptom Manage. 2009;38(3):381–389. doi: 10.1016/j.jpainsymman.2008.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Molassiotis A, Helin AM, Dabbour R, Hummerston S. The effects of P6 acupressure in the prophylaxis of chemotherapy-related nausea and vomiting in breast cancer patients. Complement Ther Med. 2007;15(1):3–12. doi: 10.1016/j.ctim.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 32.Heazell A, Thorneycroft J, Walton V, Etherington I. Acupressure for the in-patient treatment of nausea and vomiting in early pregnancy: a randomized control trial. Am J Obstet Gynecol. 2006;194(3):815–820. doi: 10.1016/j.ajog.2005.08.042. [DOI] [PubMed] [Google Scholar]
- 33.Jamigorn M, Phupong V. Acupressure and vitamin B6 to relieve nausea and vomiting in pregnancy: a randomized study. Arch Gynecol Obstet. 2007;276(3):245–249. doi: 10.1007/s00404-007-0336-2. [DOI] [PubMed] [Google Scholar]
- 34.Roscoe JA, Morrow GR, Hickok JT, et al. The efficacy of acupressure and acustimulation wrist bands for the relief of chemotherapy-induced nausea and vomiting. A University of Rochester Cancer Center Community Clinical Oncology Program multicenter study. J Pain Symptom Manage. 2003;26(2):731–742. doi: 10.1016/s0885-3924(03)00254-9. [DOI] [PubMed] [Google Scholar]
- 35.Chung UL, Hung LC, Kuo SC, Huang CL. Effects of LI4 and BL 67 acupressure on labor pain and uterine contractions in the first stage of labor. J Nurs Res. 2003;11(4):251–260. doi: 10.1097/01.jnr.0000347644.35251.c1. [DOI] [PubMed] [Google Scholar]
- 36.Maa SH, Tsou TS, Wang KY, et al. Self-administered acupressure reduces the symptoms that limit daily activities in bronchiectasis patients: pilot study findings. J Clin Nurs. 2007;16(4):794–804. doi: 10.1111/j.1365-2702.2005.01515.x. [DOI] [PubMed] [Google Scholar]
- 37.Harris RE, Jeter J, Chan P, et al. Using acupressure to modify alertness in the classroom: a single-blinded, randomized, cross-over trial. J Altern Complement Med. 2005;11(4):673–679. doi: 10.1089/acm.2005.11.673. [DOI] [PubMed] [Google Scholar]
- 38.Werntoft E, Dykes A. Effect of acupressure on nausea and vomiting during pregnancy: a randomized, placebo-controlled pilot study. J Reprod Med. 2001;46(9):835–839. [PubMed] [Google Scholar]
- 39.Schultz AA, Andrews AL, Goran SF, Mathew T, Sturdevant N. Comparison of acupressure bands and droperidol for reducing post-operative nausea and vomiting in gynecologic surgery patients. Appl Nurs Res. 2003;16(4):256–265. doi: 10.1016/s0897-1897(03)00057-0. [DOI] [PubMed] [Google Scholar]
- 40.Ho CM, Tsai HJ, Chan KH, Tsai SK. P6 acupressure does not prevent emesis during spinal anesthesia for cesarean delivery. Anesth Analg. 2006;102(3):900–903. doi: 10.1213/01.ane.0000195553.82409.00. [DOI] [PubMed] [Google Scholar]
- 41.Shin HS, Song YA, Seo A. Effect of Nei-Guan (P 6) point acupressure on ketonuria levels, nausea and vomiting in hyperemesis gravidarum. J Adv Nurs. 2007;59(5):510–519. doi: 10.1111/j.1365-2648.2007.04342.x. [DOI] [PubMed] [Google Scholar]
- 42.Klein AA, Djaiani G, Karski J, et al. Acupressure wristbands for the prevention of postoperative nausea and vomiting in adults undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 2004;18(1):68–71. doi: 10.1053/j.jvca.2003.10.014. [DOI] [PubMed] [Google Scholar]
- 43.Sadighha A, Nurai N. Acupressure wristbands versus metoclopramide for the prevention of postoperative nausea and vomiting. Ann Saudi Med. 2008;28(4):287–291. doi: 10.5144/0256-4947.2008.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Maa SH, Sun MF, Hsu KH, et al. Effect of acupuncture or acupressure on quality of life of patients with chronic obstructive asthma: a pilot study. J Altern Complement Med. 2003;9(5):659–670. doi: 10.1089/107555303322524517. [DOI] [PubMed] [Google Scholar]
- 45.Tsay S, Chen M. Acupressure and quality of sleep in patients with end-stage renal disease: a randomized controlled trial. Int J Nurs Stud. 2003;40(1):1–7. doi: 10.1016/s0020-7489(02)00019-6. [DOI] [PubMed] [Google Scholar]
- 46.Agarwal A, Pathak A, Gaur A. Acupressure wristbands do not prevent postoperative nausea and vomiting after urological endoscopic surgery. Can J Anaesth. 2000;47(4):319–324. doi: 10.1007/BF03020945. [DOI] [PubMed] [Google Scholar]
- 47.Agarwal A, Bose N, Gaur A, et al. Acupressure and ondansetron for postoperative nausea and vomiting after laparoscopic cholecystectomy. Can J Anaesth. 2002;49(6):554–560. doi: 10.1007/BF03017380. [DOI] [PubMed] [Google Scholar]
- 48.Alkaissi A, Evertsson K, Johnsson VA, Ofenbartl L, Kalman S. P6 acupressure may relieve nausea and vomiting after gynecological surgery: an effectiveness study in 410 women. Can J Anaesth. 2002;49(10):1034–1039. doi: 10.1007/BF03017897. [DOI] [PubMed] [Google Scholar]
- 49.Alkaissi A, Ledin T, Odkvist LM, Kalman S. P6 acupressure increases tolerance to nauseogenic motion stimulation in women at high risk for PONV. Can J Anaesth. 2005;52(7):703–709. doi: 10.1007/BF03016557. [DOI] [PubMed] [Google Scholar]
- 50.Pouresmail Z, Ibrahimzadeh R. Effects of acupressure and ibuprofen on the severity of primary dysmenorrhea. J Tradit Chin Med. 2002;22(3):205–210. [PubMed] [Google Scholar]
- 51.Kober A, Scheck T, Greher M, et al. Prehospital analgesia with acupressure in victims of minor trauma: a prospective, randomized, double-blinded trial. Anesth Analg. 2002;95(3):723–727. doi: 10.1097/00000539-200209000-00035. [DOI] [PubMed] [Google Scholar]
- 52.Lang T, Hager H, Funovits V. Prehospital analgesia with acupressure at the Baihui and Hegu points in patients with radial fractures: a prospective, randomized, double-blind trial. Am J Emerg Med. 2007;25(8):887–893. doi: 10.1016/j.ajem.2007.01.016. [DOI] [PubMed] [Google Scholar]
- 53.Hsieh LL, Kuo C, Lee LH, et al. Treatment of low back pain by acupressure and physical therapy: randomised controlled trial. Br Med J. 2006;332(7543):696–698. doi: 10.1136/bmj.38744.672616.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hsieh LL, Kuo CH, Yen MF, Chen TH. A randomized controlled clinical trial for low back pain treated by acupressure and physical therapy. Prev Med. 2004;39(1):169–176. doi: 10.1016/j.ypmed.2004.01.036. [DOI] [PubMed] [Google Scholar]
- 55.Sakurai M, Suleman MI, Morioka N, Akca O, Sessler DI. Minute sphere acupressure does not reduce postoperative pain or morphine consumption. Anesth Analg. 2003;96(2):493–497. doi: 10.1097/00000539-200302000-00036. [DOI] [PubMed] [Google Scholar]
- 56.Molassiotis A, Sylt P, Diggins H. The management of cancer-related fatigue after chemotherapy with acupuncture and acupressure: a randomised controlled trial. Complement Ther Med. 2007;15(4):228–237. doi: 10.1016/j.ctim.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 57.Lee A, Fan LT. Stimulation of the wrist acupuncture point P6 for preventing postoperative nausea and vomiting. Cochrane Database Syst Rev. 2009;2:CD003281–CD003281. doi: 10.1002/14651858.CD003281.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Barford KL, D’Olimpio JT. Symptom management in geriatric oncology: practical treatment considerations and current challenges. Curr Treat Options Oncol. 2008;9(2–3):204–214. doi: 10.1007/s11864-008-0062-4. [DOI] [PubMed] [Google Scholar]
- 59.Kromer TO, Tautenhahn UG, de Bie RA, Staal JB, Bastiaenen CH. Effects of physiotherapy in patients with shoulder impingement syndrome: a systematic review of the literature. J Rehabil Med. 2009;41(11):870–880. doi: 10.2340/16501977-0453. [DOI] [PubMed] [Google Scholar]
- 60.Hassett AL, Gevirtz RN. Nonpharmacologic treatment for fibromyalgia: patient education, cognitive-behavioral therapy, relaxation techniques, and complementary and alternative medicine. Rheum Dis Clin North Am. 2009;35(2):393–407. doi: 10.1016/j.rdc.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mansky PJ, Wallerstedt DB. Complementary medicine in palliative care and cancer symptom management. Cancer J. 2006;12(5):425–431. doi: 10.1097/00130404-200609000-00011. [DOI] [PubMed] [Google Scholar]
- 62.Carlson LE, Bultz BD. Mind-body interventions in oncology. Curr Treat Options Oncol. 2008;9(2–3):127–134. doi: 10.1007/s11864-008-0064-2. [DOI] [PubMed] [Google Scholar]
- 63.Dodd M, Janson S, Facione N, et al. Advancing the science of symptom management. J Adv Nurs. 2001;33(5):668–676. doi: 10.1046/j.1365-2648.2001.01697.x. [DOI] [PubMed] [Google Scholar]
- 64.Rosenberg EI, Genao I, Chen I, et al. Complementary and alternative medicine use by primary care patients with chronic pain. Pain Med. 2008;9(8):1065–1072. doi: 10.1111/j.1526-4637.2008.00477.x. [DOI] [PubMed] [Google Scholar]
- 65.Mans J, Zhi L, Revilleza MJ, et al. Structure and function of murine cytomegalovirus MHC-I-like molecules: how the virus turned the host defense to its advantage. Immunol Res. 2009;43(1–3):264–279. doi: 10.1007/s12026-008-8081-6. [DOI] [PMC free article] [PubMed] [Google Scholar]