Abstract
Summary
Background and objectives
Among people with essential hypertension, ambulatory BP measurement is superior to BP obtained in the clinic in predicting cardiovascular outcomes. In part, this is because it can detect white-coat hypertension and masked hypertension. Whether the same is true for hemodialysis patients is not known.
Design, setting, participants, & measurements
Using a threshold of 140/80 mmHg for median midweek dialysis-unit BP and 135/85 mmHg for 44-hour ambulatory BP, we defined four categories of BP: sustained normotension (SN), white-coat hypertension (WCH), masked hypertension (MHTN), and sustained hypertension (SHTN).
Results
Among 355 long-term hemodialysis patients, the prevalence of SN was 35%, WCH 15%, MHTN 15%, and SHTN 35%. Over a mean follow-up of 29.6 (SD 21.7) months, 102 patients died (29%), yielding a crude mortality rate of 121/1000 patient-years. Unadjusted and multivariate-adjusted analyses showed increasing all-cause mortality with increasing severity of hypertension (unadjusted hazard ratios from SN, WCH, MHTN, SHTN: 1, 1.12, 1.70, 1.80, respectively [P for trend < 0.01]; adjusted hazard ratios: 1, 1.30, 1.36, 1.87, respectively [P for trend 0.02]). When a predialysis BP threshold of 140/90 mmHg was used to classify patients into BP categories, the prevalence of SN was 24%, WCH 26%, MHTN 4%, and SHTN 47%. Hazard ratios for mortality were similar when compared with median midweek dialysis-unit BP.
Conclusions
As in the essential hypertension population, MHTN and WCH have prognostic significance. The prognostic value of BP obtained in the dialysis unit can be refined with ambulatory BP monitoring.
Introduction
There are over 300,000 patients on chronic hemodialysis in the United States, many of whom have hypertension (1). Hypertension remains poorly controlled in hemodialysis patients (2). In part, this poor control may be an artifact of measurement. In fact, when ambulatory BP recordings are used to assess BP control, the prevalence estimates for poor control are much lower (3,4). This suggests that patients on dialysis may have a substantial prevalence of white-coat hypertension (WCH). It is equally possible that patients on dialysis have a lower BP during dialysis but much higher BP at home. This is now called masked hypertension (MHTN), the reverse of WCH (5).
WCH in the patient not on dialysis is defined as elevated BP in the clinic and normal BP outside of the clinic (6,7). Among those without kidney disease, the diagnosis of WCH and MHTN is straightforward because clinic and ambulatory BP criteria are clearly defined. However, this is not the case for the hemodialysis patients. Although ambulatory BP measurements over the interdialytic interval can provide an estimate of average interdialytic BP, the ideal method to measure and define “clinic” BP is not clear (8). Whether the predialysis, postdialysis, or peridialysis BP should be used to define a hypertension threshold has never been determined (8). Accordingly, it is much more difficult to define WCH or MHTN in these patients.
There are several problems with predialysis and postdialysis BP measurements (9). For example, BP values obtained before or after dialysis by technicians and nurses without attention to detail differ strikingly from those obtained using standardized methods (10). Even when BP is obtained before and after dialysis using standardized methods, agreement with interdialytic ambulatory BP is poor (3,4). Furthermore, predialysis BP overestimates interdialytic ambulatory BP and postdialysis BP underestimates it (11). Recently, we reported that median midweek intradialytic BP can serve as a more appropriate surrogate of 44-hour ambulatory BP (12). A threshold of 140/80 mmHg was found to be the best correlate of ambulatory hypertension. In the study presented here, we reasoned that this threshold could also be used to classify patients into the categories of WCH and MHTN. However, proof that this is not simply a statistical phenomenon would require that outcomes based on these definitions differ from each other. We posited that an ordinal increase in all-cause mortality would be seen, with the lowest mortality in sustained normotension (SN), higher mortality in WCH, even higher mortality in MHTN, and the highest mortality associated with sustained hypertension (SHTN). If so, this study would provide evidence for the first time that the prognostic significance of WCH and MHTN seen in the essential hypertension population is similarly also seen in the hemodialysis population.
Materials and Methods
Participants
The cross-sectional data on part of this cohort have previously been reported (3,13). Patients 18 years or older who had been on chronic hemodialysis for more than 3 months; were free of vascular, infectious, or bleeding complications within 1 month of recruitment; and were dialyzed 3 times a week dialysis at one of the four dialysis units in Indianapolis affiliated with Indiana University were enrolled in the study. Those who missed two hemodialysis treatments or more over 1 month, abused drugs, had chronic atrial fibrillation, or a body mass index of ≥40 kg/m2 were excluded. Patients who had a change in dry weight or antihypertensive drugs within 2 weeks were also excluded. Antihypertensive medications were not held before dialysis. The Research and Development Committee of the Roudebush VA Medical Center in Indianapolis and the Institutional Review Board of Indiana University approved the study, and all subjects gave written informed consent.
Measurements
Ambulatory BP Monitoring
Ambulatory BP monitoring was performed after the first or midweek hemodialysis session for 44 hours. Ambulatory BP was recorded every 20 minutes during the day (6:00 a.m. to 10:00 p.m.) and every 30 minutes during the night (10:00 p.m. to 6:00 a.m.) using a Spacelab 90207 ambulatory BP monitor (SpaceLabs Medical, Inc., Redmond, WA) in the nonaccess arm, as reported previously (14). Awake and sleep readings were calculated for each patient by self-reported sleep and wake times by means of a diary. Of the 353 subjects examined, the mean number of ambulatory BP readings was 90.0 with an SD of 25.5. Only five (1.4%) of the measurements had <16 readings. Even a limited number of ambulatory BP measurements are useful for prognostic purposes in the general population; therefore, we did not exclude any patients on the basis of the number of ambulatory BP recordings (15).
Dialysis-Unit BP
Dialysis-unit BP recordings as measured by the dialysis-unit staff before and after dialysis were collected prospectively at the time of the patient visit. These BP recordings were obtained using the sphygmomanometer equipped with the hemodialysis machines without a specified technique and were averaged over 2 weeks. Thus, each patient had six predialysis and six postdialysis BP recordings to provide routine dialysis-unit BP.
Median midweek dialysis-unit BP was calculated as previously reported (12). Briefly, the median was calculated from all BP obtained during a midweek dialysis that included the predialysis and postdialysis measurements.
Definitions of Categories of Hypertension
SN was defined as a 44-hour ambulatory BP of <135/85 mmHg and a median midweek intradialytic BP of <140/80 mmHg. Notably, there are no agreed upon definitions of hypertension among dialysis patients. The threshold chosen here was that recommended by the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure for people with essential hypertension. WCH was defined as a 44-hour ambulatory BP of <135/85 mmHg and a median midweek intradialytic BP of ≥140/80 mmHg. MHTN was defined as a 44-hour ambulatory BP of ≥135/85 mmHg and a median midweek intradialytic BP of <140/80 mmHg. SHTN was defined as a 44-hour ambulatory BP of ≥135/85 mmHg and a median midweek intradialytic BP of ≥140/80 mmHg. All definitions ignored whether the patients were taking antihypertensive therapy or not.
In addition to these definitions, we used the thresholds of the Kidney Disease Outcomes Quality Initiative of 140/90 mmHg predialysis and 130/80 mmHg postdialysis to define hypertension (16).
Outcomes
All-cause mortality was the primary focus of our study, and this outcome was available in every patient. The cause of death was not ascertained. Patients were censored on the date that they had the last dialysis visit if they were transplanted or recovered kidney function.
Data Analysis
We tested the agreement between the classification methods using the kappa statistic. Cox proportional hazards regression was used to determine the significance and strength of association of factors associated with mortality outcomes. The proportionality assumption was tested by evaluating the log-minus-log plot and by testing the Schoenfeld residuals. Initially, model fits for mortality were compared between BP classifications without adjustment. We then created an age-, gender-, and race-adjusted model and then a multivariate-adjusted model. This multivariate model was adjusted for the following variables: age, race, gender, cardiovascular disease, serum albumin, hemoglobin, and dialysis vintage. Adjusted hazard ratios were calculated with continuous covariates (age, albumin, hemoglobin, dialysis vintage) at their group means and categorical variables were treated as present between BP categories. All analyses were conducted using Stata 11.0 (Stata Corporation, College Station, TX). The P values reported are two-sided and taken to be significant at <0.05.
Results
Between September 2003 and December 2010, 353 patients from four dialysis units staffed by the nephrology faculty of Indiana University in Indianapolis were recruited.
The clinical characteristics of patients by BP classification are shown in Table 1. The population was predominantly black with an average age of 55 years. All patients were on three-times weekly dialysis and were prescribed a dialysis time of approximately 4 hours and blood flow rate of 400 ml/min. Serum albumin and hemoglobin reflect the general hemodialysis population. Cardiovascular disease defined as previous history of myocardial infarction, coronary bypass surgery or angioplasty, or stroke was present in 36% of patients. Most (76%) patients received antihypertensive drugs; β-blockers were used in approximately two-thirds and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers in half. As expected, those who were overtly hypertensive with SHTN also took more antihypertensive drugs.
Table 1.
Characteristics of the study population by hypertension classification as defined by median midweek intradialytic BP
| SN | WCH | MHTN | SHTN | Total | P | |
|---|---|---|---|---|---|---|
| n | 123 (35%) | 52 (15%) | 54 (15%) | 124 (35%) | 353 (100%) | |
| Men | 82 (67%) | 32 (62%) | 38 (70%) | 76 (61%) | 228 (65%) | 0.61 |
| Race | 0.03 | |||||
| nonblack | 14 (11%) | 5 (10%) | 15 (28%) | 21 (17%) | 55 (16%) | |
| black | 109 (89%) | 47 (90%) | 39 (72%) | 103 (83%) | 298 (84%) | |
| Age (years) | 55.7 ± 14.0 | 55.6 ± 12.5 | 56.5 ± 13.3 | 54.1 ± 11.7 | 55.2 ± 12.9 | 0.63 |
| Body mass index (kg/m2) | 28.4 ± 5.8 | 28.8 ± 7.3 | 26.5 ± 5.8 | 27.1 ± 5.4 | 27.7 ± 5.9 | 0.07 |
| Etiology of end-stage renal disease | 0.20 | |||||
| diabetes mellitus | 41 (33%) | 21 (40%) | 24 (44%) | 45 (36%) | 131 (37%) | |
| hypertensive nephrosclerosis | 57 (46%) | 23 (44%) | 21 (39%) | 51 (41%) | 152 (43%) | |
| glomerulonephritis | 9 (7%) | 0 (0%) | 0 (0%) | 11 (9%) | 20 (6%) | |
| adult autosomal polycystic kidney disease | 1 (1%) | 1 (2%) | 0 (0%) | 3 (2%) | 5 (1%) | |
| other/unknown | 9 (7%) | 4 (8%) | 8 (15%) | 9 (7%) | 30 (8%) | |
| Years on dialysis | 4.7 ± 4.9 | 2.9 ± 2.6 | 3.7 ± 4.6 | 3.0 ± 3.4 | 3.7 ± 4.1 | <0.01 |
| History of smoking | 0.55 | |||||
| current | 33 (27%) | 14 (27%) | 13 (24%) | 45 (36%) | 105 (30%) | |
| past | 46 (37%) | 17 (33%) | 18 (33%) | 41 (33%) | 122 (35%) | |
| never | 41 (33%) | 16 (31%) | 22 (41%) | 37 (30%) | 116 (33%) | |
| History of diabetes mellitus | 54 (44%) | 26 (50%) | 33 (61%) | 61 (49%) | 174 (49%) | 0.22 |
| History of cardiovascular disease | 40 (33%) | 21 (40%) | 22 (41%) | 42 (34%) | 125 (35%) | 0.62 |
| Urea reduction ratio (%) | 73.9 ± 7.8 | 73.6 ± 8.4 | 74.3 ± 6.3 | 74.4 ± 7.4 | 74.1 ± 7.5 | 0.97 |
| Albumin (g/dl) | 3.7 ± 0.4 | 3.8 ± 0.4 | 3.7 ± 0.4 | 3.7 ± 0.5 | 3.7 ± 0.4 | 0.10 |
| Hemoglobin (g/dl) | 12.3 ± 1.6 | 12.3 ± 1.5 | 12.2 ± 1.5 | 11.9 ± 1.4 | 12.2 ± 1.5 | 0.22 |
| On antihypertensive medications | 77 (63%) | 41 (79%) | 48 (89%) | 102 (82%) | 268 (76%) | <0.01 |
| Number of antihypertensives in users | 1.3 ± 1.3 | 1.9 ± 1.4 | 2.5 ± 1.6 | 2.3 ± 1.6 | 1.9 ± 1.6 | <0.01 |
| β-blocker | 66 (54%) | 33 (63%) | 37 (69%) | 88 (71%) | 224 (63%) | 0.03 |
| ACE inhibitor | 38 (31%) | 16 (31%) | 29 (54%) | 64 (52%) | 147 (42%) | <0.01 |
| ARB | 8 (7%) | 6 (12%) | 9 (17%) | 16 (13%) | 39 (11%) | 0.21 |
| α-blocker | 4 (3%) | 5 (10%) | 4 (7%) | 10 (8%) | 23 (7%) | 0.31 |
| dihydropyridine calcium-channel blocker | 29 (24%) | 21 (40%) | 29 (54%) | 64 (52%) | 143 (41%) | <0.01 |
| non-dihydropyridine calcium-channel blocker | 2 (2%) | 2 (4%) | 4 (7%) | 6 (5%) | 14 (4%) | 0.30 |
| vasodilator | 19 (15%) | 7 (13%) | 12 (22%) | 17 (14%) | 55 (16%) | 0.45 |
| centrally acting agents | 15 (12%) | 15 (29%) | 15 (28%) | 40 (32%) | 85 (24%) | <0.01 |
| Interdialytic weight gain (kg) | 2.9 ± 1.2 | 2.7 ± 1.2 | 2.8 ± 1.2 | 2.7 ± 1.3 | 2.8 ± 1.2 | 0.87 |
SN, sustained normotension; WCH, white-coat hypertension; MHTN, masked hypertension; SHTN, sustained hypertension; ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker.
Patients with MHTN differed from the remaining groups in having more nonblacks and having a lower body mass index. Somewhat surprisingly, these patients used as many antihypertensives as those with SHTN and used as many angiotensin-converting enzyme inhibitors and calcium-channel blockers. However, patients with SN had more years on hemodialysis, used fewer antihypertensive medications, and when they used antihypertensive medications the number per patient was fewer. In contrast, patients with WCH had fewer years on hemodialysis. The remaining characteristics were similar between groups.
The median intradialytic BP was calculated from an average of 9.46 ± 1.72 intradialytic recordings without censoring for high or low values. Table 2 shows that, by definition, median (not the mean) midweek intradialytic BP was higher in those with WCH and SHTN and lower among those with SN and MHTN. A similar pattern was seen in the case of pre- and posthemodialysis BP as that seen for median intradialytic BP.
Table 2.
BP levels by hypertension classification as defined by median midweek intradialytic BP
| SN | WCH | MHTN | SHTN | Total | P | |
|---|---|---|---|---|---|---|
| Ambulatory BP | ||||||
| systolic | 115.6 ± 11.9 | 122.2 ± 10.0 | 150.1 ± 14.4 | 150.2 ± 15.7 | 134.0 ± 21.3 | <0.01 |
| diastolic | 66.9 ± 8.8 | 70.2 ± 8.7 | 82.5 ± 12.8 | 87.3 ± 11.8 | 76.9 ± 14.0 | <0.01 |
| heart rate | 81.1 ± 11.0 | 79.1 ± 11.0 | 78.3 ± 11.5 | 78.5 ± 11.9 | 79.4 ± 11.4 | 0.28 |
| Median midweek intradialytic BP | ||||||
| systolic | 117.3 ± 12.0 | 148.4 ± 11.3 | 125.3 ± 10.1 | 157.3 ± 17.2 | 137.2 ± 22.5 | <0.01 |
| diastolic | 64.5 ± 7.8 | 82.9 ± 10.2 | 67.6 ± 7.4 | 86.7 ± 11.0 | 75.5 ± 13.8 | <0.01 |
| heart rate | 77.7 ± 12.5 | 73.8 ± 8.5 | 74.4 ± 12.0 | 75.2 ± 12.2 | 75.7 ± 11.8 | 0.13 |
| Prehemodialysis BP | ||||||
| systolic | 135.0 ± 15.9 | 150.5 ± 15.9 | 154.8 ± 17.6 | 163.7 ± 15.8 | 150.4 ± 20.2 | <0.01 |
| diastolic | 72.6 ± 9.3 | 82.2 ± 11.5 | 81.4 ± 10.2 | 89.9 ± 11.0 | 81.5 ± 12.7 | <0.01 |
| heart rate | 81.0 ± 11.9 | 80.5 ± 9.6 | 77.4 ± 11.4 | 78.5 ± 11.6 | 79.5 ± 11.5 | 0.15 |
| Posthemodialysis BP | ||||||
| systolic | 120.8 ± 12.6 | 140.5 ± 14.5 | 133.5 ± 15.0 | 153.4 ± 21.7 | 137.1 ± 21.8 | <0.01 |
| diastolic | 66.2 ± 8.2 | 77.3 ± 9.0 | 72.9 ± 10.9 | 83.7 ± 12.2 | 75.0 ± 12.7 | <0.01 |
| heart rate | 79.8 ± 12.2 | 78.3 ± 9.9 | 77.4 ± 9.8 | 79.3 ± 11.7 | 79.0 ± 11.4 | 0.58 |
The classification of hypertension categories was based on median midweek intradialytic BP and 44-hour ambulatory BP (see text).
Median follow-up was 26 months (interquartile range 11 to 42 months) with the longest follow-up of 7 years. During this follow-up period, 102 (29%) patients died. The crude mortality rate was 121/1000 patient-years. Several patients were censored: 44 were transplanted, and 1 recovered renal function. No one was censored for leaving the dialysis unit because death could still be tracked through the social security death index.
Table 3 shows the longitudinal hazard ratio for mortality for the four categories of hypertension. Notably, those with SN and WCH had similar mortality, and those with MHTN had mortality similar to that of those with SHTN. A trend for increasing mortality was statistically significant from SN to WCH to MHTN to SHTN. An adjustment for age, gender and race did not remove this association. Furthermore, multivariate adjustment retained the linear trend seen in the unadjusted analysis.
Table 3.
Risk of all-cause mortality
| Basis of BP Classification | Unadjusted Analysis |
Age-, Gender-, Race-Adjusted Analysis |
Multivariate-Adjusted Analysisa |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Hazard Ratio | 95% CI | P | n | Hazard Ratio | 95% CI | P | n | Hazard Ratio | 95% CI | P | |
| Median midweek intradialytic | <0.01b | <0.01b | 0.02b | |||||||||
| SN | 123 | 1.00 | 123 | 1.00 | 106 | 1.00 | ||||||
| WCH | 52 | 1.12 | (0.60 to 2.11) | 0.7 | 52 | 1.16 | (0.62 to 2.17) | 0.7 | 47 | 1.30 | (0.68 to 2.48) | 0.4 |
| MHTN | 54 | 1.70 | (0.94 to 3.09) | 0.08 | 54 | 1.35 | (0.73 to 2.50) | 0.3 | 51 | 1.36 | (0.73 to 2.53) | 0.3 |
| SHTN | 124 | 1.80 | (1.12 to 2.89) | 0.02 | 124 | 1.87 | (1.16 to 3.01) | 0.01 | 115 | 1.87 | (1.13 to 3.10) | 0.01 |
| Prehemodialysis | <0.01b | 0.01b | 0.01b | |||||||||
| SN | 85 | 1.00 | 85 | 1.00 | 75 | 1.00 | ||||||
| WCH | 90 | 1.50 | (0.84 to 2.70) | 0.2 | 90 | 1.41 | (0.78 to 2.54) | 0.3 | 78 | 1.63 | (0.89 to 2.99) | 0.10 |
| MHTN | 13 | 2.66 | (0.99 to 7.11) | 0.05 | 13 | 2.05 | (0.75 to 5.65) | 0.2 | 12 | 1.71 | (0.60 to 4.86) | 0.30 |
| SHTN | 164 | 2.08 | (1.23 to 3.54) | <0.01 | 164 | 1.94 | (1.14 to 3.31) | 0.01 | 153 | 2.06 | (1.18 to 3.60) | 0.01 |
| Posthemodialysis | 0.02b | 0.05b | 0.07b | |||||||||
| SN | 113 | 1.00 | 113 | 1.00 | 98 | 1.00 | ||||||
| WCH | 62 | 0.97 | (0.52 to 1.80) | 0.9 | 62 | 0.87 | (0.47 to 1.61) | 0.7 | 55 | 1.04 | (0.55 to 1.96) | 0.90 |
| MHTN | 32 | 1.90 | (0.97 to 3.72) | 0.06 | 32 | 1.81 | (0.91 to 3.59) | 0.09 | 30 | 1.99 | (0.98 to 4.04) | 0.06 |
| SHTN | 145 | 1.65 | (1.03 to 2.63) | 0.04 | 145 | 1.48 | (0.92 to 2.38) | 0.1 | 135 | 1.49 | (0.91 to 2.43) | 0.10 |
CI, confidence interval.
Adjusted for age, race, gender, cardiovascular disease, serum albumin, hemoglobin, and dialysis vintage.
Denotes test for linear trend from SN to SHTN.
Defining the four classes of BP using a prehemodialysis BP threshold of 140/90 mmHg showed a similar linear trend. This trend was not removed by multivariate adjustment.
When posthemodialysis BP was used to define the four categories using a threshold of 130/80 mmHg as recommended by Kidney Disease Outcomes Quality Initiative (17), we found that those with MHTN had the highest mortality. It is notable that those with normal BP postdialysis but high interdialytic BP had an even higher mortality than patients who had high BP postdialysis and high interdialytic BP. Multivariate adjustment did not remove the significance of these findings. We therefore hypothesized that the interdialytic weight gain may be greater in those with MHTN. We found that the interdialytic weight gain was higher in those with MHTN (SN 2.9 kg, WCH 2.8 kg, MHTN 3.4 kg, SHTN 2.6 kg, P = 0.03). However, adjustment for interdialytic weight gain did not remove the statistical significance of the findings (hazard ratios for SN, WCH, MHTN, SHTN were 1, 1.03, 2.05, and 1.51, respectively).
We tested the agreement between the classification methods using the kappa statistic. Agreement was modest (overall kappa = 0.63, kappa for SN = 0.69, WCH 0.58, MHTN 0.24, SHTN 0.73). This indicates substantial reclassification using different methods of BP measurement (pre-, post-, or intradialytic).
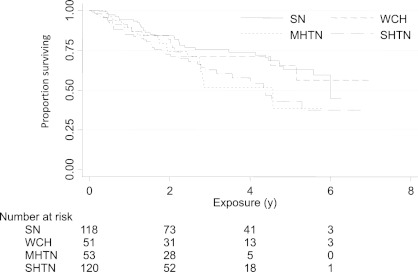
Figure 1 shows the Kaplan–Meier survival curves depicting the relationship between all-cause mortality and BP categories as determined by median midweek dialysis BP. A significant relationship between increasing levels of hypertension from SN to WCH to MHTN to SHTN and all-cause mortality was seen with pre- and postdialysis BP. It took at least 2 years before differences in survival were evident.
Figure 1.
Kaplan–Meier survival curves for ambulatory systolic BP and mortality. The numbers below the abscissa indicate those at risk. Mortality curves separate after 2 years. The mortality of white-coat hypertension (WCH) was similar to that seen with sustained normotension (SN). On the other hand, the mortality of masked hypertension (MHTN) was similar to that of sustained hypertension (SHTN). The equality of survival curves between WCH and SN on the one hand and MHTN and SHTN on the other was tested using the log rank test and found to be significant (P = 0.009).
Discussion
The major findings of our study were as follows: (1) the prevalence of MHTN and WCH were 15% each in a sizable cohort of well characterized subjects; (2) the classification of hypertension by distinguishing SN and SHTN from MHTN and WCH improved the prediction of all-cause mortality even after multivariate adjustment; and (3) classification into BP categories on the basis of pre- and postdialysis recordings suggested that WCH may have a higher risk than SN, whereas MHTN may have a mortality risk even higher than that seen with SHTN.
It is now well recognized that there is a continuum of risk from SN to WCH to MHTN to SHTN. We therefore have focused on the trend in risk increments with increasing severity of hypertension. This trend remains strong even after multivariate adjustments, which suggests that ambulatory BP measurements add to refining risk prediction among hemodialysis patients. Despite being the largest ambulatory BP study reported to date, we only had approximately 100 patients with WCH or MHTN and the 95% confidence interval for the hazards for mortality were wide. Accordingly, we have not used the confidence intervals of the individual estimates of hazards for the hypertension categories in Table 3 in making strong conclusions. We have instead focused on the trends.
A previous report from our group showed that out-of-dialysis-unit BP recordings (ambulatory or home BP recordings) were associated with increasing all-cause mortality with increasing severity of hypertension (18). These findings suggest that BP recorded outside of the dialysis unit may contain greater prognostic information compared with BP measured in the dialysis unit (19–22). The report presented here extends previous findings by providing a means to define MHTN and WCH. As in the general population, we found that WCH was associated with a better prognosis than SHTN, and that MHTN was associated with a prognosis that was worse than SN (23). Because it took at least 2 years before the survival curves separated, among hemodialysis patients, long-term follow-up is required to ascertain the relationship of BP and mortality (24).
A meta-analysis that pooled the estimates from studies performed among people with chronic kidney disease reported the prevalence of WCH to be 18.3% (25). Therefore, the prevalence of WCH of 15% in the study presented here was similar to that among people with chronic kidney disease not on dialysis. However, the prevalence of MHTN of 15% as defined by median midweek intradialytic BP was substantially higher than the 8.3% prevalence estimate from the same meta-analysis (25). On the other hand, the prevalence of MHTN defined by predialysis BP was 4%. As pointed out in the meta-analysis (25), the prevalence estimates of these conditions are strongly dependent on the threshold BP used for classification.
Surprisingly, patients with MHTN were more often treated with antihypertensive medications. This is not to be expected because if hypertension is truly masked, then physicians should not use more antihypertensive medications. One reason for this surprising finding may be because patients with MHTN had an average predialysis BP of 154.8/81.4 mmHg, which was much higher than the predialysis BP of those with SN (135.0/72.6 mmHg). Physicians often base their antihypertensive therapy on predialysis BP recording, and this may have led to greater antihypertensive medication use in these patients.
When postdialysis BP recordings were used to classify patients into hypertension categories, we found that those patients who were classified as masked hypertensives had a mortality that was even higher than that seen among sustained hypertensives. We reasoned that patients who had more weight removal during dialysis would have a lower BP postdialysis, but that these patients may have a higher interdialytic ambulatory BP. Indeed, masked hypertensives had the highest interdialytic weight gain. However, adjusting for the interdialytic weight gain did not remove the elevated mortality risk. Thus, this elevated mortality risk may be explained by another mechanism. Those with MHTN may have increased arterial stiffness and may have a greater interdialytic BP elevation compared with sustained normotensives for a given change in interdialytic volume. Because arterial stiffness strongly correlates with increased all-cause mortality, these observations may explain the increased mortality among those with MHTN (26).
There are several strengths and limitations of our work. Our study was largely limited to black people, and we excluded certain patients such as those with morbid obesity and atrial fibrillation because of difficulties with accurate BP assessment in this group. Whether the same results would hold in people of other races and of broader clinical characteristics is not known and will require verification in future cohorts. Reproducibility of the classification method proposed here needs to be addressed in future studies. Some strengths of our study are as follows: (1) we used all-cause mortality—an end point that is least prone to bias in ascertaining outcomes; (2) we validated the definitions of MHTN and WCH by several techniques that included median midweek intradialytic, pre-, and postdialysis BP.
The implications of our findings are as follows. First, among hemodialysis patients, we provide a preliminary framework to define the categories of MHTN and WCH. We suggest using the threshold of 140/80 mmHg because it shows a prevalence of WCH and MHTN that is line with what is seen in the general population. Furthermore, these classes have prognostic significance. The hypertension category was reclassified in 25% to 30% of the patients with ambulatory BP monitoring regardless of the way we defined MHTN or WCH. This suggests that these findings are not simply a statistical phenomenon. WCH and MHTN, when included in the classification of hypertension, improve the prognostic significance of BP obtained in the dialysis unit.
Disclosures
None.
Acknowledgments
This study was funded by National Institutes of Health grant 5R01-DK062030-07.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1. U.S. Renal Data System: USRDS 2010 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, Bethesda, MD, National Institute of Health, National Institute of Diabetes and Digestive and Kidney Disease, 2010 [Google Scholar]
- 2. Agarwal R, Nissenson AR, Batlle D, Coyne DW, Trout JR, Warnock DG: Prevalence, treatment, and control of hypertension in chronic hemodialysis patients in the United States. Am J Med 115: 291–297, 2003 [DOI] [PubMed] [Google Scholar]
- 3. Agarwal R, Andersen MJ, Bishu K, Saha C: Home blood pressure monitoring improves the diagnosis of hypertension in hemodialysis patients. Kidney Int 69: 900–906, 2006 [DOI] [PubMed] [Google Scholar]
- 4. Agarwal R, Lewis RR: Prediction of hypertension in chronic hemodialysis patients. Kidney Int 60: 1982–1989, 2001 [DOI] [PubMed] [Google Scholar]
- 5. Pickering TG, Davidson K, Gerin W, Schwartz JE: Masked hypertension. Hypertension 40: 795–796, 2002 [DOI] [PubMed] [Google Scholar]
- 6. Pickering TG: White coat hypertension: Time for action. Circulation 98: 1834–1836, 1998 [DOI] [PubMed] [Google Scholar]
- 7. Pickering TG, James GD, Boddie C, Harshfield GA, Blank S, Laragh JH: How common is white coat hypertension? JAMA 259: 225–228, 1988 [PubMed] [Google Scholar]
- 8. Levin NW, Kotanko P, Eckardt KU, Kasiske BL, Chazot C, Cheung AK, Redon J, Wheeler DC, Zoccali C, London GM: Blood pressure in chronic kidney disease stage 5D—Report from a Kidney Disease: Improving Global Outcomes controversies conference. Kidney Int 77: 273–284, 2010 [DOI] [PubMed] [Google Scholar]
- 9. Sinha AD, Agarwal R: Peridialytic, intradialytic, and interdialytic blood pressure measurement in hemodialysis patients. Am J Kidney Dis 54: 788–791, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rahman M, Griffin V, Kumar A, Manzoor F, Wright JT, Jr, Smith MC: A comparison of standardized versus“usual” blood pressure measurements in hemodialysis patients. Am J Kidney Dis 39: 1226–1230, 2002 [DOI] [PubMed] [Google Scholar]
- 11. Agarwal R, Peixoto AJ, Santos SF, Zoccali C: Pre and post dialysis blood pressures are imprecise estimates of interdialytic ambulatory blood pressure. Clin J Am Soc Nephrol 1: 389–398, 2006 [DOI] [PubMed] [Google Scholar]
- 12. Agarwal R, Metiku T, Tegegne GG, Light RP, Bunaye Z, Bekele DM, Kelley K: Diagnosing hypertension by intradialytic blood pressure recordings. Clin J Am Soc Nephrol 3: 1364–1372, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Agarwal R, Brim NJ, Mahenthiran J, Andersen MJ, Saha C: Out-of-hemodialysis-unit blood pressure is a superior determinant of left ventricular hypertrophy. Hypertension 47: 62–68, 2006 [DOI] [PubMed] [Google Scholar]
- 14. Agarwal R: Supervised atenolol therapy in the management of hemodialysis hypertension. Kidney Int 55: 1528–1535, 1999 [DOI] [PubMed] [Google Scholar]
- 15. Gerin W, Schwartz JE, Devereux RB, Goyal T, Shimbo D, Ogedegbe G, Rieckmann N, Abraham D, Chaplin W, Burg M, Jhulani J, Pickering TG: Superiority of ambulatory to physician blood pressure is not an artifact of differential measurement reliability. Blood Press Monit 11: 297–301, 2006 [DOI] [PubMed] [Google Scholar]
- 16. K/DOQI clinical practice guidelines for cardiovascular disease in dialysis patients. Am J Kidney Dis 45: S1–S153, 2005 [PubMed] [Google Scholar]
- 17. Egger M, Schneider M, Davey SG: Spurious precision? Meta-analysis of observational studies. BMJ 316: 140–144, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Agarwal R: Blood pressure and mortality among hemodialysis patients. Hypertension 55: 762–768, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Amar J, Vernier I, Rossignol E, Bongard V, Arnaud C, Conte JJ, Salvador M, Chamontin B: Nocturnal blood pressure and 24-hour pulse pressure are potent indicators of mortality in hemodialysis patients. Kidney Int 57: 2485–2491, 2000 [DOI] [PubMed] [Google Scholar]
- 20. Agarwal R, Peixoto AJ, Santos SF, Zoccali C: Out-of-office blood pressure monitoring in chronic kidney disease. Blood Press Monit 14: 2–11, 2009 [DOI] [PubMed] [Google Scholar]
- 21. Tripepi G, Fagugli RM, Dattolo P, Parlongo G, Mallamaci F, Buoncristiani U, Zoccali C: Prognostic value of 24-hour ambulatory blood pressure monitoring and of night/day ratio in nondiabetic, cardiovascular events-free hemodialysis patients. Kidney Int 68: 1294–1302, 2005 [DOI] [PubMed] [Google Scholar]
- 22. Alborzi P, Patel N, Agarwal R: Home blood pressures are of greater prognostic value than hemodialysis unit recordings. Clin J Am Soc Nephrol 2: 1228–1234, 2007 [DOI] [PubMed] [Google Scholar]
- 23. Ohkubo T, Kikuya M, Metoki H, Asayama K, Obara T, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai Y: Prognosis of “masked” hypertension and “white-coat” hypertension detected by 24-h ambulatory blood pressure monitoring 10-year follow-up from the Ohasama study. J Am Coll Cardiol 46: 508–515, 2005 [DOI] [PubMed] [Google Scholar]
- 24. Agarwal R: Hypertension and survival in chronic hemodialysis patients—Past lessons and future opportunities. Kidney Int 67: 1–13, 2005 [DOI] [PubMed] [Google Scholar]
- 25. Bangash F, Agarwal R: Masked hypertension and white-coat hypertension in chronic kidney disease: A meta-analysis. Clin J Am Soc Nephrol 4: 656–664, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Blacher J, Guerin AP, Pannier B, Marchais SJ, Safar ME, London GM: Impact of aortic stiffness on survival in end-stage renal disease. Circulation 99: 2434–2439, 1999 [DOI] [PubMed] [Google Scholar]