Abstract
Summary
Background and objectives
Despite significant advances in the epidemiology of acute kidney injury (AKI), prognostication remains a major clinical challenge. Unfortunately, no reliable method to predict renal recovery exists. The discovery of biomarkers to aid in clinical risk prediction for recovery after AKI would represent a significant advance over current practice.
Design, setting, participants, & measurements
We conducted the Biological Markers of Recovery for the Kidney study as an ancillary to the Acute Renal Failure Trial Network study. Urine samples were collected on days 1, 7, and 14 from 76 patients who developed AKI and received renal replacement therapy (RRT) in the intensive care unit. We explored whether levels of urinary neutrophil gelatinase-associated lipocalin (uNGAL), urinary hepatocyte growth factor (uHGF), urinary cystatin C (uCystatin C), IL-18, neutrophil gelatinase-associated lipocalin/matrix metalloproteinase-9, and urine creatinine could predict subsequent renal recovery.
Results
We defined renal recovery as alive and free of dialysis at 60 days from the start of RRT. Patients who recovered had higher uCystatin C on day 1 (7.27 versus 6.60 ng/mg·creatinine) and lower uHGF on days 7 and 14 (2.97 versus 3.48 ng/mg·creatinine; 2.24 versus 3.40 ng/mg·creatinine). For predicting recovery, decreasing uNGAL and uHGF in the first 14 days was associated with greater odds of renal recovery. The most predictive model combined relative changes in biomarkers with clinical variables and resulted in an area under the receiver-operator characteristic curve of 0.94.
Conclusions
We showed that a panel of urine biomarkers can augment clinical risk prediction for recovery after AKI.
Introduction
We recently reported results from a large multicenter clinical trial comparing two intensities of renal support for critically ill patients with acute kidney injury (AKI) in which we found that recovery of renal function was <25% at 28 days and not different between the two treatment strategies (1). These results emphasize that incomplete renal recovery is a common problem in patients surviving severe AKI (2). Failure to recover renal function has tremendous negative effects on quality of life and health care costs (3). Therefore, treatments to hasten and facilitate renal recovery are eagerly being sought. Unfortunately, there are no effective treatments to improve renal recovery. One important barrier to progress in this area has been the inability to forecast recovery in individual patients. The ability to prognosticate in this population would be extremely valuable for clinical decisions and to guide future research.
Recently, several urinary biomarkers have been investigated for the purpose of early diagnosis of AKI. Because these markers correlate with renal cell injury or function, their concentration in urine over time, alone or in combination, could provide new prognostic information regarding renal recovery. We selected six candidate markers representing three aspects of the physiology of renal recovery. First, we included three inflammatory markers: urinary neutrophil gelatinase-associated lipocalin (uNGAL) (4–7); matrix metalloproteinase protein-9 (MMP-9), a matrix degradation enzyme that is upregulated after ischemic injury in animal models and links to neutrophil gelatinase-associated lipocalin (NGAL) by a disulfide bond forming NGAL/MMP-9 (8); and urinary IL-18 (uIL-18), an inflammatory cytokine (9,10). Second, we measured urinary hepatocyte growth factor (uHGF), a marker linked to renal tubular epithelial cell regeneration (11). Finally, we measured the filtration and tubular reabsorption markers urinary cystatin C (uCystatin C) (12) and urinary creatinine (uCreatinine).
Materials and Methods
Study Design
Biological Markers of Recovery for the Kidney (BioMaRK) was a prospective observational cohort study conducted as an ancillary study to the Veterans Affairs (VA)/National Institutes of Health (NIH) Acute Renal Failure Trial Network (ATN) study. ATN was a multicenter, prospective trial of two strategies for renal replacement therapy (RRT) in critically ill patients with AKI (1). Adult patients diagnosed with AKI and requiring RRT with at least one or more nonrenal organ failures or sepsis were eligible. BioMaRK includes all patients in the ATN study who gave additional consent to blood collections (n = 820). In addition, BioMaRK included an intensive monitoring cohort comprising 109 consecutive patients who consented to undergo serial urine sampling. Incomplete data including unavailability of urine samples precluded inclusion of 33 subjects; the remaining 76 form the BioMaRK urine biomarker analysis cohort. We obtained approval from the institutional review boards of the University of Pittsburgh and all participating sites.
Data Collection/Laboratory Measurements
Medical records of study participants were prospectively reviewed to retrieve hospitalization data, including baseline demographic characteristics (Table 1), serial renal function, daily urine volume, and severity of illness scores. The presence of sepsis was defined by international consensus criteria (13). Recovery of renal function was defined by survival and dialysis independence at 60 days.
Table 1.
Summary of baseline and clinical characteristics of the study patients
| Characteristics | All Subjects (n = 76) | Recovery (n = 38) | Nonrecovery (n = 38) | P |
|---|---|---|---|---|
| Age (years) | 58.4 (17.0) | 52.2 (15.7) | 64.7 (16.2) | <0.01 |
| Female gender (%) | 30 (39.5) | 15 (39.5) | 15 (39.5) | 1.00 |
| White race (%) | 64 (84.2) | 30 (79.0) | 34 (89.5) | 0.21 |
| Baseline serum creatinine (mg/dl) | 1.1 (0.4) | 1.1 (0.4) | 1.2 (0.5) | 0.45 |
| Estimated GFR (ml/min per 1.73 m2) | 78.6 (38.1) | 84.2 (40.9) | 73.0 (34.7) | 0.16 |
| BUN at initiation of RRT (mg/dl) | 55.6 (29.9) | 51.3 (28.8) | 59.9 (30.8) | 0.23 |
| Cause of acute kidney injury | ||||
| ischemia (%) | 66 (86.8) | 29 (76.3) | 37 (97.4) | <0.01 |
| nephrotoxins (%) | 16 (21.3) | 10 (26.3) | 6 (16.2) | 0.29 |
| sepsis (%) | 50 (65.8) | 23 (60.5) | 27 (71.1) | 0.33 |
| multifactorial causes (%) | 51 (68.0) | 25 (65.8) | 26 (70.3) | 0.68 |
| Length of ICU stay before randomization (days) | 5.4 (4.1) | 4.2 (2.8) | 6.5 (4.9) | 0.03 |
| Length of hospital stay before randomization (days) | 8.5 (7.1) | 6.7 (5.0) | 10.2 (8.5) | 0.08 |
| Charlson comorbidity indexa | 4.1 (3.3) | 3.3 (3.8) | 4.9 (2.7) | <0.01 |
| Mechanical ventilation (%) | 69 (90.8) | 34 (89.5) | 35 (92.1) | 1.00 |
| Severe sepsisb (%) | 47 (62.7) | 22 (57.9) | 25 (67.6) | 0.39 |
| APACHE II scorec | 23.4 (7.2) | 21.8 (7.2) | 25.0 (6.8) | 0.06 |
| Nonrenal SOFA organ-system scored | ||||
| respiratory | 2.1 (1.3) | 2.1 (1.5) | 2.1 (1.2) | 0.98 |
| coagulation | 1.5 (1.3) | 1.4 (1.3) | 1.5 (1.3) | 0.58 |
| liver | 0.9 (1.3) | 1.2 (1.5) | 0.6 (1.0) | 0.08 |
| cardiovascular | 2.2 (1.7) | 2.0 (1.7) | 2.5 (1.6) | 0.17 |
| central nervous system | 2.2 (1.4) | 2.3 (1.3) | 2.1 (1.5) | 0.45 |
| total | 8.9 (4.0) | 9.2 (4.6) | 8.5 (3.3) | 0.43 |
| Cleveland Clinic ICU ARF scoree | 11.9 (3.0) | 11.6 (3.0) | 12.2 (3.0) | 0.49 |
| Intensive strategyf (%) | 34 (44.7) | 18 (47.4) | 16 (42.1) | 0.64 |
Data presented as mean (SD) unless otherwise noted. BUN, blood urea nitrogen; RRT, renal replacement therapy; ICU, intensive care unit; APACHE II, Acute Physiology and Chronic Health Evaluation II; SOFA, Sequential Organ Failure Assessment; ARF, acute renal failure.
According to the method of Charlson et al. (31).
Defined as sepsis plus acute organ dysfunction according to 2001 international consensus criteria for sever sepsis (13).
According to the method of Knaus et al. (32).
Nonrenal SOFA score, excluding the renal part, assessed on the first day according to the method of Vincent et al. (33).
According to the method of Thakar et al. (34).
Intensive strategy, intermittent hemodialysis, and sustained low-efficiency dialysis were provided 6 times per week (every day except Sunday), and continuous venovenous hemodiafiltration was prescribed to provide a flow rate of the total effluent (the sum of the dialysate and ultrafiltrate) of 35 ml/kg of body weight per hour on the basis of the weight before the onset of acute illness (1).
Fresh urine samples were obtained on days 1, 7, and 14. A well mixed, 30-ml sample was obtained from the Foley catheter. A protease inhibitor cocktail tablet (Roche Diagnostics Corporation, IN) was added to the urine specimen immediately on collection. Urine samples were then poured into 50-ml conical centrifuge tubes, centrifuged for 5 minutes at 1000 × G at 4°C, and frozen at −80°C until shipped to the central laboratory. Samples were then stored at −80°C until analyzed.
uNGAL, uNGAL/MMP-9, and uHGF were measured by an R&D ELISA kit and uCystatin C was measured by a Biovendor (Candler, NC) ELISA kit, all according to the respective manufacturer's instructions. Measurement of uIL-18 was performed using a Bio-Plex200 suspension array system (Bio-Rad Laboratories). Reagents were purchased from Bio-Rad (Bio-Plex Human Group II Cytokine 2-Plex Panel, MIF and IL-18) and used according to manufacturer's directions. Samples were assayed in duplicate, and data were analyzed using Bio-Plex Manager software (version 4.1). uCreatinine concentrations were measured using a nonenzymatic assay (DICT-500, BioAssay Systems). Mean intra- and interassay variations were below 10% (5.44% and 9.03% for uNGAL; 2.58% and 1.04% for uNGAL/MMP-9; 4.54% and 6.63% for IL-18; 5.25% and 5.39% for uHGF; 6.20% and 8.90% for uCystatin C; 8.54% and 4.36% for uCreatinine).
Statistical Analyses
We compared baseline characteristics between patients who recovered from AKI by 60 days after enrollment and those who failed to recover. Continuous data were compared using paired t or Mann–Whitney tests. Categorical data were expressed as proportions and compared using the chi-squared or Fisher exact test. We normalized biomarker levels by uCreatinine concentrations and analyzed them at each time point. We also performed analysis using the largest relative change in the first 14 days as compared with day 1. We fitted logistic regression models to examine the association between each marker and recovery and generated an area under the receiver-operating characteristic (ROC) curve (AUC) to assess the prediction accuracy of each marker. To assess the additive prediction ability of each marker compared with traditional clinical predictors, we first identified a clinical risk prediction model that was based on AUC analysis and then added each marker individually to this clinical model. The AUC results reported for different models are based on the estimated risk scores for each model (rather than the raw biomarker data as would be done for a single marker). We estimated the risk score function using a logistic regression model including clinical and biomarker variables as covariates. The resulting estimated risk scores were then used to construct ROC curves, and empirical estimates of AUCs were obtained by the concordance statistic (14). We evaluated the model fit by the Hosmer–Lemeshaw goodness-of-fit test. Finally, we calculated the net reclassification improvement (NRI) to estimate overall improvement in reclassification with urinary biomarkers compared with clinical variables alone (15). All of the analyses were performed using SAS version 9.0 (SAS Institute, Cary, NC) at a significance level of 0.05.
Results
Patient Characteristics and Outcome
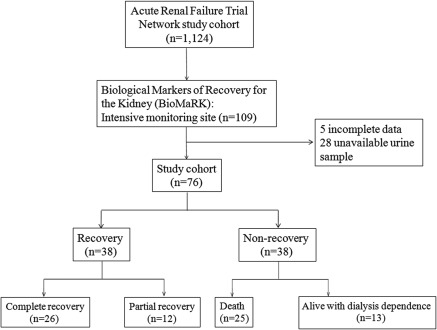
Of the 109 patients in the BioMaRK intensive monitoring cohort, 76 patients had complete data available including urine samples. Exactly half (38 patients) recovered renal function (alive and without requirement for dialysis) by day 60 (Figure 1). Baseline clinical characteristics are shown (Table 1), and the patient demographics from this cohort were quite comparable to that of the parent study—the ATN study (1).
Figure 1.
Subject disposition for the Biologic Markers of Recovery for the Kidney (BioMaRK) study cohort.
Recovering patients were more likely to be younger, have a shorter length of intensive care unit stay before randomization, lower Charlson comorbidity index (age adjusted), and lower nonrenal Sequential Organ Failure Assessment (SOFA) score compared with those not recovering. By contrast, there were no statistical differences in gender, ethnicity, baseline serum creatinine, blood urea nitrogen at initiation of RRT, length of hospital stay, length of intensive care unit stay, requirement for mechanical ventilation, Cleveland Clinic acute renal failure score, and intensity of RRT. The primary etiology of AKI, reported by the clinician investigators, was ischemia in both groups. However, a significantly lower percentage of ischemia (76.3%) was noted as the cause of AKI in the recovery group compared with 97.4% in the nonrecovery group. Of the 38 participants who recovered renal function, 26 (68%) had complete recovery. Among those failing to recover renal function, 66% (25 patients) were dead by day 60.
Relationship between Biomarker Levels and Recovery Status
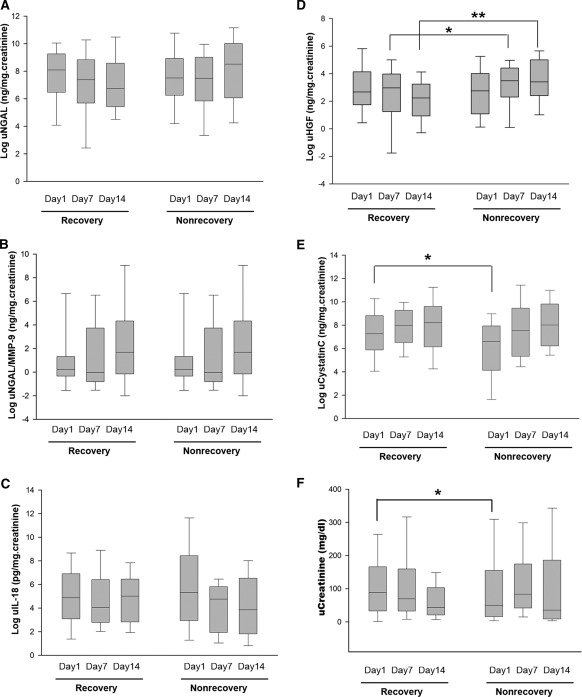
We compared urinary biomarker levels between recovery and nonrecovery groups (Figure 2). All data are presented as natural logs. On day 1, uCystatin C and uCreatinine levels in the recovery group were significantly higher than in the nonrecovery group (7.27, interquartile range [IQR] 6.50 to 8.33 versus 6.60, IQR 4.97 to 7.58 ng/mg creatinine, P = 0.02; and 88.60, IQR 44.04 to 133.72 versus 50.00, IQR 20.12 to 103.64, P = 0.03, respectively). On day 7, the renal recovery group had lower uHGF levels than the nonrecovery group (2.97, IQR 2.24 to 3.63 versus 3.48, IQR 3.04 to 4.22 ng/mg creatinine, P = 0.01). On day 14, there were lower uHGF levels in the recovery group compared with the nonrecovery group (2.24, IQR 1.35 to 2.95 versus 3.40, IQR 2.87 to 4.79 ng/mg creatinine, P = 0.04). However, there was no significant difference in the uNGAL, uNGAL/MMP-9, and uIL-18 levels on the basis of recovery status at any of these time points.
Figure 2.
Box plots for the six biomarkers evaluated. The vertical box represents the 25th percentile (bottom line), median (middle line), and 75th percentile (top line) values whereas the vertical bars represent the intervals between maximum and minimum values: (A) urinary neutrophil gelatinase associated lipocalin (uNGAL) levels, (B) uNGAL/matrix metalloproteinase-9 (MMP-9), (C) urinary IL-18 (uIL-18), (D) urine hepatocyte growth factor (uHGF), (E) urinary cystatin C (uCystatinC), and (F) urinary creatinine (uCreatinine). *P < 0.05, **P < 0.01. The mean (SD) of the largest relative change of uNGAL for recovery and nonrecovery were −1.1 (1.5) and + 4.8 (10.0), P = 0.01, respectively. The mean (SD) of the largest relative change of uHGF for recovery and nonrecovery were −1.0 (1.5) and + 5.8 (12.8), P = 0.003, respectively.
We further analyzed the largest relative change of urinary biomarkers in the first 2 weeks. The recovery group showed a significant decrease in uNGAL and uHGF level (P = 0.01 and 0.003, respectively). However, we did not find any significant changes in uCystatin C, uIL-18, uNGAL/MMP-9, and uCreatinine by recovery status. To rule out the effect of glomerular filtration on the level of biomarkers, we also normalized all concentrations by the uCreatinine concentration. The same association/prediction results were found when comparing normalized with non-normalized data (data not shown).
Urinary Biomarkers and Prediction of Renal Recovery
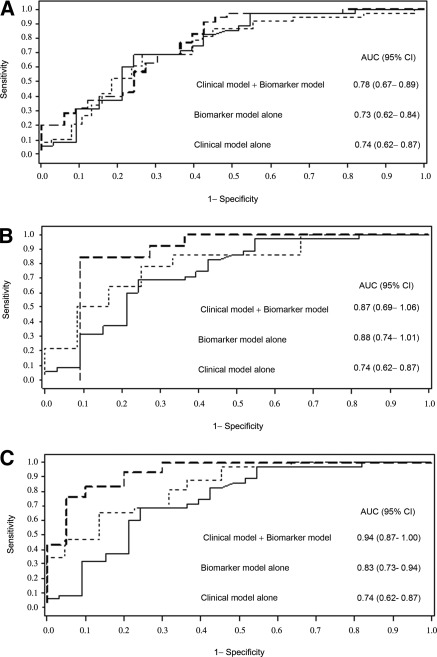
For individual biomarkers, we report the AUC for prediction of recovery in Table 2. As shown, uHGF on day 14 and the fall of uHGF over the first 14 days were moderately predictive of renal recovery (AUC = 0.74, 95% confidence interval [CI] 0.53 to 0.94; and 0.74, 95% CI 0.60 to 0.89). For models using multiple biomarkers, the greatest AUC was 0.73 (95% CI 0.62 to 0.84) on day 1, 0.88 (95% CI 0.74 to 1.01) on day 14, and 0.84 (95% CI 0.73 to 0.94) using the largest relative change over the first 14 days (Table 3b and Figure 3).
Table 2.
Area under the receiver-operating characteristic curve at each time point for urinary biomarkers and urine output for predicting renal recovery
| Urinary Biomarkers | Time after Enrollment | AUC | 95% CI |
|---|---|---|---|
| uNGAL | Day 1 | 0.58 | 0.45 to 0.71 |
| Day 7 | 0.56 | 0.40 to 0.72 | |
| Day 14 | 0.66 | 0.44 to 0.88 | |
| Largest relative changea | 0.70 | 0.55 to 0.84 | |
| uHGF | Day 1 | 0.51 | 0.37 to 0.64 |
| Day 7 | 0.70 | 0.55 to 0.84 | |
| Day 14 | 0.74 | 0.53 to 0.94 | |
| Largest relative changea | 0.74 | 0.60 to 0.89 | |
| uCystatin C | Day 1 | 0.66 | 0.53 to 0.78 |
| Day 7 | 0.40 | 0.24 to 0.57 | |
| Day 14 | 0.46 | 0.22 to 0.70 | |
| Largest relative changea | 0.61 | 0.46 to 0.77 | |
| uIL-18 | Day 1 | 0.54 | 0.41 to 0.67 |
| Day 7 | 0.52 | 0.36 to 0.69 | |
| Day 14 | 0.48 | 0.24 to 0.72 | |
| Largest relative changea | 0.42 | 0.26 to 0.58 | |
| uNGAL/MMP-9 | Day 1 | 0.48 | 0.35 to 0.62 |
| Day 7 | 0.53 | 0.37 to 0.70 | |
| Day 14 | 0.45 | 0.21 to 0.69 | |
| Largest relative changea | 0.53 | 0.37 to 0.69 | |
| uCreatinine | Day 1 | 0.62 | 0.50 to 0.75 |
| Day 7 | 0.55 | 0.39 to 0.71 | |
| Day 14 | 0.48 | 0.23 to 0.74 | |
| Largest relative changea | 0.66 | 0.51 to 0.81 | |
| Urine output >1 L/d | Day 1 | 0.55 | 0.48 to 0.62 |
| Day 7 | 0.59 | 0.48 to 0.69 | |
| Day 14 | 0.60 | 0.47 to 0.73 |
AUC, area under the receiver-operating characteristic curve; CI, confidence interval; uNGAL, urinary neutrophil gelatinase-associated lipocalin; uHGF, urinary hepatocyte growth factor; uCystatin C, urinary cystatin C; uIL-18, urinary IL-18; MMP-9, matrix metalloproteinase protein-9; uCreatinine, urinary creatinine.
Largest relative change in the first 14 days as compared with day 1.
Table 3b.
Logistic regression analysis with variables available for predicting renal recovery and model accuracy after combining variables: Biomarkers model alone
| Model | AUC (95% CI) | Pb |
|---|---|---|
| Day 1 | ||
| uCystatin C | 0.66 (0.53 to 0.78) | NA |
| uCystatin C + uNGAL | 0.68 (0.56 to 0.80) | 0.32 |
| uCystatin C + uNGAL + uIL-18 | 0.73 (0.62 to 0.85) | 0.26 |
| uCystatin C + uNGAL + uIL-18 + uHGF | 0.73 (0.62 to 0.85) | 0.26 |
| uCystatin C + uNGAL + uIL-18 + uHGF + uNGAL/MMP-9 | 0.73 (0.62 to 0.84) | 0.06 |
| Day 14 | ||
| uHGF | 0.74 (0.53 to 0.94) | NA |
| uHGF + uNGAL | 0.76 (0.57 to 0.96) | 0.53 |
| uHGF + uNGAL + uIL-18 | 0.81 (0.63 to 0.99) | 0.37 |
| uHGF + uNGAL + uIL-18 + uCystatin C | 0.80 (0.62 to 0.98) | 0.61 |
| uHGF + uNGAL + uIL-18 + uCystatin C + uNGAL/MMP-9 | 0.88 (0.74 to 1.01) | 0.44 |
| Largest relative changea | ||
| uHGF | 0.74 (0.60 to 0.89) | NA |
| uHGF + uNGAL | 0.84 (0.73 to 0.94) | 0.22 |
| uHGF + uNGAL + uCystatin C | 0.83 (0.73 to 0.94) | 0.22 |
| uHGF + uNGAL + uCystatin C + uNGAL/MMP-9 | 0.83 (0.73 to 0.94) | 0.22 |
| uHGF + uNGAL + uCystatin C + uNGAL/MMP-9 + uIL-18 | 0.84 (0.73 to 0.94) | 0.09 |
AUC, area under the receiver-operating characteristic curve; CI, confidence interval; uCystatin C, urinary cystatin C; NA, not applicable; uNGAL, urinary neutrophil gelatinase-associated lipocalin; uHGF, urinary hepatocyte growth factor.
Largest relative change in the first 14 days as compared with day 1.
Compared with uCystatin C on day1, uHGF on day 14, and uHGF in largest relative change.
Figure 3.
Receiver-operating characteristic (ROC) curves for the best prediction model for renal recovery. Shown are best combination biomarker model alone (thin dashed line), clinical prediction model alone (solid line), and best combined clinical model and best combination biomarker model (thick dashed line): (A) day 1, (B) day 14, and (C) the largest relative change. The clinical risk prediction model included age and Charlson comorbidity index. The area under the ROC curve (AUC) values and 95% confidence intervals (CIs) are also shown.
Clinical Risk Prediction Models for Renal Recovery
We constructed a clinical risk prediction model from the significant variables found in our logistic regression model of renal recovery beginning with all of the significant variables in Table 1. By stepwise selection, only age, Charlson comorbidity index, and Acute Physiology and Chronic Health Evaluation II (APACHE II) remained significant in the final model. We then chose the best clinical model on the basis of performance by AUC as shown in Table 3. Age and Charlson comorbidity index together demonstrated the best accuracy in predicting renal recovery (AUC = 0.74, 95% CI 0.62 to 0.87) (Table 3b and Figure 3). The addition of baseline severity of illness scores (e.g., APACHE II or SOFA) did not improve the risk prediction model (Table 3b). We also found that the addition of organ failure (SOFA) on day 14 did not improve the day-1 clinical risk prediction model. Irrespective of diuretic use, urine output >1 L/d, a traditional marker of recovery, was poorly predictive of renal recovery (AUC on day 1 = 0.55 [95% CI 0.48 to 0.62], AUC on day 7 = 0.59 [95% CI 0.48 to 0.69], and AUC on day 14 = 0.60 [95% CI 0.47 to 0.73]) and did not improve our clinical model. However, it is important to note that, as a study of urine biomarkers, our analysis excluded anuric patients.
Table 3a.
Logistic regression analysis with variables available for predicting renal recovery and model accuracy after combining variables: Clinical model alone
| Clinical Variables | OR (95% CI) | Model | AUC (95% CI) | P |
|---|---|---|---|---|
| Age | 0.95 (0.92 to 0.98) | A | 0.73 (0.61 to 0.84) | |
| Charlson comorbidity index | 0.86 (0.72 to 1.01) | B | 0.69 (0.56 to 0.82) | |
| APACHE II | 0.94 (0.87 to 1.01) | C | 0.63 (0.50 to 0.76) | |
| M1 = A + B | 0.74 (0.62 to 0.87) | 0.78a | ||
| M2 = A + B + C | 0.74 (0.61 to 0.87) | 0.70b |
OR, odds ratio; AUC, area under the curve; CI, confidence interval; APACHE II, Acute Physiology and Chronic Health Evaluation II. A,B,C: Univariate models; M1 and M2: Multivariate models.
Compared with age;
Compared with M1 model.
Combining Clinical and Biomarker Data
To determine the predictive value of biomarkers when added to the clinical model, we compared AUCs for models that combined multiple biomarkers with our best clinical model. We found the greatest AUC on day 1 to be 0.78 (95% CI 0.67 to 0.89) in a combined model of four biomarkers (uCystatin C, uNGAL, uIL-18, and uHGF) with our clinical model. Similarly, the greatest AUC on day 14 was 0.87 (95% CI 0.69 to 1.06) in a model combining four biomarkers (uHGF, uNGAL, uIL-18, and uCystatin C) with the clinical model. Finally, the greatest AUC observed overall was 0.94 (95% CI 0.87 to 1.00) for a model combining the largest relative change of all urinary biomarkers (uHGF, uNGAL, uCystatin C, uNGAL/MMP-9, and uIL-18) together with our clinical model (Table 3c and Figure 3). Model fits were good for the best combination of clinical and biomarker models at each time point (days 1 and 14) and the largest relative change.
Table 3c.
Logistic regression analysis with variables available for predicting renal recovery and model accuracy after combining variables: Combine clinical model with biomarkers model
| Model | AUC (95% CI) | Pd |
|---|---|---|
| Day 1 | ||
| M1 + uNGAL | 0.74 (0.62 to 0.86) | 0.56 |
| M1 + uNGAL/MMP-9 | 0.75 (0.63 to 0.87) | 0.05 |
| M1 + uIL-18 | 0.76 (0.64 to 0.87) | 0.09 |
| M1 + uHGF | 0.75 (0.63 to 0.87) | 0.08 |
| M1 + uCystatin C | 0.75 (0.63 to 0.87) | 0.02 |
| M1 + uNGAL + uHGF | 0.75 (0.63 to 0.87) | 0.25 |
| M1 + uCystatin C + uNGAL + uIL-18 + uHGFa | 0.78 (0.67 to 0.89) | 0.02 |
| Day 14c | ||
| M1 + uNGAL | 0.80 (0.60 to 0.99) | 0.85 |
| M1 + uNGAL/MMP-9 | 0.83 (0.65 to 1.00) | 0.16 |
| M1 + uIL-18 | 0.72 (0.51 to 0.93) | 0.56 |
| M1 + uHGF | 0.82 (0.63 to 1.00) | 0.04 |
| M1 + uCystatin C | 0.73 (0.51 to 0.94) | 0.32 |
| M1 + uNGAL + uHGF | 0.83 (0.65 to 1.02) | 0.03 |
| M1 + uHGF + uNGAL + uIL-18 + uCystatin Ca | 0.87 (0.69 to 1.06) | <0.01 |
| Largest relative changeb | ||
| M1 + uNGAL | 0.91 (0.83 to 0.99) | 0.08 |
| M1 + uNGAL/MMP-9 | 0.84 (0.72 to 0.95) | 0.62 |
| M1 + uIL-18 | 0.82 (0.70 to 0.95) | 0.56 |
| M1 + uHGF | 0.85 (0.73 to 0.96) | 0.46 |
| M1 + uCystatin C | 0.85 (0.73 to 0.96) | 0.80 |
| M1 + uNGAL + uHGF | 0.93 (0.86 to 1.00) | <0.01 |
| M1 + uHGF + uNGAL + uCystatin C + uNGAL/MMP-9 + uIL-18a | 0.94 (0.87 to 1.00) | <0.01 |
AUC, area under the receiver-operating characteristic curve; CI, confidence interval; M1, clinical model combining of age and Charlson comorbidity index; uNGAL, urinary neutrophil gelatinase-associated lipocalin; uCystatin C, urinary cystatin C; MMP-9, matrix metalloproteinase-9; uHGF, urinary hepatocyte growth factor.
Best prediction model (greatest AUC), combine clinical model with biomarkers.
Largest relative change in the first 14 days as compared to day 1.
SOFA score on day 14 did not improve AUC.
Compared with M1 model.
Next, we tested a model that included the best-performing single biomarkers, uHGF and uNGAL (Table 2), together with our clinical model (age, Charlson comorbidity index) on days 1 and 14 and using the largest relative change. We found moderate to excellent prediction of renal recovery (AUC was 0.75, 0.83, and 0.93, respectively).
Finally, we also assessed the ability of urinary biomarkers to “reclassify” the degree of probability for renal recovery as assessed by the clinical prediction model. On the basis of the clinical risk prediction model, subjects were categorized into prespecified “low,” “intermediate,” and “high” probability groups using cutoffs of <30%, 30% to 60%, and >60%, respectively. We then compared the proportions of reclassified subjects across these three groups when the best urinary biomarker model was introduced. On day 1, 29.9% of subjects were correctly reclassified to risk prediction categories by the best model compared with the clinical model (P = 0.018). There were significant improvements in prediction of renal recovery with the day 14 model (116.1%, P = 0.002) and for the largest relative change model (63.3%, P = 0.002).
Discussion
During the past few years, more than 30 studies have explored the role of biomarkers to predict the development of AKI. However, only a few tested biomarkers for their ability to predict AKI severity, and no study has tested the role of a biomarker to predict renal recovery (16). In this study, we have shown that a panel of urine biomarkers on days 1, 7, and 14 were significantly different in those recovering from AKI compared with those failing to recover. When combining various urinary biomarkers with a clinical model using age and Charlson comorbidity index, we found maximum AUCs of 0.78 on day 1, 0.87 on day 14, and 0.94 for the largest relative change during the first 14 days. These results likely represent diagnostic accuracy far beyond clinical judgment.
Bhandari et al. (17) reported that patients who recovered from AKI did not appear to differ in clinical characteristics (age, gender, mechanical ventilation status, or clinical severity scores) from the nonrecovery group. Secondary analysis from three randomized controlled trials comparing efficacy of continuous RRT versus intermittent RRT found that APACHE III scores >100 (18), cardiovascular instability (19), and pre-existing renal impairment (20) were associated with renal nonrecovery. However, there was no uniform definition or standard timing to assess renal recovery. The Beginning and Ending Supportive care for the Kidney study investigators reported that baseline creatinine and urine output at the time of discontinuation of RRT were most predictive of recovery (21). However, urine output was analyzed after RRT was already stopped based on a clinical decision rather than used at a fixed time point (e.g., 14 days) to predict subsequent recovery. In our study, urine output and baseline creatinine were not predictive. However, baseline creatinine might have been less valuable in our study because the ATN study excluded patients with stage 4 and 5 chronic kidney disease.
We had good reasons to believe that certain biomarkers would be useful in the prediction of renal recovery. Hepatocyte growth factor has been demonstrated to have multiple effects on physiologic or pathophysiological processes involving the kidney, including mitogenic, morphogenic, and differentiating effects (22). In animal models of toxic or ischemic acute tubular necrosis, hepatocyte growth factor therapy markedly accelerated renal recovery (23). Only one small study has demonstrated uHGF upregulation during the acute phase of AKI with a gradual decline during recovery (24). Our study has confirmed this earlier observation demonstrating a decreasing pattern in recovery but an increasing pattern from day 1 to 14 in the nonrecovery group. However, as far as we know, this is the first study to examine uHGF specifically as a marker to predict renal recovery.
NGAL expression is upregulated in the kidney soon after injury. In an established murine model of renal ischemia-reperfusion injury, intravenous NGAL administered before, during, or after ischemia resulted in marked amelioration of the morphologic and functional consequences, as evidenced by a significant decrease in damage to tubules seen using histological methods and in serum creatinine measurements (25).
Cystatin C is excreted via glomerular filtration and then undergoes essentially complete tubular reabsorption and catabolism so that it is not normally found in urine in significant amounts (12,26). We found the same pattern of uCystatin C with uCreatinine, both of which were greater on day 1 in patients who ultimately recovered renal function. Serum cystatin C has been shown to be associated with increased inflammation in a cross-sectional analysis of 3418 patients with chronic kidney disease (27). Overexpression of cystatin C actually suppressed cathepsin S activity, which suppresses CD4(+)T cell–mediated immune responses (28). Thus, a phenotype of increased cystatin C expression may be beneficial in early AKI. In our study, significantly higher levels of uCystatin C on day 1 may also have reflected an increased response to injury.
As expected, the response of biomarkers over time proved more prognostic than did single time points. The largest relative change of uHGF and uNGAL during the first 14 days demonstrated a moderate ability to predict renal recovery (AUC = 0.74 and 0.70). Because of the heterogeneous causes of AKI and underlying comorbidity, including diabetes, sepsis, and atherosclerosis, the use of multiple biomarker panels to predict renal recovery seems reasonable. Furthermore, as is the case with detection of AKI, biomarkers can only be seen as useful when they outperform or add to clinically available information. We have clearly shown a benefit to combining biomarker data with clinical information in terms of increased AUC and NRI.
There are several limitations in our study. First, because of the observational nature of the study, we could not control for missing data. Some patients did not make urine, died, or were discharged before 14 days. Thus, our results may only pertain to patients in which the outcome remains uncertain after 14 days from the start of RRT. Nevertheless, our clinical experience suggests that this is indeed the group of patients most in need of diagnostic aid. Second, because of the limited sample size, we did not attempt to compare biomarker levels between patients with complete and partial recovery of renal function or among dialysis-dependent survivors and those who died before day 60. Third, we did not test other urinary biomarkers, such as kidney injury molecule-1 and L-fatty acid binding protein, which seem to have promising results in predicting AKI (29,30).
Our study also has many strengths. First, this was a multicenter prospective study and included a wide range of patient demographics and clinical variables. Second, we tested biomarkers at multiple time points, which allowed us to explore the dynamic changes in urinary concentrations. Finally, this is, to our knowledge, the first study to focus on prediction of recovery of renal function in humans. Given the clinical uncertainty and high complexity of medical decision-making around this issue (e.g., timing and duration of RRT, placement of permanent access, long-term prognosis, and follow-up), even methods that provide modest improvement in clinical prediction are important.
In conclusion, our results indicate that urine biomarkers, especially uHGF and uNGAL, can augment clinical risk prediction for recovery after AKI requiring RRT. Further information is obtained by combining multiple urine biomarker levels with clinical information. Larger prospective studies are necessary to confirm our observations and to validate the predictive value for assessing recovery of renal function.
Disclosures
A patent application has been filed by the University of Pittsburgh concerning the use of biologic and clinical markers to aid in the prognosis for renal recovery after AKI.
Acknowledgments
BioMaRK was supported by a grant (R01DK070910) from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of NIDDK or NIH. The VA/NIH ATN study was supported by the Cooperative Studies Program of the Department of Veterans Affairs Office of Research and Development (CSP #530) and by NIDDK by interagency agreement Y1-DK-3508-01. N.S. and X.W. contributed equally to this manuscript.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1. Palevsky PM, Zhang JH, O'Connor TZ, Chertow GM, Crowley ST, Choudhury D, Finkel K, Kellum JA, Paganini E, Schein RM, Smith MW, Swanson KM, Thompson BT, Vijayan A, Watnick S, Star RA, Peduzzi P: Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med 359: 7–20, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Ronco C: Acute renal failure in critically ill patients: A multinational, multicenter study. JAMA 294: 813–818, 2005 [DOI] [PubMed] [Google Scholar]
- 3. Manns B, Doig CJ, Lee H, Dean S, Tonelli M, Johnson D, Donaldson C: Cost of acute renal failure requiring dialysis in the intensive care unit: Clinical and resource implications of renal recovery. Crit Care Med 31: 449–455, 2003 [DOI] [PubMed] [Google Scholar]
- 4. Supavekin S, Zhang W, Kucherlapati R, Kaskel FJ, Moore LC, Devarajan P: Differential gene expression following early renal ischemia/reperfusion. Kidney Int 63: 1714–1724, 2003 [DOI] [PubMed] [Google Scholar]
- 5. Mishra J, Ma Q, Kelly C, Mitsnefes M, Mori K, Barasch J, Devarajan P: Kidney NGAL is a novel early marker of acute injury following transplantation. Pediatr Nephrol 21: 856–863, 2006 [DOI] [PubMed] [Google Scholar]
- 6. Hirsch R, Dent C, Pfriem H, Allen J, Beekman RH, III, Ma Q, Dastrala S, Bennett M, Mitsnefes M, Devarajan P: NGAL is an early predictive biomarker of contrast-induced nephropathy in children. Pediatr Nephrol 22: 2089–2095, 2007 [DOI] [PubMed] [Google Scholar]
- 7. Zappitelli M, Washburn KK, Arikan AA, Loftis L, Ma Q, Devarajan P, Parikh CR, Goldstein SL: Urine neutrophil gelatinase-associated lipocalin is an early marker of acute kidney injury in critically ill children: A prospective cohort study. Crit Care 11: R84, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ronco P, Lelongt B, Piedagnel R, Chatziantoniou C: Matrix metalloproteinases in kidney disease progression and repair: A case of flipping the coin. Semin Nephrol 27: 352–362, 2007 [DOI] [PubMed] [Google Scholar]
- 9. Parikh CR, Abraham E, Ancukiewicz M, Edelstein CL: Urine IL-18 is an early diagnostic marker for acute kidney injury and predicts mortality in the intensive care unit. J Am Soc Nephrol 16: 3046–3052, 2005 [DOI] [PubMed] [Google Scholar]
- 10. Parikh CR, Mishra J, Thiessen-Philbrook H, Dursun B, Ma Q, Kelly C, Dent C, Devarajan P, Edelstein CL: Urinary IL-18 is an early predictive biomarker of acute kidney injury after cardiac surgery. Kidney Int 70: 199–203, 2006 [DOI] [PubMed] [Google Scholar]
- 11. Liu Y, Yang J: Hepatocyte growth factor: New arsenal in the fights against renal fibrosis? Kidney Int 70: 238–240, 2006 [DOI] [PubMed] [Google Scholar]
- 12. Herget-Rosenthal S, Feldkamp T, Volbracht L, Kribben A: Measurement of urinary cystatin C by particle-enhanced nephelometric immunoassay: Precision, interferences, stability and reference range. Ann Clin Biochem 41: 111–118, 2004 [DOI] [PubMed] [Google Scholar]
- 13. Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G: 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 31: 1250–1256, 2003 [DOI] [PubMed] [Google Scholar]
- 14. Hanley JA, McNeil BJ: The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143: 29–36, 1982 [DOI] [PubMed] [Google Scholar]
- 15. Pencina MJ, D'Agostino RB, Sr, D'Agostino RB, Jr, Vasan RS: Evaluating the added predictive ability of a new marker: From area under the ROC curve to reclassification and beyond. Stat Med 27: 157–172, 2008 [DOI] [PubMed] [Google Scholar]
- 16. Coca SG, Yalavarthy R, Concato J, Parikh CR: Biomarkers for the diagnosis and risk stratification of acute kidney injury: A systematic review. Kidney Int 73: 1008–1016, 2008 [DOI] [PubMed] [Google Scholar]
- 17. Bhandari S, Turney JH: Survivors of acute renal failure who do not recover renal function. QJM 89: 415–421, 1996 [DOI] [PubMed] [Google Scholar]
- 18. Mehta RL, McDonald B, Gabbai FB, Pahl M, Pascual MT, Farkas A, Kaplan RM: A randomized clinical trial of continuous versus intermittent dialysis for acute renal failure. Kidney Int 60: 1154–1163, 2001 [DOI] [PubMed] [Google Scholar]
- 19. Augustine JJ, Sandy D, Seifert TH, Paganini EP: A randomized controlled trial comparing intermittent with continuous dialysis in patients with ARF. Am J Kidney Dis 44: 1000–1007, 2004 [DOI] [PubMed] [Google Scholar]
- 20. Uehlinger DE, Jakob SM, Ferrari P, Eichelberger M, Huynh-Do U, Marti HP, Mohaupt MG, Vogt B, Rothen HU, Regli B, Takala J, Frey FJ: Comparison of continuous and intermittent renal replacement therapy for acute renal failure. Nephrol Dial Transplant 20: 1630–1637, 2005 [DOI] [PubMed] [Google Scholar]
- 21. Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Straaten HO, Ronco C, Kellum JA: Discontinuation of continuous renal replacement therapy: A post hoc analysis of a prospective multicenter observational study. Crit Care Med 37: 2576–2582, 2009 [DOI] [PubMed] [Google Scholar]
- 22. Matsumoto K, Mizuno S, Nakamura T: Hepatocyte growth factor in renal regeneration, renal disease and potential therapeutics. Curr Opin Nephrol Hypertens 9: 395–402, 2000 [DOI] [PubMed] [Google Scholar]
- 23. Vijayan A, Martin DR, Sadow JL, Kissane J, Miller SB: Hepatocyte growth factor inhibits apoptosis after ischemic renal injury in rats. Am J Kidney Dis 38: 274–278, 2001 [DOI] [PubMed] [Google Scholar]
- 24. Taman M, Liu Y, Tolbert E, Dworkin LD: Increase urinary hepatocyte growth factor excretion in human acute renal failure. Clin Nephrol 48: 241–245, 1997 [PubMed] [Google Scholar]
- 25. Mishra J, Mori K, Ma Q, Kelly C, Yang J, Mitsnefes M, Barasch J, Devarajan P: Amelioration of ischemic acute renal injury by neutrophil gelatinase-associated lipocalin. J Am Soc Nephrol 15: 3073–3082, 2004 [DOI] [PubMed] [Google Scholar]
- 26. Uchida K, Gotoh A: Measurement of cystatin-C and creatinine in urine. Clin Chim Acta 323: 121–128, 2002 [DOI] [PubMed] [Google Scholar]
- 27. Stevens LA, Schmid CH, Greene T, Li L, Beck GJ, Joffe MM, Froissart M, Kusek JW, Zhang YL, Coresh J, Levey AS: Factors other than glomerular filtration rate affect serum cystatin C levels. Kidney Int 75: 652–660, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kitamura H, Kamon H, Sawa S, Park SJ, Katunuma N, Ishihara K, Murakami M, Hirano T: IL-6-STAT3 controls intracellular MHC class II alphabeta dimer level through cathepsin S activity in dendritic cells. Immunity 23: 491–502, 2005 [DOI] [PubMed] [Google Scholar]
- 29. Liangos O, Perianayagam MC, Vaidya VS, Han WK, Wald R, Tighiouart H, MacKinnon RW, Li L, Balakrishnan VS, Pereira BJ, Bonventre JV, Jaber BL: Urinary N-acetyl-beta-(d)-glucosaminidase activity and kidney injury molecule-1 level are associated with adverse outcomes in acute renal failure. J Am Soc Nephrol 18: 904–912, 2007 [DOI] [PubMed] [Google Scholar]
- 30. Ferguson MA, Vaidya VS, Waikar SS, Collings FB, Sunderland KE, Gioules CJ, Bonventre JV: Urinary liver-type fatty acid-binding protein predicts adverse outcomes in acute kidney injury. Kidney Int 77: 708–714, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Charlson ME, Pompei P, Ales KL, MacKenzie CR: A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 40: 373–383, 1987 [DOI] [PubMed] [Google Scholar]
- 32. Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, Sirio CA, Murphy DJ, Lotring T, Damiano A, Harrell FR, Jr: The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest 100: 1619–1636, 1991 [DOI] [PubMed] [Google Scholar]
- 33. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG: The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22: 707–710, 1996 [DOI] [PubMed] [Google Scholar]
- 34. Thakar CV, Arrigain S, Worley S, Yared JP, Paganini EP: A clinical score to predict acute renal failure after cardiac surgery. J Am Soc Nephrol 16: 162–168, 2005 [DOI] [PubMed] [Google Scholar]