Abstract
Background
This study examines 30-year trajectories of heroin and other drug use among men and women who were in methadone maintenance treatment in California in the late1970s and interviewed in 1978–1981.
Methods
Nearly half (n = 428; 46.8%) of the original study sample (N = 914) was deceased. Of the remaining 486 subjects, 343 (44.3% female) completed a follow-up interview in 2005-09 (70.6% of those not deceased). Average age at follow-up was 58.3 (SD = 4.9) years for males and 55.0 (SD = 4.1) years for females. Longitudinal data was obtained on their drug use, treatment participation, and criminal justice status over the follow-up period. Trajectory group modeling was used to identify distinctive trajectory groups based on monthly averages of heroin and other drug use per year; group differences were examined.
Results
Four heroin and five alcohol and other drug (AOD) trajectory groups were identified. A greater proportion of women (60%) were in the “rapid decrease” heroin group (odds of use less than 10% by 10 years following initiation of use) as compared with the other groups. More rapid decrease of heroin use was associated with increases in AOD use, whereas a gradual decrease in heroin use was associated with a gradual decrease in AOD use. More school problems and earlier age at onset of heroin use and first arrest were associated with more persistent heroin use.
Conclusion
Heroin-use trajectories were linked with changes in AOD use. Childhood antecedents of heroin-use trajectories were identified as well as gender differences.
Keywords: longitudinal research, gender, heroin dependence, trajectory group models
1. Introduction
The study uses a life course perspective (Anglin et al., 2001; Hser et al., 2007b; Hser and Anglin, 2010) to examine longitudinal trajectories of heroin and other drug use over approximately 30 years for a sample of men and women who were enrolled in methadone maintenance treatment in the late 1970s in California. Childhood risk and protective factors and ages at critical events, including initiation of heroin and other drug use, are examined in relation to longitudinal drug-use patterns.
1.1. Childhood antecedents of heroin addiction
Childhood and family-related factors were examined in relation to onset of heroin addiction among a cohort of male heroin addicts and two matched community comparison groups (Nurco et al., 1981a, 1981b). This early retrospective study established that several childhood factors were related to onset of heroin addiction, including “deviant acts,” earlier use of alcohol and marijuana, greater levels of family deviance and family disruption, and deviant peers (Nurco et al., 1994). Moreover, several indicators of family functioning in early adolescence were identified as protective factors that decreased the likelihood of later heroin addiction (Nurco and Lerner, 1996). They later derived four subtypes of male heroin addicts who varied by age at first addiction and subsequent amount of time incarcerated and actively using over the initial 10 years following onset of addiction (Nurco et al., 1997).
Similarly, Hser and colleagues (Hser et al., 2007a) examined early “deviant” behavior and family/social problems as predictors of longitudinal (33-year) heroin use trajectories among an all-male sample. Although childhood characteristics were not predictive of later outcomes, individuals who ceased heroin use early (i.e., after approximately 10 years) had initiated heroin use at a later age than those with longer-use trajectories.
1.2. Longitudinal studies of heroin users
Several major longitudinal studies of heroin users, with assessments spanning periods of 10 – 33 years, have been conducted in the United States (Goldstein and Herrera, 1995; Hser et al., 1997; Maddux and Desmond, 1981, 1992; O'Donnell, 1964, 1969; Simpson et al., 1986; Vaillant, 1970). Most such studies, however, have included all- or mostly male samples, precluding analyses of gender differences.1
This extant body of research has established that individuals with heroin dependence have higher rates of morbidity and mortality over time, as compared with their counterparts in the general population (Darke et al., 2007a). Further, although rates of abstinence increase over time, a substantial proportion of men continue chronic heroin use over extended periods (Winick, 1974). A recent systematic review showed that most individuals dependent on opioids eventually achieve remission over variable follow-up periods (Calabria et al., 2010); however, a minority relapses to drug use even after substantial periods of abstinence (Hser et al., 2001). Moreover, when compared with stimulant users, heroin users show more persistent and higher levels of use over time (Hser et al., 2008).
The current study builds upon this foundation of longitudinal research with heroin users to examine 30-year trajectories of heroin and other drug use among both men and women. Prior research has established that men and women differ in their drug use initiation and progression (Grella and Joshi, 1999; Hser et al., 1987). We hypothesized that distinctive longitudinal trajectories would be associated with both gender and background characteristics.
2. Methods
2.1. Study design and participants
The original study sample comprises individuals who participated in two prior studies of participants in publicly funded methadone maintenance programs in six counties in Central and Southern California between 1976 and 1978. Participants (N = 921)2 were initially sampled from program records and completed baseline interviews from 1978–1981. Interviews were conducted by study research assistants outside of the treatment settings; all participants completed informed consent at that time. Descriptions of the prior study methods and study findings have been published previously (McGlothlin and Anglin, 1981; Anglin et al., 1989).
We attempted to locate and contact all participants from these two prior studies who were not identified as deceased. The original study records were used as a starting basis for locating the study participants. Information on current residence was obtained from the Department of Motor Vehicles, criminal justice records, and Internet-based programs. Upon locating the respondent, we verified that they were the same individual in the original study based on their date of birth, residence in the specific county at the time of the original study, and social security number.
Follow-up interviews were conducted from 2005–2009. Study participants were paid $100 for completion of the interview. All follow-up study procedures were reviewed and approved by the UCLA Institutional Review Board and a federal Certificate of Confidentiality was obtained.
2.2. Current study sample
At the time of the original interview, the average age of study participants was 35.4 years for males and 30.2 years for females. Average age at the follow-up interview was 58.3 (SD = 4.9) years for males and 55.0 (SD = 4.1) years for females. The average time interval between the baseline and follow-up interviews was 25.2 years for both men and women. All study participants originally met clinical criteria for heroin dependence as required for admission to methadone maintenance treatment.
The current status of subjects from the original study sample (N = 914) is as follows: 414 subjects (45.3% of original sample) were identified as deceased based on records obtained from the National Death Index. An additional 14 subjects were reported as deceased by family members or others, but no death certificate was obtained due to a lack of a match on either their name or social security number. Thus, the total verified and “probable” deceased (N = 428) constitute 46.8% of the original study sample.
Of the remaining 486 subjects, 343 completed follow-up interviews (70.6% of the still-living subjects). Six incarcerated subjects were not interviewed, 18 subjects refused to be interviewed, and 5 subjects were too ill to be interviewed (N = 29 unable to be interviewed; 3.2%). The remaining 114 subjects (12.5% of original sample; 23.5% of sample excluding deceased) were not located or interviewed.
We compared socio-demographic and background characteristics of individuals who: (1) completed the follow-up interview, (2) were deceased at the time of follow-up, and (3) were not located. Women were over-represented in the interviewed group (44%) as compared with the overall sample (37%; p < .001). There was also a higher proportion of Whites in the interviewed group, and higher proportions of Hispanics and African Americans in the other groups, relative to the total sample (p < .05). A greater proportion of the interviewed subjects had completed high school (47%) relative to the total sample (40%, p < .01). Further, a higher proportion of individuals in the deceased group had rated their health as “fair or poor” (versus good or excellent) as compared to those in the other groups (p < .05). Individuals in the deceased group were older, on average, at the baseline interview (34.2±7), as compared with the total sample (32.2±6, p < .001). There were no significant differences among groups, however, on ages at initiation of alcohol, tobacco, heroin, or other drug use.
2.4. Measures
2.4.1. Background characteristics
Background characteristics were assessed at the baseline interview. These included: socio-demographics: gender, race/ethnicity, birth year; childhood risk and protective factors: parent “had a drinking problem”; number of school problems (truancy, probation, suspension, expulsion, dropped out, other), coded as a binary variable (0 – 1 or 2 – 6); gang involvement; relationship with parents (good or excellent vs. OK or very bad); whether the respondent lived with “both natural parents up to age 16”; and family socio-economic status (poor or lower income vs. middle or upper class); age at first use of heroin, regular use of heroin, use of alcohol to intoxication, and regular use of cigarettes; and ever had an overdose on heroin.
2.4.2. Behavioral disorders
A computerized version of the Structured Clinical Interview for DSM-IV (First et al., 1997) was administered to derive diagnoses of conduct disorder and antisocial personality disorder based on DSM-IV criteria.
2.4.3. Natural history assessment
Natural history data obtained at the baseline and follow-up interviews used a similar time-line approach to demarcate periods of heroin and other drug use, incarceration, and treatment participation. The baseline timeline assessment was anchored to one year prior to the onset of regular heroin use; the follow-up assessment was anchored to the date of the prior interview. Thus, the combined natural history data cover a cumulative period of approximately 30 years.3
The natural history interview is modeled on an approach used by Nurco et al. (1975). A timeline of the follow-up period is first organized into periods of institutionalization (i.e., residential treatment, hospitalization, incarceration) and noninstitutionalization. Within each non-institutionalized period, the respondent is asked to indicate how many months they used heroin within the segment.4 Each month in the segment is then assigned an average score derived by dividing the number of months of heroin use by the total number of months in the segment. Each year in the 30-year period is then assigned the average of the corresponding 12 monthly values; if the mean score for the year is greater than or equal to 0.50, the respondent is coded as having used heroin in that year.
Similarly, yearly indicators of use of alcohol, cocaine/crack, methamphetamine/amphetamines, marijuana, and other opioids are calculated (separately) in the same way. If any of the substances is coded as positive in a given year (i.e., average use across the 12 months is ≥ 0.50), then the individual is coded as having used alcohol and/or other drugs (AOD) for that year.
With regard to treatment participation, subjects were asked about their participation in treatment in each segment, including methadone maintenance treatment (MMT), residential, outpatient. Because of the low rates of participation in treatment other than MMT, all other forms of treatment were collapsed into an aggregate category. Treatment participation was coded for each month in the segment using the same method described above for heroin and other drug use, with an average derived for each 12-month period. Percentage of time in MMT and in other treatment was calculated. Similarly, time incarcerated was based on the number of months that the participant was in jail, prison, or civil commitment over the period divided by the total number of months in the 30-year period.
2.5. Statistical analysis
The group-based trajectory modeling approach (Jones et al., 2001; Nagin, 1999) was applied to identify and estimate distinctive heroin-use trajectories. The approach was used because the normality assumption for the random effects in the conventional growth model may not be applicable if multiple different types of patterns exist across the subjects. The group-based trajectory approach is more flexible, approximating an unspecified continuous distribution of unobserved heterogeneity with a linear combination of discrete distributions. That is, different groups, each with its own growth trajectory, are used to capture the overall variation. Results thus allow subjects to be partitioned into latent classes determined by differences in their trajectory patterns. A logit model was assumed for analysis in which odds of use per year are derived. Intercept, slope, quadratic, and cubic parameters were initially included in the models, and then successively deleted if doing so resulted in improved model fit.
The first stage of the process entailed modeling trajectories separately for heroin use and alcohol and/or other drug (AOD) use, calculating the probability of belonging to each of the trajectory groups. The second stage consisted of modeling joint heroin and AOD use trajectories. Analyses were conducted with the SAS PROC TRAJ procedure (Jones et al., 2001). Estimation procedures allowed missing data, assuming it was missing at random, similar to assumptions for random effects growth modeling. Goodness of model fit was evaluated by Bayesian Information Criterion (BIC), with lower BIC indicating a better model. Also taken into consideration were parsimony and interpretability, as the BIC continued to decrease for each added group; however, the decrease in BIC was dramatically lessened after selection of a “final” model.5
Three sets of probabilities were then examined for the joint trajectories: (1) heroin use conditional on AOD use, (2) AOD use conditional on heroin use, and (3) probability of belonging to each of the unique joint heroin/AOD use trajectory groups (Nagin and Tremblay, 2001). Differences among the heroin- and AOD-use trajectory groups in socio-demographics, background characteristics, and behavioral disorders were examined using chi square tests for categorical variables and ANOVA (SAS Proc ANOVA) for continuous variables.
3. Results
3.1. Heroin use trajectory groups
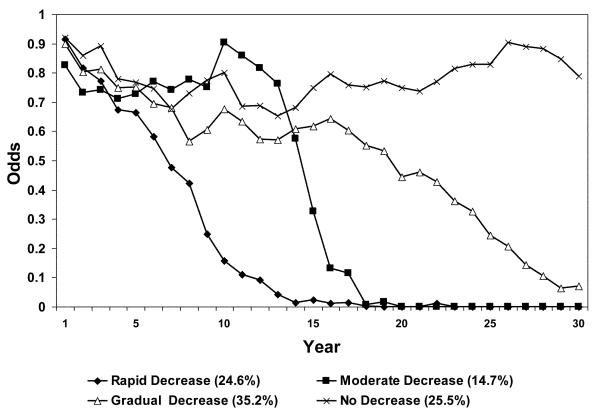
A four-group model was derived for heroin use; the final model has two cubic trajectories, one quadratic trajectory, and one linear trajectory (see Figure 1). The four trajectory groups were characterized as: rapid decrease (24.6%), moderate decrease (14.7%), gradual decrease (35.2%), and no decrease (25.5%). Mean posterior probabilities of group membership for the four groups were all greater than 0.95, indicating a very good model fit to the data (Nagin, 2005).
Figure 1.
Heroin use trajectories based on joint trajectory models; odds of use calculated per year beginning with year of heroin use initiation. N = 341.
The “rapid decrease” group had odds of heroin use of 0.16 at 10 years, but those odds were reduced to less than 0.01 by 20 years. The “moderate decrease” group had odds of heroin use of 0.90 at 10 years, but odds of use were reduced to less than 0.01 by 20 years. The “gradual decrease” group had odds of use of 0.68 at 10 years, 0.44 at 20 years, and 0.07 at 30 years. Lastly, the “no decrease” group had odds of heroin use of 0.80 at 10 years, 0.75 at 20 years, and 0.79 at 30 years.
Differences among the four groups are shown in Table 1. Women made up the largest proportion of the “rapid decrease” group (60%) and the smallest proportion of the “gradual decrease” group (39%). The “rapid decrease” group had the smallest proportion that reported two or more school-related problems (27%). The “rapid decrease” and “moderate decrease” groups had the smallest proportion of those who were diagnosed with conduct disorder (29% and 32%, respectively), whereas the “gradual decrease” group had the highest (52%). Similarly, the “gradual decrease” group had the highest proportion of participants with antisocial personality disorder (49%) and spent the highest proportion of time incarcerated (20%), whereas the “rapid decrease” group had the lowest (7%).
Table 1.
Heroin use trajectory groups.
| Rapid Decrease (n = 84) |
Moderate Decrease (n = 50) |
Gradual Decrease (n = 120) |
No Decrease (n = 87) |
Total (n = 341) |
|
|---|---|---|---|---|---|
| Female,%* | 59.5 | 46.0 | 39.2 | 46.0 | 46.9 |
| Race/ethnicity, % | |||||
| White | 78.6 | 72.0 | 70.8 | 78.2 | 74.8 |
| Hispanic | 17.9 | 24.0 | 25.0 | 17.2 | 21.1 |
| African-American | 3.6 | 4.0 | 4.2 | 4.6 | 4.1 |
| High school degree, %* | 52.4 | 62.0 | 41.7 | 37.9 | 46.3 |
| Childhood Risk/Protective Factors | |||||
| Father had drinking problem, % | 32.1 | 22.0 | 35.8 | 32.2 | 32.0 |
| Mother had drinking problem, % | 17.9 | 18.0 | 16.7 | 12.6 | 16.1 |
| School problems, %* | |||||
| 0 – 1 | 72.6 | 62.0 | 51.7 | 51.7 | 58.4 |
| 2 or more | 27.4 | 38.0 | 48.3 | 48.3 | 41.6 |
| Gang involvement, % | 14.3 | 26.0 | 24.2 | 20.7 | 21.1 |
| Good-excellent relationship with parents, % | 61.9 | 64.0 | 67.5 | 66.7 | 65.4 |
| Raised by both parents, % | 64.3 | 54.0 | 60.8 | 60.9 | 60.7 |
| Family SES: Lower income/poor, % | 35.7 | 40.0 | 42.9 | 39.3 | 39.8 |
| Behavioral Disorders | |||||
| Conduct disorder, %** | 28.6 | 32.0 | 51.7 | 34.5 | 38.7 |
| Antisocial personality disorder, %*** | 22.6 | 28.0 | 49.2 | 33.3 | 35.5 |
| Use Patterns | |||||
| Ever heroin overdose, %* | 50.0 | 64.0 | 69.2 | 72.4 | 64.5 |
| Age at Critical Events | |||||
| Alcohol intoxication < 14, % | 34.5 | 38.0 | 39.2 | 41.4 | 38.4 |
| Smoke regularly < 15, % | 36.9 | 46.0 | 45.0 | 41.4 | 42.2 |
| Used heroin < 19, %† | 50.0 | 52.0 | 65.0 | 66.7 | 59.8 |
| Birth year (SD)† | 1949.9 (4.3) | 1949.6 (3.1) | 1948.6 (4.7) | 1948.3 (5.6) | 1949.0 (4.7) |
| Age 1st used alcohol to intoxication (SD) | 14.2 (4.1) | 13.5 (3.7) | 13.9 (3.9) | 13.8 (3.1) | 13.9 (3.8) |
| Age 1st used heroin (SD)*** | 19.9 (4.1) | 19.0 (3.1) | 17.8 (3.9) | 18.1 (3.1) | 18.6 (3.4) |
| Age 1st used heroin regularly (SD)* | 20.7 (4.1) | 20.3 (3.2) | 19.4 (3.2) | 19.5 (3.0) | 19.7 (3.7) |
| Age last used heroin (SD)*** | 30.7 (7.8) | 37.1 (8.9) | 46.7 (7.4) | 53.6 (5.7) | 43.1 (11.4) |
| Age 1st arresta (SD) *** | 18.6 (4.3) | 17.1 (3.0) | 16.7 (3.6) | 16.7 (3.6) | 17.2 (3.8) |
| Age at baseline interview (SD)* | 29.5 (4.1) | 30.1 (2.9) | 30.9 (4.6) | 31.4 (6.0) | 30.6 (4.7) |
| Age at follow-up interview (SD) | 56.0 (4.4) | 56.0 (3.1) | 57.2 (4.7) | 57.4 (5.7) | 56.8 (4.7) |
| Treatment/Incarceration | |||||
| % time in MMT*** | 0.18 (0.2) | 0.23 (0.2) | 0.25 (0.2) | 0.38 (0.3) | 0.26 (0.2) |
| % time in other treatment | 0.02 (0.1) | 0.03 (0.1) | 0.03 (0.0) | 0.02 (0.0) | 0.02 (0.1) |
| % time incarcerated*** | 0.07 (0.1) | 0.07 (0.1) | 0.20 (0.2) | 0.11 (0.1) | 0.13 (0.2) |
| Alcohol & Other Drug Use b | |||||
| % time using heroin*** | 0.22 (0.1) | 0.40 (0.1) | 0.64 (0.2) | 0.84 (0.2) | 0.55 (0.3) |
| % time using marijuana† | 0.21 (0.3) | 0.30 (0.3) | 0.21 (0.3) | 0.29 (0.3) | 0.24 (0.3) |
| % time using cocaine** | 0.06 (0.2) | 0.12 (0.2) | 0.11 (0.1) | 0.16 (0.2) | 0.11 (0.2) |
| % time using other opioids*** | 0.01 (0.0) | 0.02 (0.0) | 0.02 (0.1) | 0.07 (0.2) | 0.03 (0.1) |
| % time using amphetamines* | 0.10 (0.2) | 0.07 (0.1) | 0.05 (0.1) | 0.06 (0.2) | 0.07 (0.2) |
| % time using alcohol*** | 0.40 (0.3) | 0.36 (0.3) | 0.25 (0.2) | 0.34 (0.3) | 0.33 (0.3) |
| % time using AOD*** | 0.68 (0.2) | 0.56 (0.3) | 0.47 (0.3) | 0.56 (0.3) | 0.56 (0.3) |
p < .10
p < .05
p < .01
p < .001
19 people had never been arrested
% time during non-institutionalized periods
The “no decrease” group spent the largest proportion of time in MMT (38%). The “rapid decrease” group had the oldest age at first use and first regular use of heroin, and the “gradual decrease” group had the youngest. As would be expected, the average age at last use of heroin increased across the trajectory groups, with the youngest age among those in the “rapid decrease” group and the oldest age among those in the “no decrease” group.
The “no decrease” group had the highest average proportion of time using cocaine over the 30-year period (16%), whereas the “rapid decrease” group had the lowest (6%). The “rapid decrease” group had the highest percentage of time using amphetamines (10%) and alcohol (40%).
3.2. AOD use trajectory groups
Five distinct trajectories of AOD use (excluding heroin) were derived in which there were two cubic trajectories, one quadratic trajectory, and two linear trajectories (see Figure 2). These trajectory groups were characterized as: low use (18.5%), late-onset increase (22.6%), early-onset increase (25.2%), gradual decrease (17.6%), and no decrease (16.1%). Similar to the previous, mean posterior probabilities of group membership for the five groups were all greater than 0.95, indicating a very good model fit to the data.
Figure 2.
Alcohol and/or other drug use trajectories based on joint trajectory models; odds of use calculated per year beginning with year of heroin use initiation. N = 341.
The “low use” group had odds of AOD use of 0.08 at 10 years, 0.01 at 20 years, and 0.18 at 30 years. The “late-onset increase” group had odds of AOD use of 0.06 at 10 years, 0.73 at 20 years, and 0.87 at 30 years. The “early onset increase” group had odds of AOD use of 0.66 at 10 years, 0.96 at 20 years, and 0.89 at 30 years. The “gradual decrease” group had odds of AOD use of 0.48 at 10 years, 0.26 at 20 years, and 0.17 at 30 years. Lastly, the “no decrease” AOD use group had odds of use of 0.83 at 10 years, 0.94 at 20 years, and 0.98 at 30 years.
Differences among the five AOD use groups are shown in Table 2. There were no differences among groups by gender or race/ethnicity. The “low use” group was oldest on average and the “no decrease” group was youngest. The “low use” group had the highest proportion with a history of gang involvement (38%) and the “early onset increase” and “no decrease” groups had the lowest. The “late-onset increase” group had the highest proportion that had ever had a heroin overdose (74%) and the “early-onset increase” group had the lowest proportion (52%). The “late-onset increase” group had the highest proportion that had an early age of onset of regular cigarette use (51%) and the “early-onset increase” group had the smallest (30%).
Table 2.
AOD use trajectory groups.
| Low Use (n = 63) |
Late-onset Increase (n = 77) |
Early-onset Increase (n = 86) |
Gradual Decrease (n = 60) |
No Decrease (n = 55) |
|
|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | |
| Female,% | 41.3 | 49.4 | 52.3 | 43.3 | 45.5 |
| Race/ethnicity, % | |||||
| White | 66.7 | 81.8 | 79.1 | 78.3 | 63.6 |
| Hispanic | 30.2 | 13.0 | 16.3 | 20.0 | 30.9 |
| African-American | 3.2 | 5.2 | 4.6 | 1.7 | 5.5 |
| High school degree, % | 33.3 | 45.5 | 52.3 | 45.0 | 54.6 |
| Childhood Risk/Protective Factors | |||||
| Father had drinking problem, % | 27.0 | 35.1 | 32.6 | 30.0 | 34.6 |
| Mother had drinking problem, % | 12.7 | 13.0 | 22.1 | 18.3 | 12.7 |
| School problems, % | |||||
| 0 – 1 | 54.0 | 49.4 | 68.6 | 60.0 | 58.2 |
| 2 or more | 46.0 | 50.6 | 31.4 | 40.0 | 41.8 |
| Gang involvement, %*** | 38.1 | 27.3 | 9.3 | 21.7 | 10.9 |
| Good-excellent relationship with parents, % | 74.6 | 58.4 | 64.0 | 63.3 | 69.1 |
| Raised by both parents, % | 60.3 | 57.1 | 65.1 | 65.0 | 54.6 |
| Family SES: Lower income/poor, %† | 52.4 | 41.6 | 36.1 | 32.2 | 36.5 |
| Behavioral Disorders | |||||
| Conduct disorder, %** | 50.8 | 39.0 | 24.4 | 51.7 | 37.7 |
| Antisocial personality disorder, %*** | 49.2 | 37.7 | 18.6 | 50.0 | 27.3 |
| Use Patterns | |||||
| Ever heroin overdose, %* | 71.9 | 74.0 | 52.3 | 66.7 | 60.0 |
| Age at Critical Events | |||||
| Alcohol intoxication < 14, %† | 47.6 | 48.1 | 30.2 | 33.3 | 32.7 |
| Smoke regularly < 15, %* | 50.8 | 52.0 | 30.2 | 40.0 | 40.0 |
| Used heroin < 19, %*** | 71.4 | 70.0 | 40.7 | 55.0 | 67.3 |
| Birth year (SD)*** | 1944.9 (5.8) | 1948.0 (4.3) | 1950.1 (3.7) | 1949.0 (4.5) | 1950.9 (4.1) |
| Age 1st used alcohol to intoxication (SD) | 13.2 (3.8) | 13.9 (3.6) | 14.5 (4.3) | 13.9 (3.9) | 13.7 (2.9) |
| Age 1st used heroin (SD)*** | 17.4 (3.0) | 17.6 (2.8) | 20.6 (3.9) | 18.5 (2.9) | 18.3 (3.2) |
| Age 1st used heroin regularly (SD)*** | 19.1 (3.5) | 18.9 (2.9) | 21.5 (3.8) | 20.2 (2.7) | 19.2 (3.2) |
| Age last used heroin (SD)*** | 47.0 (10.5) | 46.6 (10.6) | 36.9 (10.8) | 45.7 (9.6) | 40.7 (11.7) |
| Age 1st arresta** | 16.0 (4.3) | 17.0 (3.1) | 18.9 (4.1) | 17.0 (2.9) | 16.6 (3.5) |
| Age at baseline interview (SD) *** | 32.7 (6.1) | 31.3 (4.1) | 29.4 (3.6) | 30.6 (4.7) | 28.9 (4.1) |
| Age at follow-up interview (SD)*** | 58.7 (6.0) | 57.6 (4.4) | 55.7 (3.7) | 56.7 (4.7) | 55.0 (4.2) |
| Treatment/Incarceration | |||||
| % time in MMT* | 0.21 (0.2) | 0.32 (0.2) | 0.25 (0.3) | 0.24 (0.2) | 0.30 (0.3) |
| % time in other treatment | 0.04 (0.1) | 0.02 (0.1) | 0.02 (0.1) | 0.02 (0.1) | 0.03 (0.1) |
| % time incarcerated*** | 0.24 (0.2) | 0.12 (0.1) | 0.04 (0.1) | 0.21 (0.2) | 0.05 (0.1) |
| Alcohol & Other Drug Use b | |||||
| % time using heroin*** | 0.67 (0.3) | 0.63 (0.2) | 0.38 (0.3) | 0.63 (0.3) | 0.49 (0.3) |
| % time using marijuana*** | 0.04 (0.1) | 0.17 (0.2) | 0.18 (0.3) | 0.35 (0.2) | 0.57 (0.3) |
| % time using cocaine*** | 0.03 (0.1) | 0.15 (0.2) | 0.11 (0.2) | 0.11 (0.1) | 0.16 (0.2) |
| % time using other opioids** | 0.01 (0.0) | 0.01 (0.1) | 0.03 (0.1) | 0.04 (0.1) | 0.07 (0.2) |
| % time using amphetamines*** | 0.01 (0.0) | 0.04 (0.1) | 0.13 (0.2) | 0.04 (0.1) | 0.11 (0.2) |
| % time using alcohol*** | 0.07 (0.1) | 0.37 (0.2) | 0.51 (0.3) | 0.19 (0.2) | 0.42 (0.3) |
| % time using AOD*** | 0.13 (0.1) | 0.52 (0.1) | 0.71 (0.1) | 0.51 (0.2) | 0.91 (0.1) |
p < .10
p < .05
p < .01
p < .001
19 people had never been arrested
% time during non-institutionalized periods
The “low use” group spent the least time in MMT (21%), whereas the “late-onset increase” and the “no decrease” groups spent the most. The “low use” group spent the most time incarcerated (24%), and the “early-onset increase” and “no decrease” groups spent the least.
3.3. Probability of membership in trajectory groups
Table 3A shows probability of membership in the heroin-use groups conditional on AOD group. Among those in the “low use” AOD group, about half (51%) were in the “gradual decrease” heroin use group. Individuals in the “late-onset increase” AOD use group were about equally likely to be in the “gradual decrease” or “no decrease” heroin use groups. Among those in the “early-onset increase” AOD group, 55% were in the “rapid decrease” heroin use group, suggesting that decreases in heroin use were accompanied by increases in alcohol and/or other drug use for a majority of this group. A majority of those in the “gradual decrease” AOD use group were also in the “gradual decrease” heroin use group. Lastly, among those in the “no decrease” AOD use group, about one third each were in the “rapid decrease” or “no decrease” heroin use groups, suggesting highly divergent patterns within this group.
Table 3A.
Probability of heroin use group conditional on AOD use group.
| AOD Use Trajectory Groups | |||||
|---|---|---|---|---|---|
| Heroin Use Trajectory Groups |
Low Use (n = 63) |
Late-onset Increase (n = 77) |
Early-onset Increase (n = 86) |
Gradual Decrease (n = 60) |
No Decrease (n = 55) |
| Rapid Decrease (n = 84) |
0.12 | 0.10 | 0.54 | 0.08 | 0.31 |
| Moderate Decrease (n = 50) |
0.14 | 0.13 | 0.13 | 0.15 | 0.23 |
| Gradual Decrease (n = 120) |
0.51 | 0.39 | 0.13 | 0.63 | 0.16 |
| No Decrease (n = 87) |
0.23 | 0.38 | 0.20 | 0.14 | 0.30 |
|
| |||||
| 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| Table 3B Probability of AOD use group conditional on heroin use group. | ||||||
|---|---|---|---|---|---|---|
| AOD Use Trajectory Groups | ||||||
| Heroin Use Trajectory Groups |
Low Use (n = 63) |
Late-onset Increase (n = 77) |
Early-onset Increase (n = 86) |
Gradual Decrease (n = 60) |
No Decrease (n = 55) |
|
| Rapid Decrease (n = 84) |
0.09 | 0.09 | 0.55 | 0.06 | 0.21 | 1.00 |
| Moderate Decrease (n = 50) |
0.17 | 0.19 | 0.22 | 0.17 | 0.25 | 1.00 |
| Gradual Decrease (n = 120) |
0.27 | 0.25 | 0.09 | 0.32 | 0.07 | 1.00 |
| No Decrease (n = 87) |
0.17 | 0.33 | 0.20 | 0.09 | 0.20 | 1.00 |
| Table 3C Joint probability of heroin and AOD use groups. | ||||||
|---|---|---|---|---|---|---|
| AOD Use Trajectory Groups | ||||||
| Heroin Use Trajectory Groups |
Low Use (n = 63) |
Late-onset Increase n = 77) |
Early-onset Increase (n = 86) |
Gradual Decrease (n = 60) |
No Decrease (n = 55) |
Row Percents |
| Rapid Decrease (n = 84) |
0.02 | 0.02 | 0.13 | 0.01 | 0.05 | 0.23 |
| Moderate Decrease (n = 50) |
0.03 | 0.03 | 0.03 | 0.03 | 0.04 | 0.16 |
| Gradual Decrease (n = 120) |
0.10 | 0.09 | 0.03 | 0.11 | 0.03 | 0.36 |
| No Decrease (n = 87) |
0.04 | 0.08 | 0.05 | 0.03 | 0.05 | 0.25 |
|
| ||||||
| Column Percents | 0.19 | 0.22 | 0.24 | 0.18 | 0.17 | 1.00 |
Table 3B shows the probability of AOD use trajectory group membership contingent on heroin use groups. Among those in the “rapid decrease” heroin use group, 55% were in the “early-onset” AOD use group, again suggesting that a majority of this group increased AOD use concurrent with their reduction in heroin use. The “moderate decrease” heroin use group was diversified across the AOD use groups. Similarly, the “gradual decrease” heroin use group was diversified, with about one third in the “gradual decrease” AOD use group, 27% in the “low use” AOD group, and 25% in the “late-onset increase” AOD group. Lastly, one third of those in the “no decrease” heroin use group were in the “late-onset” AOD use group, and 20% each were in the “early-onset increase” and “no decrease” AOD use groups.
Table 3C shows the probability of membership in each of the 20 joint heroin and AOD trajectory groups and thus represents the distribution of longitudinal patterns of heroin and AOD use over time. Overall, the joint patterns of use were highly diversified, with only 3 groups each comprising 10% or more of the sample. The group with highest joint membership (13%) was the “rapid decrease” heroin use group and the “early-onset increase” AOD use group. About 11% of the sample was jointly in the heroin and AOD “gradual decrease” groups. Another 10% of the sample was in the joint “gradual decrease” heroin and “low use” AOD group. Lastly, about 8% of the sample was in the joint “no decrease” heroin use and “late-onset increase” AOD use group, suggesting that this group maintained a consistent level of heroin use as well as increasing levels of AOD use over time.
4. Discussion
Few studies have examined the status of heroin users as they enter into middle- and older-age (Rosen et al., 2011). This study identified distinctive trajectory patterns of heroin and AOD use over a 30-year period among men and women who were originally participants in methadone treatment in California in the 1970s. About two fifths of the sample ceased heroin use within 10 – 20 years of initiation. Over half used more consistently over the 30 years, including about one quarter who were using at the time of follow-up. Among those who stopped heroin use most rapidly, over half increased their use of AOD (particularly amphetamines) over time. Moreover, women were significantly more likely to be in this group as compared with those who decreased heroin use more gradually or not at all.
The finding that gender is an important covariate of longitudinal patterns of heroin and other drug use was obscured in previous studies of male heroin users. It is consistent with other research showing higher rates of remission from alcohol among women than men over periods ranging up to 16 years (Grella et al., 2010; Chi and Weisner, 2008; Moos et al., 2006). Additionally, other studies have shown high rates of polydrug use and comorbidity among heroin users, particularly women, in both treatment (Best et al., 2008; Brecht et al., 2008; Rounsaville et al., 1982) and population-based (Grella et al., 2009) samples, however, few studies have examined jointly changes in use of heroin and other drugs over time.
The two groups that persisted in using heroin the longest were characterized by relatively higher levels of childhood conduct problems and adult antisocial personality disorder. Individuals in these groups were youngest at heroin use initiation and at first arrest and spent the most time incarcerated. This profile suggests that their drug use and criminal involvement may be associated with an underlying psychopathology that stems from childhood (Darke et al., 1994; Luther et al., 1996). Moreover, such individuals may be less responsive to treatment (Brooner et al., 1997). Distinctions among these use trajectories may correspond to underlying typologies of heroin users, differentiated by age of onset, childhood risk factors, severity, and psychopathology, much as distinctions among alcoholics with differing profiles have been identified (Babor et al., 1992).
4.1. Study limitations and strengths
Several factors related to the study design need to be considered in the interpretation of findings. The sample's origin from methadone treatment in California limits the generalizability of study findings. Previous studies have shown good reliability and validity of data collected through the retrospective timeline approach (Chou et al., 1996) and good concordance with other longitudinal measures of drug-use status (Murphy et al., 2010). However, undoubtedly there were errors of recall in the frequency or timing of events over the follow-up period. In addition, the timeline data was aggregated such that use periods were based on average number of months used in a given year. Similarly, alcohol and/or other drug use was aggregated and does not indicate the specific drugs that were used in a given year (although percentage of time using specific substances indicates relative magnitude of use among the trajectory groups). Lastly, the resultant follow-up sample is inherently subject to “survivor bias.” It is noteworthy that those subjects who were deceased had rated their health more poorly at the baseline interview.
Yet the study also has several important strengths. Chief among these is the availability of background information and comparable natural history data from the original baseline assessment, which enabled us to examine distal events as predictors of longitudinal trajectory patterns. Moreover, the follow-up interview completion rate of 71% over a period of approximately 25 years is comparable to follow-up rates achieved in other studies of heroin users over much shorter durations (Darke et al., 2007b).
4.2. Conclusion
The study findings have several implications for clinical practice and policy. The significance of childhood behavioral problems and early onset of heroin use, and their relationship with longitudinal drug use patterns, supports the importance of early intervention to address childhood conduct problems. The greater involvement in methadone treatment among individuals who sustained heroin use the longest confirms the importance of opiate-substitution therapy for individuals who are at high risk of relapse and overdose. Moreover, the relatively high rates of persistent drug use over the follow-up period suggest that many aging heroin users are in need of treatment interventions.
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplementary materials for this article can be found by accessing the online version of this paper at http://dx.doi.org by entering doi:…
See online Supplement 1 for table summarizing prior longitudinal studies on opiate users in the United States.
7 subjects participated in both studies; unduplicated N = 914
4 subjects included in the analysis had data for 29 years only and were missing on year 30; 2 additional subjects were missing data on the natural history interview and were deleted from the trajectory analyses.
The baseline natural history interview recorded the number of months in which heroin was used in the segment, but did not capture frequency of use. Although the follow-up interview did assess frequency of use per month, to maintain a continuous timeline over the merged baseline and follow-up periods, all months were coded based on the average number of months each drug was used in the segment, in the manner described.
Information on BIC for the heroin and AOD use trajectory groups is available online in Supplement 2.
References
- Anglin MD, Hser YI, Grella CE, Longshore D, Prendergast ML. Drug treatment careers: conceptual overview and clinical, research, and policy applications. In: Tims FM, Leukefeld CG, Platt JJ, editors. Relapse and Recovery in Addictions. Yale University Press; New Haven and London: 2001. pp. 18–39. [Google Scholar]
- Anglin MD, Speckart GR, Booth MW, Ryan TM. Consequences and costs of shutting off methadone. Addict. Behav. 1989;14:307–326. doi: 10.1016/0306-4603(89)90062-2. [DOI] [PubMed] [Google Scholar]
- Babor TF, Hofmann M, DelBoca FK, Hesselbrock V, Meyer RE, Dolinsky ZS, Rounsaville B. Types of alcoholics, I: evidence for an empirically derived typology based on indicators of vulnerability and severity. Arch. Gen. Psychiatry. 1992;49:599–608. doi: 10.1001/archpsyc.1992.01820080007002. [DOI] [PubMed] [Google Scholar]
- Best DW, Ghufran S, Day E, Ray R, Loaring J. Breaking the habit: a retrospective analysis of desistance factors among formerly problematic heroin users. Drug Alcohol Rev. 2008;27:619–624. doi: 10.1080/09595230802392808. [DOI] [PubMed] [Google Scholar]
- Brecht ML, Huang D, Evans E, Hser YI. Polydrug use and implications for longitudinal research: ten-year trajectories for heroin, cocaine, and methamphetamine users. Drug Alcohol Depend. 2008;96:193–201. doi: 10.1016/j.drugalcdep.2008.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooner RK, King VL, Kidorf M, Schmidt CW, Bigelow GE. Psychiatric and substance use comorbidity among treatment-seeking opioid abusers. Arch. Gen. Psychiatry. 1997;54:71–80. doi: 10.1001/archpsyc.1997.01830130077015. [DOI] [PubMed] [Google Scholar]
- Calabria B, Degenhardt L, Briegleb C, Vos T, Hall W, Lynskey M, Callaghan B, Rana U, McLaren J. Systematic review of prospective studies investigating “remission” from amphetamine, cannabis, cocaine or opioid dependence. Addict. Behav. 2010;35:741–749. doi: 10.1016/j.addbeh.2010.03.019. [DOI] [PubMed] [Google Scholar]
- Chi FW, Weisner CM. Nine-year psychiatric trajectories and substance use outcomes: an application of the group-based modeling. Eval. Rev. 2008;32:39–58. doi: 10.1177/0193841X07307317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou CP, Hser YI, Anglin MD. Pattern reliability of narcotics addicts' self-reported data: a confirmatory assessment of construct validity and consistency. Subst. Use Misuse. 1996;31:1189–1216. doi: 10.3109/10826089609063972. [DOI] [PubMed] [Google Scholar]
- Darke S, Degenhardt L, Mattick R. Mortality Amongst Illicit Drug Users: Epidemiology, Causes and Intervention. Cambridge University Press; Cambridge: 2007a. [Google Scholar]
- Darke S, Ross J, Teesson M. The Australian Treatment Outcome Study (ATOS): what have we learnt about treatment for heroin dependence? Drug Alcohol Rev. 2007b;26:49–54. doi: 10.1080/09595230601036986. [DOI] [PubMed] [Google Scholar]
- Darke S, Hall WD, Swift W. Prevalence, symptoms and correlates of antisocial personality disorder among methadone maintenance clients. Drug Alcohol Depend. 1994;34:253–257. doi: 10.1016/0376-8716(94)90164-3. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Edition (SCID-I/P, version 2.0, 4/97 revision) New York State Psychiatric Institute, Biometrics Research Department; New York: 1997. [Google Scholar]
- Goldstein A, Herrera J. Heroin addicts and methadone treatment in Albuquerque: a 22-year follow-up. Drug Alcohol Depend. 1995;40:139–150. doi: 10.1016/0376-8716(95)01205-2. [DOI] [PubMed] [Google Scholar]
- Grella CE, Joshi V. Gender differences in drug treatment careers among clients in the national Drug Abuse Treatment Outcome Study. Am. J. Drug Alcohol Abuse. 1999;25:385–406. doi: 10.1081/ada-100101868. [DOI] [PubMed] [Google Scholar]
- Grella CE, Karno MP, Warda US, Niv N, Moore AA. Gender and comorbidity among individuals with opioid use disorders in the NESARC Study. Addict. Behav. 2009;34:498–504. doi: 10.1016/j.addbeh.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE, Stein JA, Weisner C, Chi F, Moos R. Predictors of longitudinal substance use and mental health outcomes for patients in two integrated service delivery systems. Drug Alcohol Depend. 2010;110:92–100. doi: 10.1016/j.drugalcdep.2010.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hser YI, Anglin MD. Addiction treatment and recovery careers. In: Kelly JF, White WL, editors. Addiction Recovery Management: Theory, Research, and Practice. Springer; New York: 2010. [Google Scholar]
- Hser YI, Anglin MD, McGlothlin W. Sex differences in addict careers: 1. Initiation of use. Am. J. Drug Alcohol Abuse. 1987;13:33–57. doi: 10.3109/00952998709001499. [DOI] [PubMed] [Google Scholar]
- Hser YI, Anglin MD, Grella C, Longshore D, Prendergast M. Drug treatment careers: a conceptual framework and existing research findings. J. Subst. Abuse Treat. 1997;14:543–558. doi: 10.1016/s0740-5472(97)00016-0. [DOI] [PubMed] [Google Scholar]
- Hser YI, Evans E, Huang D, Brecht ML, Li L. Comparing the dynamic course of heroin, cocaine, and methamphetamine use over 10 years. Addict. Behav. 2008;33:1581–1589. doi: 10.1016/j.addbeh.2008.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hser YI, Hoffman V, Grella CE, Anglin MD. A 33-year follow-up of narcotics addicts. Arch. Gen. Psychiatry. 2001;58:503–508. doi: 10.1001/archpsyc.58.5.503. [DOI] [PubMed] [Google Scholar]
- Hser YI, Huang Y, Chou C-P, Anglin MD. Trajectories of heroin addiction: growth mixture modeling results based on a 33-year follow-up study. Eval. Rev. 2007a;31:548–563. doi: 10.1177/0193841X07307315. [DOI] [PubMed] [Google Scholar]
- Hser YI, Longshore D, Anglin MD. The life course perspective on drug use: a conceptual framework for understanding drug use trajectories. Eval. Rev. 2007b;31:515–547. doi: 10.1177/0193841X07307316. [DOI] [PubMed] [Google Scholar]
- Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol. Method Res. 2001;29:374–393. [Google Scholar]
- Luthar SS, Cushing G, Rounsaville BJ. Gender differences among opioid abusers: pathways to disorder and profiles of psychopathology. Drug Alcohol Depend. 1996;43:179–190. doi: 10.1016/s0376-8716(96)01310-5. [DOI] [PubMed] [Google Scholar]
- Maddux JF, Desmond DP. Careers of Opioid Users. Praeger; New York: 1981. [Google Scholar]
- Maddux JF, Desmond DP. Ten-year follow-up after admission to methadone maintenance. Am. J. Drug Alcohol Abuse. 1992;18:289–303. doi: 10.3109/00952999209026068. [DOI] [PubMed] [Google Scholar]
- McGlothlin WH, Anglin MD. Shutting off methadone: costs and benefits. Arch. Gen. Psychiatry. 1981;38:885–892. doi: 10.1001/archpsyc.1981.01780330043004. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos BS, Timko C. Gender, treatment and self-help in remission from alcohol use disorders. Clin. Med. Res. 2006;4:163–174. doi: 10.3121/cmr.4.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy DA, Hser YI, Huang D, Brecht M-L, Herbeck DM. Self-report of longitudinal substance use: a comparison of the UCLA Natural History Interview and the Addiction Severity Index. J. Drug Issues. 2010;40:495–515. doi: 10.1177/002204261004000210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagin D. Analyzing developmental trajectories: a semi-parametric, group-based approach. Psychol. Methods. 1999;4:139–177. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- Nagin D. Group-based Modeling of Development. Harvard University Press; Cambridge, MA: 2005. [Google Scholar]
- Nagin DS, Tremblay RE. Analyzing developmental trajectories of distinct but related behaviors: a group-based method. Psychol. Methods. 2001;6:18–34. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- Nurco DN, Balter MB, Kinlock T. Vulnerability to narcotics addiction: preliminary findings. J. Drug Issues. 1994;24:293–314. [Google Scholar]
- Nurco DN, Bonito AJ, Lerner M, Balter MB. Studying addicts over time: methodology and preliminary findings. Am. J. Drug Alcohol Abuse. 1975;2:183–196. doi: 10.3109/00952997509002733. [DOI] [PubMed] [Google Scholar]
- Nurco DN, Cisin IH, Balter MB. Addict careers. I. A new typology. Int. J. Addict. 1981a;16:1305–1325. doi: 10.3109/10826088109039189. [DOI] [PubMed] [Google Scholar]
- Nurco DN, Cisin IH, Balter MB. Addict careers. II. The first ten years. Int. J. Addict. 1981b;16:1327–1356. doi: 10.3109/10826088109039190. [DOI] [PubMed] [Google Scholar]
- Nurco DN, Hanlon TE, O'Grady KE, Kinlock TW. The early emergence of narcotic addict types. Am. J. Drug Alcohol Abuse. 1997;23:523–542. doi: 10.3109/00952999709016893. [DOI] [PubMed] [Google Scholar]
- Nurco D, Lerner M. Vulnerability to narcotic addiction: family structure and functioning. J. Drug Issues. 1996;26:1007–1025. [Google Scholar]
- O'Donnell JA. A follow-up of narcotic addicts: morality, relapse and abstinence. Am. J. Orthopsychiatry. 1964;34:948–954. doi: 10.1111/j.1939-0025.1964.tb02251.x. [DOI] [PubMed] [Google Scholar]
- O'Donnell JA. Narcotic Addicts in Kentucky (U.S.P.H.S. Publication No. 1881) U.S. Government Printing Office; Washington, DC: 1969. [Google Scholar]
- Rosen D, Hunsaker A, Albert SM, Cornelius JR, Reynolds CF. Characteristics and consequences of heroin use among older adults in the United States: a review of the literature, treatment implications, and recommendations for further research. Addict. Behav. 2011;36:279–285. doi: 10.1016/j.addbeh.2010.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rounsaville BJ, Weissman MM, Kleber H, Wilber C. Heterogeneity of psychiatric diagnosis in treated opiate addicts. Arch. Gen. Psychiatry. 1982;39:161–166. doi: 10.1001/archpsyc.1982.04290020027006. [DOI] [PubMed] [Google Scholar]
- Simpson DD, Joe GW, Lehman WE, Sells SB. Addiction careers: etiology, treatment, and 12-year follow-up outcomes. J. Drug Issues. 1986;16:107–122. [Google Scholar]
- Vaillant GE. The natural history of narcotic drug addiction. Semin. Psychiatry. 1970;2:486–498. [PubMed] [Google Scholar]
- Winick C. Some aspects of careers of chronic heroin users. In: Josephson E, Carroll EE, editors. Drug Use: Epidemiological and Sociological Approaches. John Wiley; New York: 1974. pp. 105–128. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.