Abstract
Objective.
Prior studies have extensively examined the reciprocal relation between disability and depressive symptoms in late life, but little is known about whether informal care attenuates the reciprocal relation over time. This study examined whether disability and depressive symptoms mobilize informal care and whether informal care, once mobilized, protects older adults against the progression of disability and depressive symptoms.
Methods.
The analysis was based on 6,454 community-dwelling older adults who were interviewed in one or more waves of the Health and Retirement Study between 1998 and 2006. Extending an autoregressive cross-lagged model, we constructed 3 cycles of the relations among disability, depressive symptoms, and informal care. Comparing the relations across 3 cycles informs us about the attenuating effect of informal care on the relation between disability and depressive symptoms over time.
Results.
Although older adults’ disability and depressive symptoms mobilized informal care initially, worsening disability and depressive symptoms often exhausted support. Receipt of care generally increased, rather than decreased, disability and depressive symptoms, and the detrimental effects remained the same over time.
Discussion.
We need to better understand the linkage between disability and depressive symptoms and seek effective interventions to reduce caregiver strain and enhance care receivers’ well-being.
Keywords: ADL/IADL disability, Depressive symptoms, Informal care
DISABILITY and depressive symptoms increase with advanced age and significantly threaten older adults’ well-being (Conwell & Brent, 1996; Kaplan, McFarland, Huguet, & Newsom, 2007). Such age-related patterns have drawn researchers’ attention to the reciprocal relation between disability and depressive symptoms. Disability has been shown to both prevent older adults from performing social roles and disrupt their daily routines, leading to the development of depressive symptoms (Geerlings, Beekman, Deeg, & van Tilburg, 2000; Zeiss, Lewinsohn, Rohde, & Seeley, 1996). At the same time, depressive symptoms create feelings of hopelessness and helplessness and reduce individuals’ motivation to maintain good nutrition and comply with medical treatments, contributing to the emergence of disability (Bruce, Seeman, Merrill, & Blazer, 1994; Lenze et al., 2005). Given the impact of disability and depressive symptoms on older adults’ well-being, it is imperative to find ways to deter them from reinforcing each other.
Social support literature has long emphasized the importance of support networks and the protective effect of informal care (Kahn & Antonucci, 1980; Umberson, Crosnoe, & Reczek, 2010). When trying to overcome stressful life conditions, such as disability and depressive symptoms, older adults often seek help from their spouses, adult children, other relatives, or friends. Past studies have shown that individuals who receive support are able to cope with stressful events better than those who receive little or no support (Greenglass, Fiksenbaum, & Eaton, 2006; Wilcox, Kasl, & Berkman, 1994), suggesting that utilization of informal care may help attenuate the reciprocal relation between disability and depressive symptoms. Few studies, however, have considered whether the protective effect remains the same or dissipates over time.
It is critical to examine whether social support has the same protective effect for disabled or depressed older adults over time. As individuals age, the likelihood of having a health condition increases but social networks shrink (Barnes, Mendes de Leon, Bienias, & Evans, 2004). Consequently, it becomes harder for older adults to mobilize social support. In addition, caring for older adults with disability or depressive symptoms strains the time, finances, and health of many caregivers (Pinquart & Sörensen, 2003). Over time, caregiver strain is likely to generate negative interactions between older adults and their caregivers. These stressful interactions may subsequently negatively affect disabled or depressed older adults’ immune systems and motivation to get better, leading to further progression of debilitating symptoms (Berkman, Glass, Brissette, & Seeman, 2000; Uchino, 2006). Thus, informal care may eventually lose its protective effect and could even become a stressor further exacerbating the cycle of disability and depressive symptoms among older adults.
No studies have yet examined whether informal care attenuates the relation between disability and depressive symptoms over time because either the necessary data or an appropriate analytic strategy has been lacking. Most researchers use cross-sectional or two-wave data, but such data do not allow researchers to establish the temporal order of disability, informal care, and depressive symptoms. Thus, it is impossible to examine informal care’s intervening effect. In addition, although prior researchers have adopted an autoregressive cross-lagged model to examine the reciprocal relation between disability and depressive symptoms (e.g., Gayman, Turner, & Cui, 2008; Ormel, Rijsdijk, Sullivan, van Sonderen, & Kempen, 2002), none has included informal care as a mediating variable between disability and depressive symptoms. In the current study, we address this research gap by using five-wave panel data from the Health and Retirement Study (HRS) and extend an autoregressive cross-lagged model to include informal care as a mediating variable. The data and analytic strategy allow us to answer the following questions: (a) Do disability and depressive symptoms mobilize informal care? (b) Does informal care, once mobilized, reduce disability and depressive symptoms? (c) Does the pattern in which informal care is mobilized by and reduces disability and depressive symptoms remain the same over time?
RECIPROCAL RELATION BETWEEN DISABILITY AND DEPRESSIVE SYMPTOMS
The prevalence rates of both disability and depressive symptoms increase with age. It is estimated that disability is present in 9% of young–old (ages 65–74), 22% of old–old (ages 75–84), and 50% of oldest-old (ages 85+; Manton, Gu, & Lamb, 2006). Whereas 8% of young–old, 10% of old–old, and 12% of oldest-old experience depressive symptoms (Blazer, Burchett, Service, & George, 1991). Researchers have suggested that disability and depressive symptoms reinforce each other in late life (Bruce, 2001). Difficulties in performing activities of daily living (ADLs), such as shopping for groceries, managing money, dressing, or walking, make it hard to perform social roles and reduce older adults’ sense of mastery. Activity restriction, combined with a decrease in environmental mastery, is associated with increased levels of depressive symptoms among older adults with functional impairments (Williamson & Shaffer, 2000; Yang, 2006). Alternatively, older adults who are unhappy, feel lonely or sad, or think that everything is an effort do not have the energy to prepare regular meals or comply with medical treatments. Lack of good nutrition and failure to follow through with treatments are related to increased levels of disability among depressed older adults (Voils, Steffens, Flint, & Bosworth, 2005). Because disability and depressive symptoms reinforce each other and are both significant risk factors of late-life suicide (Conwell & Brent, 1996; Kaplan et al., 2007), it is critical to find effective interventions to attenuate the vicious cycle.
MOBILIZATION OF INFORMAL CARE
Individuals are embedded in networks of people to whom they provide support and from whom they receive it throughout their lives (Kahn & Antonucci, 1980). As individuals age, their social networks become smaller and are mostly constituted by family members (Barnes et al., 2004; Cornwell, Laumann, & Schumm, 2008). When disability or depressive symptoms prevent them from maintaining their daily routines, most older adults rely on their family members for help (McGarry, 1998; Silverstein, Gans, & Yang, 2006). Prior research has shown that more than three quarters of disabled older adults reside in the community (Manton et al., 2006) and two thirds of them depend on informal care (Spillman & Black, 2005). In addition, between 8% and 16% of community-dwelling older adults experience clinically significant depressive symptoms (Blazer, 2003), and depressed older adults receive significantly more hours of assistance with (instrumental) ADLs than their nondepressed counterparts (Langa, Valenstein, Fendrick, Kabeto, & Vijan, 2004; Morrow-Howell & Proctor, 1998).
PROTECTIVE EFFECT OF INFORMAL CARE
Social support literature has long documented the beneficial effects of informal care. Older adults who receive support are found to engage in more health-promoting behaviors than are older adults who do not (Greenglass et al., 2006; Umberson et al., 2010; Wilcox et al., 1994). Prior research has indicated that informal care increases disabled older adults’ adherence to medical treatments, leading to faster recovery (DiMatteo, 2004). Depressed older adults who have family members care for them and help them with errands, chores, or finances are likely to find more meaning in life, subsequently reducing depressive symptoms (Bosworth, McQuoid, George, & Steffens, 2002; Dew et al., 1997).
Given these well-documented protective effects of social support, other studies, however, suggest that receipt of informal care may have negative consequences (Liang, Krause, & Bennett, 2001). Receipt of informal care may increase disability by reducing older adults’ self-appraisals to perform ADLs (Kuypers & Bengtson, 1973). The lack of regular engagement in activities is also likely to decrease functional skills, leading to more disability (Williamson & Shaffer, 2000). Receipt of informal care may increase depressive symptoms because overreliance on family members decreases older adults’ sense of control, threatens self-esteem, and eventually may lead to depression (Newsom & Schulz, 1998; Wolff & Agree, 2004; Yang, 2006). Moreover, care that is perceived as excessive or unhelpful increases older adults’ depressive symptoms (Martire, Schulz, Wrosch, & Newsom, 2003; Silverstein, Chen, & Heller, 1996). Given the mixed findings in the literature, it is essential to examine the impact of informal care on disability and depressive symptoms over a longer period of time so that we can pinpoint exactly when informal care starts to lose its protective effect.
CHANGES IN THE INTERVENING ROLE OF INFORMAL CARE OVER TIME
Although social support is commonly viewed to attenuate the cycle of disability and depressive symptoms (Penninx, Leveille, Ferrucci, van Eijk, & Guralnik, 1999; Taylor & Lynch, 2004), its attenuating effect may not remain the same because informal care becomes harder to mobilize and its protective effect dissipates over time. As older adults age, their health tends to deteriorate, but the number of family members in the support network that older adults can call upon in times of need dwindles (Barnes et al., 2004). In addition, depressed individuals may lose contact with their social networks because interacting with them tends to be an unpleasant experience (Coyne, 1976). As a result, disabled or depressed older adults are less likely to muster the same amount of informal care from their shrinking social relationships. In addition, receipt of informal care may gradually lose its protective effect. Family members become increasingly strained by carrying out caregiving responsibilities on a day-to-day basis (Pinquart & Sörensen, 2003). Caregiver stress and burnout are likely to increase the frequency and intensity of negative interactions between older adults and their caregivers. These distressing interactions are shown to suppress older adults’ cardiovascular, endocrine, and immune systems, making them susceptible to more illness and disability (Uchino, 2006). These interactions may lead older adults to lose purpose in life and develop more depressive symptoms (Martire, Stephens, Druley, & Wojno, 2002). Past research has examined the associations among disability, depressive symptoms, and informal care; however, no study has yet examined if the mobilization effect of disability and depressive symptoms on informal care and the protective effect of informal care on disability and depressive symptoms remain the same over time. As far as we know, this is the first study to tackle the issue.
PRESENT STUDY
Although prior studies have examined the reciprocal relation between disability and depressive symptoms (Gayman et al., 2008; Ormel et al., 2002), little is known about whether informal care can attenuate the vicious cycle and if so, whether the intervening effect changes over time. The current study addresses this issue by using five waves of panel data and estimating an autoregressive cross-lagged model. With five-wave data, we constructed three cycles of the relations among disability, depressive symptoms, and informal care. Within each cycle, we established the temporal order of the relation from disability (or depressive symptoms) to informal care and from informal care to depressive symptoms (or disability). This approach enabled us to examine whether informal care intervenes in the reciprocal relation between disability and depressive symptoms and whether the intervening effect remains the same across the three cycles. The autoregressive cross-lagged model provides statistical tests on all of these relations.
This study also takes into account covariates that could confound the relations among disability, depressive symptoms, and informal care. These covariates include respondents’ gender, age, educational attainment, race and ethnicity, marital status, self-reported health, income, and number of living children. Past research has shown that disability, depressive symptoms, and informal care are positively associated with female status, age, low education, unmarried status, poor health, and low income (McGarry, 1998; Penninx et al., 1999). Compared with Whites, African Americans have more disabilities, report more depressive symptoms, and are more likely to receive care from family members (Kelley-Moore & Ferraro, 2005; Mendes de Leon, Gold, Glass, Kaplan, & George, 2001). Having more children increases the likelihood of receiving informal care (Checkovich & Stern, 2002).
METHOD
Data used in the analysis come from the HRS, a longitudinal study of nationally representative cohorts of individuals born before 1953 in the United States. This study includes community-dwelling older adults who were aged 65 years or older in 1998 and were still living in the community in 2006. We selected the 1998 wave as the baseline of the study because it includes the most birth cohorts of older adults (born in 1890–1947) who have been reinterviewed in more than three waves. Response rates for the initial interviews of each cohort are between 70% and 82%, and the reinterview response rates are above 90% in each wave (for detailed information on the study design, see http://hrsonline.isr.umich.edu). In total, five waves of data (1998, 2000, 2002, 2004, and 2006), spanning eight years, were examined in the study. The 2008 wave of the HRS data were not yet available at the time of analysis, thus we did not include the last wave.
In 1998, 11,717 respondents aged 65 years or older resided in the community. Between 1998 and 2006, 4,260 respondents died, 544 were lost to follow-up, and 459 moved into nursing homes. Older adults who died and who were lost to follow-up during the study period were excluded to avoid comparing different samples across waves. In addition, moving into nursing homes may reduce the need for informal care, thus institutionalized respondents were also excluded from the analysis. In total, the analysis included 6,454 older adults.
Measures
Respondents were asked whether they had difficulty performing ADLs (i.e., dressing, walking across a room, bathing, eating, getting in or out of bed, and using the toilet) or instrumental activities of daily living (IADLs; i.e., preparing a hot meal, shopping for groceries, making phone calls, taking medications, and managing money) for more than three months as a result of a health or memory problem. The response categories for each of these activities were “yes” versus “no.” The internal reliability coefficient for all 11 items ranged from .80 to .87 across waves. The numbers of difficulties with ADLs and IADLs were summed together in the analysis (Spector & Fleishman, 1998).
Depressive symptoms were measured as the sum of nine symptoms that respondents reported experiencing (yes vs. no) during the week prior to the interview date, including feeling depressed, feeling that everything was an effort, having restless sleep, being unhappy, feeling lonely, not enjoying life, feeling sad, being unable to get going, and not having a lot of energy. The internal reliability coefficient for all nine items ranged from .74 to .76 across waves.
Respondents were asked whether they received ADL or IADL help and if so, who helped. The current analysis combined different sources of unpaid care for two reasons. First, a preliminary analysis suggested only small differences in the patterns of disability, depressive symptoms, and informal care across various sources of care (results not shown but available upon request). Second, prior studies often categorized multiple sources of informal care together (e.g., Liang et al., 2001; Taylor & Lynch, 2004). Using a combined measure makes the current study comparable to past studies. Informal care was measured as a dichotomous variable, with 1 indicating receipt of any unpaid care and 0 otherwise.
Other covariates could confound the findings and thus were taken into consideration in the analysis. These covariates comprise respondents’ gender, age (in years), educational attainment (in years), race and ethnicity (Whites, African Americans, Hispanics, and other races), marital status (married, widowed, divorced, and never-married), self-reported health, income, and the number of living children. To simplify the analysis, all characteristics were measured in 1998. Information was missing in some respondents’ reports, including disability (5%–9%), depressive symptoms (11%–16%), informal care (5%–9%), education (0.1%), marital status (5%), self-reported health (5%), income (5%), and the number of living children (5%). Missing data were imputed using the univariate imputation procedure in Stata (Royston, 2004, 2005). In this procedure, the missing value for a single variable is imputed as a function of other covariates in the analysis.
Analytic Strategy
This study advances prior research by taking a novel approach to examining the associations among disability, depressive symptoms, and informal care. First, we estimated an autoregressive cross-lagged model using five waves of panel data. Second, using all five time points, we delineated three feedback cycles (with each cycle spanning over three time points) among disability, depressive symptoms, and informal care. Within each cycle, we established the temporal order of disability, informal care, and depressive symptoms. Estimates obtained from each cycle tell us whether informal care can be mobilized by and reduce disability and depressive symptoms. Finally, we compared the estimates across three cycles to examine if the mobilization of informal care and its protective effect were similar over time.
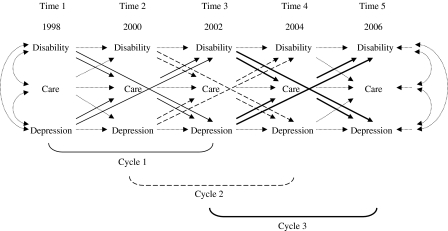
The model shown in Figure 1 conveys the relations among disability, depressive symptoms, and informal care across five time points, reflecting five sets of associations. First are the autoregressive effects of disability, depressive symptoms, and informal care on their respective measures at later times, which depict the changing levels of stability for each construct. It is important to take autoregressive effects into account; otherwise, estimates of cross-lagged effects (discussed in the following) are likely to be biased (Gollob & Reichardt, 1991). Second are the cross-lagged effects of disability on informal care, informal care on disability, depressive symptoms on informal care, and informal care on depressive symptoms between two adjacent time points. These cross-lagged effects indicate how informal care is mobilized by and protects against disability and depressive symptoms, net of autoregressive effects. Third are the direct effects from disability to depressive symptoms and from depressive symptoms to disability. These effects represent the impact of disability on depressive symptoms after controlling for autoregressive and cross-lagged effects. Fourth are concurrent associations among disability, depressive symptoms, and informal care at each wave. These associations reveal the correlations among these constructs that are not attributable to disability, depressive symptoms, and informal care measured at prior waves and control variables. Last are regression effects of disability, depressive symptoms, and informal care on control variables at each wave, intended to take into account respondents’ characteristics that may confound the associations among disability, depressive symptoms, and informal care. To simplify the presentation in Figure 1, higher order autoregressive effects, concurrent associations in 2000, 2002, and 2004, and regression effects are not shown.
Figure 1.
Associations among disability, depressive symptoms, and informal care. Note. To simplify the presentation, concurrent associations in 2000, 2002, and 2004, higher order autoregressive effects, and control variables are not shown. The five time points can be divided into three cycles: Time 1-2-3 (Cycle 1, solid lines), Time 2-3-4 (Cycle 2, dashed lines), and Time 3-4-5 (Cycle 3, bolded lines). Dotted lines are used to indicate concurrent associations in 1998 and 2006, autoregressive effects, and the cross-lagged effects that are estimated in the model but not shown as part of the three cycles in Figure 2.
These five time points can be divided into three cycles: Time 1-2-3 (Cycle 1, solid lines), Time 2-3-4 (Cycle 2, dashed lines), and Time 3-4-5 (Cycle 3, bolded lines). Within each cycle, the examination of the cross-lagged effects tells us whether informal care is mobilized by disability and depressive symptoms and whether informal support, once mobilized, can reduce the progression of disability and depressive symptoms. In addition, comparing cross-lagged effects shows whether informal care has the same attenuating effect on the relation between disability and depressive symptoms across these three cycles.
We first fitted the model that includes all hypothesized relations (Model 1) and then constrained nonsignificant effects to be zero through four steps. First, we established the associations among disability, depressive symptoms, and informal care, net of the influence of potential confounding factors by setting nonsignificant regression effects to zero (Model 2). Second, to better capture the stability of disability, depressive symptoms, and informal care, we fixed nonsignificant autoregressive effects (i.e., lagged for two, four, six, and eight years) at zero (Model 3). After imposing these constraints, a construct that has a significant effect that is lagged for a longer period indicates a greater long-term effect. Third, we examined whether informal care intervenes in the association between disability and depressive symptoms by constraining nonsignificant cross-lagged effects of disability on informal care, informal care on disability, depressive symptoms on informal care, and informal care on depressive symptoms between two adjacent time points (Model 4). Last, we set nonsignificant direct effects from disability to depressive symptoms and from depressive symptoms to disability in each cycle to zero (Model 5). Because all concurrent associations among disability, depressive symptoms, and informal care differ significantly from zero, no constraints were placed on these associations. In each step, we compared model fits between a more restricted model and a less restricted model and tested whether a more restricted model worsened the model fit (i.e., p < .05).
The analysis was performed using the statistical package Mplus Version 5.21 (Muthén & Muthén, 2009). Because both disability and depressive symptoms are continuous variables truncated at 0 and a considerable proportion of respondents reported no disability or depressive symptoms, a Tobit regression was used. In addition, because informal care is a dichotomous variable, a logistic regression was used. Of the 6,454 respondents, 2,464 were couples. Thus, Huber–White sandwich estimators (Johnston & DiNardo, 1997) were used to correct standard errors of the coefficients in the presence of clustering. Because the study uses a large sample size, a model is considered to fit the data well when a comparative fit index is greater than 0.95, a Tucker–Lewis index is greater than 0.95, and a root mean square error of approximation is less than 0.06 (Hu & Bentler, 1999).
RESULTS
Respondents’ characteristics are shown in Table 1. Overall, respondents reported relatively good health at baseline. The average number of limitations increased from 0.36 to 1.11 during the 1998–2006 period (p < .001). At the same time, the mean number of depressive symptoms increased from 1.81 to 2.14 (p < .001). During the same period, the proportions of respondents receiving informal care increased from 7.96% to 22.98% (p < .001). The sample consists of more women than men. The average age was about 72 years old in 1998. The mean number of schooling years was slightly below 12. Four of five respondents were White, 12% were African American, 7% were Hispanic, and 1% belonged to other races. Two thirds of the respondents were married, one quarter was widowed, 7% were divorced, and 2% were never-married in 1998. On average, these respondents had three children and an income of $42,033.
Table 1.
Descriptive Statistics for Variables Included in the Analysis (N = 6,454)
| 1998 | 2000 | 2002 | 2004 | 2006 | |
| Disability (0–11) | 0.36 | 0.42 | 0.53 | 0.69 | 1.11 |
| Depressive symptoms (0–9) | 1.81 | 1.86 | 1.91 | 1.97 | 2.14 |
| Receipt of informal care (%) | 7.96 | 8.61 | 11.65 | 16.19 | 22.98 |
| Control variables | |||||
| Gender (%) | |||||
| Women (reference group) | 58.71 | ||||
| Men | 41.29 | ||||
| Age (65–98) | 72.24 | ||||
| Education (0–17) | 11.78 | ||||
| Race/ethnicity (%) | |||||
| White (reference group) | 79.39 | ||||
| African American | 11.67 | ||||
| Hispanic | 7.47 | ||||
| Other races | 1.47 | ||||
| Marital status (%) | |||||
| Married (reference group) | 65.80 | ||||
| Widowed | 24.28 | ||||
| Divorced | 7.42 | ||||
| Never-married | 2.49 | ||||
| Health (1 = poor to 5 = excellent) | 3.22 | ||||
| Income | 42,033.87 | ||||
| Number of children | 3.27 | ||||
Note: Missing data were imputed for the following variables: disability (5%, 6%, 7%, 9%, and 9% for 1998, 2000, 2002, 2004, and 2006, respectively), depressive symptoms (11%, 12%, 15%, 16%, and 16% for 1998, 2000, 2002, 2004, and 2006, respectively), informal care (5%, 6%, 7%, 8%, 9% for 1998, 2000, 2002, 2004, and 2006, respectively), education (0.1%), marital status (5%), self-reported health status (5%), income (5%), and the number of living children (5%).
As presented in Table 2, we started with the full model that includes all hypothesized relations (Model 1). Following the model-trimming approach, the full model was reduced by subsequently constraining the following nonsignificant effects to be zero: regression effects (Model 2), autoregressive effects (Model 3), cross-lagged effects (Model 4), and direct effects (Model 5). Table 2 also shows fit statistics of each model, as well as whether the model-trimming approach produces models that fit the data. Our final model (Model 5) meets the criteria suggested by Hu and Bentler (1999) for a well-fitting model, with a comparative fit index of 0.996, a Tucker–Lewis index of 0.993, and a root mean square error of approximation of 0.012 (χ2 = 247.558, df = 128, p < .001). Based on this model-trimming approach, Model 5 is the most parsimonious model and can fit the data reasonably well.
Table 2.
Model Comparison (N = 6,454)
| Model fit statistics | Comparisona | p Value | |
| (1) Full model | χ2 = 242.589, df = 38, p = .000; CFI = 0.994, TLI = 0.958, RMSEA = 0.029 | ||
| (2) + Constrain nonsignificant regression effects = 0 | χ2 = 239.311, df = 117, p = .000; CFI = 0.996, TLI = 0.992, RMSEA = 0.013 | (1) vs. (2) | .56 |
| (3) + Constrain nonsignificant autoregressive effects = 0 | χ2 = 244.363, df = 121, p = .000; CFI = 0.996, TLI = 0.992, RMSEA = 0.013 | (2) vs. (3) | .33 |
| (4) + Constrain nonsignificant cross-lagged effects = 0 | χ2 = 246.790, df = 127, p = .000; CFI = 0.996, TLI = 0.993, RMSEA = 0.012 | (3) vs. (4) | .87 |
| (5) + Constrain nonsignificant direct effects = 0 | χ2 = 247.558, df = 128, p = .000; CFI = 0.996, TLI = 0.993, RMSEA = 0.012 | (4) vs. (5) | .47 |
Notes: CFI = comparative fit index; RMSEA = root mean square error of approximation; TLI = Tucker–Lewis index.
The model fit was evaluated with the weighted least square parameter estimates using a diagonal weight matrix with robust standard errors and mean- and variance-adjusted chi-square test statistics (WLSMV). Thus, chi-square values cannot be used directly for the difference test between two nested models. Instead, the difference tests were conducted using the DIFFTEST command in Mplus to take into account the mean- and variance-adjusted chi-square provided by the WLSMV estimation (Asparouhov & Muthén, 2006).
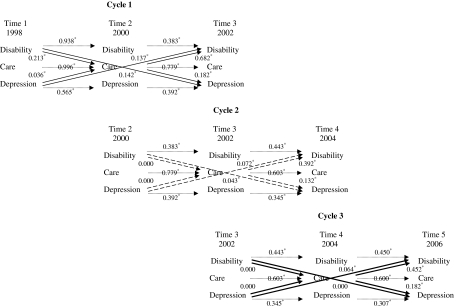
Figure 2 shows the final results from Model 5 in three cycles. The results indicate that disability, depressive symptoms, and informal care were all significant predictors of their respective measures two years later in each cycle. When autoregressive effects were examined for more than two years (i.e., higher order autoregressive effects), baseline depressive symptoms predicted depressive symptoms eight years later, baseline disability predicted disability six years later, and informal care only predicted informal care four years later (results not shown). These findings suggest that older adults’ depressive symptoms had the strongest long-term stability.
Figure 2.
Three cycles of disability, depressive symptoms, and informal care (based on Model 5). *p < .05.
In addition, in the first feedback cycle (1998–2000–2002, solid lines), disability and depressive symptoms in 1998 mobilized informal care in 2000 (i.e., coefficients are .213 and .036, respectively) and mobilized informal care increased disability (.682) and depressive symptoms (.182) in 2002. In the second cycle (2000–2002–2004, dashed lines), disability and depressive symptoms in 2000 no longer mobilized informal care in 2002 (i.e., both coefficients are 0) but informal care in 2002 continued to increase disability (.392) and depressive symptoms (.132) in 2004. In the last cycle (2002–2004–2006, bolded lines), disability and depressive symptoms in 2002 still did not mobilize informal care in 2004 (i.e., both coefficients are 0) and informal care in 2004 sustained its positive effect on disability (.452) and depressive symptoms (.182) in 2006. These findings indicate that older adults’ disability and depressive symptoms mobilized informal care in the first cycle, but the increases in disability and depressive symptoms no longer triggered additional informal care in subsequent cycles. Moreover, in all three cycles, receipt of informal care increased rather than reduced older adults’ disability and depressive symptoms, and the effects remained the same across three cycles (p > .05 for equality constraints). Therefore, consistent with the negative effects of social support in the literature, informal care does not attenuate the feedback cycle of disability and depressive symptoms.
Figure 2 also illustrates direct effects from disability to depressive symptoms and from depressive symptoms to disability across three cycles. After taking control variables, concurrent associations, autoregressive effects, and cross-lagged effects into consideration, disability had a positive direct effect on depressive symptoms only in the first (0.142) and second (0.043) cycles and the magnitudes of the direct effects diminished over time (p < .05). Conversely, depressive symptoms had a positive direct effect on disability for Cycles 1 through 3 (0.137, 0.072, and 0.064, respectively) and the magnitude of the direct effect decreased between the first and second cycles (p < .05) but remained about the same between the second and third cycles (p > .05). These findings suggest that informal care does not fully account for the reciprocal relations between disability and depressive symptoms.
Although the results on concurrent associations and the result on the relations between control variables and disability/depressive symptoms/informal care are not shown in Figure 2, their findings are summarized in the following: Disability, depressive symptoms, and informal care were all positively related at each wave. In addition, because all control variables were measured in 1998 and their causal order with disability, depressive symptoms, and informal care at baseline cannot be determined, their relations in 1998 were modeled as correlations. For 2000, 2002, 2004, and 2006, the effects of control variables on disability, depressive symptoms, and informal care were estimated as regression coefficients. Of 36 possible associations at each wave (=12 covariates × 3 key constructs [disability, depressive symptoms, and informal care]), 29, 16, 11, 8, and 11 reached statistical significance in 1998, 2000, 2002, 2004, and 2006, respectively. Three variables remained statistically significant across waves. Age was always positively related to disability and informal care. Men and older adults with better health consistently reported fewer depressive symptoms than their respective counterparts. These findings indicate that only a few of these covariates had enduring associations with disability, depressive symptoms, and informal care over time.
DISCUSSION
This study advances prior research both theoretically and methodologically. We incorporated social support literature to examine whether informal care can attenuate the reciprocal relation between disability and depressive symptoms and if so, whether the intervening effect changes over time. Prior studies have inspected how social support mediates the effect of disability on depressive symptoms (Taylor & Lynch, 2004) or how social support mediates the effect of depressive symptoms on disability (Penninx et al., 1999). However, if informal care is to have an attenuating effect on the reciprocal relation between disability and depressive symptoms, it is essential to consider both directions at the same time. Moreover, using five waves of panel data, we established the temporal order of disability, informal care, and depressive symptoms. Thus, we could determine whether disability and depressive symptoms mobilize informal care and whether informal care reduces disability and depressive symptoms. Finally, by examining whether informal care’s intervening effect changes across three cycles, we were able to examine whether the patterns in which informal care is mobilized by and reduces disability and depressive symptoms remain the same over time.
We found that older adults’ disability and depressive symptoms mobilized informal care in the first cycle only, suggesting that additional increases in disability and depressive symptoms at subsequent cycles do not trigger more care. This finding corresponds to prior literature indicating that individuals find it harder to mobilize social support as they age (Barnes et al., 2004). We also found that receipt of informal care did not bring about protective effects. Instead, informal care facilitated the progression of disability and depressive symptoms in all three cycles, and the detrimental effects persisted over time. Several reasons may explain why receipt of informal care has negative consequences for older adults. First, informal care may increase disability because receipt of help reduces disabled older adults’ self-appraisals to perform ADLs, and the lack of regular engagement in activities decreases their functional skills (Kuypers & Bengtson, 1973; Williamson & Shaffer, 2000). Second, informal care may increase depressive symptoms because overreliance on family members or care that is perceived as excessive or unhelpful decreases older adults’ sense of control, threatens self-esteem, and eventually leads to depression (Newsom & Schulz, 1998; Silverstein et al., 1996; Yang, 2006). Last, informal care may increase both disability and depressive symptoms because negative interactions between older adults and caregivers weaken older adults’ immune systems and reduce their motivation to regain their health, leading to further aggravation of disability and depressive symptoms (Martire et al., 2002; Uchino, 2006).
Several limitations need to be considered when interpreting the results. First, the analytic sample included only those who were surviving and living in the community over the eight-year period. Thus, we can compare the same older adults under similar living environments across waves. This selection, however, excluded older adults who participated in the earlier waves of the study but passed away, were lost to follow-up, or moved into nursing homes at later waves. Because these older adults often have more disabilities or depressive symptoms and thus are in greater need of care than those who remained alive, locatable, and community dwelling throughout the study period (Ormel et al., 2002), excluding the former older adults tends to underestimate the levels of disability, depressive symptoms, and informal care. Consequently, the estimated attenuating effect of informal care on the relation between disability and depressive symptoms may be biased downward.
Second, informal care also could have been mobilized by other factors, such as older adults’ cognitive limitations and illnesses. These factors were not accounted for in the analysis because including one additional factor would have significantly increased the complexity of the analytic model. Third, because informal care was measured as a dichotomous variable, this study did not examine the extent to which the quantity and quality of care attenuated the reciprocal relation between disability and depressive symptoms. These nuances should be considered more closely in future research. Fourth, because HRS respondents were reinterviewed every other year, the study contains an equal interval of two years across waves. Previous studies have suggested that the effect of disability on depressive symptoms may be more immediate than the effect of depressive symptoms on disability (Ormel et al., 2002) and that the rate of health deterioration is likely to accelerate among the oldest-old. Thus, a two-year interval may be too long a time period to detect informal care’s protective effect. Future studies using shorter intervals between waves may help researchers better capture the critical periods for effective interventions, particularly for older adults in advanced age. Last, as a first step toward understanding the intervening effect of informal care on the relation between disability and depressive symptoms, this study treated control variables as time-invariant measures to simplify the analysis. Some of these control variables, however, are likely to change over time. In future research, it is important to examine how changes in these control variables may modify the relations among disability, depressive symptoms, and informal care.
The findings that disability and depressive symptoms do not consistently mobilize informal care have important implications for future research and social policy. When informal care can no longer be mobilized because of sustained or increased levels of disability and depressive symptoms, depressed or disabled older adults must utilize formal care. A recent study shows that living in a state supportive of home and community-based services was associated with lower depression among older adults with severe functional limitations compared with older adults with few or no limitations (Muramatsu, Yin, & Hedeker, 2010). Therefore, more research is needed to understand what aspects of formal services decrease disabled older adults’ depressive symptoms and how using formal services can help reduce the negative consequences of informal care for older adults’ well-being. Also, policy makers should make formal services more readily available to families with disabled or depressed older adults.
In addition, the finding that informal care increases rather than decreases older adults’ disability and depressive symptoms suggests several important research directions. Specifically, it is vital to explore factors, other than informal care, that mediate the cycle between disability and depressive symptoms, and such findings may hint at new interventions that might attenuate the cycle. Moreover, this study followed older adults for eight years. As HRS is a continuing data collection project, it is necessary to reexamine these older adults when new follow-up data become available for a better understanding of the long-term relations among disability, depressive symptoms, and informal care. Furthermore, race, gender, and social class have been found to be related with differential levels of disability, depressive symptoms, and informal care. It is important to examine whether and how these social variables differ in the intervening effect of informal care on disability and depressive symptoms. These research directions can help policy makers better tailor services to disabled or depressed older adult and their caregivers. Until these findings are available, policy makers need to ensure that older adults learn that relying on family members for care is appropriate during late life, and they should be encouraged to accept help when they need it. In addition, enhancing clear communication between older adults and their caregivers is likely to reduce negative interactions, consequently reducing the negative effect of informal care on older adults’ well-being.
FUNDING
This research was supported by a Faculty Development Award to I-Fen Lin from the Center for Family and Demographic Research at Bowling Green State University, which receives core funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R24-HD050959).
Acknowledgments
Previous versions of this article were presented at the Annual Meeting of the Population Association of America, Dallas, Texas, April 15–17, 2010; and at the Institute of Sociology, Academia Sinica, Taipei, Taiwan, May 27, 2010. The authors thank Linda Waite, the editor, and three anonymous reviewers for their helpful comments; and Lesley Wadsworth for editorial suggestions. Any opinions expressed here are solely those of the authors and not of the funding agency or center.
References
- Asparouhov T, Muthén B. Robust chi square difference testing with mean and variance adjusted test statistics. 2006. (Mplus Web Note: No. 10). Retrieved from http://statmodel.com/download/webnotes/webnote10.pdf. [Google Scholar]
- Barnes LL, Mendes de Leon CF, Bienias JL, Evans DA. A longitudinal study of black-white differences in social resources. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2004;59:146–153. doi: 10.1093/geronb/59.3.s146. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Social Science & Medicine. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. doi:10.1016/S0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Blazer D. Depression in late life: Review and commentary. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences. 2003;58:249–265. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- Blazer D, Burchett B, Service C, George LK. The association of age and depression among the elderly: An epidemiologic exploration. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences. 1991;46:210–215. doi: 10.1093/geronj/46.6.m210. [DOI] [PubMed] [Google Scholar]
- Bosworth HB, McQuoid DR, George LK, Steffens DC. Time-to-remission from geriatric depression: Psychosocial and clinical factors. American Journal of Geriatric Psychiatry. 2002;10:551–559. doi:10.1176/appi.ajgp.10.5.551. [PubMed] [Google Scholar]
- Bruce ML. Depression and disability in late life: Directions for future research. American Journal of Geriatric Psychiatry. 2001;9:102–112. doi:10.1176/appi.ajgp.9.2.102. [PubMed] [Google Scholar]
- Bruce ML, Seeman TE, Merrill SS, Blazer DG. The impact of depressive symptomatology on physical disability: MacArthur studies of successful aging. American Journal of Public Health. 1994;84:1796–1799. doi: 10.2105/ajph.84.11.1796. doi:10.2105/AJPH.84.11.1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Checkovich TJ, Stern S. Shared caregiving responsibilities of adult siblings with elderly parents. The Journal of Human Resources. 2002;37:441–478. doi:10.2307/3069678. [Google Scholar]
- Conwell Y, Brent D. Suicide and aging I: Patterns of psychiatric diagnosis. In: Pearson JL, Conwell Y, editors. Suicide and aging: International perspective. New York, NY: Springer; 1996. pp. 15–30. [Google Scholar]
- Cornwell B, Laumann EO, Schumm LP. The social connectedness of older adults: A national profile. American Sociological Review. 2008;73:185–203. doi: 10.1177/000312240807300201. doi:10.1177/000312240807300201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyne JC. Depression and the response of others. Journal of Abnormal Psychology. 1976;85:186–193. doi: 10.1037//0021-843x.85.2.186. doi:10.1037//0021-843X.85.2.186. [DOI] [PubMed] [Google Scholar]
- Dew MA, Reynolds CF, III, Houck PR, Hall M, Buysse DJ, Frank E, Kupfer DJ. Temporal profiles of the course of depression during treatment: Predictors of pathways toward recovery in the elderly. Archives of General Psychiatry. 1997;54:1016–1024. doi: 10.1001/archpsyc.1997.01830230050007. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR. Social support and patient adherence to medical treatment: A meta-analysis. Health Psychology. 2004;23:207–218. doi: 10.1037/0278-6133.23.2.207. doi:10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- Gayman MD, Turner RJ, Cui M. Physical limitations and depressive symptoms: Exploring the nature of the association. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2008;63:219–228. doi: 10.1093/geronb/63.4.s219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geerlings SW, Beekman ATF, Deeg DJH, van Tilburg W. Physical health and the onset and persistence of depression in older adults: An eight-wave prospective community-based study. Psychological Medicine. 2000;30:369–380. doi: 10.1017/s0033291799001890. doi:10.1017/S0033291799001890. [DOI] [PubMed] [Google Scholar]
- Gollob HF, Reichardt CS. Interpreting and estimating indirect effects assuming time lags really matter. In: Collins LM, Horn JL, editors. Best methods for the analysis of change: Recent advances, unanswered questions, future directions. Washington, DC: American Psychological Association; 1991. pp. 243–259. doi:10.1037/10099-015. [Google Scholar]
- Greenglass E, Fiksenbaum L, Eaton J. The relationship between coping, social support, functional disability and depression in the elderly. Anxiety, Stress, and Coping. 2006;19:15–31. doi:10.1080/14659890500436430. [Google Scholar]
- Hu L-T, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. doi:10.1080/10705519909540118. [Google Scholar]
- Johnston J, DiNardo J. Econometric methods. 4th ed. New York, NY: McGraw-Hill; 1997. [Google Scholar]
- Kahn RL, Antonucci TC. Convoys over the life course: Attachment, roles, and social support. In: Baltes PB, Brim OG Jr, editors. Life-span development and behavior. New York, NY: Academic Press; 1980. pp. 253–286. [Google Scholar]
- Kaplan MS, McFarland BH, Huguet N, Newsom JT. Physical illness, functional limitations, and suicide risk: A population-based study. American Journal of Orthopsychiatry. 2007;77:56–60. doi: 10.1037/0002-9432.77.1.56. doi:10.1037/0002-9432.77.1.56. [DOI] [PubMed] [Google Scholar]
- Kelley-Moore JA, Ferraro KF. A 3-D model of health decline: Disease, disability, and depression among black and white older adults. Journal of Health and Social Behavior. 2005;46:376–391. doi: 10.1177/002214650504600405. doi:10.1177/002214650504600405. [DOI] [PubMed] [Google Scholar]
- Kuypers JA, Bengtson VL. Social breakdown and competence: A model of normal aging. Human Development. 1973;16:181–201. doi: 10.1159/000271275. doi:10.1159/000271275. [DOI] [PubMed] [Google Scholar]
- Langa KM, Valenstein MA, Fendrick AM, Kabeto MU, Vijan S. Extent and cost of informal caregiving for older Americans with symptoms of depression. American Journal of Psychiatry. 2004;161:857–863. doi: 10.1176/appi.ajp.161.5.857. doi:10.1176/appi.ajp.161.5.857. [DOI] [PubMed] [Google Scholar]
- Lenze EJ, Schulz R, Martire LM, Zdaniuk B, Glass T, Kop WJ, Reynolds CF. The course of functional decline in older people with persistently elevated depressive symptoms: Longitudinal findings from the cardiovascular health study. Journal of the American Geriatrics Society. 2005;53:569–575. doi: 10.1111/j.1532-5415.2005.53202.x. doi:10.1111/j.1532-5415.2005.53202.x. [DOI] [PubMed] [Google Scholar]
- Liang J, Krause NM, Bennett JM. Social exchange and well-being: Is giving better than receiving? Psychology and Aging. 2001;16:511–523. doi: 10.1037//0882-7974.16.3.511. doi:10.1037//0882-7974.16.3.511. [DOI] [PubMed] [Google Scholar]
- Manton KG, Gu X, Lamb VL. Change in chronic disability from 1982 to 2004/2005 as measured by long-term changes in function and health in the U.S. elderly population. Proceedings of the National Academy of Sciences of the United States of America. 2006;103:18374–18379. doi: 10.1073/pnas.0608483103. doi:10.1073/pnas.0608483103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martire LM, Schulz R, Wrosch C, Newsom JT. Perceptions and implications of received spousal care: Evidence from the caregiver health effects study. Psychology and Aging. 2003;18:593–601. doi: 10.1037/0882-7974.18.3.593. doi:10.1037/0882-7974.18.3.593. [DOI] [PubMed] [Google Scholar]
- Martire LM, Stephens MAP, Druley JA, Wojno WC. Negative reactions to received spousal care: Predictors and consequences of miscarried support. Health Psychology. 2002;21:167–176. [PubMed] [Google Scholar]
- McGarry K. Caring for the elderly: The role of adult children. In: Wise DA, editor. Inquiries in the economics of aging. Chicago, IL: The University of Chicago Press; 1998. pp. 133–163. [Google Scholar]
- Mendes de Leon CF, Gold DT, Glass TA, Kaplan L, George LK. Disability as a function of social networks and support in elderly African Americans and whites: The Duke EPESE 1986–1992. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2001;56:179–190. doi: 10.1093/geronb/56.3.s179. [DOI] [PubMed] [Google Scholar]
- Morrow-Howell NL, Proctor EK. Informal caregiving to older adults hospitalized for depression. Aging & Mental Health. 1998;2:222–231. doi: 10.1080/13607860500409963. doi:10.1080/13607869856704. [DOI] [PubMed] [Google Scholar]
- Muramatsu N, Yin H, Hedeker D. Functional declines, social support, and mental health in the elderly: Does living in a state supportive of home and community-based services make a difference? Social Science & Medicine. 2010;70:1050–1058. doi: 10.1016/j.socscimed.2009.12.005. doi:10.1016/j.socscimed.2009.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus: Statistical analysis with latent variables (Version 5.21) Los Angeles, CA: Author; 2009. [Google Scholar]
- Newsom JT, Schulz R. Caregiving from the recipient’s perspective: Negative reactions to being helped. Health Psychology. 1998;17:172–181. doi: 10.1037//0278-6133.17.2.172. doi:10.1037/0278-6133.17.2.172. [DOI] [PubMed] [Google Scholar]
- Ormel J, Rijsdijk FV, Sullivan M, van Sonderen E, Kempen GIJM. Temporal and reciprocal relationship between IADL/ADL disability and depressive symptoms in late life. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2002;57:338–347. doi: 10.1093/geronb/57.4.p338. [DOI] [PubMed] [Google Scholar]
- Penninx BWJH, Leveille S, Ferrucci L, van Eijk JTM, Guralnik JM. Exploring the effect of depression on physical disability: Longitudinal evidence from the established populations for epidemiologic studies of the elderly. American Journal of Public Health. 1999;89:1346–1352. doi: 10.2105/ajph.89.9.1346. doi:10.2105/AJPH.89.9.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: A meta-analysis. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2003;58:112–128. doi: 10.1093/geronb/58.2.p112. [DOI] [PubMed] [Google Scholar]
- Royston P. Multiple imputation of missing values. The Stata Journal. 2004;4:227–241. [Google Scholar]
- Royston P. Multiple imputation of missing values: Update. The Stata Journal. 2005;5:188–201. [Google Scholar]
- Silverstein M, Chen X, Heller K. Too much of a good thing? Intergenerational social support and the psychological well-being of older parents. Journal of Marriage and the Family. 1996;58:970–982. doi:10.2307/353984. [Google Scholar]
- Silverstein M, Gans D, Yang FM. Intergenerational support to aging parents: The role of norms and needs. Journal of Family Issues. 2006;27:1068–1084. doi:10.1177/0192513X06288120. [Google Scholar]
- Spector WD, Fleishman JA. Combining activities of daily living with instrumental activities of daily living to measure functional disability. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 1998;53:46–57. doi: 10.1093/geronb/53b.1.s46. [DOI] [PubMed] [Google Scholar]
- Spillman BC, Black KJ. Staying the course: Trends in family caregiving. 2005. (AARP Public Policy Institute Issue Paper Series 2005–17). Retrieved from http://assets.aarp.org/rgcenter/il/2005_17_caregiving.pdf. [Google Scholar]
- Taylor MG, Lynch SM. Trajectories of impairment, social support, and depressive symptoms in later life. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2004;59:238–246. doi: 10.1093/geronb/59.4.s238. [DOI] [PubMed] [Google Scholar]
- Uchino BN. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine. 2006;29:377–387. doi: 10.1007/s10865-006-9056-5. doi:10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- Umberson D, Crosnoe R, Reczek C. Social relationships and health behavior across the life course. Annual Review of Sociology. 2010;36:139–157. doi: 10.1146/annurev-soc-070308-120011. doi:10.1146/annurev-soc-070308-120011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voils CI, Steffens DC, Flint EP, Bosworth HB. Social support and locus of control as predictors of adherence to antidepressant medication in an elderly population. American Journal of Geriatric Psychiatry. 2005;13:157–165. doi: 10.1176/appi.ajgp.13.2.157. doi:10.1097/00019442-200502000-00010. [DOI] [PubMed] [Google Scholar]
- Wilcox VL, Kasl SV, Berkman LF. Social support and physical disability in older people after hospitalization: A prospective study. Health Psychology. 1994;13:170–179. doi: 10.1037//0278-6133.13.2.170. doi:10.1037//0278-6133.13.2.170. [DOI] [PubMed] [Google Scholar]
- Williamson GM, Shaffer DR. The activity restriction model of depressed affect: Antecedents and consequences of restricted normal activities. In: Williamson GM, Shaffer DR, Parmelee PA, editors. Physical illness and depression in older adults: A handbook of theory, research, and practice. New York, NY: Kluwer Academic/Plenum; 2000. pp. 173–200. [Google Scholar]
- Wolff JL, Agree EM. Depression among recipients of informal care: The effects of reciprocity, respect, and adequacy of support. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2004;59:173–180. doi: 10.1093/geronb/59.3.s173. [DOI] [PubMed] [Google Scholar]
- Yang Y. How does functional disability affect depressive symptoms in late life? The role of perceived social support and psychological resources. Journal of Health and Social Behavior. 2006;47:355–372. doi: 10.1177/002214650604700404. doi:10.1177/002214650604700404. [DOI] [PubMed] [Google Scholar]
- Zeiss AM, Lewinsohn PM, Rohde P, Seeley JR. Relationship of physical disease and functional impairment to depression in older people. Psychology and Aging. 1996;11:572–581. doi: 10.1037//0882-7974.11.4.572. doi:10.1037//0882-7974.11.4.572. [DOI] [PubMed] [Google Scholar]