Abstract
Background
The Lateral Septal Area (LSA) is involved with autonomic and behavior responses associated to stress. In rats, acute restraint (RS) is an unavoidable stress situation that causes autonomic (body temperature, mean arterial pressure (MAP) and heart rate (HR) increases) and behavioral (increased anxiety-like behavior) changes in rats. The LSA is one of several brain regions that have been involved in stress responses. The aim of the present study was to investigate if the neurotransmission blockade in the LSA would interfere in the autonomic and behavioral changes induced by RS.
Methodology/Principal Findings
Male Wistar rats with bilateral cannulae aimed at the LSA, an intra-abdominal datalogger (for recording internal body temperature), and an implanted catheter into the femoral artery (for recording and cardiovascular parameters) were used. They received bilateral microinjections of the non-selective synapse blocker cobalt chloride (CoCl2, 1 mM/ 100 nL) or vehicle 10 min before RS session. The tail temperature was measured by an infrared thermal imager during the session. Twenty-four h after the RS session the rats were tested in the elevated plus maze (EPM).
Conclusions/Significance
Inhibition of LSA neurotransmission reduced the MAP and HR increases observed during RS. However, no changes were observed in the decrease in skin temperature and increase in internal body temperature observed during this period. Also, LSA inhibition did not change the anxiogenic effect induced by RS observed 24 h later in the EPM. The present results suggest that LSA neurotransmission is involved in the cardiovascular but not the temperature and behavioral changes induced by restraint stress.
Introduction
Stress situations are well-known to trigger autonomic and behavior responses that are accompanied by activation of several brain structures [1]. Among these structures, the lateral septal area (LSA) has been proposed as an integrative center for autonomic, neuroendocrine and behavioral responses [2], [3], [4]. The LSA projects into several brain regions involved in the modulation of autonomic and behavioral stress responses [4], [5], [6], [7], [8], [9]. The latter includes fear and anxiety responses and learning and memory interference [3], [4], [10], [11], [12], [13], [14], [15].
Acute restraint is an uncontrollable stress situation which produces several emotional and autonomic responses. The autonomic responses includes mean arterial pressure (MAP) and heart rate (HR) increases [7], [16], [17], [18], [19], [20], skeletal muscle vasodilatation and cutaneous vasoconstriction, which are accompanied by a rapid skin temperature drop and followed by body temperature increases [21], [22]. In addition to those autonomic responses, animals submitted to restraint also present behavioral changes such as reduced exploratory activity in an open field [23], [24], [25], increased immobility in a forced swimming test [26] and reduced exploration of the open arms of an elevated plus-maze (EPM) 24 h after the stress session [27], [28]. Therefore, it is possible evaluated the consequences of this stress model acutely by autonomic responses during restraint session and later, 24 h after the restraint session, by anxiogenic like effect in EPM.
Several studies have shown that the LSA is activated during aversive situations, including restraint stress [19], [29], [30], [31], [32]. Rats submitted to restraint stress exhibit increased c-Fos protein expression in LSA when compared with control animals [19]. In the same study, the authors reported that restraint stress caused an increase in blood pressure which was inhibited by the GABA A receptor agonist, muscimol, injected into the LSA. However, no changes on HR, body temperature and behavioral consequences evoked by restraint stress were described by LSA inhibition. Finally, anxiolytic-like effect induced by systemic administration of diazepam in rats submitted to fear conditioning model is associated with a decrease in LSA neuronal activity [29]. Taken together, these data support a possible regulatory role of the LSA on behavioral and autonomic responses associated with aversive situations such as the restraint stress.
Therefore, the aim of the present study was to investigate the involvement of the LSA in the autonomic and behavior responses induced by acute restraint stress.
Materials and Methods
Animals
Male Wistar rats weighing 230–250 g were used. The animals were kept in the animal care unit of the Department of Pharmacology, School of Medicine of Ribeirão Preto, University of São Paulo. The rats were housed individually in plastic cages with free access to food and water under a 12 h light/dark cycle (lights on at 06.30 h). The institution's Animal Ethics Committee approved the housing conditions and experimental protocols (protocol n. 150/2007).
Surgery procedure
Seven days before the experiment, the rats were anesthetized with 2,2,2-tribromoethanol (Sigma, St Louis, Missouri, USA) (250 g/kg, intraperitoneally). After scalp anesthesia with 2% lidocaine, the skull was surgically exposed and stainless steel guide cannulae (0.55 mm) were implanted bilaterally into the LSA using a stereotaxic apparatus (Stoelting, Wood Dale, Illinois, USA) as described by [3]. During the surgical procedure an intra-abdominal datalogger (SubCue dataloggers, Calgary, Alberta, Canada) was also implanted to record internal body temperature. The rats were allowed to recover from the surgery during a period of seven days. Twenty-four h before the restraint stress (RS) session, the rats had a catheter (4 cm PE-10 segment heat-bound to a 13 cm PE-50 segment, Clay Adams, Parsippany, NJ, USA) inserted into the abdominal aorta through the femoral artery for blood pressure recording as described by Resstel et al. (2008). After each surgery, animals were treated with a polyantibiotic preparation of streptomycins and penicillins i.m. (Pentabiotico®, Fort Dodge, Brazil) to prevent infection and with the nonsteroidal anti-inflammatory flunixine meglumine (2.5 mg kg−1 s.c.; banamine®, Schering Plough, Brazil) for post-operative analgesia.
Acute restraint
In the morning period (07:00–12:00 hr), the animals were transported to the experimental room in their home cages and allowed to adapt to this environment for at least 30 min. Mean arterial pressure (MAP) and heart rate (HR) were recorded with a HP-7754A amplifier (Hewlett Packard, Palo Alto, CA) connected to a signal acquisition board (Biopac M-100, Goleta, CA) for computer processing. After 15 min of baseline recording, rats received bilateral microinjection into the LSA of 100 nL of vehicle (sterile artificial cerebrospinal fluid (aCSF - composition: NaCl 100 mM; Na3PO4 2 mM; KCl 2.5 mM; MgCl2 1 mM; NaHCO3 27 mM; CaCl2 2.5 mM; pH = 7.4) or 1 mM/100 nL of CoCl2 (Sigma, St Louis, Missouri, USA) [3]. A 0.3 mm needle (Small Parts, Miami Lakes, Florida, USA), 1 mm longer than the guide cannula, connected to a 2 µL syringe (7001 KH; Hamilton Co., Nevada, USA) through a PE-10 tubing, was used for this purpose. The needles were carefully inserted into the guide cannulae and the solutions were infused over a 15 s period. They remained in place for an additional 30 s period to prevent reflux. Ten minutes later, the animals were submitted to a 60-min restraint period in a plastic cylindrical restraining tube (diameter 6.5 cm and length 15 cm). After restraint, the animals returned to their cages. Each animal was submitted to only one restraint session.
Temperature measurements
Besides the cardiovascular parameters, variations in cutaneous temperature (CT) were recorded with the thermal camera Multi-Purpose Thermal Imager IRI 4010 (InfraRed Integrated Systems Ltd Park Circle, Tithe Barn Way Swan Valley Northampton, USA) at a distance of 50 cm. Internal temperature (IT) was recorded by the datalogger (SubCue dataloggers, Calgary, Alberta, Canada) implanted into the abdomen as described above.
Elevated plus maze (EPM)
The EPM test was conducted as described before [28]. Briefly, the apparatus consisted of two opposite open arms (50×10 cm) crossed at a right angle by two arms of the same dimensions enclosed by 40 cm high walls with no roof. The maze was located 50 cm above the floor. Rodents naturally avoid the open arms of the EPM and anxiolytic compounds typically increase the exploration of these arms without changing the number of enclosed-arm entries [33], [34]. The AnyMazeTM software (version 4.7, Stoelting) was employed for behavioral analysis. It detects the position of the animal in the maze and calculates the number of entries and time spent in open and enclosed arms.
Histological procedure
At the end of the experiments rats were anesthetized with urethane (1.25 g/kg, i.p.) and 100 nL of 1% Evan's blue dye was bilaterally injected into the LSA to stain the injection sites. The chest was surgically opened, the descending aorta occluded, the right atrium severed and the brain perfused with 10% formalin through the left ventricle. Brains were postfixed for 24 h at 4°C, and 40 µm sections were cut using a cryostat (CM-1900, Leica, Germany). Sections were stained with 1% neutral blue and injection sites were identified.
Data Analysis
All autonomic responses were continuously recorded for 15 min before and during the 60-min of restraint stress period. Data were expressed as means ± SEM changes (respectively MAP, HR, CT or IT) and were sampled at 2 min intervals as a mean of the changes during each 2 min. Points sampled during the 10 min before restraint were used as control baseline value. The autonomic values changes during restraint were analyzed using two-way ANOVA with treatment as independent factor and time as repeated measurement factor. The basal values changes were analyzed before and after vehicle or CoCl2 administration by Student's t Test.
The percentage of entries (100×open/total entries) and time spent in the open arms (100×open/open+enclosed) of the EPM were calculated for each rat. These data, together with the number of enclosed arm entries, were analyzed by one-way ANOVA followed by Bonferroni's post hoc test. Values of P<0.05 were taken as showing statistically significant differences between means.
Results
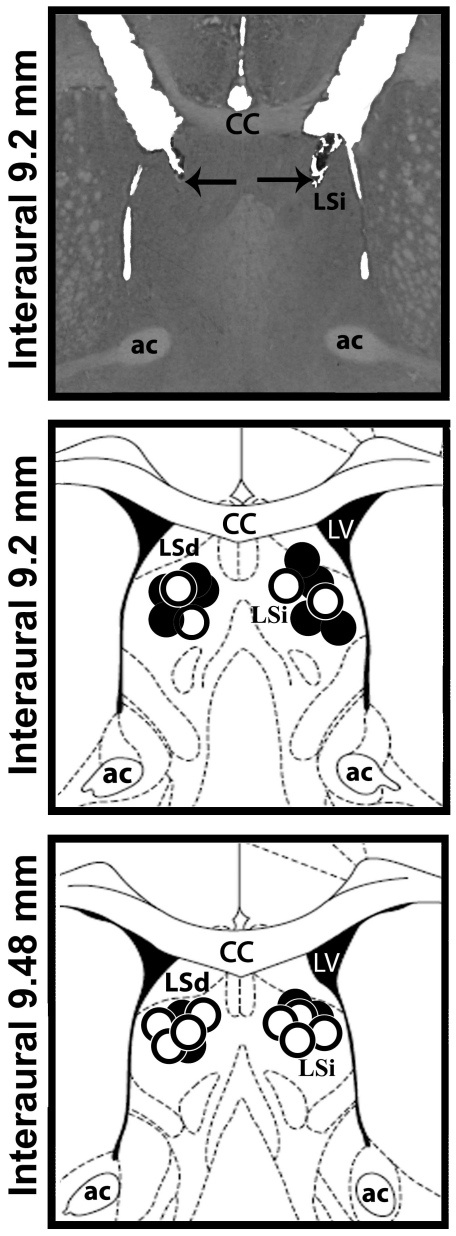
A representative photomicrograph and a diagrammatic representation indicating the injection sites in the LSA can be seen in Figure 1.
Figure 1. Anatomical sites of lateral septal area microinjections.
A photomicrograph of a coronal brain section showing bilateral microinjections sites in the lateral septal area (LSA) and a diagrammatic representation based on the rat brain atlas of Paxinos and Watson (1997) indicating injections sites of vehicle (open circle) or CoCl2 (closed circle) into the LSA. cc- corpus callosum; LV- lateral ventricle; ac – anterior commissure; LSi - lateral septal area, intermediate part; LSd - lateral septal area, dorsal part.
Effects of LSA inhibition on autonomic responses to acute restraint
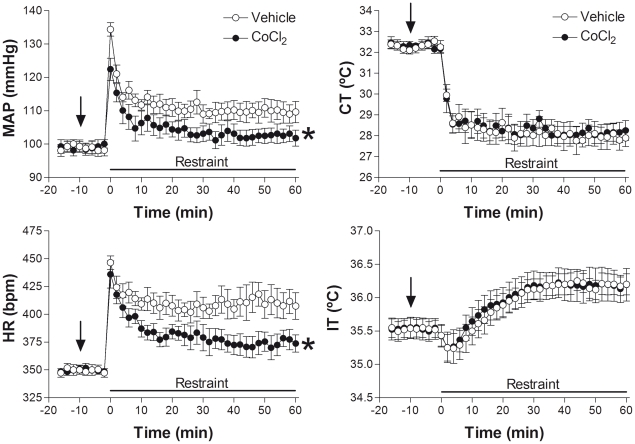
The microinjection of CoCl2 into the LSA (n = 6) did not affect baseline values of either MAP (t = 0.32, P>0.05), HR (t = 1.85, P>0.05), CT (t = 0.45, P>0.05) or IT (t = 1.23, P>0.05). Acute restraint caused significant increases in MAP (F35,360 = 8.93, P<0.001), HR (F35,360 = 8.86, P<0.001) and IT (F35,360 = 5.86, P<0.001) and a significant and long-lasting decrease of CT (F35,360 = 20.11, P<0.001). The injection of CoCl2 into the LSA significantly attenuated the increases in both (MAP: F1,360 = 93, P<0.001) and (HR: F1,360 = 126, P<0.001, Figure 2) observed during restraint. However, no changes were observed in RS induced decrease of CT (F1,360 = 0.76, P>0.05) and increase of IT (F1,360 = 0.41, P>0.05, Figure 2). A representative infrared image of CT can be seen in Figure 3.
Figure 2. Autonomic responses during restraint stress.
Time-course of bilateral microinjection of 100 nL of vehicle (n = 6) or 1 mM of CoCl2 (n = 6) on changes in mean arterial pressure (MAP), heart rate (HR), cutaneous temperature (CT) and internal temperature (IT) of animals submitted to 60 min of restraint stress. Symbols represent the means and bars the SEM. * P<0.05 Two-way ANOVA. The arrow represents the time of vehicle or CoCl2 administration.
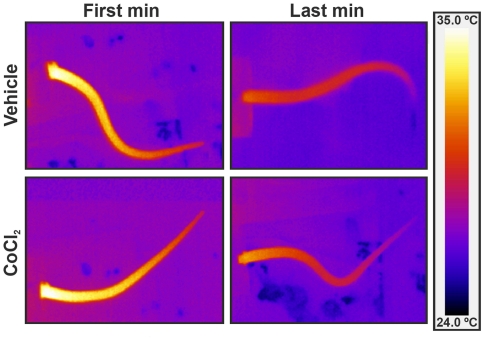
Figure 3. Infrared images of cutaneous temperature.
Tail infrared digital images of representative rats which received either vehicle or CoCl2 into lateral septal area, during the first and last minute of restraint. Note the drop in cutaneous tail temperature during the restraint. All images use the same color coding for temperature.
Effects of LSA inhibition in the delayed anxiogenic effect in the EPM of restraint
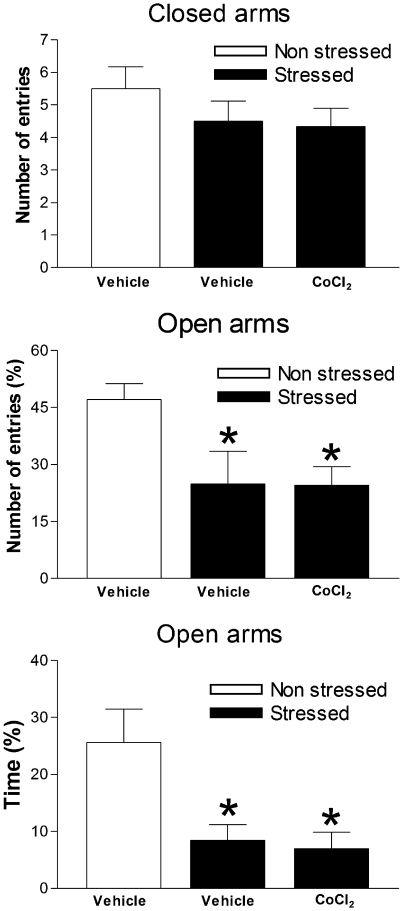
Animals submitted to acute restraint (n = 6) had a significant decrease in the percentage of time spent (F2,17 = 6.47, P<0.05) and in the number of entries in the open arms (F2,17 = 4.28, P<0.05) compared with unrestrained controls (n = 6). CoCl2 treatment (n = 6), however, failed to change these effects (P>0.05) Figure 4.
Figure 4. Consequences of restraint stress on behavioral responses.
Effects of bilateral microinjection of 100 nL of vehicle (n = 6) or 1 mM of CoCl2 (n = 6) administered immediately before 60 min restraint period on behavior observed 24 h later in the elevated plus-maze (EPM). A non-stressed group was used as control. Columns represent the means and the bars the SEM. *P<0.05, Bonferroni's post-hoc test.
Discussion
Solid and numerous evidences pointed that LSA is involved in the modulation of stress responses. The present work is the first study which analyzed several aspects of the autonomic and behavioral consequences associated by restraint stress. Our findings showing that LSA neurotransmission inhibition has a different consequence on autonomic responses observed during restraint stress, reducing hypertension and tachycardia without affecting both skin and body temperature changes. Moreover, LSA inhibition before restraint did not change the delayed increased anxiety behavior observed 24 h later in the EPM, suggesting that this inhibition failed to prevent behavioral consequences of stress exposure.
Our findings corroborate previous reports describing the autonomic and behavioral changes evoked by acute restraint [20], [35], [36]. In the present study the animals exhibited during the restraint period a significant increase in MAP and HR which were accompanied by a rapid CT drop followed by an increase in the IT. These changes reflect the activation of the autonomic nervous system that occurs during the exposure to an aversive situation [22], [37], [38].
Several studies demonstrated the activation of LSA during stress situations [19], [29]. The LSA can be subdivided in dorsal part, intermediate part and ventral part [12]. It is important to mention that in present study it was target the intermediate and dorsal parts of the LSA, avoiding reaching the ventral part due its proximity to the bed nucleus of stria terminalis [12], an area strongly involved with the cardiovascular modulation of restraint stress [18]. Despite that, it had shown that restraint stress stronger activates the medioventral part of the LSA compared to dorsal part [39]. Thus, the administration of CoCl2 in the ventral part of the lateral septal area could produce different effects on either autonomic responses or the stress-induced anxiogenesis. Therefore, we believe that more experiments are necessary to clarify the role of this LSA region, medioventral portion, on responses associated to restraint stress.
In the present study, we used CoCl2 to cause an acute and reversible LSA inhibition [3]. This compound has been employed to induce reversible inhibition of specific brain structures [9], [40], [41], [42]. CoCl2 causes a reversible inactivation that spreads over an area of about 0.1 to 2 mm2, by reducing Ca2+ pre-synaptic influx and thus interfering with neurotransmission release that leads to a synaptic blockage, without interference with fibers of passage [43], [44]. Thus, the use of CoCl2 to cause temporary inactivation of local neurotransmission can minimize several problems associated with lesion techniques, which could explain the differences between our results and previous reports.
It has been suggested that the LSA is an important central regulatory region for cardiovascular responses. Electrical stimulation of this region evokes blood pressure decreases or increases in anesthetized [45], [46] or unanesthetized rats [47], respectively. Cardiovascular changes are also reported after neurotransmitter agonist injections into the LSA, with glutamate decreasing [48] and acetylcholine, bradykinin and noradrenaline increasing MAP [49], [50], [51], [52], [53]. In addition, acute synaptic inhibition of the LSA enhances baroreflex responses, indicating an inhibitory influence of this region in this reflex [3].
Reinforcing the proposal that the LSA can regulate cardiovascular responses, the present results showed that acute neurotransmission inhibition in this region by local injection of CoCl2 reduces the cardiovascular changes observed during the restraint period. This result agrees with those from other studies reporting that LSA inactivation with muscimol reduces blood pressure increases during acute restraint stress [19] and during re-exposure to an aversive context [14]. Together they indicate that this region could be particularly related to the cardiovascular changes induced by stress exposure.
Contrasting with the decreased cardiovascular responses, LSA inhibition did not modify the stress-induced temperature changes. This finding indicates that during restraint stress the LSA could be modulating the activity of spinal sympathetic cardiomotor neurons but not that of sympathetic neurons controlling temperature changes. These latter neurons include those that control the cutaneous vascular tone in the tail skin and those that innervate the brown adipose tissue (BAT). Corroborating the present findings, distinct effects on sympathetic outflows to vasoconstrictor and thermoregulatory effectors have already been reported by several studies [54], [55], [56], [57], [58], [59]. Moreover, Beig et al. [37] found that systemic administration of a 5-HT2A receptor antagonist prevents the stress-induced hyperthermia but does not change the MAP and HR increases in rats submitted to social defeat.
Acute restraint decreased the exploration of the open arms of the EPM 24 h after restraint stress without changing the number of enclosed arms. A decreased in the exploratory activity of new environments that follows a period of acute restraint stress has been described in several models, including the open field. It is sensitive to systemic and intra-cerebral injection of anxiolytic and antidepressant drugs, suggesting that it reflects a delayed anxiogenic effect [23], [24], [25], [27].
Distinct from the results observed with cardiovascular parameters, LSA inactivation did not change the anxiogenic effects of restraint stress. This finding was somehow surprising, since a wealth of evidence indicates that this region plays an important role in fear and anxiety [4], [11], [60], [61] and lesions of the lateral septum induce anxiolytic-like effects in the EPM and in the shock-probe test [10], [61]. In agreement with these results the LSA is densely interconnected with a number of limbic, diencephalic, and midbrain regions that regulate emotions and autonomic functions (Sheehan, Chambers et al. 2004, [62]. The LSA has reciprocal connections with the amygdala and receives projections from the hippocampus [4], [63], the medial prefrontal cortex [64] and the bed nucleus of the stria terminalis [15], areas involved in the autonomic changes observed during restraint stress [8], [18], [65]. The LSA is proposed to regulate motivated behaviors by integrating sensory stimuli and conveying this information to regions responsible for controlling and adjust these behaviors to environmental demands, for review see [4]. Our cardiovascular data clearly agree with this proposal. The results, however, also suggest that the delayed behavioral consequences of stressful stimulation depend on the engagement of other brain structures. Also, restraint or immobilization stress can induce intense expression of c-Fos in several brain areas such as medial prefrontal cortex, LSA, paraventricular and dorsomedial nuclei of the hypothalamus, retrochiasmatic area, medial and cortical nuclei of the amygdala, periaqueductal gray matter, and locus coeruleus (LC) [30], [66]. The intense activation of CNS has been related to complexity of the stress response. The activation of different brain structures can be part of facilitatory or inhibitory circuitry on the HPA axis [67], [68], [69], modulating differently the responses of stress. Future studies, comparing, for example, the changes in cFos activation during restraint stress induced by LSA inhibition, could be helpful to address this question.
Therefore, our findings indicate that during restraint stress LSA activity modulates the cardiovascular but not temperature responses. Moreover, this region also does not seem to be involved on the delayed anxiogenic consequences of this procedure.
Acknowledgments
The authors wish to thank Laura H. A. de Camargo, Ivanilda A.C. Fortunato and José Carlos A. for technical help.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: D.G.R. is a FAPESP (Fundação de Amparo a Pesquisa do Estado de São Paulo) PhD fellow (2008/04069-7) and A.A.S. is a recipient of financial support from CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior)- Brazil (PNPD0176087). Research was also supported by a grant from FAPESP (2009/03187-9), CNPq (470042/2009-5 and 305996/2008-8) and FAEPA (Fundação de Apoio ao Ensino, Pesquisa e Assistência). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Pacak K, Palkovits M. Stressor specificity of central neuroendocrine responses: implications for stress-related disorders. Endocr Rev. 2001;22:502–548. doi: 10.1210/edrv.22.4.0436. [DOI] [PubMed] [Google Scholar]
- 2.Risold PY, Swanson LW. Chemoarchitecture of the rat lateral septal nucleus. Brain Res Brain Res Rev. 1997;24:91–113. doi: 10.1016/s0165-0173(97)00008-8. [DOI] [PubMed] [Google Scholar]
- 3.Scopinho AA, Crestani CC, Alves FH, Resstel LB, Correa FM. The lateral septal area modulates the baroreflex in unanesthetized rats. Auton Neurosci. 2007;137:77–83. doi: 10.1016/j.autneu.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 4.Sheehan TP, Chambers RA, Russell DS. Regulation of affect by the lateral septum: implications for neuropsychiatry. Brain Res Brain Res Rev. 2004;46:71–117. doi: 10.1016/j.brainresrev.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 5.LeDoux JE, Iwata J, Cicchetti P, Reis DJ. Different projections of the central amygdaloid nucleus mediate autonomic and behavioral correlates of conditioned fear. J Neurosci. 1988;8:2517–2529. doi: 10.1523/JNEUROSCI.08-07-02517.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Resstel LB, Correa FM. Medial prefrontal cortex NMDA receptors and nitric oxide modulate the parasympathetic component of the baroreflex. Eur J Neurosci. 2006;23:481–488. doi: 10.1111/j.1460-9568.2005.04566.x. [DOI] [PubMed] [Google Scholar]
- 7.Resstel LB, Correa FM, Guimaraes FS. The expression of contextual fear conditioning involves activation of an NMDA receptor-nitric oxide pathway in the medial prefrontal cortex. Cereb Cortex. 2008;18:2027–2035. doi: 10.1093/cercor/bhm232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tavares RF, Correa FM. Role of the medial prefrontal cortex in cardiovascular responses to acute restraint in rats. Neuroscience. 2006;143:231–240. doi: 10.1016/j.neuroscience.2006.07.030. [DOI] [PubMed] [Google Scholar]
- 9.Resstel LB, Alves FH, Reis DG, Crestani CC, Correa FM, et al. Anxiolytic-like effects induced by acute reversible inactivation of the bed nucleus of stria terminalis. Neuroscience. 2008;154:869–876. doi: 10.1016/j.neuroscience.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 10.Degroot A, Kashluba S, Treit D. Septal GABAergic and hippocampal cholinergic systems modulate anxiety in the plus-maze and shock-probe tests. Pharmacol Biochem Behav. 2001;69:391–399. doi: 10.1016/s0091-3057(01)00541-x. [DOI] [PubMed] [Google Scholar]
- 11.Menard J, Treit D. Lateral and medial septal lesions reduce anxiety in the plus-maze and probe-burying tests. Physiol Behav. 1996;60:845–853. doi: 10.1016/0031-9384(96)00138-2. [DOI] [PubMed] [Google Scholar]
- 12.Paxinos G. The rat nervous system. 2 Ed, Academic Press New York; 1995. [Google Scholar]
- 13.Pesold C, Treit D. The neuroanatomical specificity of the anxiolytic effects of intra-septal infusions of midazolam. Brain Res. 1996;710:161–168. doi: 10.1016/0006-8993(95)01359-8. [DOI] [PubMed] [Google Scholar]
- 14.Reis DG, Scopinho AA, Guimaraes FS, Correa FM, Resstel LB. Involvement of the lateral septal area in the expression of fear conditioning to context. Learn Mem. 2010;17:134–138. doi: 10.1101/lm.1534710. [DOI] [PubMed] [Google Scholar]
- 15.Risold PY, Swanson LW. Connections of the rat lateral septal complex. Brain Res Brain Res Rev. 1997;24:115–195. doi: 10.1016/s0165-0173(97)00009-x. [DOI] [PubMed] [Google Scholar]
- 16.Alves FH, Crestani CC, Correa FM. The insular cortex modulates cardiovascular responses to acute restraint stress in rats. Brain Res. 2010;1333:57–63. doi: 10.1016/j.brainres.2010.03.077. [DOI] [PubMed] [Google Scholar]
- 17.Brotman DJ, Golden SH, Wittstein IS. The cardiovascular toll of stress. Lancet. 2007;370:1089–1100. doi: 10.1016/S0140-6736(07)61305-1. [DOI] [PubMed] [Google Scholar]
- 18.Crestani CC, Alves FH, Tavares RF, Correa FM. Role of the bed nucleus of the stria terminalis in the cardiovascular responses to acute restraint stress in rats. Stress. 2009;12:268–278. doi: 10.1080/10253890802331477. [DOI] [PubMed] [Google Scholar]
- 19.Kubo T, Kanaya T, Numakura H, Okajima H, Hagiwara Y, et al. The lateral septal area is involved in mediation of immobilization stress-induced blood pressure increase in rats. Neurosci Lett. 2002;318:25–28. doi: 10.1016/s0304-3940(01)02463-6. [DOI] [PubMed] [Google Scholar]
- 20.Tavares RF, Correa FM, Resstel LB. Opposite role of infralimbic and prelimbic cortex in the tachycardiac response evoked by acute restraint stress in rats. J Neurosci Res. 2009;87:2601–2607. doi: 10.1002/jnr.22070. [DOI] [PubMed] [Google Scholar]
- 21.Blessing WW, Seaman B. 5-hydroxytryptamine(2A) receptors regulate sympathetic nerves constricting the cutaneous vascular bed in rabbits and rats. Neuroscience. 2003;117:939–948. doi: 10.1016/s0306-4522(02)00810-2. [DOI] [PubMed] [Google Scholar]
- 22.Vianna DM, Carrive P. Changes in cutaneous and body temperature during and after conditioned fear to context in the rat. Eur J Neurosci. 2005;21:2505–2512. doi: 10.1111/j.1460-9568.2005.04073.x. [DOI] [PubMed] [Google Scholar]
- 23.Kennett GA, Dickinson SL, Curzon G. Central serotonergic responses and behavioural adaptation to repeated immobilisation: the effect of the corticosterone synthesis inhibitor metyrapone. Eur J Pharmacol. 1985;119:143–152. doi: 10.1016/0014-2999(85)90290-0. [DOI] [PubMed] [Google Scholar]
- 24.Kennett GA, Dourish CT, Curzon G. Antidepressant-like action of 5-HT1A agonists and conventional antidepressants in an animal model of depression. Eur J Pharmacol. 1987;134:265–274. doi: 10.1016/0014-2999(87)90357-8. [DOI] [PubMed] [Google Scholar]
- 25.Korte SM, De Boer SF. A robust animal model of state anxiety: fear-potentiated behaviour in the elevated plus-maze. Eur J Pharmacol. 2003;463:163–175. doi: 10.1016/s0014-2999(03)01279-2. [DOI] [PubMed] [Google Scholar]
- 26.Sevgi S, Ozek M, Eroglu L. L-NAME prevents anxiety-like and depression-like behavior in rats exposed to restraint stress. Methods Find Exp Clin Pharmacol. 2006;28:95–99. doi: 10.1358/mf.2006.28.2.977840. [DOI] [PubMed] [Google Scholar]
- 27.Guimaraes FS, Del Bel EA, Padovan CM, Netto SM, de Almeida RT. Hippocampal 5-HT receptors and consolidation of stressful memories. Behav Brain Res. 1993;58:133–139. doi: 10.1016/0166-4328(93)90098-b. [DOI] [PubMed] [Google Scholar]
- 28.Padovan CM, Guimaraes FS. Restraint-induced hypoactivity in an elevated plus-maze. Braz J Med Biol Res. 2000;33:79–83. doi: 10.1590/s0100-879x2000000100011. [DOI] [PubMed] [Google Scholar]
- 29.Beck CH, Fibiger HC. Conditioned fear-induced changes in behavior and in the expression of the immediate early gene c-fos: with and without diazepam pretreatment. J Neurosci. 1995;15:709–720. doi: 10.1523/JNEUROSCI.15-01-00709.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen HC, Chen DY, Chen CC, Liang KC. Pre- and post-training infusion of prazosin into the bed nucleus of the stria terminalis impaired acquisition and retention in a Morris water maze task. Chin J Physiol. 2004;47:49–59. [PubMed] [Google Scholar]
- 31.Duncan GE, Johnson KB, Breese GR. Topographic patterns of brain activity in response to swim stress: assessment by 2-deoxyglucose uptake and expression of Fos-like immunoreactivity. J Neurosci. 1993;13:3932–3943. doi: 10.1523/JNEUROSCI.13-09-03932.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pezzone MA, Lee WS, Hoffman GE, Rabin BS. Induction of c-Fos immunoreactivity in the rat forebrain by conditioned and unconditioned aversive stimuli. Brain Res. 1992;597:41–50. doi: 10.1016/0006-8993(92)91503-7. [DOI] [PubMed] [Google Scholar]
- 33.Carobrez AP, Bertoglio LJ. Ethological and temporal analyses of anxiety-like behavior: the elevated plus-maze model 20 years on. Neurosci Biobehav Rev. 2005;29:1193–1205. doi: 10.1016/j.neubiorev.2005.04.017. [DOI] [PubMed] [Google Scholar]
- 34.Pellow S, File SE. Anxiolytic and anxiogenic drug effects on exploratory activity in an elevated plus-maze: a novel test of anxiety in the rat. Pharmacol Biochem Behav. 1986;24:525–529. doi: 10.1016/0091-3057(86)90552-6. [DOI] [PubMed] [Google Scholar]
- 35.Hsu HR, Chen TY, Chan MH, Chen HH. Acute effects of nicotine on restraint stress-induced anxiety-like behavior, c-Fos expression, and corticosterone release in mice. Eur J Pharmacol. 2007;566:124–131. doi: 10.1016/j.ejphar.2007.03.040. [DOI] [PubMed] [Google Scholar]
- 36.Resstel LB, Tavares RF, Lisboa SF, Joca SR, Correa FM, et al. 5-HT1A receptors are involved in the cannabidiol-induced attenuation of behavioural and cardiovascular responses to acute restraint stress in rats. Br J Pharmacol. 2009;156:181–188. doi: 10.1111/j.1476-5381.2008.00046.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Beig MI, Baumert M, Walker FR, Day TA, Nalivaiko E. Blockade of 5-HT2A receptors suppresses hyperthermic but not cardiovascular responses to psychosocial stress in rats. Neuroscience. 2009;159:1185–1191. doi: 10.1016/j.neuroscience.2009.01.038. [DOI] [PubMed] [Google Scholar]
- 38.Brown DR, Li SG, Lawler JE, Randall DC. Sympathetic control of BP and BP variability in borderline hypertensive rats on high- vs. low-salt diet. Am J Physiol. 1999;277:R650–657. doi: 10.1152/ajpregu.1999.277.3.R650. [DOI] [PubMed] [Google Scholar]
- 39.Martin J, Timofeeva E. Intermittent access to sucrose increases sucrose-licking activity and attenuates restraint stress-induced activation of the lateral septum. Am J Physiol Regul Integr Comp Physiol. 2010;298:R1383–1398. doi: 10.1152/ajpregu.00371.2009. [DOI] [PubMed] [Google Scholar]
- 40.Crestani CC, Tavares RF, Alves FH, Resstel LB, Correa FM. Diagonal band of Broca modulates the cardiac component of the baroreflex in unanesthetized rats. Neurosci Lett. 2008;448:189–193. doi: 10.1016/j.neulet.2008.10.055. [DOI] [PubMed] [Google Scholar]
- 41.Pelosi GG, Resstel LB, Correa FM. Dorsal periaqueductal gray area synapses modulate baroreflex in unanesthetized rats. Auton Neurosci. 2007;131:70–76. doi: 10.1016/j.autneu.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 42.Tavares RF, Correa FM, Resstel LB. Opposite role of infralimbic and prelimbic cortex in the tachycardiac response evoked by acute restraint stress in rats. J Neurosci Res. 2009 doi: 10.1002/jnr.22070. [DOI] [PubMed] [Google Scholar]
- 43.Hagiwara S, Byerly L. Calcium channel. Annu Rev Neurosci. 1981;4:69–125. doi: 10.1146/annurev.ne.04.030181.000441. [DOI] [PubMed] [Google Scholar]
- 44.Lomber SG. The advantages and limitations of permanent or reversible deactivation techniques in the assessment of neural function. J Neurosci Methods. 1999;86:109–117. doi: 10.1016/s0165-0270(98)00160-5. [DOI] [PubMed] [Google Scholar]
- 45.Covian MR. [Physiology of the septal area]. Acta Physiol Lat Am. 1966;16:119–152. [PubMed] [Google Scholar]
- 46.Calaresu FR, Ciriello J, Mogenson GJ. Identification of pathways mediating cardiovascular responses elicited by stimulation of the septum in the rat. J Physiol. 1976;260:515–530. doi: 10.1113/jphysiol.1976.sp011529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Correa FM, Polon VL. Effect of electrical stimulation of lateral septal area on blood pressure in anesthetized and unanesthetized rats. Acta Physiol Lat Am. 1978;28:69–71. [PubMed] [Google Scholar]
- 48.Gelsema AJ, Calaresu FR. Chemical microstimulation of the septal area lowers arterial pressure in the rat. Am J Physiol. 1987;252:R760–767. doi: 10.1152/ajpregu.1987.252.4.R760. [DOI] [PubMed] [Google Scholar]
- 49.Correa FM, Graeff FG. Central site of the hypertensive action of bradykinin. J Pharmacol Exp Ther. 1975;192:670–676. [PubMed] [Google Scholar]
- 50.Peres-Polon VL, Correa FM. Pressor effects of acetylcholine microinjected into forebrain nuclei of unanesthetized rats. Braz J Med Biol Res. 1992;25:257–266. [PubMed] [Google Scholar]
- 51.Peres-Polon VL, Correa FM. Pressor effects of acetylcholine injected into the lateral septal area of conscious rats. Neuropharmacology. 1994;33:1537–1544. doi: 10.1016/0028-3908(94)90127-9. [DOI] [PubMed] [Google Scholar]
- 52.Pirola CJ, Scheucher A, Balda MS, Dabsys SM, Finkielman S, et al. Serotonin mediates cardiovascular responses to acetylcholine, bradykinin, angiotensin II and norepinephrine in the lateral septal area of the rat brain. Neuropharmacology. 1987;26:561–566. doi: 10.1016/0028-3908(87)90148-1. [DOI] [PubMed] [Google Scholar]
- 53.Scopinho AA, Resstel LB, Antunes-Rodrigues J, Correa FM. Pressor effects of noradrenaline injected into the lateral septal area of unanesthetized rats. Brain Res. 2006;1122:126–134. doi: 10.1016/j.brainres.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 54.Stornetta RL. Neurochemistry of bulbospinal presympathetic neurons of the medulla oblongata. J Chem Neuroanat. 2009;38:222–230. doi: 10.1016/j.jchemneu.2009.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.DeBeck LD, Petersen SR, Jones KE, Stickland MK. Heart rate variability and muscle sympathetic nerve activity response to acute stress: the effect of breathing. Am J Physiol Regul Integr Comp Physiol. 2010;299:R80–91. doi: 10.1152/ajpregu.00246.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xia Y, Krukoff TL. Cardiovascular responses to subseptic doses of endotoxin contribute to differential neuronal activation in rat brain. Brain Res Mol Brain Res. 2001;89:71–85. doi: 10.1016/s0169-328x(01)00065-1. [DOI] [PubMed] [Google Scholar]
- 57.Xia Y, Krukoff TL. Differential neuronal activation in the hypothalamic paraventricular nucleus and autonomic/neuroendocrine responses to I.C.V. endotoxin. Neuroscience. 2003;121:219–231. doi: 10.1016/s0306-4522(03)00290-2. [DOI] [PubMed] [Google Scholar]
- 58.Kenney MJ, Claassen DE, Fels RJ, Saindon CS. Cold stress alters characteristics of sympathetic nerve discharge bursts. J Appl Physiol. 1999;87:732–742. doi: 10.1152/jappl.1999.87.2.732. [DOI] [PubMed] [Google Scholar]
- 59.Morrison SF. Differential regulation of sympathetic outflows to vasoconstrictor and thermoregulatory effectors. Ann N Y Acad Sci. 2001;940:286–298. doi: 10.1111/j.1749-6632.2001.tb03684.x. [DOI] [PubMed] [Google Scholar]
- 60.Feldon J, Rawlins JN, Gray JA. Discrimination of response-contingent and response-independent shock by rats: effects of medial and lateral septal lesions and chlordiazepoxide. Behav Neural Biol. 1982;35:121–138. doi: 10.1016/s0163-1047(82)91143-8. [DOI] [PubMed] [Google Scholar]
- 61.Menard J, Treit D. Intra-septal infusions of excitatory amino acid receptor antagonists have differential effects in two animal models of anxiety. Behav Pharmacol. 2000;11:99–108. doi: 10.1097/00008877-200004000-00001. [DOI] [PubMed] [Google Scholar]
- 62.Whitehead MC, Bergula A, Holliday K. Forebrain projections to the rostral nucleus of the solitary tract in the hamster. J Comp Neurol. 2000;422:429–447. [PubMed] [Google Scholar]
- 63.Volz HP, Rehbein G, Triepel J, Knuepfer MM, Stumpf H, et al. Afferent connections of the nucleus centralis amygdalae. A horseradish peroxidase study and literature survey. Anat Embryol (Berl) 1990;181:177–194. doi: 10.1007/BF00198957. [DOI] [PubMed] [Google Scholar]
- 64.Vertes RP. Differential projections of the infralimbic and prelimbic cortex in the rat. Synapse. 2004;51:32–58. doi: 10.1002/syn.10279. [DOI] [PubMed] [Google Scholar]
- 65.Fortaleza EA, Tavares RF, Correa FM. The medial amygdaloid nucleus modulates cardiovascular responses to acute restraint in rats. Neuroscience. 2009;159:717–726. doi: 10.1016/j.neuroscience.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 66.Cullinan WE, Herman JP, Battaglia DF, Akil H, Watson SJ. Pattern and time course of immediate early gene expression in rat brain following acute stress. Neuroscience. 1995;64:477–505. doi: 10.1016/0306-4522(94)00355-9. [DOI] [PubMed] [Google Scholar]
- 67.Figueiredo HF, Bodie BL, Tauchi M, Dolgas CM, Herman JP. Stress integration after acute and chronic predator stress: differential activation of central stress circuitry and sensitization of the hypothalamo-pituitary-adrenocortical axis. Endocrinology. 2003;144:5249–5258. doi: 10.1210/en.2003-0713. [DOI] [PubMed] [Google Scholar]
- 68.Lachuer J, Delton I, Buda M, Tappaz M. The habituation of brainstem catecholaminergic groups to chronic daily restraint stress is stress specific like that of the hypothalamo-pituitary-adrenal axis. Brain Res. 1994;638:196–202. doi: 10.1016/0006-8993(94)90650-5. [DOI] [PubMed] [Google Scholar]
- 69.Li HY, Sawchenko PE. Hypothalamic effector neurons and extended circuitries activated in “neurogenic” stress: a comparison of footshock effects exerted acutely, chronically, and in animals with controlled glucocorticoid levels. J Comp Neurol. 1998;393:244–266. [PubMed] [Google Scholar]