Abstract
Aims
We compared the prevalence and treatment of type 2 diabetes across Asian American subgroups (Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese) and Non-Hispanic Whites (NHWs) in a Northern California healthcare system.
Methods
A three-year, cross-sectional sample of patient electronic health records was accessed to compare diabetes prevalence in 21,816 Asian and 73,728 NHWs aged 35+ years. Diabetes was classified through ICD-9 codes, abnormal laboratory values, or use of oral anti-diabetic medication. Multivariate adjusted prevalence rates for each Asian subgroup, and adjusted odds ratios (OR) relative to NHWs, were compared.
Results
Age-adjusted prevalence ranged from 5.8%-18.2% (women) and 8.1%-25.3% (men). Age-adjusted ORs of Asian subgroups ranged 1.11-3.94 (women) and 1.14-4.56 (men). The odds of diabetes were significantly higher in Asian Indians (women OR 3.44, men OR 3.54) and Filipinos (women OR 3.94, men OR 4.56), compared to NHWs. Results for Asian Indians and Filipinos were similar with age-and-BMI adjustment. Treatment rates across subgroups were 59.7-82.0% (women) and 62.9-79.4% (men).
Conclusions
Heterogeneity exists in the prevalence of diabetes across Asian subgroups, independent of obesity prevalence. Asian Indian and Filipino subgroups had particularly high prevalence of diabetes when compared to NHWs. Future studies should explore these clinically important differences among Asian subgroups.
Keywords: diabetes, prevalence, Asian American, racial/ethnic subgroup
Introduction
Asian Americans are among the fastest growing minority populations in the U.S., increasing 72% between 1990 and 2000.[1] The number of Asian Americans, at over 14 million, is projected to reach nearly 34 million by 2050.[2] According to the 2000 U.S. Census, 87.5% of Asian Americans belong to one of the six largest Asian racial/ethnic subgroups: Asian Indian (16%), Chinese (24%), Filipino (18%), Japanese (8%), Korean (11%), and Vietnamese (11%), with subgroup population sizes ranging from about 800,000 to 2.3 million.[3, 4] Though Asian Americans account for only 4% of the total U.S. population, they constitute 11% of California’s population. Over 36% of all Asian Americans live in California.
Self-report survey data have shown that as an aggregated group, Asian Americans have an increased prevalence of type 2 diabetes when compared with Non-Hispanic Whites (NHWs).[5, 6] The prevalence of type 2 diabetes in aggregated Asian Americans, after adjustment for age, sex, and BMI (using self-reported height and weight), has been shown to be 60% higher than that of NHWs.[5] Little is known about the differences in prevalence of type 2 diabetes across the Asian American racial/ethnic subgroups. Chronic diseases such as type 2 diabetes manifest differently in specific racial/ethnic groups;[7, 8] thus, the use of aggregate data may mask the heterogeneity in type 2 diabetes prevalence across Asian American racial/ethnic subgroups.
The limited data that are available suggests that there may well be extensive heterogeneity in type 2 diabetes prevalence among Asian American subgroups.[9-11] Several small and geographically disparate studies have shown that Asian Indians,[12, 13] Filipinos[14-16] and Japanese[17] have increased risk of type 2 diabetes compared to NHWs, while Chinese[18, 19] are believed to have lower risk. These studies have either been limited to comparing one particular Asian American subgroup to NHWs,[14, 17] preventing examination of potential differences across Asian American subgroups, or these studies have compared type 2 diabetes prevalence in specific Asian American subgroups to cohorts of NHWs from another study.[12] Only a few studies have compared type 2 diabetes prevalence among disaggregated Asian American subgroups. These studies, however, use data from the National Health Interview Survey (NHIS)[9-11] and the California Health Interview Survey (CHIS)[20] and are limited by their reliance on self-report in defining type 2 diabetes.
Most of the large studies on racial/ethnic differences in type 2 diabetes treatment use data from the National Health and Nutrition Examination Survey (NHANES) III and compare Black/African Americans and Hispanic/Latinos with NHWs.[21-23] There is no information about differences in type 2 diabetes treatment among Asian Americans. Studies of type 2 diabetes prevalence and treatment across all six major Asian American subgroups from the same population using clinical data would facilitate comparisons and allow identification of high risk racial/ethnic subgroups.
Thus far, no studies have investigated type 2 diabetes prevalence using clinical data from electronic health records (EHR) in a large, disaggregated Asian American sample with representation from the six largest racial/ethnic subgroups. Additionally, previous studies have not examined Asian American racial/ethnic subgroup differences in type 2 diabetes treatment rates. We therefore sought to characterize the prevalence and treatment of type 2 diabetes using the EHR in a large, racially/ethnically diverse population of Asian Americans with similar socioeconomic background and access to healthcare.
Research Design and Methods
Setting
The demographic characteristics of the clinical population are similar to those of residents in the underlying service area in Northern California (Alameda, San Mateo and Santa Clara counties) with respect to race/ethnicity and age distribution, but the clinical population has a slightly higher proportion of women, NHWs and Asians, and a lower proportion of Black/African Americans and Hispanic/Latinos. Among Asian Americans, the representation of Koreans and Vietnamese in the clinic is disproportionately lower when compared to the service area. There is no difference between racial/ethnic groups in employment status; however there is some variation in median household income. Of the racial/ethnic subgroups, Asian Indians have a higher median household income compared to Vietnamese in the underlying service area. The patient population is insured (58% PPO, 23% HMO, 16% Medicare, 2% self-payer, and 1% Medicaid) and thus under-represents the medically underserved. The EpicCare EHR system[24] has been in use since 2000.
Study Design
A three-year, cross-sectional sample of patient EHRs was studied. Patients who had visited primary care departments between January 1, 2007 and December 31, 2009, and who were 35 years or older, were included. Data on patient demographics, anthropometric measures, physician diagnoses, laboratory results and prescription medications were extracted from the EHR. Only patients identified as Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese, or NHW through self-report[25] (49%) or by names[25] (51%) were included in analyses. A sensitivity analysis on the subset of patients with self-identified race/ethnicity was conducted with comparable conclusions to the primary analyses (results not shown). Over 78% of the study population had at least one glucose value on record. Results were presented for Asian Americans as an aggregated group and across individual racial/ethnic subgroups, and both compared to NHWs. All data sets analyzed by the research team were de-identified according to the Health Insurance Portability and Accountability Act (HIPAA) standard.
Clinical Definition of Type 2 Diabetes
Patients were classified as ever having type 2 diabetes during the three-year cross-sectional period (2007-2009). Patients were identified with type 2 diabetes using physician recorded diagnosis codes (87%), abnormal laboratory values according to American Diabetes Association guidelines (additional 5%),[26] or use of any oral anti-diabetic medication (additional 8%). Specifically, any of the following events qualified for a diagnosis of type 2 diabetes: physician recorded ICD-9 code of 250.X0 or 250.X2; any two abnormal laboratory values defined as hemoglobin A1c results ≥6.5%, fasting blood glucose results ≥126 mg/dL, random blood glucose ≥200 mg/dL, or oral glucose tolerance test ≥200 mg/dL; or use of any oral anti-diabetic medication. The formulary of oral anti-diabetic medications was selected by an expert panel of physicians. The treatment rate was estimated only for the subgroup of patients classified as diabetic through physician recorded ICD-9 codes and abnormal laboratory values.
Statistical Methods
The analyses sought to estimate the unadjusted, age-adjusted, and age-and-BMI adjusted prevalence, risk and treatment of type 2 diabetes by race/ethnicity and sex. Patient characteristics (age and BMI) were compared using chi-square tests or non-parametric Wilcoxon tests. Age-adjusted prevalence rates were calculated using direct standardization to the PAMF NHW population. Broad age categories (35-44, 45-54, 55-65, 65+ years), and BMI categories (<25, 25-30, 30+ kg/m2) were used to achieve stratum-specific rates for direct standardization. For age-and-BMI adjusted estimates, 11% of patients did not have a BMI available and were excluded only for age-and-BMI adjusted prevalence estimates. The subset without an available BMI, mostly due to missing height in the database, were older, a higher proportion of men, and a higher proportion of NHWs.
Direct standardization requires the categorization of all adjustment variables, and can suffer from residual confounding depending on the construction of categories.[27] Odds ratios calculated from logistic regression can provide an alternative estimate for the relative association of type 2 diabetes across racial/ethnic groups with more flexible modeling of the outcome and adjustment variables. Unlike direct standardization, logistic regression is restricted by the usual assumptions of regression and model fit. Thus both direct standardization and logistic regression have strengths and limitations, and we employed both of these methods to confirm the robustness of our conclusions. Logistic regression was used to estimate age- and age-and-BMI adjusted odds ratios for each racial/ethnic subgroup. Regression models were calculated separately for women and men with type 2 diabetes as the outcome. Each model included indicator variables for racial/ethnic subgroups, 5-year age categories, BMI as a continuous variable, and BMI2 to account for higher order contributions of BMI. NHW was the referent group in all models. As an alternative comparative metric, prevalence ratios for each Asian subgroup relative to NHWs were examined using log-binomial regression, and provided the same conclusions (results available upon request).
Treatment with an oral anti-diabetic medication was measured using data on prescriptions in the EHR. Among patients classified as having type 2 diabetes by physician recorded ICD-9 codes or abnormal laboratory values, we examined whether an oral anti-diabetic medication was ever prescribed by a provider. Proportions with Wilson confidence intervals are reported.
For all analyses, statistical significance was determined at P<0.05, and 95% confidence intervals are reported when appropriate. Statistical analyses were performed using SAS 9.2 (Cary, NC).
Results
A total of 95,544 eligible records were identified, for 21,816 Asian American patients and 73,728 NHW patients over the age of 35 years (Table 1). The age distribution was generally younger for Asian American subgroups, and average BMI was lower compared to NHWs. Among Asian subgroups, Asian Indians and Filipinos had the highest average BMI for both women and men. Unadjusted type 2 diabetes prevalence in women ranged from 4.3% for Koreans and Vietnamese to 14.8% for Filipinos (Table 2). Unadjusted type 2 diabetes prevalence in men ranged from 6.6% for Vietnamese to 22.2% for Filipinos. The Asian American subgroups with the highest unadjusted prevalence rates were Asian Indian women (11.2%) and men (13.8%) and Filipino women (14.8%) and men (22.2%) (Table 2).
Table 1.
Characteristics of Patients Aged 35 Years or Older (N=95,544)
| NHW | Asian (all) | Asian Indian |
Chinese | Filipino | Japanese | Korean | Vietnamese | |
|---|---|---|---|---|---|---|---|---|
| Total (N) | 73,728 | 21,816 | 5,171 | 10,693 | 2,276 | 1,605 | 933 | 1,138 |
|
WOMEN
(N, %) |
41,595(56) | 12,388(57) | 2,373(46) | 6,267(59) | 1,467(64) | 1,029(64) | 582(62) | 670(59) |
| Age (y) (N, %) | ||||||||
| 35 – 39 | 3,906(9) | 2,303(19) | 643(27) | 1,021(16) | 267(18) | 103(10) | 142(24) | 127(19) |
| 40 – 44 | 6,404(15) | 2,936(24) | 683(29) | 1,440(23) | 291(20) | 183(18) | 156(27) | 183(27) |
| 45 – 49 | 6,504(16) | 2,242(18) | 355(15) | 1,234(20) | 236(16) | 195(19) | 93(16) | 129(19) |
| 50 – 54 | 5,885(14) | 1,498(12) | 187(8) | 802(13) | 205(14) | 148(14) | 60(10) | 96(14) |
| 55 – 59 | 4,873(12) | 995(8) | 158(7) | 520(8) | 151(10) | 89(9) | 32(6) | 45(7) |
| 60 – 64 | 4,009(10) | 689(6) | 97(4) | 342(6) | 124(9) | 76(7) | 29(5) | 21(3) |
| 65 – 69 | 2,863(7) | 537(4) | 99(4) | 260(4) | 70(5) | 58(6) | 28(5) | 22(3) |
| 70 – 74 | 1,914(5) | 445(4) | 64(3) | 256(4) | 47(3) | 37(4) | 23(4) | 18(3) |
| 75 – 79 | 1,546(4) | 309(3) | 53(2) | 157(3) | 32(2) | 46(5) | 11(2) | 10(2) |
| 80 – 84 | 1,499(4) | 222(2) | 21(1) | 115(2) | 24(2) | 46(5) | 4(1) | 12(2) |
| 85 + | 2,192(5) | 212(2) | 13(0.5) | 120(2) | 20(1) | 48(5) | 4(1) | 7(1) |
| BMI (kg/m2) | ||||||||
| Mean | 26.2 | 23.7* | 25.6† | 22.8*† | 25.9† | 23.4*† | 23.0*† | 22.5*† |
| SD | 5.9 | 4.0 | 4.3 | 3.3 | 4.5 | 4.2 | 3.4 | 3.3 |
|
MEN
(N, %) |
32,133(44) | 9,428(43) | 2,798(54) | 4,426(41) | 809(36) | 576(36) | 351(38) | 468(41) |
| Age (y) (N, %) | ||||||||
| 35 – 39 | 3,007(9) | 1,667(18) | 750(27) | 593(13) | 117(15) | 51(9) | 96(27) | 60(13) |
| 40 – 44 | 5,133(16) | 2,275(24) | 858(31) | 918(21) | 166(21) | 112(19) | 106(30) | 115(25) |
| 45 – 49 | 5,224(16) | 1,825(19) | 476(17) | 954(22) | 155(19) | 90(16) | 51(15) | 99(21) |
| 50 – 54 | 4,795(15) | 1,129(12) | 237(9) | 587(13) | 96(12) | 93(16) | 37(11) | 79(17) |
| 55 – 59 | 3,902(12) | 792(8) | 160(6) | 410(9) | 94(12) | 68(12) | 12(3) | 48(10) |
| 60 – 64 | 3,187(10) | 540(6) | 96(3) | 298(7) | 76(9) | 41(7) | 7(2) | 22(5) |
| 65 – 69 | 2,266(7) | 358(4) | 72(3) | 175(4) | 51(6) | 33(6) | 12(3) | 15(3) |
| 70 – 74 | 1,477(5) | 285(3) | 56(2) | 169(4) | 20(3) | 21(4) | 12(3) | 7(2) |
| 75 – 79 | 1,130(4) | 269(3) | 58(2) | 151(3) | 18(2) | 20(4) | 11(3) | 11(2) |
| 80 – 84 | 895(3) | 159(2) | 25(1) | 83(2) | 10(1) | 27(5) | 6(2) | 8(2) |
| 85 + | 1,117(4) | 129(1) | 10(0.4) | 88(2) | 6(1) | 20(4) | 1(0.3) | 4(1) |
| BMI (kg/m2) | ||||||||
| Mean | 27.8 | 25.6* | 26.0*† | 25.1*† | 27.4† | 26.0*† | 25.7* | 24.6*† |
| SD | 4.6 | 3.5 | 3.4 | 3.3 | 4.0 | 4.0 | 3.4 | 3.0 |
NHW=Non-Hispanic White. SD=standard deviation. CI=confidence interval.
The age distribution of all racial/ethnic subgroups were statistically different from NHW and Asian (all), by chi-squared tests, at the P<0.05 level.
Statistically different from NHW at P<0.05 level.
Statistically different from Asians (all) at P<0.0 level.
Table 2.
Unadjusted and Multivariate Adjusted Prevalence (%) of Diabetes
| NHW | Asian (all) | Asian Indian |
Chinese | Filipino | Japanese | Korean | Vietnamese | |
|---|---|---|---|---|---|---|---|---|
| WOMEN | ||||||||
| Total | 41,595 | 12,388 | 2,373 | 6,267 | 1,467 | 1,029 | 582 | 670 |
| Diabetics (N) cases | 2,423 | 966 | 265 | 345 | 217 | 85 | 25 | 29 |
| Unadjusted | ||||||||
| Rate (%) | 5.8 | 7.8* | 11.2*† | 5.5† | 14.8*† | 8.3* | 4.3† | 4.3† |
| [95% CI] | [5.6, 6.1] | [7.3, 8.3] | [10.0, 12.5] | [5.0, 6.1] | [13.1, 16.7] | [6.7, 10.1] | [2.9, 6.3] | [3.0, 6.1] |
| Age Standardized | ||||||||
| Rate (%) | 5.8 | 10.3* | 16.2*† | 7.4*† | 18.2*† | 8.8* | 6.3† | 7.3 |
| [95% CI] | [5.6, 6.0] | [9.7, 10.9] | [14.3, 18.2] | [6.7, 8.2] | [16.0, 20.3] | [7.1, 10.6] | [3.8, 8.9] | [4.6, 9.9] |
| Age-and-BMI Standardized | ||||||||
| Rate (%) | 5.9 | 13.3* | 16.8*† | 10.9* | 18.9*† | 13.1* | 12.6* | 12.8* |
| [95% CI] | [5.7, 6.2] | [12.4, 14.2] | [14.7, 19.0] | [9.5, 12.4] | [16.6, 21.3] | [10.0, 16.1] | [6.7, 18.4] | [9.6, 16.1] |
|
Treatment of diabetics with oral anti-
diabetic medications |
||||||||
| Count | 1,430 | 624 | 182 | 210 | 149 | 46 | 17 | 20 |
| Rate (%) | 68.5 | 73.4 | 82.0*† | 66.7 | 79.7* | 59.7† | 77.3 | 74.1 |
| [95% CI] | [66.5, 70.4] | [70.3, 76.3] | [76.4, 86.5] | [61.3, 71.6] | [73.3, 84.8] | [48.6, 70.0] | [56.6, 89.9] | [55.3, 86.8] |
| MEN | ||||||||
| Total | 32,133 | 9,428 | 2,798 | 4,426 | 809 | 576 | 351 | 468 |
| Diabetics (N) cases | 2,594 | 1,053 | 386 | 358 | 180 | 63 | 35 | 31 |
| Unadjusted | ||||||||
| Rate (%) | 8.1 | 11.2* | 13.8*† | 8.1† | 22.2*† | 10.9* | 10.0 | 6.6† |
| [95% CI] | [7.8, 8.4] | [10.5, 11.8] | [12.6, 15.1] | [7.3, 8.9] | [19.5, 25.2] | [8.6, 13.7] | [7.3, 13.6] | [4.7, 9.2] |
| Age Standardized | ||||||||
| Rate (%) | 8.1 | 14.3* | 21.3*† | 10.0*† | 25.3*† | 11.4* | 15.3* | 8.7† |
| [95% CI] | [7.8, 8.4] | [13.5, 15.2] | [19.3, 23.4] | [9.0, 11.0] | [22.2, 28.4] | [8.8, 13.9] | [9.8, 20.7] | [5.6, 11.8] |
| Age-and-BMI Standardized | ||||||||
| Rate (%) | 8.6 | 17.9* | 24.8*† | 13.2*† | 26.2*† | 13.5*† | 16.8* | 9.4† |
| [95% CI] | [8.3, 8.9] | [16.7, 9.1] | [22.2, 27.5] | [11.5, 14.9] | [22.6, 29.8] | [10.4, 16.6] | [10.8, 22.7] | [5.7, 13.1] |
|
Treatment of diabetics with oral anti-
diabetic medications |
||||||||
| N | 1,698 | 781 | 296 | 263 | 133 | 39 | 27 | 23 |
| Rate (%) | 68.4 | 76.2* | 79.4* | 75.6* | 75.1 | 62.9 | 79.4 | 74.2 |
| [95% CI] | [66.6, 70.2] | [73.5,78.7] | [75.0, 83.2] | [70.8, 79.8] | [68.3, 80.9] | [50.5, 73.8] | [63.2, 89.7] | [56.8, 86.3] |
NHW=Non-Hispanic White. SD=standard deviation. CI=confidence interval.
Statistically different from NHW at P<0.05 level
Statistically different from Asians (all) at P<0.05 level
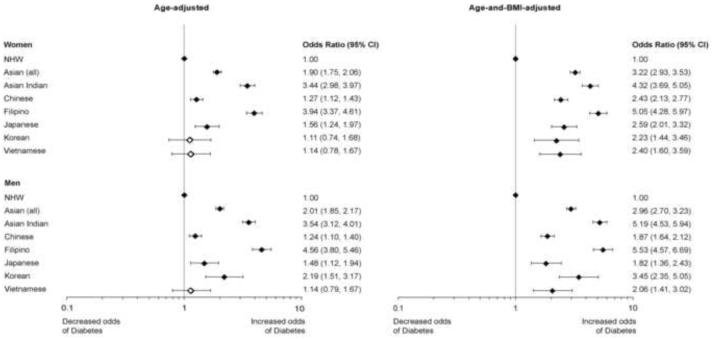
Age-adjusted prevalence was higher than the unadjusted rates in all Asian American subgroups (Table 2). Compared to NHWs, women and men in almost all Asian American subgroups had elevated prevalence rates of type 2 diabetes. Among the individual Asian American subgroups, Asian Indians and Filipinos had especially high rates. This was corroborated in analyses comparing age-adjusted odds ratios (Figure 1). Asian Indian women (OR 3.44, 95% CI: [2.98, 3.97]) and men (OR 3.54 [3.12, 4.01]) and Filipino women (OR 3.94 [3.37, 4.61]) and men (OR 4.56 [3.80, 5.46]) demonstrated the largest increased odds of having type 2 diabetes as compared to NHWs (Figure 1). Age-and-BMI adjusted prevalence was also higher than the unadjusted rates in all Asian American subgroups (Table 2). Asian Indians and Filipinos emerged again as having the highest prevalence of type 2 diabetes, compared to either NHWs or Asian Americans as a single group. This finding was confirmed in association studies (Figure 1).
Figure 1.
Age-adjusted and age-and-BMI adjusted odds ratios of type 2 diabetes by sex and Asian American subgroup, compared to Non-Hispanic Whites (NHWs). The diamond indicates the point estimate and the bar represents the 95% confidence interval. Filled diamonds indicate statistical significance compared to NHWs at (P<0.05)
Treatment rates among those classified as diabetic through physician recorded ICD-9 codes and abnormal laboratory values ranged from 59.7-82.0% in women and 62.9-79.4% in men (Table 2). Within each racial/ethnic subgroup there was no difference in treatment rates between women and men. In aggregate, Asian Americans had higher treatment rates than NHWs. In this cohort, some Asian American subgroups had higher treatment rates (Asian Indian women and men, Filipino women and men), while other subgroups were lower (Japanese women) relative to NHWs.
Sensitivity analyses were undertaken, restricting the cohort to patients with self identified race/ethnicity (49%). These analyses yielded similar conclusions across estimated prevalence, and identical conclusions across odds ratios (results not shown).
Discussion
All Asian American subgroups showed higher prevalence of type 2 diabetes in comparison to NHWs and considerable heterogeneity existed among the individual Asian American subgroups in our study, especially after adjustment for subgroup differences in age and BMI. Among Asian Americans, the Asian Indian and Filipino subgroups had the highest prevalence of type 2 diabetes, regardless of age- and age-and-BMI adjustment. Treatment rates for type 2 diabetes were also 5-8% higher for Asian Americans as a group, and there was significant variation in treatment rates among the individual racial/ethnic subgroups.
Our results corroborate some of the findings from previous studies that have investigated type 2 diabetes prevalence in Asian American subgroups from large statewide (CHIS)[20] or national datasets (NHIS).[9-11] In their 2007 CHIS analysis of five Asian American racial/ethnic subgroups, Choi and colleagues found that Filipinos had the highest age-adjusted prevalence of type 2 diabetes, followed by Japanese, Vietnamese, Koreans, and Chinese, compared to NHWs.[20] Asian Indians were not included in the study. Analyses of NHIS also demonstrate trends toward higher prevalence of diabetes in Asian Indians and Filipinos as compared to NHWs,[9] and significantly higher prevalence of diabetes in the Asian Indian subgroup alone.[10, 11] These studies rely on telephone based self-report surveys, which may be inaccurate due to recall bias, social desirability bias, and respondents’ lack of knowledge.[28] Some respondents may be misclassified when assessing the prevalence of type 2 diabetes, and there may be racial/ethnic differences in these misclassification rates due to decreased health literacy or disease knowledge in some subgroups.[29] A strength of this clinical data is that it offers analysis of type 2 diabetes prevalence with data gathered from EHRs rather than self-report and it includes large sample sizes of all six major Asian American racial/ethnic subgroups.
In this cohort of prevalent type 2 diabetes, treatment with oral anti-diabetic medication varied across racial/ethnic subgroups from 59.7-82.0%. Some Asian American subgroups (Asian Indian, Filipino) had higher treatment rates than others. Across every Asian American subgroup, no difference was observed in treatment rates between women and men. It is reassuring that along with the observed higher rates of type 2 diabetes in Asian Americans, treatment rates are also high in this population. This may reflect higher medication prescription rates by physicians in this area enriched in Asian American patients, or a greater propensity for Asian American patients to take oral anti-diabetic medication for type 2 diabetes. However, it should be noted that this was not observed across all Asian American subgroups, and that Japanese patients had lower treatment rates in this cohort. Future studies should examine physician and patient factors in treatment patterns across disparate Asian American subgroups.
In our study, type 2 diabetes was defined in part by the use of oral anti-diabetic medication. We excluded patients with insulin treatment alone in order to minimize misclassification with type 1 diabetes. A 2004 evaluation of the National Health and Nutrition Examination Survey (NHANES) III showed that 16.4% of people with type 2 diabetes used insulin alone for treatment. Other treatment regimens include diet alone (20.2%), oral anti-diabetics alone without insulin (52.5%) and oral anti-diabetics and insulin together (11.0%).[21] Most type 2 diabetics are treated with an oral anti-diabetic medication either with or without insulin. Assuming comparable usage to that found in NHANES[21] (which included Black/African Americans, Hispanic/Latinos, and NHWs), we likely underestimate treatment rates of type 2 diabetes by excluding patients who used insulin alone in our definition of treatment. We also excluded treatment of type 2 diabetes with exenatide injection (Byetta). Byetta was FDA approved as primary monotherapy on October 30, 2009,[30] however, it is doubtful that many patients in this cohort would have been treated with Byetta during the study period (January 1, 2007 – December 31, 2009).
It is unknown whether there are racial/ethnic differences between Asian Americans and NHWs in type 2 diabetes treatment regimens. For instance, if Asian Americans with type 2 diabetes are less likely to be treated with insulin alone, and NHWs with type 2 diabetes are more likely to be treated with insulin alone, then overall treatment rates may not actually be different. Therefore, our results should be interpreted with some caution. However, these observed differences in oral anti-diabetic medication treatment rates are noteworthy and should be explored further.
Relying on EHR for prevalence estimates may limit the external validity of the data, because EHR data are restricted to those individuals who choose to visit a clinic. Therefore, our results may only be generalizable to the clinical population. The sample size for women in our study is slightly higher than that of men in almost all Asian American racial/ethnic subgroups and in NHWs. The data suggest that in Asian American subgroups, women have much lower prevalence of type 2 diabetes as compared to men. It is possible that this finding results from higher use of healthcare services by women than by men.[31] The prevalence of type 2 diabetes in men may be artificially inflated because men visit a clinic (and are then entered into the EHR) only after they have fully developed the disease. Increased odds of diabetes in men (OR 1.49) were also observed in the CHIS analysis of Asian Americans by Choi and colleagues.[20] NHIS did not include Asian American subgroups by sex due to small sample size[9] and there are no sex differences in diabetes prevalence observed in national data for NHWs.[32]
In addition, the trends among different Asian American subgroups in this cohort may reflect specific cultural norms regarding rates of utilization of healthcare services. For example, Chinese have been shown to have a cultural reluctance to seek healthcare from individuals or organizations outside of their communities because of language barrier, transportation needs, and lack of trust in Western doctors.[33] Cultural attitudes could lead to under- or over-estimation of the actual prevalence of type 2 diabetes in individual racial/ethnic subgroups. Further studies should investigate the clinically relevant norms and cultural practices specific to Asian American subgroups and health-seeking behaviors, in order to determine how they may play a role in diagnosis, prevalence, and treatment of diabetes.
Data from this clinical population cannot offer absolute national or statewide diabetes prevalence estimates because it is limited to one specific Northern California region and sub-population, but it is useful for relative racial/ethnic subgroup comparisons. Confounders, such as socioeconomic status, are attenuated in this population because all patients in the cohort are insured and of similar socioeconomic status from a specific region of the country. Thus, the age- and age-and-BMI adjusted odds ratios provide robust internal comparability (patients from a single organization in one geographic region, diminishing variation due to geography or practice), high quality of clinical measures, and a large patient population. These data can reveal relative type 2 diabetes prevalence estimates as well as the need to disaggregate Asian American subgroups in future studies.
In summary, our findings suggest that all Asian American racial/ethnic subgroups have a higher prevalence of type 2 diabetes when compared to NHWs. Asian Indian and Filipino subgroups in particular, have a higher prevalence of type 2 diabetes compared to other Asian American subgroups, even after adjustment for BMI. Our study also provides some evidence that treatment rates with oral anti-diabetic medications differ by racial/ethnic subgroup. These findings strengthen the argument for the importance of disaggregating data by Asian American racial/ethnic subgroups in future studies. Culturally sensitive lifestyle changes, including promotion of physical exercise and diet modification in a relevant context (e.g., recommendations on how to modify traditional recipes and portion sizes), have been shown to significantly decrease the progression of type 2 diabetes in Asian Indians[34] and Filipinos.[35] These findings suggest that the increased prevalence of type 2 diabetes found in Asian Indians and Filipinos can be partially mitigated by weight loss through lifestyle modifications. Further research should continue investigating these clinically important differences in type 2 diabetes and its risk factors among Asian American racial/ethnic subgroups.
Acknowledgments
The Pan Asian Cohort Study is funded by the National Institutes of Health, National Institute of Diabetes and Digestive Kidney Diseases grant 5R01DK81371. There are no potential conflicts of interest relevant to this article to report. The authors thank Beinan Zhao for her assistance in reviewing the analytic data sets.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- 1.Ong P. [Accessed June 23, 2010];Estimating the 1990 to 2000 Growth of the Asian American Population. 2001 http://lewis.sppsr.ucla.edu/special/metroamerica/factsheets/LCMetroAm_DiscussPaper_1.pdf.
- 2.U.S. Census Bureau Population Projections [Accessed December 2010];Table 1a. Projected Popualtion of the United States, by Race and Hispanic Origin: 2000 to 2050. http://www.census.gov/population/www/projections/usinterimproj/
- 3.Reeves TJ, Bennett CE. [Accessed December 2010];We the People: Asians in the United States. Census 2000 Special Reports. 2004 http://www.census.gov/prod/2004pubs/censr-17.pdf.
- 4.U.S. Census Bureau . Census 2000 Summary File 1 (SF1) 2000. [Google Scholar]
- 5.McNeely MJ, Boyko EJ. Type 2 diabetes prevalence in Asian Americans: results of a national health survey. Diabetes Care. 2004;27:66–9. doi: 10.2337/diacare.27.1.66. [DOI] [PubMed] [Google Scholar]
- 6.Shai I, Jiang R, Manson MJ, Stampfer MJ, Willett WC, Colditz GA, et al. Ethnicity, obesity, and risk of type 2 diabetes in women: a 20-year follow-up study. Diabetes Care. 2006;29:1585–90. doi: 10.2337/dc06-0057. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention . National Diabetes Fact Sheet: General Information and National Estimates on Diabetes in the United States, 2333. US Dept of Health and Human Services; Atlanta, GA: 2004. [Google Scholar]
- 8.Smith SR, Svetkey LP, Dennis VW. Racial differences in the incidence and progression of renal diseases. Kidney Int. 1991;40:815–22. doi: 10.1038/ki.1991.281. [DOI] [PubMed] [Google Scholar]
- 9.Barnes PM, Adams PF, Powell-Griner E. Health characteristics of the Asian adult population: United States, 2004-2006. Adv Data. 2008;394:1–22. [PubMed] [Google Scholar]
- 10.Oza-Frank R, Ali MK, Vaccarino V, Narayan KM. Asian Americans: diabetes prevalence across U.S. and World Health Organization weight classifications. Diabetes Care. 2009;32:1644–6. doi: 10.2337/dc09-0573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ye J, Rust G, Baltrus P, Daniels E. Cardiovascular risk factors among Asian Americans: results from a National Health Survey. Ann Epidemiol. 2009;19:718–23. doi: 10.1016/j.annepidem.2009.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Venkataraman R, Nanda NC, Baweja G, Parikh N, Bhatia V. Prevalence of diabetes mellitus and related conditions in Asian Indians living in the United States. Am J Cardiol. 2004;94:977–80. doi: 10.1016/j.amjcard.2004.06.048. [DOI] [PubMed] [Google Scholar]
- 13.Rajpathak SN, Gupta LS, Waddell EN, Upadhyay UD, Wildman RP, Kaplan R, et al. Elevated risk of type 2 diabetes and metabolic syndrome among Asians and south Asians: results from the 2004 New York City HANES. Ethn Dis. 2010;20:225–30. [PubMed] [Google Scholar]
- 14.Araneta MR, Wingard DL, Barrett-Connor E. Type 2 diabetes and metabolic syndrome in Filipina-American women : a high-risk nonobese population. Diabetes Care. 2002;25:494–9. doi: 10.2337/diacare.25.3.494. [DOI] [PubMed] [Google Scholar]
- 15.Araneta MR, Barrett-Connor E. Ethnic differences in visceral adipose tissue and type 2 diabetes: Filipino, African-American, and white women. Obes Res. 2005;13:1458–65. doi: 10.1038/oby.2005.176. [DOI] [PubMed] [Google Scholar]
- 16.Cuasay LC, Lee ES, Orlander PP, Steffen-Batey L, Hanis CL. Prevalence and determinants of type 2 diabetes among Filipino-Americans in the Houston, Texas metropolitan statistical area. Diabetes Care. 2001;24:2054–8. doi: 10.2337/diacare.24.12.2054. [DOI] [PubMed] [Google Scholar]
- 17.Burchfiel CM, Curb JD, Rodriguez BL, Yano K, Hwang LJ, Fong KO, et al. Incidence and predictors of diabetes in Japanese-American men. The Honolulu Heart Program. Ann Epidemiol. 1995;5:33–43. doi: 10.1016/1047-2797(94)00038-u. [DOI] [PubMed] [Google Scholar]
- 18.Katz R, Wong ND, Kronmal R, Takasu J, Shavelle DM, Probstfield JL, et al. Features of the metabolic syndrome and diabetes mellitus as predictors of aortic valve calcification in the Multi-Ethnic Study of Atherosclerosis. Circulation. 2006;113:2113–9. doi: 10.1161/CIRCULATIONAHA.105.598086. [DOI] [PubMed] [Google Scholar]
- 19.Khan NA, Wang H, Anand S, Jin Y, Campbell NR, Pilote L, et al. Ethnicity and Sex Impact Diabetes Incidence and Outcomes. Diabetes Care. 2010 October 26; doi: 10.2337/dc10-0865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Choi SE, Chow VH, Chung SJ, Wong ND. Do Risk Factors Explain the Increased Prevalence of Type 2 Diabetes Among California Asian Adults? J Immigr Minor Health. 2010 October 9; doi: 10.1007/s10903-010-9397-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koro CE, Bowlin SJ, Bourgeois N, Fedder DO. Glycemic control from 1988 to 2000 among U.S. adults diagnosed with type 2 diabetes: a preliminary report. Diabetes Care. 2004;27:17–20. doi: 10.2337/diacare.27.1.17. [DOI] [PubMed] [Google Scholar]
- 22.Harris MI, Eastman RC, Cowie CC, Flegal KM, Eberhardt MS. Racial and ethnic differences in glycemic control of adults with type 2 diabetes. Diabetes Care. 1999;22:403–8. doi: 10.2337/diacare.22.3.403. [DOI] [PubMed] [Google Scholar]
- 23.Harris MI. Racial and ethnic differences in health care access and health outcomes for adults with type 2 diabetes. Diabetes Care. 2001;24:454–9. doi: 10.2337/diacare.24.3.454. [DOI] [PubMed] [Google Scholar]
- 24. [Accessed September 10, 2009];Epic Electronic Health Record Software. Epic Web Site. http://www.epic.com.
- 25.Palaniappan LP, Wong EC, Shin JJ, Moreno MR, Otero-Sabogal R. Collecting patient race/ethnicity and primary language data in ambulatory care settings: a case study in methodology. Health Serv Res. 2009;44:1750–61. doi: 10.1111/j.1475-6773.2009.00992.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.American Diabetes Association Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2010;33:562–569. [Google Scholar]
- 27.Wilcosky TC, Chambless LE. A comparison of direct adjustment and regression adjustment of epidemiologic measures. J Chronic Dis. 1985;38:849–56. doi: 10.1016/0021-9681(85)90109-2. [DOI] [PubMed] [Google Scholar]
- 28.Newell SA, Girgis A, Sanson-Fisher RW, Savolainen NJ. The accuracy of self-reported health behaviors and risk factors relating to cancer and cardiovascular disease in the general population: a critical review. Am J Prev Med. 1999;17:211–29. doi: 10.1016/s0749-3797(99)00069-0. [DOI] [PubMed] [Google Scholar]
- 29.Sarkar U, Karter AJ, Liu JY, Adler NE, Ngyuen R, Lopez A, et al. The literacy divide: health literacy and the use of an internet-based patient portal in an integrated health system-results from the diabetes study of northern California (DISTANCE) J Health Commun. 2010;15:183–96. doi: 10.1080/10810730.2010.499988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.U.S. Food and Drug Administration [Accessed December 2010];FDA Approved Drug Products. http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm.
- 31.Cleary PD, Mechanic D, Greenley JR. Sex differences in medical care utilization: an empirical investigation. J Health Soc Behav. 1982;23:106–19. [PubMed] [Google Scholar]
- 32.Harris MI, Flegal KM, Cowie CC, Eberhardt MS, Goldstein DE, Little RR, et al. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in U.S. adults. The Third National Health and Nutrition Examination Survey, 1988-1994. Diabetes Care. 1998;21:518–24. doi: 10.2337/diacare.21.4.518. [DOI] [PubMed] [Google Scholar]
- 33.Pang EC, Jordan-Marsh M, Silverstein M, Cody M. Health-seeking behaviors of elderly Chinese Americans: shifts in expectations. Gerontologist. 2003;43:864–74. doi: 10.1093/geront/43.6.864. [DOI] [PubMed] [Google Scholar]
- 34.Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1) Diabetologia. 2006;49:289–97. doi: 10.1007/s00125-005-0097-z. [DOI] [PubMed] [Google Scholar]
- 35.Mau MK, Keawe’aimoku Kaholokula J, West MR, Leake A, Efird JT, Rose C, et al. Translating diabetes prevention into native Hawaiian and Pacific Islander communities: the PILI ‘Ohana Pilot project. Prog Community Health Partnersh. 2010;4:7–16. doi: 10.1353/cpr.0.0111. [DOI] [PMC free article] [PubMed] [Google Scholar]