Abstract
Background
Acupuncture is commonly used in treating insomnia in China, and clinical studies have shown that acupuncture may have a beneficial effect on insomnia compared with Western medication.
Methods
We included randomized controlled trials on acupuncture for insomnia. We searched PubMed, the Cochrane Library (2008 Issue 3), China Network Knowledge Infrastructure (CNKI), Chinese Scientific Journal Database (VIP), and Wan Fang Database. All searches ended in December 2008. Two authors extracted data and assessed the trials' quality independently. RevMan 5.0.17 software was used for data analysis with effect estimate presented as relative risk (RR) and mean difference (MD) with a 95% confidence interval (CI).
Results
Forty-six (46) randomized trials involving 3811 patients were included, and the methodological quality of trials was generally fair in terms of randomization, blinding, and intention-to-treat analysis. Meta-analyses showed a beneficial effect of acupuncture compared with no treatment (MD −3.28, 95% CI −6.10 to −0.46, p = 0.02; 4 trials) and real acupressure compared with sham acupressure (MD −2.94, 95% CI −5.77 to −0.11, p = 0.04; 2 trials) on total scores of Pittsburgh Sleep Quality Index. Acupuncture was superior to medications regarding the number of patients with total sleep duration increased for >3 hours (RR 1.53, 95% CI 1.24–1.88, p < 0.0001). However, there was no difference between acupuncture and medications in average sleep duration (MD −0.06, 95% CI −0.30–0.18, p = 0.63). Acupuncture plus medications showed better effect than medications alone on total sleep duration (MD 1.09, 95% CI 0.56–1.61, p < 0.0001). Similarly, acupuncture plus herbs was significantly better than herbs alone on increase of sleep rates (RR 1.67, 95% CI 1.12–2.50, p = 0.01). There were no serious adverse effects with related to acupuncture treatment in the included trials.
Conclusions
Acupuncture appears to be effective in treatment of insomnia. However, further large, rigorous designed trials are warranted.
Introduction
Insomnia is one of the most common sleep disorders, with a prevalence of 40% in adults. It is generally believed that 10%–15% of the adult population suffers from chronic insomnia, and an additional 25%–35% have transient or occasional insomnia.1 The symptoms of insomnia may be difficult falling asleep, sleep latency more than 30 minutes, or sleep efficiency less than 85%, which usually happened more than 4 nights a week and occurred at least 3 weeks.2 Patients with insomnia may feel tired, tense, lazy, or have delayed reactions, distraction, or headache. The serious consequence of insomnia can be mental illness, and the worst mental illness is schizophrenia.
Insomnia can be treated with medications, herbal therapy, and psychologic or physical therapy. The commonly used medications include hypnotic sedative agents, such as zaleplon and benzodiazepines, but they may cause adverse effects such as damage of memory, drug resistance, dependency, and addiction.3 Nondrug therapy including acupuncture is commonly used by patients with insomnia. The mechanism of acupuncture treatment may be regulating yin and yang to reinforce health and eliminate the pathogenic, thus improving sleep.4 In modern medicine, acupuncture can increase the content of γ-amino butyric acid, and then enhance sleep quality.5 We performed this systematic review to evaluate the beneficial and harmful effects of acupuncture for treatment of insomnia in randomized trials.
Methods
Inclusion criteria
Parallel randomized controlled trials (RCTs) of acupuncture compared with no treatment, placebo, or basic medical therapy in patients with insomnia were included. Combined therapy of acupuncture and other interventions compared with other interventions in RCTs was also included. Outcome measures include duration and quality of sleep, such as total sleep duration and increased sleep duration, Pittsburgh Sleep Quality Index (PSQI) scores, Index of Severity of Insomnia, Sleep Quality, and other validated scores, as well as adverse effects. Multiple publications reporting the same groups of participants were excluded. There was no limitation on language and publication type.
Identification and selection of studies
We searched China Network Knowledge Infrastructure (1979–2008), Chinese Scientific Journal Database VIP (1989–2008), Wan Fang Database (1985–2008), PubMed (1966–2008), and the Cochrane Library (Issue 3, 2008). All of the searches ended at December 2008. The search terms included “acupuncture,” “acupressure,” “acupoint,” “electroacupuncture,” or “meridian” combined with “insomnia,” “sleepless,” or “dysomnia.” Two authors (H.J. Cao and H. Li) selected studies for eligibility and checked against the inclusion criteria independently.
Data extraction and quality assessment
Two authors (H.J. Cao and H. Li) extracted the data from the included trials independently. Quality of the included trials was evaluated according to the following categories6: Category A (good): studies have the least biases and their results are considered valid. These studies are likely to consist of (1) clear description of the population, setting, interventions, and comparison groups; (2) appropriate measurement of outcomes; (3) appropriate statistical and analytical methods; (4) no reporting errors; (5) less than 20% dropouts; (6) clear reporting of dropouts; and (7) appropriate consideration and adjustment for potential confounders. Category B (fair): studies are susceptible to some degrees of biases that are not sufficient to invalidate the results. These studies may have suboptimal adjustments for potential confounders and may also lack certain information that is needed to assess limitations and potential problems. Category C (poor): studies have significant biases that may invalidate the results. These studies either do not consider potential confounders or do not make adjustments for them appropriately. These studies may have critical flaw in design, analysis, and/or reporting, missing information, and/or discrepancies in reporting.
Data analysis
Data were summarized using relative risk (RR) with 95% confidence intervals (CI) for binary outcomes or mean difference (MD) with 95% CI for continuous outcomes. Revman5.0.17 software was used for data analyses. Meta-analysis was used if the trials had a good homogeneity on study design, participants, interventions, control, and outcome measures. Publication bias was explored by funnel plot analysis.
Results
Description of studies
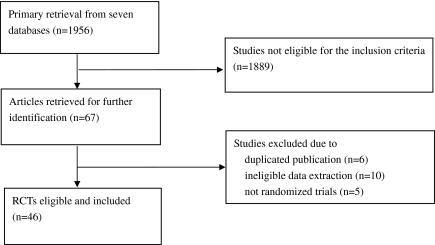
After primary searches from seven databases, 1956 citations were identified, and the majority were excluded due to obvious ineligibility, and full text papers of 67 studies were retrieved. Forty-six (46) RCTs were included in this review (Fig. 1),7–47 and among them, five trials were unpublished and were from graduate student dissertations.* There were 21 studies including 16 RCTs excluded from this review due to multiple publications, non-RCT design, data unavailable, or not meeting one of the inclusion criteria.48–68 The characteristics of included trials are listed in Table 1, and the reasons for excluded studies are listed in Table 2.
FIG. 1.
The process of study selection. RCTs, randomized controlled trials.
Table 1.
Characteristics of Included Studies
| |
Number of patients |
|
|
|
|
|
|
||
|---|---|---|---|---|---|---|---|---|---|
| Study | Treatment M/F | Control M/F | Age (mean or range) | Diagnostic criteria | Acupuncture (no. of points used) | Control group | Duration of treatment (day) | Outcome measure | |
| Chen M 19997 | 28 | 28 | 79 | Pittsburgh Sleep Quality Index (PSQI) | Real acupressure (5) 15 min per session, 5 sessions per week for 3 weeks | 1) Sham acupressure at nonacupressure points 15 min per session, 5 sessions per week for 3 weeks | 21 | PSQI | |
| 28 | 28 | Real acupressure (5) 15 min per session, 5 sessions per week for 3 weeks | 2) Conversation only | ||||||
| Chen X 20038 | 17/23 | 19/21 | 50 | Government guideline in China | Electroacupuncture (3 + x)a plus auricular acupuncture (8), 25 min, once daily; estazolam 2 mg once per night | Estazolam 2 mg once per night | 36 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to improvement of symptom | |
| Chen F 20079 | 18/22 | 17/23 | 18–64 | Unavailable | Electroacupuncture (2), 30 min, once daily | Diazepam 2.5 mg plus oryzanol 20 mg and VB1 20 mg 3 times a day | 14 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to sleeping efficacy | |
| Cui R 200110 | 34/26 | 28/32 | 27–67 | Government criteria in China | Body acupuncture (8) once daily plus estazolam 1–2 mg once per night | Estazolam 1–2 mg once per night | 30 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to sleeping efficacy | |
| Ding D 200811 | 13/19 | 11/13 | 20–71 | CCMD-2 | Body acupuncture (7 + x)a 30 min/3 hours once daily | Estazolam 1 mg once per night | 28 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to improvement of symptom | |
| Ding W 200612 | 44/40 | 16/16 | 13–75 | Unavailable | Body acupuncture (2 + x)a | Diazepam 5 mg 3 times a day | 7–14 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to improvement of symptom | |
| Du M 200713 | 12/22 | 7/13 | 20–82 | Unavailable | Body acupuncture (5 + x)a 30–60 min every 2 days plus herbal medicine twice a day | Herbal medicine 200 mL twice a day | 20 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to sleeping efficacy | |
| Fan D 200614 | 17/23 | 12/16 | 19–65 | CCMD-2 | Body acupuncture (5) 30 min once daily | Diazepam 5 mg once per night plus oryzanol 10 mg 3 times a day | 22 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to sleeping efficacy | |
| Hong Y 200515 | 30 | 30 | 22–76 | ICD-10/CCMD-3 | Electroacupuncture (2 + x)a 45 min once daily | Trazodone 50 mg–100 mg once per night | 28 | Self-rating Depression Scale (SDS) and Self-rating Anxiety Scale (SAS) AsbergRating Scale (ARS) | |
| Huang X 2000 | 40 | 36 | 18–65 | Government criteria in China | Body acupuncture (17 + x)a 30 min once daily | Estazolam 2 mg once per night | 21 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to sleeping efficacy; PSQI | |
| Huang L 200716 | 38/52 | 34/56 | Unavailable | ICD-10 | Rolling acupuncture 15–20 min once daily | Clonazepam 4–6 mg once per night | 28 | PSQI | |
| Jian J 200517 | 50 | 30 | 29–76 | Hollister | Body acupuncture (9)a 40 min once daily plus Ciwujia injection 60 mL once daily | Ciwujia injection 60 mL once daily | 25 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to sleeping efficacy | |
| Kang F 200618 | 36/42 | 14/16 | 18–61 | CCMD-3 | Body acupuncture (3 + x)a 30 min once daily plus auricular therapy (7) | Diazepam 5 mg once per night plus oryzanol 20 mg 3 times a day | 12 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to improvement of symptom | |
| Kim 200419 | 15 | 15 | 67 | Insomnia Severity Index (ISI) | Acupuncture (4) 2 days | Placebo (sham) acupuncture 2 days | 2 | MQ (morning questionnaire), ISI | |
| Kou J 2003 | 14/16 | 15/15 | 18–70 | CCMD-2 | Body acupuncture (17) 30 min once daily | Stilnox 10 mg once per night | 28 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to improvement of symptom | |
| Li Q 200520 | 10/16 | 9/15 | 31–80 | Unavailable | Electroacupuncture (3) 45 min every 2 days plus Prozac 20 mg once daily | Prozac 20 mg once daily | 28 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to improvement of symptom | |
| Li X 200721 | 53/80 | 21/27 | 17–65 | Government guideline in China | Body acupuncture (6 + x)a 30 min every 2 days plus auricular therapy (4 + x) | Estazolam 2 mg once per night | 20 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to sleeping efficacy | |
| Li T 200722 | 18/14 | 17/15 | 68 | Unavailable | Body acupuncture (7) 20–30 min once daily plus auricular therapy (1) | Diazepam 2.5 mg once per night or estazolam 1 mg once per night | 28 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to improvement of symptom | |
| Liu Y 200123 | 56 | 30 | 56–82 | Unavailable | Body acupuncture (4 + x)a 40 min once daily plus Ciwujia injection 60 mL once daily | Ciwujia injection 60 mL once daily | 25 | Significant as “cured,” “improved,” “ineffective” according to improvement of symptom | |
| Liu Q 200024 | 36 | 36 | 18–70 | Unavailable | Body acupuncture (4 + x)a once daily plus auricular therapy (4) | Estazolam 2 mg once per night | 32–51 | Significant as “markedly effective,” “improved,” “ineffective” according to improvement of symptom | |
| Liu J 200625 | 15/17 | 15/15 | 68 | Unavailable | Body acupuncture (8) 30 min once daily plus auricular therapy (1) | Diazepam 2.5 mg once per night or estazolam 1 mg once per night | 28 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to improvement of symptom | |
| Liu Z 200726 | 34/36 | 35/45 | 49 | CCMD-3 | Scalp acupuncture 6 hours once daily | Clonazepam 4 mg once per night | 28 | Significant as “cured,” “improved,” “ineffective” according to improvement of symptom | |
| Lu W 199827 | 14/21 | 10/13 | 16–60 | Government criteria in China | Body acupuncture (2) 30 min once daily plus Qiye Anshen tablet 100 mg 3 times a day | Qiye Anshen tablet 100 mg 3 times a day | 30 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to sleeping efficacy | |
| Luo L 2005 | 13/19 | 15/17 | 41 | CCMD-3 | Rolling acupuncture 10–15 min once daily/every 2 days plus clonazepam 2 mg once per night | Clonazepam 2 mg once per night | 28 | Significant as “cured,” “improved,” “ineffective” according to improvement of symptom; PSQI; Visual Analogue Scale (VAS) | |
| Luo W 2006 | 33 | 32 | 21–64 | CCMD-3 | Body acupuncture (8) 30 min once daily | Trazodone 50–150 mg once per night | 28 | PSQI; SDS; Asberg Rating Scale (ARS); Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to improvement of symptom | |
| Lv Y 200728 | 13/21 | 11/23 | 18–70 | ICD-10 | Electroacupuncture (10 + x)a 20 min once daily and auricular therapy (5) plus Suanzaoren decoction once daily | Suanzaoren decoction 300 mL once daily | 30 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to improvement of symptom | |
| Ma X 200629 | 4/26 | 5/25 | 17–75 | Unavailable | Body acupuncture (6 + x)a 30 min once daily plus alprazolam 0.4–0.8 mg once per night and antipsychotic drug | Alprazolam 0.4–0.8 mg plus antipsychotic drug | 21–32 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to improvement of symptom | |
| Ma Z 200630 | 11/20 | 16/15 | 17–72 | CCMD-3 | Electroacupuncture (5 + x)a 60 min once daily | Clonazepam 2 mg once per night plus oryzanol 20 mg 3 times a day | 30 | Sleep Dysfunction Rating Scale (SDRS); Self-rating Sleep Dysfunction Scale (SSDS); Hamilton Anxiety Scale (HAMA) | |
| Pan Q 200531 | 22/34 | 20/36 | 15–70 | CCMD-2 | Body acupuncture (more than 5) 30 min once daily | Estazolam 1 mg once per night | 36 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to improvement of symptom | |
| Qiu R 199932 | 53 | 36 | Unavailable | Unavailable | Acupressure once per night plus herbal medicine once daily | Estazolam 2 mg once per night plus herbal medicine once daily | 23 | Significant as “markedly effective,” “improved,” “ineffective” according to improvement of symptom | |
| Tang W 200733 | 16/24 | 18/22 | 47–84 | Unavailable | Auricular therapy (7) plus Tuina and acupressure | No treatment | 21 | Significant as “excellent,” “good,” “fair,” “ineffective” according to improvement of symptom | |
| Tian H 200634 | 39 | 39 | 35–70 | Government criteria in China | Body acupuncture (6)a 30 min once daily plus herbal medicine once daily | Herbal medicine once daily | 25 | Significant as “cured,” “improved,” “ineffective” according to improvement of symptom | |
| Tsay S 200335 | 35 | 31 | 55.52 | PSQI | Real acupressure (3) 14 min 3 days per week | Usual care | 28 | Medical Outcome Study–Short Form 36 (SF-36) | |
| 35 | 32 | Real acupressure (3) 14 min 3 days per week | Sham acupressure (3) 14 min 3 days per week | ||||||
| Tsay S 200436 | 35 | 35 | 58.16 | PSQI | Acupressure (4) 15 min 3 times a week | Usual care | 30 | Piper Fatigue Scale (PFS); PSQI; Beck Depression Inventory (BDI) | |
| 36 | 35 | Transcutaneous electrical acupoint stimulation | Usual care | ||||||
| Wang M 200337 | 22/38 | 19/36 | 16–70 | CCMD-2 | Body acupuncture (7) 30 min once daily | Diazepam 5 mg once per night | 22 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to improvement of symptom | |
| Wang Q 200338 | 17/23 | 17/23 | 19–65 | Unavailable | Electroacupuncture (4) 30 min once daily plus acupoint injection with Ciwujia injection (2) 4 mL once daily | Diazepam 2.5 mg 3 times a day plus oryzanol 20 mg 3 times a day and VB120 mg 3 times a day | 14 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to sleeping efficacy | |
| Wang X 200839 | 21 | 23 | 22–56 | CCMD-3 | Abdominal acupuncture (12) once daily for the first 3 days and once every 3 days for the remaining 11 days plus placebo pill once daily | Estazolam once daily plus sham acupuncture once daily for the first three days and once every three days for the remaining 11 days | 14 | Leeds Sleep Evaluation Questionnaire (LSEQ) | |
| Wang Y 200440 | 22/12 | 17/13 | 41–70.5 | Unavailable | Scalp acupuncture with electrical stimulation plus auricular therapy (1) and body acupuncture (5) 20–30 min 5 times a week | Diazepam 2.5 mg once per night plus clozapine 25 mg once per night | 28 | PSQI; Hamilton Rating Scale for Depression (HRSD) | |
| Xuan Y 200741 | 11/13 | 10/12 | 49 | ICD-10 | Body acupuncture (5) 30 min once daily | Estazolam 1 mg every two night | 30 | PSQI | |
| Ye T 200842 | 10 | 12 | 29–67 | Diagnostic and Statistical Manual of Mental Disorders 4th ed. (DSM-IV) | Abdominal acupuncture (12) 30 min once daily 5 times a week plus estazolam 2 mg once per night | Estazolam 2 mg once per night | 14 | PSQI | |
| Zhang H 200343 | 55/82 | 25/20 | 16–62 | CCMD-3/SRSS | Body acupuncture (8 + x)a 30–60 min once daily | Clonazepam 2 mg once per night | 28 | Self-Rating Sleep Scale (SRSS) | |
| Zhang X 200544 | 10/35 | 14/31 | 23–70 | Unavailable | Body acupuncture (3 + x)a 45 min once daily | Estazolam 2 mg once per night plus oryzanol 20 mg 3 times a day | 25 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to improvement of symptom | |
| Zhang Q 2006 | 18/20 | 20/17 | 18–64 | ICD-10/CCMD-3 | Body acupuncture (10 + x)a 1 hour once daily | Estazolam 2 mg once per night | 20 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to sleeping efficacy | |
| Zhong Z 200845 | 15/17 | 12/14 | 40 | CCMD-3 | Body acupuncture (7 + x)a 30 min once per night and massage of sole once daily plus alprazolam 0.4–0.8 mg once per night | Alprazolam 0.4–0.8 mg once per night | 40 | PSQI, SDS, SAS, significant as “cured,” “markedly effective,” “improved,” “ineffective” according to improvement of symptom | |
| Zhu Z 200446 | 50/0 | 50/0 | 18–47 | ICD-10 | Electroacupuncture (6) 20 min 3 times a week | No treatment | 40 | Scores evaluated by patients | |
| Zou Y 200847 | 28/32 | 30/28 | 18–68 | Government criteria in China | Electroacupuncture (8 + x)a 30 min once daily | Alprazolam 0.4 mg once per night | 20 | Significant as “cured,” “markedly effective,” “improved,” “ineffective” according to improvement of symptom | |
CCMD, Chinese Classification of Mental Disease; CCMD-2, second version of CCMD; CCMD-3, third version of CCMD; ICD-10, 10th version of International Classification of Disease.
The selection of the acupoints according to syndrome differentiation.
Table 2.
Excluded Studies with Reasons
| Study | Reason for exclusion |
|---|---|
| Chen Z 200248 | Randomized controlled trial but data were not available for analysis due to inadequate reporting |
| Chen Z 200249 | Randomized controlled trial that was a replicated publication of Chen Z 200253 |
| Chen X 200350 | Randomized controlled trial that was a replicated publication of Chen X 20038 |
| Chen H 200451 | Randomized controlled trial but data were not available for analysis due to inadequate reporting |
| Cui G 200052 | Randomized controlled trial but data were not available for analysis due to inadequate reporting |
| Cui R 200353 | Randomized controlled trial that was a replicated publication of Cui R 200310 |
| Dai M 200254 | Randomized controlled trial but data were not available for analysis due to inadequate reporting |
| Gao H 200155 | Randomized controlled trial but data were not available for analysis due to inadequate reporting |
| Hou C 200556 | Randomized controlled trial but data were not available for analysis due to inadequate reporting |
| Li Z 200657 | Quasi-randomized trial that did not meet the include criteria of this review |
| Luo L 200658 | Randomized controlled trial that was a replicated publication of Luo L 200530 |
| Sjoling M 200859 | Quasi-randomized trial that did not match the included criteria of this review |
| Su X 200560 | Randomized controlled trial but data were not available for analysis due to inadequate reporting |
| Tsay S 200361 | Randomized controlled trial that was a replicated publication of Tsay 200339 |
| Wang J 200462 | Randomized controlled trial but data were not available for analysis due to inadequate reporting |
| Wang J 200663 | Quasi-randomized trial that did not match the include criteria of this review |
| Wang C 199264 | Retrospective study that did not match the include criteria of this review |
| Huang L 200716 | Randomized controlled trial that was a replicated publication of Huang L 200716 |
| Weng M 200766 | Randomized controlled trial but data were not available for analysis due to inadequate reporting |
| Yang Z 200867 | Prospective cohort study that did not match the included criteria of this review |
| Zhu H 200268 | Randomized controlled trial but data were not available for analysis due to inadequate reporting |
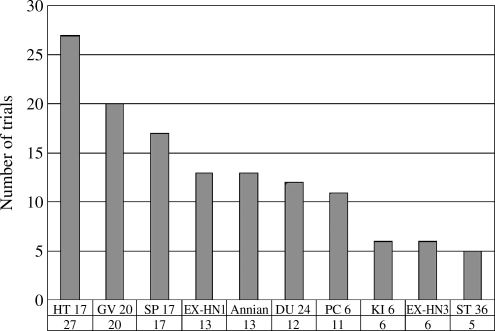
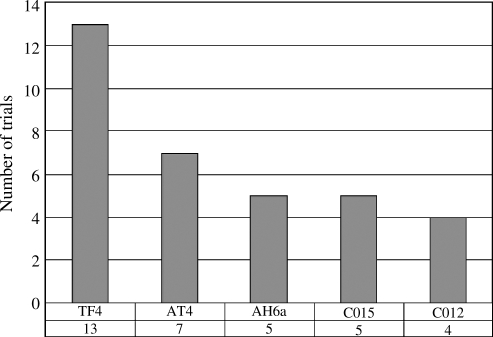
The 46 trials involved a total of 3811 patients with insomnia, of whom 2882 were patients with primary insomnia, 220 were insomnia patients with poststroke, 179 with depression, 60 in remittent stage with schizophrenia, 166 with cervical spondylosis, 100 with drug addiction, and 204 with end-stage renal disease. There was a wide variation in the age of subjects (13–85 years) and disease duration (10 days–40 years). Thirty-three (33) trials specified six diagnostic criteria, including four national criteria in China, one criterion from the United States, and one international classification of disease (ICD). The interventions included acupuncture (body, auricular acupuncture, electroacupuncture, acupressure, and acupoint injection), acupuncture plus conventional medication, or herbal medicine. The controls included no treatment, sham acupuncture, medication, or herbal medicine. The acupoints used were not fixed, the number of acupoints selected ranged from 2 to 20, and the total treatment duration ranged from 2 days to 10 weeks. The top 10 commonly used body acupoints and top 5 auricular acupoints are presented in Figures 2 and 3 Ten (10) of the 46 trials used the scores (PSQI) as the outcome measure and 12 kinds of scores were used for sleep measurement. Thirty-three (33) trials used four classes to evaluate treatment effects including cure, markedly effective, effective, and ineffective according to the degree of overall symptom improvement.
FIG. 2.
Top 10 points used for meridian acupuncture treatment.
FIG. 3.
Top five points for auricular acupuncture treatment.
Methodological quality
The majority of the included trials were assessed to be of generally fair methodological quality. According to our predefined quality assessment criteria, seven trials (15.22%) were evaluated as good (A), and the remaining as fair (B). The sample size varied from 22 to 182 participants, with an average of 35 patients in each group. Only 1 of the 46 trials40 reported sample size calculation that used Sample Power software, essential for ensuring adequate statistical power of 82%. Fourteen (14) trials described the randomization procedure, using random number table, drawing, or coin tossing. Three trials37,41 (Luo L 2005, unpublished data) used envelope as the method for allocation concealment. Eight trials7,27,35,39,42 (Huang X 2000; Kou J 2003; Zhang Q 2006, unpublished data) employed a blinding procedure: four of them used patient blinding, three used assessor blinding, and one trial provide no information on blinding. There was high potential to have bias caused by belief of the subjects and the measurers in the remaining 38 trials. Nine (9) of the 46 trials reported the number of dropouts7,15,17,27,35,36,41 (Kou J 2003; Luo L 2005, unpublished data), six trials7,8,16,35,36,40 (Huang X 2000, unpublished data) mentioned follow-up, and none of them used intention to treat method. The reporting quality of 46 trials according to Standards for Reporting Interventions in Controlled Trials of Acupuncture (STRICTA) varied among different trials (Table 3).
Table 3.
Reporting Quality of 46 Randomized Controlled Trials According to Standards for Reporting Interventions in Controlled Trials of Acupuncture (STRICTA)
| Intervention | Description of item | No. trials eligible to the principle | Percentage | |
|---|---|---|---|---|
| (1) Acupuncture rationale | 1 | 1a) Style of acupuncture | 46 | 100.00% |
| 1b) Rationale for treatment (e.g., syndrome patterns, segmental levels, trigger points) and individualization if used | 46 | 100.00% | ||
| 1c) Literature sources to justify rationale | 33 | 71.74% | ||
| (2) Needling details | 2 | 2a) Points used (uni/bilateral) | 46 | 100.00% |
| 2b) Numbers of needles inserted | 24 | 52.17% | ||
| 2c) Depths of insertion (e.g., cun or tissue level) | 21 | 45.65% | ||
| 2d) Responses elicited (e.g., de qi or twitch response) | 21 | 45.65% | ||
| 2e) Needle stimulation (e.g., manual or electrical) | 27 | 58.70% | ||
| 2f) Needle retention time | 46 | 100.00% | ||
| 2g) Needle type (gauge, length, and manufacturer or material) | 25 | 54.35% | ||
| (3) Treatment regimen | 3 | 3a) Number of treatment sessions | 46 | 100.00% |
| 3b) Frequency of treatment | 46 | 100.00% | ||
| (4) Co-interventions | 4 | 4a) Other interventions (e.g., moxibustion, cupping, herbs, exercises, lifestyle advice) | 46 | 100.00% |
| (5) Practitioner background | 5 | 5a) Duration of relevant training | 2 | 4.35% |
| 5b) Length of clinical experience | 2 | 4.35% | ||
| 5c) Expertise in specific condition | 3 | 6.52% | ||
| (6) Control intervention(s) | 6 | 6a) Intended effect of control intervention and its appropriateness to research question and, if appropriate, blinding of participants (e.g., active comparison, minimally active penetrating or nonpenetrating sham, inert) | 11 | 23.91% |
| 6b) Explanations given to patients of treatment and control interventions | 7 | 15.22% | ||
| 6c) Details of control intervention (precise description, as for item 2 above, and other items if different) | 12 | 26.09% | ||
| 6d) Sources that justify choice of control | 7 | 15.22% |
Effect estimates (Table 4)
Table 4.
Effect Estimates of Acupuncture Treatment in 46 Included Trials
| Study | Comparisons | Effect estimate (95% CI) | p value |
|---|---|---|---|
| Acupuncture/auricular/acupressure/TEAS versus no treatment | |||
| 1 No. patients with total sleeping time increased >3 hours | |||
| Tang W 200733 | Auricular therapy plus Tuina and acupressure versus no treatment | RR 1.81 (1.19, 2.77) | 0.006 |
| 2 Quality scores of sleeping evaluated by patients | |||
| Zhu Z 200446 | Electroacupuncture versus no treatment | MD −2.16 (−2.80, −1.52) | <0.0001 |
| 3 Total scores of PSQI | |||
| Chen M 19997 | Acupressure versus conversation | −6.32 (−7.47, −5.17) | |
| Tsay 200335 | Acupressure versus usual care | −3.78 (−5.98, −1.58) | |
| Tsay 200436 | Acupressure versus usual care | −1.20 (−3.91, 1.51) | |
| Tsay 200436 | Transcutaneous electrical acupoint stimulation versus usual care | −1.45 (−4.06, 1.16) | |
| Meta-analysis | MD −3.28 (−6.10, −0.46) | 0.02 | |
| Real acupuncture/acupressure versus sham acupuncture/acupressure | |||
| 1 Total scores of PSQI | |||
| Chen M 19997 | Real acupressure versus sham acupressure | −4.25 (−5.49, −3.01) | |
| Tsay 200335 | Real acupressure versus sham acupressure | −1.35 (−3.49, 0.79) | |
| Meta-analysis | MD −2.94 (−5.77, −0.11) | 0.04 | |
| 2 Total sleeping duration (hours) | |||
| Kim 200419 | Real acupuncture versus sham acupuncture | MD 74.00 (15.61, 132.39) | 0.01 |
| 3 Quality of sleeping (scores) | |||
| Kim 200419 | Real acupuncture versus sham acupuncture | MD 34.00 (19.30, 48.70) | <0.0001 |
| Acupuncture/auricular/acupressure versus Western medicine | |||
| 1 No. patients with total sleeping time increased >3 hours | |||
| Ding D 200811 | Body acupuncture versus estazolam | 1.01 (0.73, 1.42) | |
| Huang X 2000 | Body acupuncture versus estazolam | 1.50 (1.03, 2.18) | |
| Kang F 200518 | Body acupuncture plus auricular therapy versus diazepam and oryzanol | 3.91 (1.89, 8.08) | |
| Kou J 2003 | Body acupuncture versus stilnox | 1.80 (1.23, 2.62) | |
| Liu J 200625 | Body plus auricular acupuncture versus diazepam or estazolam | 2.25 (1.31, 3.88) | |
| Liu Z 200726 | Scalp acupuncture versus clonazepam | 0.97 (0.68, 1.39) | |
| Luo W 2006 | Body acupuncture versus trazodone | 1.55 (1.02, 2.37) | |
| Wang M 200337 | Body acupuncture versus diazepam | 1.64 (1.26, 2.15) | |
| Wang Y 200440 | Scalp with electrical stimulation plus body acupuncture and auricular therapy versus diazepam and clonzapine | 2.03 (1.16, 3.54) | |
| Zhang X 200544 | Body acupuncture versus estazolam plus oryzanol | 1.20 (0.94, 1.54) | |
| Meta-analysis | RR 1.53 (1.24, 1.88) | <0.0001 | |
| 2 No. patients with total sleeping time increased >2 hours | |||
| Liu Q 200024 | Body plus auricular acupuncture versus estazolam | 0.78 (0.46, 1.31) | |
| Qiu R 199932 | Acupressure plus herbal medicine versus estazolam plus herbal medicine | 0.79 (0.50, 1.26) | |
| Zou Y 200847 | Electroacupuncture versus alprazolam | 1.25 (1.08, 1.44) | |
| Meta-analysis | RR 0.95 (0.61, 1.50) | 0.84 | |
| 3 No. patients with total sleeping time >4 hours | |||
| Ding W 200612 | Body acupuncture versus diazepam | 1.58 (1.18, 2.12) | |
| Pan Q 200531 | Body acupuncture versus estazolam | 1.48 (1.17, 1.89) | |
| Meta-analysis | RR 1.53 (1.27, 1.84) | <0.00001 | |
| 4 Total scores of PSQI | |||
| Huang X 2000 | Body acupuncture versus estazolam | 1.50 (1.03, 2.18) | |
| Kou J 2003 | Body acupuncture versus stilnox | 1.80 (1.23, 2.62) | |
| Li T 200722 | Body plus auricular acupuncture versus diazepam or estazolam | −2.66 (−4.91, −0.41) | |
| Liu J 200625 | Body plus auricular acupuncture versus diazepam or estazolam | 2.25 (1.31, 3.88) | |
| Liu Z 200726 | Scalp acupuncture versus clonazepam | 0.97 (0.68, 1.39) | |
| Luo W 2006 | Body acupuncture versus trazodone | 1.55 (1.02, 2.37) | |
| Wang Y 200440 | Scalp with electrical stimulation plus body acupuncture and auricular therapy versus diazepam and clonzapine | −5.48 (−8.16, −2.80) | |
| Meta-analysis | MD −2.83 (−4.47, −1.19) | 0.0007 | |
| 5 Scores of sleep time evaluated by patients | |||
| Huang L 200716 | Rolling acupuncture versus clonazepam | −0.15 (−0.42, 0.12) | |
| Xuan Y 200741 | Body acupuncture versus estazolam | 0.32 (−0.24, 0.88) | |
| Meta-analysis | MD −0.06 (−0.30, 0.18) | 0.63 | |
| 6 No. patients with sleep rates >65% | |||
| Chen F 20079 | Electroacupuncture versus diazepam plus oryzanol and VitB1 | 1.36 (1.04, 1.79) | |
| Fan D 200614 | Body acupuncture versus diazepam plus oryzanol | 1.28 (0.91, 1.80) | |
| Li X 200721 | Body plus auricular acupuncture versus diazepam or estazolam | 1.33 (0.99, 1.78) | |
| Wang Q 200338 | Electroacupuncture plus acupoint injection versus diazepam plus oryzanol and VitB1 | 1.46 (1.10, 1.93) | |
| Zhang Q 2006 | Body acupuncture versus estazolam | 0.79 (0.45, 1.41) | |
| Meta-analysis | RR 1.28 (1.11, 1.48) | 0.001 | |
| 7 Total scores of SDS | |||
| Hong Y 200515 | Electroacupuncture versus trazodone | −0.06 (−5.91, 5.79) | |
| Luo W 2006 | Body acupuncture versus trazodone | −0.02 (−0.34, 0.30) | |
| Meta-analysis | MD −0.02 (−0.34, 0.30) | 0.9 | |
| 8 Total scores of SQ | |||
| Hong Y 200515 | Electroacupuncture versus trazodone | MD −19.01 (−21.65, −16.37) | <0.00001 |
| 9 Total scores of ASR | |||
| Hong Y 200515 | Electroacupuncture versus trazodone | −4.00 (−5.19, −2.81) | |
| Luo W 2006 | Body acupuncture versus trazodone | −2.16 (−3.58, −0.74) | |
| Meta-analysis | MD −3.12 (−4.92, −1.32) | 0.0007 | |
| 10 Total scores of LSEQ | |||
| Wang X 200839 | Abdominal acupuncture plus placebo pill versus estazolam plus sham acupuncture | MD −18.78 (−29.81, −7.76) | <0.01 |
| 11 Total scores of SRSS | |||
| Zhang H 200343 | Body acupuncture versus clonazepam | MD −3.00 (−4.41, −1.59) | <0.0001 |
| 12 Total scores of HAMA | |||
| Ma ZX 200630 | Electroacupuncture versus clonazepam | MD −1.55 (−4.25, 1.15) | 0.26 |
| Acupuncture/auricular plus Chinese medicine versus Chinese medicine | |||
| 1 No. patients with total sleeping time increased >3 hours | |||
| Lv Y 200728 | Electroacupuncture plus auricular acupuncture and Suanzaoren decoction versus Suanzaoren decoction | RR 1.30 (0.93, 1.82) | 0.13 |
| 2 No. patients with total sleeping time >4 hours | |||
| Tian H 200634 | Body acupuncture plus herbal medicine versus herbal medicine | RR 1.71 (1.26, 2.32) | 0.0005 |
| 3 Total sleeping duration (hour) | |||
| Lv Y 200728 | Electroacupuncture plus auricular therapy and Suanzaoren decoction versus Suanzaoren decoction | MD 1.25 (1.13, 1.37) | <0.00001 |
| 4 No. patients with sleep rates >60% | |||
| Du M 200713 | Body acupuncture plus herbal medicine versus herbal medicine | 1.41 (0.87, 2.30) | |
| Lu W 199827 | Body acupuncture plus Qiyeanshen tablet versus Qiyeanshen tablet | 2.07 (1.06, 4.03) | |
| Meta-analysis | RR 1.67 (1.12, 2.50) | 0.01 | |
| Acupuncture/auricular plus Western medicine versus Western medicine | |||
| 1 Total sleeping duration (hour) | |||
| Chen X 20038 | Body plus auricular acupuncture and estazolam versus estazolam | 1.01 (0.31, 1.71) | |
| Li Q 200520 | Electroacupuncture plus Prozac versus Prozac | 1.18 (0.40, 1.96) | |
| Meta-analysis | MD 1.09 (0.56, 1.61) | <0.0001 | |
| 2 Total scores of PSQI | |||
| Luo L 2005 | Rolling acupuncture plus clonazepam versus clonazepam | −1.00 (−4.00, 2.00) | |
| Ye T 200842 | Abdominal acupuncture plus estazolam versus estazolam | −2.08 (−3.77, −0.39) | |
| Zhong Z 200845 | Body acupuncture and massage of sole plus alprazolam versus alprazolam | −2.10 (−3.03, −1.17) | |
| Meta-analysis | −2.02 (−2.81, −1.24) | <0.00001 | |
| 3 No. patients with total sleeping time increased >3 hours | |||
| Chen X 20038 | Body plus auricular acupuncture and estazolam versus estazolam | 1.01 (0.31, 1.71) | |
| Li Q 200520 | Electroacupuncture plus Prozac versus Prozac | 1.28 (0.82, 2.00) | |
| Luo L 2005 | Rolling acupuncture plus clonazepam versus clonazepam | 1.18 (0.40, 1.96) | |
| Ma X 200629 | Body acupuncture plus alprazolam and antipsychotic drug versus alprazolam plus antipsychotic drug | 1.73 (1.18, 2.55) | |
| Meta-analysis | RR 1.33 (1.03, 1.71) | 0.03 | |
| 4 No. patients with total sleeping time increased >2 hours | |||
| Liu Y 200123 | Body acupuncture plus Ciwujia injection versus Ciwujia injection | RR 1.48 (1.06, 2.07) | 0.02 |
| 5 No. patients with sleep rates >55% | |||
| Jian J 200517 | Body acupuncture plus Ciwujia injection versus Ciwujia injection | RR 2.00 (1.47, 2.73) | <0.0001 |
| 6 No. patients with sleep rates increased >10% | |||
| Cui R 200110 | Body acupuncture plus estazolam versus estazolam | RR 1.79 (1.33, 2.39) | 0.0001 |
TEAS, transcutaneous electrical acupoint stimulation; CI, confidence interval; PSQI, Pittsburgh Sleep Quality Index; MD, mean difference; RR, relative risk; SDS, Self-rating Depression Scale; SQ, sleep quality; ARS, Asberg Rating Scale; LSEQ, Leeds Sleep Evaluation Questionnaire; SRSS, Self-Rating Sleep Scale; HAMA, Hamilton Anxiety Scale.
Acupuncture versus no treatment
Five (5) trials7,33,35,36,46 compared acupuncture with no treatment. Data from the no-treatment group was divided in half when compared with the other two interventional groups to avoid duplicated use in a three-arm trial40 in the meta-analysis. The result showed that acupressure was significantly better than no treatment on improving the total scores of PSQI (MD −3.28, 95% CI −6.10 to −0.46, p = 0.02).
Real acupuncture versus sham acupuncture
Three trials7,19,35 compared real versus sham acupuncture or acupressure, respectively. The result of meta-analysis showed that real acupuncture was more effective than sham acupuncture on improving total scores of PSQI (MD −2.94, 95% CI −5.77 to −0.11, p = 0.04).
Acupuncture versus Western medication
Twenty-six (26) trials compared acupuncture with Western medications. Most meta-analyses showed positive effect of acupuncture in treatment of insomnia, but one meta-analysis16,41 reported no difference between acupuncture and drugs on improving sleep duration evaluated by patients (MD −0.06, 95% CI −0.30 to 0.18, p = 0.63), one pooled results15 (Luo W 2006, unpublished data) showed no difference between acupuncture and trazodone on improving total scores of the Self-rating depression scale (SDS; MD −0.02, 95% CI −0.34 to 0.30, p = 0.90), and also another one trial30 reported no significant difference (MD −1.55, 95% CI −4.25 to 1.15, p = 0.26) between electroacupuncture and clonazepam on improving the scores of Hamilton Anxiety Scale.
Acupuncture plus other interventions versus other interventions
Seven trials compared acupuncture plus Western medications versus medications. Meta-analysis of two trials8,20 showed significant difference between acupuncture plus medications compared with the same medications on increasing the total sleep duration by hour (MD 1.09, 95% CI 0.56–1.61, p < 0.0001). Other results of meta-analysis were consistent that acupuncture plus medications had a much more therapeutic effect than medications alone.
Four trials13,27,28,34 compared acupuncture plus herbal medicine with herbal medicine. Only one trial28 showed there was no significant difference between the combination therapy and herbal group on increasing the numbers of patients whose total sleeping time increased for more than 3 hours (RR 1.30, 95% CI 0.93–1.82, p = 0.13). However, the meta-analyses showed a positive effect of acupuncture plus herbal medicine compared with herbal medicine on increasing the numbers of patients with sleep rates that increased by more than 60% (RR 1.67, 95% CI 1.12–2.50, p = 0.01).
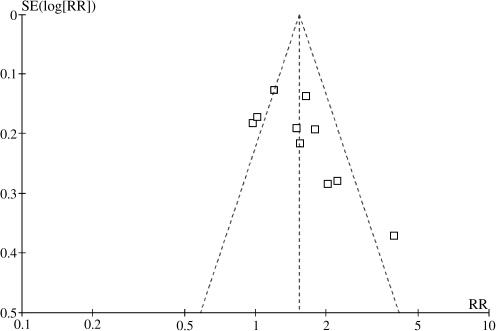
Meta-analysis of 10 trials showed a better effect of acupuncture than medications for the outcome of the number of patients whose total sleep duration increased for more than 3 hours (RR 1.53; 95% CI 1.24–1.88; p < 0.0001; 10 trials).
A funnel plot analysis of the 10 trials was generated, and it showed a significant asymmetry (Fig. 4).
FIG. 4.
Funnel plot of 10 randomized controlled trials for the outcome of number of patients with sleeping time increased over 3 hours. SE, standard error; RR, relative risk.
Adverse effect
Outcome of adverse effect with relation to acupuncture was described in 12 trials; only 3 of them reported minor adverse effect in the acupuncture group. Two (2) trials16 (Kou J, 2003, unpublished data) reported no adverse effect observed in the acupuncture group. Another trial15 reported mild headache (1 case), and lassitude (1 case) in the acupuncture group (n = 28), whereas there was dizziness (3 cases), constipation (3 cases), dry mouth (2 cases), palpitation (1 case), and oscitation (1 case) in the trazodone group (n = 27).
Two (2) trials15,28 evaluated the scores of the adverse effect rating scale. The result showed that acupuncture was safer than trazodone (MD −3.12, 95% CI −4.92 to −1.32, p = 0.0007).
Discussion
Based on the results of meta-analyses, the majority showed that compared with no treatment, sham acupuncture, or medications, acupuncture was significantly better on improving parameters in sleep quality and duration, and the combination of acupuncture and other interventions appears more effective than those interventions alone, though it was possible that the beneficial effect from acupuncture is overvalued because of the small sample size, flawed methodology of the included trials and the short follow-up duration.
There are several limitations in this review. First, the quality of the included studies is generally fair, which means the existence of moderate risk of bias. Because of inadequate reporting of randomization and blinding in the majority of trials, it was possible that there was performance bias and detection bias due to patients and researchers being aware of the therapeutic interventions for the subjective outcome measures. Intention-to-treat analysis was not applied in data analyses in the trials. The funnel plot asymmetry suggests the possibility of publication bias and small, low-quality trials. In addition, there is probably language bias because 43 of 46 included trials were published in Chinese, and 3 were published in English, but conducted in Taiwan and Korea. Vickers69 found that some Asian countries including China publish unusually high proportions of positive results, for which publication bias is a possible explanation. Second, 22 trials used Chinese diagnostic criteria of insomnia, 1 trial used U.S. criterion, and 6 trials used an ICD, but there were no specified diagnostic criteria for insomnia in the remaining trials. The participants are quite heterogeneous in terms of type of insomnia, such as in elderly with an average age of 81 years, or in heroin addicts with dyssomnia after detoxification. Third, there were different acupunctures used in the trials, which included acupuncture as a unique treatment in 18 trials, and acupuncture combined with other treatments in 28 trials. Twenty (20) trials selected the acupoints according to syndrome differentiation based on Chinese medicine theory, and 26 trials used fixed acupoints throughout the treatment. According to STRICTA, all of the 46 trials reported the style of acupuncture, rationale for treatment, points used, number of treatment sessions, frequency of treatment, and other interventions, but only about 50% of trials reported needling techniques such as the depth of insertion, responses elicited, needle stimulation and needle type, and less than 30% of trials mentioned the details of control intervention and practitioner's background. Controls were also heterogeneous in these trials, including Western medications, no treatment, sham acupuncture, acupressure, or herbal medicine. The treatment duration varied from 2 days to 10 weeks. Fourth, the use of composite outcome measures in 34 trials to evaluate overall improvement of symptoms limits the generalization of the findings. The classification of cure—markedly effective, effective, or ineffective—is not internationally recognized, and it is hard to interpret the effect. We suggest future trials to comply with international standards in the evaluation of treatment effect. Although there is no major statistical heterogeneity among the data analyses, we realized that the clinical heterogeneity would be very significant due to the variations in study quality, participants, intervention, control, and outcome measures. The interpretation of the positive findings from the meta-analyses needs to be incorporated with the clinical characteristics of the included trials and evidence strength. Therefore, the conclusion of the beneficial effect of acupuncture for insomnia needs to be confirmed in large and rigorously designed RCTs.
Our latest searches identified three systematic reviews of acupuncture for insomnia. One (1) Cochrane review published in 2007 included only 7 randomized trials published in English, and it concluded that current evidence was not sufficient to support the use of any form of acupuncture for the treatment of insomnia.70 Another systematic review published in Chinese in 2005 included only 6 Chinese trials with low quality, and had a similar conclusion.71 The most recent review published in 200972 included 12 clinical trials (including 3 randomized trials) and 18 case series. However, the authors were not able to access Chinese databases and quite a lot of studies published in Chinese were missed. This review by Huang and colleagues described the TCM diagnosis for insomnia and acupuncture treatment, which is considered relevant to clinical practice. We conducted comprehensive searches in both English and Chinese databases, and included 46 randomized trials. Our review suggests that acupuncture improves sleep quality and increases sleep duration. However, the beneficial findings of this systematic review still are not conclusive due to the limitations of the methodological quality of the included trials. Further rigorous trials are warranted.
Most of the existing trials are small and there is a moderate risk of bias. Further high-quality studies with larger sample size are needed to confirm the effectiveness of acupuncture in treating insomnia. Randomization methods need to be clearly described and fully reported. Although blinding of the acupuncturists might be very difficult, blinding of patients and outcome assessors should be attempted as far as possible to minimize performance and assessment biases. Analysis of outcomes based on intention-to-treat principle is important. Since insomnia is a highly heterogeneous disease with different etiology and severity, acupuncture is likely to have different effects on different subgroups of patients. Therefore, future clinical trials should be focused on particular subgroups or include a very large sample size to delineate the effect of acupuncture on different types of patients or different treatment techniques. In addition, well-defined diagnostic or classified criteria such as ICD-10 or the third version of Chinese Classification of Mental Disease should be employed to make a precise clinical diagnosis of insomnia, and hence increase the comparability between trials. Reporting of trials should follow the Consolidated Standards of Reporting Trials73 to explicitly explain the process of the treatment, so that the clinicians or other researchers can possibly use this process. Because the acupuncturist's technical competence may influence the therapeutic effect, we suggest that researchers describe the detailed treatment and that trials be conducted by qualified, well-trained acupuncturist in future studies according to STRICTA.74 Since insomnia may wax and wane with or without treatment, a longer follow-up period with serial measurement of outcomes is important to determine the effectiveness and long-term effect of acupuncture.
Footnotes
Huang XQ, Dong GR. Clinical study of acupuncture with combining Yin-Yang or Qi-Blood points on treatment of insomnia [in Chinese]. Dissertation for the master degree from Heilongjiang University of Traditional Chinese Medicine. 2000;
Kou JY, Sun YZ. Clinical observation of effect of acupuncture with Tiaozang Anshen method on Treatment of Insomnia [in Chinese]. Dissertation for the master degree from Heilongjiang University of Traditional Chinese Medicine. 2003;
Luo L, Yu SG. Effect of rolling acupuncture on treatment of insomnia [in Chinese]. Dissertation for the master degree from Chengdu University of Traditional Chinese Medicine. 2005;
Luo WZ, Lai XS. Clinical study of therapeutic effect of acupuncture with Jieyutiaoshen method on treatment of insomnia with depressive disorder [in Chinese]. Dissertation for the master degree from Guangzhou University of Traditional Chinese Medicine. 2006;
Zhang Q, Dong GR. Study of therapeutic effect of acupuncture with combining Yin-Yang or Qi-Blood points method on treatment of insomnia and its effect on polysomnography [in Chinese]. Dissertation for the master degree from Heilongjiang University of Traditional Chinese Medicine. 2006;
Acknowledgments
H.J. Cao and J.P. Liu were supported by a grant from the National Basic Research Program of China (“973” Program, no. 2006CB504602) and the 111 Project (B08006). J.P. Liu was supported in part by grant number R24 AT001293 from the National Center for Complementary and Alternative Medicine (NCCAM) of the U.S. National Institutes of Health. We also thank medical student Zhanguo Xie for his help in identifying articles for this review.
Disclosure Statement
No competing financial interests exist.
References
- 1.Doghramji K. The epidemiology and diagnosis of insomnia. Am J Managed Care. 2006;12:S214–S220. [PubMed] [Google Scholar]
- 2.Pei L. Insomnia [in Chinese] Chin Med Press Sci Technol. 2005;6:2–3. [Google Scholar]
- 3.Tang JL. Wang S. Clinical evidence [in Chinese] Peking Univ Med Press. 2008;1:778–780. [Google Scholar]
- 4.Wang QC. Therapeutics of acupuncture [in Chinese] China Press Traditional Chin Med. 2003;1:1–3. [Google Scholar]
- 5.Pi M. Du SH. Zhang Y. Study of therapeutic effect of acupuncture on insomnia and its effect on γ-amino butyric acid [in Chinese] J Jiangxi Coll Traditional Chin Med. 2000;12:160. [Google Scholar]
- 6.Agency for Healthcare Research Quality. www.Ahrq.gov/downloads/pub/evidence/pdf/brfout/brfout.pdf. [Dec 19;2008 ]. www.Ahrq.gov/downloads/pub/evidence/pdf/brfout/brfout.pdf
- 7.Chen ML. Lin LC. Wu SC. Lin JG. The effectiveness of acupressure in improving the quality of sleep of institutionalized residents [in Chinese] J Gerontol Ser A Biol Sci Med Sci. 1999;54:389–394. doi: 10.1093/gerona/54.8.m389. [DOI] [PubMed] [Google Scholar]
- 8.Chen XH. Clinical observation of therapeutic effect of acupuncture according to syndrome differentiation combined with medicine on treatment of asthenia insomnia [in Chinese] Guangxi J Chin Med. 2003;26:36–37. [Google Scholar]
- 9.Chen FK. Xu XH. Chen HL. Wang QQ. Clinical observation of effect of electroacupuncture combined frequency spectrum therapy on treatment of 40 patients of insomnia [in Chinese] J Clin Acup Moxibust. 2007;23:28. [Google Scholar]
- 10.Cui R. Zhou DA. Treatment of Phlegm-and Heat-induced insomnia by acupuncture in 120 cases [in Chinese] Beijing J Trad Chin Med. 2001;20:38–39. [PubMed] [Google Scholar]
- 11.Ding DG. Luo HP. Jiao Y. Clinical research of long-playing acupuncture on insomnia [in Chinese] J Clin Acup Med. 2008;24:10–11. [Google Scholar]
- 12.Ding WC. Observation of effect of acupuncture mainly on Shenmen and Sanyinjiao on treatment of 84 cases of insomnia [in Chinese] Jilin J Traditional Chin Med. 2006;26:46. [Google Scholar]
- 13.Du MX. Effect of acupuncture and medicine on treatment of insomnia: 34 cases clinical observation [in Chinese] J Pract Traditional Chin Med. 2007;23:18–19. [Google Scholar]
- 14.Fan D. Sun BY. Zhao X. Wang FC. Clinical observation of acupuncture with tranquilizing and allaying excitement method on treatment of 40 cases of insomnia [in Chinese] J Changchun Univ Traditional Chin Med. 2006;22:28. [Google Scholar]
- 15.Hong YB. Zhu W. Yao WH. Clinical therapeutic controlled study of electroacupuncture combined medicine on treatment of insomnia [in Chinese] Bull Med Res. 2005;34:72–74. [Google Scholar]
- 16.Huang LS. Wang DL. Wang CW, et al. Clinical study on rolling needle therapy for treatment of cases of nonorganic chronic insomnia [in Chinese] J Traditional Chin Med. 2007;48:331–334. [Google Scholar]
- 17.Jian J. Liu J. 50 cases observation on effect of acupuncture combined medicine on treatment of refractoriness insomnia [in Chinese] Henan Traditional Chin Med. 2005;25:62–63. [Google Scholar]
- 18.Kang FH. 78 cases clinical observation of effect of auricular therapy combined acupuncture on treatment of insomnia [in Chinese] J Tianjin Univ Traditional Chin Med. 2005;24:89–90. [Google Scholar]
- 19.Kim YS. Lee SH. Jung WS, et al. Intradermal acupuncture on Shenmen and Neiguan acupoints in patients with insomnia after stroke. Am J Chin Med. 2004;32:771–778. doi: 10.1142/S0192415X04002399. [DOI] [PubMed] [Google Scholar]
- 20.Li QY. Dong YF. 26 cases observation on electroacupuncture and Western medicine combined on treatment of dyssomnia of depression [in Chinese] Chin J Information TCM. 2005;12:71–72. [Google Scholar]
- 21.Li XJ. Bi LP. Differentiation of syndromes and use acupuncture combined auricular therapy on treatment of insomnia: 133 cases clinical observation [in Chinese] Lishizhen Med Materia Med Res. 2007;18:6678. [Google Scholar]
- 22.Li TB. Effect of acupuncture on post stroke insomnia [in Chinese] Chin J Rehabil Theory Pract. 2007;13:656–657. [Google Scholar]
- 23.Liu Y. Jiang ZQ. Acupuncture combined Ciwujia injection in treatment of senile insomnia [in Chinese] Pract J Rural Doctor. 2001;8:26. [Google Scholar]
- 24.Liu Q. Acupuncture and auricular therapy for 36 cases insomnia [in Chinese] Jilin J Traditional Chin Med. 2000;20:63. [Google Scholar]
- 25.Liu JH. Huang XH. Chen XH. 32 cases clinical observation of effect of acupuncture on treatment of post stroke insomnia [in Chinese] Int Med Health Guidance News. 2006;12:107–108. [Google Scholar]
- 26.Liu ZB. Niu WM. Observation of effect of acupuncture in area of hair line and scalp on treatment of 160 patients of insomnia [in Chinese] Shanxi J Chin Med. 2007;28:716–717. [Google Scholar]
- 27.Lu WW. Effect of acupuncture on Neiguan and Chinese medicine named Qiyeanshen Tablet used on treatment of insomnia: 35 cases clinical observation [in Chinese] J Nanjing Univ TCM. 1998;14:164. [Google Scholar]
- 28.Lv YE. Effect observation of acupuncture combined with TCM therapy on 68 cases of insomnia [in Chinese] World J Integrated Traditional West Med. 2007;2:355–356. [Google Scholar]
- 29.Ma X. Effect of acupuncture combined with Western medicine on treatment of dyssomnia of patients of paracme of schizophrenia [in Chinese] Henan Traditional Chin Med. 2006;26:57–58. [Google Scholar]
- 30.Ma ZX. Li GH. Duan HM. 31 cases clinical observation of effect of acupuncture on insomnia [in Chinese] J Traditional Chin Med. 2006;21:25–26. [Google Scholar]
- 31.Pan QL. Zhang LM. Yang JY. He YL. Results in treatment of obstinate insomnia by acupuncture [in Chinese] China Trop Med. 2005;5:1641. , 1705. [Google Scholar]
- 32.Qiu RJ. Zheng CM. Lun ZX, et al. Observation of effect of a kind of massage on treatment of 53 patients of insomnia [in Chinese] New J Traditional Chin Med. 1999;31:23. [Google Scholar]
- 33.Tang WH. Clinical observation of auricular therapy and head's massage on treatment of patients with insomnia [in Chinese] Hunan J Traditional Chin Med. 2007;23:75–76. [Google Scholar]
- 34.Tian HZ. Li JQ. Clinical observation of acupuncture combined with medicine on treatment of insomnia [in Chinese] Chin Arch Traditional Chin Med. 2006;24:1146–1147. [Google Scholar]
- 35.Tsay SL. Rong JR. Lin PF. Acupoints massage in improving the quality of sleep and quality of life in patients with end-stage renal disease. J Adv Nurs. 2003;42:134–142. doi: 10.1046/j.1365-2648.2003.02596.x. [DOI] [PubMed] [Google Scholar]
- 36.Tsay SL. Cho YC. Chen ML. Acupressure and transcutaneous electrical acupoint stimulation in improving fatigue, sleep quality and depression in hemodialysis patients. Am J Chin Med. 2004;32:407–416. doi: 10.1142/S0192415X04002065. [DOI] [PubMed] [Google Scholar]
- 37.Wang MZ. Wei Y. 115 cases clinical observation of effect of Jiannao Anshen Granule of acupuncture therapy on treatment of insomnia [in Chinese] J Clin Acup Moxibust. 2003;19:32–33. [Google Scholar]
- 38.Wang QQ. Chen HL. Observations on the curative effect of combined acupoint injection and electroacupuncture on 40 insomnia cases [in Chinese] Shanghai J Acup Moxibust. 2003;22:27–28. [Google Scholar]
- 39.Wang XY. Yuan SH. Yang HY, et al. Abdominal acupuncture for insomnia in women: A randomized controlled clinical trial [in Chinese] Acup Electrother Res. 2008;33:33–41. doi: 10.3727/036012908803861203. [DOI] [PubMed] [Google Scholar]
- 40.Wang Y. Zhao ZF. Wu Y, et al. Clinical therapeutic effect of acupuncture on post stroke depression with insomnia [in Chinese] Chin Acup Moxibust. 2004;24:603–606. [Google Scholar]
- 41.Xuan YB. Guo J. Wang LP. Wu X. Randomized and controlled study on effect of acupuncture on sleep quality in the patient of primary insomnia [in Chinese] Chin Acup Moxibust. 2007;27:886–888. [PubMed] [Google Scholar]
- 42.Ye TS. Wang QJ. Xie WX, et al. A randomized control study of abdominal acupuncture treatment for primary insomnia [in Chinese] Shanghai J Acup Moxibust. 2008;27:3–5. [Google Scholar]
- 43.Zhang H. Deng H. Xiong K. Acupuncture regulating Yinqiao meridians for treatment of 87 cases of insomnia [in Chinese] Chin Acup Moxibust. 2003;23:392–396. [Google Scholar]
- 44.Zhang XY. Effect of acupuncture on 45 cases insomnia. J Clin Acup Moxibust [in Chinese]. 2005;21:24. [Google Scholar]
- 45.Zhong ZG. Cai H. Li XL. Lv D. Effect of acupuncture combined with massage of sole on sleeping quality of the patient with insomnia [in Chinese] Chin Acup Moxibust. 2008;28:411–413. [PubMed] [Google Scholar]
- 46.Zhu ZC. Mu JP. Liang Y, et al. Clinical observation on treatment of dyssomnia of heroin addicts after detoxification by electro-acupuncture [in Chinese] Shanghai J Acup Moxibust. 2004;24:6–8. [Google Scholar]
- 47.Zou Y. Clinical observation of electroacupuncture with Anshen Dingzhi method on psychogenic insomnia [in Chinese] Heilongjiang J Traditional Chin Med. 2008;37:40–41. [Google Scholar]
- 48.Chen ZW. Chen XH. Clinical observation of effect of Sishenzhen combined auricular therapy on treatment of insomnia [in Chinese] Hubei J Traditional Chin Med. 2002;24:45. [Google Scholar]
- 49.Chen ZW. Chen XH. Clinical observation of effect of Sishenzhen combined with auricular therapy on treatment of insomnia [in Chinese] Fujian J Traditional Chin Med. 2002;33:19. [Google Scholar]
- 50.Chen XH. Observations on the curative effect of combined acupuncture and medicine on insomnia [in Chinese] Shanghai J Acup Moxibust. 2003;22:30–31. [Google Scholar]
- 51.Chen HW. Cao DF. Tang YC. Clinical observations on the treatment of insomnia by a Yang-reducing and Yin-reinforcing method [in Chinese] Shanghai J Acup Moxibust. 2004;23:14–15. [Google Scholar]
- 52.Cui GM. Zhang S. Liu JX. Shao HL. 42 cases observation of therapeutic effect of electroacupuncture on treatment of insomnia [in Chinese] Gansu J Traditional Chin Med. 2000;13:52–53. [Google Scholar]
- 53.Cui R. Zhou D. Treatment of phlegm-and heat-induced insomnia by acupuncture in 120 cases. J Traditional Chin Med. 2003;23:57–58. [PubMed] [Google Scholar]
- 54.Dai M. 80 cases clinical observation of effect of acupuncture on treatment of insomnia [in Chinese] Hebei J Traditional Chin Med. 2002;24:838. [Google Scholar]
- 55.Gao H. Clinical observation of effect of acupuncture with therapy of purging heart fire to nourish renal water and restoring normal coordination between heart and kidney on treatment of 60 patients of insomnia [in Chinese] Res Traditional Chin Med. 2001;17:16. [Google Scholar]
- 56.Hou CY. Liu Q. 150 clinical observation of effect of acupuncture on treatment of insomnia [in Chinese] New J Traditional Chin Med. 2005;37:61–62. [Google Scholar]
- 57.Li ZP. Clinical observation of therapeutic effect of acupuncture on Baihui and Shenting for treatment of 110 cases of insomnia [in Chinese] J Clin Acup Moxibust. 2006;22:38–39. [Google Scholar]
- 58.Luo L. Hu YP. Yu SG. Li N. Observation on therapeutic effect of rolling needle therapy on insomnia [in Chinese] Chin Acup Moxibust. 2006;26:183–185. [PubMed] [Google Scholar]
- 59.Sjoling M. Rolleri M. Englund E. Auricular acupuncture versus sham acupuncture in the treatment of women who have insomnia. J Altern Complement Med. 2008;14:39–46. doi: 10.1089/acm.2007.0544. [DOI] [PubMed] [Google Scholar]
- 60.Su X. Wu ZQ. 90 cases clinical observation of effect of acupuncture on treatment of cervical insomnia [in Chinese] New J Traditional Chin Med. 2005;37:52–53. [Google Scholar]
- 61.Tsay SL. Chen ML. Acupressure and quality of sleep in patients with end-stage renal disease: A randomized controlled trial. Int J Nurs Studies. 2003;40:1–7. doi: 10.1016/s0020-7489(02)00019-6. [DOI] [PubMed] [Google Scholar]
- 62.Wang JL. Shi GQ. Chang QY. Observations on effect of combined acupuncture, auricular therapy and massage on treatment of 120 patients of insomnia [in Chinese] J Sichuan Traditional Chin Med. 2004;22:90–91. [Google Scholar]
- 63.Wang J. Jiang JF. Wang LL. Clinical observation on Governor Vessel Daoqi method for treatment of dyssomnia in the patient of depression [in Chinese] Chin Acup Moxibust. 2006;26:328–330. [PubMed] [Google Scholar]
- 64.Wang CH. 70 cases observation of therapeutic effect of acupuncture on treatment of insomnia [in Chinese] Shanghai J Acup Moxibust. 1992;12:18–19. [Google Scholar]
- 65.Wang CW. Kang J. Zhou JW, et al. Effect of rolling needle therapy on quality of life in the patient of non-organic chronic insomnia: A randomized controlled trial [in Chinese] Chin Acup Moxibust. 2006;26:461–465. [PubMed] [Google Scholar]
- 66.Weng M. Liao HQ. Effect of electroacupuncture on treatment of senile insomnia: Analysis of scale [in Chinese] J Clin Acup Moxibust. 2007;23:33–34. [Google Scholar]
- 67.Yang ZW. Clinical observation on therapeutic effect of acupuncture on insomnia [in Chinese] Shanghai J Acup Moxibust. 2008;27:6–8. [Google Scholar]
- 68.Zhu HQ. Effect of balance of Yinqiao and Yangqiao meridian acupuncture on obstinate insomnia [in Chinese] J Traditional Chin Med Lit. 2002;2:55–56. [Google Scholar]
- 69.Vickers A. Goyal N. Harland R. Rees R. Do certain countries produce only positive results? A systematic review of controlled trials. Controlled Clin Trials. 1998;19:159–166. doi: 10.1016/s0197-2456(97)00150-5. [DOI] [PubMed] [Google Scholar]
- 70.Cheuk DKL. Yeung WF. Chung KF. Wong V. Acupuncture for insomnia. Cochrane Database Syst Rev. 2007;18:CD005472. doi: 10.1002/14651858.CD005472.pub2. [DOI] [PubMed] [Google Scholar]
- 71.Li N. Wu B. Wang CW, et al. A systematic evaluation of randomized controlled trials for acupuncture and moxibustion treatment of insomnia [in Chinese] Chin Acup Moxibust. 2005;25:7–10. [PubMed] [Google Scholar]
- 72.Huang W. Kutner N. Bliwise DL. A systematic review of the effects of acupuncture in treating insomnia. Sleep Med Rev. 2009;13:73–104. doi: 10.1016/j.smrv.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 73.CONSORT Statement 2001—Checklist: Items to Include When Reporting a Randomized Trial. www.consort-statement.org. [Dec 19;2008 ]. www.consort-statement.org
- 74.Checklist of STRICTA Items to Reporting Interventions in Controlled Trials of Acupuncture. www.stricta.info/checklist.htm. [Dec 19;2008 ]. www.stricta.info/checklist.htm