Abstract
Exosomes are small (30 to 100 nm) membrane-bound particles that are released from normal, diseased, and neoplastic cells and are present in blood and other bodily fluids. Exosomes contain a variety of molecules including signal peptides, mRNA, microRNA, and lipids. Exosomes can function to export from cells unneeded endogenous molecules and therapeutic drugs. When exosomes are taken up by specific cells, they may act locally to provide autocrine or paracrine signals or, at a distance, as a newly described nanoparticle-based endocrine system. Specifically, mRNA transferred to cells by exosomes can result in the production of new proteins. In cancer, signals via exosomes affect the immune system by inhibiting the functions of T cells and normal killer (NK) cells and by inhibiting the differentiation of precursors to mature antigen-presenting cells. Also, exosomes increase the number and/or activity of immune suppressor cells, including myeloid-derived suppressor cells, T-regulatory cells, and CD14+, HLA-DR–/low cells. The effects of exosomes on the development and progression of cancers, with an emphasis on suppression of immune surveillance, is described. Also discussed are potential uses of exosomes clinically, in the development of vaccines, in targeting tumors, and in diagnosis and/or early detection.
Introduction
Exosomes are membrane-bound nanoparticles that are ovoid to cup shaped and develop from exophytic budding of the cellular membrane after the fusion of multivesicular bodies or mature endosomes with the cellular membrane (1–5). After release from diseased or normal cells, some exosomes are transported by the blood to distant sites (6). Thus, normal individuals have exosomes present in blood and other bodily fluids.
In studies of exosomes, exosomes usually are separated using ultra-centrifugation or by immunoprecipitation using antibodies to typical surface antigens of exosomes. Analysis of isolated exosomes has shown their morphology using electron microscopy and the localization of molecules in exosomes using either immunoelectron microscopy and/or fluorescent techniques. For biochemical analysis, exosomes isolated from bodily fluids are washed to remove contaminating bodily fluids. Also, controls frequently include the associated bodily fluids from which the exosomes have been removed.
Exosomes contain signal proteins and/or peptides, microRNAs, mRNAs, and lipids (7, 8). In exosomes from mast cells, mRNAs for more than 1,300 genes and more than 100 microRNAs were detected (7). Some of the mRNAs from exosomes have been shown to be functional, and murine exosomes that were “taken up” by human cells resulted in the synthesis of mouse proteins (7). How a molecule is determined to be excluded or included in exosomes and which molecules are functional after their cellular uptake are questions whose answers are still elusive; however, JAB1/CSN5, a component of the COP9 signalosome regulatory complex, may play a role in sorting ubiquitinated proteins into exosomes (9).
Exosomes aid in the removal of unneeded and/or harmful molecules from cells (2, 10, 11) including proteins without sequences for secretion. Of importance, exosomes can remove specific therapeutic drugs from cells, and cells releasing exosomes containing therapeutic drugs have been reported to be resistant to these drugs (11, 12). Specifically, Shedden and colleagues (12) correlated genes associated with the shedding of exosomes into a “vesicle shedding index,” which in the “National Cancer Institute (NCI) 60-cell-line panel” positively correlated with the 50% growth inhibition (GI50) for most of the 171 compounds of the NCI “Standard Anticancer Agent Database.” Also, when the actual shedding of exosomes from 6 cell lines were measured, the shedding rate correlated positively with resistance to doxorubicin, which is exported in exosomes; however, there was not a correlation with resistance to 5-fluorouracil, which is not extensively exported in exosomes.
Other functions of exosomes are not adequately characterized, including their functions in autocrine and paracrine signaling (7). Because exosomes provide signals to distant cells, exosomes act as a newly described nanoparticle-based endocrine system (7, 13). For cells affected by exosomes, cellular membranes and the surface molecules of exosomes interact in uptake of exosomes probably via class I and class II MHC molecules, ICAM-1, integrins, and tetraspanins on exosomal surfaces (13, 14).
Exosomes are present in biological fluids including ascites, pleural fluid, urine, and semen (15–18). Exosomes from different environments may have varying molecular and biophysical properties; prostasomes were described as round to egg shaped with internal vesicles and as ranging in size from 50 to 500 nm (16), but ascitic exosomes were similar to those in matching blood, which typically measure 30 to 100 nm (17). Exosomes obtained from media from some cultured cells are biphasic in size: 100 to 200 nm and 400 to 1,000 nm.
Neoplasia and exosomes
Tumor-derived (TD) exosomes can be isolated from tumors and bodily fluids from patients with tumors. Tumors reported to release exosomes include cancers of the breast, oral cavity, colorectum, brain, ovary, bladder, prostate, and melanomas (4, 18, 19). Exosomes in bodily fluids from patients with tumors are the same exosomes found in normal individuals plus TD exosomes. Exosomes contain molecules of the neoplastic cells of origin, for example, urinary exosomes have molecular features of associated urologic malignancies (15), and exosomes from patients with melanomas contain Melan A/Mart 1 (4). TD exosomes in the blood of patients with gliomas, which were assumed to be behind an intact blood-brain barrier, contained L1-NCAM/CD171, which was present in exosomes isolated from the brain tumors, but not in exosomes in blood from controls (6, 18); however, heat shock protein (HSP) 70 was detected in exosomes in blood from individuals with or without brain tumors (6). TD exosomes variably contain epidermal growth factor receptor (EGFR), EGFRvIII, HSPs 27, 60, 70, 72, 73, 80, and 90 (6, 18, 20), tumor necrosis factor alpha (TNFα), Fas ligand (FasL), and TGFβ (6, 7). How these heterogenic exosomes from different cells and the signal molecules they contain can preferentially target and modulate specific cells is yet to be determined.
Immune regulation by exosomes
Exosomal regulation of immunity is exemplified by autoimmunity. Treatment of dendritic cells (DC) by interleukin 10 (IL-10) increased secretions of exosomes, which inhibited inflammation as well as arthritis induced in animals by collagen injections (21). Exosomes from the salivary gland contain autoantigens that may be involved in autoimmunity (22). Some types of exosomes efficiently provide antigens to antigen-presenting cells (APC), which present these to T lymphocytes and NK cells (23, 24).
Fibroblasts from patients with rheumatoid arthritis produce exosomes containing TNFα, which can kill cells that are sensitive to TNFα (25) and induce in T cells the phosphorylation of Akt and increase nuclear factor kB (NFκB), potentially affecting the severity of rheumatoid arthritis. Exosomes also are involved in other diseases including liver inflammation caused by fatty diets and type 2 diabetes (26, 27).
Effects of exosomes in immune surveillance of neoplasia
The immune system should be activated as immune cells infiltrate and are activated by their contact with tumors and as neoplastic cells continuously die releasing antigens that cause production of acute phase reactants, activation of T and NK cells, and production of antibodies (28–31). Also, hypoxia causes increased cellular death and tissue damage, activating the immune system and releasing cytokines, for example, IL-6 and IL-8 (29, 30).
In contrast, tumors typically cause suppression of the immune system, which facilitates their growth and progression (31). Thus, tumors must have mechanisms that overcome their activation of the immune system. The involvement of TD exosomes in the progression of neoplasia is supported by our observation that tumors transplanted into mice increased in size compared with controls after injection into the mice of exosomes from the tumors. The mechanisms associated with the decrease in the size of tumors are postulated to be decreased cytotoxicity and reduced IL-2–mediated proliferation of both T and NK cells. The changes in NK cells involved decreased perforin release and inhibition of Jak-3 (17, 25, 32-34). Thus, immune suppression has been hypothesized to be mediated by exosomes (17, 25, 32–34).
Some tumors release exosomes that express FasL and/or tumor necrosis factor–related apoptosis-inducing ligand (TRAIL; refs. 17, 22, 35–37) and can cause apoptosis in activated T cells (17, 35–38). Specifically, exosomes from ovarian carcinomas that express FasL suppress CD-3ζ and Jak-3 in T lymphocytes, leading to apoptosis (33). Neither FasL nor TRAIL were expressed on the exosomes in our prior study (34), suggesting alternative mechanisms of immune suppression. For example, TD exosomes containing TGFβ1 cause a downregulation of the NKG2D receptor, which is an activating receptor for NK and CD8+T cells (23). Thus, the exosomes from tumors can partially suppress immune reactions by multiple mechanisms.
Immune suppression is facilitated via an increase in CD11b+ Gr-1+, myeloid-derived suppressor cells (MDSC) in the spleens, blood, and tumors of mice with syngenic tumors; this increase can be reversed by removal of the tumors (32, 39, 40). MDSCs in humans with tumors correlate with poor survival and tumor progression (39, 40, 41), probably via suppression of CD4+ and CD8+ lymphocytes and NK cells. MDSC-NK contact inhibits IL-2–mediated NK activation and expression of perforin via inhibiting the phosphorylation of Stat-5 (32). Increases in MDSCs may be secondary to release of both exosomes and soluble factors, for example, granulocyte-macrophage colony-stimulating factor (GM-CSF; refs. 34, 39, 40, 42–44). Exosomes also increase MDSCs via TGFβ and regulation of prostaglandin E2 (PGE2; ref. 45). In addition, HSP 72 on exosomes may interact with toll-like receptor 2 and MyD88 of MDSCs, causing activation of MDSCs via increased expression of IL-6 and phosphorylation of Stat 3 (20, 46). However, the biological effects of TD exosomes via toll-like receptor pathways should be evaluated carefully because tumor cells undergoing many passages frequently have different phenotypes than cells isolated in vivo from tumors.
Because exosomes from DCs can potentiate presentation of antigens by APCs so that they attack tumors and, thus, inhibit tumor growth (4, 47–52), TD exosomes could inhibit immune responses by reducing APCs. In support of this, TD exosomes cause time-dependent inhibition of the maturation of immature DCs via a dose-dependent, increased expression of IL-6 and phosphorylation of Stat 3 (32, 49). Similarly, TD exosomes impair the differentiation of CD14+ monocytes to APCs and generate a CD14+ HLA-D –/low subset of cells, which can secrete TGFβ-inhibiting T cells (50).
Exosomal suppression of immunity may also be caused by a transition of CD4+, CD25– T cells to CD4+, CD25+, Foxp3+ T-regulatory cells (Treg) via phosphorylation of SMAD2/3 and Stat3 (53). Such interactions in peripheral tissues mediated by TD exosomes may participate in the maintenance of immune tolerance (54, 55).
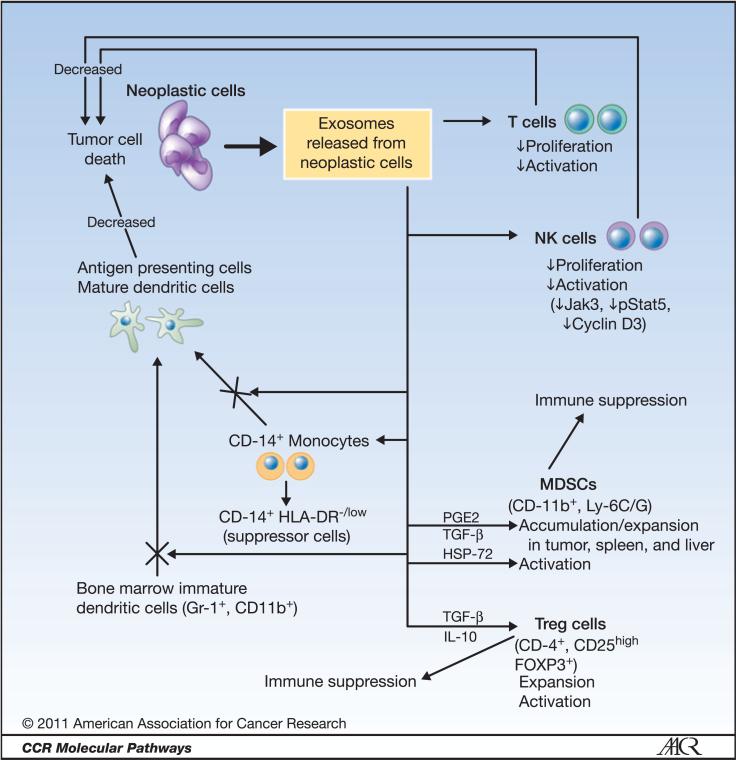
Thus, exosomes from DCs would be expected to cause tumor regression; however, this response is decreased by signals mediated by TD exosomes that inhibit the maturation of DCs, cause increases in MDSCs, Tregs, and CD14+, HLA-DR–/low cells, and reduce numbers and cytotoxic capabilities of T and NK cells (see murine model; Fig. 1).
Figure 1.
A murine model of the multiple actions to suppress immune surveillance of exosomes released from neoplastic cells. Exosomes reduce APCs (i.e., mature DCs), and the activity and/or proliferation of NK and T cells. In addition, cells that suppress the immune system, including Treg, MDSCs, and CD14+, HLA-DR–/low are increased in number and/or activity via the actions of exosomes. Overall these actions reduce the cytotoxicity against tumor cells of the immune system.
Clinical-Translational Advances
Because TD exosomes contain many molecules characteristic of their matched tumors, exosomes have been proposed as a vehicle via which cytotoxic T-lymphocyte responses (CTL) could be increased via the interaction of TD exosomes and DCs (2). The production of exosomes derived from the DCs could be carried out in vitro to avoid the immunosuppressive effects of TD exosomes. Such approaches have been shown to be relatively safe and have resulted in limited responses in patients with tumors (56, 57).
In contrast, because TD exosomes are involved in the suppression of the immune system in patients with cancers, TD exosomes could be targeted to permit the immune system to suppress tumors more effectively. Specifically, developing strategies to prevent the selective sorting of molecules into TD exosomes that could suppress the immune system could lead to exosomes that can activate immune cells and target tumors in an antigen-specific manner. Also, because exosomes act in the selective removal of some drugs (e.g., doxorubicin and cis-platinum) from cells (11, 12), targeting exosomes might have a dual effect by making specific drugs more effective. Approaches to targeting TD exosomes could also rely on drugs that affect the secretion and/or release of exosomes. An alternative approach could be to selectively remove TD exosomes from the circulation using purification of blood, for example, the use of a “hemopurifier” adapted to remove TD exosomes (53). Specifically, this removal might be accomplished via bound antibodies similar to those currently used to precipitate exosomes.
Because exosomes may be taken up selectively by the cells of tumors, exosomes may serve as a specific delivery system of molecules and/or drugs targeted to specific tumors. The polyphenol, curcumin, has been reported to have antiinflammatory and antitumor activities (58, 59). Curcumin also reduces the inhibitory effects of exosomes on NK cytotoxicity (60). The poor solubility of curcumin has limited its usefulness, although its bioavailability and activity can be improved by its encapsulation in liposomes (61). However, the delivery of curcumin by exosomes was found to be much more effective than delivery by liposomes in preventing septic shock (62). This finding shows how drugs could be delivered selectively by exosomes to target specific cellular populations.
TD exosomes contain some molecular features of tumors at an enriched concentration. Thus, the detection of the biomarkers in exosomes might be useful in early detection, diagnosis, and risk assessment, and for determining prognosis of tumors (29, 30). For example, exosomes collected from the blood of women with ovarian carcinoma contained the biomarker claudin-4 (63) and from patients with lung carcinomas, microRNAs that could aid in the diagnosis of lung cancer (64). In addition, δ-catenin, a potential biomarker of prostate cancer, has been found in urinary exosomes from patients with prostatic adenocarcinomas (65).
In summary, exosomes function as a newly described pathway of intercellular communication, which may be a major factor in suppression of immune surveillance in patients with specific tumors. In addition, exosomes are likely involved in the resistance of some tumors to various chemotherapeutic agents. Thus, the release of exosomes from tumors or circulating exosomes might be novel targets for therapy. Also, exosomes could represent a vehicle for selective delivery to tumors of drugs, therapeutic small molecules, or agents for gene therapy. In addition, molecules in exosomes might serve as biomarkers for the early detection and diagnosis of diseases, for determining prognosis, and for prediction of therapeutic efficacy via a molecular pattern of exosomes, which differs from that of the exosomes found either in associated different diseased controls or in normal controls.
Acknowledgments
Grant Support
Supported in part by the Early Detection Research Network (EDRN), grant number 5U24CA086359–10, and Susan G. Komen for the Cure, grant number BCTR0600484, and the Breast (CA089019) and Pancreatic (CA101955) SPORES at the University of Alabama at Birmingham.
Footnotes
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
- 1.Trams EG, Lauter CJ, Salem N, Jr, Heine U. Exfoliation of membrane ecto-enzymes in the form of micro-vesicles. Biochim Biophys Acta. 1981;645:63–70. doi: 10.1016/0005-2736(81)90512-5. [DOI] [PubMed] [Google Scholar]
- 2.Johnstone RM, Adam M, Hammond JR, Orr L, Turbide C. Vesicle formation during reticulocyte maturation. Association of plasma membrane activities with released vesicles (exosomes). J Biol Chem. 1987;262:9412–20. [PubMed] [Google Scholar]
- 3.Clayton A, Court J, Navabi H, Adams M, Mason MD, Hobot JA, et al. Analysis of antigen presenting cell derived exosomes, based on immuno-magnetic isolation and flow cytometry. J Immunol Methods. 2001;247:163–74. doi: 10.1016/s0022-1759(00)00321-5. [DOI] [PubMed] [Google Scholar]
- 4.Wolfers J, Lozier A, Raposo G, Regnault A, Théry C, Masurier C, et al. Tumor-derived exosomes are a source of shared tumor rejection antigens for CTL cross-priming. Nat Med. 2001;7:297–303. doi: 10.1038/85438. [DOI] [PubMed] [Google Scholar]
- 5.Théry C, Zitvogel L, Amigorena S. Exosomes: composition, biogenesis and function. Nat Rev Immunol. 2002;2:569–79. doi: 10.1038/nri855. [DOI] [PubMed] [Google Scholar]
- 6.Graner MW, Alzate O, Dechkovskaia AM, Keene JD, Sampson JH, Mitchell DA, et al. Proteomic and immunologic analyses of brain tumor exosomes. FASEB J. 2009;23:1541–57. doi: 10.1096/fj.08-122184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Valadi H, Ekström K, Bossios A, Sjöstrand M, Lee JJ, Lötvall JO. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol. 2007;9:654–9. doi: 10.1038/ncb1596. [DOI] [PubMed] [Google Scholar]
- 8.Thëry C, Boussac M, Véron P, Ricciardi-Castagnoli P, Raposo G, Garin J, et al. Proteomic analysis of dendritic cell-derived exosomes: a secreted subcellular compartment distinct from apoptotic vesicles. J Immunol. 2001;166:7309–18. doi: 10.4049/jimmunol.166.12.7309. [DOI] [PubMed] [Google Scholar]
- 9.Liu Y, Shah SV, Xiang X, Wang J, Deng ZB, Liu C, et al. COP9-associated CSN5 regulates exosomal protein deubiquitination and sorting. Am J Pathol. 2009;174:1415–25. doi: 10.2353/ajpath.2009.080861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blanc L, Barres C, Bette-Bobillo P, Vidal M. Reticulocyte-secreted exosomes bind natural IgM antibodies: involvement of a ROS-activatable endosomal phospholipase iPLA2. Blood. 2007;110:3407–16. doi: 10.1182/blood-2007-04-085845. [DOI] [PubMed] [Google Scholar]
- 11.Safaei R, Larson BJ, Cheng TC, Gibson MA, Otani S, Naerdemann W, et al. Abnormal lysosomal trafficking and enhanced exosomal export of cisplatin in drug-resistant human ovarian carcinoma cells. Mol Cancer Ther. 2005;4:1595–604. doi: 10.1158/1535-7163.MCT-05-0102. [DOI] [PubMed] [Google Scholar]
- 12.Shedden K, Xie XT, Chandaroy P, Chang YT, Rosania GR. Expulsion of small molecules in vesicles shed by cancer cells: association with gene expression and chemosensitivity profiles. Cancer Res. 2003;63:4331–7. [PubMed] [Google Scholar]
- 13.Blanc L, De Gassart A, Gëminard C, Bette-Bobillo P, Vidal M. Exosome release by reticulocytes—an integral part of the red blood cell differentiation system. Blood Cells Mol Dis. 2005;35:21–6. doi: 10.1016/j.bcmd.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 14.Savill J, Dransfield I, Gregory C, Haslett C. A blast from the past: clearance of apoptotic cells regulates immune responses. Nat Rev Immunol. 2002;2:965–75. doi: 10.1038/nri957. [DOI] [PubMed] [Google Scholar]
- 15.Welton JL, Khanna S, Giles PJ, Brennan P, Brewis IA, Staffurth J, et al. Proteomics analysis of bladder cancer exosomes. Mol Cell Proteomics. 2010;9:1324–38. doi: 10.1074/mcp.M000063-MCP201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Poliakov A, Spilman M, Dokland T, Amling CL, Mobley JA. Structural heterogeneity and protein composition of exosome-like vesicles (prostasomes) in human semen. Prostate. 2009;69:159–67. doi: 10.1002/pros.20860. [DOI] [PubMed] [Google Scholar]
- 17.Taylor DD, Gerçel-Taylor C. Tumour-derived exosomes and their role in cancer-associated T-cell signalling defects. Br J Cancer. 2005;92:305–11. doi: 10.1038/sj.bjc.6602316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Graner MW, Cumming RI, Bigner DD. The heat shock response and chaperones/heat shock proteins in brain tumors: surface expression, release, and possible immune consequences. J Neurosci. 2007;27:11214–27. doi: 10.1523/JNEUROSCI.3588-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang H-G, Liu Y, Deng Z-B, Liu C, Xiang X, Grizzle WE. Exosomes and immune surveillance of neoplastic lesions: a review. Biotech Histochem. 2011 doi: 10.3109/10520291003659042. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chalmin F, Ladoire S, Mignot G, Vincent J, Bruchard M, Remy-Martin J-P, et al. Membrane-associated Hsp72 from tumor-derived exosomes mediates STAT3-dependent immunosuppressive function of mouse and human myeloid-derived suppressor cells. J Clin Invest. 2010;120:457–71. doi: 10.1172/JCI40483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim SH, Lechman ER, Bianco N, Menon R, Keravala A, Nash J, et al. Exosomes derived from IL-10-treated dendritic cells can suppress inflammation and collagen-induced arthritis. J Immunol. 2005;174:6440–8. doi: 10.4049/jimmunol.174.10.6440. [DOI] [PubMed] [Google Scholar]
- 22.Kapsogeorgou EK, Abu-Helu RF, Moutsopoulos HM, Manoussakis MN. Salivary gland epithelial cell exosomes: A source of autoantigenic ribonucleoproteins. Arthritis Rheum. 2005;52:1517–21. doi: 10.1002/art.21005. [DOI] [PubMed] [Google Scholar]
- 23.Clayton A, Mitchell JP, Court J, Linnane S, Mason MD, Tabi Z. Human tumor-derived exosomes down-modulate NKG2D expression. J Immunol. 2008;180:7249–58. doi: 10.4049/jimmunol.180.11.7249. [DOI] [PubMed] [Google Scholar]
- 24.Vincent-Schneider H, Stumptner-Cuvelette P, Lankar D, Pain S, Raposo G, Benaroch P, et al. Exosomes bearing HLA-DR1 molecules need dendritic cells to efficiently stimulate specific T cells. Int Immunol. 2002;14:713–22. doi: 10.1093/intimm/dxf048. [DOI] [PubMed] [Google Scholar]
- 25.Zhang HG, Liu C, Su K, Yu S, Zhang L, Zhang S, et al. A membrane form of TNF-alpha presented by exosomes delays T cell activation-induced cell death. J Immunol. 2006;176:7385–93. doi: 10.4049/jimmunol.176.12.7385. [DOI] [PubMed] [Google Scholar]
- 26.Deng ZB, Liu Y, Liu C, Xiang X, Wang J, Cheng Z, et al. Immature myeloid cells induced by a high-fat diet contribute to liver inflammation. Hepatology. 2009;50:1412–20. doi: 10.1002/hep.23148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Deng ZB, Poliakov A, Hardy RW, Clements R, Liu C, Liu Y, et al. Adipose tissue exosome-like vesicles mediate activation of macrophage-induced insulin resistance. Diabetes. 2009;58:2498–505. doi: 10.2337/db09-0216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chatterjee M, Wojciechowski J, Tainsky MA. Discovery of antibody biomarkers using protein microarrays of tumor antigens cloned in high throughput. Methods Mol Biol. 2009;520:21–38. doi: 10.1007/978-1-60327-811-9_3. [DOI] [PubMed] [Google Scholar]
- 29.Grizzle WE, Srivastava S, Manne U. Translational pathology of cancer. In: Srivastava S, Grizzle WE, editors. Translational pathology of early cancer. IOS Press BV; Amsterdam: 2011. [Google Scholar]
- 30.Grizzle WE, Srivastava S, Manne U. The biology of incipient, preinvasive or intraepithelial neoplasia. In: Srivastava S, Grizzle WE, editors. Translational pathology of early cancer. IOS Press BV; Amsterdam: 2011. [Google Scholar]
- 31.Zhang HG, Grizzle WE. Aging, immunity, and tumor susceptibility. Immunol Allergy Clin North Am. 2003;23:83–102. vi [vi.]. doi: 10.1016/s0889-8561(02)00085-1. [DOI] [PubMed] [Google Scholar]
- 32.Liu C, Yu S, Kappes J, Wang J, Grizzle WE, Zinn KR, et al. Expansion of spleen myeloid suppressor cells represses NK cell cytotoxicity in tumor-bearing host. Blood. 2007;109:4336–42. doi: 10.1182/blood-2006-09-046201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Taylor DD, Gerçel-Taylor C, Lyons KS, Stanson J, Whiteside TL. T-cell apoptosis and suppression of T-cell receptor/CD3-ζ by Fas ligand-containing membrane vesicles shed from ovarian tumors. Clin Cancer Res. 2003;9:5113–9. [PubMed] [Google Scholar]
- 34.Taylor DD, Akyol S, Gerçel-Taylor C. Pregnancy-associated exosomes and their modulation of T cell signaling. J Immunol. 2006;176:1534–42. doi: 10.4049/jimmunol.176.3.1534. [DOI] [PubMed] [Google Scholar]
- 35.Kim SH, Bianco N, Menon R, Lechman ER, Shufesky WJ, Morelli AE, et al. Exosomes derived from genetically modified DC expressing FasL are anti-inflammatory and immunosuppressive. Mol Ther. 2006;13:289–300. doi: 10.1016/j.ymthe.2005.09.015. [DOI] [PubMed] [Google Scholar]
- 36.Kim JW, Wieckowski E, Taylor DD, Reichert TE, Watkins S, Whiteside TL. Fas ligand-positive membranous vesicles isolated from sera of patients with oral cancer induce apoptosis of activated T lymphocytes. Clin Cancer Res. 2005;11:1010–20. [PubMed] [Google Scholar]
- 37.Abusamra AJ, Zhong Z, Zheng X, Li M, Ichim TE, Chin JL, et al. Tumor exosomes expressing Fas ligand mediate CD8+ T-cell apoptosis. Blood Cells Mol Dis. 2005;35:169–73. doi: 10.1016/j.bcmd.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 38.Sabapatha A, Gerçel-Taylor C, Taylor DD. Specific isolation of placenta-derived exosomes from the circulation of pregnant women and their immunoregulatory consequences. Am J Reprod Immunol. 2006;56:345–55. doi: 10.1111/j.1600-0897.2006.00435.x. [DOI] [PubMed] [Google Scholar]
- 39.Serafini P, De Santo C, Marigo I, Cingarlini S, Dolcetti L, Gallina G, et al. Derangement of immune responses by myeloid suppressor cells. Cancer Immunol Immunother. 2004;53:64–72. doi: 10.1007/s00262-003-0443-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol. 2009;9:162–74. doi: 10.1038/nri2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Serafini P, Borrello I, Bronte V. Myeloid suppressor cells in cancer: recruitment, phenotype, properties, and mechanisms of immune suppression. Semin Cancer Biol. 2006;16:53–65. doi: 10.1016/j.semcancer.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 42.Almand B, Clark JI, Nikitina E, van Beynen J, English NR, Knight SC, et al. Increased production of immature myeloid cells in cancer patients: a mechanism of immunosuppression in cancer. J Immunol. 2001;166:678–89. doi: 10.4049/jimmunol.166.1.678. [DOI] [PubMed] [Google Scholar]
- 43.Ochoa AC, Zea AH, Hernandez C, Rodriguez PC. Arginase, prostaglandins, and myeloid-derived suppressor cells in renal cell carcinoma. Clin Cancer Res. 2007;13:721s–6s. doi: 10.1158/1078-0432.CCR-06-2197. [DOI] [PubMed] [Google Scholar]
- 44.Diaz-Montero CM, Salem ML, Nishimura MI, Garrett-Mayer E, Cole DJ, Montero AJ. Increased circulating myeloid-derived suppressor cells correlate with clinical cancer stage, metastatic tumor burden and doxorubicin-cyclophosphamide chemotherapy. Cancer Immunol Immunother. 2009;58:49–59. doi: 10.1007/s00262-008-0523-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xiang X, Poliakov A, Liu C, Liu Y, Deng ZB, Wang J, et al. Induction of myeloid-derived suppressor cells by tumor exosomes. Int J Cancer. 2009;124:2621–33. doi: 10.1002/ijc.24249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu Y, Xiang X, Zhuang X, Zhang S, Liu C, Cheng Z, et al. Contribution of MyD88 to the tumor exosome-mediated induction of myeloid derived suppressor cells. Am J Pathol. 2010;176:2490–9. doi: 10.2353/ajpath.2010.090777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zitvogel L, Regnault A, Lozier A, Wolfers J, Flament C, Tenza D, et al. Eradication of established murine tumors using a novel cell-free vaccine: dendritic cell-derived exosomes. Nat Med. 1998;4:594–600. doi: 10.1038/nm0598-594. [DOI] [PubMed] [Google Scholar]
- 48.Andre F, Schartz NE, Movassagh M, Flament C, Pautier P, Morice P, et al. Malignant effusions and immunogenic tumour-derived exosomes. Lancet. 2002;360:295–305. doi: 10.1016/S0140-6736(02)09552-1. [DOI] [PubMed] [Google Scholar]
- 49.Yu S, Liu C, Su K, Wang J, Liu Y, Zhang L, et al. Tumor exosomes inhibit differentiation of bone marrow dendritic cells. J Immunol. 2007;178:6867–75. doi: 10.4049/jimmunol.178.11.6867. [DOI] [PubMed] [Google Scholar]
- 50.Valenti R, Huber V, Filipazzi P, Pilla L, Sovena G, Villa A, et al. Human tumor-released microvesicles promote the differentiation of myeloid cells with transforming growth factor-b-mediated suppressive activity on T lymphocytes. Cancer Res. 2006;66:9290–8. doi: 10.1158/0008-5472.CAN-06-1819. [DOI] [PubMed] [Google Scholar]
- 51.Luketic L, Delanghe J, Sobol PT, Yang P, Frotten E, Mossman KL, et al. Antigen presentation by exosomes released from peptide-pulsed dendritic cells is not suppressed by the presence of active CTL. J Immunol. 2007;179:5024–32. doi: 10.4049/jimmunol.179.8.5024. [DOI] [PubMed] [Google Scholar]
- 52.Viaud S, Terme M, Flament C, Taieb J, André F, Novault S, et al. Dendritic cell-derived exosomes promote natural killer cell activation and proliferation: a role for NKG2D ligands and IL-15Ralpha. PLoS ONE. 2009;4:e4942. doi: 10.1371/journal.pone.0004942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Szajnik M, Czystowska M, Szczepanski MJ, Mandapathil M, Whiteside TL. Tumor-derived microvesicles induce, expand and up-regulate biological activities of human regulatory T cells (Treg). PLoS ONE. 2010;5:e11469. doi: 10.1371/journal.pone.0011469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wang GJ, Liu Y, Qin A, Shah SV, Deng ZB, Xiang X, et al. Thymus exosomes-like particles induce regulatory T cells. J Immunol. 2008;181:5242–8. doi: 10.4049/jimmunol.181.8.5242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ichim TE, Zhong Z, Kaushal S, Zheng X, Ren X, Hao X, et al. Exosomes as a tumor immune escape mechanism: possible therapeutic implications. J Transl Med. 2008;6:37. doi: 10.1186/1479-5876-6-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Andre F, Escudier B, Angevin E, Tursz T, Zitvogel L. Exosomes for cancer immunotherapy. Ann Oncol. 2004;15(Suppl 4):iv141–4. doi: 10.1093/annonc/mdh918. [DOI] [PubMed] [Google Scholar]
- 57.Iero M, Valenti R, Huber V, Filipazzi P, Parmiani G, Fais S, et al. Tumour-released exosomes and their implications in cancer immunity. Cell Death Differ. 2008;15:80–8. doi: 10.1038/sj.cdd.4402237. [DOI] [PubMed] [Google Scholar]
- 58.Jaiswal AS, Marlow BP, Gupta N, Narayan S. b-catenin-mediated transactivation and cell-cell adhesion pathways are important in curcumin (diferuylmethane)-induced growth arrest and apoptosis in colon cancer cells. Oncogene. 2002;21:8414–27. doi: 10.1038/sj.onc.1205947. [DOI] [PubMed] [Google Scholar]
- 59.Narayan S. Curcumin,a multi-functional chemopreventiveagent, blocks growth of colon cancer cells by targeting b-catenin-mediated transactivation and cell-cell adhesion pathways. J Mol Histol. 2004;35:301–7. doi: 10.1023/b:hijo.0000032361.98815.bb. [DOI] [PubMed] [Google Scholar]
- 60.Zhang HG, Kim H, Liu C, Yu S, Wang J, Grizzle WE, et al. Curcumin reverses breast tumor exosomes mediated immune suppression of NK cell tumor cytotoxicity. Biochim Biophys Acta. 2007;1773:1116–23. doi: 10.1016/j.bbamcr.2007.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Narayanan NK, Nargi D, Randolph C, Narayanan BA. Liposome encapsulation of curcumin and resveratrol in combination reduces prostate cancer incidence in PTEN knockout mice. Int J Cancer. 2009;125:1–8. doi: 10.1002/ijc.24336. [DOI] [PubMed] [Google Scholar]
- 62.Sun D, Zhuang X, Xiang X, Liu Y, Zhang S, Liu C, et al. A novel nanoparticle drug delivery system. The anti-inflammatory activity of curcumin is enhanced when encapsulated in exosomes. Mol Ther. 2010;18:1606–14. doi: 10.1038/mt.2010.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Li J, Sherman-Baust CA, Tsai-Turton M, Bristow RE, Roden RB, Morin PJ. Claudin-containing exosomes in the peripheral circulation of women with ovarian cancer. BMC Cancer. 2009;9:244. doi: 10.1186/1471-2407-9-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rabinowits G, Gerçel-Taylor C, Day JM, Taylor DD, Kloecker GH. Exosomal microRNA: a diagnostic marker for lung cancer. Clin Lung Cancer. 2009;10:42–6. doi: 10.3816/CLC.2009.n.006. [DOI] [PubMed] [Google Scholar]
- 65.Lu Q, Zhang J, Allison R, Gay H, Yang W-X, Bhowmick NA, et al. Identification of extracellular δ-catenin accumulation for prostate cancer detection. Prostate. 2009;69:411–8. doi: 10.1002/pros.20902. [DOI] [PMC free article] [PubMed] [Google Scholar]