Abstract
BACKGROUND AND OBJECTIVES:
The most frequent procedures performed on women with abnormal uterine bleeding are 2D and 3D ultrasound. The most common accepted approach for the management of abnormal uterine bleeding is 2D TV scan followed by therapeutic hysteroscopy. The purpose of this prospective study was to assess whether 3D saline infusion sonohysterography (3D SIS) could replace diagnostic hysteroscopy (DH) for the diagnosis of endometrial pathology, in patients with abnormal uterine bleeding.
DESIGN AND SETTING:
A prospective study in the ultrasound department of the Women's Specialized Hospital, King Fahad Medical City, Riyadh, Saudi Arabia from January 2008 to February 2010.
PATIENTS AND METHODS:
0One hundred and one patients with abnormal uterine bleeding, suspected to have endometrial abnormality by 2D and 3D transvaginal scan, were prospectively studied. Of these, 55 patients had undergone both 3D SIS and DH, followed by verification of results with histopathology.
RESULTS:
Upon comparison of 3D SIS and DH individually with histopathology, specificity and sensitivity for 3D SIS were 67% and 100%, respectively, and for hysteroscopy 67% and 98%, respectively. In addition, the positive predictive value and negative predictive value were 98% and 100%, respectively, for 3D SIS, while for DH they were 98% and 67%, respectively.
CONCLUSION:
3D SIS is a safe alternative to hysteroscopy. However, larger randomized controlled trials should be conducted to ascertain the validity and reliability of this advantageous, less-invasive procedure, for women with abnormal uterine bleeding, who require evaluation of the endometrial cavity.
Abnormal uterine bleeding (AUB) is one of the most common reasons for women seeking gynecological advice.1–5 Other than dysfunctional uterine bleeding (DUB), intrauterine abnormalities are the leading cause of AUB. More than 40% of affected women with AUB are reported to have intrauterine abnormalities.6 The most common anatomical causes of AUB in women are submucosal fibroids, endometrial polyps, and endometrial hyperplasia.4 As 10% to 15% of postmenopausal vaginal bleeding is due to endometrial cancer, a thorough investigation should be carried out to evaluate these symptoms.7 The most frequent procedure performed on women with abnormal uterine bleeding is 2D and 3D ultrasound.1–5,7 For many years the most common accepted approach for the management of abnormal uterine bleeding has been the 2D TV scan followed by therapeutic hysteroscopy combined with a histological examination of the obtained specimen.8
Transvaginal sonography (TVS) is used as an initial investigation because it is easy, rapid and cost effective, but it is unable to differentiate intrauterine pathology with complete certainty.5 The gold standard for diagnosis of intrauterine abnormalities is diagnostic hysteroscopy combined with a histological examination of endometrial aspiration or biopsy.1,5,6,9–12 Hysteroscopy is invasive, reasonably expensive, time consuming, and involves general anesthesia.9–11 Hysteroscopy is also associated with risks like uterine perforation and ascending genitourinary infection.10,13
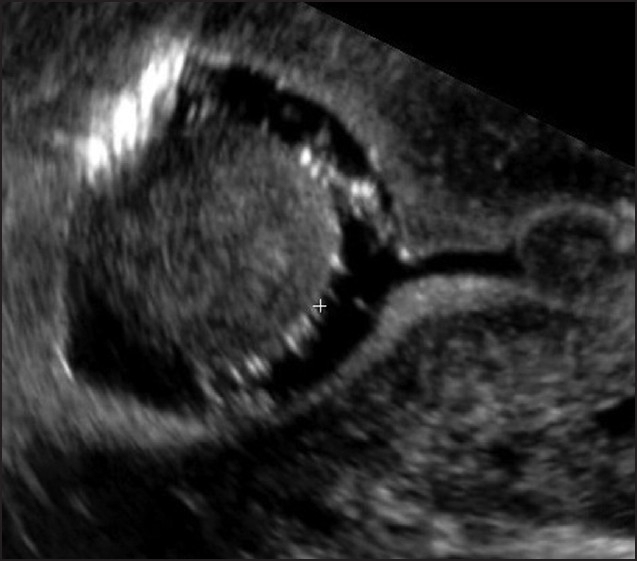
Three-dimensional saline infusion sonography (3D SIS) in comparison to hysteroscopy is less invasive, cheaper, and does not require general anesthesia.9,10 3D SIS reliably evaluates uterine contour, adhesions, and focal pathologies.8 Furthermore, in 3D SIS, after distending the cavity with saline, there is clear visualization of the inner surface of both sides of the endometrium.8,13 Focal and diffuse abnormalities can be distinguished, and in most cases an endometrial polyp can be differentiated from the submucous fibroid based on the imaging characteristics.8,9 The polyps are typically round in shape, smooth in outline, and are generally echogenic, compared to the endometrium or are isoechoic to it. The underlying endometrial-myometrial interface is preserved (Figures 1, 2).2,8 The presence of a vascular pedicle has a positive predictive value of up to 81.3%.8 Fibroids are more inhomogeneous, hypoechoic, and there is a loss of endometrial-myometrial interface. The percentage of the intracavitary portions of the submucous fibroids can be assessed by 3D SIS (Figure 3). In addition, the submucous fibroids can be differentiated from the intramural fibroids that are distorting the cavity (Figure 4). Thus by distending the inner walls of the endometrium, focal and diffuse lesions can be identified, along with the location and size of the pathology, with reasonable accuracy.2,8,10,13
Figure 1.

Saline infusion sonography demonstrating posterior wall uterine polyp, protruding into the cavity, measuring 15×10 mm.
Figure 2.

Saline infusion sonography demonstrating a 13×11 mm uterine polyp arising from the left fundal uterine wall.
Figure 3.
Saline infusion sonography demonstrating a 30×30 mm intrcavitary uterine fibroid, protruding from the fundus.
Figure 4.

Saline infusion sonography demonstrating a 34×35 mm intramural fibroid distorting the cavity.
3D SIS is easily accepted by most patients as an outpatient procedure.6 Complications are rare with 3D SIS. The patient may experience anxiety, discomfort, and mild lower abdominal cramps during balloon inflation and instillation of saline. However, the symptoms abate soon after the end of the procedure.10,13 Vaginal spotting may also occur for one or two days after the procedure. Only 1% to 2% infection was reported, mostly as endometritis.2
The procedure is usually well-tolerated.12 The purpose of the study was to assess whether three-dimensional saline infusion sonohysterography (3D SIS) can replace diagnostic hysteroscopy (DH) for the diagnosis of endometrial pathology in patients with abnormal uterine bleeding.
PATIENTS AND METHODS
A prospective study was conducted in the Ultrasound Department, of the Women's Specialized Hospital, King Fahad Medical City, a tertiary care hospital between January 2008 and February 2010. Data acquired included TVS, SIS, hysteroscopy, and histopathogy results. In addition, patient age, and duration and description of AUB were also noted.
The study was approved by the institutional review board (IRB). The study group included both women in their reproductive age and postmenopausal women who had irregular or excessive uterine bleeding, along with abnormal endometrial lining on transvaginal 2D and 3D ultrasound. Women with bleeding due to pregnancy or pelvic infections were excluded. All patients were offered 3D SIS and were further offered hysteroscopy after completion of 3D SIS.
3D SIS was performed on cycle day 5 to day 10 post menses. This was recommended to prevent abortion of an early pregnancy and also to minimize confusion of a thickened secretory endometrium of the second half of the cycle. If the bleeding was irregular, the examination could be performed after a negative pregnancy test. Bleeding was not a contraindication to perform 3D SIS; however, it was avoided whenever possible, as the blood clot could give false positive results. No prophylactic antibiotics or analgesics were used at our institute. Written informed consent was taken and the risks for 3D SIS were discussed with the patient before the procedure. All cases were performed on the same machine by a single experienced and expert operator.
To perform 3D SIS, the patient is placed in the dorsal lithotomy position, a sterile bivalve vaginal speculum is used, and the cervix is visualized and cleaned with povidone-iodine (Betadine). A single lumen, 5 French H/S elliptoshpere catheter (Ackrad Labs, Cooper Surgical, Berlin, Germany) is then introduced through the cervix and into the uterine cavity. The balloon is inflated to fix the catheter into the cavity, as this provides stable filling and minimal backflow of saline. After this, 10 mL to 15 mL saline is instilled into the uterine cavity resulting in distention of the uterine cavity. The mean time required for the procedure is about 10 minutes. The speculum is removed and a 3D transvaginal scan is performed by a high frequency (7 MHZ) 3D transvaginal transducer (Philips iU22 Ultrasound System, USA). A 3D ultrasound is generated by the automatic sweep of the transducer, to calculate the volume where multiple sagittal and coronal images of the endometrium are taken. The use of 3D SIS involves acquisition of data volume, which is then digitally stored in orthogonal planes for subsequent analysis. It can also be studied at length at a latter time for endometrial pathology. The addition of 3D US makes the examination rapid, enhances visualization and illustrates a more detailed pathology of the endometrial cavity. On the other hand the hysteroscopy recorded data cannot be modified after the procedure and final diagnosis is determined by the initial findings at the time of the procedure. Data collection was completed and data analysis was done using SPSS software (Chicago, IL, USA).
RESULTS
Of 101 patients with abnormal uterine bleeding, 43 (43%) patients had menorrhagia, 37 patients (37%) had irregular bleeding, 12 patients (12%) had perimenopausal bleeding, and nine patients (9%) had postmenopausal bleeding. The mean age (standard deviation) was 44 (8.8) years. Transvaginal 2D and 3D scan in these 101 patients revealed homogenous endometrial thickness in six patients (6%) and inhomogeneous endometrial thickness in nine patients (9%). Polyps were seen in 51 patients (50%), submucosal fibroids in 28 patients (28%), and a normal cavity in seven patients (7%).
3D SIS was attempted in these 101 patients revealing homogenous endometrial thickness in three patients (3%) and inhomogeneous endometrial thickness in four patients (4%). Polyps were seen in 60 patients (59%), submucosal fibroids in 17 patients (17%), a normal cavity in eight patients (8%), a distorted cavity in three patients (3%), and 3D SIS was not done in six patients (6%). Among these six patients, we were unable to introduce the catheter in three patients (3%) due to cervical stenosis, one (1%) patient refused 3D SIS, one (1%) had marked vaginal adhesions, and one (1%) had a large cervical polyp obscuring the external os.
Hysteroscopy was done in 58 (57%) patients, 12 (12%) patients were lost to follow-up, in 13 (13%) patients hysteroscopy was not required, as the endometrial sampling results were normal, hysterectomy was performed in two (2%), and 16 patients were awaiting hysteroscopy. Of the 58 patients in whom hysteroscopy was performed, normal cavities were found in three patients (3%), endometrial polyps in 40 patients (39%), submucous fibroids in 13 patients (13%), a distorted cavity in one (1%) patient, and thickened endometrium in one patient (1%). Of these 58 patients we were unable to perform 3D SIS in two patients and a sample for histopathology could not be obtained in one, due to distorted endometrial cavity. Thus, there were a total of 55 patients, who had both 3D SIS and hysteroscopy and the results were verified by histopathology.
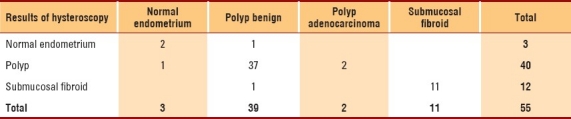
Histopathology results were collected in 59 patients. The histopathology results were obtained by curetting the endometrium during hysteroscopy in 57 patients and by hysterectomy in two patients. Proliferative endometrium was found in 4 patient (7%), endometrial polyp in 39 patients (66%), submucous fibroids in 14 patients (24%), and hyperplasia in 2 patients. Of the 39 polyps confirmed by histopathology, 2 (5%) were found to be adenomcarcinoma of the uterus. The histopathology results were then individually compared with the 3D SIS and hysteroscopy results (Table 1).
Table 1.
Test validation between saline infusion sonohysterography (SIS) and hysteroscopy.
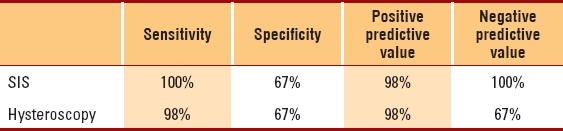
Forty-two 3D SIS results were categorized as polyps and 41 were confirmed by histopathology. Although, during hysteroscopy, 40 polyps were identified, 39 were confirmed by histopathology and one result came as normal endometrium. One polyp was missed by hysteroscopy. Submucosal fibroids were confirmed in 11 of 55 patients by histopathology. 3D SIS identified all 11 cases accurately. Hysteroscopy identified 12 cases of submucous fibroids in total, of which 11 were confirmed by histopathology and one submucous fibroid result came as a polyp (Tables 2, 3).
Table 2.
Comparison of saline infusion sonohysterography (SIS) with pathological findings.
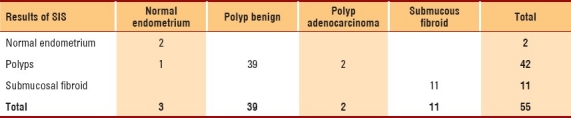
Table 3.
Comparison of hysteroscopy with pathological findings.
No infection occurred in any of the patients at our institute, thus it is indicating a very safe procedure.
DISCUSSION
Abnormal uterine bleeding is a very common symptom in women of all ages. Its management is a significant financial burden on healthcare resources. For patients with AUB, 2D and 3D US is performed as an initial investigation. If the endometrium is found to be normal, ≤5 mm in postmenopausal women or ≤16 mm in a premenopausal patient, a clinical evaluation is made.
In cases where TVS demonstrates an abnormal endometrial thickness or if TVS is suboptimal, 3D SIS or hysteroscopy is performed. 3D SIS is also recommended in patients with normal TVS who are unresponsive to medical management.8 Evaluation of AUB is of special importance in postmenopausal women, because of the high prevalence of endometrial cancer in these women.9 Ninety-five percent of women with endometrial cancer present with postmenopausal bleeding.
Various investigation modalities are adopted to distinguish between the functional causes and organic causes of AUB, such as, polyps, uterine fibroids, endometrial hyperplasia, and endometrial cancer. It is important to find the underlying cause, as management of the organic causes is surgical, while the functional causes are treated medically. Information about the type of lesion, location, and extent of involvement of the myometrium facilitates the management decision and selection of the surgical procedure.4,13
Hysteroscopy is widely available and is a reliable method for investigating women with AUB. It allows for direct visualization of the endometrial cavity, with accurate assessment of intracavitary lesions,13 and thus, accurate removal of lesions such as polyps and submucosal fibroids.9,13 However, it provides limited assessment with regard to the myometrial extension of the fibroid.13 Both 3D SIS and DH have excellent diagnostic accuracy in diagnosing submucous fibroids, polyps, and endometrial hyperplasia.4 In our study, 3D SIS proved to be equal to DH, as determined by the gold standard, histopathology. The sensitivity and specificity of 3D SIS were found to be slightly superior to DH. In addition SIS effectively differentiated polyps from submucosal fibroids. There was 100% accuracy in detecting submucosal fibroids by SIS in comparison to 91.6% detection by DH. Regarding polyps the accuracy of detection was found to be equal, which was 97.6% and 97.5% for SIS and DH, respectively.
Considering the accuracy, convenience, time, and cost-effectiveness, 3D SIS should replace DH as an initial investigation in women with AUB. Salim et al, published a prospective double blind study in which he evaluated the European Society classification of submucosal fibroid with 3D SIS results. Their results were further compared with the findings from DH. They concluded that there was good agreement between 3D SIS and DH for classification of submucosal fibroids.13 Salim et al was mentioned that a new classification of submucosal fibroids by 3D SIS was required, which might improve the preoperative selection of patients that are suitable for hysteroscopy. For the assessment of a submucosal fibroid, 3D SIS and magnetic resonance imaging (MRI) were found to be superior to hysteroscopy.13 Glanc reported a similar performance of both 3D SIS and DH as investigation tools in premenopausal women with AUB, with a sensitivity and specificity of 95% and 88%, respectively, for 3D SIS, and 96% and 90% for hysteroscopy.8 In another study by Erdem et al, the sensitivity and specificity by 3D SIS in the diagnosis of an endometrial polyp were 100% and 91.8%, respectively, and in the diagnosis of fibroids were 95% and 100%, respectively.10 Ryu et al, also supported the accuracy of 3D SIS in diagnosing the endometrial pathology, giving a sensitivity and specificity of 95.1% and 83.3%, respectively.7 Thus, many studies have proved combined TVS and 3D SIS to be more accurate and cost-effective than hysteroscopy.7,12
Concerns have been raised about hysteroscopy being not only an expensive and invasive procedure, but unnecessary in 50% of the women who had normal findings, suggesting 3D SIS as an initial alternative approach in investigating women with AUB.5,11
In a meta-analysis, a total of 2228 procedures were reviewed that compared 3D SIS with hysteroscopy or hysterectomy. The pooled sensitivity of 3D SIS for evaluating uterine cavity was 0.95 (95% confidence interval [CI], 0.93–0.97), and the pooled specificity was 0.88 (95% CI, 0.85–0.92). This meta analysis suggested that SIS was an accurate means of evaluating the endometrial cavity in pre- and postmenopausal women with AUB.11 The procedure (3D SIS) when combined with aspiration biopsy could become the standard means of evaluating the uterine cavity in both pre- and postmenopausal women.11
There could be significant cost savings if 3D SIS combined with guided biopsy replaces diagnostic hysteroscopy.5,11 Hysteroscopy cannot be used as a first-line test in all women with AUB, because it is invasive and expensive. However, 3D SIS when combined with TVS can be a reliable, first-line investigation procedure in women with AUB4,5 , as it is rapid, cost-effective, and is relatively safe.5 In a prospective study by Bonnamy et al., the performance of 3D SIS prior to any surgical intervention avoided 30% of DH and indicated unnecessary operative hysteroscopies that could have been hysterectomies.5
The high diagnostic accuracy of 3D SIS has been supported by many recent articles and it has been concluded that 3D SIS can replace DH.6 It is now widely accepted that 3D SIS is the method of choice for the evaluation of endometrial pathology7 and after 3D SIS, the patient can be directed to the appropriate therapeutic option.8 As a result, hysteroscopy should no longer be considered as an initial diagnostic modality for evaluating women with AUB. Hysteroscopy should be reserved for cases where an intrauterine lesion has already been diagnosed on 3D SIS or when 3D SIS is inconclusive. In the future, 3D SIS can be combined with guided endometrial biopsies, which will further increase the sensitivity and specificity of the procedure. The new technique of ultrasound-guided biopsies has promising results.14,15
In summary, 3D SIS is rapid, safe, highly effective, painless, and a less invasive method in comparison to hysteroscopy. 3D SIS can be used as a first-line diagnostic approach in patients with AUB.
Acknowledgments
The authors would like to thank Dr. Sahar Al-Swailem, Dr. Mamoun Awad, and Dr. Saleh Al-Salih for their support in this study. Gratitude is extended to Mrs. Sandra Al-Abdulmunem for her literature search assistance and finally Hanan Al Amodi and Hoda Al saigh for their typing assistance.
REFERENCES
- 1.Moschos E, Ashfaq R, McIntire DD, Liriano B, Twickler DM. Saline infusion sonography endometrial sampling compared with endometrial biopsy in diagnosing endometrial pathology. Obstet Gynecol. 2009;113:881–7. doi: 10.1097/AOG.0b013e31819b3fc7. [DOI] [PubMed] [Google Scholar]
- 2.Li Ong C. Saline infusion sonohysterography. Ultrasound Clin. 2007;2:121–3. [Google Scholar]
- 3.Susanna I. An imaging algorithm for evaluation of abnormal uterine bleeding: Does sonohysterogrphy play a role? Menopause. 2007;14:823–5. doi: 10.1097/gme.0b013e318136e1c6. [DOI] [PubMed] [Google Scholar]
- 4.Farquhar C, Ekeroma A, Furness S, Arroll B. A systematic review of transvaginal ultrasonography, sonohysterography and hysteroscopy for the investigation of abnormal uterine bleeding in premenopausal women. Acta Obstet Gynecol Scand. 2003;82:493–504. doi: 10.1034/j.1600-0412.2003.00191.x. [DOI] [PubMed] [Google Scholar]
- 5.Bonnamy L, Marret H, Perrotin F, Body G, Berger C, Lansac J. Sonohysterography: A prospective survey of results and complications in 81 patients. Eur J Obstet Gynecol Reprod Bio. 2002;102:42–7. doi: 10.1016/s0301-2115(01)00567-x. [DOI] [PubMed] [Google Scholar]
- 6.de Kroon CD, Jansen FW. Saline infusion sonography in women with abnormal uterine bleeding: An update of recent findings. Curr Opin Obstet Gynecol. 2006;18:653–7. doi: 10.1097/01.gco.0000247395.32711.68. [DOI] [PubMed] [Google Scholar]
- 7.Ryu J, Kim B, Lee J, Kim S, Lee S. Comparison of transvaginal ultrasonography with hysterosonography as a screening method in patients with abnormal uterine bleeding. Korean J Radiol. 2004;5:39–46. doi: 10.3348/kjr.2004.5.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Glanc P, Betel C, LevToaff A. Sonohysterography: Technique and clinical applications. Ultrasound Clin. 2008;3:427–31. [Google Scholar]
- 9.Alfhaily F, Ewies A. The first-line investigation of postmenopausal bleeding: Transvaginal ultrasound scanning and endometrial biopsy may be enough. Int J Gynecol Cancer. 2009;19:892–5. doi: 10.1111/IGC.0b013e3181a83387. [DOI] [PubMed] [Google Scholar]
- 10.Erdem M, Bilgin U, Bozkurt N, Erdem A. Comparison of transvaginal ultrasound and saline infusion sonohysteroscopy in evaluating the endometrial cavity in pre- and postmenopausal women with abnormal uterine bleeding. Menopause. 2007;14:846–52. doi: 10.1097/gme.0b013e3180333a6b. [DOI] [PubMed] [Google Scholar]
- 11.De Kroon CD, De Bock GH, Dieben SW, Jansen FW. Saline contrast hysterosonography in abnormal uterine bleeding: A systematic review and meta- analysis. Obstet Gynecol Survey. 2004;59:265–6. doi: 10.1111/j.1471-0528.2003.02472.x. [DOI] [PubMed] [Google Scholar]
- 12.Hamilton JA, Larson AJ, Lower AM, Hasnain S, Grudzinskas JG. Routine use of saline hysterosonography in 500 consecutive, unselected, infertile women. Hum Reprod. 1998;13:2463–73. doi: 10.1093/humrep/13.9.2463. [DOI] [PubMed] [Google Scholar]
- 13.Salim R, Lee C, Davies B, Jolaoso E, Ofuasia E, Jurkovic D. A comparative study of three-dimensional saline infusion sonohysterography and diagnostic hysteroscopy for the classification of submucous fibroids. Hum Reprod. 2005;20:253–7. doi: 10.1093/humrep/deh557. [DOI] [PubMed] [Google Scholar]
- 14.Lee C, Ben-Nagi J, Ofili-Yebovi D, Davies A, Jurkovic D. A new method of transvaginal ultrasound guided polypectomy, a feasibility study. Ultrasound Obstet Gynecol. 2006;27:198–207. doi: 10.1002/uog.2668. [DOI] [PubMed] [Google Scholar]
- 15.Wei AY, Schink JC, Pritts EA, Olive DL, Lindheim SR. Saline contrast sonohysterography and directed extraction, resection and biopsy of intrauterine pathology using a uterine Explora curette. Ultrasound Obstet Gynecol. 2006;27:202–5. doi: 10.1002/uog.2599. [DOI] [PubMed] [Google Scholar]


