Abstract
Stressors of different psychological, physical or immune origin play a critical role in the pathophysiology of irritable bowel syndrome participating in symptoms onset, clinical presentation as well as treatment outcome. Experimental stress models applying a variety of acute and chronic exteroceptive or interoceptive stressors have been developed to target different periods throughout the lifespan of animals to assess the vulnerability, the trigger and perpetuating factors determining stress influence on visceral sensitivity and interactions within the brain-gut axis. Recent evidence points towards adequate construct and face validity of experimental models developed with respect to animals' age, sex, strain differences and specific methodological aspects such as non-invasive monitoring of visceromotor response to colorectal distension as being essential in successful identification and evaluation of novel therapeutic targets aimed at reducing stress-related alterations in visceral sensitivity. Underlying mechanisms of stress-induced modulation of visceral pain involve a combination of peripheral, spinal and supraspinal sensitization based on the nature of the stressors and dysregulation of descending pathways that modulate nociceptive transmission or stress-related analgesic response.
Keywords: Irritable bowel syndrome; Models, animal; Pain
Introduction
Alterations of visceral sensation such as enhanced perception of physiological or experimental visceral stimuli along with hypervigilance to those, are at the origin of visceral hypersensitivity, a phenomenon commonly considered to play a major role in the pathophysiology of irritable bowel syndrome (IBS).1-7 Epidemiological studies have implicated stress of psychosocial, physical or immune origin as a trigger of first onset or exacerbation of IBS symptoms.8-10 Early adverse life events in the form of emotional, sexual, or physical abuse are major predisposing factors for the development of IBS later in life.11,12 Childhood trauma, especially in genetically predisposed individuals, is thought to induce persistent changes in the brain arousal response system that impacts on the neuroendocrine hypothalamic-pituitary-adrenal (HPA) axis.12 In adult IBS patients, acute stress episodes, chronic social stress, anxiety disorders, and maladaptive coping style determine the illness experience, health care-seeking behavior as well as treatment outcome.12,13 Stress-related psychosocial factors such as somatization, neuroticism, and hypochondriasis are also important predictors in the development of post-infectious IBS.14,15 Emotional or physical stressors may cause disturbances at every levels of the brain-gut axis including the central, autonomic and enteric nervous systems and affect regulation of visceral perception and emotional response to visceral events.16
Over the past 15 years, various animal models have been developed to get insight into the underlying mechanisms of visceral hypersensitivity and the influence of stress on visceral pain pathways.1,17-20 While in humans the evaluation of visceral sensitivity is predominantly based on the conscious perception to gut distension, the measurement of this subjective response cannot be performed in animal studies. Objective evaluation of responses to visceral stimulation in clinical studies includes the assessment of reflex activity (eg, a somatic nociceptive cutaneo-muscular flexion reflex can be inhibited by painful visceral stimulation) or evoked central processes (eg, changes in activation of the anterior cingulated cortex involved in pain inhibition).21,22 Indeed, during the last decade functional imaging techniques have been applied successfully to examine the human brain response to noxious visceral stimuli.23 In experimental animals, the pattern of brain and spinal circuitries activated by various stressors and colorectal distension (CRD) under basal or hypersensitive state have been early on mapped in a number of studies using the induction of the Fos protein expression as a direct marker of neuronal cell activation and double immunohistochemical labeling to identify the phenotype of Fos positive spinal and supraspinal neurons.24-31 Recently, preliminary reports applied imaging techniques to get insight into brain circuit activated by visceral stimulation in rodents. Similarity in some regional brain activation induced by CRD have been found when comparing Fos expression and functional magnetic resonance imaging.32 In addition this comparative study indicates that both methods are complementary as Fos immunohistochemistry provides a higher spacial resolution over imaging while imaging displays a higher sensitivity to detect a large number of brain area. Development of imaging in conscious animals with removal of additional stress linked with conditions of functional imaging monitoring will enable bridging the gap between the multidimensional nature of human pain experience and preclinical studies.33
In this review we will outline some of the most relevant preclinical models that have been developed, comment on their contribution to our understanding of stress modulation of visceral pain mechanisms, and assess the clinical relevance of these preclinical studies to unravel potential molecular targets to alleviate visceral pain symptoms in IBS.
Stress Pathways: Corticotropin Releasing Factor Signaling as an End Point Effector
First coined by the endocrinologist Hans Selye, the term "stress" defines the physiological adaptive responses to real or perceived emotional or physical threats ("stressors") to the organism homeostasis.34 When exposed to an acute threatening challenge, the body engages a "fight or flight" response35 driven by sympathetic activation leading to rapid heart rate and respiration, increased arousal, alertness, and inhibition of acutely non adaptive vegetative functions (feeding, digestion, growth and reproduction).34 Concurrently, a negative feedback is activated to terminate the stress response and bring the body back to a state of homeostasis or eustasis,36 that engages neural, neuroendocrine and immune components, a process called allostasis37 or "stability through changes".37,38 However, persistence or chronicity of the stressors can overload this adaptive system which then becomes defective or excessive. The organism is no longer brought back to basal homeostasis leading to a state of allostatic load37,39 or "cacostasis."36 This state lies at the origin of a variety of stress-related diseases that develop in the context of a vulnerable genetic, epigenetic and/or constitutional background.36 The pathogenesis of stress-induced disorders affects the whole body, including the viscera of which the gastrointestinal (GI) tract is a sensitive target.36,40
Over the past decades, important components of the stress-activated pathways whereby the brain translates stimuli into final integrated bodily response have been identified through the characterization of corticotropin releasing factor (CRF) signaling system. This is composed of the 41 amino acid peptide CRF, and related peptides, urocortin 1, urocortin 2 and urocortin 3 along with the CRF receptors CRF1 and CRF2 and their variants which display specific affinity for CRF and related agonists.41 The development of selective CRF receptor antagonists has also largely contributed to delineate the role of activation of CRF receptor subtypes in the stress response.42,43 In particular convergent reports indicate that the activation of CRF1 receptor underlies the multiple faceted components of the stress response.40,44,45 CRF/CRF1 signaling plays a primary neuroendocrine role in stimulating the HPA axis leading to the release of adrenocorticotropic hormone and corticosterone in rodents and cortisol in humans.43,46 In addition the CRF signaling system also acts as a neurotransmitter/neuromodulator to coordinate the behavioral, immune, and visceral efferent limbs of the stress response.44,45,47-49 It does so via the activation of the locus coeruleus and its noradrenergic projections to the forebrain which contribute to arousal, alertness as well as the modulation of forebrain, hindbrain and spinal sites regulating the autonomic nervous system activity leading to the stimulation of the sympathetic nervous system and release of catecholamines,50-52 and sacral parasympathetic activity while decreasing vagal efferent output53-55 that influences immune and visceral function.56,57 In addition the brain CRF/CRF1 signaling pathway is involved in stress-related induction of anxiety/depression44,45,58 and alterations of colonic motor and visceral pain while both central and peripheral CRF2 receptor activation may exert a counteracting influence.59-63 Moreover recent experimental and clinical studies point to an equally important contribution of the peripheral CRF/CRF1 signaling locally expressed in the gut to the GI stress response.19,64
Visceral Pain Pathways
Pain perception in peripheral tissues depends on the signal transmission from the site of pain origin to the CNS. Nociceptors (receptors activated by noxious stimuli)65 located in 2 sets of primary small afferent fibers (C and Aδ afferents) innervating the viscera that project to distinct regions in the CNS,66 are the primary pathways of pain transmission. From the esophagus to the transverse colon, the GI tract innervation is provided by vagal afferent fibers originating in the nodose ganglia and projecting centrally to the nucleus of the solitary tract. Pelvic nerve afferent fibers, which originate in the lumbosacral dorsal root ganglia, and project centrally to the lumbar 6 - sacral segments of the spinal cord innervate the remaining part of the large bowel (descending and sigmoid colon, rectum). The entire GI tract is also innervated by afferent fibers contained in the splanchnic nerves projecting to the thoracic 5 - lumbar 2 segments of the spinal cord.67 Even though visceral afferents constitute only 10% of all afferents, they are able to monitor changes in the gut milieu and participate in the transmission of visceral sensory information.68,69 Of note, vagal afferents do not encode painful stimuli however, changes in their activity can modulate nociceptive processing in the spinal cord and the brain.68,70,71
Upon entering the dorsal horn, visceral primary afferents carried out by the pelvic and splanchnic nerves terminate in spinal cord laminae I, II, V and X72 converges onto spinal neurons in the lumbosacral segments and thoracolumbar segments respectively. Lumbosacral segments process reflex responses to acute visceral pain, while thoracolumbar segments' involvement in normal visceral sensation is uncertain,73 however, both segments process inflammatory stimuli.73 Subpopulations of neurons within the dorsal horn project to discrete nuclei within the thalamus (ie, ventral posterior lateral thalamus) as well as other structures in the brain stem (parabrachial nucleus, periaqueductal gray, nucleus tractus solitarius). From the thalamus, the information is conveyed to cortical areas involved in sensory processing (such as the somatosensory cortex) or those involved in processing emotional or affective information (such as the anterior cingulate gyrus and insular cortex).65,74
In addition to the ascending system, which enables pain perception described above, other neural circuits originating from supraspinal sites can influence nociceptive activity in the spinal cord and in primary afferents, a system referred to as descending pathways.75 There are 2 types of descending control pathways: inhibitory, which produce analgesia (periaqueductal gray, locus coeruleus) and facilitatory which produce hyperalgesia (rostroventral medulla and OFF and ON cells).76,77
Visceral Pain Monitoring in Rodents
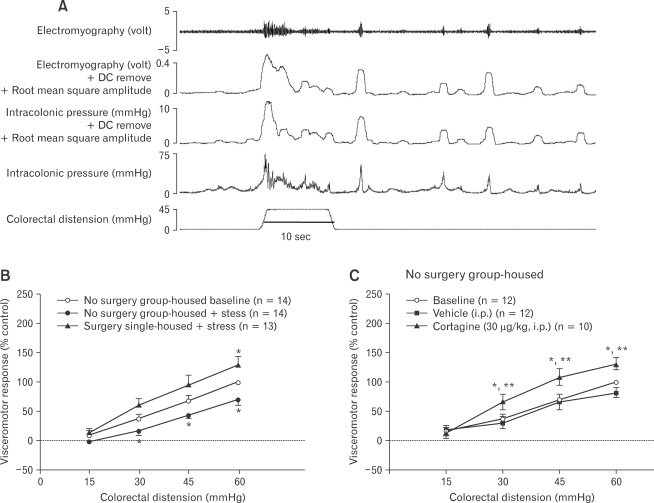
The primary readout and the standard assay for the measurement of visceral pain in rodents consists in the monitoring of abdominal muscles contraction or visceromotor response (VMR) to controlled isobaric distensions of the distal colon by an inflatable balloon.78 The VMR can directly be assessed as electromyographic (EMG) signals monitored via surgically-implanted recording electrodes in external or internal abdominal muscle which are either externalized through the skin (abdomen, neck)79-81 or connected to radiotelemetric implants in the abdominal cavity.82,83 Although the method is of significant value in the field of visceral pain study, it has experimental shortfalls such as damage to EMG electrodes, loss of signal and electrical interferences which is of particular concerns in chronic experimental settings. Additionally, EMG surgery involves skin and/or muscle incision depending on the technique used (subcutaneous abdominal electrodes or intraperitoneal cannula) and chronic implantation of a foreign body. Even though no data are available in the literature in relation to the impact of chronic EMG electrodes placed into the abdominal wall, such intervention could induce a host-tissue response with local micro-inflammation (neutrophils, lymphocytes and macrophages) as it has been shown for other types of implants in the skin and peritoneum.84,85 A recent report suggests that the preconditions of animals (EMG surgery, and post-surgical delivery of antibiotic and single housing) has considerable impact on their visceral pain responses, particularly in the context of stress studies.86 Other approaches consist of recording manometric changes in the pressure of the balloon inserted into the distal colon86,87 or changes in pressure inside the colonic lumen.19,88 These 2 later techniques present the advantage of being minimally invasive as they do not require surgery and post-surgical treatments such as antibiotic, analgesics which can affect the visceral pain responses and still remain an objective and sensitive measure of abdominal contractions (Fig. 1). However, they require the animals to be partially restrained in Bollman cages, a context to which they need to be habituated and which by itself may bring a component of stress.
Figure 1.
Differential influence of intermittent repeated stress on visceral response to colorectal distension (CRD) in rodents with or without surgical procedure for recording visceral pain (Adapted from Larauche et al19,88). (A) Original and rectified representative electromyographic (EMG) and intraluminal colonic pressure (ICP) traces recorded simultaneously on the same mouse in response to CRD (45 mmHg, 10 seconds). When both raw EMG (upper line) and ICP (second line to the bottom) signals are analyzed in Spike 2 by computing "DC Remove" 1 second to exclude all slow events > 2 seconds (ie, colonic smooth muscle contractions) and "root mean square amplitude" to extract the area under the curve of the signal, the resulting EMG and phasic ICP signals (middle lines) present a significant overlap. (B) Mice were equipped with EMG electrodes or not and exposed to water avoidance stress for 1 hour per day for 10 days tested with ICP for visceromotor response (VMR) to CRD. (C) Intraperitoneal injection of the selective corticotropin releasing factor receptor subtype 1 agonist, cortagine-induced visceral hypersensitivity in C57BL/6 mice tested with ICP for VMR to CRD. Data are expressed as mean ± SEM, n = 10-14 per group as specified in graph legends. *P<0.05 compared with baseline, **P< 0.05 vs vehicle.
Behavioral approaches such as operant behavioral assays78 have also been used in early studies and capitalized on the learning and fear behaviors of animals in response to painful CRD. Visual monitoring of the abdominal withdrawal reflex89 has also been applied in a few studies, and while having the great advantage of being one of the less invasive technique employed to date, it is a very subjective method. Indirect endpoints such as Fos or extracellular signal-regulated protein kinase induction in the CNS,29,62,90-92 and functional brain imaging of integrated brain responses to nociceptive stimuli33,93 have also been utilized in some studies. These approaches allow for direct assessment of the neuronal circuitries recruited by the visceral pain stimulus and, in the case of functional brain imaging is very similar to the monitoring of CRD responses in healthy and IBS human subjects. Unfortunately, in animals these brain mapping techniques require euthanasia and limit the assessment to specific time points. However, as more stringent brain imaging approaches are developed in rodents, they will open new venues to parallel human studies.94
Experimental Stress Models and Visceral Pain
By convention, stressors are categorized in exteroceptive (psychological or neurogenic) and interoceptive (physical or systemic) classes95,96 and both have been used in animal models to investigate the relationship between stress and visceral pain.97 Dual visceral pain responses: hyperalgesia and analgesia have been described in rodents exposed to exteroceptive stressors. Though only recently investigated, the analgesic response bears very relevant implications in the understanding of visceral pain-associated pathologies (detailed in section "Stress-induced visceral analgesia: how does it help us to model and understand visceral hypersensitivity?") In contrast, interoceptive stressors have been most consistently associated with the development of stress-induced hyperalgesia.
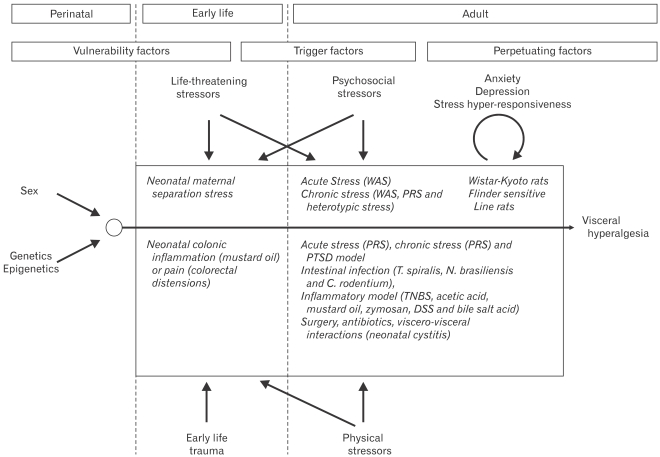
Stress modulates visceral pain in IBS patients as well as in healthy subjects,9,98 therefore experimental animal models, involving exposure to various clinically relevant stressors have been developed to recapture features of IBS symptoms, of which hyperalgesia to sigmoid distensions is a hallmark.99,100 Moreover clinical studies have stratified that the stress-related modulation of IBS symptoms9 may be occurring through (1) permanent enhancement of stress responsiveness, (2) transient symptom exacerbation and/or (3) symptom perpetuation. Consequently existing experimental stress models target different periods throughout the lifespan of animals to assess the vulnerability, the trigger and perpetuating factors determining stress influence on visceral hypersensitivity (Fig. 2).
Figure 2.
Animal models of stress-induced modulation of visceral sensitivity throughout the lifespan (Modified from Mayer et al9). Experimental stress models have been developed that target different periods throughout the lifespan of animals to assess the vulnerability, trigger and perpetuation influences of stress on visceral sensitivity. During early life, trauma due to maternal neglect (neonatal maternal separation stress) or injury (neonatal chronic colonic inflammation or pain) can enhance the susceptibility of individuals to develop altered visceral pain responses at adulthood. During adulthood, life-threatening stressors (post-traumatic stress disorder model), psychosocial stressors (acute and chronic stress) or physical stressors (intestinal infection or inflammation, antibiotic administration and surgery) have all clearly been established as triggering factors to the development of visceral hypersensitivity in rats and mice. Lastly, the use of specific strains of rodents known to exhibit various levels of anxiety, depression or stress hyper-responsiveness (Wistar-Kyoto and Flinders Sensitive Line) help mimic the influence of perpetuating factors on symptoms of visceral pain. WAS, water avoidance stress; PRS, partial restraint stress; PTSD, post-traumatic stress disorder; DSS, dextran sodium sulfate.
Stress in the Perinatal Period: Genetic/Epigenetic Factors
Twin studies in IBS patients showed higher (but relatively low) concordance rates in monozygotic than dizygotic twins suggesting that although genetic factors are not dominant, they play a role in the occurrence of IBS.101 There is also a growing literature reporting the association between functional genetic polymorphisms and IBS at the level of serotonin transporter gene (associated with diarrhea in female IBS patients), or α2-adrenoreceptor gene (associated with constipation), and more recently, additional gene polymorphisms have been unraveled supporting the potential permissive role of genetics in IBS pathophysiology.102-105 Of interest, it has been postulated that epigenetic factors related to heritable changes in gene expression that occur without alteration in gene sequence, determine the manner in which gene activity may be altered either transiently or permanently in response to environmental challenges.106 Such epigenetic modifications could account for symptoms persistence, familial clustering and the transgenerational impact of IBS. However, experimental studies have not dwelled on strain differences in terms of stress responsiveness, anxiety and depression in rodents,107-110 to assess and compare how genetic predisposition together with perinatal (maternal prenatal stress) or early life stressors (neonatal maternal separation stress) could affect visceral pain responses at adulthood in the context of epigenetic modifications. There is only one preliminary report suggesting that strain may determine the duration of the visceral hyperalgesia in response to chronic heterotypic stress (detailed in section "Stress in the adult period: trigger factors, Psychosocial stressors"). The influence of genes on the vulnerability of rodents to exhibit visceral hypersensitivity has however been assessed in relation with anxiety behavior at adulthood in rat strains with different anxiety/depression backgrounds110 (detailed in section "Genetic models of anxiety & depression").
Stress in the Early-life Period: Vulnerability/Trigger Factors
Early life events and childhood trauma by biopsychosocial factors (neglect, abuse, loss of caregiver or life threatening situation) enhance the vulnerability of individuals later in life to develop affective disorders (depression, anxiety and emotional distress) and put them at a greater risk for developing IBS.12,99 In the context of epigenetic modifications, experimental studies showed that early developmental trauma decreases glucocorticoid receptor expression by hypermethylation of a key regulatory component and consequently affects the feedback regulation the HPA-axis with impact on the endocrine/behavioral adaptation and the susceptibility to stress-related disorders.112 In addition, experimental studies indicate that the newborn's gut through stress-related changes in intestinal permeability may be exposed to a variety of factors resulting in mucosal inflammation and tissue irritation which could have long-term consequences at adulthood even though no longitudinal clinical studies exist showing that gut irritation in early life is a risk factor for IBS development at adulthood.97 Moreover, postnatal microbial colonization has been also suggested as a potential factor programming the HPA-axis response to stress in mice.113
An experimental model commonly used as a stress model to mimic early stress/childhood trauma is the neonatal maternal separation in rodents. This is achieved by isolating pups from the dam for 2-3 hours/day during the first 2 weeks after birth from postnatal day (PND) 1-2 to PND 14.17,114-116 At adulthood, rats previously subjected to neonatal maternal separation exhibit visceral hypersensitivity to CRD under basal conditions which is further exacerbated by exposure to the acute psychological stressor in the form of water avoidance stress (WAS) consisting in placing rodents on a small platform surrounded by water for 1h.117,118 Other models used repeated intermittent colonic irritation during the neonatal period (PND 8-21) either in the form of daily noxious CRD (60 mmHg-60 seconds distension twice separated by 30-minute period of rest) or by performing daily intracolonic injection of mustard oil (5%), increases pain behavior to CRD from postnatal week 5 up to postnatal week 12.89,119 Likewise, an acute somatic injury (saline or carrageenan injections into the hind paw) performed during the critical period of postnatal development, ie, before PND 14, produces visceral analgesia to CRD in adult rats.120
Based on these studies and the extensive amount of evidence originating from somatic pain studies,121,122 it appears that neonatal insults either acute or repeated, somatic vs visceral occurring during the development of the organism contribute to induce a state of visceral hypersensitivity in adulthood which may reflect long-term changes in visceral sensory processing.120
Stress in the Adult Period: Trigger Factors
Psychosocial stressors
Psychosocial stressors (eg, threat to social status, social esteem, respect and/or acceptance within a group; threat to self-worth) activate stress circuits within the emotional motor system and induce neuroendocrine response (CRF and cortisol) and autonomic response (norepinephrine and epinephrine) that result in the modulation of gut sensory, motor and immune function as well as intestinal permeability.9 In experimental studies, the 2 main acute stressors that are prominently used in visceral pain studies are WAS for 1 hour and partial restraint stress for 2 hours, a stressor with stronger psychological component than WAS, which entails taping the forelimb of rats in order to prevent their movements.123-125 Exposure of male Wistar rats to WAS for 1 hour leads to the development of a delayed visceral hyperalgesia to CRD, appearing 24 hours after the end of the stress,126 while exposure to partial restraint stress, induces an immediate hyperalgesia to CRD in male127 and female Wistar rats.115
However, in the context of clinical studies in which daily chronic stress predicts the intensity and severity of subsequent symptoms in IBS patients,4-6,99,128,129 a variety of chronic stress models divided in 2 categories have been recently developed in adult rodents. The first category consists in exposing animals repeatedly (over a few days to weeks) but intermittently (once or twice per day) to 1 or different stressors, with the aim of mimicking the daily exposure to psychosocial stress that humans can encounter through their personal and professional interactions. The second category consists in continuous exposure to stressors as part of change in internal state, for instance inflammation, or external milieu, for instance single housing, or social crowding which mimics the effect of social milieu in humans or using genetic rodent strains that have constitutive stress hyper-reactivity (Wistar Kyoto, Flinders Sensitive Line). In particular, repeated intermittent exposure to WAS is one of the first "chronic" stress model to have been adapted to the study of visceral hypersensitivity 81 and is presently widely used.88,130,131 Initial studies in which the visceral pain response was monitored using EMG recording that entails surgical implantation of electrodes, male Wistar rats exposed to 10 consecutive days of WAS for 1 hour daily developed visceral hypersensitivity to CRD lasting up to 30 days after the end of the last session of WAS.81,130 In our laboratories however, we found that when naïve male and female Wistar rats were exposed to a similar WAS schedule and their VMR was monitored by intraluminal colonic solid-state manometry, a technique that does not require surgery, animals developed visceral analgesia to CRD.132 Similar results have been obtained in C57BL/6 mice88 and analgesic vs hyperalgesic responses were established to be dependent upon preconditions (surgery and single housing) associated with the method of recording of VMR (Fig. 1).88,133 Therefore, the impact of repeated mild stress such as 1-hour exposure to WAS on visceral pain response to CRD is largely influenced by the basal state conditions of the animals before applying the repeated stressor (detailed in section "Stress-induced visceral analgesia: how does it help us to model and understand visceral hypersensitivity?" and reference 88). Repeated exposure to unpredictable sound stress has also been recently shown to provide a model of delayed visceral hyperalgesia in male Sprague-Dawley rats.134
Because habituation can occur in response to repeated exposure to an homotypic stressor,135,136 heterotypic stress models with different and alternating modalities to induce stress have been recently developed. However male Wistar rats exposed randomly to a combination of cold restraint stress (45 minutes), WAS (1 hour) or forced swimming (20 minutes), 1 stressor per day for 9 consecutive days develop visceral hypersensitivity only at 8 hours but not at 24 hours or 7 days after the end of the last stressor.137 Interestingly however, the same regimen of alternating stressors in a different strain of rats, Sprague-Dawley, led to a sustained visceral hypersensitivity lasting up to 2 weeks after the end of the stressor (S. Sarna and J. Winston, pers. comm.), suggesting that the strain and therefore genetic background of the animals, affects the visceral pain responses to repeated intermittent exposure to different stressors.
Life-threatening stressors
Retrospective clinical studies indicate that living through or seeing a traumatic event, such as war, environmental disasters, rape, physical abuse or a bad accident in adulthood can lead to post-traumatic stress disorder (PTSD).138-144 There is evidence of increased prevalence of GI symptoms, in particular IBS in PTSD sufferers including war veterans.138-142 Additionally, patients with IBS who have experienced traumatic events may be at higher risk for other co-morbid psychiatric disorders than IBS patients without a trauma history.141
In adult rats, treatment with a relatively short-lasting session of shocks or a social confrontation with a predator or aggressive conspecific animals induces long-lasting (weeks-months) conditioned fear-responses to trauma-related cues, and a generalized behavioral sensitization to novel stressful stimuli that persists or grows stronger over time.145-148 Repetitive balloon distention of the distal colon causes increased cardiovascular 'pseudoaffective' reflexes in pre-shocked rats compared to controls, 2 weeks after a single session of foot shocks.145-148 Of note, female rats appear to show a different pattern of sensitized behavioral responsiveness to the same challenge, possibly pointing to sex-related alterations in the neuronal substrates involved.149
Interoceptive stressors
In approximately 10% of patients with IBS, the onset of symptoms began with an intestinal infectious illness.150 Bile salt malabsorption resulting from infectious damage with organisms such as Salmonella and Campylobacter within the terminal ileum and right colon may also underlie some forms of post-infectious IBS.151 Inflammation, antibiotic treatments, bladder infection and surgery may also contribute to the symptoms in some patients. Below are described some experimental models of interoceptive stressors that have been used to mimic these clinical conditions.
Post-infectious irritable bowel syndrome model
Prospective studies have shown that 3% to 36% of enteric infections lead to persistent new IBS symptoms depending on the infecting organism. In addition, the co-existence of adverse psychological factors at time of infection is also an important determinant to the susceptibility to develop post-infectious IBS.152 Other risk factors include female sex and some psychological characteristics such as anxiety, depression and somatization.152 While viral gastroenteritis seems to have only short-term effects, bacterial enteritis and protozoan and helminth infestations are followed by prolonged post-infectious IBS.152 The vast majority of human post-inflammatory hypersensitivity symptoms are observed after bacterial infection (Campylobacter, Shigella, Salmonella or Escherichia coli infections).
In preclinical models, long-lasting visceral hyperalgesia has been observed in mice after transient intestinal inflammation induced by Trichinella spiralis infestation153,154 or in rats infested by Nippostrongylus brasiliensis.155 Recently, however, it was found that male C57BL/6 mice infected with Citrobacter rodentium, an attaching-effacing murine enteropathogen similar in its mechanisms of infection to enteropathogenic Escherichia coli, do not spontaneously develop visceral hypersensitivity symptoms assessed by the increase in EMG response to CRD156 unless exposed to a stressor (WAS, 1 hr/day for 9 days) during the time of infection (S. Vanner and N. Cenac, pers. comm.).
Post-inflammatory irritable bowel syndrome model
Despite some controversies on the origin of the symptoms,157,158 "IBS-like" symptoms appear to be common in patients in remission from ulcerative colitis.15,159 In rats, chemical irritants applied to the colon such as acetic acid,160 mustard oil161,162 and zymosan163,164 evoke short-term hyperalgesia associated with transmural tissue damage/colonic inflammation. Intracolonic trinitrobenzene sulfonic acid induces a severe colonic transmural inflammation and visceral hypersensitivity that develops at 4-5 days with the disappearance of symptoms by 14 days.165,166 Interestingly, in 24% of rats there is reoccurrence of visceral hyperalgesia 16 weeks after the induction of inflammation, while there is no evidence of microscopic inflammation in rat colonic tissues at this time point.166,167 In a similar manner, daily intracolonic instillation of bile acid deoxycholic acid for 3 days induces a mild, transient colonic inflammation within 3 days of administration that resolves within 3 weeks in adult male Sprague-Dawley rats. In this model, a persistent visceral hyperalgesia starts after 1 week of bile acid administration which lasts up to 4 weeks.168
Mild non-specific colitis and acute dextran sodium sulfate (DSS, 5% in drinking water for 5 days)-induced colitis have been associated with increased responsiveness to CRD on days 5 or 60 after the induction of colitis in male Balb/c mice while chronic colitis induced by DSS (3 cycles of 5% DSS for 5 days/cycle and 15 days of normal drinking water in between each cycle) has not.167 These results are in contrast with another study showing that 4% DSS in drinking water for 5-7 days-induced colitis but failed to cause the development of visceral hypersensitivity in response to CRD in C57BL/6 or Balb/c mice when tested on days 5, 12, 16, 20, 30, 40 or 51 after the induction of colitis.170 These disparate findings suggest that inflammation alone may not always lead to visceral hypersensitivity and that the type of inflammatory insult and severity determine whether this will result in the development of postinflammatory hypersensitivity. The interaction between colonic inflammation and the development of visceral pain has to be substantiated in future investigations.166
Antibiotics
Patients treated with antibiotics for non-GI complaints are 3 times more likely to report functional bowel symptoms. Antibiotic use disrupts the intestinal microbiota, fragilizes the host's intestinal homeostasis and integrity of intestinal defenses,171 and has been associated with IBS.172 In support of this hypothesis, administration to Balb/c mice of an oral combination of non-absorbable antibiotics (neomycin, bacitracin and pimaricin) which disturbed the commensal intestinal microflora results in visceral hypersensitivity to CRD in these animals.173 Paradoxically, clinical studies support that specific antibiotics (rifaximin or neomycin) are an effective treatment option in non-constipated IBS patients, over a 3-month period174,175 or even longer,176 thereby confirming the role of dysbiosis in developing IBS symptoms.177
Surgery and somato-visceral convergence
Despite controversies, studies suggest that IBS is associated with an increased risk of abdominal and pelvic surgeries.178 Surgical procedure as both a visceral and psychological stressor can initiate a series of events that either disturb GI function and interactions within the brain-gut axis and/or alter gut microbiota, which consequently may lead to generation of IBS symptoms.179 Hind paw (plantar) incision or injection of low pH (4.0) sterile saline in the gastrocnemius muscle of adult male Sprague-Dawley rats induce a significant visceral hyperalgesia to CRD that lasts up to 2 weeks after the somatic injury occurred.180,181 As a model of postsurgical pain, the plantar incision model is particularly relevant because surgical procedures are relatively common and possible visceral hypersensitivity may also thus be a relatively common postsurgical event.179 The impact of somato-visceral convergence has to be considered in experimental models of visceral pain where animals are surgically equipped within the abdominal wall with EMG electrodes84 (detailed in section "Stress-induced visceral analgesia: how does it help us to model and understand visceral hypersensitivity?).
Viscero-visceral interactions: neonatal cystitis
A significant overlap is observed between IBS and urinary symptoms, in particular those resulting from interstitial cystitis (IC).182 Like IBS, IC predominantly affects female patients (90%) and shows a high comorbidity rate with psychological disorders. By analogy to IBS, an increased number of mast cells have been found in bladder biopsies in IC.183 Recurrent urinary tract infections during childhood correlate with the development of chronic pelvic pain, a condition that often overlaps with IBS.184 In an animal model of bowel-bladder cross-sensitization, acute bladder chemical irritation causes a significant decrease in colorectal sensory thresholds to CRD.185 Very recently, the induction of neonatal cystitis in female Sprague-Dawley rats at PND 14 was shown to result in colonic hypersensitivity to CRD during adulthood,186 supporting a potential key role for viscero-visceral convergence in IBS and comorbid disorders such as IC and chronic pelvic pain.182
Stress in the Adult Period: Perpetuating Factors
There is a strong overlap between IBS and psychiatric disorders, as established by the high percentage (54% to even 94%) of IBS patients meeting the criteria for at least 1 primary psychiatric disorder, most notably mood and anxiety disorders.182 Although comorbid psychiatric disorders seem to be not directly connected with the occurrence of IBS, they strongly influence how the symptoms are experienced, the individual illness behavior, and ultimately the outcome. The influence of cognitive aspects as well as motivational and emotional components on the processing of sensory information is mediated by extensive neuro-anatomical network with a pivotal role of the insular and anterior cingulate cortices.9,187,188 Autonomic dysfunction, in particular decreased parasympathetic activity and increased sympathetic outflow observed in psychiatric disorders as well as in IBS,16,189,190 has been also suggested to have a relevant impact on the neurally mediated regulation of colonic sensory-motor and immune function.191 The neuroimmune cross-talk involving the stress-induced changes in vagal nerve activity and/or sensitization of mast-cells seems to play a critical role in altering visceral sensitivity and intestinal barrier.192
Genetic models of anxiety and depression
In a comparative study using 3 strains of rats known to have varying levels of baseline anxiety, the high-anxiety Wistar-Kyoto rats had increased VMR to CRD compared to low-anxiety Sprague-Dawley and Fisher-344 animals suggesting a direct link between anxiety and visceral hypersensitivity.111 In addition, compared to low-anxiety strains of rats, the sensitivity of high-anxiety rats was highly exacerbated by peripheral sensitization of the colon with a small dose of acetic acid.111 Of note, Wistar-Kyoto rats are also considered as a model of depression,193,194 as are rats from the Flinders Sensitive Line which exhibit increased cholinergic sensitivity compared to control rats of the Flinders Resistant Line.195,196 Similarly to Wistar-Kyoto rats, Flinders Sensitive Line rats exhibit increased VMR to CRD as well as a blunted corticosterone response to acute noise stress compared to Flinders Resistant Line, suggesting a link between depression, HPA axis dysfunction and visceral hyperalgesia.197
Genetic models of chronic stress
Genetic models that blocked chronically the stress pathways by deleting CRF1 receptors showed a decrease in anxiety and colonic sensitivity to CRD.198 Conversely, genetic models of chronic stress relying on the over-expression of CRF stress system in mice199 are available and could be useful to study IBS-like manifestations, but the visceral sensitivity of these transgenic animals has not been assessed yet. However, as CRF over-expressing mice display phenotypes of Cushing's syndrome,200 new promising genetic models with more selective conditional and/or region-targeted genetic manipulations including RNAi gene silencing technology to modify CRF-related genes are continuously developed.201-206 These models will be suitable to explore specific stress circuitries in the context of targeted chronic CRF expression/deletion and the impact on visceral pain modulation which so far is lagging behind.
Stress-Induced Visceral Analgesia: How Does It Help Us to Model and Understand Visceral Hypersensitivity?
While extensively described in somatic pain field,207 to date activation of descending inhibitory pathways in stress-related visceral responses has received less attention. Opioids have been implicated in descending inhibition of visceral sensitivity following an acute stress as evidenced by the fact that naloxone unmasked WAS-induced hyperalgesia to CRD in normal Long-Evans rats and exacerbated the pain response to CRD in maternally-separated rats.117 In another study, a non-opioid, neurotensin-dependent visceral analgesic response was observed 6 hours after exposure to an acute session of WAS in Sprague-Dawley rats, with males exhibiting stronger analgesia than females as well as in wild-type but not in neurotensin knock-out mice.208 In another experimental model, a daily short period (15 minutes) of separation from PND 2 to 14, decreased VMR to CRD performed immediately after WAS and prevented the development of hyperalgesia 24 hours after WAS in adult male Long-Evans rats.209 These data suggest a potential upregulation of endogenous pain-modulatory systems by this short maternal separation stress.209 Similar findings in adult rats have been recently reported, such that Wistar rats handled daily for 9 days develop visceral hypoalgesia in response to CRD that becomes significant 7 days after the last handling.137
These studies point to the type of stress itself contributing to the differential recruitment of those descending inhibitory pathways. However, importantly, we recently demonstrated that mice that had undergone surgery for the placement of EMG electrodes on abdominal wall and were subsequently single housed to avoid deterioration of implanted electrodes by cage-mate, developed visceral hyperalgesia in response to repeated WAS (1 hr/day, 10 days) while mice tested for visceral pain using the non-invasive solid-state intraluminal pressure recording and kept group housed developed a strong visceral analgesia under otherwise similar conditions of repeated intermittent WAS.88 As mentioned before surgery per se is known to induce a long lasting visceral hyperalgesia and recent reports suggest that previous injury or exposure to opioids in male rats can switch stress influence on pain responses from analgesia to hyperalgesia.210 Collectively these data demonstrate that the state of the animal tested (naïve vs exposed to surgery), its social environment (group housing vs single housing, cage enrichment or not), the handling performed by the investigator, the methods used to record VMRs (EMG requiring surgery and antibiotic post surgery vs manometry not requiring surgery/antibiotic), as well as the sex of animals can significantly affect the response to exteroceptive stressors. Therefore these preconditions should be carefully detailed in describing the experimental conditions and taken into consideration in the design, conduct and interpretations of the data when investigating the influence of stress on visceral sensitivity in experimental animals.
Based on recent clinical findings demonstrating that IBS patients have compromised engagement of the inhibitory descending pain modulation systems,21,211,214 gaining a deeper understanding of the mechanisms involved in the expression of stress-induced visceral analgesia or lack thereof are promising avenues to be explored and may lead to new therapeutic targets for IBS. Therefore the use of non-invasive methods of monitoring VMR that alleviates the surgical, antibiotic and housing impacts on repeated stress modulation of visceral pain represents a step forward to gain insight into the underlying mechanisms in particular the neural substrates and neurochemistry of stress-related analgesia as established in the somatic field.207
Sex Differences in Stress-Induced Alterations of Visceral Sensitivity
Women are more susceptible to stress-related disorders which is consistent with female predominance in IBS patients (women to men ratio about 2:1).215,216 Sex differences in the stress response and stress-induced pain modulation have been documented in a number of human studies.217 Clinical trials have also revealed important sex-related differences in therapeutic efficacy of some serotonergic drugs used in IBS treatment (eg, alosetron, 5-HT3 receptor antagonist) suggesting a conceivable link between estrogens and serotonergic mechanisms in the modulation of stress-related visceral hypersensitivity.218,219 Contrasting with this clinical evidence, most of the preclinical studies assessing stress-related alterations in visceral sensitivity have been conducted in male rodents.208,220 However, the few studies performed in female indicate that sex hormones have a significant effect on visceral sensitivity in rodents.220-224 Therefore, addressing the influence of sex and sex hormones in the modulation of visceral pain by stress appears critical to develop novel therapies relevant to sex difference in IBS.216,225
Mechanisms Involved in Stress-Induced Modulation of Visceral Pain
Maladaptive neuroplastic changes leading to persistent increased perception and responsiveness to noxious stimuli, or response to normally non-noxious stimuli are key for the expression of pathological pain (hyperalgesia and allodynia). Such neuroplastic changes can occur in primary afferent terminals (peripheral sensitization) but also in the spinal cord (central sensitization) and in the brain (supraspinal pain modulation) or in descending pathways that modulate spinal nociceptive transmission. Such alterations in the processing of sensory information are all considered as possible mechanisms of visceral hypersensitivity in IBS patients.66,226
Peripheral Sensitization: Corticotropin Releasing Factor System, Mast Cells, Gut Microbiota and Ion Channels
Several reports in both humans and rodents have well documented the key role played by the peripheral CRF signaling, via CRF1 receptors, in the development and expression of visceral pain.19,60,227-231 Stress and peripheral administration of CRF induce mast cells degranulation in the colon in experimental animals and humans,232,233 which contributes to the development of visceral hypersensitivity (Fig. 1) via the release of several preformed or newly generated mediators118,234-237 (histamine, tryptase, prostaglandin E2, nerve growth factor) that can stimulate or sensitize sensory afferents66,238 by activating a number of ion channels widely expressed in colonic afferents239-242 such as N-methyl-D-aspartate receptor,242 proteinase-activated receptor,236 and transient receptor potential vanilloid 1243-245 to name a few.
Stress can also disrupt the intestinal epithelial barrier thereby increasing the penetration of soluble factors (antigens) into the lamina propria, leading to nociceptors sensitization,235,246 a phenomenon which appears as a prerequisite for the development of visceral hypersensitivity in both humans and rodents.246-248 Alterations of epithelial permeability following stress involves the activation of the peripheral CRF system and may249-253 or may not be dependent from mast cell activation238,253 in a time-dependent manner. In addition to inducing a leaky epithelial barrier, stress can also change the composition of the intestinal and fecal microbiota of rodents.254-256 This can in turn have significant impact on the host and affect behavior, visceral sensitivity and inflammatory susceptibility.257-261
Spinal Cord Plasticity and Glia Activation: Central Processing of Peripheral Pain Perception
Once peripheral sensitization has occurred, it activates the release of mediators in the spinal cord including growth factors262,263 (nerve growth factor or brain-derived neurotrophic factor) and upregulates some key ion channels and receptors such as acid-sensing ion channels 1A and neurokinin 1 receptor264-267 contributing to the phenomenon of spinal sensitization which has been associated with visceral hypersensitivity.
Very recently, spinal cord glia activation has been suggested as being another potential mechanism through which spinal sensitization may occur in response to stress linked to the development and maintenance of visceral hypersensitivity.268-270 Candidate molecules involved in glia activation signaling include neurotransmitters such as susbstance P or glutamate, but also purinergic agents, opioids, chemokines and glucocorticoids (for review see reference268). Glutamate uptake through spinal glutamate transporters is critical for maintaining normal sensory transmission under physiologic conditions.271,272 A potential deficiency in glutamate reuptake by astrocytes associated with the activation of spinal cord glia273 has been recently suggested to play a role in the spinal sensitization and the development of visceral hypersensitivity in rats.274 Together, these data strongly support the concept that transmission of visceral nociceptive signals may be enhanced in various conditions of spinal microglia activation.275
Supraspinal Pain Modulation: A Fine-tuning between Pain Facilitation and Inhibition
Various supraspinal sites are involved in the modulation of visceral pain signals. Rectosigmoid distension in humans activates sensory (insula and somatosensory cortex), and limbic and paralimbic regions (including anterior cingulate cortex, amygdala and locus coeruleus).276 Many of these brain regions were also found to be significantly activated by CRD in rats.25-27,33,277
The anterior cingulate cortex mediates key emotional-aversive aspects of pain and may also have a mnemonic role in which it allows transient storage of information during pain processing.189,278 Wistar-Kyoto rats, high-anxiety rats exhibiting visceral hypersensitivity111 have greater prefrontal cortex activation in response to CRD compared to Sprague-Dawley.91 Another key limbic system structure that has been implicated in the affective component of pain is the central amygdala. It is involved in the processing of visceral information, attention, emotion and integrating the physical and psychological components of the stress response.279 It has also been found to contribute to visceral hypersensitivity in rats.280-283 Of relevance in the context of stress response, the CRF gene expression in the amygdaloid nucleus is upregulated in a mouse model of visceral pain and such a response is attenuated under conditions of anesthesia.283,284 Likewise, the locus coeruleus is a well established target of stress that expresses CRF1 receptors, receives CRF innervation from nearby Barrington nucleus and increases firing in response to CRD that is mediated by CRF1 receptor activation as shown by the use of CRF receptor antagonists and the responsiveness of LC neurons to both CRD and to central injection of CRF.53,285-290 Therefore these limbic and pontine sites are well positioned to coordinate gut-brain interaction with visceral information from the gut impacting on cortical and limbic activities under conditions of stress-CRF1 signaling activation which may modulate the visceral pain responses.60,76,291
Thalamic relay nuclei have a key role in gating, filtering and processing sensory information en route to the cerebral cortex and are subject to similar activity-induced plasticity processes as the spinal cord.292-294 Upregulation of CRF1 receptor in the thalamus is associated with visceral hyperalgesia in the rat model of neonatal maternal separation stress.275 Lastly, spinal visceral nociceptive reflexes are subject to facilitatory modulation from the rostroventral medulla, providing the basis for a mechanism by which visceral sensations can be enhanced from supraspinal sites295,296 under stress conditions associated with development of visceral hyperalgesia.297 Compromised engagement of descending pain inhibitory pathways as observed in maternally-stressed rats may also contribute to increase the visceral pain responses in those animals.117
Therapeutic Implications-Treatment Targeting Stress Reduction in Irritable Bowel Syndrome
The modulatory role of stress-related brain-gut interactions in the IBS pathophysiology, in particular neuroimmune modulation associated with psychological factors and emotional state16,189 has been confirmed by the encouraging outcome of non-pharmacologic and pharmacologic treatment modalities aimed at reducing stress perception.298-300 A broad range of evidence-based mind-body interventions including psychotherapy, cognitive behavioral therapy, hypnotherapy, relaxation exercises or mindfulness mediation has been shown to amend stress coping strategies, both at a cognitive level (catastrophic or self-defeating thoughts) and at a behavioral level (problem solving, especially interpersonal problems).300,301 The symptomatic improvement appears to result from the modulation of stress response, the autonomic nervous system balance restoration, and changes in the brain activation pattern in response to visceral stimuli. In addition to psychological mind-body approaches, clinical trials confirm the effectiveness of centrally-targeted pharmacological interventions such as with antidepressants, and anxiolytics, or combination of drugs from both groups in the treatment of chronic pain disorders.299,302,303 Many other pharmacological agents with anxiolytic and/or antidepressant properties, such as serotonergic and opioidergic agents, cannabinoid receptor 1 (CB1) and somatostatin receptors agonists, CRF1, tachykinin and cholecystokinin receptors antagonists, have been recently shown to modulate stress-induced visceral hyperalgesia in animal models (for detailed review see reference304). Preliminary data suggest that anxiolytic activity of γ-aminobutyric acid-ergic agents (gabapentin) and α2δ ligand (pregabalin) may be also efficient in reducing central sensitization in hyperalgesia in clinical setting305 as shown in experimental models.306 New centrally acting agents providing analgesic effects include dextofisopam (2,3-benzodoazepine receptor modulator) and quetiapine (atypical antipsychotic agent).307
Recent developments showing the critical interdependence between the composition and stability of the microbiota and GI sensory-motor function indicate a novel approach to IBS treatment with a use of probiotics, prebiotics and antibiotics.260,308 Specific modulation of the enteric microbiota in the context of neuroimmune interactions within the brain-gut axis opens a new promising strategy for stress-related disorders, particularly in the aspects of comorbidity in functional GI disorders such as IBS.257
However, some of the encouraging data from animal models concerning efficiency in alleviating stress-induced visceral hypersensitivity of such agents as CRF1 receptor antagonist,309 CB1/CB2 receptor antagonist310 or somatostatin receptor agonist (octreotide),311 are yet to be confirmed in clinical trials, especially with regard to global symptoms improvement and well-being. For example, CRF1 receptor antagonists are being investigated in Phase II/III clinical trials for depression, anxiety and IBS.42 In fact, a recent clinical trial confirmed CRF1 receptor antagonist efficacy in an anxiety model in healthy participants (7.5% CO2 model).312 Some observed discrepancies between preclinical models and clinical trials may result from limited correlation between readout from animal studies being based on pseudoaffective reflex responses or unlearned behaviors and symptoms in IBS patients reflecting subjective pain experience highly modulated by cortical influences.1 As discussed in this review, the methods used to monitor visceral sensitivity in rodents by inducing some bias in the observed responses could also potentially contribute to the lack of clinical translation of some drugs.
Amelioration of animal models of visceral pain, in their construct and face validity, particularly through the development of non-invasive methods to monitor visceral sensitivity together with a recently emerging algorithm of drug screening based on pharmacological brain imaging techniques opens promising venues in establishing an adequate approach in identifying effective treatment for IBS symptoms as well as IBS-related quality of life impairment.
Acknowledgements
The authors thank Miss E. Hu for reviewing the manuscript.
Footnotes
Financial support: This review is part of studies supported by the VA Research Career Scientist Award, NIH grants R01 DK-57238 and DK 33061 and P50 DK-64539 (YT) and K01 DK088937 (ML).
Conflicts of interest: None.
References
- 1.Mayer EA, Bradesi S, Chang L, Spiegel BM, Bueller JA, Naliboff BD. Functional GI disorders: from animal models to drug development. Gut. 2008;57:384–404. doi: 10.1136/gut.2006.101675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Posserud I, Agerforz P, Ekman R, Björnsson ES, Abrahamsson H, Simrén M. Altered visceral perceptual and neuroendocrine response in patients with irritable bowel syndrome during mental stress. Gut. 2004;53:1102–1108. doi: 10.1136/gut.2003.017962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elsenbruch S, Rosenberger C, Bingel U, Forsting M, Schedlowski M, Gizewski ER. Patients with irritable bowel syndrome have altered emotional modulation of neural responses to visceral stimuli. Gastroenterology. 2010;139:1310–1319. doi: 10.1053/j.gastro.2010.06.054. [DOI] [PubMed] [Google Scholar]
- 4.Elsenbruch S, Rosenberger C, Enck P, Forsting M, Schedlowski M, Gizewski ER. Affective disturbances modulate the neural processing of visceral pain stimuli in irritable bowel syndrome: an fMRI study. Gut. 2010;59:489–495. doi: 10.1136/gut.2008.175000. [DOI] [PubMed] [Google Scholar]
- 5.Lackner JM, Brasel AM, Quigley BM, et al. The ties that bind: perceived social support, stress, and IBS in severely affected patients. Neurogastroenterol Motil. 2010;22:893–900. doi: 10.1111/j.1365-2982.2010.01516.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choung RS, Locke GR, 3rd, Zinsmeister AR, Schleck CD, Talley NJ. Psychosocial distress and somatic symptoms in community subjects with irritable bowel syndrome: a psychological component is the rule. Am J Gastroenterol. 2009;104:1772–1779. doi: 10.1038/ajg.2009.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shen L, Kong H, Hou X. Prevalence of irritable bowel syndrome and its relationship with psychological stress status in Chinese university students. J Gastroenterol Hepatol. 2009;24:1885–1890. doi: 10.1111/j.1440-1746.2009.05943.x. [DOI] [PubMed] [Google Scholar]
- 8.Blanchard EB, Lackner JM, Jaccard J, et al. The role of stress in symptom exacerbation among IBS patients. J Psychosom Res. 2008;64:119–128. doi: 10.1016/j.jpsychores.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 9.Mayer EA, Naliboff BD, Chang L, Coutinho SV. V. Stress and irritable bowel syndrome. Am J Physiol Gastrointest Liver Physiol. 2001;280:G519–G524. doi: 10.1152/ajpgi.2001.280.4.G519. [DOI] [PubMed] [Google Scholar]
- 10.Dufton LM, Konik B, Colletti R, et al. Effects of stress on pain threshold and tolerance in children with recurrent abdominal pain. Pain. 2008;136:38–43. doi: 10.1016/j.pain.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 11.Chitkara DK, van Tilburg MA, Blois-Martin N, Whitehead WE. Early life risk factors that contribute to irritable bowel syndrome in adults: a systematic review. Am J Gastroenterol. 2008;103:765–774. doi: 10.1111/j.1572-0241.2007.01722.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Videlock EJ, Adeyemo M, Licudine A, et al. Childhood trauma is associated with hypothalamic-pituitary-adrenal axis responsiveness in irritable bowel syndrome. Gastroenterology. 2009;137:1954–1962. doi: 10.1053/j.gastro.2009.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leserman J, Drossman DA. Relationship of abuse history to functional gastrointestinal disorders and symptoms: some possible mediating mechanisms. Trauma Violence Abuse. 2007;8:331–343. doi: 10.1177/1524838007303240. [DOI] [PubMed] [Google Scholar]
- 14.Gwee KA, Leong YL, Graham C, et al. The role of psychological and biological factors in postinfective gut dysfunction. Gut. 1999;44:400–406. doi: 10.1136/gut.44.3.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spiller R, Garsed K. Infection, inflammation, and the irritable bowel syndrome. Dig Liver Dis. 2009;41:844–849. doi: 10.1016/j.dld.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 16.Mulak A, Bonaz B. Irritable bowel syndrome: a model of the brain-gut interactions. Med Sci Monit. 2004;10:RA55–RA62. [PubMed] [Google Scholar]
- 17.Barreau F, Ferrier L, Fioramonti J, Bueno L. New insights in the etiology and pathophysiology of irritable bowel syndrome: contribution of neonatal stress models. Pediatr Res. 2007;62:240–245. doi: 10.1203/PDR.0b013e3180db2949. [DOI] [PubMed] [Google Scholar]
- 18.Qin HY, Wu JC, Tong XD, Sung JJ, Xu HX, Bian ZX. Systematic review of animal models of post-infectious/post-inflammatory irritable bowel syndrome. J Gastroenterol. 2011;46:164–174. doi: 10.1007/s00535-010-0321-6. [DOI] [PubMed] [Google Scholar]
- 19.Larauche M, Gourcerol G, Wang L, et al. Cortagine, a CRF1 agonist, induces stresslike alterations of colonic function and visceral hypersensitivity in rodents primarily through peripheral pathways. Am J Physiol Gastrointest Liver Physiol. 2009;297:G215–G227. doi: 10.1152/ajpgi.00072.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yarushkina NI. The role of hypothalamo-hypophyseal-adrenocortical system hormones in controlling pain sensitivity. Neurosci Behav Physiol. 2008;38:759–766. doi: 10.1007/s11055-008-9044-z. [DOI] [PubMed] [Google Scholar]
- 21.Coffin B, Bouhassira D, Sabate JM, Barbe L, Jian R. Alteration of the spinal modulation of nociceptive processing in patients with irritable bowel syndrome. Gut. 2004;53:1465–1470. doi: 10.1136/gut.2003.031310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Naliboff BD, Mayer EA. Brain imaging in IBS: drawing the line between cognitive and non-cognitive processes. Gastroenterology. 2006;130:267–270. doi: 10.1053/j.gastro.2005.11.034. [DOI] [PubMed] [Google Scholar]
- 23.Mayer EA, Naliboff BD, Craig AD. Neuroimaging of the brain-gut axis: from basic understanding to treatment of functional GI disorders. Gastroenterology. 2006;131:1925–1942. doi: 10.1053/j.gastro.2006.10.026. [DOI] [PubMed] [Google Scholar]
- 24.Lantéri-Minet M, Isnardon P, de Pommery J, Menétrey D. Spinal and hindbrain structures involved in visceroception and visceronociception as revealed by the expression of Fos, Jun and Krox-24 proteins. Neuroscience. 1993;55:737–753. doi: 10.1016/0306-4522(93)90439-m. [DOI] [PubMed] [Google Scholar]
- 25.Wang L, Martinez V, Larauche M, Taché Y. Proximal colon distension induces Fos expression in oxytocin-, vasopressin-, CRF- and catecholamines-containing neurons in rat brain. Brain Res. 2009;1247:79–91. doi: 10.1016/j.brainres.2008.09.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martinez V, Wang L, Taché Y. Proximal colon distension induces Fos expression in the brain and inhibits gastric emptying through capsaicin-sensitive pathways in conscious rats. Brain Res. 2006;1086:168–180. doi: 10.1016/j.brainres.2006.02.063. [DOI] [PubMed] [Google Scholar]
- 27.Mönnikes H, Rüter J, König M, et al. Differential induction of c-fos expression in brain nuclei by noxious and non-noxious colonic distension: role of afferent C-fibers and 5-HT3 receptors. Brain Res. 2003;966:253–264. doi: 10.1016/s0006-8993(02)04197-5. [DOI] [PubMed] [Google Scholar]
- 28.Murphy AZ, Suckow SK, Johns M, Traub RJ. Sex differences in the activation of the spinoparabrachial circuit by visceral pain. Physiol Behav. 2009;97:205–212. doi: 10.1016/j.physbeh.2009.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wu JC, Ziea ET, LAo L, et al. Effect of electroacupuncture on visceral hyperalgesia, serotonin and fos expression in an animal model of irritable bowel syndrome. J Neurogastroenterol Motil. 2010;16:306–314. doi: 10.5056/jnm.2010.16.3.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stam R, Ekkelenkamp K, Frankhuijzen AC, Bruijnzeel AW, Akkermans LM, Wiegant VM. Long-lasting changes in central nervous system responsivity to colonic distention after stress in rats. Gastroenterology. 2002;123:1216–1225. doi: 10.1053/gast.2002.36029. [DOI] [PubMed] [Google Scholar]
- 31.Traub RJ, Silva E, Gebhart GF, Solodkin A. Noxious colorectal distention induced-c-Fos protein in limbic brain structures in the rat. Neurosci Lett. 1996;215:165–168. doi: 10.1016/0304-3940(96)12978-5. [DOI] [PubMed] [Google Scholar]
- 32.Lazovic J, Wizos HF, Yang QX, et al. Regional activation in the rat brain during visceral stimulation detected by c-fos expression and fMRI. Neurogastroenterol Motil. 2005;17:548–556. doi: 10.1111/j.1365-2982.2005.00655.x. [DOI] [PubMed] [Google Scholar]
- 33.Wang Z, Bradesi S, Maarek JM, et al. Regional brain activation in conscious, nonrestrained rats in response to noxious visceral stimulation. Pain. 2008;138:233–243. doi: 10.1016/j.pain.2008.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Selye H. A syndrome produced by diverse nocuous agents. Nature. 1936;138:32. doi: 10.1176/jnp.10.2.230a. [DOI] [PubMed] [Google Scholar]
- 35.Cannon WB. Bodily Changes in Pain, Hunger, Fear and Rage: an account of recent researches into the function of emotional excitement. New York and London: D. Appleton and company; 1915. p. 311. [Google Scholar]
- 36.Chrousos GP. Stress and disorders of the stress system. Nat Rev Endocrinol. 2009;5:374–381. doi: 10.1038/nrendo.2009.106. [DOI] [PubMed] [Google Scholar]
- 37.McEwen BS. Stress, adaptation, and disease. Allostasis and allostatic load. Ann N Y Acad Sci. 1998;840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- 38.Sterling P, Eyer J. Allostasis: a new paradigm to explain arousal pathology. In: Fisher S, editor. Handbook of life stress, cognition and health. Oxford: John Wiley & Sons; 1988. pp. 629–649. [Google Scholar]
- 39.McEwen BS, Stellar E. Stress and the individual. Mechanisms leading to disease. Arch Intern Med. 1993;153:2093–2101. [PubMed] [Google Scholar]
- 40.Stengel A, Taché Y. Corticotropin-releasing factor signaling and visceral response to stress. Exp Biol Med (Maywood) 2010;235:1168–1178. doi: 10.1258/ebm.2010.009347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hauger RL, Grigoriadis DE, Dallman MF, Plotsky PM, Vale WW, Dautzenberg FM. International Union of Pharmacology. XXXVI. Current status of the nomenclature for receptors for corticotropin-releasing factor and their ligands. Pharmacol Rev. 2003;55:21–26. doi: 10.1124/pr.55.1.3. [DOI] [PubMed] [Google Scholar]
- 42.Zorrilla EP, Koob GF. Progress in corticotropin-releasing factor-1 antagonist development. Drug Discov Today. 2010;15:371–383. doi: 10.1016/j.drudis.2010.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rivier CL, Grigoriadis DE, Rivier JE. Role of corticotropin-releasing factor receptors type 1 and 2 in modulating the rat adrenocorticotropin response to stressors. Endocrinology. 2003;144:2396–2403. doi: 10.1210/en.2002-0117. [DOI] [PubMed] [Google Scholar]
- 44.Koob GF, Heinrichs SC. A role for corticotropin releasing factor and urocortin in behavioral responses to stressors. Brain Res. 1999;848:141–152. doi: 10.1016/s0006-8993(99)01991-5. [DOI] [PubMed] [Google Scholar]
- 45.Bale TL, Vale WW. CRF and CRF receptors: role in stress responsivity and other behaviors. Annu Rev Pharmacol Toxicol. 2004;44:525–557. doi: 10.1146/annurev.pharmtox.44.101802.121410. [DOI] [PubMed] [Google Scholar]
- 46.Turnbull AV, Rivier C. Corticotropin-releasing factor (CRF) and endocrine responses to stress: CRF receptors, binding protein, and related peptides. Proc Soc Exp Biol Med. 1997;215:1–10. doi: 10.3181/00379727-215-44108. [DOI] [PubMed] [Google Scholar]
- 47.Taché Y, Martinez V, Million M, Wang L. Stress and the gastrointestinal tract III. Stress-related alterations of gut motor function: role of brain corticotropin-releasing factor receptors. Am J Physiol Gastrointest Liver Physiol. 2001;280:G173–G177. doi: 10.1152/ajpgi.2001.280.2.G173. [DOI] [PubMed] [Google Scholar]
- 48.Caso JR, Leza JC, Menchen L. The effects of physical and psychological stress on the gastro-intestinal tract: lessons from animal models. Curr Mol Med. 2008;8:299–312. doi: 10.2174/156652408784533751. [DOI] [PubMed] [Google Scholar]
- 49.Friedman EM, Irwin MR. A role for CRH and the sympathetic nervous system in stress-induced immunosuppression. Ann N Y Acad Sci. 1995;771:396–418. doi: 10.1111/j.1749-6632.1995.tb44698.x. [DOI] [PubMed] [Google Scholar]
- 50.Yorimitsu M, Okada S, Yamaguchi-Shima N, Shimizu T, Arai J, Yokotani K. Role of brain adrenoceptors in the corticortopin-releasing factor-induced central activation of sympatho-adrenomedullary outflow in rats. Life Sci. 2008;82:487–494. doi: 10.1016/j.lfs.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 51.Usui D, Yamaguchi-Shima N, Okada S, Shimizu T, Wakiguchi H, Yokotani K. Selective activation of the sympathetic ganglia by centrally administered corticotropin-releasing factor in rats. Auton Neurosci. 2009;146:111–114. doi: 10.1016/j.autneu.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 52.Tsatsanis C, Dermitzaki E, Venihaki M, et al. The corticotropin-releasing factor (CRF) family of peptides as local modulators of adrenal function. Cell Mol Life Sci. 2007;64:1638–1655. doi: 10.1007/s00018-007-6555-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Valentino RJ, Foote SL, Page ME. The locus coeruleus as a site for integrating corticotropin-releasing factor and noradrenergic mediation of stress responses. Ann N Y Acad Sci. 1993;697:173–188. doi: 10.1111/j.1749-6632.1993.tb49931.x. [DOI] [PubMed] [Google Scholar]
- 54.Kosoyan HP, Wei JY, Taché Y. Intracisternal sauvagine is more potent than corticotropin-releasing factor to decrease gastric vagal efferent activity in rats. Peptides. 1999;20:851–858. doi: 10.1016/s0196-9781(99)00072-8. [DOI] [PubMed] [Google Scholar]
- 55.Wiersma A, Bohus B, Koolhaas JM. Corticotropin-releasing hormone microinfusion in the central amygdala diminishes a cardiac parasympathetic outflow under stress-free conditions. Brain Res. 1993;625:219–227. doi: 10.1016/0006-8993(93)91062-w. [DOI] [PubMed] [Google Scholar]
- 56.Friedman EM, Irwin MR. Modulation of immune cell function by the autonomic nervous system. Pharmacol Ther. 1997;74:27–38. doi: 10.1016/s0163-7258(96)00200-8. [DOI] [PubMed] [Google Scholar]
- 57.Taché Y. The parasympathetic nervous system in the pathophysiology of the gastrointestinal tract. In: Bolis CL, Licinio J, Govoni S, editors. Handbook of autonomic nervous system in health and diseases. New York: Marcel Dekker, Inc; 2002. pp. 463–503. Chapter 15. [Google Scholar]
- 58.Holsboer F, Ising M. Central CRH system in depression and anxiety - evidence from clinical studies with CRH1 receptor antagonists. Eur J Pharmacol. 2008;583:350–357. doi: 10.1016/j.ejphar.2007.12.032. [DOI] [PubMed] [Google Scholar]
- 59.Fukudo S. Role of corticotropin-releasing hormone in irritable bowel syndrome and intestinal inflammation. J Gastroenterol. 2007;42(suppl 17):48–51. doi: 10.1007/s00535-006-1942-7. [DOI] [PubMed] [Google Scholar]
- 60.Taché Y, Brunnhuber S. From Hans Selye's discovery of biological stress to the identification of corticotropin-releasing factor signaling pathways: implication in stress-related functional bowel diseases. Ann N Y Acad Sci. 2008;1148:29–41. doi: 10.1196/annals.1410.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Million M, Maillot C, Adelson DA, et al. Peripheral injection of sauvagine prevents repeated colorectal distension-induced visceral pain in female rats. Peptides. 2005;26:1188–1195. doi: 10.1016/j.peptides.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 62.Million M, Wang L, Wang Y, et al. CRF2 receptor activation prevents colorectal distension induced visceral pain and spinal ERK1/2 phosphorylation in rats. Gut. 2006;55:172–181. doi: 10.1136/gut.2004.051391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Skórzewska A, Lehner M, Hamed A, et al. The effect of CRF2 receptor antagonists on rat conditioned fear responses and c-Fos and CRF expression in the brain limbic structures. Behav Brain Res. 2011;221:155–165. doi: 10.1016/j.bbr.2011.02.036. [DOI] [PubMed] [Google Scholar]
- 64.Larauche M, Kiank C, Taché Y. Corticotropin releasing factor signaling in colon and ileum: regulation by stress and pathophysiological implications. J Physiol Pharmacol. 2009;60(suppl 7):33–46. [PMC free article] [PubMed] [Google Scholar]
- 65.Basbaum AI, Bautista DM, Scherrer G, Julius D. Cellular and molecular mechanisms of pain. Cell. 2009;139:267–284. doi: 10.1016/j.cell.2009.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sengupta JN. Visceral pain: the neurophysiological mechanism. Handb Exp Pharmacol. 2009;194:31–74. doi: 10.1007/978-3-540-79090-7_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Robinson DR, Gebhart GF. Inside information: the unique features of visceral sensation. Mol Interv. 2008;8:242–253. doi: 10.1124/mi.8.5.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Grundy D. Neuroanatomy of visceral nociception: vagal and splanchnic afferent. Gut. 2002;51(suppl 1):i2–i5. doi: 10.1136/gut.51.suppl_1.i2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Blackshaw LA, Brookes SJ, Grundy D, Schemann M. Sensory transmission in the gastrointestinal tract. Neurogastroenterol Motil. 2007;19:1–19. doi: 10.1111/j.1365-2982.2006.00871.x. [DOI] [PubMed] [Google Scholar]
- 70.Ness TJ, Fillingim RB, Randich A, Backensto EM, Faught E. Low intensity vagal nerve stimulation lowers human thermal pain thresholds. Pain. 2000;86:81–85. doi: 10.1016/s0304-3959(00)00237-2. [DOI] [PubMed] [Google Scholar]
- 71.Randich A, Gebhart GF. Vagal afferent modulation of nociception. Brain Res Brain Res Rev. 1992;17:77–99. doi: 10.1016/0165-0173(92)90009-b. [DOI] [PubMed] [Google Scholar]
- 72.Sugiura Y, Terui N, Hosoya Y, Tonosaki Y, Nishiyama K, Honda T. Quantitative analysis of central terminal projections of visceral and somatic unmyelinated (C) primary afferent fibers in the guinea pig. J Comp Neurol. 1993;332:315–325. doi: 10.1002/cne.903320305. [DOI] [PubMed] [Google Scholar]
- 73.Wang G, Tang B, Traub RJ. Differential processing of noxious colonic input by thoracolumbar and lumbosacral dorsal horn neurons in the rat. J Neurophysiol. 2005;94:3788–3794. doi: 10.1152/jn.00230.2005. [DOI] [PubMed] [Google Scholar]
- 74.Price DD. Central neural mechanisms that interrelate sensory and affective dimensions of pain. Mol Interv. 2002;2:392–403. 339. doi: 10.1124/mi.2.6.392. [DOI] [PubMed] [Google Scholar]
- 75.Heinricher MM, Tavares I, Leith JL, Lumb BM. Descending control of nociception: Specificity, recruitment and plasticity. Brain Res Rev. 2009;60:214–225. doi: 10.1016/j.brainresrev.2008.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tsuruoka M, Wang D, Tamaki J, Inoue T. Descending influence from the nucleus locus coeruleus/subcoeruleus on visceral nociceptive transmission in the rat spinal cord. Neuroscience. 2010;165:1019–1024. doi: 10.1016/j.neuroscience.2009.11.055. [DOI] [PubMed] [Google Scholar]
- 77.Zhuo M, Gebhart GF. Facilitation and attenuation of a visceral nociceptive reflex from the rostroventral medulla in the rat. Gastroenterology. 2002;122:1007–1019. doi: 10.1053/gast.2002.32389. [DOI] [PubMed] [Google Scholar]
- 78.Ness TJ, Gebhart GF. Colorectal distension as a noxious visceral stimulus: physiologic and pharmacologic characterization of pseudoaffective reflexes in the rat. Brain Res. 1988;450:153–169. doi: 10.1016/0006-8993(88)91555-7. [DOI] [PubMed] [Google Scholar]
- 79.Christianson JA, Gebhart GF. Assessment of colon sensitivity by luminal distension in mice. Nat Protoc. 2007;2:2624–2631. doi: 10.1038/nprot.2007.392. [DOI] [PubMed] [Google Scholar]
- 80.Larsson M, Arvidsson S, Ekman C, Bayati A. A model for chronic quantitative studies of colorectal sensitivity using balloon distension in conscious mice-effects of opioid receptor agonists. Neurogastroenterol Motil. 2003;15:371–381. doi: 10.1046/j.1365-2982.2003.00418.x. [DOI] [PubMed] [Google Scholar]
- 81.Bradesi S, Schwetz I, Ennes HS, et al. Repeated exposure to water avoidance stress in rats: a new model for sustained visceral hyperalgesia. Am J Physiol Gastrointest Liver Physiol. 2005;289:G42–G53. doi: 10.1152/ajpgi.00500.2004. [DOI] [PubMed] [Google Scholar]
- 82.Welting O, Van Den Wijngaard RM, De Jonge WJ, Holman R, Boeckxstaens GE. Assessment of visceral sensitivity using radio telemetry in a rat model of maternal separation. Neurogastroenterol Motil. 2005;17:838–845. doi: 10.1111/j.1365-2982.2005.00677.x. [DOI] [PubMed] [Google Scholar]
- 83.Nijsen MJ, Ongenae NG, Coulie B, Meulemans AL. Telemetric animal model to evaluate visceral pain in the freely moving rat. Pain. 2003;105:115–123. doi: 10.1016/s0304-3959(03)00170-2. [DOI] [PubMed] [Google Scholar]
- 84.Klueh U, Kreutzer DL. Murine model of implantable glucose sensors: a novel model for glucose sensor development. Diabetes Technol Ther. 2005;7:727–737. doi: 10.1089/dia.2005.7.727. [DOI] [PubMed] [Google Scholar]
- 85.Marois Y, Roy R, Vidovszky T, et al. Histopathological and immunological investigations of synthetic fibres and structures used in three prosthetic anterior cruciate ligaments: in vivo study in the rat. Biomaterials. 1993;14:255–262. doi: 10.1016/0142-9612(93)90115-i. [DOI] [PubMed] [Google Scholar]
- 86.Arvidsson S, Larsson M, Larsson H, Lindstrom E, Martinez V. Assessment of visceral pain-related pseudo-affective responses to colorectal distension in mice by intracolonic manometric recordings. J Pain. 2006;7:108–118. doi: 10.1016/j.jpain.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 87.Tammpere A, Brusberg M, Axenborg J, Hirsch I, Larsson H, Lindström E. Evaluation of pseudo-affective responses to noxious colorectal distension in rats by manometric recordings. Pain. 2005;116:220–226. doi: 10.1016/j.pain.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 88.Larauche M, Gourcerol G, Million M, Adelson DW, Taché Y. Repeated psychological stress-induced alterations of visceral sensitivity and colonic motor functions in mice: Influence of surgery and postoperative single housing on visceromotor responses. Stress. 2010;13:343–354. doi: 10.3109/10253891003664166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Al-Chaer ED, Kawasaki M, Pasricha PJ. A new model of chronic visceral hypersensitivity in adult rats induced by colon irritation during postnatal development. Gastroenterology. 2000;119:1276–1285. doi: 10.1053/gast.2000.19576. [DOI] [PubMed] [Google Scholar]
- 90.Zhang XJ, Li Z, Chung EK, et al. Activation of extracellular signal-regulated protein kinase is associated with colorectal distension-induced spinal and supraspinal neuronal response and neonatal maternal separation-induced visceral hyperalgesia in rats. J Mol Neurosci. 2009;37:274–287. doi: 10.1007/s12031-008-9134-y. [DOI] [PubMed] [Google Scholar]
- 91.Gibney SM, Gosselin RD, Dinan TG, Cryan JF. Colorectal distension-induced prefrontal cortex activation in the Wistar-Kyoto rat: implications for irritable bowel syndrome. Neuroscience. 2010;165:675–683. doi: 10.1016/j.neuroscience.2009.08.076. [DOI] [PubMed] [Google Scholar]
- 92.Ait-Belgnaoui A, Eutamene H, Houdeau E, Bueno L, Fioramonti J, Theodorou V. Lactobacillus farciminis treatment attenuates stress-induced overexpression of Fos protein in spinal and supraspinal sites after colorectal distension in rats. Neurogastroenterol Motil. 2009;21:567–569. doi: 10.1111/j.1365-2982.2009.01280.x. [DOI] [PubMed] [Google Scholar]
- 93.Johnson AC, Myers B, Lazovic J, Towner R, Greenwood-Van Meerveld B. Brain activation in response to visceral stimulation in rats with amygdala implants of corticosterone: an FMRI study. PLoS One. 2010;5:e8573. doi: 10.1371/journal.pone.0008573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Coello C, Hjornevik T, Courivaud F, Willoch F. Anatomical standardization of small animal brain FDG-PET images using synthetic functional template: Experimental comparison with anatomical template. J Neurosci Methods. 2011;199:166–172. doi: 10.1016/j.jneumeth.2011.04.026. [DOI] [PubMed] [Google Scholar]
- 95.Sawchenko PE, Li HY, Ericsson A. Circuits and mechanisms governing hypothalamic responses to stress: a tale of two paradigms. Prog Brain Res. 2000;122:61–78. doi: 10.1016/s0079-6123(08)62131-7. [DOI] [PubMed] [Google Scholar]
- 96.Herman JP, Cullinan WE. Neurocircuitry of stress: central control of the hypothalamo-pituitary-adrenocortical axis. Trends Neurosci. 1997;20:78–84. doi: 10.1016/s0166-2236(96)10069-2. [DOI] [PubMed] [Google Scholar]
- 97.Mayer EA, Collins SM. Evolving pathophysiologic models of functional gastrointestinal disorders. Gastroenterology. 2002;122:2032–2048. doi: 10.1053/gast.2002.33584. [DOI] [PubMed] [Google Scholar]
- 98.Rosenberger C, Elsenbruch S, Scholle A, et al. Effects of psychological stress on the cerebral processing of visceral stimuli in healthy women. Neurogastroenterol Motil. 2009;21:740-e45. doi: 10.1111/j.1365-2982.2009.01295.x. [DOI] [PubMed] [Google Scholar]
- 99.Elsenbruch S. Abdominal pain in irritable bowel syndrome: a review of putative psychological, neural and neuro-immune mechanisms. Brain Behav Immun. 2011;25:386–394. doi: 10.1016/j.bbi.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 100.Bouin M, Plourde V, Boivin M, et al. Rectal distention testing in patients with irritable bowel syndrome: sensitivity, specificity, and predictive values of pain sensory thresholds. Gastroenterology. 2002;122:1771–1777. doi: 10.1053/gast.2002.33601. [DOI] [PubMed] [Google Scholar]
- 101.Hotoleanu C, Popp R, Trifa AP, Nedelcu L, Dumitrascu DL. Genetic determination of irritable bowel syndrome. World J Gastroenterol. 2008;14:6636–6640. doi: 10.3748/wjg.14.6636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Camilleri M. Genetics and irritable bowel syndrome: from genomics to intermediate phenotype and pharmacogenetics. Dig Dis Sci. 2009;54:2318–2324. doi: 10.1007/s10620-009-0903-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zucchelli M, Camilleri M, Nixon Andreasson A, et al. Association of TNFSF15 polymorphism with irritable bowel syndrome. Gut. doi: 10.1136/gut.2011.241877. Published Online First: 2 June 2011. doi: 10.1136/gut.2011.241877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Markoutsaki T, Karantanos T, Gazouli M, Anagnou NP, Ladas SD, Karamanolis DG. Serotonin transporter and G protein beta 3 subunit gene polymorphisms in Greeks with irritable bowel syndrome. Dig Dis Sci. doi: 10.1007/s10620-011-1726-7. Published Online First: 11 May 2011. doi: 10.1007/s10620-011-1726-7. [DOI] [PubMed] [Google Scholar]
- 105.Vazquez-Roque MI, Camilleri M, Carlson P, et al. HLA-DQ genotype is associated with accelerated small bowel transit in patients with diarrhea-predominant irritable bowel syndrome. Eur J Gastroenterol Hepatol. 2011;23:481–487. doi: 10.1097/MEG.0b013e328346a56e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Dinan TG, Cryan J, Shanahan F, Keeling PW, Quigley EM. IBS: An epigenetic perspective. Nat Rev Gastroenterol Hepatol. 2010;7:465–471. doi: 10.1038/nrgastro.2010.99. [DOI] [PubMed] [Google Scholar]
- 107.Wu HH, Wang S. Strain differences in the chronic mild stress animal model of depression. Behav Brain Res. 2010;213:94–102. doi: 10.1016/j.bbr.2010.04.041. [DOI] [PubMed] [Google Scholar]
- 108.Porterfield VM, Zimomra ZR, Caldwell EA, Camp RM, Gabella KM, Johnson JD. Rat strain differences in restraint stress-induced brain cytokines. Neuroscience. 2011;188:48–54. doi: 10.1016/j.neuroscience.2011.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.O'Mahony CM, Clarke G, Gibney S, Dinan TG, Cryan JF. Strain differences in the neurochemical response to chronic restraint stress in the rat: relevance to depression. Pharmacol Biochem Behav. 2011;97:690–699. doi: 10.1016/j.pbb.2010.11.012. [DOI] [PubMed] [Google Scholar]
- 110.Shepard JD, Myers DA. Strain differences in anxiety-like behavior: association with corticotropin-releasing factor. Behav Brain Res. 2008;186:239–245. doi: 10.1016/j.bbr.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 111.Gunter WD, Shepard JD, Foreman RD, Myers DA, Greenwood-Van Meerveld B. Evidence for visceral hypersensitivity in high-anxiety rats. Physiol Behav. 2000;69:379–382. doi: 10.1016/s0031-9384(99)00254-1. [DOI] [PubMed] [Google Scholar]
- 112.Meaney MJ, Szyf M, Seckl JR. Epigenetic mechanisms of perinatal programming of hypothalamic-pituitary-adrenal function and health. Trends Mol Med. 2007;13:269–277. doi: 10.1016/j.molmed.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 113.Sudo N, Chida Y, Aiba Y, et al. Postnatal microbial colonization programs the hypothalamic-pituitary-adrenal system for stress response in mice. J Physiol. 2004;558:263–275. doi: 10.1113/jphysiol.2004.063388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.O'Mahony SM, Hyland NP, Dinan TG, Cryan JF. Maternal separation as a model of brain-gut axis dysfunction. Psychopharmacology (Berl) 2011;214:71–88. doi: 10.1007/s00213-010-2010-9. [DOI] [PubMed] [Google Scholar]
- 115.Rosztóczy A, Fioramonti J, Jarmay K, Barreau F, Wittmann T, Buéno L. Influence of sex and experimental protocol on the effect of maternal deprivation on rectal sensitivity to distension in the adult rat. Neurogastroenterol Motil. 2003;15:679–686. doi: 10.1046/j.1350-1925.2003.00451.x. [DOI] [PubMed] [Google Scholar]
- 116.Plotsky PM, Meaney MJ. Early, postnatal experience alters hypothalamic corticotropin-releasing factor (CRF) mRNA, median eminence CRF content and stress-induced release in adult rats. Brain Res Mol Brain Res. 1993;18:195–200. doi: 10.1016/0169-328x(93)90189-v. [DOI] [PubMed] [Google Scholar]
- 117.Coutinho SV, Plotsky PM, Sablad M, et al. Neonatal maternal separation alters stress-induced responses to viscerosomatic nociceptive stimuli in rat. Am J Physiol Gastrointest Liver Physiol. 2002;282:G307–G316. doi: 10.1152/ajpgi.00240.2001. [DOI] [PubMed] [Google Scholar]
- 118.Barreau F, Cartier C, Ferrier L, Fioramonti J, Bueno L. Nerve growth factor mediates alterations of colonic sensitivity and mucosal barrier induced by neonatal stress in rats. Gastroenterology. 2004;127:524–534. doi: 10.1053/j.gastro.2004.05.019. [DOI] [PubMed] [Google Scholar]
- 119.Lin C, Al-Chaer ED. Long-term sensitization of primary afferents in adult rats exposed to neonatal colon pain. Brain Res. 2003;971:73–82. doi: 10.1016/s0006-8993(03)02358-8. [DOI] [PubMed] [Google Scholar]
- 120.Wang G, Ji Y, Lidow MS, Traub RJ. Neonatal hind paw injury alters processing of visceral and somatic nociceptive stimuli in the adult rat. J Pain. 2004;5:440–449. doi: 10.1016/j.jpain.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 121.LaPrairie JL, Murphy AZ. Long-term impact of neonatal injury in male and female rats: Sex differences, mechanisms and clinical implications. Front Neuroendocrinol. 2010;31:193–202. doi: 10.1016/j.yfrne.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.LaPrairie JL, Murphy AZ. Neonatal injury alters adult pain sensitivity by increasing opioid tone in the periaqueductal gray. Front Behav Neurosci. 2009;3:31. doi: 10.3389/neuro.08.031.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Bonaz B, Taché Y. Water-avoidance stress-induced c-fos expression in the rat brain and stimulation of fecal output: role of corticotropin-releasing factor. Brain Res. 1994;641:21–28. doi: 10.1016/0006-8993(94)91810-4. [DOI] [PubMed] [Google Scholar]
- 124.Enck P, Merlin V, Erckenbrecht JF, Wienbeck M. Stress effects on gastrointestinal transit in the rat. Gut. 1989;30:455–459. doi: 10.1136/gut.30.4.455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Eutamene H, Bradesi S, Larauche M, et al. Guanylate cyclase C-mediated antinociceptive effects of linaclotide in rodent models of visceral pain. Neurogastroenterol Motil. 2010;22:312-e84. doi: 10.1111/j.1365-2982.2009.01385.x. [DOI] [PubMed] [Google Scholar]
- 126.Schwetz I, Bradesi S, McRoberts JA, et al. Delayed stress-induced colonic hypersensitivity in male Wistar rats: role of neurokinin-1 and corticotropin-releasing factor-1 receptors. Am J Physiol Gastrointest Liver Physiol. 2004;286:G683–G691. doi: 10.1152/ajpgi.00358.2003. [DOI] [PubMed] [Google Scholar]
- 127.Gué M, Del Rio-Lacheze C, Eutamene H, Théodorou V, Fioramonti J, Buéno L. Stress-induced visceral hypersensitivity to rectal distension in rats: role of CRF and mast cells. Neurogastroenterol Motil. 1997;9:271–279. doi: 10.1046/j.1365-2982.1997.d01-63.x. [DOI] [PubMed] [Google Scholar]
- 128.Chang L. Review article: epidemiology and quality of life in functional gastrointestinal disorders. Aliment Pharmacol Ther. 2004;20(suppl 7):31–39. doi: 10.1111/j.1365-2036.2004.02183.x. [DOI] [PubMed] [Google Scholar]
- 129.Bennett EJ, Tennant CC, Piesse C, Badcock CA, Kellow JE. Level of chronic life stress predicts clinical outcome in irritable bowel syndrome. Gut. 1998;43:256–261. doi: 10.1136/gut.43.2.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Hong S, Fan J, Kemmerer ES, Evans S, Li Y, Wiley JW. Reciprocal changes in vanilloid (TRPV1) and endocannabinoid (CB1) receptors contribute to visceral hyperalgesia in the water avoidance stressed rat. Gut. 2009;58:202–210. doi: 10.1136/gut.2008.157594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Larauche M, Bradesi S, Million M, et al. Corticotropin-releasing factor type 1 receptors mediate the visceral hyperalgesia induced by repeated psychological stress in rats. Am J Physiol Gastrointest Liver Physiol. 2008;294:G1033–G1040. doi: 10.1152/ajpgi.00507.2007. [DOI] [PubMed] [Google Scholar]
- 132.Larauche M, Mulak A, Kim YS, Million M, Taché Y. Sex differences in visceral sensitivity induced by repeated psychological stress in rats: differential role of opioid pathway. Gut. 2010;59:A104. [Google Scholar]
- 133.Larauche M, Mulak A, Yuan P-Q, Kanauchi O, Taché Y. Stress-induced visceral analgesia assessed non-invasively in rats is enhanced by prebiotic. World J Gastroenterol. 2011 doi: 10.3748/wjg.v18.i3.225. (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Green PG, Alvarez P, Gear RW, Mendoza D, Levine JD. Further validation of a model of fibromyalgia syndrome in the rat. J Pain. doi: 10.1016/j.jpain.2011.01.006. Published Online First: 8 Apr 2011. doi: 10.1016/j.jpain.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zheng J, Babygirija R, Bülbül M, Cerjak D, Ludwig K, Takahashi T. Hypothalamic oxytocin mediates adaptation mechanism against chronic stress in rats. Am J Physiol Gastrointest Liver Physiol. 2010;299:G946–G953. doi: 10.1152/ajpgi.00483.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Patel S, Hillard CJ. Adaptations in endocannabinoid signaling in response to repeated homotypic stress: a novel mechanism for stress habituation. Eur J Neurosci. 2008;27:2821–2829. doi: 10.1111/j.1460-9568.2008.06266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Winston JH, Xu GY, Sarna SK. Adrenergic stimulation mediates visceral hypersensitivity to colorectal distension following heterotypic chronic stress. Gastroenterology. 2010;138:294–304. doi: 10.1053/j.gastro.2009.09.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Savas LS, White DL, Wieman M, et al. Irritable bowel syndrome and dyspepsia among women veterans: prevalence and association with psychological distress. Aliment Pharmacol Ther. 2009;29:115–125. doi: 10.1111/j.1365-2036.2008.03847.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.White DL, Savas LS, Daci K, et al. Trauma history and risk of the irritable bowel syndrome in women veterans. Aliment Pharmacol Ther. 2010;32:551–561. doi: 10.1111/j.1365-2036.2010.04387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Cohen H, Jotkowitz A, Buskila D, et al. Post-traumatic stress disorder and other co-morbidities in a sample population of patients with irritable bowel syndrome. Eur J Intern Med. 2006;17:567–571. doi: 10.1016/j.ejim.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 141.Irwin C, Falsetti SA, Lydiard RB, Ballenger JC, Brock CD, Brener W. Comorbidity of posttraumatic stress disorder and irritable bowel syndrome. J Clin Psychiatry. 1996;57:576–578. doi: 10.4088/jcp.v57n1204. [DOI] [PubMed] [Google Scholar]
- 142.Drossman DA, Leserman J, Nachman G, et al. Sexual and physical abuse in women with functional or organic gastrointestinal disorders. Ann Intern Med. 1990;113:828–833. doi: 10.7326/0003-4819-113-11-828. [DOI] [PubMed] [Google Scholar]
- 143.Klooker TK, Braak B, Painter RC, et al. Exposure to severe wartime conditions in early life is associated with an increased risk of irritable bowel syndrome: a population-based cohort study. Am J Gastroenterol. 2009;104:2250–2256. doi: 10.1038/ajg.2009.282. [DOI] [PubMed] [Google Scholar]
- 144.Yehuda R, Schmeidler J, Labinsky E, et al. Ten-year follow-up study of PTSD diagnosis, symptom severity and psychosocial indices in aging holocaust survivors. Acta Psychiatr Scand. 2009;119:25–34. doi: 10.1111/j.1600-0447.2008.01248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Stam R, Akkermans LM, Wiegant VM. Trauma and the gut: interactions between stressful experience and intestinal function. Gut. 1997;40:704–709. doi: 10.1136/gut.40.6.704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Stam R. PTSD and stress sensitisation: a tale of brain and body Part 2: animal models. Neurosci Biobehav Rev. 2007;31:558–584. doi: 10.1016/j.neubiorev.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 147.Wang W, Liu Y, Zheng H, et al. A modified single-prolonged stress model for post-traumatic stress disorder. Neurosci Lett. 2008;441:237–241. doi: 10.1016/j.neulet.2008.06.031. [DOI] [PubMed] [Google Scholar]
- 148.Rau V, DeCola JP, Fanselow MS. Stress-induced enhancement of fear learning: an animal model of posttraumatic stress disorder. Neurosci Biobehav Rev. 2005;29:1207–1223. doi: 10.1016/j.neubiorev.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 149.Stam R, van Laar TJ, Akkermans LM, Wiegant VM. Variability factors in the expression of stress-induced behavioural sensitisation. Behav Brain Res. 2002;132:69–76. doi: 10.1016/s0166-4328(01)00387-4. [DOI] [PubMed] [Google Scholar]
- 150.Collins SM, Vallance B, Barbara G, Borgaonkar M. Putative inflammatory and immunological mechanisms in functional bowel disorders. Baillieres Best Pract Res Clin Gastroenterol. 1999;13:429–436. doi: 10.1053/bega.1999.0037. [DOI] [PubMed] [Google Scholar]
- 151.Spiller RC. Postinfectious irritable bowel syndrome. Gastroenterology. 2003;124:1662–1671. doi: 10.1016/s0016-5085(03)00324-x. [DOI] [PubMed] [Google Scholar]
- 152.Spiller R, Garsed K. Postinfectious irritable bowel syndrome. Gastroenterology. 2009;136:1979–1988. doi: 10.1053/j.gastro.2009.02.074. [DOI] [PubMed] [Google Scholar]
- 153.Long Y, Liu Y, Tong J, Qian W, Hou X. Effectiveness of trimebutine maleate on modulating intestinal hypercontractility in a mouse model of postinfectious irritable bowel syndrome. Eur J Pharmacol. 2010;636:159–165. doi: 10.1016/j.ejphar.2010.03.037. [DOI] [PubMed] [Google Scholar]
- 154.Bercik P, Wang L, Verdú EF, et al. Visceral hyperalgesia and intestinal dysmotility in a mouse model of postinfective gut dysfunction. Gastroenterology. 2004;127:179–187. doi: 10.1053/j.gastro.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 155.McLean PG, Picard C, Garcia-Villar R, Moré J, Fioramonti J, Buéno L. Effects of nematode infection on sensitivity to intestinal distension: role of tachykinin NK2 receptors. Eur J Pharmacol. 1997;337:279–282. doi: 10.1016/s0014-2999(97)01275-2. [DOI] [PubMed] [Google Scholar]
- 156.Vergnolle N. Postinflammatory visceral sensitivity and pain mechanisms. Neurogastroenterol Motil. 2008;20(suppl 1):73–80. doi: 10.1111/j.1365-2982.2008.01110.x. [DOI] [PubMed] [Google Scholar]
- 157.Keohane J, O'Mahony C, O'Mahony L, O'Mahony S, Quigley EM, Shanahan F. Irritable bowel syndrome-type symptoms in patients with inflammatory bowel disease: a real association or reflection of occult inflammation? Am J Gastroenterol. 2010;105:1788, 1789–1794. doi: 10.1038/ajg.2010.156. [DOI] [PubMed] [Google Scholar]
- 158.Long MD, Drossman DA. Inflammatory bowel disease, irritable bowel syndrome, or what?: a challenge to the functional-organic dichotomy. Am J Gastroenterol. 2010;105:1796–1798. doi: 10.1038/ajg.2010.162. [DOI] [PubMed] [Google Scholar]
- 159.Van Hoboken EA, Thijssen AY, Verhaaren R, et al. Symptoms in patients with ulcerative colitis in remission are associated with visceral hypersensitivity and mast cell activity. Scand J Gastroenterol. doi: 10.3109/00365521.2011.579156. Published Online First: 30 May 2011. doi: 10.3109/00365521.2011.579156. [DOI] [PubMed] [Google Scholar]
- 160.Burton MB, Gebhart GF. Effects of intracolonic acetic acid on responses to colorectal distension in the rat. Brain Res. 1995;672:77–82. doi: 10.1016/0006-8993(94)01382-r. [DOI] [PubMed] [Google Scholar]
- 161.Palecek J, Willis WD. The dorsal column pathway facilitates visceromotor responses to colorectal distention after colon inflammation in rats. Pain. 2003;104:501–507. doi: 10.1016/S0304-3959(03)00075-7. [DOI] [PubMed] [Google Scholar]
- 162.Ji Y, Tang B, Traub RJ. Modulatory effects of estrogen and progesterone on colorectal hyperalgesia in the rat. Pain. 2005;117:433–442. doi: 10.1016/j.pain.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 163.Traub RJ, Murphy A. Colonic inflammation induces fos expression in the thoracolumbar spinal cord increasing activity in the spinoparabrachial pathway. Pain. 2002;95:93–102. doi: 10.1016/s0304-3959(01)00381-5. [DOI] [PubMed] [Google Scholar]
- 164.Coutinho SV, Meller ST, Gebhart GF. Intracolonic zymosan produces visceral hyperalgesia in the rat that is mediated by spinal NMDA and non-NMDA receptors. Brain Res. 1996;736:7–15. doi: 10.1016/0006-8993(96)00661-0. [DOI] [PubMed] [Google Scholar]
- 165.Gschossmann JM, Liebregts T, Adam B, et al. Long-term effects of transient chemically induced colitis on the visceromotor response to mechanical colorectal distension. Dig Dis Sci. 2004;49:96–101. doi: 10.1023/b:ddas.0000011609.68882.3a. [DOI] [PubMed] [Google Scholar]
- 166.Adam B, Liebregts T, Gschossmann JM, et al. Severity of mucosal inflammation as a predictor for alterations of visceral sensory function in a rat model. Pain. 2006;123:179–186. doi: 10.1016/j.pain.2006.02.029. [DOI] [PubMed] [Google Scholar]
- 167.Zhou Q, Price DD, Caudle RM, Verne GN. Visceral and somatic hypersensitivity in a subset of rats following TNBS-induced colitis. Pain. 2008;134:9–15. doi: 10.1016/j.pain.2007.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Traub RJ, Tang B, Ji Y, Pandya S, Yfantis H, Sun Y. A rat model of chronic postinflammatory visceral pain induced by deoxycholic acid. Gastroenterology. 2008;135:2075–2083. doi: 10.1053/j.gastro.2008.08.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Verma-Gandhu M, Verdu EF, Bercik P, et al. Visceral pain perception is determined by the duration of colitis and associated neuropeptide expression in the mouse. Gut. 2007;56:358–364. doi: 10.1136/gut.2006.100016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Larsson MH, Rapp L, Lindström E. Effect of DSS-induced colitis on visceral sensitivity to colorectal distension in mice. Neurogastroenterol Motil. 2006;18:144–152. doi: 10.1111/j.1365-2982.2005.00736.x. [DOI] [PubMed] [Google Scholar]
- 171.Wlodarska M, Willing B, Keeney KM, et al. Antibiotic treatment alters the colonic mucus layer and predisposes the host to exacerbated Citrobacter rodentium-induced colitis. Infect Immun. 2011;79:1536–1545. doi: 10.1128/IAI.01104-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Mendall MA, Kumar D. Antibiotic use, childhood affluence and irritable bowel syndrome (IBS) Eur J Gastroenterol Hepatol. 1998;10:59–62. doi: 10.1097/00042737-199801000-00011. [DOI] [PubMed] [Google Scholar]
- 173.Verdú EF, Bercik P, Verma-Gandhu M, et al. Specific probiotic therapy attenuates antibiotic induced visceral hypersensitivity in mice. Gut. 2006;55:182–190. doi: 10.1136/gut.2005.066100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Pimentel M, Chatterjee S, Chow EJ, Park S, Kong Y. Neomycin improves constipation-predominant irritable bowel syndrome in a fashion that is dependent on the presence of methane gas: subanalysis of a double-blind randomized controlled study. Dig Dis Sci. 2006;51:1297–1301. doi: 10.1007/s10620-006-9104-6. [DOI] [PubMed] [Google Scholar]
- 175.Pimentel M, Lembo A, Chey WD, et al. Rifaximin therapy for patients with irritable bowel syndrome without constipation. N Engl J Med. 2011;364:22–32. doi: 10.1056/NEJMoa1004409. [DOI] [PubMed] [Google Scholar]
- 176.Pimentel M, Morales W, Chua K, et al. Effects of Rifaximin Treatment and Retreatment in Nonconstipated IBS Subjects. Dig Dis Sci. 2011;56:2067–2072. doi: 10.1007/s10620-011-1728-5. [DOI] [PubMed] [Google Scholar]
- 177.Salonen A, de Vos WM, Palva A. Gastrointestinal microbiota in irritable bowel syndrome: present state and perspectives. Microbiology. 2010;156(Pt 11):3205–3215. doi: 10.1099/mic.0.043257-0. [DOI] [PubMed] [Google Scholar]
- 178.Minocha A, Johnson WD, Wigington WC. Prevalence of abdominal and pelvic surgeries in patients with irritable bowel syndrome: comparison between Caucasian and African Americans. Am J Med Sci. 2008;335:82–88. doi: 10.1097/MAJ.0b013e31815879ac. [DOI] [PubMed] [Google Scholar]
- 179.Li S, Yu Y, Prakash R. Possible pathogenetic roles of abdominal surgery in irritable bowel syndrome. Med Hypotheses. 2011;76:497–499. doi: 10.1016/j.mehy.2010.11.034. [DOI] [PubMed] [Google Scholar]
- 180.Miranda A, Peles S, Rudolph C, Shaker R, Sengupta JN. Altered visceral sensation in response to somatic pain in the rat. Gastroenterology. 2004;126:1082–1089. doi: 10.1053/j.gastro.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 181.Cameron DM, Brennan TJ, Gebhart GF. Hind paw incision in the rat produces long-lasting colon hypersensitivity. J Pain. 2008;9:246–253. doi: 10.1016/j.jpain.2007.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Whitehead WE, Palsson O, Jones KR. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: what are the causes and implications? Gastroenterology. 2002;122:1140–1156. doi: 10.1053/gast.2002.32392. [DOI] [PubMed] [Google Scholar]
- 183.Pang X, Boucher W, Triadafilopoulos G, Sant GR, Theoharides TC. Mast cell and substance P-positive nerve involvement in a patient with both irritable bowel syndrome and interstitial cystitis. Urology. 1996;47:436–438. doi: 10.1016/S0090-4295(99)80469-5. [DOI] [PubMed] [Google Scholar]
- 184.Peters KM, Killinger KA, Ibrahim IA. Childhood symptoms and events in women with interstitial cystitis/painful bladder syndrome. Urology. 2009;73:258–262. doi: 10.1016/j.urology.2008.09.014. [DOI] [PubMed] [Google Scholar]
- 185.Pezzone MA, Liang R, Fraser MO. A model of neural cross-talk and irritation in the pelvis: implications for the overlap of chronic pelvic pain disorders. Gastroenterology. 2005;128:1953–1964. doi: 10.1053/j.gastro.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 186.Miranda A, Mickle A, Schmidt J, et al. Neonatal cystitis-induced colonic hypersensitivity in adult rats: a model of viscero-visceral convergence. Neurogastroenterol Motil. 2011;23:683-e281. doi: 10.1111/j.1365-2982.2011.01724.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Van Oudenhove L, Coen SJ, Aziz Q. Functional brain imaging of gastrointestinal sensation in health and disease. World J Gastroenterol. 2007;13:3438–3445. doi: 10.3748/wjg.v13.i25.3438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Seminowicz DA, Mikulis DJ, Davis KD. Cognitive modulation of pain-related brain responses depends on behavioral strategy. Pain. 2004;112:48–58. doi: 10.1016/j.pain.2004.07.027. [DOI] [PubMed] [Google Scholar]
- 189.Mayer EA, Tillisch K. The brain-gut axis in abdominal pain syndromes. Annu Rev Med. 2011;62:381–396. doi: 10.1146/annurev-med-012309-103958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Jarrett ME, Burr RL, Cain KC, Hertig V, Weisman P, Heitkemper MM. Anxiety and depression are related to autonomic nervous system function in women with irritable bowel syndrome. Dig Dis Sci. 2003;48:386–394. doi: 10.1023/a:1021904216312. [DOI] [PubMed] [Google Scholar]
- 191.Tougas G. The autonomic nervous system in functional bowel disorders. Gut. 2000;47(suppl 4):iv78–iv80. doi: 10.1136/gut.47.suppl_4.iv78. discussion iv 87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Keita AV, Söderholm JD. The intestinal barrier and its regulation by neuroimmune factors. Neurogastroenterol Motil. 2010;22:718–733. doi: 10.1111/j.1365-2982.2010.01498.x. [DOI] [PubMed] [Google Scholar]
- 193.Bravo JA, Dinan TG, Cryan JF. Alterations in the central CRF system of two different rat models of comorbid depression and functional gastrointestinal disorders. Int J Neuropsychopharmacol. 2011;14:666–683. doi: 10.1017/S1461145710000994. [DOI] [PubMed] [Google Scholar]
- 194.Lemos JC, Zhang G, Walsh T, et al. Stress-hyperresponsive WKY rats demonstrate depressed dorsal raphe neuronal excitability and dysregulated CRF-mediated responses. Neuropsychopharmacology. 2011;36:721–734. doi: 10.1038/npp.2010.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Overstreet DH, Djuric V. A genetic rat model of cholinergic hypersensitivity: implications for chemical intolerance, chronic fatigue, and asthma. Ann N Y Acad Sci. 2001;933:92–102. doi: 10.1111/j.1749-6632.2001.tb05816.x. [DOI] [PubMed] [Google Scholar]
- 196.Overstreet DH. The Flinders sensitive line rats: a genetic animal model of depression. Neurosci Biobehav Rev. 1993;17:51–68. doi: 10.1016/s0149-7634(05)80230-1. [DOI] [PubMed] [Google Scholar]
- 197.Elsenbruch S, Wang L, Hollerbach S, Schedlowski M, Tougas G. Pseudo-affective visceromotor responses and HPA axis activation following colorectal distension in rats with increased cholinergic sensitivity. Neurogastroenterol Motil. 2004;16:801–809. doi: 10.1111/j.1365-2982.2004.00563.x. [DOI] [PubMed] [Google Scholar]
- 198.Trimble N, Johnson AC, Foster A, Greenwood-van Meerveld B. Corticotropin-releasing factor receptor 1-deficient mice show decreased anxiety and colonic sensitivity. Neurogastroenterol Motil. 2007;19:754–760. doi: 10.1111/j.1365-2982.2007.00951.x. [DOI] [PubMed] [Google Scholar]
- 199.Million M, Wang L, Stenzel-Poore MP, et al. Enhanced pelvic responses to stressors in female CRF-overexpressing mice. Am J Physiol Regul Integr Comp Physiol. 2007;292:R1429–R1438. doi: 10.1152/ajpregu.00626.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Stenzel-Poore MP, Cameron VA, Vaughan J, Sawchenko PE, Vale W. Development of Cushing's syndrome in corticotropin-releasing factor transgenic mice. Endocrinology. 1992;130:3378–3386. doi: 10.1210/endo.130.6.1597149. [DOI] [PubMed] [Google Scholar]
- 201.Kimura M, Müller-Preuss P, Lu A, et al. Conditional corticotropin-releasing hormone overexpression in the mouse forebrain enhances rapid eye movement sleep. Mol Psychiatry. 2010;15:154–165. doi: 10.1038/mp.2009.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Lu A, Steiner MA, Whittle N, et al. Conditional mouse mutants highlight mechanisms of corticotropin-releasing hormone effects on stress-coping behavior. Mol Psychiatry. 2008;13:1028–1042. doi: 10.1038/mp.2008.51. [DOI] [PubMed] [Google Scholar]
- 203.Bakshi VP, Kalin NH. Corticotropin-releasing hormone and animal models of anxiety: gene-environment interactions. Biol Psychiatry. 2000;48:1175–1198. doi: 10.1016/s0006-3223(00)01082-9. [DOI] [PubMed] [Google Scholar]
- 204.Kolber BJ, Bovle MP, Wieczorek L, et al. Transient early-life forebrain corticotropin-releasing hormone elevation causes long-lasting anxiogenic and despair-like changes in mice. J Neurosci. 2010;30:2571–2581. doi: 10.1523/JNEUROSCI.4470-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Deussing JM, Wurst W. Dissecting the genetic effect of the CRH system on anxiety and stress-related behaviour. C R Biol. 2005;328:199–212. doi: 10.1016/j.crvi.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 206.Delic S, Streif S, Deussing JM, et al. Genetic mouse models for behavioral analysis through transgenic RNAi technology. Genes Brain Behav. 2008;7:821–830. doi: 10.1111/j.1601-183X.2008.00412.x. [DOI] [PubMed] [Google Scholar]
- 207.Butler RK, Finn DP. Stress-induced analgesia. Prog Neurobiol. 2009;88:184–202. doi: 10.1016/j.pneurobio.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 208.Gui X, Carraway RE, Dobner PR. Endogenous neurotensin facilitates visceral nociception and is required for stress-induced antinociception in mice and rats. Neuroscience. 2004;126:1023–1032. doi: 10.1016/j.neuroscience.2004.04.034. [DOI] [PubMed] [Google Scholar]
- 209.Schwetz I, McRoberts JA, Coutinho SV, et al. Corticotropin-releasing factor receptor 1 mediates acute and delayed stress-induced visceral hyperalgesia in maternally separated Long-Evans rats. Am J Physiol Gastrointest Liver Physiol. 2005;289:G704–G712. doi: 10.1152/ajpgi.00498.2004. [DOI] [PubMed] [Google Scholar]
- 210.Rivat C, Laboureyras E, Laulin JP, Le RC, Richebe P, Simonnet G. Non-nociceptive environmental stress induces hyperalgesia, not analgesia, in pain and opioid-experienced rats. Neuropsychopharmacology. 2007;32:2217–2228. doi: 10.1038/sj.npp.1301340. [DOI] [PubMed] [Google Scholar]
- 211.Berman SM, Naliboff BD, Suyenobu B, et al. Reduced brainstem inhibition during anticipated pelvic visceral pain correlates with enhanced brain response to the visceral stimulus in women with irritable bowel syndrome. J Neurosci. 2008;28:349–359. doi: 10.1523/JNEUROSCI.2500-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Piche M, Arsenault M, Poitras P, Rainville P, Bouin M. Widespread hypersensitivity is related to altered pain inhibition processes in irritable bowel syndrome. Pain. 2010;148:49–58. doi: 10.1016/j.pain.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 213.Song GH, Venkatraman V, Ho KY, Chee MW, Yeoh KG, Wilder-Smith CH. Cortical effects of anticipation and endogenous modulation of visceral pain assessed by functional brain MRI in irritable bowel syndrome patients and healthy controls. Pain. 2006;126:79–90. doi: 10.1016/j.pain.2006.06.017. [DOI] [PubMed] [Google Scholar]
- 214.Wilder-Smith CH, Schindler D, Lovblad K, Redmond SM, Nirkko A. Brain functional magnetic resonance imaging of rectal pain and activation of endogenous inhibitory mechanisms in irritable bowel syndrome patient subgroups and healthy controls. Gut. 2004;53:1595–1601. doi: 10.1136/gut.2003.028514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Heitkemper MM, Chang L. Do fluctuations in ovarian hormones affect gastrointestinal symptoms in women with irritable bowel syndrome? Gend Med. 2009;6(suppl 2):152–167. doi: 10.1016/j.genm.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Adeyemo MA, Spiegel BM, Chang L. Meta-analysis: do irritable bowel syndrome symptoms vary between men and women? Aliment Pharmacol Ther. 2010;32:738–755. doi: 10.1111/j.1365-2036.2010.04409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL., 3rd Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain. 2009;10:447–485. doi: 10.1016/j.jpain.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Mulak A, Taché Y. Sex difference in irritable bowel syndrome: do gonadal hormones play a role? Gastroenterol Pol. 2010;17:89–97. [PMC free article] [PubMed] [Google Scholar]
- 219.Koch KM, Palmer JL, Noordin N, Tomlinson JJ, Baidoo C. Sex and age differences in the pharmacokinetics of alosetron. Br J Clin Pharmacol. 2002;53:238–242. doi: 10.1046/j.0306-5251.2001.01565.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Taché Y, Million M, Nelson AG, Lamy C, Wang L. Role of corticotropin-releasing factor pathways in stress-related alterations of colonic motor function and viscerosensibility in female rodents. Gend Med. 2005;2:146–154. doi: 10.1016/s1550-8579(05)80043-9. [DOI] [PubMed] [Google Scholar]
- 221.Aloisi AM, Affaitati G, Ceccarelli I, et al. Estradiol and testosterone differently affect visceral pain-related behavioural responses in male and female rats. Eur J Pain. 2010;14:602–607. doi: 10.1016/j.ejpain.2009.10.016. [DOI] [PubMed] [Google Scholar]
- 222.Ji Y, Tang B, Traub RJ. The visceromotor response to colorectal distention fluctuates with the estrous cycle in rats. Neuroscience. 2008;154:1562–1567. doi: 10.1016/j.neuroscience.2008.04.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Holdcroft A, Sapsed-Byrne S, Ma D, Hammal D, Forsling ML. Sex and oestrous cycle differences in visceromotor responses and vasopressin release in response to colonic distension in male and female rats anaesthetized with halothane. Br J Anaesth. 2000;85:907–910. doi: 10.1093/bja/85.6.907. [DOI] [PubMed] [Google Scholar]
- 224.Sapsed-Byrne S, Ma D, Ridout D, Holdcroft A. Estrous cycle phase variations in visceromotor and cardiovascular responses to colonic distension in the anesthetized rat. Brain Res. 1996;742:10–16. doi: 10.1016/s0006-8993(96)00989-4. [DOI] [PubMed] [Google Scholar]
- 225.Ouyang A, Wrzos HF. Contribution of gender to pathophysiology and clinical presentation of IBS: should management be different in women? Am J Gastroenterol. 2006;101(12 Suppl):S602–S609. doi: 10.1111/j.1572-0241.2006.00975.x. [DOI] [PubMed] [Google Scholar]
- 226.Azpiroz F, Bouin M, Camilleri M, et al. Mechanisms of hypersensitivity in IBS and functional disorders. Neurogastroenterol Motil. 2007;19(1 Suppl):62–88. doi: 10.1111/j.1365-2982.2006.00875.x. [DOI] [PubMed] [Google Scholar]
- 227.Lembo T, Plourde V, Shui Z, et al. Effects of the corticotropin-releasing factor (CRF) on rectal afferent nerves in humans. Neurogastroenterol Motil. 1996;8:9–18. doi: 10.1111/j.1365-2982.1996.tb00237.x. [DOI] [PubMed] [Google Scholar]
- 228.Nozu T, Kudaira M. Corticotropin-releasing factor induces rectal hypersensitivity after repetitive painful rectal distention in healthy humans. J Gastroenterol. 2006;41:740–744. doi: 10.1007/s00535-006-1848-4. [DOI] [PubMed] [Google Scholar]
- 229.Sagami Y, Shimada Y, Tayama J, et al. Effect of a corticotropin releasing hormone receptor antagonist on colonic sensory and motor function in patients with irritable bowel syndrome. Gut. 2004;53:958–964. doi: 10.1136/gut.2003.018911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Tayama J, Sagami Y, Shimada Y, Hongo M, Fukudo S. Effect of alpha-helical CRH on quantitative electroencephalogram in patients with irritable bowel syndrome. Neurogastroenterol Motil. 2007;19:471–483. doi: 10.1111/j.1365-2982.2007.00903.x. [DOI] [PubMed] [Google Scholar]
- 231.La JH, Sung TS, Kim HJ, Kim TW, Kang TM, Yang IS. Peripheral corticotropin releasing hormone mediates post-inflammatory visceral hypersensitivity in rats. World J Gastroenterol. 2008;14:731–736. doi: 10.3748/wjg.14.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Barreau F, Cartier C, Leveque M, et al. Pathways involved in gut mucosal barrier dysfunction induced in adult rats by maternal deprivation: corticotrophin-releasing factor and nerve growth factor interplay. J Physiol. 2007;580(Pt 1):347–356. doi: 10.1113/jphysiol.2006.120907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Wallon C, Yang PC, Keita AV, et al. Corticotropin-releasing hormone (CRH) regulates macromolecular permeability via mast cells in normal human colonic biopsies in vitro. Gut. 2008;57:50–58. doi: 10.1136/gut.2006.117549. [DOI] [PubMed] [Google Scholar]
- 234.Barbara G, Wang B, Stanghellini V, et al. Mast cell-dependent excitation of visceral-nociceptive sensory neurons in irritable bowel syndrome. Gastroenterology. 2007;132:26–37. doi: 10.1053/j.gastro.2006.11.039. [DOI] [PubMed] [Google Scholar]
- 235.Van den Wijngaard RM, Klooker TK, de Jonge WJ, Boeckxstaens GE. Peripheral relays in stress-induced activation of visceral afferents in the gut. Auton Neurosci. 2010;153:99–105. doi: 10.1016/j.autneu.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 236.Cenac N, Andrews CN, Holzhausen M, et al. Role for protease activity in visceral pain in irritable bowel syndrome. J Clin Invest. 2007;117:636–647. doi: 10.1172/JCI29255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Gold MS, Zhang L, Wrigley DL, Traub RJ. Prostaglandin E(2) modulates TTX-R I(Na) in rat colonic sensory neurons. J Neurophysiol. 2002;88:1512–1522. doi: 10.1152/jn.2002.88.3.1512. [DOI] [PubMed] [Google Scholar]
- 238.Van den Wijngaard RM, Kooker TK, Welting O, et al. Essential role for TRPV1 in stress-induced (mast cell-dependent) colonic hypersensitivity in maternally separated rats. Neurogastroenterol Motil. 2009;21:1107-e94. doi: 10.1111/j.1365-2982.2009.01339.x. [DOI] [PubMed] [Google Scholar]
- 239.Holzer P. Gastrointestinal afferents as targets of novel drugs for the treatment of functional bowel disorders and visceral pain. Eur J Pharmacol. 2001;429:177–193. doi: 10.1016/s0014-2999(01)01319-x. [DOI] [PubMed] [Google Scholar]
- 240.Jones RC, 3rd, Xu L, Gebhart GF. The mechanosensitivity of mouse colon afferent fibers and their sensitization by inflammatory mediators require transient receptor potential vanilloid 1 and acid-sensing ion channel 3. J Neurosci. 2005;25:10981–10989. doi: 10.1523/JNEUROSCI.0703-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Cregg R, Momin A, Rugiero F, Wood JN, Zhao J. Pain channelopathies. J Physiol. 2010;588(Pt 11):1897–1904. doi: 10.1113/jphysiol.2010.187807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.McRoberts JA, Coutinho SV, Marvizón JC, et al. Role of peripheral N-methyl-D-aspartate (NMDA) receptors in visceral nociception in rats. Gastroenterology. 2001;120:1737–1748. doi: 10.1053/gast.2001.24848. [DOI] [PubMed] [Google Scholar]
- 243.Yu YB, Yang J, Zuo XL, Gao LJ, Wang P, Li YQ. Transient receptor potential vanilloid-1 (TRPV1) and ankyrin-1 (TRPA1) participate in visceral hyperalgesia in chronic water avoidance stress rat model. Neurochem Res. 2010;35:797–803. doi: 10.1007/s11064-010-0137-z. [DOI] [PubMed] [Google Scholar]
- 244.Winston J, Shenoy M, Medley D, Naniwadekar A, Pasricha PJ. The vanilloid receptor initiates and maintains colonic hypersensitivity induced by neonatal colon irritation in rats. Gastroenterology. 2007;132:615–627. doi: 10.1053/j.gastro.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 245.Ravnefjord A, Brusberg M, Kang D, et al. Involvement of the transient receptor potential vanilloid 1 (TRPV1) in the development of acute visceral hyperalgesia during colorectal distension in rats. Eur J Pharmacol. 2009;611:85–91. doi: 10.1016/j.ejphar.2009.03.058. [DOI] [PubMed] [Google Scholar]
- 246.Piche T, Barbara G, Aubert P, et al. Impaired intestinal barrier integrity in the colon of patients with irritable bowel syndrome: involvement of soluble mediators. Gut. 2009;58:196–201. doi: 10.1136/gut.2007.140806. [DOI] [PubMed] [Google Scholar]
- 247.Ait-Belgnaoui A, Bradesi S, Fioramonti J, Theodorou V, Bueno L. Acute stress-induced hypersensitivity to colonic distension depends upon increase in paracellular permeability: role of myosin light chain kinase. Pain. 2005;113:141–147. doi: 10.1016/j.pain.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 248.Zhou Q, Zhang B, Verne GN. Intestinal membrane permeability and hypersensitivity in the irritable bowel syndrome. Pain. 2009;146:41–46. doi: 10.1016/j.pain.2009.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Santos J, Yang PC, Söderholm JD, Benjamin M, Perdue MH. Role of mast cells in chronic stress induced colonic epithelial barrier dysfunction in the rat. Gut. 2001;48:630–636. doi: 10.1136/gut.48.5.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Söderholm JD, Yang PC, Ceponis P, et al. Chronic stress induces mast cell-dependent bacterial adherence and initiates mucosal inflammation in rat intestine. Gastroenterology. 2002;123:1099–1108. doi: 10.1053/gast.2002.36019. [DOI] [PubMed] [Google Scholar]
- 251.Yu LC, Perdue MH. Role of mast cells in intestinal mucosal function: studies in models of hypersensitivity and stress. Immunol Rev. 2001;179:61–73. doi: 10.1034/j.1600-065x.2001.790107.x. [DOI] [PubMed] [Google Scholar]
- 252.Vicario M, Guilarte M, Alonso C, et al. Chronological assessment of mast cell-mediated gut dysfunction and mucosal inflammation in a rat model of chronic psychosocial stress. Brain Behav Immun. 2010;24:1166–1175. doi: 10.1016/j.bbi.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 253.Demaude J, Salvador-Cartier C, Fioramonti J, Ferrier L, Bueno L. Phenotypic changes in colonocytes following acute stress or activation of mast cells in mice: implications for delayed epithelial barrier dysfunction. Gut. 2006;55:655–661. doi: 10.1136/gut.2005.078675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Bailey MT, Dowd SE, Galley JD, Hufnagle AR, Allen RG, Lyte M. Exposure to a social stressor alters the structure of the intestinal microbiota: Implications for stressor-induced immunomodulation. Brain Behav Immun. 2011;25:397–407. doi: 10.1016/j.bbi.2010.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Bailey MT, Dowd SE, Parry NM, Galley JD, Schauer DB, Lyte M. Stressor exposure disrupts commensal microbial populations in the intestines and leads to increased colonization by Citrobacter rodentium. Infect Immun. 2010;78:1509–1519. doi: 10.1128/IAI.00862-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.O'Mahony SM, Marchesi JR, Scully P, et al. Early life stress alters behavior, immunity, and microbiota in rats: implications for irritable bowel syndrome and psychiatric illnesses. Biol Psychiatry. 2009;65:263–267. doi: 10.1016/j.biopsych.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 257.Cryan JF, O'Mahony SM. The microbiome-gut-brain axis: from bowel to behavior. Neurogastroenterol Motil. 2011;23:187–192. doi: 10.1111/j.1365-2982.2010.01664.x. [DOI] [PubMed] [Google Scholar]
- 258.Bercik P. The microbiota-gut-brain axis: learning from intestinal bacteria? Gut. 2011;60:288–289. doi: 10.1136/gut.2010.226779. [DOI] [PubMed] [Google Scholar]
- 259.Heijtz RD, Wang S, Anuar F, et al. Normal gut microbiota modulates brain development and behavior. Proc Natl Acad Sci U S A. 2011;108:3047–3052. doi: 10.1073/pnas.1010529108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Rhee SH, Pothoulakis C, Mayer EA. Principles and clinical implications of the brain-gut-enteric microbiota axis. Nat Rev Gastroenterol Hepatol. 2009;6:306–314. doi: 10.1038/nrgastro.2009.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Collins SM, Bercik P. The relationship between intestinal microbiota and the central nervous system in normal gastrointestinal function and disease. Gastroenterology. 2009;136:2003–2014. doi: 10.1053/j.gastro.2009.01.075. [DOI] [PubMed] [Google Scholar]
- 262.Chung EK, Zhang XJ, Xu HX, Sung JJ, Bian ZX. Visceral hyperalgesia induced by neonatal maternal separation is associated with nerve growth factor-mediated central neuronal plasticity in rat spinal cord. Neuroscience. 2007;149:685–695. doi: 10.1016/j.neuroscience.2007.07.055. [DOI] [PubMed] [Google Scholar]
- 263.Chung EK, Bian ZX, Xu HX, Sung JJ. Neonatal maternal separation increases brain-derived neurotrophic factor and tyrosine kinase receptor B expression in the descending pain modulatory system. Neurosignals. 2009;17:213–221. doi: 10.1159/000224631. [DOI] [PubMed] [Google Scholar]
- 264.Matricon J, Gelot A, Etienne M, Lazdunski M, Muller E, Ardid D. Spinal cord plasticity and acid-sensing ion channels involvement in a rodent model of irritable bowel syndrome. Eur J Pain. 2011;15:335–343. doi: 10.1016/j.ejpain.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 265.Gaudreau GA, Plourde V. Role of tachykinin NK1, NK2 and NK3 receptors in the modulation of visceral hypersensitivity in the rat. Neurosci Lett. 2003;351:59–62. doi: 10.1016/s0304-3940(03)00414-2. [DOI] [PubMed] [Google Scholar]
- 266.Bradesi S, Kokkotou E, Simeonidis S, et al. The role of neurokinin 1 receptors in the maintenance of visceral hyperalgesia induced by repeated stress in rats. Gastroenterology. 2006;130:1729–1742. doi: 10.1053/j.gastro.2006.01.037. [DOI] [PubMed] [Google Scholar]
- 267.Bradesi S, Svensson CI, Steinauer J, Pothoulakis C, Yaksh TL, Mayer EA. Role of spinal microglia in visceral hyperalgesia and NK1R up-regulation in a rat model of chronic stress. Gastroenterology. 2009;136:1339–1348. e1–e2. doi: 10.1053/j.gastro.2008.12.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Bradesi S. Role of spinal cord glia in the central processing of peripheral pain perception. Neurogastroenterol Motil. 2010;22:499–511. doi: 10.1111/j.1365-2982.2010.01491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Saab CY, Park YC, Al-Chaer ED. Thalamic modulation of visceral nociceptive processing in adult rats with neonatal colon irritation. Brain Res. 2004;1008:186–192. doi: 10.1016/j.brainres.2004.01.083. [DOI] [PubMed] [Google Scholar]
- 270.Bradesi S, Svensson CI, Steinauer J, Pothoulakis C, Yaksh TL, Mayer EA. Role of spinal microglia activation in visceral hyperalgesia following chronic psychological stress in Wistar rats. Gastroenterology. 2009;136:1339–1348. doi: 10.1053/j.gastro.2008.12.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Liaw WJ, Stephens RL, Jr, Binns BC, et al. Spinal glutamate uptake is critical for maintaining normal sensory transmission in rat spinal cord. Pain. 2005;115:60–70. doi: 10.1016/j.pain.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 272.Lin Y, Tian G, Roman K, et al. Increased glial glutamate transporter EAAT2 expression reduces visceral nociceptive response in mice. Am J Physiol Gastrointest Liver Physiol. 2009;296:G129–G134. doi: 10.1152/ajpgi.90556.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Svensson CI, Hua XY, Protter AA, Powell HC, Yaksh TL. Spinal p38 MAP kinase is necessary for NMDA-induced spinal PGE(2) release and thermal hyperalgesia. Neuroreport. 2003;14:1153–1157. doi: 10.1097/00001756-200306110-00010. [DOI] [PubMed] [Google Scholar]
- 274.Gosselin RD, O'Connor RM, Tramullas M, Julio-Pieper M, Dinan TG, Cryan JF. Riluzole normalizes early-life stress-induced visceral hypersensitivity in rats: role of spinal glutamate reuptake mechanisms. Gastroenterology. 2010;138:2418–2425. doi: 10.1053/j.gastro.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 275.Tjong YW, Ip SP, Lao L, et al. Neonatal maternal separation elevates thalamic corticotrophin releasing factor type 1 receptor expression response to colonic distension in rat. Neuro Endocrinol Lett. 2010;31:215–220. [PubMed] [Google Scholar]
- 276.Tillisch K, Mayer EA, Labus JS. Quantitative meta-analysis identifies brain regions activated during rectal distension in irritable bowel syndrome. Gastroenterology. 2011;140:91–100. doi: 10.1053/j.gastro.2010.07.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Zhang R, Zou N, Li J, et al. Elevated expression of c-fos in central nervous system correlates with visceral hypersensitivity in irritable bowel syndrome (IBS): a new target for IBS treatment. Int J Colorectal Dis. doi: 10.1007/s00384-011-1153-4. Published Online First: 22 Feb 2011. doi: 10.1016/j.expneurol.2011.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Chang L. Brain responses to visceral and somatic stimuli in irritable bowel syndrome: a central nervous system disorder? Gastroenterol Clin North Am. 2005;34:271–279. doi: 10.1016/j.gtc.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 279.Dayas CV, Buller KM, Crane JW, Xu Y, Day TA. Stressor categorization: acute physical and psychological stressors elicit distinctive recruitment patterns in the amygdala and in medullary noradrenergic cell groups. Eur J Neurosci. 2001;14:1143–1152. doi: 10.1046/j.0953-816x.2001.01733.x. [DOI] [PubMed] [Google Scholar]
- 280.Greenwood-Van Meerveld B, Gibson M, Gunter W, Shepard J, Foreman R, Myers D. Stereotaxic delivery of corticosterone to the amygdala modulates colonic sensitivity in rats. Brain Res. 2001;893:135–142. doi: 10.1016/s0006-8993(00)03305-9. [DOI] [PubMed] [Google Scholar]
- 281.Myers B, Dittmeyer K, Greenwood-Van MB. Involvement of amygdaloid corticosterone in altered visceral and somatic sensation. Behav Brain Res. 2007;181:163–167. doi: 10.1016/j.bbr.2007.03.031. [DOI] [PubMed] [Google Scholar]
- 282.Myers B, Greenwood-Van Meerveld B. Corticosteroid receptor-mediated mechanisms in the amygdala regulate anxiety and colonic sensitivity. Am J Physiol Gastrointest Liver Physiol. 2007;292:G1622–G1629. doi: 10.1152/ajpgi.00080.2007. [DOI] [PubMed] [Google Scholar]
- 283.Kim SH, Han JE, Hwang S, Oh DH. The expression of corticotropin-releasing factor in the central nucleus of the amygdala, induced by colorectal distension, is attenuated by general anesthesia. J Korean Med Sci. 2010;25:1646–1651. doi: 10.3346/jkms.2010.25.11.1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Nishii H, Nomura M, Aono H, Fujimoto N, Matsumoto T. Up-regulation of galanin and corticotropin-releasing hormone mRNAs in the key hypothalamic and amygdaloid nuclei in a mouse model of visceral pain. Regul Pept. 2007;141:105–112. doi: 10.1016/j.regpep.2006.12.022. [DOI] [PubMed] [Google Scholar]
- 285.Kosoyan HP, Grigoriadis DE, Taché Y. The CRF(1) receptor antagonist, NBI-35965, abolished the activation of locus coeruleus neurons induced by colorectal distension and intracisternal CRF in rats. Brain Res. 2005;1056:85–96. doi: 10.1016/j.brainres.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 286.Curtis AL, Pavcovich LA, Grigoriadis DE, Valentino RJ. Previous stress alters corticotropin-releasing factor neurotransmission in the locus coeruleus. Neuroscience. 1995;65:541–550. doi: 10.1016/0306-4522(94)00496-r. [DOI] [PubMed] [Google Scholar]
- 287.Lechner SM, Curtis AL, Brons R, Valentino RJ. Locus coeruleus activation by colon distention: role of corticotropin-releasing factor and excitatory amino acids. Brain Res. 1997;756:114–124. doi: 10.1016/s0006-8993(97)00116-9. [DOI] [PubMed] [Google Scholar]
- 288.Rouzade-Dominguez ML, Curtis AL, Valentino RJ. Role of Barrington's nucleus in the activation of rat locus coeruleus neurons by colonic distension. Brain Res. 2001;917:206–218. doi: 10.1016/s0006-8993(01)02917-1. [DOI] [PubMed] [Google Scholar]
- 289.Reyes BA, Glaser JD, Van Bockstaele EJ. Ultrastructural evidence for co-localization of corticotropin-releasing factor receptor and mu-opioid receptor in the rat nucleus locus coeruleus. Neurosci Lett. 2007;413:216–221. doi: 10.1016/j.neulet.2006.11.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Reyes BA, Valentino RJ, Van Bockstaele EJ. Stress-induced intracellular trafficking of corticotropin-releasing factor receptors in rat locus coeruleus neurons. Endocrinology. 2008;149:122–130. doi: 10.1210/en.2007-0705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Valentino RJ, Miselis RR, Pavcovich LA. Pontine regulation of pelvic viscera: pharmacological target for pelvic visceral dysfunctions. Trends Pharmacol Sci. 1999;20:253–260. doi: 10.1016/s0165-6147(99)01332-2. [DOI] [PubMed] [Google Scholar]
- 292.Kuner R. Central mechanisms of pathological pain. Nat Med. 2010;16:1258–1266. doi: 10.1038/nm.2231. [DOI] [PubMed] [Google Scholar]
- 293.Cheong E, Lee S, Choi BJ, Sun M, Lee CJ, Shin HS. Tuning thalamic firing modes via simultaneous modulation of T- and L-type Ca2+ channels controls pain sensory gating in the thalamus. J Neurosci. 2008;28:13331–13340. doi: 10.1523/JNEUROSCI.3013-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Ren Y, Zhang L, Lu Y, Yang H, Westlund KN. Central lateral thalamic neurons receive noxious visceral mechanical and chemical input in rats. J Neurophysiol. 2009;102:244–258. doi: 10.1152/jn.90985.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Zhuo M, Gebhart GF. Facilitation and attenuation of a visceral nociceptive reflex from the rostroventral medulla in the rat. Gastroenterology. 2002;122:1007–1019. doi: 10.1053/gast.2002.32389. [DOI] [PubMed] [Google Scholar]
- 296.Sanoja R, Tortorici V, Fernandez C, Price TJ, Cervero F. Role of RVM neurons in capsaicin-evoked visceral nociception and referred hyperalgesia. Eur J Pain. 2010;14:120.e1–120.e9. doi: 10.1016/j.ejpain.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Martenson ME, Cetas JS, Heinricher MM. A possible neural basis for stress-induced hyperalgesia. Pain. 2009;142:236–244. doi: 10.1016/j.pain.2009.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Kearney DJ, Brown-Chang J. Complementary and alternative medicine for IBS in adults: mind-body interventions. Nat Clin Pract Gastroenterol Hepatol. 2008;5:624–636. doi: 10.1038/ncpgasthep1257. [DOI] [PubMed] [Google Scholar]
- 299.Palsson OS, Drossman DA. Psychiatric and psychological dysfunction in irritable bowel syndrome and the role of psychological treatments. Gastroenterol Clin North Am. 2005;34:281–303. doi: 10.1016/j.gtc.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 300.Whorwell PJ. Behavioral therapy for IBS. Nat Clin Pract Gastroenterol Hepatol. 2009;6:148–149. doi: 10.1038/ncpgasthep1361. [DOI] [PubMed] [Google Scholar]
- 301.Blanchard EB, Lackner JM, Sanders K, et al. A controlled evaluation of group cognitive therapy in the treatment of irritable bowel syndrome. Behav Res Ther. 2007;45:633–648. doi: 10.1016/j.brat.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 302.Warnock JK, Clayton AH. Chronic episodic disorders in women. Psychiatr Clin North Am. 2003;26:725–740. doi: 10.1016/s0193-953x(03)00042-x. [DOI] [PubMed] [Google Scholar]
- 303.Verdu B, Decosterd I, Buclin T, Stiefel F, Berney A. Antidepressants for the treatment of chronic pain. Drugs. 2008;68:2611–2632. doi: 10.2165/0003495-200868180-00007. [DOI] [PubMed] [Google Scholar]
- 304.Larauche M, Mulak A, Taché Y. Stress and visceral pain: from animal models to clinical therapies. Exp Neurol. doi: 10.1016/j.expneurol.2011.04.020. Published Online First: 6 May 2011. doi: 10.1016/j.expneurol.2011.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Camilleri M, Andresen V. Current and novel therapeutic options for irritable bowel syndrome management. Dig Liver Dis. 2009;41:854–862. doi: 10.1016/j.dld.2009.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Million M, Wang L, Adelson DW, Roman F, Diop L, Taché Y. Pregabalin decreases visceral pain and prevents spinal neuronal activation in rats. Gut. 2007;56:1482–1484. doi: 10.1136/gut.2007.129304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Camilleri M. Review article: new receptor targets for medical therapy in irritable bowel syndrome. Aliment Pharmacol Ther. 2010;31:35–46. doi: 10.1111/j.1365-2036.2009.04153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Collins SM, Denou E, Verdu EF, Bercik P. The putative role of the intestinal microbiota in the irritable bowel syndrome. Dig Liver Dis. 2009;41:850–853. doi: 10.1016/j.dld.2009.07.023. [DOI] [PubMed] [Google Scholar]
- 309.Dukes GE, Mayer EA, Kelleher DL, Hicks KJ, Boardley RL, Alpers DH. A randomized, double blind, placebo (PLA) controlled, crossover study to evaluate the efficacy and safety of the corticotropin releasing factor 1 (CRF1) receptor antagonist (RA) GW876008 in irritable bowel syndrome (IBS) patients (Pts) Neurogastroenterol Motil. 2009;21(suppl 1):84. [Google Scholar]
- 310.Klooker TK, Leliefeld KE, van den Wijngaard RM, Boeckxstaens GE. The cannabinoid receptor agonist delta-9-tetrahydrocannabinol does not affect visceral sensitivity to rectal distension in healthy volunteers and IBS patients. Neurogastroenterol Motil. 2011;23:30–35. e2. doi: 10.1111/j.1365-2982.2010.01587.x. [DOI] [PubMed] [Google Scholar]
- 311.Klooker TK, Kuiken SD, Lei A, Boeckxstaens GE. Effect of long-term treatment with octreotide on rectal sensitivity in patients with non-constipated irritable bowel syndrome. Aliment Pharmacol Ther. 2007;26:605–615. doi: 10.1111/j.1365-2036.2007.03398.x. [DOI] [PubMed] [Google Scholar]
- 312.Bailey JE, Papadopoulos A, Diaper A, et al. Preliminary evidence of anxiolytic effects of the CRF1 receptor antagonist R317573 in the 7.5% CO2 proof-of-concept experimental model of human anxiety. J Psychopharmacol. doi: 10.1177/0269881111400650. Published Online First: 9 May 2011. doi: 10.1177/0269881111400650. [DOI] [PubMed] [Google Scholar]