Abstract
Patients with chronic heart failure (CHF) have a significantly lower peak aerobic capacity compared to healthy subjects, and, may therefore experience more inconvenience during the performance of domestic activities of daily life (ADLs). To date, the extent to which task-related oxygen uptake, heart rate, ventilation and symptoms during the performance of ADLs in CHF patients is different than in healthy subjects remains uncertain. General demographics, pulmonary function, body composition and peak aerobic capacity were assessed in 23 CHF outpatients and 20 healthy peers. In addition, the metabolic requirement of five simple self-paced domestic ADLs was assessed using a mobile oxycon. Task-related oxygen uptake (ml/min) was similar or lower in CHF patients compared to healthy subjects. In contrast, patients with CHF performing ADLs consumed oxygen at a higher proportion of their peak aerobic capacity than healthy subjects (p < 0.05). For example, getting dressed resulted in a mean task-related oxygen uptake of 49% of peak aerobic capacity, while sweeping the floor resulted in a mean task-related oxygen uptake of 52% of peak aerobic capacity, accompanied by significantly higher Borg symptom scores for dyspnea and fatigue (p < 0.05). Patients with CHF experience use a higher proportion of their peak aerobic capacity, peak ventilation and peak heart rate during the performance of simple self-paced domestic ADL than their healthy peers. These findings represent a necessary step in improving our understanding of improving what troubles patients the most—not being able to do the things that they could when they were healthy.
Keywords: Self-paced, ADL, Domestic, Chronic heart failure
Introduction
Oxygen uptake increases during the performance of simple activities of daily life (ADLs) and, in turn, laying claim to the aerobic capacity of individuals (Ainsworth et al. 2000; Velloso et al. 2003). Patients with chronic heart failure (CHF) have a significantly lower peak aerobic capacity compared to age-matched healthy subjects (Gosker et al. 2003). Patients with CHF may therefore experience more inconvenience during the performance of simple self-paced domestic ADLs. In fact, a reduced peak aerobic capacity has been shown to contribute to a reduced ability to perform habitual ADLs in CHF (Gosker et al. 2003; Mezzani et al. 2000; van den Berg-Emons et al. 2005).
Patients with chronic obstructive pulmonary disease (COPD) use a higher proportion of their peak oxygen consumption during the performance of simple domestic ADLs (Velloso and Jardim 2006; Velloso et al. 2003). Based on the striking similarities in systemic factors contributing to exercise intolerance in patients with COPD and CHF (Gosker et al. 2003), the present authors reasoned that patients with CHF may also use a higher proportion of their peak aerobic capacity during the performance of simple domestic ADLs compared to healthy elderly subjects.
To date, actual assessment of task-related oxygen uptake, heart rate and ventilation during the performance of domestic ADLs in patients with CHF has not been performed. So, whether task-related oxygen uptake during the performance of ADLs in patients with CHF is different than in healthy subjects remains uncertain. Nevertheless, a better insight in the task-related metabolic requirement of simple domestic ADLs in patients with CHF may allow clinicians to better develop patient management methodologies to reduce daily symptoms and to improve the performance of problematic ADLs in these patients.
We aimed to study task-related oxygen uptake, heart rate, minute ventilation and symptoms of dyspnoea and fatigue during the performance of five self-paced domestic ADLs in patients with CHF and healthy subjects. A priori, we hypothesized that patients with CHF have a relatively higher task-related oxygen uptake, heart rate and minute ventilation during domestic ADLs than healthy elderly subjects, accompanied by higher symptoms perception.
Methods
Population
Patients and healthy subjects (45–80 years of age) were recruited between July 2008 and February 2009. Twenty-three clinically stable CHF outpatients and 20 healthy peers volunteered to participate in the present study, which was approved by the institutional review board of the Maastricht University Medical Centre (MEC08-3-032). All tests were performed at the CIRO+ and were in accordance with the World Medical Association declaration of Helsinki (2004).
Patients were recruited at the outpatient clinic of CIRO+, a centre of expertise for chronic organ failure (Horn, the Netherlands). Patients had to be diagnosed with CHF and had the willingness to participate. Exclusion criteria were any unstable medical conditions that were contraindicative to exercise testing (e.g., hospitalization or unstable angina <4 weeks of enrolment or acute myocardial infarction <6 months of enrolment), neurological diseases, locomotor disorders and/or the use of long-term oxygen therapy. Healthy subjects [e.g., no current (drug) treatment by a medical specialist] were recruited by posters and amongst healthy subjects who participated in previous trials. At enrolment, written informed consent was obtained from potential participants, and study eligibility was determined.
Clinical phenotyping
General demographics, pulmonary function, body composition and peak aerobic capacity were assessed in all participants. Standard spirometry was obtained by a mass flowmeter (Masterscreen PFT, Carefusion Netherlands, Houten, the Netherlands) with numerical integration of the flow signal to determine forced expiratory volume and forced vital capacity (Miller et al. 2005; Spruit et al. 2007).
A symptom-limited cardiopulmonary exercise test on a bicycle was used to determine peak aerobic capacity and was performed according to international guidelines (American Thoracic Society; American College of Chest Physicians 2003). In brief, after calibration of the oxygen and carbon dioxide analyzer and flow mass sensor, the participants were asked to sit on an microprocessor controlled eddy current brake cycle ergometer (Ergoline type Ergoselect 200P, Carefusion Netherlands, Houten, the Netherlands). This stationary bicycle can handle cycling loads up to 400 Watts independent of the number of revolutions per minute. The saddle was mechanically adjusted properly to avoid the maximal extension of the knee. After a 3-min rest period sitting on the ergometer, exercise began with a 3-min warmup period at 0 Watts, followed by a progressively increasing ramp protocol of 10–15 Watts/min (CHF patients) or 15–25 Watts/min (healthy age-matched subjects), based on anthropometric data and functional impairment degree of the patients, to perform for an exercise time lasting 8–12 min. All patients had to maintain a pedaling frequency of 60–65 revolutions per minute, indicated by a digital display placed on the monitor of the ergometer. Breath-by-breath oxygen uptake (ml/min), carbon dioxide production (ml/min) and minute ventilation (l) were collected during the test (Oxycon Pro, Carefusion Netherlands, Houten, the Netherlands). Participants were continuously monitored by a 12-lead electrocardiogram (Corina; GE Medical Systems IT, Milwaukee, WI, USA) and a pulse oximeter (Model 9600; Nonin Medical Inc, Minneapolis, MN, USA). Blood pressure was measured at 2-min intervals. Peak aerobic capacity was recorded as the mean value of oxygen uptake during the last 30 s of the test and expressed as absolute value in ml/min.
Co-existing morbidities were assessed using the Charlson comorbidity index, which is a weighted index that takes into account the number and seriousness of co-morbid diseases (Charlson et al. 1987).
Patients with CHF were on various cardiac drug therapies: ACE-inhibitors or angiotensin receptor blockers (96%); β-blockers (92%); diuretics (92%); anticoagulant therapy (warfarin, 57%; aspirin, 43%); statins (57%) and/or isosobide mononitrate (26%). Moreover, some patients also received non-cardiac drug treatment: drugs to treat gastroesophageal reflux disease (22%); drugs to treat diabetes mellitus type II (22%); a benzodiazepine (9%); a drug prescribed for the pain of gouty arthritis (13%); and/or pulmonary inhalation drugs (13%). None of the healthy age-matched subjects used physician-prescribed drugs.
Activities of daily life
The metabolic requirement of 5 simple self-paced domestic ADLs was assessed using a mobile oxycon (Oxycon Mobile, CareFusion, San Diego, CA, USA) which provides reliable measurements of oxygen uptake and ventilation (Diaz et al. 2008). A mobile oxycon has been used before in patients with COPD without adverse events (Sillen et al. 2008; Sillen et al. 2010). Indeed, participants are able to move freely without discomfort.
Online breath-by-breath calculations of oxygen uptake and ventilation were recorded by the portable metabolic system during the performance of five domestic ADLs in the kitchen of the Department of Occupational Therapy of CIRO+: putting on two socks (sitting in a chair), two shoes (sitting in a chair) and a vest (standing, ADL1); folding eight towels (standing, ADL2); putting away groceries (i.e. 6 cans of beans of 400 g each) in the cupboard (standing and walking, ADL3); washing up 4 dishes, 4 cups and 4 saucers (standing, ADL4); and sweeping the floor for 4 min (standing and walking, ADL5). All ADLs were preceded with 4-min resting intervals (sitting in a chair). All participants were asked to perform the ADLs at their own pace as the participants accomplish them in their real life; and to score the degree of dyspnoea and fatigue at the beginning and end of all ADLs using a modified Borg symptom score ranging from 0 (no symptoms) to 10 points (worst symptoms ever experienced). Heart rate was monitored using a Polar belt (Polar Electro, Kempele, Finland).
Oxygen uptake during ADLs expressed as a proportion of the pre-determined peak aerobic capacity was chosen as primary outcome. Task-related oxygen uptake (ml/min and ml/kg/min); task-related heart rate and ventilation (both expressed as proportion of the peak heart rate and ventilation, respectively); the time to accomplish the first 4 ADLs (ADL5 was always 4 min); and Borg symptom scores for dyspnoea and fatigue at the end of each ADL were chosen as secondary outcomes.
Statistics
Data are presented as mean ± standard error of the mean or as prevalence (%), as appropriate. Unpaired Student’s t test was used to determine differences between patients with CHF and healthy peers. A posteriori, an unpaired Student’s t-test was used to determine differences in task-related oxygen uptake between CHF patients without COPD (n = 19) and healthy peers. All data analyses were performed using GraphPad/Prism version 5 software and SPSS 15.0. Based on data from a previous manuscript on task-related oxygen uptake in patients with COPD (Velloso et al. 2003) a sample size was estimated. Indeed, to have a 90% chance of detecting a 15% difference in task-related oxygen uptake at an α level of 0.05, the power calculation indicates that each of the two groups needed to enrol at least 20 subjects. A priori, the level of significance was set at ≤0.05. No adjustment was made to the statistical significance level for multiple comparisons.
Results
Characteristics
Patients had symptoms compatible with New York Heart Association (NYHA) functional class I, II or III (n = 2, 15 and 6, respectively). CHF was of a non-ischemic aetiology in 14 patients (61%). Seven patients (30%) had an implantable cardioverter defibrillator and three patients had a cardiac pacemaker (13%). Twelve patients (52%) had mitral regurgitation, in combination with aortic regurgitation (n = 2), tricuspid regurgitation (n = 1) or a combination thereof (n = 1). Moreover, 13 patients (57%) had a score of ≥2 points on the Charlson co-morbidity index: myocardial infarction (n = 7); peripheral artery disease (n = 3); COPD (n = 4); moderate renal failure (n = 1); and/or diabetes mellitus II (n = 5). All healthy age-matched subjects scored 0 points on the Charlson co-morbidity index. Consequently, CHF patients had a significantly higher score on the Charlson co-morbidity index (p < 0.01).
Although the proportion of men, and the average age, body weight and body mass index were comparable between groups, patients with CHF had significantly worse resting pulmonary function and lower peak aerobic capacity during the CPET than healthy peers (Table 1). Moreover, CHF patients had a significantly lower peak heart rate, while peak ventilation (expressed as a proportion of the calculated maximal voluntary ventilation), Borg dyspnoea scores and Borg fatigue scores at the end of CPET were comparable (Table 1).
Table 1.
Demographic, lung function characteristics and exercise capacity of CHF patients and age-matched healthy subjects
| CHF (n = 23) | Healthy (n = 20) | p-Value | |
|---|---|---|---|
| Demographics | |||
| Men/women (n) | 16/7 | 12/8 | – |
| Age (years) | 59.5 ± 2.6 | 62.1 ± 1.2 | 0.40 |
| Cardiac and pulmonary function | |||
| LVEF (%) | 36 ± 2 | – | – |
| NYHA class I/II/III/IV (n) | 2/15/6/0 | – | – |
| FEV1 (l) | 2.6 ± 0.2 | 3.4 ± 0.1 | 0.0020 |
| FEV1 (% predicted) | 84 ± 3.0 | 119 ± 5.4 | 0.0001 |
| FEV1/FVC (%) | 70 ± 2.4 | 77 ± 1.0 | 0.0165 |
| Body composition | |||
| Body weight (kg) | 82 ± 3 | 79 ± 3 | 0.56 |
| Body mass index (kg/m2) | 27 ± 1 | 27 ± 1 | 0.89 |
| Cardiopulmonary exercise test | |||
| Peak power output (Watts) | 108 ± 9 | 212 ± 13 | 0.0016 |
| Peak VO2 (ml/min) | 1,475 ± 104 | 2,155 ± 172 | 0.0012 |
| Peak VO2 (ml/kg/min) | 18.1 ± 1.1 | 27.5 ± 2.3 | 0.0004 |
| Peak VE (l) | 60 ± 4 | 87 ± 6 | 0.0005 |
| Peak VE (% MVV) | 60 ± 3 | 65 ± 4 | 0.31 |
| Peak HR (bpm) | 123 ± 5 | 155 ± 4 | 0.0001 |
| Peak HR (% max HR) | 77 ± 2 | 98 ± 2 | 0.0001 |
| Borg score dyspnoea (points) | 4.5 ± 0.4 | 5.5 ± 0.5 | 0.12 |
| Borg score fatigue (points) | 5.3 ± 0.5 | 5.7 ± 0.5 | 0.54 |
Results are presented as mean ± standard error of the mean. FEV1, forced expiratory volume in the first second; FVC, forced vital capacity; l, litre; kg, kilogram; kg/m2, kilogram per square meter; ml/min, millilitre per minute; % MVV, percentage of calculated maximal voluntary ventilation (40× FEV1 in litres); bpm, beats per minute; % max HR, percentage of calculated heart rate (220—age in years); VE, ventilation
Domestic ADLs
All participants were able to complete the study protocol. However, patients with CHF needed more time to complete ADL1, ADL2 and ADL4 than healthy age-matched subjects: 94.6 ± 5.0 versus 62.8 ± 3.0 s; 149.2 ± 6.3 versus 115.4 ± 4.6 s and 117.1 ± 6.5 versus 72.3 ± 4.4 s, respectively (all p < 0.001). The time needed to complete ADL3 was comparable (65.6 ± 4.0 vs. 62.8 ± 3.7 s, p = 0.61).
Task-related metabolic requirements
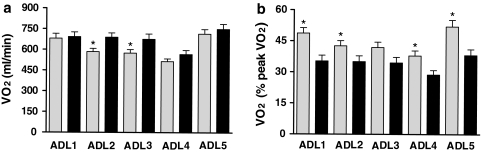
Task-related oxygen uptake (ml/min) was similar between patients with CHF and healthy age-matched subjects for ADL1 [mean difference (95%CI): −11 ml/min (−110, 87), p = 0.82], ADL4 [−52 ml/min (−121, 17), p = 0.14] and ADL5 [−35 ml/min (−133, 64), p = 0.4831]; and lower for ADL2 [−105 ml/min (−182, −27), p = 0.01] and ADL3 [−101ml/min (−191, −10), p = 0.03] in patients with CHF (Fig. 1a).
Fig. 1.
Oxygen uptake during domestic activities of daily life in patients with CHF and healthy subjects. a Mean ± SEM task-related oxygen uptake (VO2, ml/min) during the performance of five domestic activities of daily life (ADLs) in patients with chronic heart failure (n = 23, grey bars) and healthy subjects (n = 20, black bars). *p < 0.05 versus healthy subjects. b Mean ± SEM task-related oxygen uptake (VO2, proportion of the peak oxygen uptake measured during CPET, % peak VO2) during the performance of five domestic activities of daily life (ADL 1–5) in patients with chronic heart failure (n = 23, grey bars) and healthy subjects (n = 20, black bars). *p < 0.05 versus healthy subjects
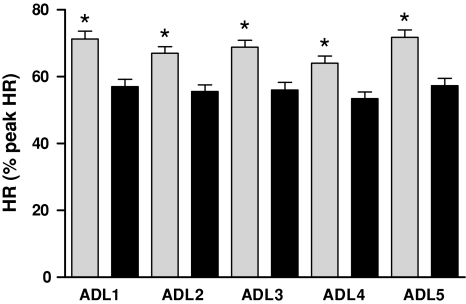
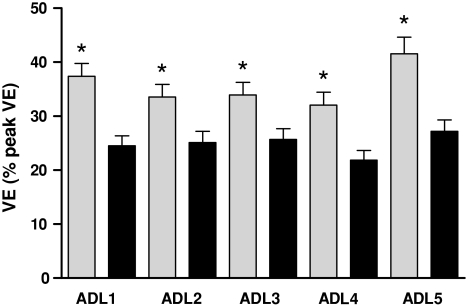
Patients with CHF performed ADLs 1, 2, 4 and 5 at a higher proportion of their peak oxygen uptake than healthy peers: ADL1 [13.4% (5.7, 21.1), p = 0.0011]; ADL2 [7.6% (0.0, 15.1), p = 0.05]; ADL4 [9.2% (2.4, 15.9), p = 0.01]; and ADL5 [13.8% (5.1, 22.6), p = 0.003], while task-related oxygen uptake for ADL3 tended to be higher [7.4% (−0.2, 14.9), p = 0.055, Fig. 1b]. In accordance, the task-related heart rate and ventilation were significantly higher for all time points (p < 0.01, Figs. 2, 3).
Fig. 2.
Heart rate during domestic activities of daily life in patients with CHF and healthy subjects. Mean ± SEM task-related heart rate (HR, percent peak heart rate measured during CPET, % peak HR) during the performance of five domestic activities of daily life (ADL 1–5) in patients with chronic heart failure (n = 23, grey bars) and healthy subjects (n = 20, black bars). *p < 0.05 versus healthy subjects
Fig. 3.
Ventilation during domestic activities of daily life in patients with CHF and healthy subjects. Mean ± SEM task-related ventilation (VE, percent peak ventilation measured during CPET, % peak VE) during the performance of five domestic activities of daily life (ADL 1–5) in patients with chronic heart failure (n = 23, grey bars) and healthy subjects (n = 20, black bars). *p < 0.05 versus healthy subjects
Differences in task-related oxygen uptake (expressed as proportion of the peak aerobic capacity) between CHF patients and the healthy subjects remained after exclusion of 4 CHF patients with COPD: ADL1 [13.6% (5.5, 21.6), p = 0.0016]; ADL4 [9.2% (2.2, 16.1), p = 0.0115]; and ADL5 [14.6% (5.2, 24.0), p = 0.0033]. Task-related oxygen uptake for ADL2 [7.5% (−0.4, 15.4), p = 0.06] and ADL3 [7.2% (−0.6, 15.0), p = 0.07] tended to be higher in the CHF patients without COPD compared to healthy age-matched subjects.
Borg symptom scores
Even though Borg symptom scores for dyspnoea and fatigue at the end of all ADLs were significantly higher in patients with CHF compared to healthy peers (p < 0.01), patients’ task-related symptom scores were quite low (Table 2).
Table 2.
Task-related Borg symptom scores for CHF patients and age-matched healthy subjects
| CHF (n = 23) | Healthy (n = 20) | p-Value | |
|---|---|---|---|
| Borg dyspnea scores (points) | |||
| ADL1 | 0.9 ± 0.2 (range 0–4) | 0.0 ± 0.0 (range 0–0) | 0.001 |
| ADL2 | 1.0 ± 0.2 (range 0–4) | 0.0 ± 0.0 (range 0–0.5) | 0.001 |
| ADL3 | 1.2 ± 0.3 (range 0–5) | 0.0 ± 0.0 (range 0–0) | 0.001 |
| ADL4 | 1.1 ± 0.3 (range: 0–5) | 0.0 ± 0.0 (range 0–0) | 0.001 |
| ADL5 | 2.0 ± 0.3 (range 0–5) | 0.1 ± 0.1 (range 0–1) | 0.001 |
| Borg fatigue scores (points) | |||
| ADL1 | 0.5 ± 0.2 (range 0–3) | 0.0 ± 0.0 (range 0–0.5) | 0.019 |
| ADL2 | 0.5 ± 0.2 (range 0–3) | 0.0 ± 0.0 (range 0–0) | 0.017 |
| ADL3 | 0.5 ± 0.2 (range 0–3) | 0.0 ± 0.0 (range 0–0) | 0.012 |
| ADL4 | 0.7 ± 0.2 (range 0–4) | 0.0 ± 0.0 (range 0–0) | 0.008 |
| ADL5 | 1.1 ± 0.3 (range 0–3) | 0.1 ± 0.1 (range 0–1) | 0.001 |
Results are presented as mean ± standard error of the mean (range)
Discussion
The present study is the first to report detailed information about the metabolic requirement of five simple self-paced domestic ADLs in patients with CHF. Despite optimal cardiac drug treatment, patients with CHF performing simple self-paced domestic ADLs consumed oxygen at a higher proportion to their peak oxygen uptake than healthy elderly subjects. Moreover, patients with CHF had significantly higher Borg symptom scores for dyspnoea and fatigue after each domestic ADL.
Metabolic requirement of simple domestic ADLs
Even though the task-related oxygen uptake (ml/min and ml/kg/min) was similar or even a little bit lower in patients with CHF compared to healthy age-matched subjects, the relative metabolic requirement was clearly higher in patients. Indeed, a significantly lower peak oxygen uptake obtained during CPET in patients with CHF is most probably the main reason for this finding.
So, the performance of five simple domestic ADLs is laying a relatively moderate-to-high claim to the impaired peak aerobic capacity of patients with CHF (Fig. 1b). To our surprise, putting on two socks, two shoes and a vest resulted in a mean task-related oxygen uptake of 49% of the peak oxygen uptake obtained during CPET, while sweeping the floor for 4 min resulted in a mean task-related oxygen uptake of 52% of the peak oxygen uptake obtained during CPET. Indeed, many physical exercise training programs in CHF are initially performed at a training intensity of 50–60% of peak oxygen uptake obtained during CPET (Barnard et al. 2000; Delagardelle et al. 2002; Feiereisen et al. 2007). These findings may, at least in part, explain the daily experience of symptoms of dyspnoea and fatigue that patients with CHF frequently report (Raphael et al. 2007). Indeed, the relative requirement on the impaired cardiopulmonary system is clearly higher than in healthy peers (Figs. 1b, 2, 3).
Interestingly, patients with COPD also used about 50% of the peak aerobic capacity during sweeping the floor for 5 min (Velloso et al. 2003). So, patients with chronic organ failure seem to have comparable metabolic requirements to execute simple domestic ADLs, irrespective of the type of primary organ failure. This may not come as a complete surprise. Indeed, similarities between patients with CHF or COPD were reported for body composition, muscle strength and endurance of the upper and lower limbs, self-reported physical activity levels and peak aerobic capacity (Franssen et al. 2002; Gosker et al. 2003).
The extent to which improvements in peak aerobic capacity following an exercise-based CHF rehabilitation program (Rees et al. 2004) may improve the performance of domestic ADLs and decrease symptom scores in patients with CHF remains uncertain and warrants additional research. Indeed, it seems reasonable to postulate that an improved peak aerobic capacity can at least in part reduce the relatively high metabolic requirement on the impaired cardiopulmonary system in CHF.
Methodological considerations
The external validity of the present findings is limited to CHF patients with NYHA II and III. Thus, the present data should not be uncritically applied to NYHA I and IV patient subsets. Moreover, the authors a priori choose to assess the metabolic requirement of five simple domestic ADLs, specifically excluding relevant daily physical activities like walking. In fact, the relatively high metabolic requirement of walking has already been studied in CHF (Kervio et al. 2004).
The extent to which task-related oxygen uptake will change by altering the order of the tested five domestic ADLs remains uncertain. Surprisingly, Borg symptom scores for dyspnea and fatigue were rather low after each domestic ADL, which suggests that the tested ADLs were not ADLs that the patients found particularly troublesome. These results suggest that patients with CHF may adjust their activity level such that with a relatively higher strain they reach rather low symptom scores. In addition, it may also be an indication that any individual ADL task in isolation does not create symptoms. It will therefore be important in future studies to assess the specific ADL tasks which patients find particularly troubling as well as the effects of a combination of tasks in various orders of succession. Certainly, this may be challenging, as the variability in ADL tasks that individuals find troubling is likely to be wide (Raphael et al. 2007). Nonetheless, such detailed examination of the effects of ADLs will potentially lead to a better understanding of what makes ADL tasks troubling in CHF and the further development of known interventional strategies, like comprehensive patient-tailored rehabilitation programs. For daily clinical routine, validated questionnaires and/or semi-structured interviews are suitable to identify problematic ADLs in patients with CHF (Raphael et al. 2007; Sewell and Singh 2001).
Unfortunately, the degree of task-related hyperventilation (reflected by the slope of increase of ventilation relative to carbon dioxide production) remains unknown. In fact, the portable system used to assess task-related metabolic requirements provides reliable measurement of task-related oxygen uptake and ventilation, but is less reliable for measuring carbon dioxide production (Diaz et al. 2008). Moreover, the ventilatory threshold has been widely applied in patients with CHF. Nevertheless, significant error in interpreting the ventilatory threshold in CHF patients will occur even with experienced reviewers (Myers et al. 2010). Therefore, future studies may want to consider the assessment of (arterial) lactate to determine inadequate oxygen supply to the mitochondria during simple ADLs (Wasserman et al. 1990).
The increased physiologic strain in patients with CHF may be due to the presence of COPD (Dickstein et al. 2008; Norberg et al. 2008). Indeed, 17% of the current CHF patients have COPD, which is in line with previous studies (Le Jemtel et al. 2007). Nevertheless, differences in task-related oxygen uptake between CHF patients and healthy subjects remained after exclusion of CHF patients with COPD. Finally, the current findings need to be interpreted in the light of the number of comparisons/correlations that were made in the present study (Perneger 1998). However, multiple findings in the same direction, rather than a single ‘statistically significant’ result, suggest that these are not due to chance alone.
To conclude, patients with CHF experience a relative metabolic requirement during the performance of self-paced domestic ADLs that is not similar that seen in their healthy peers. These findings may not be extraordinary, but are novel and represent a necessary step in improving our understanding of what troubles patients the most—not being able to do the things that they could when they were healthy. Building upon our current findings and carrying out more detailed descriptive studies as well as interventional studies including studying the effects of exercise-based rehabilitation programs [using interval type of training (Meyer et al. 1998)] and/or patient-tailored occupation therapy [using energy-conservation techniques (Velloso and Jardim 2006)] will certainly be worthwhile endeavours and may get us to the heart of the matter.
Ethical standards: The present study complies with the current laws of the Netherlands. The institutional review board of the Maastricht University Medical Centre (MEC08-3-032) approved this study. All tests were performed at the CIRO+ and were in accordance with the World Medical Association declaration of Helsinki.
Acknowledgments
The authors want to acknowledge the patients with CHF and the healthy subjects who volunteered to participate in the present study. Moreover, the authors are grateful to Martijn Cuijpers, Lucie Fransen, Rob Op ‘t Veld, Marco Schipper, Marco Akkermans, Jos Peeters, Annie van de Kruijs, and Irma Timmermans for planning all tests and/or gathering the data; and to Daisy Janssen and Miriam Groenen for statistical advise.
Conflict of interest
The authors state to have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O’Brien WL, Bassett DR, Jr, Schmitz KH, Emplaincourt PO, Jacobs DR, Jr, Leon AS. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32:S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- American Thoracic Society; American College of Chest Physicians (2003) ATS/ACCP Statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med 167:211–277 [DOI] [PubMed]
- Barnard KL, Adams KJ, Swank AM, Kaelin M, Kushnik MR, Denny DM. Combined high-intensity strength and aerobic training in patients with congestive heart failure. J Strength cond res. 2000;14:383–388. [Google Scholar]
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Delagardelle C, Feiereisen P, Autier P, Shita R, Krecke R, Beissel J. Strength/endurance training versus endurance training in congestive heart failure. Med Sci Sports Exerc. 2002;34:1868–1872. doi: 10.1097/00005768-200212000-00002. [DOI] [PubMed] [Google Scholar]
- Diaz V, Benito PJ, Peinado AB, Alvarez M, Martin C, Di Salvo V, Pigozzi F, Maffulli N, Calderon FJ. Validation of a new portable metabolic system during an incremental running test. J Sports Sci Med. 2008;7:532–536. [PMC free article] [PubMed] [Google Scholar]
- Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, Stromberg A, van Veldhuisen DJ, Atar D, Hoes AW, Keren A, Mebazaa A, Nieminen M, Priori SG, Swedberg K, Vahanian A, Camm J, De Caterina R, Dean V, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the task force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM) Eur Heart J. 2008;29:2388–2442. doi: 10.1093/eurheartj/ehn309. [DOI] [PubMed] [Google Scholar]
- Feiereisen P, Delagardelle C, Vaillant M, Lasar Y, Beissel J. Is strength training the more efficient training modality in chronic heart failure? Med Sci Sports Exerc. 2007;39:1910–1917. doi: 10.1249/mss.0b013e31814fb545. [DOI] [PubMed] [Google Scholar]
- Franssen FM, Wouters EF, Schols AM. The contribution of starvation, deconditioning and ageing to the observed alterations in peripheral skeletal muscle in chronic organ diseases. Clin Nutr. 2002;21:1–14. doi: 10.1054/clnu.2001.0485. [DOI] [PubMed] [Google Scholar]
- Gosker HR, Lencer NH, Franssen FM, van der Vusse GJ, Wouters EF, Schols AM. Striking similarities in systemic factors contributing to decreased exercise capacity in patients with severe chronic heart failure or COPD. Chest. 2003;123:1416–1424. doi: 10.1378/chest.123.5.1416. [DOI] [PubMed] [Google Scholar]
- Kervio G, Ville NS, Leclercq C, Daubert JC, Carre F. Intensity and daily reliability of the six-minute walk test in moderate chronic heart failure patients. Arch Phys Med Rehabil. 2004;85:1513–1518. doi: 10.1016/j.apmr.2003.09.035. [DOI] [PubMed] [Google Scholar]
- Le Jemtel TH, Padeletti M, Jelic S. Diagnostic and therapeutic challenges in patients with coexistent chronic obstructive pulmonary disease and chronic heart failure. J Am Coll Cardiol. 2007;49:171–180. doi: 10.1016/j.jacc.2006.08.046. [DOI] [PubMed] [Google Scholar]
- Meyer K, Foster C, Georgakopoulos N, Hajric R, Westbrook S, Ellestad A, Tilman K, Fitzgerald D, Young H, Weinstein H, Roskamm H. Comparison of left ventricular function during interval versus steady-state exercise training in patients with chronic congestive heart failure. Am J Cardiol. 1998;82:1382–1387. doi: 10.1016/S0002-9149(98)00646-8. [DOI] [PubMed] [Google Scholar]
- Mezzani A, Corra U, Baroffio C, Bosimini E, Giannuzzi P. Habitual activities and peak aerobic capacity in patients with asymptomatic and symptomatic left ventricular dysfunction. Chest. 2000;117:1291–1299. doi: 10.1378/chest.117.5.1291. [DOI] [PubMed] [Google Scholar]
- Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P, Jensen R, Johnson DC, MacIntyre N, McKay R, Navajas D, Pedersen OF, Pellegrino R, Viegi G, Wanger J. Standardisation of spirometry. Eur Respir J. 2005;26:319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- Myers J, Goldsmith RL, Keteyian SJ, Brawner CA, Brazil DA, Aldred H, Ehrman JK, Burkhoff D. The ventilatory anaerobic threshold in heart failure: a multicenter evaluation of reliability. J Card Fail. 2010;16:76–83. doi: 10.1016/j.cardfail.2009.08.009. [DOI] [PubMed] [Google Scholar]
- Norberg EB, Boman K, Lofgren B. Activities of daily living for old persons in primary health care with chronic heart failure. Scand J Caring Sci. 2008;22:203–210. doi: 10.1111/j.1471-6712.2007.00514.x. [DOI] [PubMed] [Google Scholar]
- Perneger TV. What’s wrong with Bonferroni adjustments. Bmj. 1998;316:1236–1238. doi: 10.1136/bmj.316.7139.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raphael C, Briscoe C, Davies J, Ian Whinnett Z, Manisty C, Sutton R, Mayet J, Francis DP. Limitations of the New York Heart Association functional classification system and self-reported walking distances in chronic heart failure. Heart. 2007;93:476–482. doi: 10.1136/hrt.2006.089656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rees K, Taylor RS, Singh S, Coats AJ, Ebrahim S (2004) Exercise based rehabilitation for heart failure. Cochrane Database Syst Rev: CD003331 [DOI] [PMC free article] [PubMed]
- Sewell L, Singh SJ. The Canadian occupational performance measure: is it a reliable measure in clients with chronic obstructive pulmonary disease? Br J Occup Ther. 2001;64:305–310. [Google Scholar]
- Sillen MJ, Janssen PP, Akkermans MA, Wouters EF, Spruit MA. The metabolic response during resistance training and neuromuscular electrical stimulation (NMES) in patients with COPD, a pilot study. Respir Med. 2008;102:786–789. doi: 10.1016/j.rmed.2008.01.013. [DOI] [PubMed] [Google Scholar]
- Sillen MJ, Wouters EF, Franssen FM, Meijer K, Stakenborg KH, Spruit MA (2010) Oxygen uptake, ventilation, and symptoms during low-frequency versus high-frequency NMES in COPD: a pilot study. Lung [Epub ahead of print] [DOI] [PubMed]
- Spruit MA, Pennings HJ, Janssen PP, Does JD, Scroyen S, Akkermans MA, Mostert R, Wouters EF. Extra-pulmonary features in COPD patients entering rehabilitation after stratification for MRC dyspnea grade. Respir Med. 2007;101:2454–2463. doi: 10.1016/j.rmed.2007.07.003. [DOI] [PubMed] [Google Scholar]
- van den Berg-Emons RJ, Bussmann JB, Balk AH, Stam HJ. Factors associated with the level of movement-related everyday activity and quality of life in people with chronic heart failure. Phys Ther. 2005;85(12):1340–1348. [PubMed] [Google Scholar]
- Velloso M, Jardim JR. Study of energy expenditure during activities of daily living using and not using body position recommended by energy conservation techniques in patients With COPD. Chest. 2006;130:126–132. doi: 10.1378/chest.130.1.126. [DOI] [PubMed] [Google Scholar]
- Velloso M, Stella SG, Cendon S, Silva AC, Jardim JR. Metabolic and ventilatory parameters of four activities of daily living accomplished with arms in COPD patients. Chest. 2003;123:1047–1053. doi: 10.1378/chest.123.4.1047. [DOI] [PubMed] [Google Scholar]
- Wasserman K, Beaver WL, Whipp BJ. Gas exchange theory and the lactic acidosis (anaerobic) threshold. Circulation. 1990;81:II14–II30. [PubMed] [Google Scholar]
- World Medical Association General Assembly (2004) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Int Bioethique 15:124–129 [PubMed]