Abstract
Introduction:
The World Health Organization has declared India as the “diabetic capital” of the world. In controlling of such chronic, mostly asymptomatic disease, patients’ role can’t be overemphasized.
Aims:
To assess the level of compliance to anti-diabetic therapies and to ascertain the determinants of non-compliance, if any.
Materials and Methods:
A cross-sectional observational study was conducted for 3 months in a diabetic clinic of R G Kar Medical College and Hospital, Kolkata. Data were collected by interviewing the patients, examining their prescriptions and laboratory reports and anthropometry after obtaining informed consent.
Results:
Blood report at the point of data collection revealed controlled glucose homeostasis in 38.93% patients but evaluation of past 3 months report showed only 24.3% had control over hyperglycemia. Glycemic control was seen to be positively related to short duration of disease, compliance to therapies, and high knowledge about diabetes. Compliance to therapies found in 32.22% of study subjects was in turn associated with short duration of disease. House-wives showed poor compliance; insulin treatment with or without oral-anti-diabetic agent showed better compliance. Knowledge of diabetes was significantly high among higher educated; poor among women, house-wives, and rural people.
Conclusion:
Patient-providers collaboration is to be developed through a patient-centered care model based on the mutual responsibility of both so that each patient is considered in the mesh of his/her other goals of life and helped to promote empowerment to take informed decision for behavioral change conducive to control the disease.
Keywords: Adherence, compliance, diabetic-knowledge, glycemic control
INTRODUCTION
Due to economic, demographic, and epidemiological transition, India is facing double burden of diseases, i.e. rapid emergence of the noncommunicable disease which is the second highest (44%) cause of death only next to the unfinished agenda of communicable diseases which still shares 47% mortality of the country.[1] Our health system traditionally developed to tackle the communicable diseases and nutritional disorders is not yet reformed fully to handle the rapid march of the noncommunicable health problems. Moreover, the expensive and technology oriented curative care seriously depletes the scarce societal resources which are still very much needed to cope with the traditional communicable and nutritional disorders.[2] Diabetes mellitus (DM) has grown very fast during the past two decades.[3] At present, India leads the global top ten countries in terms of highest number of people with diabetes with current figure of 40.9 million followed by China having 39.8 million.[4] It is projected to increase to 69.9 million by 2025.[3] Every fifth patient visiting a consulting physician is a diabetic and every seventh patient visiting a family physician is a diabetic.[5] The World Health Organization (WHO) has declared India as the “diabetic capital” of the world.[6] Studies have shown that increasing patient knowledge regarding disease and its complications has significant benefits with regard to patient compliance to treatment and to decreasing complications associated with the disease.[7] Considering this, it was sought to quantify in a population of diabetics visiting the clinic, the level of knowledge about diabetes and compliance to its treatment.
Objective(s)
To describe the socio-demographic profile of patients attending the clinic,
To assess the level of compliance to anti-diabetic therapies,
To ascertain the causes of noncompliance, if any.
MATERIALS AND METHODS
Study type and design
An Institution based cross-sectional observational study was conducted from January to March 2010 among the diabetic patients attending diabetes clinic (held once a week) at R G Kar Medical College and Hospital (RGKMC and H), Kolkata, a tertiary care teaching hospital.
Sampling design and sample size
As on records, average attendance of diabetic clinic was 180 per day. Among them, approximately 70% were follow-up visits/patients and they were the study population for the present study. About 1500 follow-up patients would attend the clinic in three months duration. 10% of these patients were included into the study with the help of systematic random sampling method. Thus, 152 patients were selected for the study.
Data collection and analysis
After getting approval, data pertaining to socio-demographic variables, information of diabetic condition e.g. duration, treatment modalities with duration, complication, family history, compliance to treatment and height-weight etc. were collected by interviewing patients using a predesigned and pretested questionnaire; examining medical records and by anthropometry after obtaining informed consent. Socio-economic status (SES) was judged as per modified B.G. Prasad's scale.[8] Patients were also asked some questions that tested their knowledge about causation of diabetes, desired blood sugar level, and how to be achieved, complication if untreated, ways of prevention of DM, and comprehensibility of physician's advices. The knowledge score was calculated by points given for correct answers.[5] 20 was the maximum score. Score of 50% or less (≤10) and more than that were considered as poor/average and good. Plasma sugar approximate to recommended value, i.e. fasting <110, <90 mg%, and post-prandial <140, <120 mg% for normal individual and pregnant lady, respectively, was considered “controlled.” Three response sheets were duplicated and excluded. Thus, data collected from 149 diabetic subjects were analyzed using simple proportion, “t”, “χ2” tests and odds ratio (OR) with 95% confidence interval (CI), SPSS 17, and Epi info 3.4.3 version.
RESULTS
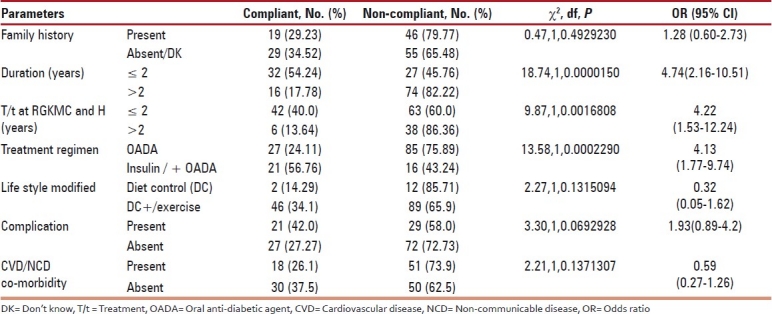
The mean, median, and range of age of participants were 49.4±12.9, 49 and 5-76 years, respectively. Of the participants, 28.18%, 61.07% and 10.74 % belonged to the age groups of ≤44, 45-65, and ≥66 years, respectively. Males were 33.6% and older than females (52.8±13.6 yrs vs 47.7±12.3 yrs with t=2.21 at df=147, P≤0.05). Majority (77.2%) were Hindu and urban residents (75.8%). About 45% were either illiterate or had schooling up to primary level; 41.61%, 13.42% had secondary, higher secondary (HS) and above level of education. Out of 149 cases, 4 were type-I diabetics, 2 were Gestational diabetics (GDM) and rest were type-II diabetics. On the whole, present plasma glucose level was within normal limit in 38.93% subjects and 50%, 100%, and 37.76% in type-I, GDM, and type-II DM subjects. Glycemic control was not found to be associated with age, sex, religion, residence, education, occupation, SES, family history of DM, regularity and type of anti-diabetic drug intake, presence of cardiovascular disease (CVD) or other non-communicable disease (NCD) co-morbidity (33.56% patients had hypertension, 7.38% were hypothyroid, 3.36% were suffering from CHD, 4.69% had dyslipidemia, 1.34% were patients of COPD and 2.68% were suffering from anxiety/insomnia/depression, etc.) for which they were being treated concurrently [Tables 1 and 2]. It was also found not to have association with DM-related complications [Table 2] (6.71% patients reported abscess/gangrene of foot/toe, 13.42% complained of low vision, 6.71% had early cataract, 1.34% had glaucoma, 4.03% were diagnosed to suffer from peripheral neuropathy and 0.67% had compromised renal functions). However, satisfactory plasma glucose was seen among those who were reportedly suffering from DM for last 2 years or less and the same was true for those who were being treated at diabetic clinic of RGKMC and H for last 2 years or less [Table 2]. More than two-third (67.78%) participants were non-compliant who mentioned the component(s) of advice (multiple responses) they couldn’t comply and indicated as cause of poor glycemic control. Financial constraints was reported by 11.88%, 37.37% confessed their inability to carry out physical exercise as advised, majority (54.54%) were unable to maintain dietary restriction, 6.06% reported alteration of drug regimen by their own and another 13.13% participants stated anxiety as cause of elevated plasma glucose. Anti-diabetic drugs were boosted/altered for 35.2% of participants with abnormal glucose homeostasis whereas 13.8% of patients of controlled hyperglycemia revealed reduction of drugs and or dose.
Table 1.
Present status of glucose homeostasis and socio-demographic profile (N=149)
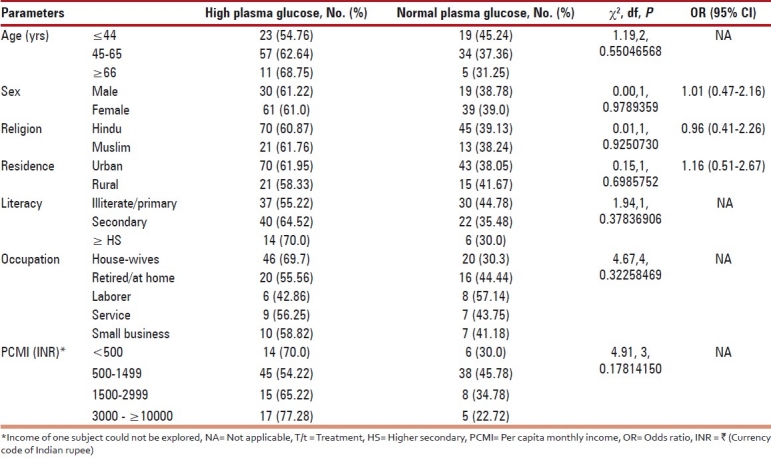
Table 2.
Present status of glucose homeostasis and some correlates (N=149)
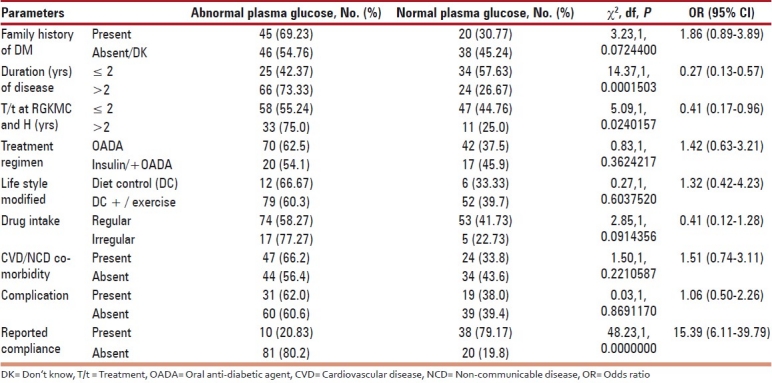
Proportion of person with desirable plasma glucose was significantly more among the compliant group [Table 2]. The compliance was not found to be related to age, sex, residence, religion, education, SES [Table 3], family background of diabetes, co-morbidity of CVD/NCD, difference in advice for life style modification etc. [Table 4]. However, occupation, short duration of disease and treatment at RGKMC and H, anti-diabetic drug regimen were shown to have significant effect on compliance [Tables 3 and 4]. All the reportedly irregular anti-diabetic drug users (14.77%) were found among the non-compliant group.
Table 3.
Compliance as per socio-demographic profile (N=149)
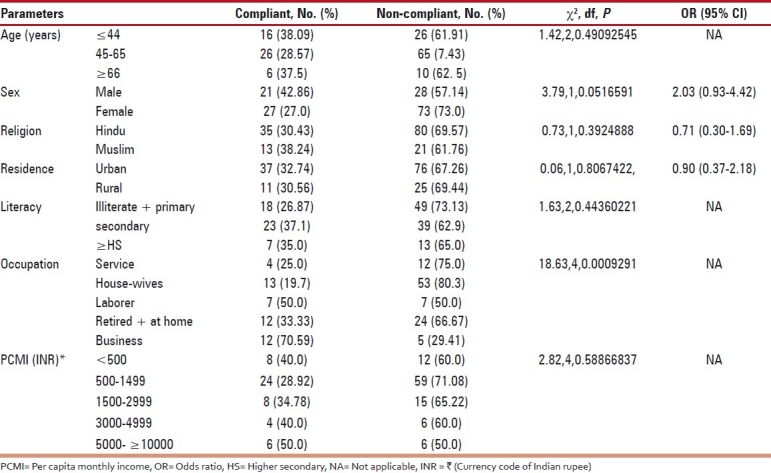
Table 4.
Compliance and some attributes of the disease (N=149)
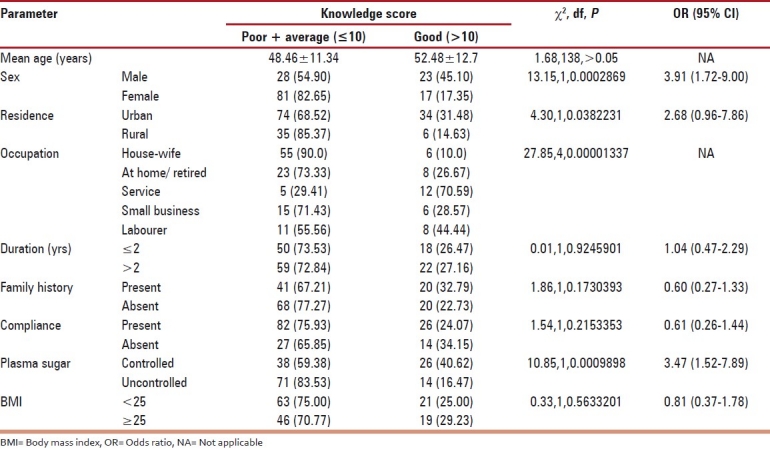
Only 26.85% of participants had good scoring (>50% marks) in knowledge about DM and showed proportionately more subjects with controlled plasma glucose [Table 5]. Knowledge was found to have significant association with sex, residence, occupation [Table 5], and literacy [F (ANOVA) =7.533 and P=0.001 among illiterate, primary, secondary, and higher secondary and above groups].
Table 5.
Knowledge (score) about diabetes (N=149)
Almost 61% knew nothing about causation of DM, 38.5% didn’t have any/correct idea about the desired plasma glucose level; 42.86%, 40.0%, 22.86%, and 20.0% reportedly knew eye, kidney involvement, CVD risk, and other specific harmful effects of DM, respectively. 27.9% were unaware about major complications of uncontrolled hyperglycemia and 37.1% didn′t know how DM can be prevented. Hopefully, 92.9% study subjects knew at least one measure to control hyperglycemia. With multiple responses, 77.14%, 80.0%, and 42.85% of patients mentioned physical exercise, dietary restriction, and anti-diabetic drugs, respectively, as measures to achieve blood glucose homeostasis. More than 98% participants reportedly comprehended all their physician's advices, 57.14% showed recommended BMI value (<25).
Retrospective tracking of 3 months laboratory results revealed that target blood sugar level was achieved and maintained on long-term basis only in 24.3% cases and was revealed to be influenced significantly by compliance (χ2 = 12.19 at df = 1, OR = 7.68 with 95% CI of 1.94 to 31.92) and short duration of the disease (χ2 = 4.07 at df=1, P=0.0436933, OR=3.13 with 95% CI of 0.88 to 11.33).
DISCUSSION
Lion's share of participants were women, middle aged (45-65 years), and senior citizen (≥66 years) suffering from type-II DM. The study revealed an unsatisfactory level of present and past glycemic control which was found associated with poor compliance [Table 2]. Poor compliance was noted in 67.78% cases and was less than that (89.62%) observed by Bhattacharya et al,[9] in their study. Compliance was very poor among house-wives and good in people engaged in small scale business. Bhattacharya et al.[9] also found poor compliance among the house-wives. This might be partly due to significantly high illiteracy/low literacy among the house-wives (χ2 test of goodness of fit between occupations = 25.35, df = 2, P<0.001) who failed to produce better yield of knowledge as also observed by Bhattacharya et al.[9] Poor compliance of the house-wives might be attributed partly to their higher economic dependence (χ2 =89.94 at df=1, P=0.00000001; OR= 0.01 with 95% CI= 0.00-0.04), 87% of whom were house-wives or at home elderly women dependent either on husband, son, daughter, or others. All 12 non-complaints due to financial constraints were women. Like Bhattacharya et al,[9] the present study failed to elicit any difference in compliance among the patients with or without family history of diabetes but unlike her, significantly high compliance among those having better knowledge regarding DM [Table 5].
The present study showed 37.37% non-compliance to physical exercise as against 18.58% by Bhattacharya[10] and 11.88% non-compliance due to financial constraints as against 16.98% revealed by Bhattacharya et al.[9] Studies showed that compliance to chronic disease, particularly in asymptomatic conditions like diabetes, hypertension, etc. was found to be unsatisfactory[11,12] due to the traditional physician-directed/compliance-oriented approach where patients are considered as passive receivers of the medical expertise ignoring his/her other goals of life and is judged and blamed for inability or unwillingness to achieve medical goal.[13,14] It brings dissatisfaction/frustrations among the patients which begets non-compliance and ends in frustration among the physicians.[13] These patients need to be empowered to take informed decision how to achieve control over the disease on daily basis in the context of other goals of their life.[13] However, poor knowledge scores by 73.15% of participants were not very evident for empowering them as also showed by Gulabani et al,[5] in their study at diabetic clinic of Christian Medical College, Ludhiana. The knowledge about DM showed no relationship with duration of disease. This might be the by-product of the poor patient care model[13,14] and huge patients’ load in the clinic leads to a poor patients-physicians interaction.[15] Similarly, Gulabani[5] and Viswanathan et al,[16] found that significantly poor knowledge among women might be due to low literacy among them (58% vs. 18.4%, χ2 = 20.87, at df=1, P = 0.0000049, OR= 6.14 with 95% CI=2.52-15.30). The same observation was true for the rural people (χ2=4.19, df = 1, P =0.0406713; OR=0.44 with 95% CI=0.19-1.04) who in addition might not receive information about DM through other channels of communication. 91% patients were told for physical exercise, 77.14% knew its role, still 37.37% missed it and 57.14% achieved recommended BMI. 80.0% subjects mentioned dietary restriction to combat hyperglycemia but 54.54% failed to implement. Moreover, the knowledgeable group failed to show a significant difference in practice, e.g. recommended BMI, compliance to therapies. So a gap between knowledge and practice was conspicuous and might be due to the lack of inner force for a positive behavioral change.
CONCLUSION
To achieve the complex target of diabetes control which needs persistent motivation on the part of the patients is a critical issue. Chronic disease care is fundamentally different and requires a different vision and redefinition of the patient-physician relationship. Because diabetes is mostly a self-managed disease, patients are more than passive recipients of medical expertise and sound patient-physician collaboration is to be developed for controlling DM on the basis of trust and understanding of every client's other facets of life. The patients are to be empowered to take informed decision for sustained change in life styles and behavior using this patient-centered and adherence-oriented approach. The roles and responsibility need to be redefined to match the reality of diabetic care and patient and physicians must create relationships that promote collaboration and partnership.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Lal S, Adarsh P. 2nd ed. New Delhi: CBS Publishers and Distributors; 2009. Textbook of Community Medicine. [Google Scholar]
- 2.Bal A. Diabetes: Ethical, social and economic aspects. [Last accessed on 2010 Aug];Issues Med Ethics. 2000 8:77–8. Available from: http://www.issuesinmedicalethics.org/083mi077.html . [PubMed] [Google Scholar]
- 3.Taneja DK. 8th ed. Delhi-93: Doctors Publications (Regd); 2010. Health Policies and Programmes in India. [Google Scholar]
- 4.Diabetes Epidemic out of Control, Press release, International Diabetic Federation. 2006. Dec, [Last accessed on 2010 Sep 2]. Available from: http://www.IDF (http://www.idf.org/node/1354?unode=7F22F450-B1ED-43BB-A57C-B975D16A812D .
- 5.Gulabani Ml, John M, Isaac R. Knowledge of diabetes, its treatment and complications amongst diabetic patients in a tertiary care hospital. Indian J Community Med. 2008;33:204–6. doi: 10.4103/0970-0218.42068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta V, Suri P. Diabetes in elderly patients. JK Pract. 2002;91:258–9. [Google Scholar]
- 7.Heisler M, Pietee JD, Spencer M, Kieffer E, Vijan S. The relationship between knowledge of recent HbA1c values and diabetes care understanding and self-management. Diabetes Care. 2005;28:816–22. doi: 10.2337/diacare.28.4.816. [DOI] [PubMed] [Google Scholar]
- 8.Agarwal AK. Social classification: The need to update in the present scenario. Indian J Community Med. 2008;33:50–1. doi: 10.4103/0970-0218.39245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bhattacharya N, Biswas R, Das MK, Chatterjee PS. A study on compliance status of diabetes mellitus patients. Indian J Public Health. 2005;49:34–5. [PubMed] [Google Scholar]
- 10.Bhattacharya M. A study of medical dedication behaviour of Varanasi urban of diabetic mellitus patients. Indian J Prev Soc Med. 2009;40:130–7. [Google Scholar]
- 11.Sweileh W, Aker O, Hamooz S. Rate of compliance among patients with diabetes mellitus and hypertension. J Res (N.Sc.) 2005;19:1–12. [Google Scholar]
- 12.Pendleton L, House WC, Parker LE. Physicians’ and Patients’ Views of Problems of Compliance with Diabetes Regimens. Public Health Rep. 1987;102:21–6. [PMC free article] [PubMed] [Google Scholar]
- 13.Funnell MM, Anderson RM. The Problem with Compliance in Diabetes. JAMA. 2000;284:1709. [PubMed] [Google Scholar]
- 14.Delamater AM. Improving Patient Adherence. Clin Diabetes. 2006;26:71–7. [Google Scholar]
- 15.Shah JH, Murata GH, Duckworth WC, Hoffman RM, Wendel CS. Factors Affecting Compliance in Type 2 Diabetic Patients: Experience from the Diabetes Outcomes in Veterans Study (DOVES) Int J Diabetes Dev Ctries. 2003;23:75–82. [Google Scholar]
- 16.Viswanathan V, Shobhana R, Snehalatha C, Seena R, Ramachandran A. Need of education on foot care in diabetic patients in India. J Assoc Physicians India. 1999;47:1083–5. [PubMed] [Google Scholar]


