Abstract
Leiomyomas are common benign tumors in the uterus. However, vaginal leiomyomas remain an uncommon entity with only about 300 reported cases. Here, we report a case of a 38-year-old multigravida who presented with lower abdominal pain and vaginal bleeding. A physical examination and ultrasonography were performed, and a diagnosis of cervical fibroid was made. Pervaginal removal of the tumor was performed and subsequent histopathology revealed a vaginal leiomyoma. Although a rare tumor, vaginal leiomyomas may present with a variety of clinical features and may be mistaken preoperatively for cervical fibroid. Removal of tumor by vaginal route, wherever possible, with subsequent histopathological examination appears to be the optimum management plan.
Keywords: Leiomyoma, vaginal tumour, benign uterine tumour
INTRODUCTION
Vaginal tumors are rare and include papilloma, hemangioma, mucus polyp, and rarely leiomyoma. Vaginal leiomyomas remain an uncommon entity with only about 300 reported cases since the first detected case back in 1733 by Denys de Leyden.[1] Bennett and Erlich[2] found only nine cases in 50,000 surgical specimens and only one case in 15,000 autopsies reviewed at Johns Hopkins Hospital. These tumors arise most commonly from the anterior vaginal wall causing varied clinical presentations. They may or may not be associated with leiomyomas elsewhere in the body. We report a case of primary leiomyoma of vagina arising from anterior wall and presenting with lower abdominal pain, bleeding, and a feeling of something coming out of vagina.
CASE REPORT
A 38-year-old female gravid 2, para 2 presented to the outpatient department with complaints of lower abdominal pain, abnormal vaginal bleeding, and dyspareunia since 8 months. There was no history of dysuria, increased frequency, or any feature of urinary retention. The patient complained that she noticed something appeared to come down her vagina for the last 2 months. A pervaginal examination revealed a mass in the vagina, but the upper limit of the mass could not be delineated. An ultrasonography was performed which showed a 6 × 4 cm hypoechoic mass in the upper part of vagina and a possibility of pedunculated cervical fibroid was made. There was no other abnormality on ultrasonography. The tumor was surgically removed by vaginal route. A Foley's catheter was introduced in the urethra for protecting the latter. The tumor was then sent for histopathological examination with a peroperative diagnosis of vaginal leiomyoma. Gross examination revealed a 6 × 5 cm solid mass with a whorling appearance in the cut section [Figure 1]. Microscopic examination revealed a well-circumscribed leiomyoma underlying the squamous epithelium, consistent with the diagnosis of vaginal leiomyoma [Figure 2].
Figure 1.

Photograph showing the whorling pattern on cut section of the vaginal tumor
Figure 2.
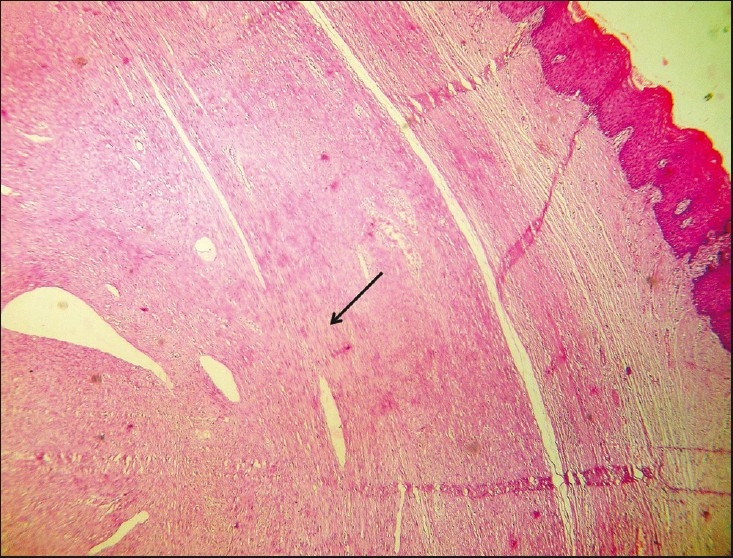
Microphotograph showing the leiomyoma (arrow) with the overlying vaginal squamous epithelium (right side) (hematoxylin and eosin stain, ×100 magnification)
DISCUSSION
Tumors of vagina are rare and there are only around 300 reported cases of vaginal leiomyomas since the first described case in 1733 by Denys de Leyden.[1] Leiomyomas in female genital tract are common in the uterus and to some extent in the cervix followed by the round ligament, utero-sacral ligament, ovary, and inguinal canal.[1] Occurrence in vagina is very rare. Vaginal leiomyomas are commonly seen in the age group ranging from 35 to 50 years and are reported to be more common among Caucasian women.[2] They usually occur as single, well-circumscribed mass arising from the midline anterior wall[1,3] and less commonly, from the posterior and lateral walls.[4] They may be asymptomatic but depending on the site of occurrence, they can give rise to varying symptoms including lower abdominal pain, low back pain, vaginal bleeding, dyspareunia, frequency of micturation, dysuria, or other features of urinary obstruction These tumors can be intramural or pedunculated and solid as well as cystic. Usually these tumors are single, benign, and slow growing but sarcomatous transformation has been reported.[5] Preoperatively, diagnosis by ultrasonography may be difficult, but magnetic resonance imaging usually clinches the diagnosis. In magnetic resonance imaging, they appear as well-demarcated solid masses of low signal intensity in T1- and T2-weighted images, with homogenous contrast enhancement, while leiomyosarcomas and other vaginal malignancies show characteristic high T2 signal intensity with irregular and heterogeneous areas of necrosis or hemorrhage.[6,7] However, histopathological confirmation is the gold standard of diagnosis and also beneficial to rule out any possible focus of malignancy. Surgical removal of the tumor through vaginal approach, preferably with urethral catheterization to protect the urethra during surgery, is usually the treatment of choice. In case of large tumors, however, an abdomino-perineal approach is preferred. The patient needs to be followed up for chance of recurrence. Our patient was symptom-free at 5-month follow-up.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Young SB, Rose PG, Reuter KL. Vaginal fibromyomata: Two cases with preoperative assessment, resection and reconstruction. Obstet Gynecol. 1991;78:972–4. [PubMed] [Google Scholar]
- 2.Bennett HG, Jr, Erlich MM. Myoma of the vagina. Am J Obstet Gynecol. 1941;42:314–20. [Google Scholar]
- 3.Shimada K, Ohashi I, Shibuya H, Tanabe F, Akashi T. MR imaging of an atypical vaginal leiomyoma. Am J Roentg. 2002;178:752–4. doi: 10.2214/ajr.178.3.1780752. [DOI] [PubMed] [Google Scholar]
- 4.Elsayes KM, Narra VR, Dillman JR, Velcheti V, Hameed O, Tongdee R, et al. Vaginal Masses: Magnetic Resonance Imaging Features with Pathologic Correlation. Acta Radiol. 2007;8:921–33. doi: 10.1080/02841850701552926. [DOI] [PubMed] [Google Scholar]
- 5.Cobanoğlu O, Gürkan Zorlu C, Ergun Y, Kutluay L. Leiomyosarcoma of the vagina. Eur J Obstet Gynecol Reprod Biol. 1996;70:205–7. doi: 10.1016/s0301-2115(95)02554-5. [DOI] [PubMed] [Google Scholar]
- 6.Bae J H, Choi SK, Kim JW. Vaginal leiomyoma: A case report and review of the literature. J Women's Med. 2008;1:92–4. [Google Scholar]
- 7.Shadbolt CL, Coakley FV, Qayyum A, Donat SM. MRI of vaginal leiomyomas. J Comput Assist Tomogr. 2001;25:355–7. doi: 10.1097/00004728-200105000-00005. [DOI] [PubMed] [Google Scholar]


