Abstract
Dyspepsia is a syndrome consisting of epigastric pain, burning, fullness, discomfort, early satiety, nausea, vomiting and belching. Functional dyspepsia (FD) is diagnosed if upper gastrointestinal endoscopy does not show structural abnormality explaining these symptoms. 8%-30% and 8%-23% of Asian people suffer from of uninvestigated dyspepsia and FD, respectively. Most patients with uninvestigated dyspepsia are found to have FD. Patients with FD are usually young and there is no predilection to any gender. Overlap of FD with other functional bowel diseases such as irritable bowel syndrome and gastroesophageal reflux disease is common in Asia. Cultural difference in reporting of symptoms of dyspepsia is well-known. Moreover, dietary factors, socio-cultural and psychological issues, gastrointestinal infection including that caused by Helicobacter pylori, frequency of organic diseases such as peptic ulcer and gastric cancer responsible for dyspeptic symptoms in the study population may also influence epidemiology of dyspepsia. There is considerable heterogeneity in the above issues among different Asian countries. More studies on epidemiology of FD are needed in Asia.
Keywords: Dyspepsia, Gastroparesis, Gastrointestinal disease, Helicobacter pylori, Quality of life
Introduction
Dyspepsia refers to a combination of upper gut symptoms such as epigastric pain, burning, fullness, discomfort, early satiety, nausea, vomiting and belching. Cultural difference in reporting of symptoms of dyspepsia is well known. Moreover, dietary factors, socio-cultural and psychological issues, gastrointestinal (GI) infection including that caused by Helicobacter pylori, frequency of organic diseases such as peptic ulcer and gastric cancer responsible for dyspeptic symptoms in the study population may also influence epidemiology of dyspepsia. Since there is considerable heterogeneity in the above issues among different Asian countries, it is important to review the epidemiology of dyspepsia in Asia.
Patients having chronic dyspeptic symptoms for the past 3 months with onset at least 6 months before diagnosis in absence of structural abnormality on upper GI endoscopy and metabolic or systemic causes explaining the symptoms are classified as functional dyspepsia (FD).1 It was previously termed non-ulcer dyspepsia, or idiopathic dyspepsia. Dyspepsia is a common condition in clinical practice and in the community.2 FD is not associated with any increase in mortality. However, its impact on patients and health care services has been shown to be considerable.2
Frequency of Uninvestigated and Functional Dyspepsia in Asia
The frequency of uninvestigated dyspepsia (UD) and FD vary considerably in different populations. Such differences might be related to, (1) true difference in frequency of the condition, (2) criteria used to diagnose it and (3) degree of meticulousness to exclude organic causes. Though the data on UD in general and FD in particular are somewhat scanty from Asia, quite a few studies from Asian countries explored the epidemiology of these conditions. These data will be reviewed in this paper.
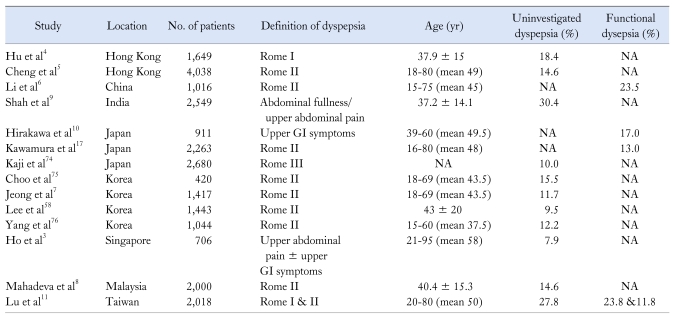
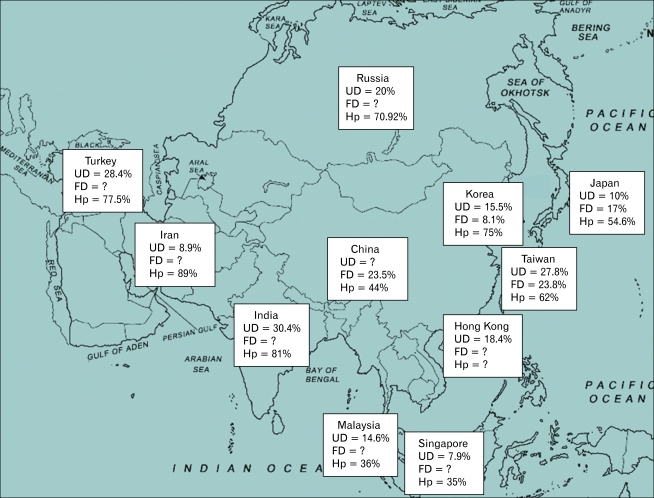
Frequency of UD and FD varied between 8%-30% and 8%-23%, respectively in Asia (Tables 1 and 2, Figure). However, the frequency of FD is not known in several countries as esophagogastroduodenoscopy (EGD) has not been done in most community studies.
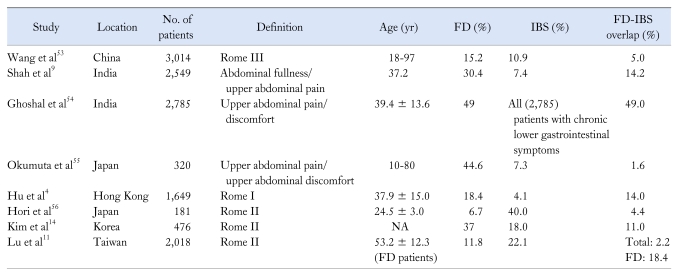
Table 1.
Summary of Studies on Uninvestigated and Functional Dyspepsia in Asia
GI, gastrointestinal.
Table 2.
Summary of Studies on Functional Dyspepsia in Asia
Figure.
It shows the prevalence of uninvestigated dyspepsia, functional dyspepsia and seroprevalence of Helicobacter pylori infection in different Asian countries. Both population-based studies and institutional studies were included. UD, uninvestigated dyspepsia; FD, functional dyspepsia; Hp, Helicobacter pylori. For references, refer to Tables 1 and 2.
Frequency of UD in a cross-sectional community study from Singapore was 53 of 696 (7.9%) respondents when dyspepsia was defined as upper abdominal pain.3 In a study from Hong Kong, of 1,649 Chinese subjects completing a survey, 304 (18.4%) had dyspepsia using Rome I criteria.4 In another cross-sectional study from Hong Kong, 4,038 subjects were surveyed for dyspepsia using Rome II criteria. The frequency of dyspepsia was found to be 14.6%.5 In a population-based study from China, of 1,016 subjects interviewed, 23.5% had dyspepsia using Rome II criteria.6 Studies from other Asian countries such as Korea and Malaysia reported frequency of UD to be approximately 14% by Rome II criteria.7,8 Data on UD and FD from India are scanty. In a community study from Mumbai city, 30.4% had dyspepsia defined as epigastric pain or discomfort in a door to door survey of 2,549 subjects.9 In a prospective study on 1,139 subjects undergoing annual medical check-up for gastric cancers from June 1997 to April 1998 in a Japanese center, 228 were excluded (124 had structural abnormalities on EGD like ulcers, cancer and polyps and 104 abnormal abdominal ultrasonography or serum biochemical tests); of the remaining 911 subjects (512 males), 17% had epigastric pain with normal EGD.10
Criteria used to diagnose dyspepsia may influence its prevalence. In a study on Chinese people residing in Taiwan,11 of 2,018 respondents, 561 subjects (27.8%) reported dyspeptic symptoms; of those 561 subjects, 80 (14.3%) had structural abnormalities (gastric ulcer in 25, duodenal ulcer in 33, reflux esophagitis in 15, both gastric and duodenal ulcers in 6, and both gastric ulcer and reflux esophagitis in 1) on EGD. The frequency of FD was 23.8% using Rome I criteria and 11.8% using Rome II criteria, respectively. Unfortunately, the community studies available from Asian countries used different criteria to diagnose UD. Hence, it is difficult to conclude whether difference in prevalence of dyspepsia shown in these studies truly reflect difference in frequency of this condition in different countries or is related to criteria used to diagnose the condition.
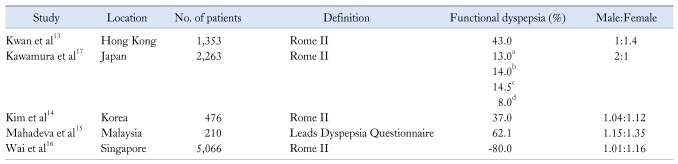
Frequency of Functional Dyspepsia in Patients Visiting Hospital in Asia
Most patients with UD are found to have FD in Asia. In a study from Shanghai, China, of 782 patients older than 18 years with dyspeptic symptoms, 69% had FD and 31% had organic causes.12 In another study from Hong Kong on 1,115 patients with uninvestigated functional gastrointestinal diseases (FGIDs, Rome II criteria) attending 14 medical clinics from 9 regions of Asia (China, Hong Kong, Indonesia, Korea, Malaysia, Singapore, Taiwan, Thailand and Vietnam), 43% had FD after investigations.13 In a Korean study on patients referred to gastroenterologist of a tertiary hospital, 332 were diagnosed as FGIDs using Rome II criteria and 90 had organic causes on endoscopic examination.14 In a prospective study from Malaysia on 210 young patients with UD (age 30 ± 8 years), 62% were diagnosed as having FD by Leads dyspepsia questionnaires (8 item symptoms).15 In a study from Singapore, of 5,066 dyspeptic patients (defined as pain and discomfort centered in the upper abdomen), organic causes for dyspepsia were found in 988 patients and the remaining 79.5% had FD.16
Older patients with UD in Asia are more likely to have organic causes than younger people. In a study on 2,500 people visiting Shimane Institute of Health Science, Shimane, Japan undergoing annual medical check-ups, 13% had FD by Rome II criteria. Frequency of FD was lower in people older than 50 years (P < 0.05).17
Validity of Rome II and III Criteria for Functional Dyspepsia
Validation of Rome II criteria for FGIDs by factor analysis had been done among Asian patients.13 An English version of Talley's bowel disease questionnaire was developed with the help of various research teams according Rome II criteria. This questionnaire was translated into different local languages in nine Asian regions: China, Hong Kong, Indonesia, Korea, Malaysia, Singapore, Taiwan, Thailand and Vietnam. Factor analysis of symptoms from a sample of these 1,012 Asian patients with functional GI disorders supported the use of Rome II classification. Another validation study of Rome II criteria for FGIDs in Korean population had been done in 274 patients visiting hospital.18 81.2% patients satisfied Rome II criteria for FGIDs. This study showed that Rome II criteria could be applied to Korean patients with FGIDs. Rome III criteria for FGIDs in Korean population had been validated.19 Using the Rome III questionnaires, prevalence of dyspepsia was found 13.4% in community subjects. 47% of these FD patients were classified as postprandial distress syndrome, 26% as epigastric pain syndrome and 27% as overlapping condition. Sensitivity and specificity of Rome III criteria in discriminating FGIDs from organic diseases of the upper GI tract was 60% and 53%, respectively.
Risk Factors Associated With Uninvestigated Dyspepsia
Gender
Several population-based studies from Asia showed that frequency of UD was not related to gender (Table 3), except one Japanese study that showed a male preponderance.17
Table 3.
Summary of Studies Showing Gender Distribution of Patients With Functional Dyspepsia in Asia
Percentage of people with functional dyspepsia in the age groups a≤ 29-year, between b30 to 39-year, c40 to 49-year and d≥ 50-year.
Age
Most Asian studies failed to show occurrence of UD in any particular age group (Table 1). However, an Indian study on 2,549 community subjects (age range 13-80 years, mean age 37.2, SD = 14.1) in Mumbai city, India, UD was commoner in older subjects (401/1,143 [35%] above and 373/1,407 [26.5%] subjects below 40 years of age; P = 0.00003).9 FD is more common in younger age group. A study from Japan reported that prevalence of FD was 13% and 8% in age groups below and above 50 years, respectively.17
Infection
Gastric H. pylori infection may be associated with dyspeptic symptoms.15,20-29 One GI peptide hormone named ghrelin (secreted from oxyntic glands) stimulates gastric motility and food intake.30,31 Patients with H. pylori may have reduction in ghrelin secretion that may reduce gastric motility causing symptoms of dyspepsia particularly symptoms of post-prandial distress syndrome.32-34 Eradication of H. pylori has been shown to improve dyspeptic symptoms.35-44 Enteric infection caused by bacteria and protozoa such as Giardia lamblia may be followed by development of post-infectious irritable bowel syndrome (IBS) and FD.45 Though GI infection is common in several developing countries of Asia, there is limited data on post-infectious FD from world in general and Asia in particular. In a study from Pakistan, patients with giardiasis reported dyspeptic symptoms.46 In a study from Japan47 on 615 industrial workers, 345 had H. pylori infection by 13C-urea breath test. 220 of 345 H. pylori-infected workers had dyspeptic symptoms (215 of whom had normal EGD); in contrast, 148 of 270 H. pylori non-infected workers had dyspeptic symptoms (P < 0.025). Scores for dyspeptic symptoms improved significantly in patients who were cured for H. pylori than the patients in whom H. pylori persisted (P < 0.0001). This study suggests pathogenic role of H. pylori in dyspepsia and may raise concern whether dyspeptic patients with H. pylori should be considered as FD. In a study from China, of 522 patients with acute gastroenteritis, 35 (6.7%) patients developed FD on follow-up after acute gastroenteritis.48
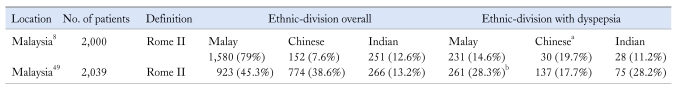
Ethnicity
In a door to door survey on 2,000 subjects of a rural multi-ethnic Malaysian population consisting of Chinese, Indian and Malay, 14.6% had dyspepsia (Rome II criteria). Frequency of dyspepsia was 14.6%, 19.7% and 11.2% in Malay, Chinese and Indian ethnic groups, respectively. Dyspepsia was commoner among Chinese than non-Chinese (19.7% vs 14.2%, P = 0.062).8 In another study on urban Malaysian population, of 2,039 subjects, 24.3% had dyspepsia (Rome II criteria). Malay ethnicity (prevalence of dyspepsia: 28.3%) was an independent risk factor for dyspepsia (OR, 2.17; 95% CI, 1.57-2.99; Table 4).49
Table 4.
Summary of Studies on Ethnic Factors in Patients With Functional Dyspepsia in Asia
aDyspepsia was found to be associated with Chinese ethnicity (19.7% vs 14.2% non-Chinese), bDyspepsia was found to be associated with Malay and Indian ethnicity (28% vs 17%).
Dietary Factors
Asian diet is somewhat different than the Western diet. Some food ingredients like chilly is taken by Asian people of different countries in variable amount. How chilly affects GI symptoms is largely unknown. In a study from Thailand on patients with diarrhea-predominant IBS, abdominal pain and burning increased after chilly intake.50 In another study from Thailand, red chilly was shown to induce rectal hypersensitivity in healthy subjects.51 A population-based study from Malaysia showed that high chilly intake was an independent risk factor for dyspepsia (OR, 2.35; 95% CI, 1.15-4.80).49 Rice-based diet, popular among many Asian population may be better tolerated than Western wheat-based diet by many patients with functional bowel disorders.52 However, data on these issues are somewhat scanty. More studies are needed on dietary issues on functional bowel diseases in different population in the world in general and Asia in particular.
Frequency of Irritable Bowel Syndrome in Patients With Dyspepsia in Asia
Frequency of IBS among patients with FD varies from 1.6 to 49% in Asia (Table 5). In a study from China, of 3,014 subjects, 5% had FD-IBS overlap using Rome III criteria.53 In a study from India, dyspepsia-IBS overlap was found in 14.2% of 2,549 subjects; in this study, dyspepsia was defined as abdominal pain and discomfort centered in upper abdomen and lasting for at least one month and IBS was diagnosed using Manning's criteria.9 Another Indian study showed similar high frequency of dyspeptic symptoms among patients with IBS.54 In a study from Japan, of 818 patients with upper abdominal symptoms visiting GI clinic, 320 were found to have FGIDs. The frequency of FD, IBS and FD-IBS overlap were found to be 53%, 21% and 1.6%, respectively.55 In this study, dyspepsia was defined as combination of upper abdominal symptoms such as abdominal pain, discomfort, early satiety, fullness, nausea and IBS was defined as a combination of frequent abdominal pain and altered bowel habits. In a study from Hong Kong, of 1,649 subjects, 18.4%, 4.1% and 14% had dyspepsia, IBS and overlap syndrome, respectively using Rome I criteria.4 In a Japanese study, of 181 medical students 6.7%, 40% and 4.4% had UD, IBS and dyspepsia-IBS overlap, respectively using Rome II criteria.56 In a Korean study on 476 patients referred to gastroenterologist in a tertiary hospital, 37%, 18% and 11% had FD, IBS and FD-IBS overlap, respectively using Rome II criteria.14 Such wide variation in overlap syndrome in different studies might be related to diagnostic criteria, study population and sociocultural issues, which might determine symptom reporting.
Table 5.
Summary of Studies on Overlapping Functional Dyspepsia and Irritable Bowel Syndrome Symptoms in Asia
FD, functional dyspepsia; IBS, irritable bowel syndrome.
Frequency of Gastroesophageal Reflux Disease in Patients With Dyspepsia
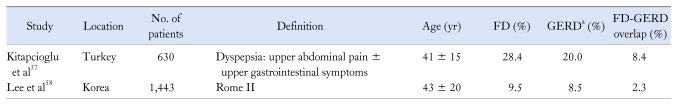
A few studies suggest that overlap of FD and gastroesophageal reflux disease (GERD) is not uncommon in Asia (Table 6). In a study from Turkey, 11.6%, 20% and 8.4% of 630 subjects had dyspepsia, GERD and dyspepsia-GERD overlap, respectively.57 In a Korean study, 9.5%, 8.5% and 2.3% of 1,433 subjects had dyspepsia, GERD and dyspepsia-GERD overlap, respectively.58 However, in both the studies, GERD was diagnosed by questionnaires and not by 24 hour pH-impedance monitoring, which is currently the gold standard for diagnosis of GERD. Symptoms of GERD such as heartburn may be influenced by variation of reporting by the patients due to socio-cultural issues and lack of appropriate terminology in some Asian languages.59
Table 6.
Asian Studies on Overlap of Symptoms of Functional Dyspepsia and Gastroesophageal Reflux Disease
aGERD was defined by weekly or more frequent heartburn and/or acid regurgitation during the preceding 12 months.
FD, functional dyspepsia; GERD, gastroesophageal reflux disease.
Quality of Life in Patients With Dyspepsia
Though FD is not a fatal disease, it is associated with substantial impairment of quality of life (QOL) and poses significant burden to the society due to work absenteeism, reduced productivity and use of health care resources.11,60 However, data on QOL of patients with FD from Asia are scanty. In a Korean study on 1417 subjects, 11.7%, 2.2% and 3.5% had dyspepsia, IBS (Rome III criteria) and GERD, respectively. Health-related QOL scores, evaluated by Korean version of SF-36, were worse for all 8 domains in patients with dyspepsia and IBS compared with those not having chronic GI symptoms.7,61 Two studies from Malaysia from same group of workers, one on rural and other on urban populations showed that subjects with dyspepsia (Rome II and III criteria) had lower health-related QOL using EuroQOL (EQ-5D) instrument.8,49,62 More studies on this issue are needed from Asia.
Psychological Co-morbidity
Psychological co-morbidity is often associated with FD.4,5,63-68 In a study from China, psychological assessment on patients with FD and healthy subjects before and after treatment using the Hamilton Rating Scale for Depression (HRSD) and Hamilton Anxiety Scale revealed that there was significant difference of scores for HRSD and Hamilton Anxiety Scale between patients with FD and healthy subjects. Treatment with anti-depressant for 8 weeks resulted in improvement in scores.69 In a prospective, cross-sectional Malaysian study on 839 patients with dyspepsia undergoing EGD, 472 turned out to be FD and 367 had organic cause;70 this study showed that patients with FD had lower health-related QOL than patients with organic dyspepsia though anxiety was associated with both the groups. Associated psychological factors may influence consultation behavior in some population. A population-based study from Hong Kong revealed that anxiety was associated medical consultation and sick leave among patients with dyspepsia and IBS.4 There are limited data on consultation behavior of patients with FD in Asia. One population based study from China showed that the degree of anxiety was an independent factor associated with health care seeking behaviour in dyspeptic patients (P = 0.003).4 However, in a recent review on epidemiology of IBS, another common type of functional bowel disease that may have overlapping dyspeptic symptoms, bloating and incomplete evacuation was found to be more important determinants of consultation behavior, than psychological factors in patients with functional bowel disorders.71 More studies on this issue are needed. A study from Australia showed that consulting behavior amongst patients with dyspepsia was driven in part by psychological factors and symptom-related anxiety.72 In a study from Sweden, educational illustrations, which might allay anxiety by explaining nature of the problem to the patient with an explanatory model, were found useful to benefit patients.73
Conclusion
Dyspepsia is common in Asia. FD is commonest cause of dyspepsia in most Asian population, particularly in absence of alarm features and in young age. Variation in frequency of dyspepsia in different studies might be related to criteria used to diagnose, variation in survey population and environmental factors. FD is not associated with any increase in mortality. However, its impact on patients' QOL and health care services has been shown to be considerable. Overlap of symptoms of FD, IBS and GERD is not uncommon in Asia. Associated psychological co-morbidity may influence consultation behavior among patients with FD.
Whilst previous reviews on epidemiology of FD in Asia have been published, new data have become available in the last few years, necessitating an update on the epidemiology of dyspepsia. However, one of the major concerns is that most population-based studies published till date on epidemiology of dyspepsia, are mainly on uninvestigated dyspepsia and not FD. Most of the data on FD are from institution-based studies, which may not represent the true epidemiology as the majority of patients with dyspepsia do not consult a medical practitioner or institution for their symptoms. An ideal population-based epidemiological study of FD would involve performing EGD on symptomatic adults in the community, but this is not easy to do. Hence, in spite of having quite a few studies on uninvestigated dyspepsia in Asia substantiating several facts, much of the knowledge on epidemiology of FD in Asia remains fiction. Hence, more cross-cultural studies to explore the real facts of epidemiology of FD in Asia and world are needed.
Footnotes
Financial support: None.
Conflicts of interest: None.
References
- 1.Tack J, Talley NJ, Camilleri M, et al. Functional gastroduodenal disorders. Gastroenterology. 2006;130:1466–1479. doi: 10.1053/j.gastro.2005.11.059. [DOI] [PubMed] [Google Scholar]
- 2.Mahadeva S, Goh KL. Epidemiology of functional dyspepsia: a global perspective. World J Gastroenterol. 2006;12:2661–2666. doi: 10.3748/wjg.v12.i17.2661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ho KY, Kang JY, Seow A. Prevalence of gastrointestinal symptoms in a multiracial Asian population, with particular reference to reflux-type symptoms. Am J Gastroenterol. 1998;93:1816–1822. doi: 10.1111/j.1572-0241.1998.00526.x. [DOI] [PubMed] [Google Scholar]
- 4.Hu WH, Wong WM, Lam CL, et al. Anxiety but not depression determines health care-seeking behaviour in Chinese patients with dyspepsia and irritable bowel syndrome: a population-based study. Aliment Pharmacol Ther. 2002;16:2081–2088. doi: 10.1046/j.1365-2036.2002.01377.x. [DOI] [PubMed] [Google Scholar]
- 5.Cheng C, Hui WM, Lam SK. Psychosocial factors and perceived severity of functional dyspeptic symptoms: a psychosocial interactionist model. Psychosom Med. 2004;66:85–91. doi: 10.1097/01.psy.0000106885.40753.c1. [DOI] [PubMed] [Google Scholar]
- 6.Li Y, Nie Y, Sha W, Su H. The link between psychosocial factors and functional dyspepsia: an epidemiological study. Chin Med J (Engl) 2002;115:1082–1084. [PubMed] [Google Scholar]
- 7.Jeong JJ, Choi MG, Cho YS, et al. Chronic gastrointestinal symptoms and quality of life in the Korean population. World J Gastroenterol. 2008;14:6388–6394. doi: 10.3748/wjg.14.6388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mahadeva S, Yadav H, Rampal S, Goh KL. Risk factors associated with dyspepsia in a rural Asian population and its impact on quality of life. Am J Gastroenterol. 2010;105:904–912. doi: 10.1038/ajg.2010.26. [DOI] [PubMed] [Google Scholar]
- 9.Shah SS, Bhatia SJ, Mistry FP. Epidemiology of dyspepsia in the general population in Mumbai. Indian J Gastroenterol. 2001;20:103–106. [PubMed] [Google Scholar]
- 10.Hirakawa K, Adachi K, Amano K, et al. Prevalence of non-ulcer dyspepsia in the Japanese population. J Gastroenterol Hepatol. 1999;14:1083–1087. doi: 10.1046/j.1440-1746.1999.02012.x. [DOI] [PubMed] [Google Scholar]
- 11.Lu CL, Lang HC, Chang FY, et al. Prevalence and health/social impacts of functional dyspepsia in Taiwan: a study based on the Rome criteria questionnaire survey assisted by endoscopic exclusion among a physical check-up population. Scand J Gastroenterol. 2005;40:402–411. doi: 10.1080/00365520510012190. [DOI] [PubMed] [Google Scholar]
- 12.Li XB, Liu WZ, Ge ZZ, et al. Analysis of clinical characteristics of dyspeptic symptoms in Shanghai patients. Chin J Dig Dis. 2005;6:62–67. doi: 10.1111/j.1443-9573.2005.00200.x. [DOI] [PubMed] [Google Scholar]
- 13.Kwan AC, Bao TN, Chakkaphak S, et al. Validation of Rome II criteria for functional gastrointestinal disorders by factor analysis of symptoms in Asian patient sample. J Gastroenterol Hepatol. 2003;18:796–802. doi: 10.1046/j.1440-1746.2003.03081.x. [DOI] [PubMed] [Google Scholar]
- 14.Kim JS, Lee KJ, Kim JH, Hahm KB, Cho SW. [Functional gastrointestinal disorders in patients referred to specialist gastroenterologists in a tertiary hospital] Korean J Neurogastroenterol Motil. 2004;10:111–117. [Korean] [Google Scholar]
- 15.Mahadeva S, Chia YC, Vinothini A, Mohazmi M, Goh KL. Cost-effectiveness of and satisfaction with a Helicobacter pylori "test and treat" strategy compared with prompt endoscopy in young Asians with dyspepsia. Gut. 2008;57:1214–1220. doi: 10.1136/gut.2007.147728. [DOI] [PubMed] [Google Scholar]
- 16.Wai CT, Yeoh KG, Ho KY, Kang JY, Lim SG. Diagnostic yield of upper endoscopy in Asian patients presenting with dyspepsia. Gastrointest Endosc. 2002;56:548–551. doi: 10.1067/mge.2002.128493. [DOI] [PubMed] [Google Scholar]
- 17.Kawamura A, Adachi K, Takashima T, et al. Prevalence of functional dyspepsia and its relationship with Helicobacter pylori infection in a Japanese population. J Gastroenterol Hepatol. 2001;16:384–388. doi: 10.1046/j.1440-1746.2001.02454.x. [DOI] [PubMed] [Google Scholar]
- 18.Ji SW, Park HJ, Choi JP, Lee TH, Lee SI. [Validation of Rome II criteria for functional gastrointestinal disorders in Korean patients] Korean J Gastroenterol. 2003;41:183–189. [Korean] [Google Scholar]
- 19.Park H. Functional gastrointestinal disorders and overlap syndrome in Korea. J Gastroenterol Hepatol. 2011;26(suppl 3):12–14. doi: 10.1111/j.1440-1746.2011.06644.x. [DOI] [PubMed] [Google Scholar]
- 20.Wu HC, Tuo BG, Wu WM, Gao Y, Xu QQ, Zhao K. Prevalence of peptic ulcer in dyspeptic patients and the influence of age, sex, and Helicobacter pylori infection. Dig Dis Sci. 2008;53:2650–2656. doi: 10.1007/s10620-007-0177-7. [DOI] [PubMed] [Google Scholar]
- 21.Naffeza MI, Isa MR, Kudva MV, et al. Helicobacter pylori related functional dyspepsia in a defined Malaysian population. Malaysian Journal of Medical Sciences. 2000;7:22–26. [PMC free article] [PubMed] [Google Scholar]
- 22.Hsu PI, Lai KH, Lo GH, et al. Risk factors for ulcer development in patients with non-ulcer dyspepsia: a prospective two year follow up study of 209 patients. Gut. 2002;51:15–20. doi: 10.1136/gut.51.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miwa H, Hirai S, Nagahara A, et al. Cure of Helicobacter pylori infection does not improve symptoms in non-ulcer dyspepsia patients - double-blind placebo-controlled study. Aliment Pharmacol Ther. 2000;14:317–324. doi: 10.1046/j.1365-2036.2000.00706.x. [DOI] [PubMed] [Google Scholar]
- 24.Su YC, Wang WM, Wang SY, et al. The association between Helicobacter pylori infection and functional dyspepsia in patients with irritable bowel syndrome. Am J Gastroenterol. 2000;95:1900–1905. doi: 10.1111/j.1572-0241.2000.02252.x. [DOI] [PubMed] [Google Scholar]
- 25.Kaur G, Naing NN. Prevalence and ethnic distribution of Helicobacter pylori among endoscopic patients in north eastern peninsular Malaysia. Malaysian Journal of Medical Sciences. 2003;10:66–70. [PMC free article] [PubMed] [Google Scholar]
- 26.Tan HJ, Rizal AM, Rosmadi MY, Goh KL. Role of Helicobacter pylori virulence factor and genotypes in non-ulcer dyspepsia. J Gastroenterol Hepatol. 2006;21:110–115. doi: 10.1111/j.1440-1746.2005.04063.x. [DOI] [PubMed] [Google Scholar]
- 27.Kim JE, Rhee PL, Kim YH, et al. [Association of Helicobacter pylori infection with gastric hypersensitivity in functional dyspepsia] Korean J Gastroenterol. 1999;34:717–723. doi: 10.1111/j.1572-0241.1999.01511.x. [Korean] [DOI] [PubMed] [Google Scholar]
- 28.Shim SG, Rhee PL, Hyun JG, et al. [Alimentary tract: correlation between DOB 30 of 13 C-urea breath test and proximal gastric motor functions in functional dyspepsia] Korean J Gastroenterol. 2001;38:405–410. [Korean] [Google Scholar]
- 29.Tahara T, Arisawa T, Shibata T, et al. Association of endoscopic appearances with dyspeptic symptoms. J Gastroenterol. 2008;43:208–215. doi: 10.1007/s00535-007-2149-2. [DOI] [PubMed] [Google Scholar]
- 30.Murray CD, Kamm MA, Bloom SR, Emmanuel AV. Ghrelin for the gastroenterologist: history and potential. Gastroenterology. 2003;125:1492–1502. doi: 10.1016/j.gastro.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 31.Akamizu T, Iwakura H, Ariyasu H, et al. Repeated administration of ghrelin to patients with functional dyspepsia: its effects on food intake and appetite. Eur J Endocrinol. 2008;158:491–498. doi: 10.1530/EJE-07-0768. [DOI] [PubMed] [Google Scholar]
- 32.Suzuki H, Matsuzaki J, Hibi T. Ghrelin and oxidative stress in gastrointestinal tract. J Clin Biochem Nutr. 2011;48:122–125. doi: 10.3164/jcbn.10-16GFR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shinomiya T, Fukunaga M, Akamizu T, et al. Plasma acylated ghrelin levels correlate with subjective symptoms of functional dyspepsia in female patients. Scand J Gastroenterol. 2005;40:648–653. doi: 10.1080/00365520510015403. [DOI] [PubMed] [Google Scholar]
- 34.Shindo T, Futagami S, Hiratsuka T, et al. Comparison of gastric emptying and plasma ghrelin levels in patients with functional dyspepsia and non-erosive reflux disease. Digestion. 2009;79:65–72. doi: 10.1159/000205740. [DOI] [PubMed] [Google Scholar]
- 35.Suzuki H, Masaoka T, Sakai G, Ishii H, Hibi T. Improvement of gastrointestinal quality of life scores in cases of Helicobacter pylori-positive functional dyspepsia after successful eradication therapy. J Gastroenterol Hepatol. 2005;20:1652–1660. doi: 10.1111/j.1440-1746.2005.04039.x. [DOI] [PubMed] [Google Scholar]
- 36.Jin X, Li YM. Systematic review and meta-analysis from Chinese literature: the association between Helicobacter pylori eradication and improvement of functional dyspepsia. Helicobacter. 2007;12:541–546. doi: 10.1111/j.1523-5378.2007.00520.x. [DOI] [PubMed] [Google Scholar]
- 37.Hsu PI, Lai KH, Tseng HH, et al. Eradication of Helicobacter pylori prevents ulcer development in patients with ulcer-like functional dyspepsia. Aliment Pharmacol Ther. 2001;15:195–201. doi: 10.1046/j.1365-2036.2001.00903.x. [DOI] [PubMed] [Google Scholar]
- 38.Gwee KA, Teng L, Wong RK, Ho KY, Sutedja DS, Yeoh KG. The response of Asian patients with functional dyspepsia to eradication of Helicobacter pylori infection. Eur J Gastroenterol Hepatol. 2009;21:417–424. doi: 10.1097/MEG.0b013e328317b89e. [DOI] [PubMed] [Google Scholar]
- 39.Peng NJ, Hsu PI, Lee SC, et al. Follow-up of Helicobacter pylori status by using 13C-Urea Breath Test in non-ulcer dyspeptic patients after eradication therapy. Zhonghua Yi Xue Za Zhi (Taipei) 2001;64:337–342. [PubMed] [Google Scholar]
- 40.Chanatrirattanapan R, Gonlachanvit S. Effects of Helicobacter pylori eradication on proximal gastric motor functions in Helicobacter pylori associated functional dyspepsia patients. Thai J Gastroenterol. 2006;7:151–156. [Google Scholar]
- 41.Ang TL, Fock KM, Teo EK, et al. Helicobacter pylori eradication versus prokinetics in the treatment of functional dyspepsia: a randomized, double-blind study. J Gastroenterol. 2006;41:647–653. doi: 10.1007/s00535-006-1818-x. [DOI] [PubMed] [Google Scholar]
- 42.Chang YW, Min SK, Kim KJ, et al. Delta (13)C-urea breath test value is a useful indicator for Helicobacter pylori eradication in patients with functional dyspepsia. J Gastroenterol Hepatol. 2003;18:726–731. doi: 10.1046/j.1440-1746.2003.03049.x. [DOI] [PubMed] [Google Scholar]
- 43.Miyaji H, Azuma T, Ito S, et al. The effect of Helicobacter pylori eradication therapy on gastric antral myoelectrical activity and gastric emptying in patients with non-ulcer dyspepsia. Aliment Pharmacol Ther. 1999;13:1473–1480. doi: 10.1046/j.1365-2036.1999.00634.x. [DOI] [PubMed] [Google Scholar]
- 44.Kamada T, Haruma K, Hata J, et al. The long-term effect of Helicobacter pylori eradication therapy on symptoms in dyspeptic patients with fundic atrophic gastritis. Aliment Pharmacol Ther. 2003;18:245–252. doi: 10.1046/j.1365-2036.2003.01669.x. [DOI] [PubMed] [Google Scholar]
- 45.Hopper AD, Cross SS, McAlindon ME, Sanders DS. Symptomatic giardiasis without diarrhea: further evidence to support the routine duodenal biopsy? Gastrointest Endosc. 2003;58:120–122. doi: 10.1067/mge.2003.199. [DOI] [PubMed] [Google Scholar]
- 46.Yakoob J, Jafri W, Abid S, et al. Giardiasis in patients with dyspeptic symptoms. World J Gastroenterol. 2005;11:6667–6670. doi: 10.3748/wjg.v11.i42.6667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Azuma T, Ito Y, Suto H, et al. The effect of Helicobacter pylori eradication therapy on dyspepsia symptoms in industrial workers in Japan. Aliment Pharmacol Ther. 2001;15:805–811. doi: 10.1046/j.1365-2036.2001.00987.x. [DOI] [PubMed] [Google Scholar]
- 48.Li X, Chen H, Lu H, et al. The study on the role of inflammatory cells and mediators in post-infectious functional dyspepsia. Scand J Gastroenterol. 2010;45:573–581. doi: 10.3109/00365521003632576. [DOI] [PubMed] [Google Scholar]
- 49.Mahadeva S, Yadav H, Rampal S, Everett SM, Goh KL. Ethnic variation, epidemiological factors and quality of life impairment associated with dyspepsia in urban Malaysia. Aliment Pharmacol Ther. 2010;31:1141–1151. doi: 10.1111/j.1365-2036.2010.04270.x. [DOI] [PubMed] [Google Scholar]
- 50.Gonlachanvit S, Mahayosnond A, Kullavanijaya P. Effects of chili on postprandial gastrointestinal symptoms in diarrhoea predominant irritable bowel syndrome: evidence for capsaicin-sensitive visceral nociception hypersensitivity. Neurogastroenterol Motil. 2009;21:23–32. doi: 10.1111/j.1365-2982.2008.01167.x. [DOI] [PubMed] [Google Scholar]
- 51.Gonlachanvit S, Fongkam P, Wittayalertpanya S, Kullavanijaya P. Red chili induces rectal hypersensitivity in healthy humans: possible role of 5HT-3 receptors on capsaicin-sensitive visceral nociceptive pathways. Aliment Pharmacol Ther. 2007;26:617–625. doi: 10.1111/j.1365-2036.2007.03396.x. [DOI] [PubMed] [Google Scholar]
- 52.Wahnschaffe U, Schulzke JD, Zeitz M, Ullrich R. Predictors of clinical response to gluten-free diet in patients diagnosed with diarrhea-predominant irritable bowel syndrome. Clin Gastroenterol Hepatol. 2007;5:844–850. doi: 10.1016/j.cgh.2007.03.021. [DOI] [PubMed] [Google Scholar]
- 53.Wang A, Liao X, Xiong L, et al. The clinical overlap between functional dyspepsia and irritable bowel syndrome based on Rome III criteria. BMC Gastroenterol. 2008;8:43. doi: 10.1186/1471-230X-8-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ghoshal UC, Abraham P, Bhatt C, et al. Epidemiological and clinical profile of irritable bowel syndrome in India: report of the Indian Society of Gastroenterology Task Force. Indian J Gastroenterol. 2008;27:22–28. [PubMed] [Google Scholar]
- 55.Okumura T, Tanno S, Ohhira M, Tanno S. Prevalence of functional dyspepsia in an outpatient clinic with primary care physicians in Japan. J Gastroenterol. 2010;45:187–194. doi: 10.1007/s00535-009-0168-x. [DOI] [PubMed] [Google Scholar]
- 56.Hori K, Matsumoto T, Miwa H. Analysis of the gastrointestinal symptoms of uninvestigated dyspepsia and irritable bowel syndrome. Gut Liver. 2009;3:192–196. doi: 10.5009/gnl.2009.3.3.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kitapcioglu G, Mandiracioglu A, Caymaz Bor C, Bor S. Overlap of symptoms of dyspepsia and gastroesophageal reflux in the community. Turk J Gastroenterol. 2007;18:14–19. [PubMed] [Google Scholar]
- 58.Lee SY, Lee KJ, Kim SJ, Cho SW. Prevalence and risk factors for overlaps between gastroesophageal reflux disease, dyspepsia, and irritable bowel syndrome: a population-based study. Digestion. 2009;79:196–201. doi: 10.1159/000211715. [DOI] [PubMed] [Google Scholar]
- 59.Sperber AD. The challenge of cross-cultural, multi-national research: potential benefits in the functional gastrointestinal disorders. Neurogastroenterol Motil. 2009;21:351–360. doi: 10.1111/j.1365-2982.2009.01276.x. [DOI] [PubMed] [Google Scholar]
- 60.Moayyedi P, Mason J. Clinical and economic consequences of dyspepsia in the community. Gut. 2002;50(suppl 4):iv10–iv12. doi: 10.1136/gut.50.suppl_4.iv10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hu WH, Lam KF, Wong YH, et al. The Hong Kong index of dyspepsia: a validated symptom severity questionnaire for patients with dyspepsia. J Gastroenterol Hepatol. 2002;17:545–551. doi: 10.1046/j.1440-1746.2002.02713.x. [DOI] [PubMed] [Google Scholar]
- 62.Mahadeva S, Wee HL, Goh KL, Thumboo J. The EQ-5D (Euroqol) is a valid generic instrument for measuring quality of life in patients with dyspepsia. BMC Gastroenterol. 2009;9:20. doi: 10.1186/1471-230X-9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cheng C, Hui WM, Lam SK. Coping style of individuals with functional dyspepsia. Psychosom Med. 1999;61:789–795. doi: 10.1097/00006842-199911000-00011. [DOI] [PubMed] [Google Scholar]
- 64.Ochi M, Tominaga K, Iketani T, et al. Perfectionism underlying psychological background correlated with the symptoms of functional dyspepsia. J Gastroenterol. 2008;43:699–704. doi: 10.1007/s00535-008-2210-9. [DOI] [PubMed] [Google Scholar]
- 65.Chen TS, Lee YC, Chang FY, Wu HC, Lee SD. Psychosocial distress is associated with abnormal gastric myoelectrical activity in patients with functional dyspepsia. Scand J Gastroenterol. 2006;41:791–796. doi: 10.1080/00365520500495599. [DOI] [PubMed] [Google Scholar]
- 66.Hsu YC, Liou JM, Liao SC, et al. Psychopathology and personality trait in subgroups of functional dyspepsia based on Rome III criteria. Am J Gastroenterol. 2009;104:2534–2542. doi: 10.1038/ajg.2009.328. [DOI] [PubMed] [Google Scholar]
- 67.Chou LT, Wu CY, Chen HP, et al. The Correlation of depression and gastric dysrhythmia in functional dyspepsia. J Clin Gastroenterol. 2001;33:127–131. doi: 10.1097/00004836-200108000-00007. [DOI] [PubMed] [Google Scholar]
- 68.Tominaga K, Higuchi K, Iketani T, et al. Comparison of gastrointestinal symptoms and psychological factors of functional dyspepsia to peptic ulcer or panic disorder patients. Inflammopharmacology. 2007;15:84–89. doi: 10.1007/s10787-006-0011-4. [DOI] [PubMed] [Google Scholar]
- 69.Xiaoping P, Yuyuan L, Weihong S, Fuying Y. Psychological factors in functional dyspepsia and its treatment. Chin J Dig Dis. 2000;1:17–20. [Google Scholar]
- 70.Mahadeva S, Goh KL. Anxiety, depression and quality of life differences between functional and organic dyspepsia. J Gastroenterol Hepatol. 2011;26(suppl 3):49–52. doi: 10.1111/j.1440-1746.2011.06656.x. [DOI] [PubMed] [Google Scholar]
- 71.Gwee KA, Lu CL, Ghoshal UC. Epidemiology of irritable bowel syndrome in Asia: something old, something new, something borrowed. J Gastroenterol Hepatol. 2009;24:1601–1607. doi: 10.1111/j.1440-1746.2009.05984.x. [DOI] [PubMed] [Google Scholar]
- 72.Howell S, Talley NJ. Does fear of serious disease predict consulting behaviour amongst patients with dyspepsia in general practice? Eur J Gastroenterol Hepatol. 1999;11:881–886. doi: 10.1097/00042737-199908000-00012. [DOI] [PubMed] [Google Scholar]
- 73.Wohrm A. Educational illustrations as an aid in patient-doctor communication, exemplified by patients with dyspepsia. Scand J Prim Health Care. 1994;12:84–87. doi: 10.3109/02813439409003680. [DOI] [PubMed] [Google Scholar]
- 74.Kaji M, Fujiwara Y, Shiba M, et al. Prevalence of overlaps between GERD, FD and IBS and impact on health-related quality of life. J Gastroenterol Hepatol. 2010;25:1151–1156. doi: 10.1111/j.1440-1746.2010.06249.x. [DOI] [PubMed] [Google Scholar]
- 75.Choo KY, Choi MG, Choi H, et al. [The prevalences of gastrointestinal symptoms in a rural community in Korea] Korean J Gastrointest Motil. 2000;6:31–43. [Korean] [Google Scholar]
- 76.Yang SY, Lee OY, Bak YT, et al. Prevalence of gastroesophageal reflux disease symptoms and uninvestigated dyspepsia in Korea: a population-based study. Dig Dis Sci. 2008;53:188–193. doi: 10.1007/s10620-007-9842-0. [DOI] [PubMed] [Google Scholar]
- 77.Ji SW, Park HJ, Choi JP, Lee TH, Lee DY, Lee SI. [Validation of Rome II criteria for functional gastrointestinal disorders in Korean patients] Korean J Gastroenterol. 2003;41:183–189. [Korean] [Google Scholar]
- 78.Noh YW, Jung HK, Kim SE, Jung SA. Overlap of erosive and non-erosive reflux diseases with functional gastrointestinal disorders according to Rome III criteria. J Neurogastroenterol Motil. 2010;16:148–156. doi: 10.5056/jnm.2010.16.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]