Abstract
Background
Adherence to medication in inflammatory bowel disease (IBD) improves outcomes. Current practices of screening for adherence to IBD medications are unknown. The goal of this study was to determine current practice and perception of screening for medication adherence among US-based gastroenterologists.
Methods
A survey was mailed electronically to gastroenterologists whose electronic-mail address was listed in the American College of Gastroenterology database. Physicians who cared for IBD patients were invited to answer.
Results
About 6830 surveys were sent to gastroenterologists nationwide, and 395 physicians who cared for IBD patients completed the survey. The true response rate is unknown, as the number of physicians caring for IBD patients in the database is unknown. About 77% (n=303) of physicians who responded stated they screen for adherence to medication. Of the 77% of physicians who screened for adherence, only 19% (n=58) use accepted measures of screening for adherence (pill counts, prescription refill rates, or adherence surveys). The remaining 81% used patient interview to screen for adherence, a measure considered least accepted to determine adherence, as it overestimates adherence. The average number of IBD patients observed in 1 week had no statistical significance in predilection for screening (P=0.82). Private practice physicians (P=0.05), younger physicians (P=0.03), and physicians with fewer years of experience (P=0.02) all were more likely to screen. About 95% of responders thought determining a low adherer to medicine was important because an intervention can increase adherence.
Conclusions
The majority of gastroenterologists surveyed recognize that adherence to medication is important and improves outcomes. The majority of physicians in this study are screening for nonadherence in IBD, but are not using accepted measures for adherence detection. If this study truly reflects the majority of physicians nationwide, changing the way physicians screen for adherence, may detect more low adherers to medication.
Key Words: adherence, compliance, IBD, medication, screening
The inflammatory bowel diseases (IBD), Crohn's disease, and ulcerative colitis are chronic inflammatory disorders of the gastrointestinal tract for which a wide array of medication treatments are used. These include mesalamine-based compounds, corticosteroids, thiopurines, methotrexate, antibiotics, and antitumor necrosis therapies. Adherence to these medications is essential to prevent flares in these chronic disorders. Unfortunately, adherence to therapy is suboptimal in chronic disease,1–4 with IBD being no exception: nonadherence rates to oral IBD medication have been reported to be as high as 40% to 72%.1–3
Recently, medical adherence has been called for as a priority for healthcare reform.4 IBD showcases why this should be the case. Nonadherence to IBD medications has both patient-specific and societal implications; it causes increased morbidity with a greater chance of relapse, increased disease activity, and a decreased quality of life.5,6 Nonadherence affects society in that it raises healthcare inpatient and outpatient expenditures by at least 30%, according to a BlueCross/BlueShield database study.7 In a UK-based study, higher adherence was associated with lower healthcare costs and fewer patient visits.8
Screening for nonadherence has the capacity to identify low adherers, an important first step to remedy the problem. Once low adherers are identified, the etiology for nonadherence can be explored before an intervention is initiated. Current approaches to address nonadherence are tailored to the etiology but include improving the physician-patient relationship, individualizing therapy, providing patient information and support, self-management programs, and practical memory aids.3
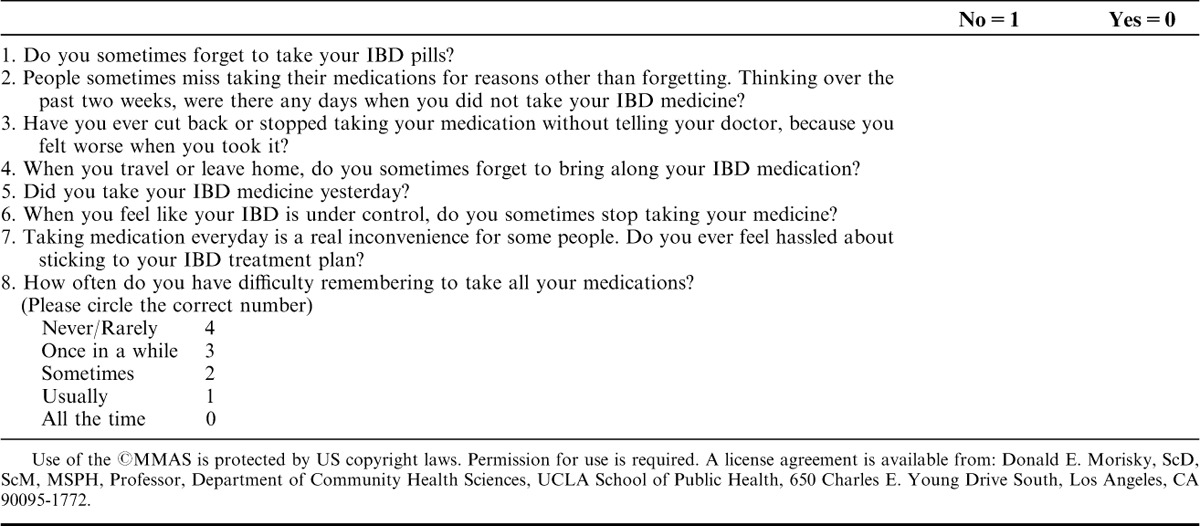
Identifying low adherers, however, can be difficult. Currently accepted methods to determine adherence include patient interview, reviewing pharmacy refill data, pill counting, and checking serum or urinary metabolite levels. Screening for nonadherence can be performed using adherence surveys developed for chronic diseases.9,10 According to Fletcher et al and many other groups, determining adherence by patient interview is the least valid way of determining adherence.11,12 Pill counts and obtaining prescription refill data are time-intensive measures and not conducive to busy clinical practice. Adherence surveys, although rarely used, are more feasible in practice-based settings because of their low cost and ease of use. The Morisky Medication Adherence Scale-8 (MMAS-8) adherence scale, which was recently validated in IBD and is the only validated scale for IBD, was developed to be nonaccusatory and patient friendly.2
A recent study by our group suggested that gastroenterologists are incompletely adept at identifying patients who are low adherers to medicine. Our study compared physician perception of adherence with the MMAS-8 survey adherence group that categorizes adherers as low, medium, or high. Physicians overestimated adherence in 67% of patients when compared with the results of the MMAS-8 survey.2 One of the unresolved questions that the study did not answer was how physicians were determining adherence in their patients. In fact, the current screening patterns for nonadherence to IBD medicine amongst gastroenterologist are unknown. The goal of this study was to determine current practice and beliefs of medication adherence screening in IBD in the United States.
METHODS
The study protocol was exempt from the Institutional Review Board as no identifying information was recorded.
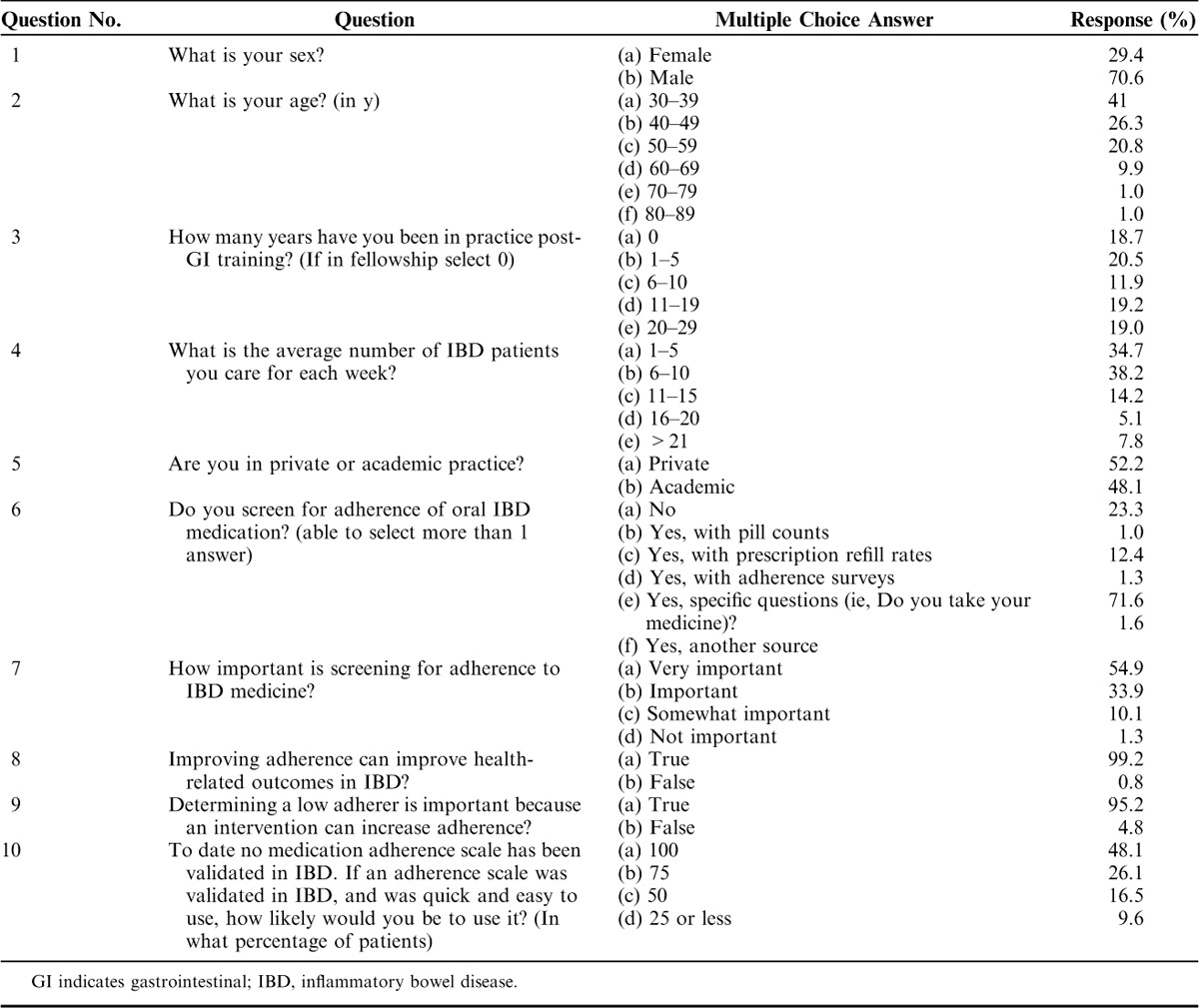
A 10-question survey (Table 1) was mailed electronically to gastroenterologists whose electronic mail (e-mail) address was listed in the American College of Gastroenterology roster that is publicly available to members. Physicians, both pediatric and adult, who cared for IBD patients were invited to answer the survey. It was unknown which gastroenterologists listed in the database cared for IBD patients, and thus the survey was sent to every gastroenterologist with a listed e-mail address in all 50 states. Physicians who did not care for patients with IBD were asked not to complete the survey; and thus excluded themselves from the study. The survey was anonymous and no names, Internet Protocol addresses, or other identifying information was recorded. The survey, the survey responses, and data compilation was performed through Survey Monkey, an online survey company. No compensation was offered or provided to survey responders.
TABLE 1.
Summary of the 10-Question Survey that was Electronically Mailed to Gastroenterologists and the Responses
A 3-month response time was given, and after this period, the survey was closed. Results were tabulated after the 3-month period was over. The survey monkey software added the responses and calculated the overall results. Surveys were excluded if they were not completely filled out.
Statistical comparisons among binary variables were made using χ2 tests with P≤0.05 considered significant. All calculations were performed using SPSS 18.0 for Windows (SPSS, Inc, Chicago, IL).
RESULTS
About 6830 surveys were sent nationwide. This number excludes e-mails that were not able to be received because of outdated or expired e-mail addresses, e-mail accounts not accepting e-mails, and for various other reasons that resulted in incomplete or absent delivery. Four hundred and two responses to the survey were completed for a gross response rate of 6%. A true response rate could not be calculated as the number of physicians who cared for IBD patients was unknown. Seven surveys were excluded for not being completely filled out, leaving 395 surveys for further analysis.
Table 1 lists the characteristics of the responders. Characteristics of nonresponders were unavailable in the database. Overall, 71% of responders were men and 29% were women. The majority of responders, 41%, were aged 30 to 39 years. There was a wide variation in the number of years of practice for responders of the survey. There was also a wide variation in number of patients seen in a week. The majority of responders, 38%, observed 6 to 10 IBD patients a week. About 35% observed 5 or less IBD patients a week and 27% observed more than 11 IBD patients a week. The percentage of responders in private versus academic practice was about equal, 52% versus 48%, respectively.
In terms of screening behavior, 23% (n=92) of responders reported that they do not screen for adherence to oral medications. About 77% (n=303) of the physicians who responded stated that they screen for adherence to medication. Of the 77% who screen for adherence, only 19% (n=58) reported use of accepted measures for screening for adherence (pill counts, prescription refill rates, or adherence surveys). The remaining 81% used patient interview to screen for adherence, a measure considered least accepted to determine adherence.
Statistical tests were used to analyze the obtained data and are summarized in Table 2. Responders were assessed for presence of screening (yes vs. no). The number of IBD patients observed by a physician in 1 week did not affect whether the physician screened patients for adherence (P=0.82). Physicians in private practices were more likely to screen their patients for adherence [relative risk (RR)=1.66, P=0.05]. The number of years past fellowship training predicted the presence of screening methods; physicians still in training or with up to 10 years of posttraining experience were more likely to screen patients as compared with physicians with greater than 10 years of experience (RR=2.16, P=0.004). Similarly, younger physicians were more likely to use an accepted screening method (up to age 39 y vs. age 40 y or above, RR=1.78, P=0.032). In this study, physician age correlated with years of experience. Physician age when compared with years of experience did not add any additional risk or benefit.
TABLE 2.
Statistics for Factors Related to Screening (Based on Questions From Table 1)
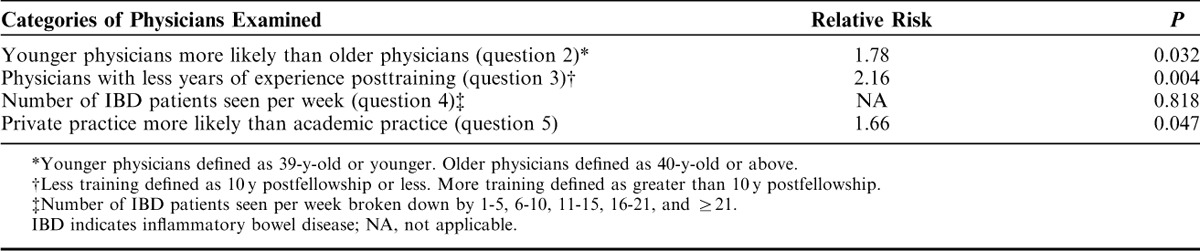
In addition, subgroup analysis showed that there were a greater number of younger physicians aged 39 years or below in academic medicine. Therefore, age was not a confounder and does not explain why private practice physicians screen more often.
In terms of screening beliefs, 89% of responders thought screening was very important or important versus 11% who thought screening was somewhat important or not important. About 99% of responders thought improving adherence would improve health-related outcomes and 95% of responders thought determining a low adherer to medicine was important because an intervention could increase adherence. About 74% of responders would use a validated adherence survey in practice in a majority of their patients and 48% of responders stated that they would use it in every patient.
DISCUSSION
Our results help to elucidate the current practice and beliefs of screening for medication adherence in IBD, assuming our survey population is representative of all physicians who care for patients with IBD. We found that the majority of physicians surveyed believe that screening for adherence is important and can change outcomes. In fact, the majority of physicians stated that they screen for adherence (77% of physicians). However, of this majority, very few use accepted methods for determining adherence, as most used patient interview to screen for adherence.
Patient interview is the simplest form of screening, and involves asking the patient directly whether he is adherent to medication. As mentioned earlier, patients often overestimate or perhaps misrepresent their adherence, and thus this is not an accurate method for determining true adherence. In 1 study in patients with human immunodeficiency virus, patient interview had a sensitivity of 14% and a specificity of 96%.11 Thus, those needing interventions for nonadherence would not be identified by patient interview. Other studies on patient interview have shown similar results.12–16 Only 2 studies in IBD have looked at patient interview for detecting adherence. In 1 study of patients taking 5-aminosalicylic acid medications for IBD, patient interview was concordant with urinary drug measurement in only 66% of patients.17 The other study is by Hommel et al, in which objective measurement of adherence was compared with the subjective patient perception of adherence by the patient through patient interview. Their group found that patients grossly overestimated or overstated adherence. In their cohort of 42 IBD patients, they found that objective nonadherence rates were 64% for thiopurines and 88% for 5-aminosalicylic acid compounds; however, subjective nonadherence rates as per the patients were 10% and 2%, respectively.18 Many other studies of patient interview in non-IBD disease groups have similar sensitivities.12–16 The consensus from the adherence literature is that this is the least accepted way of determining adherence in chronic disease12–16; yet, it is the most popular way to screen in IBD according to our results.
Pill counts and obtaining prescription refill information are more accepted for determining adherence. The downfall to these measures are that they are time consuming and not practical in a busy clinical practice. Adherence surveys are easy to use, accepted as screening tools for adherence, and do not take excessive time. The only adherence scale to be validated in IBD is the MMAS-8.2,19 This scale was developed from the original Morisky scale.20 The new scale was developed as the earlier scale was considered accusatory in nature, isolating, and often evoked defensiveness from patients.21 For example, 1 of the 4 questions was, “Are you careless about taking your medicine?” The authors concluded that the MMAS-8 scale was relatively simple and practical to use in clinical settings, could identify patients with adherence problems, and could be used to monitor adherence over the course of the treatment. Given the ease of use and the patient-friendly nature of the scale, the MMAS-8 is a convenient scale for use in IBD (Table 3). According to this survey, close to half of all responders stated they would use a validated adherence scale in every patient. An additional quarter of the responders would use it at least 75% of the time. The MMAS-8 seems like a tool that physicians would use once it becomes known that it is already a recently validated tool in IBD.
TABLE 3.
Morisky Medication Adherence Scale-819
Of interest, the physicians who were more likely to screen for nonadherence were those with less than 10 years of experience, those below 40 years of age, and those in private practice. It is unclear why these groups are more likely to screen, and further research is needed to further clarify these features.
Although nonadherence to medication raises healthcare expenditures and results in worse clinical outcomes, it is not formally recommended to screen for adherence in clinical practice and is absent from IBD guidelines.22,23 The point of screening for adherence is to detect low adherers, and administer an intervention that results in improved adherence and consequently in improved outcomes; however, no study to date has been performed showing improved outcomes, and may explain why screening for nonadherence is not formally recommended. Many interventions are available and have been shown to improve adherence.3 Examples are improving the physician-patient relationship, individualizing therapy, providing patient information and support, self-management programs, or practical memory aids. Interestingly, improving the physician-patient relationship may be the most important factor as a recent systematic review by Jackson et al,24 showed that no clinical, demographic, or treatment variables affected adherence. Patient-doctor relationship, physiological distress, and patient beliefs about medicine were important determinants of adherence.
This study suffers the traditional weaknesses of survey studies which include reactivity (respondents give socially desirable responses that make them look good or seem to be what the researcher is looking for), sampling frame (difficult to access the proper number and type of people who are needed for a representative sample of the target population), measurement error (inherent systematic biases), and errors because of nonresponse (people who choose to respond on the survey may be different from those who do not respond, thus biasing the estimates).25 We were unable to compare characteristics with those who completed the survey versus those who did not, as characteristics for nonresponders were not available in the database. In addition, we chose the survey to have answer choices that had discrete cut-off points, as opposed to collecting data in continuous form. This facilitated the ease of responders to complete the survey. There are limitations to this style of survey, mainly in that it can attenuate the relationship between a variable and outcome. In addition, individual responses may be more similar across categories than within categories.
In addition, many survey studies traditionally suffer from low response rate, and thus a low survey accuracy or sampling bias. However, this notion has been challenged. It has been assessed whether lower response rates are associated with less unweighted demographic representativeness of a sample.26 By examining the results of 81 national surveys with response rates varying from 5% to 54% were examined. Surveys with much lower response rates were only minimally less accurate. Our study had a gross response rate of 6%, however, this is an underestimation as many members of the American College of Gastroenterology database do not practice clinical IBD, and thus as per our instructions asked not to complete the survey. Examples of people who could fall into this category include physicians or members who are retired, related careers without patient contact (pathologists), and physicians who do not see IBD patients in their office. Thus, the true response rate is in fact much higher.
Overall, the study showed the majority of physicians surveyed are not using accepted measures to screen for nonadherence to medication. Cutler and Everett4 wrote “The bottom line is this: We've known for some time that improved adherence can lead to improvements in health outcomes and reductions in healthcare spending. What we haven't known is where to start.” Screening with the appropriate available tools may be the place to start if we can show improved outcomes. A prospective trial is needed in the future that can evaluate outcomes in those screened for nonadherence versus those not screened.
Footnotes
Funding: National Institutes for Health, NIH K-08-DK069393 (T.A.U.). No other authors have sources of funding to report.
The authors declare that they have nothing to disclose.
REFERENCES
- 1.Robinson A. Improving adherence to medication in patients with IBD. Aliment Pharmacol Ther. 2008;2:9–14. doi: 10.1111/j.1365-2036.2008.03604.x. [DOI] [PubMed] [Google Scholar]
- 2.Trindade AJ, Ehrlich A, Kornbluth A, et al. Are your patients taking their medicine? Validation of a new adherence scale in patients with inflammatory bowel disease and comparison with physician perception of adherence. Inflamm Bowel Dis. 2011;17:599–604. doi: 10.1002/ibd.21310. doi: 10.1002/ibd.21310. [DOI] [PubMed] [Google Scholar]
- 3.Hawthorne AB, Rubin G, Ghosh S. Review article: medication non-adherence in ulcerative colitis: strategies to improve adherence with mesalazine and other maintenance therapies. Aliment Pharmacol Ther. 2008;27:1157–1166. doi: 10.1111/j.1365-2036.2008.03698.x. [DOI] [PubMed] [Google Scholar]
- 4.Cutler DM, Everett W. Thinking outside the pillpox Medication adherence as a priority for healthcare reform. N Engl J Med. 2010;362:1553–1555. doi: 10.1056/NEJMp1002305. [Epub April 7]. [DOI] [PubMed] [Google Scholar]
- 5.Kane SV. Systematic review: adherence issues in ulcerative colitis. Aliment Pharmacol Ther. 2006;23:577–585. doi: 10.1111/j.1365-2036.2006.02809.x. [DOI] [PubMed] [Google Scholar]
- 6.Kane SV, Aikens J, Huo D, et al. Medication adherence is associated with improved outcomes in patients with quiescent ulcerative colitis. Am J Med. 2003;113:39–42. doi: 10.1016/s0002-9343(02)01383-9. [DOI] [PubMed] [Google Scholar]
- 7.Bassi A, Dodd S, Williamson P, et al. Cost of illness of IBD in the UK. Gut. 2004;53:1471–1478. doi: 10.1136/gut.2004.041616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garc´ia Rodŕguez LA, Gonzalez-Perez A, Johansson S, et al. Risk factors for inflammatory bowel disease in the general population. Aliment Pharmacol Ther. 2005;22:309–315. doi: 10.1111/j.1365-2036.2005.02564.x. [DOI] [PubMed] [Google Scholar]
- 9.Kane S. A 38-year-old with recurrent colitis. Is it non-compliance? Clin Gastroenterol Hepatol. 2009;7:1164–1167. doi: 10.1016/j.cgh.2009.06.022. [DOI] [PubMed] [Google Scholar]
- 10.Fletcher SW, Pappius EM, Harper SJ. Measurement of compliance in a clinical setting. Arch Intern Med. 1979;139:635–638. [PubMed] [Google Scholar]
- 11.Liu H, Golin C, Miller L, et al. A comparison study of multiple measures of adherence to HIV protease inhibitors. Ann Intern Med. 2001;134:968–977. doi: 10.7326/0003-4819-134-10-200105150-00011. [DOI] [PubMed] [Google Scholar]
- 12.Jasti S, Siega-Riz AM, Cogswell ME, et al. Correction for errors in measuring adherence to prenatal multivitamin/mineral supplement use among low-income women. J Nutr. 2006;136:479–483. doi: 10.1093/jn/136.2.479. [DOI] [PubMed] [Google Scholar]
- 13.O'Brien MK, Petrie K, Raeburn J. Adherence to medication regimens: updating a complex medical issue. Med Care Rev. 1992;49:435–434. doi: 10.1177/002570879204900403. [DOI] [PubMed] [Google Scholar]
- 14.Pekovic V, Mayanja H, Vjecha M, et al. Comparison of three composite compliance indices in a trial of self-administered preventive therapy for tuberculosis in HIV-infected Ugandan adults. Uganda Case Western Reserve University Research Collaboration. J Clin Epidemiol. 1998;51:597–607. doi: 10.1016/s0895-4356(98)00033-x. [DOI] [PubMed] [Google Scholar]
- 15.Stephenson BJ, Rowe BH, Haynes RB, et al. Is this patient taking the treatment as prescribed? JAMA. 1993;269:2779–2781. [PubMed] [Google Scholar]
- 16.Wright EC. Non-compliance or how many aunts has Matilda? Lancet. 1993;342:909–913. doi: 10.1016/0140-6736(93)91951-h. [DOI] [PubMed] [Google Scholar]
- 17.Hommel KA, Davis CM, Baldassano RN. Objective versus subjective assessment of oral medication adherence in pediatric inflammatory bowel disease. Inflamm Bowel Dis. 2009;15:589–593. doi: 10.1002/ibd.20798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Higgins PD, Rubin DT, Kaulback K, et al. Systematic review: impact of non-adherence to 5-ASA products on the frequency and cost of ulcerative colitis flares. Aliment Pharmacol Ther. 2009;29:247–257. doi: 10.1111/j.1365-2036.2008.03865.x. [DOI] [PubMed] [Google Scholar]
- 19.Morisky DE, Alfonso A, Krousel-Wood M, et al. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10:348–354. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 20.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Rigby D. Adherence assessment tools: drugs don't work when they are not taken. Aust J Pharm. 2007;88:32–37. [Google Scholar]
- 22.Hanauer SB, Sandborn W. Management of Crohn's disease in adults. Am J Gastroenterol. 2001;96:635–643. doi: 10.1111/j.1572-0241.2001.3671_c.x. [DOI] [PubMed] [Google Scholar]
- 23.Kornbluth A, Sachar DB. Ulcerative colitis practice guidelines in adults. Am J Gastroenterol. 2010;105:501–523. doi: 10.1038/ajg.2009.727. [DOI] [PubMed] [Google Scholar]
- 24.Jackson CA, Clatworthy J, Robinson A, et al. Factors associated with non-adherence to oral medication for inflammatory bowel disease: a systematic review. Am J Gastroenterol. 2010;105:525–539. doi: 10.1038/ajg.2009.685. [DOI] [PubMed] [Google Scholar]
- 25.Landry JA, Smyer MA, Tubman JG, et al. Validation of two methods of data collection of self-reported medicine use among the elderly. Gerontologist. 1988;28:672–676. doi: 10.1093/geront/28.5.672. [DOI] [PubMed] [Google Scholar]
- 26.Allyson H, Krosnick J, Pfent A, et al. “The causes and consequences of response rates in surveys by the news media and government contractor survey research firms. In: Lepkowski JM, Clyde Tucker N, Michael Brick J, editors. Advances in Telephone Survey Methodology. New York: Wiley; 2007. pp. 499–678. [Google Scholar]


