Abstract
Objective
Investigate moderators of a randomized clinical trial of group Dialectical Behavior Therapy for Binge Eating Disorder (DBT-BED) compared to an active comparison group control (ACGT) on the post-treatment outcome of binge frequency after twenty 2-hour weekly sessions.
Method
Moderation analyses.
Results
Participants were 101 adults with BED [mean (SD) age, 52.2 (10.6) years and BMI, 36.4 (8.6)]. Analyses identified two moderators of post-treatment outcome. Participants with (1) Avoidant Personality Disorder or (2) an earlier onset of overweight and dieting (< 15 years old) evidenced significantly worsened outcome when treated with ACGT versus DBT-BED.
Discussion
Participants with certain indicators of higher baseline pathology respond better to DBT-BED than ACGT at post-treatment.
Keywords: Dialectical Behavior Therapy, Binge Eating Disorder, moderators, randomized clinical trial, emotion regulation
Background
Lifetime prevalence estimates for Binge Eating Disorder (BED) in the general population are 3.5% in woman and 2% in men (1), 4–8% among obese individuals in a community based sample, and up to 30% of weight control program participants (2, 3). To date, the most studied treatments for BED include Cognitive Behavioral Therapy (CBT), Interpersonal Psychotherapy (IPT), and Behavioral Weight Loss (BWL). Results from two randomized clinical trials (RCTs) comparing CBT and IPT indicate the two treatments have equivalent immediate and longer term binge abstinence rates (4, 5). A comparison of CBT and BWL demonstrated that there were no significant between group differences in reducing self-reported weekly binges at 16 weeks post-treatment or at 12 month follow-up using intention-to-treat data (6).
While CBT, IPT, and BWL are effective, a substantial number of patients remain symptomatic at post-treatment or follow-up (4, 5, 6). Consequently, new treatments such as Dialectical Behavior Therapy for BED (DBT-BED) were developed. DBT, originally developed by Linehan (7; 8) to treat emotion dysregulation in Borderline Personality Disorder, was adapted to target binge eating and has shown initial promise both in an uncontrolled and controlled comparison trial against a wait-list population (9, 10). In a recent RCT comparing DBT-BED to an active comparison group therapy (ACGT), DBT-BED had significantly higher post treatment binge abstinence rates than ACGT (67% vs. 33% respectively) however at 12 month follow-up, the differences were smaller and no longer statistically significant (11). Identifying moderators of outcome (i.e., baseline characteristics of the sample such as age, baseline symptom severity, presence of co-morbid personality disorders, etc.) is instrumental in differentiating subsets of patients for whom one treatment works better than another (12). Moderation analyses are two-step processes. First, an exploratory analysis is used to generate hypotheses about putative moderators. If the effect of an intervention depends upon the level of a third variable (e.g., an effect modifier), moderation is present. The second step is designing a subsequent trial of adequate power to test the validity of the previously identified moderators.
This RCT comparing DBT-BED to a carefully designed active comparison group therapy (ACGT) provides an opportunity to explore putative moderators of DBT-BED. While recent work has investigated preliminary moderators of BED treatment (13, 14), no previous study has been published investigating such characteristics of DBT-BED. Therefore, the purpose of this study is to generate and evaluate hypotheses about putative moderators of post-treatment outcome in a RCT of DBT-BED compared to an ACGT.
Methods
Participants
The study was reviewed and approved by the Institutional Review Board of Stanford University Medical Center. Participants were recruited through newspaper advertisements, flyers, and clinic referrals for “treatment for binge eating.” Eligibility was assessed via an initial telephone screen followed by an in-person clinical interview, during which potential participants provided informed written consent. Men and women who lived or worked within commuting distance of the clinic meeting Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) research criteria for BED (15) were included. Exclusionary criteria were: 1) body mass index (BMI) less than 17.5 kilograms/meters2 (kg/m2); 2) concurrent psychotherapy treatment; 3) unstable dosage of psychotropic medications over the 3 months prior to initial assessment; 4) regular use of purging or other compensatory behaviors over the past six months; 5) psychosis; 6) current alcohol/drug abuse or dependence; 7) severe depression with recent (e.g., within past month) suicidality; 8) current use of weight altering medications (e.g., phentermine); 9) severe medical condition affecting weight or appetite (e.g., insulin dependent diabetes, cancer requiring active chemotherapy); 10) current pregnancy or breast feeding; 11) imminently planning for gastric bypass surgery; and 12) lack of availability for times of group meetings and/or for the duration of the study.
The sample consisted of 101 adults, 85% (n=86) women, with a mean (± SD) age of 52.2 (± 10.6) years and BMI of 36.38 (± 8.62) kg/m2. Participants were 76% (n=77) Caucasian, 13% (n=13) Latino, 5% (n=5) Asian, and 3% (n=3) African American. Sixty percent (n=61) of participants were married, 19% (n=19) divorced, 17% (n=17) single or never married, and 4% (n=4) widowed. Four percent (n=4) had not completed high school, 3% (n=2) had high school degrees or the equivalent, 29.7% (n= 30) completed some college or a 2 year degree, 25.7% (n=26) graduated from a 4 year college, 8.9% (n=9) completed some graduate school, and 29.7% (n=30) completed at least one graduate degree. About half of the sample was employed (49.5%, n=50), 18.8% (n=19) retired, 13.9% (n=14) homemakers, 12% (n= 11) unemployed, and 6% (n= 6) students or other. On average, participants were 17.35 (± 11.25) years old when first overweight, 17.70 (± 9.02) years old when they first began dieting, and 19.42 (± 12.69) years old when they began to binge eat.
Treatment
Both treatments were manual-based and consisted of a pre-treatment orientation to the theoretical model followed by 20 two-hour weekly group sessions.
DBT-BED
The manual for the DBT treatment was based on Linehan’s Dialectical Behavior Therapy for Borderline Personality Disorder (7, 8) that was previously adapted for BED (16). Briefly (for greater detail see 10, 11, 17), the highly structured 20 session treatment consisted of two introductory sessions presenting the DBT rationale along with an orientation and commitment to treatment, sixteen sessions teaching adaptive emotion regulation skills over three modules (Mindfulness, Emotion Regulation, and Distress Tolerance), and two final sessions devoted to review and relapse prevention. Each two hour DBT group session was divided into a review of homework (e.g., a chain analysis of a recent binge episode) and an hour of didactic teaching of new emotion regulation skills.
ACGT
ACGT was developed with the goal of creating a comparison therapy whose rationale and procedures would be credible enough to generate therapeutic factors in common with DBT (i.e., therapeutic alliance, treatment expectations, therapeutic optimism) while lacking the specific elements of DBT and other BED treatments. Each 2-hour session followed a non-directive Rogerian approach. The manual was modeled after Markowitz and Sacks’ (18) manual of supportive therapy for chronic depression and subsequently modified to address binge eating for the current study. While homework was assigned within the ACGT condition, the homework review was much less structured than in DBT. Interested readers are referred to Safer & Hugo (19) for a detailed discussion of the design of the credible comparison control.
Analysis Plan: The MacArthur Method
The MacArthur Method of investigating moderators was developed as an exploratory approach to identifying how risk factors work together (12, 20, 21). This method was employed in the present RCT to investigate putative moderators of treatment. The primary outcome of interest was number of days of objective binge eating over the past 28 days as assessed at post-treatment. In summary, analysis steps were (1) to identify, a priori, the constructs hypothesized to be moderators of treatment (e.g., between DBT and ACGT), (2) re-code and center putative moderator variables (binary variables had been coded as +1/2 and −1/2, ordinal variables were centered around their median score), and (3) test the putative moderators of treatment via linear regression models [where the potential moderator (M), treatment (T), and the T × M interaction are independent variables regressed on the outcome (O), as defined by Kraemer et al. (12)]. Significant moderators were further analyzed via two-way Analysis of Variance (ANOVA) and subsequent t-tests to determine the direction of the differences between the groups.
Assessments
Outcome Measure
The Eating Disorder Examination (EDE; 22) was used to assess the primary outcomes: frequency of binge eating (over the prior 28 days) at post treatment. The EDE is a widely used semi-structured interview that assesses primary behavioral and attitudinal eating disorder features. All EDE interviewers received extensive training, with the lead assessors trained by Dr. Christopher Fairburn, who developed the measure. All EDE interviews were audiotaped and consistency of examiners’ interviewing techniques was checked by an independent rater who reviewed randomly selected audiotapes. Interrater agreement for the EDE has been shown to be above .90 for all subscales and behavior items and test-retest agreement above 0.70, except for the item on subjective bulimic episodes (0.40) (23).
Moderator Measures
Putative moderators were divided into three categories including (1) demographic variables, (2) eating disorder psychopathology variables, and (3) general psychopathology variables. The demographic putative moderators were: age, sex, education, and ethnicity/race. Eating disorder pathology putative moderators included: the Eating Disorder Examination (restraint, weight, shape, and eating concerns subscales), the Questionnaire on Eating and Weight Patterns (onset of overweight, dieting, binge eating, and lowest/highest weight variables), and the Emotional Eating Scale (anger, depression, and anxiety subscales). General psychopathology putative moderators were garnered from the following measures: The Structured Clinical Interview for DSM-IV for Axis II, Disorders of Emotion Regulation Scale (impulse, goals, non-acceptance, awareness, strategies, and clarity subscales), the Beck Depression Inventory, and the Rosenberg Self-Esteem Scale. Due to the large number of moderator variables explored in this study, only ones relevant to the findings will be described with more detail.
Eating Pathology Measures
The Emotional Eating Scale (EES; 24) has 25-items assessing the extent to which specific negative emotional states prompt an individual to feel an urge to eat. Respondents indicate on a 5-point Likert scale the extent to which 25 different feelings (e.g., sad, irritated, guilty, uneasy) lead them to feel an urge to eat. The EES contains three separate subscales: Anger/Frustration, Anxiety, and Depression. It is internally consistent and demonstrates adequate temporal stability (24).
The Questionnaire on Eating and Weight Patterns (QEWP; 2) is a self-report instrument that asks retrospective questions about the onset of binge eating, dieting, and obesity (e.g. “How old were you when you first started dieting?”, and “At what age did you first weigh more than people thought you should?”).
General Psychopathology Measures
The Structured Clinical Interview for DSM-IV for Axis II (SCID-II; 25) was used to determine the presence of personality disorders in the participants. The reliability and validity of the SCID II has been well documented (26, 27, 28).
The Beck Depression Inventory (BDI; 29) is a 21-item questionnaire of the degree of depressive symptoms, including somatic, affective, cognitive, and behavioral dimensions. It has good test-retest reliability, internal consistency, and convergent validity (30).
The Rosenberg Self Esteem Scale (RSE; 31) is a 10-item questionnaire assessing beliefs and attitudes regarding general self-worth. Higher scores indicate higher self-esteem. The RSE has been shown to have satisfactory internal consistency, test-retest reliability, and convergent validity (32).
The Difficulties of Emotion Regulation Scale (DERS; 33) is a 36-item self-report measure that examines difficulties in the ability to regulate emotions. Participants rate how often statements such as “I feel at ease with my emotions” apply to them using a 5-point Likert scale, with higher scores reflecting greater difficulties with emotion regulation. A global score can be derived, as well as six subscale scores (subscales include: Goals, Impulsive, Non-Acceptance, Awareness, Strategies, and Clarity). Research suggests the DERS has high internal consistency, good test retest reliability, and adequate construct and predictive validity (33).
Results
The sample included 101 men (15%) and women (85%) meeting DSM-IV research criteria for binge eating disorder (American Psychiatric Association, 1994) with a mean age of 52.2 (±10.6) and mean BMI of 36.4 (±8.6) kg/m2. Please see Safer et al. (11) for details regarding demographics, methodological procedures, and primary outcome results.
All data (demographic, eating and general pathology) were tested for between group differences. The only significant between group difference was presence of a current major depressive episode, which was significantly more prevalent in the DBT-BED group (22% or 11/50) than in the ACGT group (7.8% or 4/51) (χ2(1, n=101)=4.00, p=.045). However, baseline BDI scores did not significantly differ between groups. See Safer et al. (11) for further detail.
Intent to treat analysis was completed on the primary outcome variable post-treatment frequency of binge eating (assessed over the prior 28 days). This included the scores of three individuals who did not complete post-treatment assessment (completers were 97%, n= 98/101) using last-observation-carried forward for missing data at post-treatment.
Moderation Analyses
Two baseline variables were moderators of post-treatment, by evidencing a significant interaction with treatment condition when regressed on outcome (number of binge days over the previous 28 days).
Post-Treatment Moderators
Initially, there were three moderators of post-treatment outcome: Avoidant Personality Disorder (Avoidant PD; p=.026), age at onset of initial overweight status (p=.006) and age at onset of first diet which resulted in a loss of 10 lbs or more (p=.026).
Two variables, onset of initial overweight status and onset of first diet, were found to be overlapping. Overlapping variables are variables that are correlated with each other, occur at the same time period, and each influence the outcome of interest. In the present study, age at initial overweight status and age at first diet were significantly correlated (r=.76, p<.01), both occurred at relatively similar time points [overweight status mean (±SD) age=17.35 (±11.25); first diet mean age=17.70 (±9.02)], and both accounted for significant variance in the outcome of interest. In order to reduce redundancy, the two variables were combined into one variable, the age at onset of overweight and dieting, which was created to reflect the combined constructs of the original two variables. Combining overlapping risk factors into a single risk factor is a general recommendation of moderation analysis (20). The new variable, age at onset of overweight and dieting, was subject to the linear regression moderator analysis and was found to be a significant moderator of treatment on outcome (p=.025).
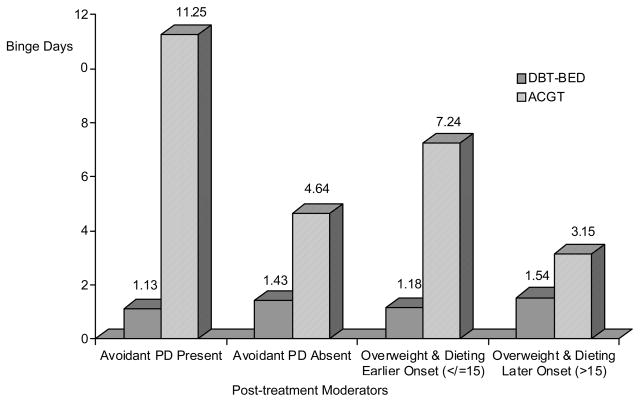
Two-way Analysis of Variance (ANOVA) and subsequent t-tests were applied to each moderator to determine the direction of the differences between the groups. Both Avoidant Personality Disorder (PD) and age at onset of overweight and dieting were divided into four subgroups each (e.g., Within DBT-BED, Avoidant PD present and Avoidant PD absent vs. within ACGT, Avoidant PD present and Avoidant PD absent). Comparison of the post-treatment moderator subgroups is presented in Figure 1.
Figure 1.
Comparison of post-treatment moderator subgroups
Note. Binge Days=number of binge days over the previous 28 days assessed via the Eating Disorder Examination; DBT-BED=Dialectical Behavior Therapy for Binge Eating Disorder; ACGT=Active Comparison Group Therapy; Avoidant PD=Avoidant Personality Disorder.
(1) Avoidant PD
DBT-BED participants with Avoidant PD had significantly fewer binge days at post-treatment compared to ACGT participants with Avoidant PD (DBT-BED: 1.13 (±1.73) vs. ACGT: 11.25 (±9.78), p=.014). DBT-BED participants without Avoidant PD had significantly fewer binge days compared to ACGT participants without Avoidant PD (p=.002).
(2) Age of Onset of Overweight and Dieting
The variable age of onset of dieting and overweight was subjected to a split at age 15, which was the average of the original variables’ medians (overweight’s median=14 and dieting’s median=16), to reflect two groups: 1) Early onset (i.e., participants who were overweight and began dieting at 15 years or younger) and 2) Late onset (i.e., participants who were older than 15 years when they were initially overweight and/or began dieting). Post-treatment analyses for the onset of overweight and dieting indicated that earlier onset participants in DBT-BED had significantly fewer binge days compared to earlier onset participants in ACGT (DBT-BED: 1.3(±2.02) vs. ACGT: 6.62(±7.06), p=.003). There was no significant difference between later onset participants in DBT-BED and ACGT (p=.054).
Discussion
The present study investigated moderators in an RCT comparing DBT-BED to an active comparison group control therapy (ACGT). Two moderators of post-treatment outcome were identified. In general, participants for whom the moderator indicated the presence of higher baseline pathology responded better to DBT-BED than to a control. The present findings are of interest as they support previous work documenting the impact of specific factors (e.g., personality disorders) on binge eating remission in BED treatment (13, 14).
Post-Treatment Moderators
The presence or absence of Avoidant PD (as measured by the SCID II) moderated the effect of the treatment on binge days at post-treatment. In other words, for participants with Avoidant PD, treatment with DBT-BED was associated with improved outcomes (e.g., fewer binge days over the prior month) compared to those randomized to ACGT. One potential explanation for this finding is that ACGT’s largely patient-led process-oriented sessions, compared with DBT-BED’s highly structured and didactic sessions, were not optimal for participants with Avoidant PD. Another possible explanation is that participants with Avoidant PD - one of the most common co-morbid PDs in BED (35), benefit specifically from DBT-BED’s emotion regulation focus. However, such hypotheses need to be investigated in future research.
The presence of an early (≤15 years old) versus later (≥15 years old) onset of overweight and dieting was a second moderator of post-treatment outcome as measured by frequency of binge days over the previous 28 days. Participants with an earlier age at the onset of overweight and dieting randomized to ACGT responded more poorly, with significantly higher binge frequencies at post-treatment, compared to those randomized to DBT-BED. An earlier onset of overweight and dieting may be associated with earlier and more highly entrenched maladaptive food-related coping behaviors. If so, one possible implication is that participants with this earlier age of onset may benefit from a specific teaching focus on alternative adaptive emotion regulation skills and thus differentially gain from DBT-BED compared to ACGT, with its more broadly-based consideration of self-esteem.” Participants whose onset of overweight and dieting was later, and whose maladaptive behaviors may have been less firmly established, showed similar rates of binge eating at post-treatment in both ACGT and DBT-BED. Such findings are consistent with previous research linking early age of onset of binge eating to poorer recovery outcomes among individuals with BED (36). In this study, age of onset of binge eating (mean 19.42 (±=12.69) was highly correlated with onset of overweight and dieting (mean=17.53(±=9.55); r=.689, p<.001).
This study has various strengths. First, it contributes to a limited research literature investigating moderators of treatment outcome in BED by generating hypotheses regarding moderators of DBT-BED, a relatively recently introduced treatment. In addition, the present study’s findings support previous results that personality disorders (13, 14) are related to poorer prognosis in BED patients. Other strengths of this study include its overall moderately large sample size and a carefully designed comparison group (see 19 for further detail).
Limitations of the study include that its recommendations are preliminary. By definition, moderator analyses are exploratory and intended to be used to design a subsequent, adequately powered, study to replicate the original findings (20). Also, while the overall sample size of the study was moderately large, identification of subgroups among whom the moderator was present or absent resulted in smaller cell sizes for each condition. This was particularly evident in relation to the moderator Avoidant PD, as only 12 study participants overall met criteria for this diagnosis (n=8 in DBT-BED and n=4 in ACGT). Nonetheless, this finding remains of clinical relevance. As mentioned, Avoidant PD is one of the more common Axis II diagnoses within the BED population (35). Also, the presence of Cluster C disorders, such as Avoidant PD, was found to predict worsened outcome in terms of higher levels of eating disorder psychopathology and negative affect (13).
The purpose of the present study was to generate hypotheses about potential moderators of DBT-BED. Future studies might stratify participants based on these moderators so that, at the outset, those with higher baseline pathology on specific measures could be purposefully treated with the more skills intensive, more expensive DBT-BED. Identifying moderators of treatments for BED is an important endeavor as such data will ultimately lead to the development of interventions that yield greater effect sizes at a decreased cost.
Acknowledgments
The authors gratefully acknowledge Brenda Brownlow, Emily Hugo, and Rebecca Klein for their involvement on this study.
Funding: This research was funded by a grant from the National Institute of Mental Health, K23MH066330
Footnotes
No financial disclosures or conflicts of interest exist regarding the subject matter of this manuscript.
References
- 1.Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kalarchian MA, Marcus MD, Levine MD, Courcoulas AP, Pilkonis PA, Ringhma RM, et al. Psychiatric disorders among bariatric surgery candidates: Relationship to obesity and functional health status. American Journal of Psychiatry. 2007;164:328–334. doi: 10.1176/ajp.2007.164.2.328. [DOI] [PubMed] [Google Scholar]
- 3.Marcus MD, Levine MD. Obese patients with binge eating disorder. In: Goldstein DF, editor. The management of eating disorders and obesity. 2. Totowa, NJ: Humana Press; 2004. pp. 143–160. [Google Scholar]
- 4.Wilfley DE, Agras WS, Telch CF, Rossiter EM, Schneider JA, Cole AG, Sifford LA, Raeburn SD. Group cognitive-behavioral therapy and group interpersonal psychotherapy for the nonpurging bulimic individual: a controlled comparison. Journal of Consulting and Clinical Psychology. 1993;61:296–305. doi: 10.1037//0022-006x.61.2.296. [DOI] [PubMed] [Google Scholar]
- 5.Wilfley DE, Welch RR, Stein RI, Spurrell EB, Cohen LR, Saelens BE, Dounchis JZ, Frank MA, Wiseman CV, Matt GE. A randomized comparison of group cognitive-behavioral therapy and group interpersonal psychotherapy for the treatment of overweight individuals with binge eating disorder. Archives of General Psychiatry. 2002;59:713–721. doi: 10.1001/archpsyc.59.8.713. [DOI] [PubMed] [Google Scholar]
- 6.Munsch S, Biedert E, Meyer A, Michael T, Schlup B, Tuch A, Margraf J. A randomized comparison of cognitive behavioral therapy and behavioral weight loss treatment for overweight individuals with Binge Eating Disorder. International Journal of Eating Disorders. 2007;40:102–113. doi: 10.1002/eat.20350. [DOI] [PubMed] [Google Scholar]
- 7.Linehan MM. Cognitive behavioral therapy of borderline personality disorder. New York: Guilford Press; 1993a. [Google Scholar]
- 8.Linehan MM. Skills training manual for treating borderline personality disorder. New York: Guilford Press; 1993b. [Google Scholar]
- 9.Telch CF, Agras WS, Linehan MM. Group dialectical behavior therapy for binge eating disorder: A preliminary, uncontrolled trial. Behavior Therapy. 2000;31:569–582. [Google Scholar]
- 10.Telch CF, Agras WS, Linehan MM. Dialectical behavior therapy for binge eating disorder. Journal of Consulting and Clinical Psychology. 2001;69:1061–1065. doi: 10.1037//0022-006x.69.6.1061. [DOI] [PubMed] [Google Scholar]
- 11.Safer DL, Robinson AH, Jo B. Outcomes from a randomized controlled trial of group therapy for Binge Eating Disorder: Comparing Dialectical Behavior Therapy and an active comparison group therapy. Behavior Therapy. 2010;41:106–120. doi: 10.1016/j.beth.2009.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 13.Masheb RM, Grilo CM. Examination of predictors and moderators for self-help treatments of binge-eating disorder. Journal of Consulting and Clinical Psychology. 2008;76:900–904. doi: 10.1037/a0012917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilson GT, Wilfley DE, Agras WS, Bryson SW. Psychological treatments of binge eating disorder. Archives of General Psychiatry. 2010;67:94–101. doi: 10.1001/archgenpsychiatry.2009.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 16.Telch CF. Emotion regulation skills training treatment for binge eating disorder: Therapist manual. 1997. Copyrighted unpublished manuscript. [DOI] [PubMed] [Google Scholar]
- 17.Wiser S, Telch CF. Dialectical behavior therapy for binge eating disorder. Journal of Clinical Psychology. 1999;55:155–768. doi: 10.1002/(sici)1097-4679(199906)55:6<755::aid-jclp8>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 18.Markowitz J, Sacks M. Unpublished manuscript. 2002. Manual for brief supportive psychotherapy. [Google Scholar]
- 19.Safer DL, Hugo EM. Designing a control for a behavioral group therapy. Behavior Therapy. 2006;37:120–130. doi: 10.1016/j.beth.2005.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kraemer HC, Lowe KK, Kupfer DJ. To Your Health: How to Understand What Research Tells Us About Risk. New York, NY: Oxford University Press; 2005. [Google Scholar]
- 21.Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer DJ. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. American Journal of Psychiatry. 2001;158:848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- 22.Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating: nature, assessment, and treatment. 12. New York: Guildford Press; 1993. pp. 317–360.pp. 317–331. [Google Scholar]
- 23.Rizvi SL, Peterson CB, Crow SJ, Agras WS. Test-retest reliability of the Eating Disorder Examination. International Journal of Eating Disorders. 2000;28:311–316. doi: 10.1002/1098-108x(200011)28:3<311::aid-eat8>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 24.Arnow B, Kenardy J, Agras WS. The Emotional Eating Scale: The development of a measure to assess coping with negative affect by eating. Int J Eat Disord. 1995;18:79–90. doi: 10.1002/1098-108x(199507)18:1<79::aid-eat2260180109>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 25.First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured clinical interview for DSM-IV axis II personality disorders self-report. Washington, DC: American Psychiatric Association; 1997. [Google Scholar]
- 26.Segal DL, Hersen M, Van Hasselt VB. Reliability of the Structured Clinical Interview for DSM-III-R: An evaluative review. Comprehensive Psychiatry. 1994;35:316–327. doi: 10.1016/0010-440x(94)90025-6. [DOI] [PubMed] [Google Scholar]
- 27.Renneberg B, Chambless DL, Dowdall DJ, Fauerbach JA, Gracely EJ. The Structured Clinical Interview for DSM-III-R, Axis II and the Millon Clinical Multiaxial Inventory: A concurrent validity study of personality disorders among anxious outpatients. Journal of Personality Disorders. 1992;6:117–124. [Google Scholar]
- 28.O’Boyle M, Self D. A comparison of two interviews for DSM-III-R personality disorders. Psychiatric Research. 1990;32:85–92. doi: 10.1016/0165-1781(90)90138-u. [DOI] [PubMed] [Google Scholar]
- 29.Beck A, Ward C, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 30.Beck AT, Steer RM, Garbin M. Psychometric properties of the Beck Depression Inventory: 25 years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- 31.Rosenberg M. Society and the Adolescent Self Image. Princeton: Princeton University Press; 1965. [Google Scholar]
- 32.Demo DH. The measurement of self-esteem: refining our methods. Journal of Personality and Social Psychology. 1985;48:1490–1502. [Google Scholar]
- 33.Gratz KL, Rommer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Psychopathology and Behavioral Assessment. 2004;26:41–54. [Google Scholar]
- 34.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 35.Grilo CM. Recent research of relationships among eating disorders and personality disorders. Current Psychiatry Reports. 2002;4:18–24. doi: 10.1007/s11920-002-0007-8. [DOI] [PubMed] [Google Scholar]
- 36.Agras WS, Telch CF, Arnow B, Eldredge K, Detzer MJ, Henderson J, Marnell M. Does interpersonal therapy help patients with binge eating disorder who fail to respond to cognitive-behavioral therapy? Journal of Consulting and Clinical Psychology. 1995;63:356–360. doi: 10.1037//0022-006x.63.3.356. [DOI] [PubMed] [Google Scholar]