Abstract
The public’s level of mental health literacy remains low, despite growing access to information regarding mental illnesses. Because few measures exist to assess the level of knowledge of mental illnesses in lay samples, the Multiple-Choice Knowledge of Mental Illnesses Test (MC-KOMIT) was developed, initially for use in a study involving police officers, some of whom received 40 hours of training focused on recognizing mental illnesses, using verbal de-escalation techniques, and making mental health referrals when appropriate. This report details the initial development of the 100 questions in the item bank and the eventual selection of the final 33 items that were retained. For these 33 items, internal consistency was demonstrated, and test-retest reliability was examined among officers who completed the test on Monday morning and again on Friday afternoon. Construct validity was examined by three hypothesis tests: the MC-KOMIT was sensitive to change related to the educational intervention, scores were significantly correlated with years of educational attainment, and officers reporting past or current treatment for a mental health problem scored higher than those without such a history. This initial report suggests that the MC-KOMIT may be useful in quantifying knowledge of mental illnesses in police officers and other diverse lay samples.
Keywords: Item analysis, Knowledge, Mental health literacy, Mental illnesses, Reliability, Validity
1. Introduction
At a time when there is an unprecedented volume of information in the public domain, the level of knowledge about mental illnesses (sometimes called ‘mental health literacy’) is meager (Crisp et al., 2005). Mental health literacy encompasses an individual’s knowledge and beliefs about mental illnesses, which aid in their recognition, management, or prevention (Jorm et al., 1997a). Mental health literacy consists of several components, including: (a) the ability to recognize specific disorders or different types of psychological distress; (b) knowledge and beliefs about risk factors and causes, (c) knowledge and beliefs about self-help interventions, (d) knowledge and beliefs about professional help available, (e) attitudes that facilitate recognition and appropriate help-seeking, and (f) knowledge of how to seek mental health information (Jorm et al., 2006). It is assumed that people with greater mental health literacy should be able to recognize discrete mental disorders, name their causes and risk factors, know where to seek relevant help and information, and appreciate that they are illnesses that can be treated (Dunn et al., 2009). Discouragingly, however, research has shown that most people in the general public cannot accurately label common mental disorders (Jorm et al., 1997a; Lauber et al., 2003).
Thus, knowledge of mental illnesses is an important variable that may be applicable to many areas of investigation. Examples of the multitude of research questions that might seek to quantify the knowledge of mental illnesses construct include: “Is a primary care provider’s level of knowledge of mental illnesses related to improved quality of care for patients?”, “Is a mental health service user’s willingness to adhere to treatment associated with greater knowledge of mental illnesses?”, and “Does the public’s extent of knowledge of mental illnesses play an influential role in shaping attitudes and perceptions about people diagnosed with a mental illness, contributing to avoidance and social distance?” Additionally, researchers may seek to answer, “Does knowledge of mental illnesses among police officers partly determine the ways they interact with persons with a mental illness during their patrol and response duties?”
Despite the potential relevance of knowledge of mental illnesses as a research construct, remarkably few instruments have been developed to measure this domain of knowledge. Although very few instruments measure lay samples’ knowledge about mental illnesses broadly, several scales have been constructed specifically to assess Alzheimer’s disease knowledge in the general public; knowledge of anxiety and depression among health care providers; and knowledge of schizophrenia among family members, caregivers, and others; several of these are very briefly reviewed here. First, Blay and Peluso (2008) used a face-to-face interview administered by trained professionals to assess knowledge and perceptions of Alzheimer’s disease in the lay public. As part of the assessment, a written vignette was provided, with open-ended questions examining identification of the illness, and follow-up questions assessing causal beliefs of the identified illness using a 5-point Likert scale. Second, to measure clinical knowledge about the recognition, diagnosis, and management of anxiety disorders and depression, McCall and colleagues (2004) developed a 24-item multiple choice and true/false knowledge questionnaire, which reflected the content of a continuing medical education course. Twelve of the items, limited to depression, had previously been developed and used by Blashki (2003). Third, Dunn et al. (2009) created a scoring mechanism to allow an overall, general measure of depression-related mental health literacy to be calculated and examined in terms of validity. Fourth, the Knowledge about Schizophrenia Test (KAST), developed by Compton and colleagues (2007), is a multiple-choice test to measure knowledge about schizophrenia among family members of patients, lay community members, and police officers participating in Crisis Intervention Team (CIT) training (Compton et al., 2006).
Because so few measures exist to assess knowledge of mental illnesses among lay samples in general, the Multiple-Choice Knowledge of Mental Illnesses Test (MC-KOMIT) was constructed. This report describes the development, item analysis, and final item selection of the MC-KOMIT, which was designed for use in a study involving police officers, some of whom received a specialized, 40-hour training on mental illnesses and how best to respond to individuals with mental illnesses during crisis situations. Initial testing of reliability (internal consistency and test-retest stability) and construct validity in a sample of police officers is provided.
2. Methods
2.1. Initial development of the 100 questions in the item bank
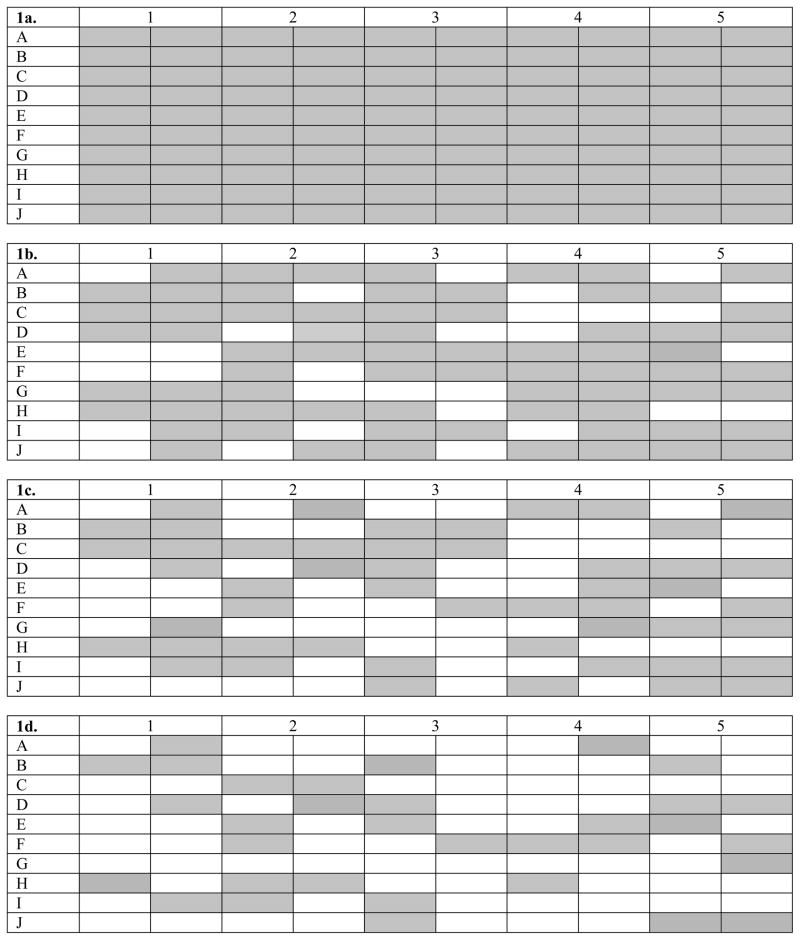
as further reduced from 70 to 50. Again, items were deleted in a systematic way, this time informed by item analyses of responses among these participants. Figure 1c shows the coverage matrix for the resultant 50-item bank that would then be administered to all other participants.
Figure 1. Coverage Matrices.
1a, the fully saturated initial coverage matrix depicting the 100 items (shaded cells) in the original item bank; 1b., coverage matrix after initial removal of 30 items; 1d., coverage matrix after removal of an additional 20 items; 1d., coverage matrix of the final 33-item MC-KOMIT selected through detailed item analysis.
2.2. Setting, sample, and general procedures
Data for further item analysis and psychometric assessment of the MC-KOMIT were collected from officers in non-CIT (n=125) and CIT classes (n=74) from several jurisdictions in Georgia. The non-CIT police officers were in week-long training classes on topics that included sexual assault, domestic violence, and management/supervision at the Georgia Public Safety Training Center. The CIT officers were in week-long classes that provide select officers with specialized training on recognizing mental illnesses, addictive disorders, and developmental disorders; verbally de-escalating crisis situations involving individuals with such disorders; and referring subjects to mental health services rather than arrest/incarceration, when appropriate (Bahora et al., 2008; Compton & Chien, 2008; Oliva & Compton, 2008; Compton et al., 2010). The MC-KOMIT was administered on Monday mornings and Friday afternoons for both types of class participants. For 53 participating non-CIT officers, matching data were available from both the Monday and Friday administration times; and CIT officers completed the test at the beginning and end of their specialized training. All participants provided written informed consent, and all study procedures were approved by the university’s institutional review board.
2.3. Data analyses
After the final item bank of 50 questions had been derived, item analyses were conducted in three steps. First, items with a corrected point-biserial correlation of <0.13 were omitted. This value can range from −1 to +1 and indicates the correlation between that item (correct/incorrect) and the total score of the test, when the total score is derived excluding that item (thus, it is “corrected”). Second, items that had more than one distractor breaking the “2% rule” (identifying problematic distractors that were selected by ≤2% of the sample, meaning that very few participants deemed it to be a plausible answer choice) were removed. Third, items with a proportion correct value of <0.20 or >0.80, indicating that the items were too difficulty or too easy, respectively, were removed. The proportion correct is simply the proportion getting the item correct, and is a measure of item difficulty, ranging from 0 to 1.
Internal consistency reliability of the final test was assessed with the Kuder-Richardson formula 20 (KR-20) reliability coefficient for dichotomous items (Streiner & Norman, 2001; Streiner, 2003). As is true for Cronbach’s alpha, values typically range from 0 to 1, and the preferred value for the KR-20 is usually considered to be >0.70. The KR-20 can be thought of as the mean of all possible split-half reliabilities. The internal consistency was computed for all officers on both their Monday morning and Friday afternoon test administrations. Additionally, scores from non-CIT officers and those undergoing CIT training were examined separately for each test administration. Test-retest reliability was assessed by calculating a Pearson correlation coefficient for scores from 50 non-CIT officers who completed the MC-KOMIT on the Monday morning and Friday afternoon of their training week, which did not pertain to mental health.
Construct validity was assessed using three hypothesis tests. First, sensitivity to change through an educational intervention (CIT training) was tested using a paired samples t-test among officers at the beginning and end of their CIT training week. Second, an association between knowledge test scores and years of educational attainment was examined. Third, construct validity was further tested with an independent samples t-test using the “known groups” approach based on the hypothesis that officers reporting a personal history of psychiatric treatment would have higher MC-KOMIT scores than those without a history of treatment. To address this, we asked participants, “Have you ever received, or are you currently receiving, treatment for a mental health problem (such as therapy, counseling, or medicine for mental or emotional problems)?” as part of the demographics questionnaire. The SPSS 16.0 statistical software package was used for all descriptive statistics, reliability assessments, and validity tests.
3. Results
3.1. Study sample
Basic demographic characteristics of the study sample are shown in Table 1. The mean age of participants was 38.3±8.4 years, and the average years of education completed was 13.9±1.7 years. As expected, the majority of participants were non-Hispanic, White/Caucasian males. Two thirds (131, 66.5%) were married or living with a partner, and over half (113, 57.4%) reported a total annual income for everyone in their household last year of >$60,000.
Table 1.
Basic Sociodemographic Characteristics of the Study Sample (n=199)
| Age, years (range, 21–66) | 38.3±8.4 |
|
| |
| Educational attainment, years (range, 10–18) | 13.9±1.7 |
|
| |
| Gender, male (n=197) | 162 (82.2%) |
|
| |
| Ethnicity, non-Hispanic (n=194) | 187 (96.4%) |
|
| |
| Race (n=196) | |
| White/Caucasian | 134 (68.4%) |
| Black/African American | 54 (27.6%) |
| American Indian or Alaska Native | 2 (1.0%) |
| Asian | 1 (0.5%) |
| Other | 5 (2.6%) |
|
| |
| Relationship status (n=197) | |
| Married or living with a partner | 131 (66.5%) |
| Separated or divorced | 38 (19.3%) |
| Single and never married | 28 (14.2%) |
|
| |
| Last year’s total annual income for everyone in the household (n=197) | |
| <$40,000 | 40 (20.3%) |
| $40,001–$60,000 | 44 (22.3%) |
| >$60,000 | 113 (57.4%) |
3.2. Item analysis and derivation of the 33-item MC-KOMIT
Analysis of the 50 items completed by the overall sample (n=199) was conducted in three steps as outlined above. Ten items were removed due to a low point-biserial correlation and two items were deleted because more than one distractor broke the 2% rule. A number of other items were de-selected because they met more than one of the criteria for removal; two items were removed because they had a point-biserial correlation of <0.13 and an unacceptable proportion correct value; one was removed because it broke the 2% rule and had an unacceptable proportion correct value; another item was removed because it broke the 2% rule and had a point-biserial correlation of <0.13; and another item was de-selected because it met all three criteria for removal. Thus, the final version of the MC-KOMIT included 33 items (shown in the Appendix) with good item performance based on these criteria. Figure 1d shows the coverage matrix for the final 33 items, which reveals a good range of content areas, content domains, and taxonomy types.
3.3. Test score description, internal consistency reliability, and test-retest reliability
Mean 33-item MC-KOMIT scores are shown in Table 2. These scores were derived by simple summation of the 33 items, where each correct item counts as one point. When respondents skipped one or two items (e.g., 15 of 199 officers (7.5%) in the Monday morning test administrations), those items were considered incorrect in the calculation of the score. In cases in which more than two items were skipped (e.g., 10 of 199 officers (5.0%) in the Monday morning test administrations), a score was not computed as this was often due to the officer not completing the test or skipping an entire page of the test.
Table 2.
Mean (±Standard Deviation) 33-item MC-KOMIT Scores
| Monday morning assessment | 18.7±5.0 |
| Officers in CIT training | 18.7±5.0 |
| Non-CIT officers | 18.6±5.2 |
|
| |
| Friday afternoon assessment | 19.1±5.2 |
| Officers in CIT training | 20.8±5.2 |
| Non-CIT officers | 17.3±4.8 |
Across all four administrations, the test appeared to perform well, with no obvious floor or ceiling effects. KR-20 statistics were 0.72 and 0.73 for all participants completing the test on Mondays and Fridays, respectively. When non-CIT officers and officers in CIT training were examined separately, these values were 0.74 and 0.73, respectively, for the Monday morning administration and 0.68 and 0.75, respectively, for the Friday afternoon administration.
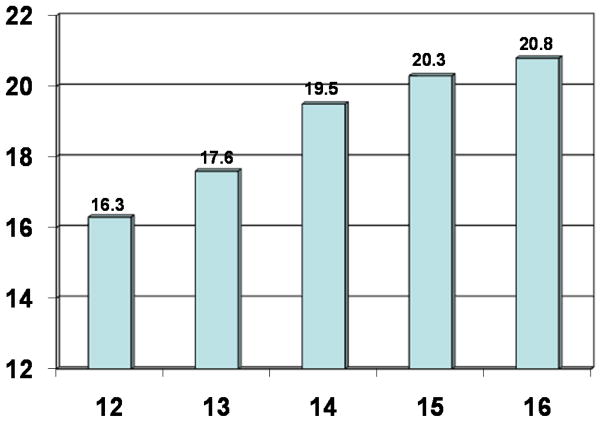
Test-retest reliability was examined among 53 non-CIT officers who completed the MC-KOMIT on the Monday morning and Friday afternoon of their non-mental health training week. The Pearson correlation coefficient was 0.79 (P<0.001). The scatter plot illustrating this correlation is shown in Figure 2.
Figure 2. Scatter Plot Depicting the Test-Retest Reliability of the 33-item MC-KOMIT among 53 Police Officers Completing the Test on Monday Morning and Friday Afternoon.
Dark circles represent overlapping observations.
3.4. Validity
Construct validity was first tested by examining mean MC-KOMIT scores of police officers at the beginning and the end of their CIT training week, to demonstrate sensitivity to change. Among 68 participants with available data at both time points, the mean MC-KOMIT score among officers at the beginning of the training week was 18.6±5.2, compared to 20.8±5.2 at the end of the training week (paired samples t=4.24, df=67, P<0.001), representing a mean difference of 2.2. Thus, the test is sensitive to change after an intervention designed to convey knowledge of mental illnesses.
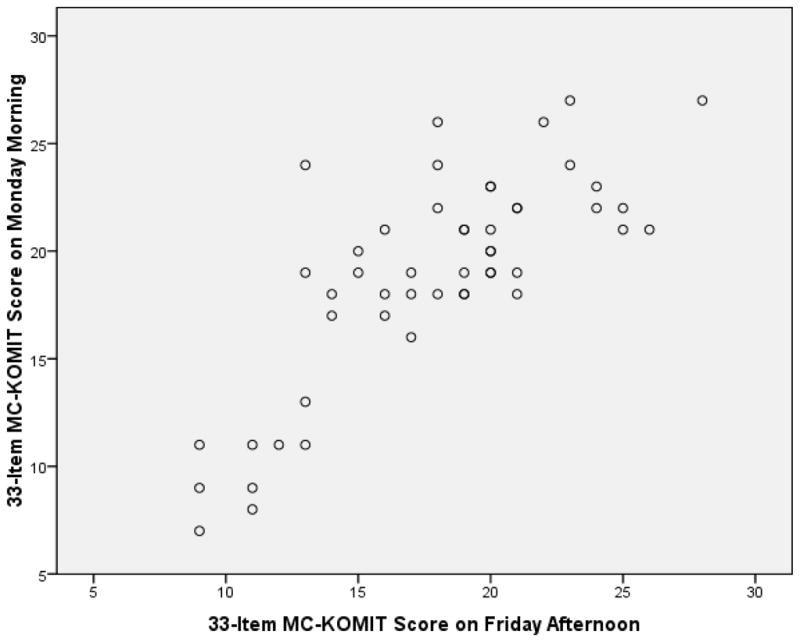
Second, Monday morning MC-KOMIT scores were significantly correlated with years of educational attainment (ρ=0.35, P<0.001). This is depicted graphically in Figure 3, which shows mean MC-KOMIT scores by 12–16 years of educational attainment. A third test of construct validity was conducted using the known-groups approach in which officers who reported having received past or current treatment for a mental health problem were compared to those not endorsing this item. The 15 officers with a history of treatment had a mean score of 22.5±3.4, compared to 18.3±5.0 among the 172 officers without a history of treatment (t=3.19, df=185, P=0.002).
Figure 3.
Mean 33-item MC-KOMIT Scores (Vertical Axis) by Years of Educational Attainment (Horizontal Axis)
4. Discussion
Knowledge of mental illnesses can be measured efficiently with a brief, self-administered, multiple-choice test. This study provides initial support for the psychometric properties of the MC-KOMIT, which appears to have utility among law enforcement officers. Such a knowledge test may also be applicable in studies measuring knowledge in other lay samples in which a high level of variability in knowledge is expected. Starting with an initial item bank of 100 questions, the item bank was narrowed to 70 items and then 50 items. In-depth item analysis of these 50 items resulted in the derivation of the final 33-item instrument. Scores from the 33-item MC-KOMIT were demonstrated to have acceptable internal consistency reliability, test-retest stability, and construct validity, the latter being assessed through three hypothesis tests.
The development and initial testing of the MC-KOMIT demonstrates that the knowledge of mental illnesses construct can be efficiently measured with a brief, self-administered, multiple-choice test in settings outside of the formal mental health system. The need for the public to have greater mental health literacy is highlighted by the remarkably high lifetime prevalence of mental disorders (up to 50%, according to Kessler et al., 1994) and the great number of individuals who are indirectly affected. The field of psychiatric research may make use of such a measure in addressing diverse research questions, beyond the initial use of the MC-KOMIT in a study of police officers engaged in specialized mental health training. Several examples can be given to illustrate this potential as a variable of interest. First, knowledge tests may be useful in studies involving caregivers, who oftentimes do not possess the knowledge needed to adequately care for a loved one with a mental illness. Studies show that families routinely request information on basic facts about mental illnesses and their treatments, behavior management skills, and the mental health system in order to better cope with their relatives’ illnesses (Mueser et al., 1992; Ascher-Svanum et al., 1997; Gasque-Carter and Curlee, 1999). Second, among society at large, having basic knowledge of mental illnesses, before any personal or family encounter with a mental illness, would potentially be beneficial. One consequence of poor mental health literacy is that the bulk of the intervening around mental disorders is largely confined to professionals. However, the prevalence of mental disorders is so high that the mental health workforce cannot adequately serve everyone affected, and therefore mental health professionals tend to focus on those with more serious and chronic problems (Jorm, 2000). Third, there is a significant problem of non-detection of prevalent mental illnesses in primary care settings; many individuals with psychiatric disorders are either undiagnosed or misdiagnosed and therefore inadequately treated (Freeman, 1992).
Measuring the knowledge of mental illnesses variable may also be crucial in research on stigma and related attitudes and perceptions. It is thought that an individual’s knowledge of mental illnesses may play a major role in shaping attitudes and perceptions about people diagnosed with such disorders, and that a lack of knowledge could contribute to avoidance and social distance stigma (Esterberg et al., 2008), as well as impede early recognition and appropriate help-seeking behaviors (Jorm, 2000; Jorm et al., 1997a; Jorm et al., 1997b). Somewhat similar to the knowledge of mental illnesses construct, perceptions of illness are highly relevant to psychological and social research. In being faced with a situation such as the experience of an unusual symptom, or the provision of a diagnosis from a doctor, individuals will construct their own representation which, in turn, will determine their behavior and other responses, including help-seeking and medicine-taking (Weinman & Petrie, 1997).
Several methodological limitations of this study should be recognized. First, although the MC-KOMIT is likely to be useful in research involving diverse lay samples (e.g., the general public), the present item analysis and psychometric testing was conducted specifically with police officers by virtue of the investigative team’s ongoing research. When used with other samples, reliability and validity should be re-assessed. Second, in assessing construct validity, one approach was to demonstrate sensitivity to change after an educational intervention; yet, the mean difference in scores before and after CIT training was only 2.2 points, which is arguably a relatively small change. This is likely driven by the fact that the week-long CIT training program for police officers focuses not only on conveying knowledge in a didactic format, but more importantly on shifting attitudes through interactions with individuals with mental illnesses and their family members and also on practical de-escalation training that is not tied to specific knowledge of mental illnesses. A third limitation, pertaining to the instrument rather than the study, is that the MC-KOMIT focuses on knowledge of mental illnesses in a broad sense, but in some instance it may be much more appropriate to assess knowledge in specific areas (e.g., pertaining to specific mental illnesses amongst caregivers or primary care practitioners). Knowledge gains in the specific areas of a curriculum’s objectives—rather than using an all-purpose knowledge test—would also be more appropriate in some instances. In terms of stigma research, although knowledge of mental illnesses in general may be beneficial, it is also conceivable that for some research endeavors the development of instruments focusing on one particular disorder would be more advantageous.
Clearly, there are diverse research questions that may pertain to the construct of knowledge of mental illnesses. Yet, there exists a prominent dearth of established, psychometrically tested instruments to measure this construct. This initial description and analysis of the MC-KOMIT suggests that this and similar carefully constructed multiple-choice knowledge tests may be very useful. Further research is needed in diverse samples.
Acknowledgments
This study was supported by a grant from the National Institute of Mental Health (R01 MH082813) to the first author. The authors greatly appreciate assistance provided by Ms. Letheshia Husbands, Ms. Shaily Krishan, Ms. Harriett Laurence, Ms. Tarianna Stewart, and Ms. Pat Strode in the recruitment of study participants and the collection of data.
Appendix A. Items of the Final, 33-item Version of the MC-KOMIT
Bold font indicates correct responses, and the original numbering system is retained.
E5a. Some people with obsessive-compulsive disorder may benefit from which of the following?
Developing new hobbies
Dietary counseling
Legal restraining orders
Limiting social contacts
Support groups
J5b. A 76-year-old man has mild memory problems, difficulty maintaining his house, and some confusion about what month it is. Which of the following resources may be most beneficial to him?
Assisted living facility
Nursing home
Outpatient psychotherapy
Physical exercise counseling
Rehabilitation hospital
A1b. A 19-year-old begins to hear voices and act paranoid several months after graduating from high school. Which of the following is the most likely cause of these problems?
Excessive worries about other peoples’ intentions
Genetic tendency toward developing an illness
Increasing use of alcohol during adolescence
Not enough support from parents
Stress of graduating from high school
J5a. Which of the following community services is especially important for people with dementia and their families?
Detoxification programs for those with alcohol abuse
Hygiene programs for those with grooming problems
Memory retrieval programs for those with memory loss
Re-orientation programs for those who are disoriented
Safe return programs for those who become lost
D5b. A man is evaluated by a psychiatrist, who tells him that psychotherapy is much more important for his problems than any medications. Which of the following disorders is he most likely being seen for?
Bipolar disorder
Dependent personality disorder
Dyslexia
Heroin withdrawal
Paranoid schizophrenia
B3a. People who have had an episode of major depression are at most risk for which of the following?
Becoming addicted to anti-depressant medicines
Being diagnosed with migraines
Developing schizophrenia
Experiencing flashbacks about their depression
Having another episode of depression
D5a. Psychotherapy may be the most beneficial resource for which of the following conditions?
Alcohol withdrawal
Cognitive disorders
Developmental disorders
Learning disorders
Personality disorders
F2a. Which of the following is a feature of all developmental disabilities?
Difficulties walking
Impairment in daily functioning
Inability to communicate verbally
Mental retardation
Unusual body appearance
H4a. Which of the following is most true of psychiatric medicines for children?
They are helpful for all psychiatric disorders
They are often crushed and mixed in food
They improve some types of symptoms
They require a signature from both parents
They should only be used after puberty
D1b. A woman sees a therapist weekly to work on her maladaptive patterns of behavior which have repeatedly interfered with relationships and work. When stressed out, she becomes very impulsive, feels empty, thinks of suicide, and makes multiple cuts on her forearms. Which of the following most likely contributed to her problems?
A brain infection in childhood
Abusive or neglecting parents
Influence of bad friends in adulthood
Lack of everyday rest and relaxation
Not enough vitamins and minerals in her diet
E2a. Which of the following is a common symptom of obsessive-compulsive disorder?
Fear of social situations
Intrusive thoughts or impulses
Ongoing concern about having a panic attack
Overeating and weight gain
Thinking that others are watching or following
F3b. A woman brings her 16-year-old son to a psychologist for an evaluation of failing grades. In order for the psychologist to ensure that this young man does not have mental retardation, which of the following questions is he likely to ask?
Did any of his family members have learning problems?
Do his classmates make fun of him?
Does he also have unusual beliefs?
When did his learning difficulties first begin?
Which class does he currently like the least?
I1b. A 35-year-old woman has been court-ordered to see a psychologist for problems stemming from her alcohol and cocaine use. Which of the following is the psychologist likely to be working to change?
Avoidance
Denial
Pessimism
Violence
Withdrawal
D2b. A woman who has borderline personality disorder frequently becomes suicidal due to an ongoing fear. Which of the following is she most likely subconsciously afraid of?
Abandonment
Being followed
Contamination
Gaining weight
Growing old
E3a. People who have posttraumatic stress disorder are at highest risk for also having which of the following?
Alcohol abuse
Bipolar disorder
Early-onset dementia
Mental retardation
Schizophrenia
F4b. A 13-year-old girl with severe mental retardation has been followed by a child psychiatrist for ten years. She has never taken medications, but the psychiatrist has now decided that a medication may be beneficial. Which of the following is the most likely reason the medication is being prescribed now?
It is now clear that the mental retardation is not getting better without medicine
Medicine may help with problems that are worsening, such as behavior outbursts
School demands are now greater and she will need medicine to help with learning
She is now an adolescent and can take psychiatric medications
The mental retardation has advanced from a moderate to severe level
I2a. Delirium and seizures may occur during withdrawal from heavy, long-term use of which of the following substances?
Alcohol
Inhalants
Marijuana
Mushrooms
Narcotics
A4b. Which of the following is a common reason why a woman with schizophrenia might not regularly take her medicine?
Her anxiety disorder makes her too nervous
She does not recognize that she has an illness
She needs psychotherapy instead of medicine
The medicine is addictive and she is afraid to take it
The pills are very large and hard to swallow
B5a. Most people in treatment for depression are treated by which of the following?
Case managers
Family therapists
Primary care physicians
Psychiatrists in hospitals
The clergy
F4a. Which of the following best describes the treatment approach for developmental disabilities?
Combination of medications to control behavior
Combination of special supports and services
Long-term institutional care
Long-term psychotherapy
Supervision by a life coach
G5b. A mother and father meet with a mental health professional for three sessions over the course of a month after their 25-year-old son committed suicide. Which of the following is the most likely reason for their meetings?
To assess for any mental illnesses
To attempt to determine what the warning signs had been
To begin processing their grief and loss
To determine what could have been done to prevent the suicide
To make a diagnosis of their son’s likely mental illness
H1a. Which of the following is likely a cause of attention-deficit/hyperactivity disorder in children?
An inherited risk
Certain medications
Eating too much sugar
Not getting enough sleep
Poor control over classrooms
J3a. Which of the following is the most common long-term course of dementia?
Improvement
Paralysis
Progression
Remission
Stabilization
B1b. A woman is diagnosed with depression by her doctor during a hospital stay for asthma. Her doctor was most likely prompted to screen for depression because the woman has which of the following?
A long history of smoking cigarettes
Family members with depression
Little improvement from asthma treatment
Poor understanding of her condition
Three children under the age of 18
C2a. Which of the following is a common sign of mania?
Becoming forgetful
Being more talkative than usual
Experiencing repeated flashbacks
Feeling helpless or hopeless
Having anxiety attacks
F5b. A 25-year-old woman receives a number of services through the local mental health system and social agencies, including someone to visit her at home to help with hygiene and cooking, a job coach, a psychiatrist, and a neurologist. Which of the following conditions does she most likely have?
Adjustment disorder
Dementia
Developmental disability
Drug addiction
Personality disorder
H2b. An 8-year-old boy is diagnosed as having depression by a psychiatrist. The psychiatrist tells the boy’s parents that sometimes depression in children appears different from depression in adults. Which of the following is an example of what the psychiatrist is describing?
Having high energy rather than low energy
Hearing voices rather than feeling hopeless
High self-esteem rather than low self-esteem
Homicidal thoughts rather than suicidal thoughts
Irritability rather than feeling depressed
I3a. Which of the following best describes an addiction?
Family members are often unaware that any problem exists
It is a chronic disorder requiring many treatment approaches
It is a short-term behavioral problem usually tied to a major life event
Recovery is rare when a psychiatric disorder is also present
Treatment usually includes a medicine that is taken long-term
B1a. Which of the following is most likely to increase one’s risk for depression?
Being abused as a child
Eating a high-fat diet
Moving to a new residence
Not relaxing enough
Working past the age of 65
C2b. A man at an airport is talking and laughing very loudly, passing out twenty-dollar bills, and telling people he plans to fly around the world to attend sixteen diplomatic meetings. He likely has which of the following?
Alcohol abuse
Delirium
Mania
Obsessions
Pathological lying
D3a. People who have personality disorders usually have these problems during which of the following life stages?
Adolescence and adulthood
After major life events
Childhood and adolescence
Older adulthood
When going through puberty
E4b. A man has been having episodes of chest pain, hyperventilation, and extreme anxiety during the past few months. He is afraid that he will die of a heart attack during one of these episodes. He has seen several doctors, who assure him that his heart is healthy. He now avoids driving because it seems to trigger these attacks. Which of the following treatments would be most helpful?
Counseling
Herbal supplements
Mood stabilizer
Physical therapy
Regular exercise
H2a. Which of the following is a common sign of oppositional defiant disorder in childhood?
Arguing with teachers
Being teased at school
Crying at doctors’ offices
Feeling depressed
Not wanting to get on the school bus
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ascher-Svanum H, Lafuze JE, Barrickman PJ, Van Dusen C, Fompa-Loy J. Educational needs of families of mentally ill adults. Psychiatric Services. 1997;48:1072–1074. doi: 10.1176/ps.48.8.1072. [DOI] [PubMed] [Google Scholar]
- Bahora M, Hanafi S, Chien VH, Compton MT. Preliminary evidence of effects of Crisis Intervention Team training on self-efficacy and social distance. Administration and Policy in Mental Health and Mental Health Services Research. 2008;35:159–167. doi: 10.1007/s10488-007-0153-8. [DOI] [PubMed] [Google Scholar]
- Blashki G. dissertation. Monash University; Melbourne: 2003. A distance education course in depression for general practitioners: a randomised control trial. [Google Scholar]
- Blay SL, Peluso ETP. The public’s ability to recognize Alzheimer disease and their beliefs about its causes. Alzheimer Disease & Associated Disorders. 2008;22:79–85. doi: 10.1097/WAD.0b013e31815ccd47. [DOI] [PubMed] [Google Scholar]
- Compton MT, Chien VH. Factors related to knowledge retention after Crisis Intervention Team (CIT) training for police officers. Psychiatric Services. 2008;59:1049–1051. doi: 10.1176/ps.2008.59.9.1049. [DOI] [PubMed] [Google Scholar]
- Compton MT, Demir Neubert BN, Broussard B, McGriff JA, Morgan R, Oliva JR. Use of force preferences and perceived effectiveness of actions among Crisis Intervention Team (CIT) police officers and non-CIT officers in an escalating psychiatric crisis involving a subject with schizophrenia. Schizophrenia Bulletin. 2010 doi: 10.1093/schbul/sbp146. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton MT, Esterberg ML, McGee R, Kotwicki RJ, Oliva JR. Crisis Intervention Team training: changes in knowledge, attitudes, and stigma related to schizophrenia. Psychiatric Services. 2006;57:1199–1202. doi: 10.1176/ps.2006.57.8.1199. [DOI] [PubMed] [Google Scholar]
- Compton MT, Quintero L, Esterberg ML. Assessing knowledge of schizophrenia: development and psychometric properties of a brief, multiple-choice knowledge test for use across various samples. Psychiatry Research. 2007;151:87–95. doi: 10.1016/j.psychres.2006.05.019. [DOI] [PubMed] [Google Scholar]
- Crisp A, Gelder MG, Goddard E, Meltzer H. Stigmatization of people with mental illnesses: a follow-up study within the changing minds campaign of the royal college of psychiatrists. World Psychiatry. 2005;4:106–113. [PMC free article] [PubMed] [Google Scholar]
- Dunn KI, Goldney RD, Dal Grande E, Taylor A. Quantification and examination of depression-related mental health literacy. Journal of Evaluation in Clinical Practice. 2009;15:650–653. doi: 10.1111/j.1365-2753.2008.01067.x. [DOI] [PubMed] [Google Scholar]
- Esterberg ML, Compton MT, McGee R, Shim R, Hochman K. Knowledge about schizophrenia and social distance toward individuals with schizophrenia: a survey among predominantly low-income, urban, African American community members. Journal of Psychiatric Practice. 2008;14:86–93. doi: 10.1097/01.pra.0000314315.94791.80. [DOI] [PubMed] [Google Scholar]
- Freeman M. Providing mental health care for all in South African – structure and strategy. Centre for the Study of Health Policy, Dept. of Community Health, University of the Witwatersrand; Johannesburg: 1992. [Google Scholar]
- Gasque-Carter OK, Curlee MB. The educational needs of families of mentally ill adults: the South Carolina experience. Psychiatric Services. 1999;50:520–524. doi: 10.1176/ps.50.4.520. [DOI] [PubMed] [Google Scholar]
- Haladyna TM. Developing and Validating Multiple-Choice Test Items. 2. Lawrence Erlbaum Associates, Publishers; Mahwah, New Jersey: 1999. [Google Scholar]
- Jorm AF. Public knowledge and beliefs about mental disorders. British Journal of Psychiatry. 2000;177:396–401. doi: 10.1192/bjp.177.5.396. [DOI] [PubMed] [Google Scholar]
- Jorm AF, Barney LJ, Christensen H, Highet NJ, Kelly CM, Kitchener BA. Research on mental health literacy: what we know and what we still need to know. Australian and New Zealand Journal of Psychiatry. 2006;40:3–5. doi: 10.1080/j.1440-1614.2006.01734.x. [DOI] [PubMed] [Google Scholar]
- Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P. Mental health literacy’: a survey of the public’s ability to recognize mental disorders and their beliefs about the effectiveness of treatment. Medical Journal of Australia. 1997a;166:182–186. doi: 10.5694/j.1326-5377.1997.tb140071.x. [DOI] [PubMed] [Google Scholar]
- Jorm AF, Korten AE, Rodgers B, Pollitt P, Jacomb PA, Christensen H, Jiao Z. Beliefs systems of the general public concerning the appropriate treatments for mental illness. Social Psychiatry and Psychiatric Epidemiology. 1997b;32:468–473. doi: 10.1007/BF00789141. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Archives of General Psychiatry. 1994;1:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Lauber C, Nordt C, Falcato L, Rossler W. Do people recognize mental illness? Factors influencing mental health literacy. European Archives of Psychiatry and Clinical Neuroscience. 2003;253:248–251. doi: 10.1007/s00406-003-0439-0. [DOI] [PubMed] [Google Scholar]
- McCall LM, Clarke DM, Rowley G. Does a continuing medical education course in mental health change general practitioner knowledge, attitude and practice and patient outcomes? Primary Care Mental Health. 2004;2:13–22. [Google Scholar]
- Mueser KT, Bellack AS, Wade JH, Sayers SL, Rosenthal CK. An assessment of the educational needs of chronic psychiatric patients and their relatives. British Journal of Psychiatry. 1992;160:674–680. doi: 10.1192/bjp.160.5.674. [DOI] [PubMed] [Google Scholar]
- Oliva JR, Compton MT. A statewide Crisis Intervention Team (CIT) initiative: Evolution of the Georgia CIT program. Journal of the American Academy of Psychiatry and the Law. 2008;36:38–46. [PubMed] [Google Scholar]
- Streiner DL. Starting at the beginning: an introduction to coefficient alpha and internal consistency. Journal of Personality Assessment. 2003;80:99–103. doi: 10.1207/S15327752JPA8001_18. [DOI] [PubMed] [Google Scholar]
- Streiner DL, Norman GR. Health Measurement Scales: A Practical Guide to Their Development and Use. 2. Oxford University Press; New York: 2001. [Google Scholar]
- Weinman JA, Petrie KJ. Perceptions of Health and Illness. Harwood Academic Publishers; The Netherlands: 1997. [Google Scholar]