Abstract
BACKGROUND
African-American breast cancer survivors may be at high risk for reproductive health problems, including menopause symptoms, sexual dysfunction, and distress about cancer-related infertility. We partnered with Sisters Network® Inc. to create the SPIRIT program, a culturally sensitive intervention program combining a written workbook and peer counseling.
METHODS
Three hundred women were randomized either to receive the workbook plus three in-person sessions with a trained peer counselor, or the workbook plus ≤ 30 minutes of telephone counseling, to be initiated by the participant. Questionnaires at baseline, post-treatment, and 6- and 12-month follow-ups assessed emotional distress, sexual function, relationship satisfaction, spirituality, menopause symptoms, and knowledge. Satisfaction with the program and utilization of medical care were also assessed.
RESULTS
Both groups of women improved significantly in knowledge, decreased in distress, and had decreased hot flashes. Sexually active women had improved sexual function at 6-month follow-up, but not at one year. Peer counseling had little incremental benefit over the telephone counseling group, however.
CONCLUSIONS
The SPIRIT program was rated very useful by 66% of women. Outcomes justify continued use of the workbook and further research to optimize the impact of peer counseling.
Keywords: sexuality, menopause, fertility, breast neoplasms, peer counseling, African American
Survivors of breast cancer rate their overall quality of life positively, 1–3 yet problems with reproductive health remain long-term concerns for as many as half of women.1,2,4–7 Psychological distress diminishes over the first year after breast cancer diagnosis, but sexual dysfunction, menopausal symptoms, and infertility-related distress remain severe and pervasive.1–7 Premenopausal women who experience abrupt, treatment-related, premature ovarian failure have the greatest risk of developing such symptoms,4,8,9 but women treated with aromatase inhibitors also experience severe sexual and menopausal complaints.10
African American women may be particularly vulnerable to reproductive health problems after breast cancer. Compared to Caucasian women, African American women are less likely to be diagnosed at an early stage,11 have higher mortality rates,12 and are more likely to be diagnosed before age 40.11 African American breast cancer survivors over age 50 report poorer physical quality of life than white survivors.13,14
Though sexuality is not always openly discussed in the African American community, it is salient for African American women. In fact, African American women unselected for health rate sex as more important than Caucasian women and report higher rates of sexual activity.15,16 They also report more frequent and distressing hot flashes17,18 and more severe vaginal dryness17,19 than Caucasian women. African American women have higher rates of infertility than white or Hispanic women, are less likely to seek medical help, and have poorer success rates if they use assisted reproductive technology.17
Pilot Study
We partnered with the national advocacy organization, Sisters Network® Inc. to create a pilot intervention, SPIRIT (Sisters Peer Counseling In Reproductive Issues after Treatment) designed to improve knowledge and reduce symptoms related to sexual dysfunction, menopause, and distress about infertility in African-American breast cancer survivors.20 Forty-eight women were randomized either to begin counseling with one of three trained, peer counselors, or to enter a three-month waitlist control group followed by the intervention. The program included a written workbook with detailed information on menopause, sexual function; and issues of pregnancy and fertility. Peer counseling was accomplished in three sessions, each focusing on one of the chapters. Since no significant changes in outcome measures occurred during the waitlist period, the groups were combined in analyzing the efficacy of the intervention. At 3-month follow-up, women’s knowledge about reproductive health improved significantly. Hot flashes and emotional distress decreased. Although sexual function did not change significantly, emotional distress improved over time in women who were sexually dysfunctional at baseline. Eighty-one percent of women rated the program as “very useful to me.”
Given these positive results, we began a national trial of the SPIRIT program, again in partnership with Sisters Network® Inc. The aims were as follows:
Assess effectiveness of the full peer counseling program compared to a brief, phone counseling condition, both including the workbook;
Examine the influence of medical, demographic, and psychosocial factors, on baseline levels of reproductive problems, and on the outcome of the intervention.
MATERIALS AND METHODS
This study was approved by the UT MD Anderson Cancer Center Institutional Review Board (IRB).
Subject Recruitment
Participants needed to self-identify as African-American and to be at least one year post-diagnosis of breast cancer, off active treatment other than hormonal therapy, and have adequate English skills. Recruitment sources included Sisters Network® Inc. chapters, community events, health fairs, and church support groups. IRB-approved flyers were supplied to local beauty shops, car washes, mastectomy prosthesis and lingerie stores, etc. Peer counselors identified potential participants.
Screening, informed consent, and assessment procedures were conducted by research staff in Houston. Counselors were only responsible for the intervention. A team member elicited verbal consent for telephone screening for study eligibility. Women were subsequently mailed a written informed consent form along with the baseline questionnaires. If forms were not completed and returned within 3 weeks, the Houston team made up to 3 reminder calls and then sent one reminder letter before stopping further contact.
Study Design
Participants were assigned to one of the two treatment groups using minimization, a form of adaptive randomization.21 Before a participant was assigned to a group, the number of participants in each group with similar covariate characteristics were totaled, based on marginal sums. Each covariate was considered separately. Assignment to treatment was based on maintaining the best overall balance. Variables used were age (= 45 vs. > 45), marital status (married vs. not married), menopausal status at diagnosis, and current menopausal status.
Participants received a welcome letter with instructions on proceeding, a signed copy of the informed consent form, and the SPIRIT workbook. For the peer counseled group, a counselor was assigned to meet with the participant three times during the 6-week treatment period, either in the participant’s home or at a site such as a church or community center. Each 60- to 90-minute session focused on one chapter of the workbook. Counselors sometimes traveled overnight to accommodate participants who lived in remote areas, conducting three sessions within a period of one or two days.
The telephone group’s packet included the workbook, the counselor’s contact information, encouragement to call the counselor for up to 30 minutes to discuss issues in the SPIRIT workbook, and a prepaid phone card. The counselor kept a log of the date, time, duration, and topic of any calls from the participant. The counselor did not initiate any contacts in the telephone condition unless the Houston team identified a need; for example a questionnaire result might trigger a telephone assessment of psychological distress.
The SPIRIT Workbook
A 77-page workbook using African-American themed clipart was revised using the pilot study results.29 The reading level was 8th grade (readability score 61.2). Each chapter began with a list of topics (for example “Learning more about ways to overcome vaginal dryness”). The survivor rated the personal importance of each topic before each counseling session, which helped to tailor the focus according to factors such as patient age, concerns about sexuality or childbearing, etc. Breast cancer and menopause was discussed and strategies suggested for decreasing hot flashes, vaginal dryness, and urinary incontinence. The sexuality chapter explained the impact of breast cancer treatments on pain with sex and loss of desire. Chapter 3, “Cancer and Your Family,” discussed inherited breast cancer, health of offspring, and becoming an advocate of cancer screening—issues important to women of all ages. For younger women, information was presented on infertility and pregnancy. Eac0h chapter included an index of problems addressed, with a summary of proposed solutions (self-help and medical).
Counselor Selection and Training
Forty-one peer counselors (African-American breast cancer survivors) were trained, but only 27 saw at least one participant. The original 35 were chosen by Karen Jackson, founder and National President of Sisters Network® Inc.. Their expenses were paid to attend a 5-day counselor training conference at the UT MD Anderson Cancer Center in November, 2003. The curriculum included didactic material and experiential learning in supervised role plays. Each counselor received detailed treatment manuals for the peer counseling sessions and the phone counseling condition.
Fourteen women dropped out of the counselor group, including four just after the training. Common reasons included poor health or life stress. Discomfort with the sexual topics was a factor for a few. During the course of the study, five counselors who were not fulfilling their responsibilities were dropped. Another eight women were trained as counselors through intensive meetings with an experienced and successful counselor. New counselors passed a telephone evaluation by a Houston team member that included role plays using standardized scenarios.
Using a template, each counselor developed a local and national reproductive health resource list to give to participants. Counselors were compensated $40/session for peer counseling and $30 per telephone case (which might involve 0 to 30 minutes of phone time plus keeping a log of calls). As an incentive to recruit participants, counselors who contributed more than 15 cases per year received a $10 raise for each additional peer counseling session or telephone counseling case.
Quality Assurance: Regional Managers and the Houston Research Team
Seven counselors were appointed as regional managers. Managers acted as counselors, but received additional compensation for weekly quality control duties: checking by phone with assigned counselors on recruitment efforts and counseling sessions and reviewing mental health or medical concerns. Counselors notified their manager of any urgent mental health issues. Managers consulted in turn with the Houston team. Counselors could also contact the Houston team directly for advice.
Houston team members included the principal investigator (LRS), the project coordinator (PL), and postdoctoral fellows. Two counselors from the pilot study became research assistants. All were African-American women other than Dr. Schover and one fellow. Monthly teleconference calls included regional managers and members of the Houston team. Common topics included recruitment strategies, reaching out into underserved and rural communities, and problems with participants or counselors.
Demographic and Medical Information
Demographic information obtained during the telephone screening included age, marital status, education, occupation, income, and ethnic identity. Women also reported years since breast cancer diagnosis, menstrual status at diagnosis and currently, and major categories of breast cancer treatment (see Table 1).
Table 1.
Demographic and Medical Characteristics of Participants by Intervention Group
| Variable | Peer Counseled (N=151) | Phone Contact (N=146) | Significance |
|---|---|---|---|
| Age | 54.4 ± 9.7 | 54.0 ± 9.8 | NS |
|
| |||
| Years since diagnosis | 7.0 ± 7.0 | 6.0 ± 5.4 | NS |
|
| |||
| Marital status: | |||
| Married | 39% | 40% | |
| Divorced/separated | 32% | 38% | |
| Widowed | 12% | 6% | |
| Never married | 17% | 16% | NS |
|
| |||
| Education: | |||
| Less than high school | 4% | 6% | |
| High school | 13% | 13% | |
| Some college | 41% | 42% | |
| 4-year college degree | 21% | 19% | |
| Postgraduate degree | 19% | 20% | |
| Missing | 2% | 0% | NS |
|
| |||
| Family Income: | |||
| Less than $25,000 | 25% | 21% | |
| $26,000–$50,000 | 28% | 40% | |
| $51,000–$75,000 | 19% | 23% | |
| $76,000–$100,000 | 11% | 6% | |
| Greater than $100,000 | 7% | 6% | |
| Missing | 10% | 4% | NS |
|
| |||
| Menstrual Status: | |||
| Regular cycles | 8% | 7% | |
| Irregular cycles | 5% | 10% | |
| Postmenopausal | 44% | 44% | |
| Hysterectomy | 40% | 35% | |
| Missing | 3% | 4% | NS |
|
| |||
| Breast surgery: | |||
| Lumpectomy (unilateral) | 35% | 39% | |
| Mastectomy (unilateral) | 44% | 44% | |
| Mastectomy (bilateral) | 7% | 8% | |
| Combination | 13% | 8% | |
| Missing | 1% | 1% | NS |
|
| |||
| Breast Radiotherapy | 59% | 51% | NS |
|
| |||
| Chemotherapy | 71% | 68% | NS |
|
| |||
| Sexually active at all assessment points | 50% | 41% | NS |
Outcome Measures
Participants filled out questionnaires at baseline, after the 6-week treatment period, and at 6-month and 1-year follow-up. At each follow-up, women were compensated $20 for time and trouble. Packets were mailed by the Houston team at the designated time interval. If they were not returned within 3 weeks, participants received up to 3 reminder calls and a letter.
Questionnaires included the 12-item Spiritual Well-Being Subscale of the Functional Assessment of Cancer (FACIT-Sp),22 since spirituality has been identified as a particularly important factor in coping with cancer for African-American women.23 Women who were married or in a serious relationship of ≥ 6 months completed an abbreviated 7-item form 24 of the widely used Dyadic Adjustment Scale (A-DAS).25 Participants who were not in a serious relationship instead completed the 5-item dating subscale of the Cancer Rehabilitation Evaluation System (CARES),26 measuring comfort in dating after cancer.
To measure emotional distress, women completed the Brief Symptom Inventory-18 (BSI-18), an 18-item form of the BSI that includes items from the subscales measuring Somatization, Depression, and Anxiety, as well as a Global Severity Index (GSI) summary score. 27 Norms are based on 741 female oncology patients, including 298 with breast cancer.
The 19-item Female Sexual Function Index (FSFI) assessed five domains: sexual desire, arousal, lubrication, orgasm, satisfaction, and pain. A total FSFI score below 26.55 indicated sexual dysfunction.28
To evaluate menopausal symptoms, we included 7 items from the Breast Cancer Prevention Trial (BCPT) Symptom Checklist.29 Respondents rated each symptom on a 5-point scale from not at all to extremely bothersome over the past four weeks. The items yield three subscales, urinary incontinence, vaginal irritation, and hot flashes, and a summary score.30
We included six multiple-choice items from our previous surveys on having children after cancer:7,31 Women rated their interest in having a child at the time of cancer diagnosis, and concerns about becoming infertile after treatment, pregnancy triggering a cancer recurrence, cancer treatment damaging the health of subsequent children, and the lifetime cancer risk of offspring. An item asked whether experiencing cancer influenced desire to have children. Responses were added to create a composite score with a possible range of 6 to 25.
We created a 25-item True/False knowledge test for the SPIRIT pilot study, basing items on material in the workbook.20 For the national study, we replaced several items that were too easy with more difficult questions.
Utilization of Reproductive Health Care
At baseline, women were asked whether they had utilized eight types of health care within the past year: a routine pelvic examination with pap smear; help for a menopause-related problem, tests or treatment related to fertility, visit with an obstetrician about the safety of pregnancy, medical visit for a sexual problem, mental health visit for a sexual problem, and mental health visit for a problem unrelated to sex. These types of health care were discussed in the SPRIT workbook as potentially useful to some breast cancer survivors. At subsequent assessments, women were asked if they had utilized each type of health care since joining the SPIRIT program.
Program Evaluation
At the post-treatment assessment, each participant was mailed a program evaluation questionnaire with a return envelope so that it could be sent anonymously, separate from other questionnaires. Many participants knew their counselors well and if their questionnaire was identifiable, could be reluctant to give negative feedback. Women were asked to write the name of their counselor on the form, since ratings were used to check counselor performance.
Statistical Analyses
Descriptive analyses were conducted on questionnaire data from baseline and follow-up (post-treatment and 6- and 12-month) assessments. Descriptive statistics (e.g., frequencies, mean, range, standard deviation, skewness, and kurtosis) together with 95% confidence intervals (CIs) were obtained where appropriate. A two-tailed probability of 0.05 was considered significant. Distributional characteristics of the variables were examined using boxplots, histograms, quantile-quantile plots, and the Kolmogorov-Smirnov test of normality where appropriate. Knowledge scores, the prevalence of sexual dysfunction, menopausal symptoms, emotional distress, concern regarding childbearing, and medical service utilization were established with proportions of participants, along with 95% CIs.
If differences between treatment groups did not approach significance at baseline or across time, mixed model analyses were calculated using all women in the sample. Each woman’s change from baseline to subsequent follow-up points on an outcome measure was assessed to control for participant attrition across time. For all mixed models, a random intercept was used for the subject with a repeated statement for the variable of time. An autoregressive correlation matrix was used. In addition, for the FSFI, models were calculated separately for the sample as a whole and only for women who were sexually active at all assessment time points.
RESULTS
Demographic and Medical Factors
Table 1 presents demographic and medical factors by intervention group for the women who participated in the study. Only 2 participants identified themselves as Latinas. Minimization was successful in ensuring that the two groups did not differ significantly.
Attrition across Time
Table 2 presents the number of women completing questionnaires at each assessment time point. Attrition across time did not differ significantly between the intervention groups. Fifteen women (13% of missing cases) stopped participation due to death or cancer recurrence.
Table 2.
Questionnaire Completion across Time
| Assessment Point | Intervention Group | |||
|---|---|---|---|---|
| Peer Counseling | Phone Counseling | |||
| N | % | N | % | |
| Baseline | 152 | 100% | 148 | 100% |
| Post-Counseling | 111 | 73% | 104 | 70% |
| 6-month Follow-up | 94 | 62% | 97 | 66% |
| One Year Follow-up | 89 | 59% | 96 | 65% |
Psychosocial Outcome Variables
Table 3 presents questionnaire scores across time for the entire sample. Between-group comparisons did not differ significantly across time. In a mixed model (N = 291 participants at baseline and 184 at 12-month follow-up), a significant decrease in distress occurred across time, with a slight increase again at 12-month follow-up F(3,293) = 4.97, P = 0.0022). Mean scores for the Somatization subscale decreased significantly across time (P = 0.0002). There was a trend for Depression to decrease (P = 0.0699). Initial mean GSI scores were only elevated by 0.5 SD compared to the oncology norms and were close to the normative mean at follow-up. The percentage of women who met criteria for “caseness” on the BSI-18, i.e. distress according to screening criteria, did not differ significantly between the intervention groups at any time point. The prevalence of “caseness” decreased over time, but not significantly (16.1% at baseline, 11.2% post-treatment, and 10.6% and 10.9% respectively at 6-month and 12-month follow-up).
Table 3.
Outcomes across Time for the Entire Sample
| Variable | Baseline | Post-TX | 6-mo | 12-mo | P-Level |
|---|---|---|---|---|---|
| Knowledge Scores | 16.4 ± 2.8 | 17.8 ± 3.5 | 17.5 ± 3.5 | 18.1 ± 3.3 | < 0.0001 |
| BSI-18 GSI Scores | 11.2 ± 12.3 | 9.3 ± 11.5 | 9.1 ± 10.6 | 9.6 ± 11.1 | <0.0022 |
| FSFI Total Score | 18.2 ± 10.7 | 18.1± 10.7 | 18.5 ± 10.8 | 17.3 ± 10.7 | NS |
| Total Menopause Symptom Scores | 2.7 ± 1.7 | 2.7 ± 1.8 | 2.7 ± 1.8 | 2.8 ± 1.7 | NS |
| Hot Flash Scores | 1.8 ± 1.4 | 1.7 ± 1.4 | 1.6 ± 1.4 | 1.7 ± 1.3 | 0.0063 |
| A-DAS Scores | 21.0 ± 6.5 | 21.5 ± 7.0 | 21.0 ± 7.2 | 20.9 ± 7.2 | NS |
| Childbearing Distress | 15.6 ± 3.1 | 15.3 ± 2.6 | 15.5 ± 2.6 | 15.4 ± 3.1 | NS |
| FACIT-Sp | 42.0 ± 6.4 | 40.8 ± 6.6 | 41.8 ± | 42.2 ± 6.4 | NS |
An interaction effect between treatment group and time was significant for depression scores (P = 0.0362, see Figure 1). Depression decreased after treatment in the Peer Counseled group but temporarily increased in the Phone Counseled group. By 12-month follow-up, scores in the two groups were very similar.
Figure 1.
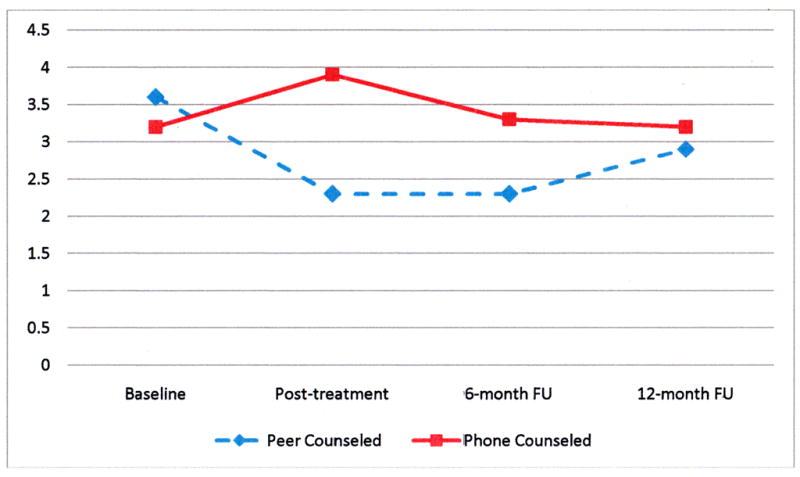
Mean BSI Depression Subscale Raw Scores (Time × Treatment Group)
No significant change was observed across time in the FSFI total score or subscale scores. However, when only the 115 women sexually active at all assessment points were included, total FSFI scores improved significantly from baseline to 6-month follow-up, but decreased by 12-month follow-up: F(3,185) = 2.47, P = 0.0630. Mean scores at all points remained in the dysfunctional range.30
Only 15% of our sample was still menstruating. On the Menopausal Symptom Scale, hot flashes decreased significantly across time in both intervention groups F(3, 572) = 4.15, P = 0.0063. The N was 293 at baseline and 180 at 12-month follow-up. Urinary symptoms and vaginal dryness did not change significantly across time, nor did the total symptom score.
Neither scores on the Abbreviated Dyadic Adjustment Scale (A-DAS) nor on the CARES dating subscale differed significantly by group or across time.
Distress about childbearing issues was measured across time for 135 women who completed at least 6 of the 7 items. No significant changes were found. At diagnosis, 20 women (7%) definitely wanted to have a child in the future, 9 (3%) probably wanted a child in the future, and 15 (5%) were unsure. The mean baseline Childbearing Distress Scale for this group of women (N =42, 2 missing cases) was 18.7 ± 4.6, significantly greater (P < 0.0001) than the mean for other participants (N = 200, 14.8 ± 2.0). Within this subgroup, distress decreased by 12-month follow-up (N = 26, mean: 17.7 ± 4.1), but the difference across time was not significant (P = 0.2340).
The two intervention groups did not differ significantly on Knowledge Test scores, at baseline or across time. Although the Cronbach’s alpha of 0.53 for this sample was less than optimal, knowledge about reproductive health increased significantly over time F(3,579) = 22.48, P < 0.0001.
Factors Correlated with Knowledge and Sexual Function/Satisfaction at Baseline
Knowledge Scores were significantly higher for women with 4-year college degrees: t(286) = =2.17, P = 0.0305 and higher incomes: t(270) = −1.89, P = 0.0592. Women with higher knowledge scores also had higher FSFI total scores: Pearson R2 = 0.20, P = 0.0038.
Married women (N = 103) had significantly better FSFI total scores than unmarried (N = 119): 20.2 ± 10.0 vs. 16.5 ± 11.1, t(220) = −2.56, P = 0.0112. Total FSFI scores were highly correlated with abbreviated DAS scores for women in committed relationships (N = 127): Pearson R2 = 0.49, P < 0.0001. FACIT-Sp scores are correlated significantly with FSFI total scores: Pearson R2 = 0.15, P = 0.0213, particularly among women in committed relationships: Pearson R2 = 0.31, P = 0.0002.
Utilization of Reproductive Health Care
Health care utilization did not differ between intervention groups. Table 4 compares 175 women with both baseline and 1-year data on rates of utilization during the past year. Little change is evident in any one type of healthcare. Women used fewer types of healthcare at one-year follow-up compared to baseline (F(3, 573) = 33.75, Pr >F < 0.00010. However, some women reported having a new type of health care at 12-month follow-up.
Table 4.
Percentage of Women Utilizing Health Care in the Past Year (N = 175)
| Type of Health Care | Baseline (in past year) | 12 months (since study began) | Utilized at 12-month follow-up but not at baseline |
|---|---|---|---|
| Saw family doctor or gynecologist for routine pelvic exam and pap smear | 87% | 86% | 8% |
|
| |||
| Saw family doctor or gynecologist for menopause-related problem (i.e. hot flashes, vaginal pain or dryness, trouble controlling urination, irregular cycles) | 33% | 30% | 12% |
|
| |||
| Had tests or treatment related to fertility (being able to get pregnant) | 2% | 1% | 1% |
|
| |||
| Saw an OB doctor to discuss safety and health in pregnancy | 4% | 2% | 1% |
|
| |||
| Saw a family doctor or gynecologist for a sexual problem | 6% | 8% | 6% |
|
| |||
| Saw a mental health counselor for a sexual problem | 2% | 2% | 2% |
|
| |||
| Had genetic counseling and/or testing to see if inherited breast cancer was in my family | 10% | 7% | 5% |
|
| |||
| Saw a mental health counselor for a nonsexual problem | 8% | 9% | 7% |
|
| |||
| Mean (± SD) number of types of health care utilized: | |||
| Peer Group | 1.48 ± 0.08 | 1.36 ± 0.10 | |
| Phone Group | 1.51 ± 0.08 | 1.47 ± 0.10 | |
Program Evaluation
The program evaluation questionnaire was completed by 169 women, including 72 in each intervention group and 23 who did specify their group clearly. Comparisons between groups only include the women in a known treatment condition. Table 5 summarizes women’s evaluations of the SPIRIT program for the entire sample. The only significant difference between groups was that peer counseled women were significantly more likely to rate the workbook as easy to understand (Chi-square (2) = 6.69, P = 0.0352). Ninety-six percent versus 83% of the phone counseled group rate the booklet as very easy to understand.
Table 5.
Evaluations of the SPIRIT Program at Post-Treatment Assessment
| Evaluation Question | Percentage of Total Sample |
|---|---|
| Ease of understanding SPIRIT workbook | |
| Very easy | 83% |
| Somewhat easy | 10% |
| A little to very difficult | 7% |
|
| |
| Personal usefulness of the SPIRIT workbook | |
| Very useful to me | 61% |
| Somewhat useful to me | 29% |
| A little useful/not useful | 10% |
|
| |
| Efficacy of workbook in covering special concerns of African-American breast cancer survivors | |
| Very good job | 66% |
| Fairly good job | 24% |
| Could have been better | 10% |
|
| |
| Counselor’s knowledge of the facts in the SPIRIT program | |
| Knew facts very well | 78% |
| Knew facts reasonably well | 6% |
| Lacked knowledge | 16% |
|
| |
| Counselor’s skills in being a good listener, communicating well, and making participant feel respected and valued | |
| Very skillful | 79% |
| Somewhat skillful | 5% |
| Could have been more skillful/poor skills | 16% |
|
| |
| Personal utility of overall SPIRIT program | |
| Very useful to me | 66% |
| Somewhat useful to me | 22% |
| A little useful/not useful to me | 12% |
|
| |
| Sharing information from SPIRIT with others | |
| Told several people | 44% |
| Told one or two people | 34% |
| Did not discuss with anyone | 22% |
In the peer counseled group, 35% of women met with their counselor at home. The rest met in other community or medical settings. The meeting place was rated very convenient by 96% of women. Similarly 97% rated their counselor as easy to contact and usually on time. Only 4% of women in the peer counseled group would have liked more sessions. Three sessions was rated “about right” by 77% and 19% would have preferred fewer sessions.
In the phone group, only 22% of women called their counselor during the 6-week intervention period. Ninety-eight percent of women who attempted to call their counselor said she was easily available and responded promptly to messages. The 30 minutes of phone time allowed was rated as about right by 53% of respondents. Thirty-one percent said it was more time than they needed but 16% would have preferred more time.
Influence of Counselor Investment in the SPIRIT Study
Although very few counselors received negative ratings on skill, knowledge, or accessibility, they varied greatly in the number of participants they recruited. Out of 27 counselors, 15 recruited 1 to 5 (including peer counseled and phone counseled women), 6 recruited 6 to 20 women, and 6 recruited over 20 women (range 22 to 47). To see whether counselor motivation affected outcomes, scores on the FSFI, BSI-18, and Knowledge Test at were compared across time for 31 participants assigned to counselors who recruited ≤ 5 women versus the other 257 women in the study; and for 109 women assigned to counselors who recruited ≤ 20 participants and the other 179 participants. No significant differences were found between these groups.
Influence of Use of Telephone Time
We compared outcomes (FSFI total score, BSI-18 GSI, or Knowledge scores) for women in the phone group who initiated ≥ 1 call to their counselor (N = 33) with those who had no contact (N = 115). The mean total number of minutes on the phone with the counselor was 28 ± 17. No significant differences were found at baseline or across time.
DISCUSSION
As in the pilot study, participants benefitted from the SPIRIT program. Women gained significantly in knowledge about breast cancer and reproductive health and reported significant decreases in hot flashes. Sexually active women reported improved sexual function through 6-month follow-up, though the advantage was lost at one year. Not surprisingly, given the greater difficulty in supervising a national group of counselors and longer follow-up in the national study (12-month vs. 3-month), the effect sizes were somewhat smaller than in the pilot (Cohen’s d from baseline to final assessment in the pilot versus the current study: for emotional distress 0.34 vs. 0.14; knowledge 0.63 vs. 0.56; hot flashes 0.22 vs. 0.10). Improvements in outcomes remained significant because of the much larger sample size. Two-thirds of the women in the national study rated the SPIRIT program as very useful compared to 81% in the pilot, and 78% shared information from the program with others in their lives. About 6% to 12% of women sought new medical care for gynecological screening, menopause symptoms, or sexual problems.
Although the national SPIRIT program was modestly successful, women in the phone counseling condition gained as much as those in the peer counseling group, suggesting that the workbook accounted for most of the benefit. The program was rated as very useful by 68% of peer counseled and 61% of phone group women. Outcomes were no better in the 22% of women in the phone condition who actually contacted their counselor, nor in women seen by more experienced and motivated peer counselors. The lack of an incremental benefit of full peer counseling surprised us, particularly since our counselors reported discussions of painful sexual and fertility issues not typically disclosed in support groups. Women who received peer counseling did have a drop in depression scores after the intervention, whereas depression actually increased for women in the phone condition, but mean scores remained within normal limits for both groups and were virtually identical by 12-month follow-up. Peer counseled women were also more likely to find the workbook easy to understand. Unfortunately, these small advantages cannot justify the time and expense of training and supervising peer counselors.
The SPIRIT program followed the important principles of working with a trusted community organization32 and developing culturally sensitive materials.33 Despite efforts to recruit underserved women, most participants were well-educated and had incomes above the poverty level. The high proportion of unmarried participants is consistent with national rates for African-American women.34 More affluent and educated women had better knowledge about breast cancer and reproductive health at baseline. Although sexual function and satisfaction were generally poor, women who were married and had better knowledge about reproductive health had better baseline scores. Among women with a committed partner, relationship satisfaction and strong spirituality both contributed to better FSFI scores. The older age range of our sample may have limited our power to detect improvements in distress about infertility.
Limitations of this study include the attrition rate. Despite reminders and financial compensation, only 72% of women completed the assessment after treatment and 62% at one year. It is possible that results are biased in a positive direction, since women dissatisfied with the program may have been more likely to drop out. We also did not target women at high distress for reproductive symptoms, and our sample was generally well adjusted emotionally. Only a small percentage were grieving about cancer-related infertility, although most were sexually dysfunctional. The loss at 1-year follow-up of gains in sexual function observed at 6 months may be related to the brief nature of the intervention and the lack of a mechanism for relapse prevention. We do not know which components of the program were responsible for the more enduring improvement in hot flashes, but 12% of women did see physicians for menopausal symptoms during the year of the study.
In fact, this intervention may be more powerful if targeted to premenopausal African-American women diagnosed with cancer. They are likely to have greater distress about sexual function and infertility,4,6,7 and to feel very isolated. 35 The SPIRIT program also might have more impact if administered soon after diagnosis, with periodic telephone or internet-based booster sessions. In the future we hope to test these modifications to optimize the effects of the program on quality of life.
Acknowledgments
This project was supported by grant RO1 CA102097 (Schover, PI) from the National Cancer Institute. None of the authors have financial disclosures to make.
References
- 1.Dorval M, Maunsell E, Deschenes L, Brisson J, Masse B. Long-term quality of life after breast cancer: comparison of 8-year survivors with population controls. J Clin Oncol. 1998;16:487–494. doi: 10.1200/JCO.1998.16.2.487. [DOI] [PubMed] [Google Scholar]
- 2.Helgeson VS, Tomich PL. Surviving cancer: a comparison of 5-year disease-free breast cancer survivors with healthy women. Psychooncology. 2005;14:307–317. doi: 10.1002/pon.848. [DOI] [PubMed] [Google Scholar]
- 3.Ganz PA, Desmond KA, Leedham B, Rowland JH, Meyerowitz BE, Belin TR. Quality of life in long-term, disease-free survivors of breast cancer: a follow-up study. J Natl Cancer Inst. 2002;94:39–49. doi: 10.1093/jnci/94.1.39. [DOI] [PubMed] [Google Scholar]
- 4.Schover LR. Premature ovarian failure and its consequences: vasomotor symptoms, sexuality, and fertility. J Clin Oncol. 2008;26:753–758. doi: 10.1200/JCO.2007.14.1655. [DOI] [PubMed] [Google Scholar]
- 5.Bordeleau L, Pritchard K, Goodwin P, Loprinzi C. Therapeutic options for the management of hot flashes in breast cancer survivors: an evidence-based review. Clin Ther. 2007;29:230–241. doi: 10.1016/j.clinthera.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 6.Peate M, Meiser B, Hickey M, Friedlander M. The fertility-related concerns, needs and preferences of younger women with breast cancer: a systematic review. Breast Cancer Res Treat. 2009;116:215–223. doi: 10.1007/s10549-009-0401-6. [DOI] [PubMed] [Google Scholar]
- 7.Canada AL, Schover LR. The psychosocial impact of interrupted childbearing in long-term female cancer survivors. Psychooncol. doi: 10.1002/pon.1875. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Malinovszky KM, Gould A, Foster E, Cameron D, et al. Quality of life and sexual function after high-dose or conventional chemotherapy for high-risk breast cancer. Br J Cancer. 2006;95:1626–1631. doi: 10.1038/sj.bjc.6603454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berglund G, Nystedt M, Bolund C, Sjoden PO, Rutquist LE. Effect of endocrine treatment on sexuality in premenopausal breast cancer patients: a prospective randomized study. J Clin Oncol. 2001;19:2788–2796. doi: 10.1200/JCO.2001.19.11.2788. [DOI] [PubMed] [Google Scholar]
- 10.Cella D, Fallowfield LJ. Recognition and management of treatment-related side effects for breast cancer patients receiving adjuvant endocrine therapy. Breast Cancer Res Treat. 2008;107:167–180. doi: 10.1007/s10549-007-9548-1. [DOI] [PubMed] [Google Scholar]
- 11.Baquet CS, Mishra SI, Commiskey P, Ellison GLl, DeShields M. Breast cancer epidemiology in blacks and whites: disparities in incidence, mortality, survival rates and histology. J Natl Med Assoc. 2008;100:480–488. doi: 10.1016/s0027-9684(15)31294-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Summers C, Saltzstein SL, Blair SL, Tsukamoto TT, Sadler GR. Racial/ethnic differences in early detection of breast cancer: a study of 250,985 cases from the California Cancer Registry. J Women’s Health. 2008;19:203–207. doi: 10.1089/jwh.2008.1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paskett ED, Alfano CM, Davidson MA, et al. Breast cancer survivors’ health-related quality of life: racial differences and comparisons with non-cancer controls. Cancer. 2008;113:3222–3230. doi: 10.1002/cncr.23891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Janz NK, Mujahid MS, Hawley ST, et al. Racial/ethnic differences in quality of life after diagnosis of breast cancer. J Cancer Surviv. 2009;3:212–222. doi: 10.1007/s11764-009-0097-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Avis NE, Brockwell S, Randolph JF, et al. Longitudinal changes in sexual functioning as women transition through menopause: results from the Study of Women’s Health Across the Nation. Menopause. 2009;16:442–452. doi: 10.1097/gme.0b013e3181948dd0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lutfey KE, Link CL, Rosen RC, Wiegel M, Mckinlay JB. Prevalence and correlates of sexual activity and function in women: results from the Boston Area Community Health (BACH) survey. Arch Sex Behav. 2009;38:514–527. doi: 10.1007/s10508-007-9290-0. [DOI] [PubMed] [Google Scholar]
- 17.Butts SF, Seifer DB. Racial and ethnic differences in reproductive potential across the life cycle. Fertil Steril. 2010;93:681–690. doi: 10.1016/j.fertnstert.2009.10.047. [DOI] [PubMed] [Google Scholar]
- 18.Thurston RC, Bromberger JT, Joffe H, et al. Beyond frequency: who is most bothered by vasomotor symptoms? Menopause. 2008;15:821–822. doi: 10.1097/gme.0b013e318168f09b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang AJ, Moore EE, Boyko EJ, et al. Vaginal symptoms in postmenopausal women: self-reported severity, natural history, and risk factors. Menopause. 2010;17:121–126. doi: 10.1097/gme.0b013e3181acb9ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schover LR, Jenkins R, Sui D, Harned Adams J, Marion MS, Jackson KE. Randomized Trial of Peer Counseling on Reproductive Health in African American Breast Cancer Survivors. J Clin Oncol. 2006;24:1620–1626. doi: 10.1200/JCO.2005.04.7159. [DOI] [PubMed] [Google Scholar]
- 21.Birkett NJ. Adaptive allocation in randomized controlled trials. Control Clin Trials. 1985;6:146–155. doi: 10.1016/0197-2456(85)90120-5. [DOI] [PubMed] [Google Scholar]
- 22.Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: The Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being Scale (FACIT-Sp) Ann Beh Med. 2002;24:49–58. doi: 10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- 23.Levine EG, Yoo G, Aviv C, Ewing C, Au A. Ethnicity and spirituality in breast cancer survivors. J Cancer Surviv. 2007;1:212–225. doi: 10.1007/s11764-007-0024-z. [DOI] [PubMed] [Google Scholar]
- 24.Hunsley J, Pinsent C, Lefebvre M, et al. Construct Validity of the Short Forms of the Dyadic Adjustment Scale. Fam Relat. 1995;44:231–237. [Google Scholar]
- 25.Sharpley CF, Cross DG. A psychometric evaluation of the Spanier Dyadic Adjustment Scale. J Marriage Fam. 1982;44:739–741. [Google Scholar]
- 26.Schag CAC, Heinrich RL, Aadland RL, et al. Assessing problems of cancer patients: Psychometric properties of the Cancer Inventory of Problem Situations. Health Psychol. 1990;9:83–102. doi: 10.1037//0278-6133.9.1.83. [DOI] [PubMed] [Google Scholar]
- 27.Zabora J, Brintzenhofe-Szoc K, Jacobsen P, et al. A new psychosocial screening instrument for use with cancer patients. Psychosomatics. 2001;42:241–246. doi: 10.1176/appi.psy.42.3.241. [DOI] [PubMed] [Google Scholar]
- 28.Wiegel M, Meston C, Rosen R. The Female Sexual Function Index (FSFI): a cross-validation and development of clinical cutoff scores. J Sex Marital Ther. 2005;31:1–20. doi: 10.1080/00926230590475206. [DOI] [PubMed] [Google Scholar]
- 29.Ganz PA, Rowland JH, Desmond K, et al. Life after breast cancer: understanding women’s health related quality of life and sexual functioning. J Clin Oncol. 1998;16:501–514. doi: 10.1200/JCO.1998.16.2.501. [DOI] [PubMed] [Google Scholar]
- 30.Ganz PA, Greendale GA, Petersen L, et al. Managing menopausal symptoms in breast cancer survivors: results of a randomized controlled trial. J Natl Cancer Inst. 2000;92:1054–1064. doi: 10.1093/jnci/92.13.1054. [DOI] [PubMed] [Google Scholar]
- 31.Schover LR, Rybicki LA, Martin BA, et al. Having children after cancer: a pilot survey of survivors’ attitudes and experiences. Cancer. 1999;86:697–709. doi: 10.1002/(sici)1097-0142(19990815)86:4<697::aid-cncr20>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 32.Freeman HP. Patient navigation: a community centered approach to reducing cancer mortality. J Cancer Educ. 2006;21:S11–S14. doi: 10.1207/s15430154jce2101s_4. [DOI] [PubMed] [Google Scholar]
- 33.Sheppard VB, Williams KP, Harrison TM, et al. Development of a decision-support intervention for Black women with breast cancer. Psycho-Oncology. 2010;19:62–70. doi: 10.1002/pon.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hummer RA, Hamilton ER. Race and ethnicity in fragile families. Future Child. 2010;20:113–121. doi: 10.1353/foc.2010.0003. [DOI] [PubMed] [Google Scholar]
- 35.Kantsiper M, McDonald EL, Geller G, Shockney L, Snyder C, Wolff AC. Transitioning to breast cancer survivorship: Perspectives of patients, cancer specialists, and primary care providers. J Gen Intern Med. 2009;24(Supp 2):S459–S466. doi: 10.1007/s11606-009-1000-2. [DOI] [PMC free article] [PubMed] [Google Scholar]


