Abstract
Background
Despite an increased propensity to primary failure in forearm arteriovenous fistulae compared to upper arm fistulae, forearm fistulae remain the preferred primary access type for chronic hemodialysis patients. In a high risk patient population with multiple medical comorbidities associated with requirement for intravenous access we compared the rates of access failure in forearm and upper arm fistulae.
Materials and Methods
The records of all patients having primary native arteriovenous fistulae placed between 2004 and 2009 at the VA Connecticut Healthcare system were reviewed (n=118). Primary and secondary patency of upper arm and forearm fistulae were evaluated using Kaplan-Meier survival analysis. The effects of medical comorbidities on access patency were analyzed with Cox regression.
Results
The median time to primary failure of the vascular access was 0.288 years in the forearm group compared to 0.940 years in the upper arm group (p=0.028). Secondary patency was 52% at 4.9 years in upper arm fistulae compared to 52% at 1.1 years in the forearm group (p=0.036). There was no significant effect of patient comorbidities on fistula failure; however, there was a trend toward upper arm surgical site as a protective factor for primary fistula patency (Hazard Ratio=0.573, p=0.076).
Conclusions
In veterans needing hemodialysis, a high risk population with extensive comorbid factors often requiring intravascular access, upper arm fistulae are not only a viable option for primary vascular access, but are likely to be a superior option to classic forearm fistulae.
Keywords: Arteriovenous fistula, radiocephalic fistula, brachiocephalic fistula, hemodialysis, vascular patency, veteran, risk factor
Creating and maintaining long-term access for hemodialysis remains both a clinical challenge and necessity. Arteriovenous (AV) fistulae are the preferred access type for chronic hemodialysis patients, with current practice guidelines choosing radiocephalic forearm fistulae as the preferred initial location for primary vascular access, followed by brachiocephalic and brachiobasilic upper arm fistulae, respectively (1, 2). When placed prior to the initiation of hemodialysis fistulae are preferred as they eliminate the need for indwelling dialysis catheters, which are associated with increased patient mortality as well as an increased risk of sepsis (3-7). Prosthetic AV grafts, while also preferred to central venous catheters, are generally reserved for use in patients with inadequate native vasculature as they have worse long-term patency and increased rates of infection compared to native fistulae (8). Nonetheless, AV fistulae are not without their own complications, including thrombosis, infection, aneurysm, seromas, steal syndrome, heart failure, and bleeding, complicating the placement algorithm.
In a systematic review of 34 studies, primary patency rates of upper arm fistulae were approximately 81% and 60%, at 6 and 18 months, respectively, compared to 71% and 49%, in forearm fistulae at 6 and 18 months. Likewise, primary patency rates of upper arm prosthetic grafts were approximately 69% and 49%, at 6 and 18 months, respectively, compared to 51% and 28%, in forearm grafts at 6 and 18 months (8). As such, many patients with AV access require invasive procedures to maintain secondary patency; otherwise the site may need to be abandoned and a new access performed. Although access failure rates have varied slightly from study to study and across patient populations, forearm fistulae in particular are well documented as failing to mature at rates greater than that of upper arm fistulae (8, 9). In spite of this, forearm fistulae remain the primary vascular access of choice due to relative ease of creation and preservation of proximal vasculature for future access attempts.
We evaluated primary and secondary patency rates of upper arm and forearm AV access when placed for primary hemodialysis access in veterans. We have previously shown that veterans often have large numbers of comorbid medical conditions compared to nonveterans, suggesting that this population is at particularly high risk for complications (10, 11). We hypothesized that, since patients with multiple medical comorbidities often require high rates of intravascular (IV) access, high risk patients may have particularly poor rates of forearm access maturation. If veterans have poor rates of access maturation, then upper arm fistulae may be preferred in these patients.
Materials and Methods
The records of all patients who underwent primary AV access creation at the VA Connecticut Healthcare System, West Haven, CT, between April 2004 and December 2009 were reviewed. Charts were reviewed through June 2010 follow up data. Patients with functional fistulae were not included in the study if the AV fistula, was surgically created prior to April 2004. In patients who had two or more fistulae placements during the study period, only data pertaining to the initial operation was collected. Selection for forearm or upper arm fistulae was at the operative surgeon's discretion and included factors such as presence of a palpable vein as well as the venous diameter recorded on preoperative duplex mapping.
Patient demographics were determined via chart review, and included age, race, and gender. Patient charts were evaluated for the preoperative presence or absence of the following comorbidities: hypertension, diabetes mellitus, current smoking, current dialysis, congestive heart failure (CHF), coronary artery disease (CAD), pulmonary disease, stroke, transient ischemic attack (TIA), and cancer. Preoperative laboratory values included albumin and creatinine. Preoperative measures evaluated were body mass index (BMI) and ejection fraction (EF, %). Patient medications were reviewed for the presence or absence of prescribed aspirin (ASA), anti-platelet agents, anticoagulation agents, and statin therapy. Surgical variables included: surgical site (upper arm, i.e. brachiocephalic or basilic access; forearm, i.e. radiocephalic access), surgical side (right or left), and size of upper arm and forearm veins as recorded on preoperative duplex (cephalic at the distal humerus and cephalic at the wrist, respectively). Postoperative variables recorded included known use of the access for successful hemodialysis.
The primary study outcomes were fistula status (patent versus failed) and duration of fistula patency. Primary patency was calculated as the time period between the date of access placement and the date of either the last follow-up with known fistula patency without failure, or until the date of first fistula failure. Secondary patency was calculated as the time period between the date of access placement and the date of either the last follow-up with known fistula patency without failure, or until the date of absolute fistula failure requiring disuse and site abandonment, i.e. including all secondary procedures to maintain the access. Postoperative survival outcomes included date of death or date of last follow-up in the VA records and patient status (deceased or living). Length of survival was calculated using the date of fistula access as the baseline.
Results are reported as mean ± SEM. Statistical analysis was performed with SigmaPlot 11.0 (Systat Software, San Jose, CA). The study population was divided by upper or forearm fistula site and analyzed across these two groups. Categorical variables were analyzed using Chi-square test, and continuous variables were analyzed using the t-test. Primary and secondary graft patency were analyzed using Kaplan-Meier statistics, and the difference between the upper and forearm strata were compared using the Gehan-Breslow statistic. Overall survival of the study population was analyzed using Kaplan-Meier statistics. The effect of all independent patient demographic variables collected on primary fistula patency and long-term survival of the study population was analyzed with Cox regression.
Results
Patient Demographics and Comorbidities
A total of 118 patients underwent primary AV fistula placement at the VA Connecticut Healthcare System between April 2004 and December 2009. Of these patients, 44 had upper arm fistulae and 74 had forearm fistulae.
The demographics of the study population are listed in Table 1. There were 116 men and 2 women. The mean age of patients who had upper arm fistulae was 65.8 ± 1.9 years, and the mean age of patients who had forearm fistulae was 65.8 ± 1.4 years; there was no significant difference between these two groups (p= 0.985). All of the patients were either Caucasian (67.8%) or African American (32.2%); patient race did not vary across groups (p= 0.785).
Table 1.
Demographics and risk factors.
| Variable | Total (n) | Total (%) | Upper Arm | Upper (%) | Forearm | Forearm (%) | p-value |
|---|---|---|---|---|---|---|---|
| Total Patients (n) | 118 | 44 | 37.3% | 74 | 62.7% | ||
|
| |||||||
| Age (yrs) | 65.8±1.1 | 65.8 ± 1.8 | 65.8± 1.4 | 0.985 | |||
| Race | |||||||
| Caucasian | 80 | 67.8% | 31 | 75.0% | 49 | 66.2% | 0.785 |
| African American | 38 | 32.2% | 13 | 29.5% | 25 | 33.8% | |
| Gender | |||||||
| Male | 116 | 98.3% | 43 | 97.7% | 73 | 98.6% | 0.717 |
| Female | 2 | 1.7% | 1 | 2.3% | 1 | 1.4% | |
|
| |||||||
| Comorbidities | |||||||
|
| |||||||
| Hypertension | |||||||
| Yes | 117 | 99.2% | 43 | 97.7% | 74 | 100.0% | 0.792 |
| No | 1 | 0.8% | 1 | 2.3% | 0 | 0.0% | |
| Diabetes Mellitus | |||||||
| Yes | 47 | 39.8% | 21 | 47.7% | 26 | 35.1% | 0.247 |
| No | 71 | 60.2% | 23 | 52.3% | 48 | 64.9% | |
| Current Smoker | |||||||
| Yes | 36 | 30.5% | 6 | 13.6% | 30 | 40.5% | 0.004 |
| No | 82 | 69.5% | 38 | 86.4% | 44 | 59.5% | |
| Current Dialysis | |||||||
| Yes | 51 | 43.2% | 18 | 40.9% | 33 | 44.6% | 0.843 |
| No | 67 | 56.8% | 26 | 59.1% | 41 | 55.4% | |
| Heart Disease (CAD or CHF) | |||||||
| Yes | 59 | 50.0% | 21 | 47.7% | 38 | 51.4% | 0.792 |
| No | 59 | 50.0% | 23 | 52.3% | 36 | 48.6% | |
| CAD | |||||||
| Yes | 55 | 46.6% | 21 | 47.7% | 34 | 45.9% | 0.997 |
| No | 63 | 53.4% | 23 | 52.3% | 40 | 54.1% | |
| CHF | |||||||
| Yes | 23 | 19.5% | 5 | 11.4% | 18 | 24.3% | 0.139 |
| No | 95 | 80.5% | 39 | 88.6% | 56 | 75.7% | |
| Pulmonary Disease | |||||||
| Yes | 31 | 26.3% | 8 | 18.2% | 23 | 31.1% | 0.186 |
| No | 87 | 73.7% | 36 | 81.8% | 51 | 68.9% | |
| Stroke | |||||||
| Yes | 16 | 13.6% | 5 | 11.4% | 11 | 14.9% | 0.795 |
| No | 102 | 86.4% | 39 | 88.6% | 63 | 85.1% | |
| TIA | |||||||
| Yes | 2 | 1.7% | 0 | 0.0% | 2 | 2.7% | 0.717 |
| No | 120 | 98.4% | 44 | 100.0% | 72 | 97.3% | |
| Cancer | |||||||
| Yes | 20 | 16.9% | 10 | 22.7% | 10 | 13.5% | 0.3 |
| No | 98 | 83.1% | 34 | 77.3% | 64 | 86.5% | |
|
| |||||||
| Preoperative Labs | |||||||
|
| |||||||
| Albumin (g/dL) | 3.1± .1 | 2.9± .2 | 3.2± .1 | 0.157 | |||
| Creatinine (mg/dL) | 5.2± .2 | 4.9± .3 | 5.3± .3 | 0.304 | |||
|
| |||||||
| Preoperative Measures | |||||||
|
| |||||||
| BMI | 28.4± .8 | 28.2± 1.4 | 28.2± 1.4 | 0.799 | |||
| LVEF (%) | 42.7± 2.4 | 42.3± 4.0 | 43.0± 3.1 | 0.903 | |||
|
| |||||||
| Medications | |||||||
|
| |||||||
| ASA | |||||||
| Yes | 47 | 39.8% | 16 | 36.4% | 31 | 41.9% | 0.69 |
| No | 71 | 60.2% | 28 | 63.6% | 43 | 58.1% | |
| Anti-platelet | |||||||
| Yes | 5 | 4.2% | 1 | 2.3% | 4 | 5.4% | 0.731 |
| No | 113 | 95.8% | 43 | 97.7% | 70 | 94.6% | |
| Anticoagulated? | |||||||
| Yes | 24 | 19.7% | 9 | 19.6% | 15 | 19.7% | 0.832 |
| No | 98 | 80.3% | 37 | 80.4% | 61 | 80.3% | |
| Statin | |||||||
| Yes | 70 | 59.3% | 24 | 54.5% | 46 | 62.2% | 0.535 |
| No | 48 | 40.7% | 20 | 45.5% | 28 | 37.8% | |
|
| |||||||
| Surgical Variables | |||||||
|
| |||||||
| Side | |||||||
| Right | 18 | 18.0% | 9 | 20.5% | 9 | 12.2% | 0.344 |
| Left | 100 | 84.7% | 35 | 79.5% | 65 | 87.8% | |
| Duplex U/S Vein Mapping | |||||||
| Cephalic @ Wrist (cm) | .13± .02 | .08± .02 | .15± .02 | 0.016 | |||
| Cephalic @ Distal Humerus (cm) | .34± .02 | .32± .03 | .35± .02 | 0.405 | |||
|
| |||||||
| Postoperative Variables | |||||||
|
| |||||||
| AVF Used? | |||||||
| Yes | 50 | 42.4% | 20 | 45.5% | 30 | 40.5% | 0.666 |
| No | 63 | 53.4% | 23 | 52.3% | 40 | 54.1% | |
| Unknown | 5 | 4.2% | 1 | 2.3% | 4 | 9.1% | |
Hypertension was highly prevalent in patients with either upper (97.7%) or forearm fistulae (100%). Diabetes mellitus had a similar prevalence across the two groups, present in 39.8% of the upper arm patients and 35.1% of the forearm patients (p=0.247). 30.5% of patients reported current tobacco use at the time of fistula placement; current tobacco use was more prevalent in the forearm group than the upper arm group (40.5% versus 13.6%; p=0.004). Patients who were receiving dialysis at the time of their operation were evenly distributed across the groups (40.9% upper arm vs. 44.6% forearm; p=0.929). 50% of patients were identified as having heart disease; there was no difference in prevalence across the upper and forearm groups (p=0.792); both CAD (p=0.997) and CHF (p=0.139) were similarly distributed across the study groups. There was no significant difference between the two groups in prevalence of pulmonary disease (p=0.186). Prior stroke and TIA were identified in 11.4% and 0% of the upper arm patients and 14.9% and 2.7% of the forearm patients, respectively; however this was not statistically significant (stroke, p=0.795; TIA, p=0.717). 17% of patients had a diagnosis of cancer at the time of operation, which was similar between groups (p=.300).
Preoperative Labs, Measures, and Medications
The mean preoperative albumin in the study population was 3.1 ± 0.1 g/dL and did not vary across groups (p=0.157). The mean creatinine was 5.2 ± 0.2 mg/dL; preoperative creatinine also did not vary between the surgical site groups (p=0.304). BMI and EF were similar across the upper and forearm groups (p=0.799 and p=0.903, respectively)
At the preoperative visit 39.8% of patient were taking aspirin, 4.24% were taking an antiplatelet agent, 19.5% of patients were anticoagulated, and 59.3% of patients were taking a statin; these medications did not vary significantly across groups (p=.535-.971).
Surgical and Postoperative Variables
The majority of study patients received left upper extremity fistulae (84.8%, n=100); however the distribution of surgical side did not vary significantly between groups (p=0.344). Preoperative duplex ultrasound vein mapping showed a significant difference between cephalic vein size at the wrist in the upper and forearm groups; patients who received forearm fistulae had a mean cephalic vein width at the wrist of 0.15 ± .021 cm compared to a width of 0.08 ± .021 cm in patients who had an upper arm fistula placed (p=.016). The cephalic vein diameter at the distal humerus was similar between the two groups, measuring 0.320 ± .0317 cm in the upper arm group and 0.35 ± .024 cm in the forearm group (p=.405). The number of patients that were successfully dialyzed through their primary AV fistula at least once did not vary across groups (p=0.666).
Access Patency
Cumulative primary patency was reduced in forearm fistulae compared to upper arm fistulae, with forearm fistulae having only 34% primary patency at 1 year compared to 41% at 1 year for upper arm fistulae; the median time to primary failure of the vascular access was 0.288 ± 0.164 years in the forearm group compared to 0.940 ± 0.456 years in the upper arm group (Figure 1A; p=0.028). Similarly, cumulative secondary patency was also reduced in forearm fistulae compared to upper arm fistulae; secondary patency was 52% at 4.9 years in upper arm fistulae compared to 52% at 1.1 years in the forearm group (Figure 1B; p=0.036).
Figure 1.
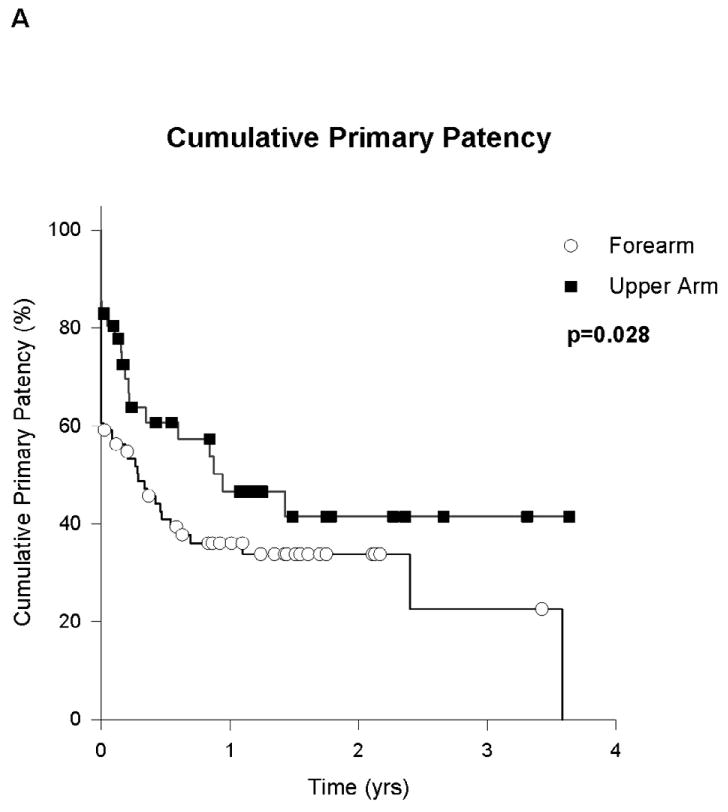
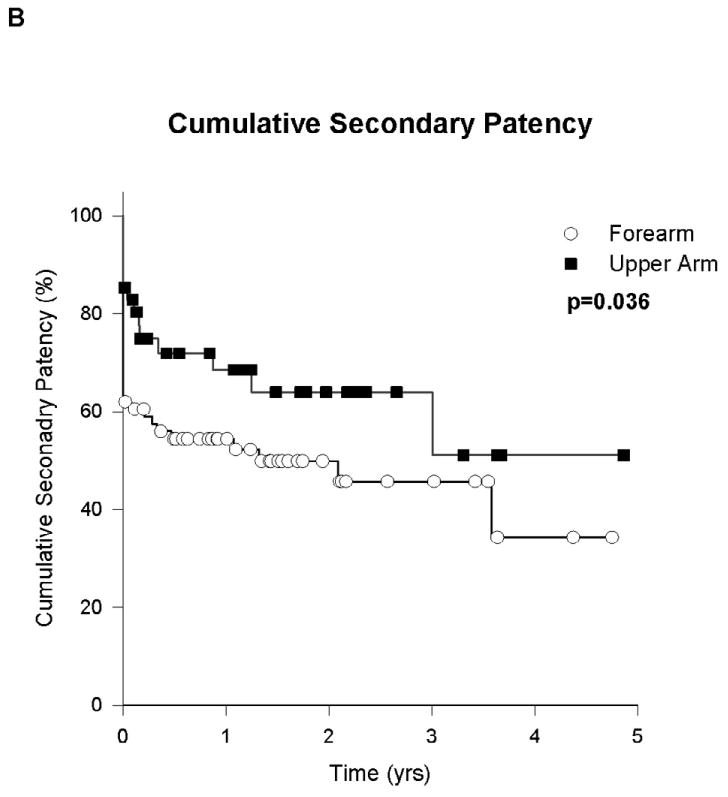
Primary and secondary patency of forearm vs. upper arm fistulae. (A) Kaplan-Meier analysis of primary fistulae patency. (B) Kaplan-Meier analysis of secondary fistulae patency.
Cox regression analysis of factors affecting primary fistula patency showed no significant effect of patient comorbidities, laboratory values, or medications on fistula failure (Table 2). There was a trend towards upper arm surgical site being a protective factor (hazard ratio=0.573; p=0.076); surgical side did not affect fistula patency (p=0.901).
Table 2.
Cox Proportional Hazards Analysis of Factors affecting Primary Fistula Patency
| Covariate | Hazard Ratio | 95%Conf-L | 95%Conf-U | P Value |
|---|---|---|---|---|
| Age | 1.0 | 1.0 | 1.0 | 0.718 |
|
| ||||
| Comorbidities | ||||
|
| ||||
| Hypertension | 1.3 | 0.1 | 13.1 | 0.798 |
| Diabetes Mellitus | 1.1 | 0.6 | 2.0 | 0.739 |
| Current Smoking | 0.9 | 0.5 | 1.6 | 0.669 |
| Current Dialysis | 1.1 | 0.6 | 2.1 | 0.718 |
| Heart disease (CHF or CAD) | 1.0 | 0.5 | 1.8 | 0.899 |
| Pulmonary Disease | 0.9 | 0.5 | 1.6 | 0.656 |
| Cancer | 1.1 | 0.5 | 2.2 | 0.859 |
|
| ||||
| Preoperative Labs | ||||
|
| ||||
| Albumin | 0.9 | 0.7 | 1.1 | 0.35 |
| Creatinine | 1.0 | 0.8 | 1.1 | 0.528 |
|
| ||||
| Preopeartive Measures | ||||
|
| ||||
| BMI | 1.0 | 1.0 | 1.0 | 0.949 |
| LVEF (%) | 1.0 | 1.0 | 1.0 | 0.606 |
|
| ||||
| Medications | ||||
|
| ||||
| ASA | 0.9 | 0.5 | 1.6 | 0.775 |
| Antiplatelet | 0.5 | 0.1 | 2.4 | 0.419 |
| Anticoagulated | 1.0 | 0.5 | 2.0 | 0.941 |
| Statin | 1.2 | 0.6 | 2.1 | 0.631 |
|
| ||||
| Surgical Variables | ||||
|
| ||||
| Site-Upper arm | 0.6 | 0.3 | 1.1 | 0.076 |
| Side | 1.0 | 0.5 | 2.0 | 0.901 |
Patient Survival
There were 35 (29.7%) patient deaths in the study group. Cumulative survival analysis reflected poor survival in this patient population, with 88% survival at 1 year, 62% survival at 3 years, and 58% survival at 5 years after fistula placement (Figure 2). The only preoperative demographic factor that was associated with reduced mortality was use of an anti-platelet agent (Table 3; hazard ratio=4.3; p=0.019). The surgical site, upper arm versus forearm, did not influence patient mortality (hazard ratio=-0.956; p=0.919).
Figure 2.
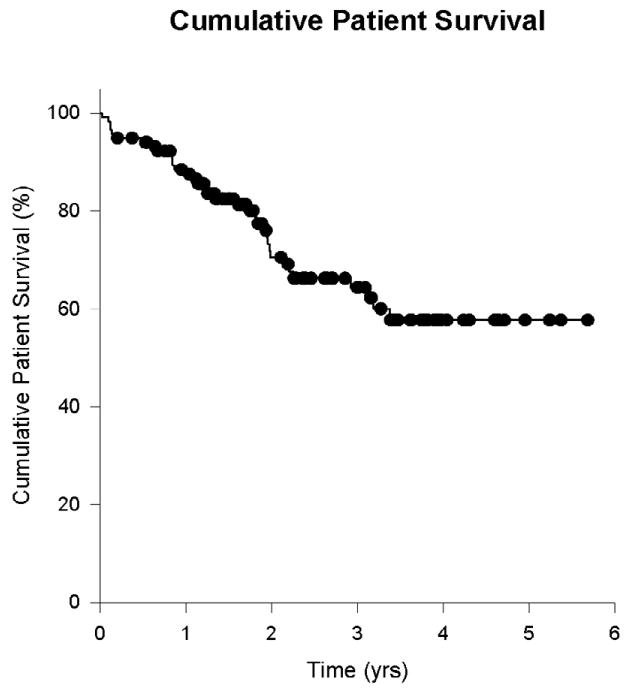
Kaplan-Meier analysis of post-operative survival.
Table 3.
Cox Proportional Hazards Analysis of Factors Affecting Patient Survival
| Covariate | Hazard Ratio | 95%Conf-L | 95%Conf-U | P Value |
|---|---|---|---|---|
| Age | 1.027 | 0.986 | 1.069 | 0.201 |
|
| ||||
| Comorbidities | ||||
|
| ||||
| Hypertension | 9.34E-08 | 0 | ∞ | 0.998 |
| Diabetes Mellitus | 1.881 | 0.815 | 4.34 | 0.139 |
| Current Smoking | 0.943 | 0.39 | 2.28 | 0.897 |
| Current Dialysis | 1.411 | 0.559 | 3.559 | 0.466 |
| Heart disease (CHF or CAD) | 0.649 | 0.253 | 1.665 | 0.368 |
| Pulmonary Disease | 1.264 | 0.505 | 3.165 | 0.617 |
| Cancer | 1.001 | 0.351 | 2.86 | 0.998 |
|
| ||||
| Preoperative Labs | ||||
|
| ||||
| Albumin | 0.864 | 0.609 | 1.227 | 0.415 |
| Creatinine | 1.032 | 0.863 | 1.234 | 0.732 |
|
| ||||
| Preopeartive Measures | ||||
|
| ||||
| BMI | 1 | 0.952 | 1.051 | 0.996 |
| LVEF (%) | 1.007 | 0.992 | 1.022 | 0.394 |
|
| ||||
| Medications | ||||
|
| ||||
| ASA | 0.711 | 0.303 | 1.671 | 0.434 |
| Antiplatelet | 4.314 | 1.273 | 14.62 | 0.019 |
| Anticoagulated | 0.78 | 0.309 | 1.97 | 0.599 |
| Statin | 1.068 | 0.45 | 2.535 | 0.882 |
|
| ||||
| Surgical Variables | ||||
|
| ||||
| Site-Upper arm | 0.956 | 0.401 | 2.279 | 0.919 |
| Side | 0.675 | 0.229 | 1.987 | 0.475 |
Discussion
Forearm fistulae have long been the gold standard for primary hemodialysis access. Our results, however, argue that forearm fistulae are far from a simple solution for hemodialysis access in veterans with end stage renal disease (ESRD). In a patient population with reduced life expectancy, we found superior primary and secondary patency of upper arm AV fistulae in comparison to forearm access. We conclude that upper arm access is not only a viable option for primary vascular access, but is likely to be a superior option to classic forearm fistulae in these high-risk patients.
Historically, the radiocephalic fistula, which has been used for hemodialysis access since the mid 1960s, has been the preferred initial access site, as the wrist is easily accessible for the surgeon and use of this site preserves more proximal access sites for future placement once the wrist site fails. Once hemodialysis became more prevalent in patients with diabetes, it was noticed that diabetic patients had increased rates of failure of radiocephalic fistulae due to both early thrombosis and low AVF blood flow (12). These observations led to the suggestion that upper arm fistulae be considered for initial access in complicated access patients, especially those with diabetes, hypertension, stroke, peripheral vascular disease, and prior amputation (12). It was also suggested that preoperative evaluations of such patients include blood pressure in both arms, a meticulous search for a suitable vein, thorough evaluation of arterial pulses, phlebography in obese patients, x-rays to detect arterial calcifications, and ultrasound evaluation of both arterial and venous blood flow in the upper extremity (12).
In a prospective study of 204 access patients, Dixon et. al. found that primary and cumulative patency of upper arm native access were significantly longer than that of forearm access (13). In their study 1-, 3-, and 5-year cumulative secondary patency of upper arm AVF were 69%, 53%, and 53%, respectively, compared to 52%, 43%, and 34% for lower arm access. Primary patency of upper arm access was also superior to that of forearm access. In a larger, systematic review of 34 studies, Huber et. al. also reported significantly greater primary patency of upper arm native access compared to forearm access (60% vs. 49% at 18 mo.) (8). As such, our results are consistent with a number of studies in the literature that suggest that forearm fistulae are not the best option in many patients.
Interestingly, we found no significant effect of patient comorbidities on access failure. Several patient risk factors have been previously identified as significant predictors of access patency, including diabetes, age greater than 65 years, white race, peripheral vascular disease, and coronary artery disease (14). Hernicus et al. reported peripheral vascular disease and diabetes to be significant predictors of fistula failure (15). Although our study did not identify these factors as predictive of access patency, our study may have been limited by small sample size, high prevalence of comorbid conditions, and homogeneity of the veteran population. Nevertheless, we were able to identify a trend towards upper arm surgical site as a protective factor for primary fistula patency (Table 2), which agrees with the results of our cumulative patency analysis (Figure 1).
Overall survival in the ESRD population is poor, with 5-year survival estimated to be 30-50% in nondiabetics, and 25% in diabetics (16). Our results were consistent with these reports, with 58% survival at 5 years in our study population (Figure 2). However, mortality is typically higher in hemodialysis patients requiring central venous catheters (CVC) and AV grafts for access compared to mortality patients using native access. Using data from the U.S. Renal Data System Dialysis Morbidity and Mortality Study Wave 1, the relative risk of death patients with diabetes was shown to be greater than that of patients with native fistulae (AVG, relative risk=1.41, p<0.003; CVC, relative risk=1.54, p<0.002). Similarly, in non-diabetic patients, CVC remained associated with greater risk of mortality (relative risk=1.70, p<0.001), with the vast majority of complications due to infection in both diabetic and non-diabetic patients. In addition, in spite of the historical association of AV fistulae with shunting and cardiac failure, the risk of cardiac death was greater in patients using CVC (diabetic relative risk=1.47, p<0.05; non-diabetic relative risk= 1.34, p<0.005) (3, 17). In one report, non-fistula access was the most important risk factor for infection (p=0.02), with the majority of infections occurring in patients with temporary vascular access such as CVC (9, 18). As such, our findings of poor survival in these patients with fistulae may underestimate mortality in comparison to other ESRD populations that include patients with AV grafts and CVC.
We suggest that in choosing a site for primary vascular access, the predicted long-term survival of the patient be considered, choosing a more definitive solution for hemodialysis access in patients with an overall poor predicted survival. In such poor risk patients, we believe that preservation of proximal access becomes less important than establishing reliable, long-term access that will probably be durable for the remainder of the patient's lifetime. Although the standard algorithm for site selection starts with the wrist and forearm sites, our data suggests that the use of the larger upper arm veins are more likely to provide flow rates amenable to hemodialysis and are less likely to fail to mature, serving as a suitable initial access. Preferential use of upper arm sites may thus avoid the need for temporary CVC usage, as well as reduce patient morbidity and redo surgery, improving patient satisfaction with care.
Limitations of our study include its retrospective nature, its small size, and its analysis of only a single center. In addition, since only half of our patients in which we perform access procedures have dialysis at our center, followup of these patients remains problematic. Similarly, it is not clear whether data regarding prior access sites, before the study period, is reliable. However, a prospective trial would necessary to test the hypothesis that a period of forearm access may allow maturation of upper arm veins, and, as such, cannot be answered by this retrospective study.
In young patients with few medical comorbidities and a reasonable predicted lifespan, we believe that, all other factors being equal, distal access remains a reasonable first choice option for permanent access. Such patients will likely require the use of more proximal sites within their lifespan, as no fistula can yet provide infinite hemodialysis access. In this study, veterans requiring hemodialysis form a high risk population with poor survival and need for immediate access. Additional studies are needed to define the impact of particular risk factors, especially in more heterogeneous ESRD populations. Nonetheless, commitment to maintaining hemodialysis access for this difficult group of patients may require abandoning the rigid historical dogma of creating a distal hemodialysis access site first under all circumstances.
Acknowledgments
This study was supported in part by the National Institutes of Health-NHLBI Medical Student Research Fellowship, NIH grant R01-HL095498-01, the American Vascular Association William J. von Liebig Award, as well as with the resources and the use of facilities at the VA Connecticut Healthcare System, West Haven, CT.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Clinical practice guidelines for vascular access. American Journal of Kidney Diseases. 2006;48(Suppl 1) doi: 10.1053/j.ajkd.2006.04.040. [DOI] [PubMed] [Google Scholar]
- 2.Jindal K, Chan CT, Deziel C, Hirsch D, Soroka SD, Tonelli M, et al. Hemodialysis clinical practice guidelines for the canadian society of nephrology. Journal of the American Society of Nephrology : JASN. 2006;17(3 Suppl 1):S1–27. doi: 10.1681/ASN.2005121372. [DOI] [PubMed] [Google Scholar]
- 3.Dhingra RK, Young EW, Hulbert-Shearon TE, Leavey SF, Port FK. Type of vascular access and mortality in U.S. hemodialysis patients. Kidney Int. 2001;60(4):1443–51. doi: 10.1046/j.1523-1755.2001.00947.x. [DOI] [PubMed] [Google Scholar]
- 4.Oliver MJ, Rothwell DM, Fung K, Hux JE, Lok CE. Late creation of vascular access for hemodialysis and increased risk of sepsis. Journal of the American Society of Nephrology. 2004;15(7):1936–42. doi: 10.1097/01.asn.0000131524.52012.f8. [DOI] [PubMed] [Google Scholar]
- 5.Pastan S, Soucie JM, McClellan WM. Vascular access and increased risk of death among hemodialysis patients. Kidney Int. 2002;62(2):620–6. doi: 10.1046/j.1523-1755.2002.00460.x. [DOI] [PubMed] [Google Scholar]
- 6.Polkinghorne KR, Mcdonald SP, Atkins RC, Kerr PG. Vascular access and all-cause mortality: A propensity score analysis. Journal of the American Society of Nephrology. 2004;15(2):477–86. doi: 10.1097/01.asn.0000109668.05157.05. [DOI] [PubMed] [Google Scholar]
- 7.Xue JL, Dahl D, Ebben JP, Collins AJ. The association of initial hemodialysis access type with mortality outcomes in elderly medicare ESRD patients. American Journal of Kidney Diseases. 2003;42(5):1013–9. doi: 10.1016/j.ajkd.2003.07.004. [DOI] [PubMed] [Google Scholar]
- 8.Huber TS, Carter JW, Carter RL, Seeger JM. Patency of autogenous and polytetrafluoroethylene upper extremity arteriovenous hemodialysis accesses: A systematic review. Journal of Vascular Surgery. 2003;38(5):1005–11. doi: 10.1016/s0741-5214(03)00426-9. 11. [DOI] [PubMed] [Google Scholar]
- 9.Miller PE, Tolwani A, Luscy CP, Deierhoi MH, Bailey R, Redden DT, et al. Predictors of adequacy of arteriovenous fistulas in hemodialysis patients. Kidney Int. 1999;56(1):275–80. doi: 10.1046/j.1523-1755.1999.00515.x. [DOI] [PubMed] [Google Scholar]
- 10.Weiss JS, Dumas P, Cha C, Gusberg RJ, Dardik A. Safety of carotid endarterectomy in a high-risk population: Lessons from the VA and connecticut. J Am Coll Surg. 2006;203(3):277–82. doi: 10.1016/j.jamcollsurg.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 11.Westvik TS, Krause LK, Pradhan S, Westvik HH, Maloney SP, Rutland R, et al. Malnutrition after vascular surgery: Are patients with chronic renal failure at increased risk? Am J Surg. 2006;192(5 Spec Iss):e22–7. doi: 10.1016/j.amjsurg.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 12.Konner K. Primary vascular access in diabetic patients: An audit. Nephrology Dialysis Transplantation. 2000;15(9):1317–25. doi: 10.1093/ndt/15.9.1317. [DOI] [PubMed] [Google Scholar]
- 13.Dixon BS, Novak L, Fangman J. Hemodialysis vascular access survival: Upper-arm native arteriovenous fistula. Am J Kidney Dis. 2002 Jan;39(1):92–101. doi: 10.1053/ajkd.2002.29886. [DOI] [PubMed] [Google Scholar]
- 14.Lok CE, Allon M, Moist L, Oliver MJ, Shah H, Zimmerman D. Risk equation determining unsuccessful cannulation events and failure to maturation in arteriovenous fistulas (REDUCE FTM I) Journal of the American Society of Nephrology. 2006;17(11):3204–12. doi: 10.1681/ASN.2006030190. [DOI] [PubMed] [Google Scholar]
- 15.Huijbregts HJT, Bots ML, Wittens CHA, Schrama YV, Moll FL, Blankestijn PJ. Hemodialysis arteriovenous fistula patency revisited: Results of a prospective, multicenter initiative. Clinical Journal of the American Society of Nephrology. 2008;3(3):714–9. doi: 10.2215/CJN.02950707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.United States Renal Data System. Excerpts from the USRDS 2009 annual data report: Atlas of end-stage renal disease in the united states. Am J Kidney Dis. 2010;1(suppl 1) doi: 10.1053/j.ajkd.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 17.Ethier J, Mendelssohn DC, Elder SJ, Hasegawa T, Akizawa T, Akiba T, et al. Vascular access use and outcomes: An international perspective from the dialysis outcomes and practice patterns study. Nephrology Dialysis Transplantation. 2008;23(10):3219–26. doi: 10.1093/ndt/gfn261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gulati S, Sahu KM, Avula S, Sharma RK, Ayyagiri A, Pandey CM. Role of vascular access as a risk factor for infections in hemodialysis. Ren Fail. 2003;25(6):967–73. doi: 10.1081/jdi-120026031. [DOI] [PubMed] [Google Scholar]


