Abstract
BACKGROUND AND OBJECTIVE:
Accreditation is usually a voluntary program in which trained external peer reviewers evaluate a healthcare organization's compliance and compare it with pre-established performance standards. The aim of this study was to evaluate the impact of accreditation programs on the quality of healthcare services
METHODS:
We did a systematic review of the literature to evaluate the impact of accreditation programs on the quality of healthcare services. Several databases were systematically searched, including Medline, Embase, Healthstar, and Cinhal.
RESULTS:
Twenty-six studies evaluating the impact of accreditation were identified. The majority of the studies showed general accreditation for acute myocardial infarction (AMI), trauma, ambulatory surgical care, infection control and pain management; and subspecialty accreditation programs to significantly improve the process of care provided by healthcare services by improving the structure and organization of healthcare facilities. Several studies showed that general accreditation programs significantly improve clinical outcomes and the quality of care of these clinical conditions and showed a significant positive impact of subspecialty accreditation programs in improving clinical outcomes in different subspecialties, including sleep medicine, chest pain management and trauma management.
CONCLUSIONS:
There is consistent evidence that shows that accreditation programs improve the process of care provided by healthcare services. There is considerable evidence to show that accreditation programs improve clinical outcomes of a wide spectrum of clinical conditions. Accreditation programs should be supported as a tool to improve the quality of healthcare services.
Accreditation is usually a voluntary program, sponsored by a non-governmental organization (NGO), in which trained external peer reviewers evaluate a healthcare organization's compliance and compare it with pre-established performance standards.1 Quality standards for hospitals and other medical facilities were first introduced in the United States in the “Minimum Standard for Hospitals” developed by the American College of Surgeons in 1917. After World War II, increased world trade in manufactured goods led to the creation of the International Standards Organization (ISO) in 1947.2 Accreditation formally started in the United States with the formation of the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) in 1951. This model was exported to Canada and Australia in the 1960s and 1970s and reached Europe in the 1980s. Accreditation programs spread all over the world in the 1990s.3 There are other forms of systems used worldwide to regulate, improve and market the services of healthcare providers and organizations, including Certification and Licensure. Certification involves formal recognition of compliance with set standards (e.g., ISO 9000 standards) validated by external evaluation by an authorized auditor. Licensure involves a process by which governmental authority grants permission, usually following inspection against minimal standards, to an individual practitioner or healthcare organization to operate in an occupation or profession.3 Although the terms accreditation and certification are often used interchangeably, accreditation usually applies only to organizations, while certification may apply to individuals, as well as to organizations.2
The aim of this study was to evaluate the impact of accreditation programs on the quality of healthcare services. Another recently published review of the literature related to accreditation had several limitations.4 It was not limited to health services accreditation, but also included heterogeneous types of accreditation programs, including medical education accreditation programs. In our review, we limited our search to health services accreditation. Second, the period covered in the search in the other review was only up to May 2007 and several important publications have been published since May 2007. Third, several important papers relevant to accreditation were missed in the other review.
METHODS
A comprehensive updated search of several electronic bibliographic databases was performed, including Medline, from 1996 to June 2009; Cinhal, from 1982 to June 2009; Embase, from 1980 to June 2009; and HealthStar, from 1980 to June 2009. Several keywords were utilized in different combinations, including “accreditation,” “health services,” “quality,” “quality indicators,” “quality of health care,” and “impact.” We included all studies that evaluated the impact of general or subspecialties accreditation programs on the quality of healthcare services. No language restrictions were used. We excluded studies that were published in “abstract” format only, studies evaluating the cost of accreditation and studies that evaluated the attitude of healthcare professionals towards accreditation. The bibliographies of all selected articles and relevant review articles were reviewed to identify additional studies. Experts in the area of accreditation were contacted to identify relevant studies. We included studies with different study designs, including clinical trials, observational studies and qualitative studies.
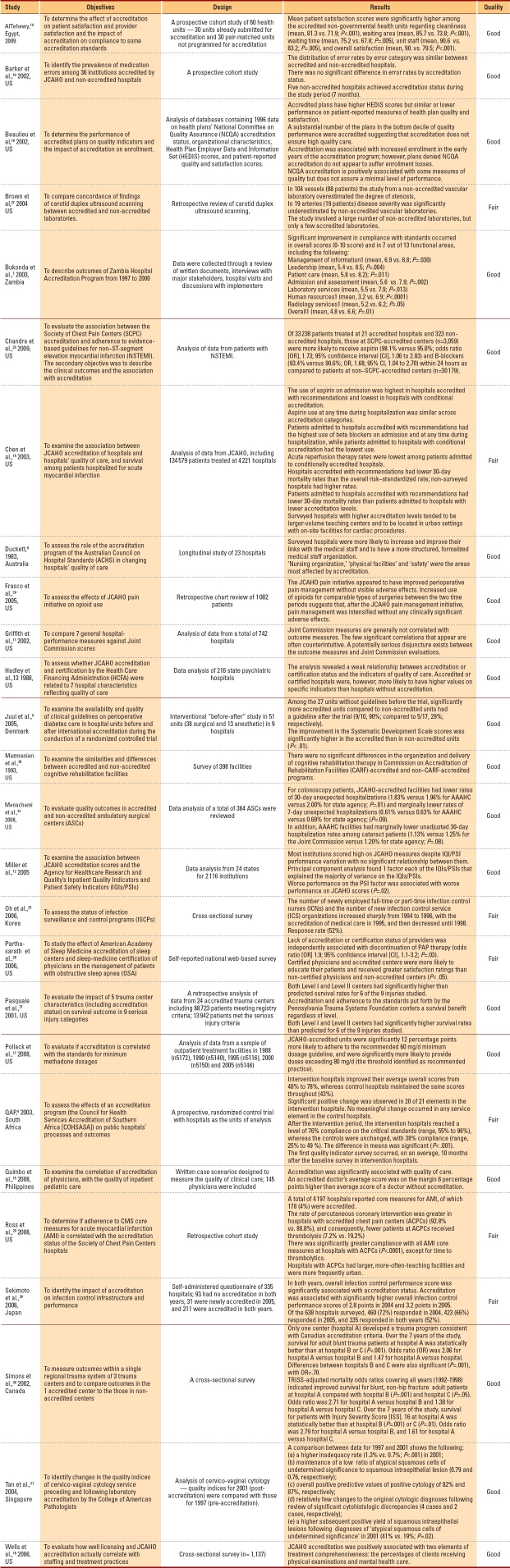
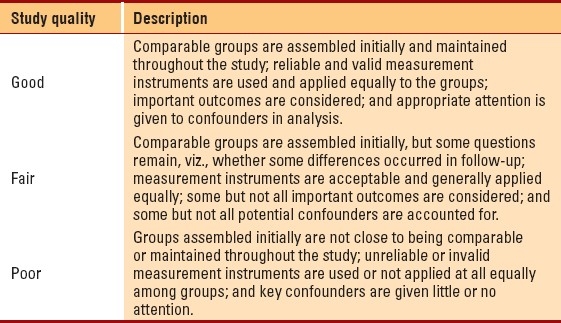
Our search identified 520 references. An analysis of abstracts of the citations was conducted to identify substantial studies relevant to health services accreditation (by AK). Fifty-one studies were identified as potentially eligible for inclusion in the review. The full text of these studies was reviewed. Twenty studies were excluded that described the attitude of healthcare professionals towards accreditation. Five studies were excluded that described the cost of accreditation of healthcare services. The assessment of quality of included studies was performed using the US Preventive Services Task Force approach (Table 1).5 We could not assess and compare the quality of included studies as there are no standardized criteria to assess and compare the quality of studies of different study designs; however, we described important quality features of each included study, including the study design and sample size.
Table 1.
Study quality grading approach.
RESULTS
Twenty-six studies were identified (Table 2). Ten studies evaluated the impact of a general accreditation program on the overall performance of hospitals. Nine studies evaluated the impact of a general accreditation program on a single aspect of hospital performance. Seven studies evaluated the impact of subspecialty accreditation programs.
Table 2.
Description of included impact studies.
The impact of general accreditation programs on the overall performance of hospitals
In the South African randomized controlled trial, 20 randomly selected public hospitals, stratified by size, were selected. Ten of these hospitals were randomized to the accreditation program in 1998; the other 10 served as controls. Survey data from the Council for Health Services Accreditation of Southern Africa (COHSASA) program were used; in addition, data on 8 indicators of hospital quality of care were collected by an independent research team. About 2 years after accreditation began; intervention hospitals significantly improved their average compliance with COHSASA accreditation standards, while no appreciable increase was observed in the control hospitals. However, with the exception of nurse perceptions of clinical quality, the independent research team observed little or no effect of accreditation on 7 other indicators of quality, including patient's satisfaction (n=1923), which was not found improved among accredited hospitals compared to non-accredited hospitals.6 In a large analysis of the Zambia Hospital Accreditation Program (n=79 hospitals), accreditation was associated with significant improvement in compliance with standards in the overall scores, and in 7 out of 13 important functional areas.7 In a longitudinal study of 23 hospitals in Australia, hospitals were monitored over 2 years for their response to accreditation requirements and the general changes in accreditation in the hospital's environment. There was an increase and improvement in the structure of medical staff organization, nursing organization and physical facilities and safety.8 In another study conducted in Copenhagen on 51 units (38 surgical and 13 anesthetic), significantly more accredited units had guidelines in place compared to non-accredited units. The improvement on the Systematic Development Scale was significantly higher in accredited than in non-accredited units.9 In an analysis of the National Committee on Quality Assurance (NCQA) and Health Plan Employer Data and Information Set (HEDIS) databases, accredited plans had higher HEDIS scores, but similar or lower performance on patient-reported measures of health plan quality and satisfaction. A substantial number of the plans in the bottom decile of quality performance were accredited, suggesting that accreditation does not ensure high-quality care.10 In an analysis of data from 742 hospitals using 7 performance measures against JCAHO accreditation scores, Joint Commission measures were found to be not correlated with outcome measures.11 In another large analysis of JCAHO accreditation scores and the Agency for Healthcare Research (AHRQ), Inpatient Quality Indicators (IQI) and Patient Safety Indicators (PSI) (n=2116 institutions), worse performance on the PSI factor was associated with worse performance on JCAHO scores (P=.02).12 In a large data analysis of 216 state psychiatric hospitals, there was a weak relationship between accreditation and indicators of quality of care.13 In a large Egyptian study involving 30 units already submitted for accreditation and 30 pair-matched units not programmed for accreditation, the overall satisfaction score of providers was significantly higher among accredited health units. Most of the checked standards had compliance above 90% in accredited units and were significantly higher than compliance in non-accredited units.14 In a cross-sectional survey (n=145) conducted in the Philippines, using vignettes or case scenarios scores, the quality of clinical care was significantly higher among accredited physicians compared to non-accredited physicians.15
The impact of general accreditation programs on a single aspect of a hospital's performance
In a large analysis of data from Centers for Medicare and Medicaid Services (CMS) in US (n=134 579 patients from 4221 hospitals), patients treated at accredited hospitals were more likely to receive higher quality of care for the management of acute myocardial infarction (AMI) than those treated at non-accredited hospitals. In this study, the mortality rate was lower post AMI in accredited hospitals than in non-accredited hospitals.16 In a cross-sectional survey conducted in the US in 1988 (n=5172), 1990 (n=5140), 1995 (n=5116), 2000 (n=5150) and 2005 (n=5146), methadone maintenance facilities accredited by JCAHO were more likely to adhere to the recommended dosage guideline of methadone, compared to non-accredited hospitals.17 In a large cross-sectional survey of outpatient substance abuse treatment programs conducted in the US (n=1137), JCAHO accreditation was positively associated with two elements of treatment comprehensiveness: the percentages of clients receiving physical examinations and mental health care.18 In an American prospective study (n=36 institutions), medication error rates were similar between accredited and non-accredited hospitals. In this study, 5 non-accredited hospitals achieved accreditation during the study.19 In a large cross-sectional survey conducted in Japan over 2 consecutive years (n=638 hospitals), the overall infection control performance score was significantly associated with accreditation status.20 In a retrospective analysis at 24 accredited trauma centers in the United States (n=88 723 patients), accreditation was significantly associated with higher survival rates for patients presenting with six types of trauma injuries.21 In an analysis of huge data from ambulatory surgical centers in the US, there was a significant reduction in unexpected hospitalizations in patients undergoing colonoscopy (n=315 070) in accredited ambulatory surgical centers (ASC) compared to non-accredited ASC. In this study, there was also a reduction in unexpected hospitalizations in patients undergoing cataract surgery (n=245 154; P=.08) in accredited ASC compared to non-accredited ASC.22 In a large cross-sectional survey of acute care hospitals (n=85), the number of newly employed full-time or part-time infection control nurses (ICNs) and the number of new infection control service (ICS) organizations increased sharply from 1994 to 1996 with the accreditation of medical care services in 1995, and then decreased until 1998.23 In a retrospective chart review (n=1082), JCAHO pain initiatives on opioids use significantly improved perioperative pain management without a visible increase in adverse effects.24
The impact of subspecialty accreditation programs
A large analysis was conducted in the United States to evaluate the association between the Society of Chest Pain Centers (SCPC) accreditation and adherence to evidence-based guidelines for the management of AMI (n= 33 238 patients treated at 344 hospitals). Patients treated at accredited centers (n=3059) were significantly more likely to receive aspirin and B-blockers within 24 hours than patients at non-accredited centers (n=30 179).25 In another large retrospective analysis conducted in the US (n= 4197 hospitals), the rate of percutaneous coronary intervention was greater in hospitals accredited by the Society of Chest Pain Centers than in non-accredited hospitals (92.8% vs. 80.8%). There was significantly greater compliance with eight acute myocardial infarction (AMI) core measures at accredited hospitals compared with non-accredited hospitals.26 A retrospective analysis (n=178) reviewed the findings of carotid duplex ultrasound scanning performed at accredited and non-accredited laboratories in the United States (accreditation by the Intersocietal Commission for Accreditation of Vascular Laboratories). There was a significant overestimation by non-accredited laboratories of the degree of stenosis of carotid arteries in 51% of patients. In this study, there was a significant underestimation of the degree of stenosis of carotid arteries by non-accredited laboratories among 11% of patients.27 In a self-reported web-based survey, lack of accreditation (by the American Academy of Sleep Medicine accreditation) was independently associated with suboptimal sleep medicine management. Accredited centers received greater satisfaction ratings than non-accredited centers.28 In a large survey of 398 cognitive rehabilitation therapy facilities in the US, there were no significant differences in the organization and delivery of cognitive rehabilitation therapy in facilities accredited by Commission on Accreditation of Rehabilitation Facilities (CARF) and in non–CARF-accredited facilities.29 In an analysis of data from three Canadian trauma centers, over 7 years, survival of blunt trauma patients at the accredited hospitals was statistically better than survival at non-accredited hospitals.30 A large analysis of cervico-vaginal cytology showed a modest overall positive predictive value of positive cytology in laboratory accredited by the College of American Pathologists.31
DISCUSSION
General accreditation programs appear to improve the structure and process of care, with a good body of evidence showing that accreditation programs improve clinical outcomes. The best study that evaluated this area was the Quality Assurance Program (QAP) trial. Randomization of this important trial controlled for important factors known to affect a hospital's ability to comply with and achieve accreditation standards for indicators such as hospital size, staffing levels, staff qualifications and budget levels. The first quality-indicator survey occurred, on an average, 10 months after the COHSASA baseline survey in the intervention hospitals. It is possible that these hospitals had already made considerable progress that was not captured because the first round of the survey was too late to be a true baseline, which may explain the lack of effect of accreditation on the selected quality indicators.5 Evidence is consistent from several studies to support a positive impact of general accreditation programs on different specific clinical outcomes, including the management of AMI, trauma, ambulatory surgical care, infection control and pain management. Several studies have shown a significant positive impact of subspecialty accreditation programs in improving clinical outcomes in different subspecialties, including sleep medicine, chest pain management and trauma management (Table 2). General accreditation programs of health organizations and accreditation of subspecialties should be encouraged and supported to improve the quality of healthcare services. One of the most important barriers to the implementation of accreditation programs is the skepticism of healthcare professionals in general and physicians in particular about the positive impact of accreditation programs on the quality of healthcare services.32,33 There is a need to educate healthcare professionals about the potential benefits of accreditation to resolve any skeptical attitude of healthcare professionals towards accreditation.
Conclusion
There is consistent evidence that shows that general accreditation programs improve the process of care provided by healthcare services. There is considerable evidence to show that general accreditation programs improve clinical outcomes of a wide spectrum of clinical conditions. There is also considerable evidence to show that accreditation programs of subspecialties improve clinical outcomes. Accreditation programs should be supported as a tool to improve the quality of healthcare services.
Acknowledgments
We would like to thank Dr. Abdulaziz Alnasser, Chairman of the Department of Family Medicine, King Faisal Specialist Hospital, for his support for this project. We are also grateful to Prof. David Haran, University of Liverpool; Dr. Vanja Berggren, University of Liverpool; Prof. M. Magzoub, King Saud bin Abdulaziz University for Health Sciences, for their valuable feedback during the thesis-defense process.
REFERENCES
- 1.Shaw CD. Toolkit for Accreditation Programs.The International Society for Quality In Health Care. Australia: 2004. [Google Scholar]
- 2.Montagu D. London: Department for international development health systems resource centre; [Last accessed on 2003]. Accreditation and other external quality assessment systems for healthcare: Review of experience and lessons learned. Available from: http://www.dfidhealthrc.org/publications/health_service_delivery/Accreditation.pdf . [Google Scholar]
- 3.Shaw CD. External quality mechanisms for health care: Summary of the ExPeRT project on visitatie, accreditation, EFQM and ISO assessment in European Union countries. External peer review techniques. European foundation for quality management. International organization for standardization. Int J Qual Health Care. 2000;12:169–75. doi: 10.1093/intqhc/12.3.169. [DOI] [PubMed] [Google Scholar]
- 4.Greenfield D, Braithwaite J. Health sector accreditation research: A systematic review. Int J Qual Health Care. 2008;20:172–83. doi: 10.1093/intqhc/mzn005. [DOI] [PubMed] [Google Scholar]
- 5.Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, et al. Current methods of the U.S. Preventive Services Task Force: A review of the process. Am J Prev Med. 2001;20:21–35. doi: 10.1016/s0749-3797(01)00261-6. [DOI] [PubMed] [Google Scholar]
- 6.Salmon J, Heavens J, Lombard C, Tavrow P. The impact of accreditation on the quality of hospital Care: KwaZulu-Natal Province Republic of South Africa: Published for the U.S. Agency for International Development (USAID) by the quality assurance project. University Research Co. 2003 (QAP trial) [Google Scholar]
- 7.Bukonda N, Tavrow P, Abdallah H, Hoffner K, Tembo J. Implementing a national hospital accreditation program: The Zambian experience. Int J Qual Health Care. 2003;14:716. doi: 10.1093/intqhc/14.suppl_1.7. [DOI] [PubMed] [Google Scholar]
- 8.Duckett S. Changing hospitals: The role of hospital accreditation. Soc Sci Med. 1983;17:1573–9. doi: 10.1016/0277-9536(83)90102-8. [DOI] [PubMed] [Google Scholar]
- 9.Juul AB, Gluud C, Wetterslev J, Callesen T, Jensen G, Kofoed-Enevoldsen A. DIPOM Group. The effects of a randomised multi-centre trial and international accreditation on availability and quality of clinical guidelines. Int J Health Care Qual Assur Inc Leadersh Health Serv. 2005;18:321–8. doi: 10.1108/09526860510602587. [DOI] [PubMed] [Google Scholar]
- 10.Beaulieu N, Epstein AM. National committee on quality Assurance health-plan accreditation: Predictors, correlates of performance, and market impact. Med Care. 2002;40:325–37. doi: 10.1097/00005650-200204000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Griffith JR, Knutzen SR, Alexander JA. Structural versus outcomes measures in hospitals: A comparison of Joint Commission and Medicare outcomes scores in hospitals. Qual Manag Health Care. 2002;10:29–38. doi: 10.1097/00019514-200210020-00007. [DOI] [PubMed] [Google Scholar]
- 12.Miller MR, Pronovost P, Donithan M, Zeger S, Zhan C, Morlock L, et al. Relationship between performance measurement and accreditation: Implications for quality of care and patient safety. Am J Med Qual. 2005;20:239–52. doi: 10.1177/1062860605277076. [DOI] [PubMed] [Google Scholar]
- 13.Hadley T, McGurrin M. Accreditation, certffication, and the quality of care in state hospitals. Hosp Community Psychiatry. 1988;39:739–42. doi: 10.1176/ps.39.7.739. [DOI] [PubMed] [Google Scholar]
- 14.Al Tehewy M, Bssiouni S, Habil I, EL Okda S. Evaluation of accreditation program in non-governmental organizations’ health units in Egypt: Short-term outcomes. Int J Qual Health Care. 2009;21:183–9. doi: 10.1093/intqhc/mzp014. [DOI] [PubMed] [Google Scholar]
- 15.Quimbo S, Peabody J, Shimkhada R, Woo K, Solon O. Should we have confidence if a physician is accredited? A study of the relative impacts of accreditation and insurance payments on quality of care in the Philippines. Soc Sci Med. 2008;63:505–10. doi: 10.1016/j.socscimed.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen J, Rathore SS, Radford MJ, Krumholz HM. JCAHO accreditation and quality of care for acute myocardial infarction. Health Aff. 2003;22:243–54. doi: 10.1377/hlthaff.22.2.243. [DOI] [PubMed] [Google Scholar]
- 17.Pollack HA, D’Aunno T. Dosage patterns in methadone treatment: Results from a national survey, 1988-2005. Health Serv Res. 2008;43:2143–63. doi: 10.1111/j.1475-6773.2008.00870.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wells R, Lemak C, Alexander J, Nahra T, Ye Y, Campbell C. Do licensing and accreditation matter in outpatient substance abuse treatment programs? J Subst Abuse Treat. 2007;33:43–50. doi: 10.1016/j.jsat.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 19.Barker K, Flynn E, Pepper G, Bates D, Mikeal R. Medication errors observed in 36 health care facilities. Arch Intern Med. 2002;162:1897–903. doi: 10.1001/archinte.162.16.1897. [DOI] [PubMed] [Google Scholar]
- 20.Sekimoto M, Imanaka Y, Kobayashi H, Okubo T, Kizu J, Kobuse H. Impact of hospital accreditation on infection control programs in teaching hospitals in Japan. Am J Infect Control. 2008;36:212–9. doi: 10.1016/j.ajic.2007.04.276. [DOI] [PubMed] [Google Scholar]
- 21.Pasquale MD, Peitzman AB, Bednarski J, Wasser TE. Outcome analysis of Pennsylvania trauma centers: Factors predictive of nonsurvival in seriously injured patients. J Trauma. 2001;50:465–72. doi: 10.1097/00005373-200103000-00010. [DOI] [PubMed] [Google Scholar]
- 22.Menachemi N, Chukmaitov A, Brown S, Saunders C, Brook R. Quality of care in accredited and nonaccredited ambulatory surgical centers. Jt Comm J Qual Patient Saf. 2008;34:546–51. doi: 10.1016/s1553-7250(08)34069-0. [DOI] [PubMed] [Google Scholar]
- 23.Oh Ha Won H, Kim J, Cho S. National survey of the status of infection surveillance and control programs in acute care hospitals with more than 300 beds in the Republic of Korea. Am J Infect Control. 2006;34:223–33. doi: 10.1016/j.ajic.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 24.Frasco P, Sprung J, Trentman T. The impact of the joint commission for accreditation ofhealthcare organizations pain initiative on perioperative opiate consumption and recovery room length of stay. Anesth Analg. 2005;100:162–8. doi: 10.1213/01.ANE.0000139354.26208.1C. [DOI] [PubMed] [Google Scholar]
- 25.Chandra A, Glickman SW, Ou FS, Peacock WF, McCord JK, Cairns CB, et al. An analysis of the association of society of chest pain centers accreditation to american college of cardiology/american heart association non-st-segment elevation myocardial infarction guideline adherence. Ann Emerg Med. 2009;54:17–25. doi: 10.1016/j.annemergmed.2009.01.025. [DOI] [PubMed] [Google Scholar]
- 26.Ross M, Amsterdam E, Peacock W, Graff L, Fesmire F, Garvey J. Chest pain center accreditation is associated with better performance of centers for medicare and medicaid services core measures for acute myocardial infarction. Am J Cardiol. 2008;102:120–4. doi: 10.1016/j.amjcard.2008.03.028. [DOI] [PubMed] [Google Scholar]
- 27.Brown W, Bendick P, Bove P, Graham L, Cornelius P, Zelenock G, et al. Reliability of extracranial carotid artery duplex ultrasound scanning: Value of vascular laboratory accreditation. Bro J Vasc Surg. 2004;39:366–71. doi: 10.1016/j.jvs.2003.08.018. [DOI] [PubMed] [Google Scholar]
- 28.Parthasarathy S, Haynes PL, Budhiraja R, Habib MP, Quan SF. A national survey of the effect of sleep medicine specialists and American Academy of Sleep Medicine Accreditation on management of obstructive sleep apnea. J Clin Sleep Med. 2006;2:133–42. [PubMed] [Google Scholar]
- 29.Mazmanian PE, Kreutzer JS, Devany CW, Martin KO. A survey of accredited and other rehabilitation facilities: Education, training and cognitive rehabilitation in brain-injury programmes. Brain Injury. 1993;7:319–31. doi: 10.3109/02699059309034958. [DOI] [PubMed] [Google Scholar]
- 30.Simons R, Kasic S, Kirkpatrick A, Vertesi L, Phang T, Appleton L. Relative importance of designation and accreditation of trauma centers during evolution of a regional trauma system. J Trauma. 2002;52:827–34. doi: 10.1097/00005373-200205000-00002. [DOI] [PubMed] [Google Scholar]
- 31.Tan K, Chang S, Soh V, Thamboo T, Nilsson B, Chan N. Quality indices in a cervicovaginal cytology service: Before and after laboratory accreditation. Arch Pathol Lab Med. 2004;128:303–7. doi: 10.5858/2004-128-303-QIIACC. [DOI] [PubMed] [Google Scholar]
- 32.Stoelwinder J. A study of doctors’ views on how hospital accreditation can assist them provide quality and safe care to consumers: Department of epidemiology and preventive medicine. Australia: Monash University; 2004. [Google Scholar]
- 33.Pomey MP, Contandriopoulos AP, François P, Bertrand D. Accreditation as a tool for organisational change. Int J Health Care Qual Assur. 2004;17:113–24. doi: 10.1108/09526860410532757. [DOI] [PubMed] [Google Scholar]