Abstract
Purpose
Patients with high grade gliomas (HGG) routinely receive radiation, temozolomide, and glucocorticoids. As each of these is immunosuppressive, we conducted a prospective, multicenter study to follow CD4 counts over time and determine if low CD4 counts were associated with adverse outcomes.
Experimental design
Patients with newly diagnosed HGG had CD4 counts drawn before initiating standard therapy and monthly thereafter for one year. Information on hospitalizations, infections, glucocorticoid use, survival, and cause of death were also collected.
Results
Ninety-six evaluable patients were accrued (85% glioblastoma, median age of 57, median KPS 90). The median CD4 count before radiation and temozolomide was 664 cells/mm3. The CD4 count nadir occurred 2 months after initiating therapy when 73% of patients had CD4 counts <300 cells/mm3 and 40% had <200 cells/mm3. CD4 counts remained low throughout the year of follow-up. Patients with CD4 counts <200 cells/mm3 at 2 months had shorter survival than those with higher counts (median 13.1 versus 19.7 months, p=0.002). Median survival was related to CD4 toxicity grades (I=23.8 months, II=19.7 months, III–IV=13.1 months, p=0.009). The adjusted hazard ratio for death attributable to 2-month CD4 count below 200 was 1.66 (p=0.03). Eighty-eight percent of deaths resulted from disease progression while only 2.5% were due to infection.
Conclusions
Severe reductions in CD4 counts in patients with newly diagnosed HGG treated with radiation and temozolomide are common, treatment-related, long-lasting, and associated with early death from tumor progression.
Keywords: CD4 counts, immunosuppression, glioblastoma, high grade glioma, temozolomide
INTRODUCTION
Most patients with high grade gliomas receive glucocorticoids, radiation, and chemotherapy as part of their therapeutic regimen. Each of these treatment modalities is toxic to lymphocytes and their combined use can result in substantial immunosuppression and opportunistic infections. Pneumocystis jiroveci pneumonia (PJP), formerly known as Pneumocystis carinii pneumonia (PCP), occurs in severely immunosuppressed patients. This infection is caused by a unicellular fungus which exists in the respiratory tract of healthy mammals and humans throughout the world. It is a major cause of life-threatening illness in patients with acquired immune deficiency syndrome (AIDS) and solid-organ transplant recipients treated with potent immunosuppressive agents.(1, 2) PJP also occurs in patients with lymphoma or leukemia following chemotherapy.(3–10)
PJP has also been noted with increasing frequency in patients with primary brain tumors.(11) CD4 counts were found to be severely reduced in individual patients with high grade gliomas and PJP at the Johns Hopkins Hospital. These observations prompted a study measuring CD4 counts before and during radiation in patients with newly diagnosed high grade gliomas treated only with glucocorticoids and radiation.(12) Chemotherapy was not administered as this study was conducted before temozolomide was known to be efficacious in this patient population. We found that CD4 counts began in the normal range but fell rapidly. After six weeks of radiation, 47% of patients had CD4 counts <300 cells/mm3 and 26% of patients had CD4 counts <200 cells/mm3.
In 2005, temozolomide was shown to have a substantial survival benefit in patients with glioblastoma when administered daily during radiation and for five days each month for six months thereafter.(13) Given the paucity of other efficacious therapies, this regimen quickly became standard therapy for this disease. Prophylactic antibiotics are recommended as earlier experience in combining temozolomide and radiation in patients with high grade gliomas was associated with PJP and a high mortality rate.(14) As reductions in CD4 counts are observed following radiation and glucocorticoid administration, and temozolomide is known to be toxic to CD4 lymphocytes(15), we hypothesized that adding temozolomide to the treatment of all patients with high grade gliomas could result in further immunosuppression and infectious complications. In addition, information on treatment-related immunosuppression is needed to guide immunologically based clinical trials in patients with brain tumors. The study we report here is a federally funded, prospective, multicenter investigation which followed patients with high grade gliomas receiving standard radiation, temozolomide, and glucocorticoids to determine the frequency and severity of immunosuppression, as monitored by CD4 counts, and the association between low CD4 counts and infections or other adverse outcomes.
MATERIALS AND METHODS
This study was conducted by the New Approaches to Brain Tumor Therapy (NABTT) CNS Consortium and funded by the National Institutes of Health through the National Cancer Institute (NIH: CA-62475 New Approaches to Brain Tumor Therapy CNS Consortium (PI Grossman). Participating institutions included the Johns Hopkins University, Wake Forest University and the H. Lee Moffitt Cancer Center. This study was reviewed and approved by the National Cancer Institute and the institutional review board of each participating institution.
This study was designed to prospectively monitor CD4 counts in patients with newly diagnosed high grade glioma before, during, and after the administration of standard radiation, temozolomide, glucocorticoids, and PJP prophylaxis. The specific objectives of the study were to determine: 1) the frequency and severity of CD4 count reductions and 2) the relationship between reduced CD4 counts and significant infections or other adverse outcomes.
Eligible patients were at least 18 years of age with newly diagnosed, histologically confirmed anaplastic astrocytoma (WHO Grade III), anaplastic oligodendroglioma (WHO Grade III) or glioblastoma multiforme (WHO Grade IV) who were to receive standard radiation and temozolomide. Eligible patients were permitted to have had prior surgery with or without placement of Gliadel® wafers (polifeprosan 20 with carmustine implant, Eisai Inc) and glucocorticoids as required for control of peritumoral edema. Patients were required to have a Karnofsky performance status (KPS) of ≥ 60%, a negative HIV serology, and written informed consent. Prior radiation or systemic chemotherapy for their high grade glioma rendered patients ineligible for this study.
This study was designed to have 85% power to detect reductions in CD4 counts to <300 cells/mm3 in 30% of 100 high grade glioma patients receiving radiation and temozolomide versus 5% of 25 low grade glioma patients observed without antineoplastic therapies using a two-sided significance level of 0.05. CD4 counts and complete blood counts with differential and platelet count were monitored monthly. Data were also collected monthly on radiation and chemotherapy treatments, documented infections, hospitalizations, and dexamethasone and antibiotic use. All episodes of pneumonia or inpatient hospitalization prompted a record review to determine if Pneumocystis jiroveci or other opportunistic infections were present. The above information was collected for one year. All patients were followed for survival at least every 2 months.
The original study design included the accrual of 25 patients with newly diagnosed low grade gliomas where observation without glucocorticoids or antineoplastic therapies was planned. This sub-cohort was added to ensure that gliomas were not inherently associated with low CD4 counts. However, early results from the patients with high grade gliomas demonstrated that pre-treatment CD4 counts were within the normal range despite weeks of peri- and post-operative glucocorticoids prior to these patients being enrolled. As these observations answered this question, accrual to the low grade glioma cohort glioma was quickly discontinued and results from this cohort are not included in this report.
The statistical design was based on preliminary observations in high grade gliomas treated with only radiation and glucocorticoids where a reduction in CD4 counts was evident at six weeks.(12) Therefore, the primary outcome measure was chosen to be the proportion of subjects with a CD4 count < 300 cells/mm3 at two months. We also hypothesized that low CD4 counts would be associated with an increased incidence of infection. Furthermore, we intended to explore if there was an association between low CD4 counts and infection or survival. NCI CTCAE 3.0 toxicity classifications were used to define the severity of CD4 count reductions and used for the relevant analyses. These criteria define grade III–IV toxicity as CD4 counts <200 cells/mm3. In the event that a CD4 measurement at two months was missing, the three or one month values were used.
Patient baseline characteristics were summarized using descriptive statistics. The proportion of patients with low CD4 counts at each specific time point was assumed to follow an independent binomial distribution. Overall survival time was calculated from the time of histological diagnosis until death from any cause. Survival time was censored if the subject was alive at the time of last follow-up. Survival probability was estimated using the Kaplan–Meier method.(16)
Univariate analysis was used to assess an association between the known prognostic factors of patients at baseline and overall survival. Important patient characteristics associated with survival were identified in the univariate analysis using a p value of ≤ 0.05. These characteristics were selected as covariates to construct the multivariate proportional-hazards regression model. (17) Karnofsky performance status, an established prognostic factor in high grade gliomas, was added as a covariate to this model. The proportional-hazards regression model was used to estimate the hazard ratio for death attributable to prognostic factors. All p-values are reported as two-sided and all analyses were performed using the SAS software (version 9.1, SAS institute, Cary, NC).
RESULTS
STUDY POPULATION
A total of 103 subjects were accrued to this protocol between August 2004 and July 2008. Seven patients who did not receive temozolomide were excluded from analysis. Data from the remaining 96 subjects who received standard radiation and temozolomide are the focus of this report. Fifty percent of the subjects were female, 95% were Caucasian, and 80% had a debulking surgical procedure (Table 1). The histologic diagnosis was glioblastoma in 85%, anaplastic astrocytoma in 12%, anaplastic oligodendroglioma in 2%, and an otherwise unspecified malignant glioma in 1%. The median age of the subjects was 57 years (range 28–85) and the median KPS was 90. Eighty-one percent of the subjects were prescribed anticonvulsants and 82% were taking glucocorticoids when they began radiation and temozolomide. The average elapsed time between surgery and the initiation of radiation and temozolomide was 3.9 weeks (range 2–12.6). In addition to the standard radiation and temozolomide, 24% of patients received experimental agents. These were non-cytotoxic agents unlikely to affect lymphocyte counts. They included talampanel, an oral glutamate receptor blocker (14 subjects); cilengitide, an integrin antagonist (5 subjects); poly-ICLC, an immunostimulant (3 subjects); and BSI, a PARP inhibitor, (1 subject). Talampanel and cilengitide were initiated on the first day of radiation and temozolomide and continued until tumor progression or toxicity while BSI and poly-ICLC were added in the tenth week of therapy. As this study was designed before the overall importance of MGMT was appreciated, the MGMT status of patients accrued to this multi-institutional study was not evaluated.
Table 1.
Baseline Patient Characteristics
| All patients (N=96) |
Patients with CD4 counts ≥200 at 2 months (N=58) |
Patients with CD4 counts < 200 at 2 months (N=38) |
P-value* | |
|---|---|---|---|---|
| Age: median (range) | 57.4 (28–85) | 56.6 (28–85) | 60.9 (33–78) | 0.07 |
| Age: ≥55 years (%) | 61 (64%) | 35 (60%) | 26 (66%) | 0.42 |
| Sex: Percent male | 48 (50%) | 30 (52%) | 18 (47%) | 0.68 |
| KPS of 80–100: # (%) | 90 (94%) | 53(91%) | 37 (97%) | 0.24 |
| Biopsy only: # (%) | 19 (20%) | 9 (16%) | 10 (26%) | 0.19 |
| Weeks from diagnosis to treatment: median (range) | 3.9 (2–12.6) | 4.2 (2–12.6) | 3.7 (2.3–7.6) | 0.08 |
| Baseline CD4 count: median (range) | 664 (90–2010) | 933 (145–2010) | 401 (90–1309) | 0.0001 |
| Baseline lymphocyte count: median (range) | 1418 (331–4736) | 1645 (672– 4736) | 1044 (331–2790) | 0.0001 |
| Baseline steroid use: # (%) | 79 (82%) | 44 (76%) | 35 (92%) | 0.04 |
| Histology: Glioblastoma # (%) | 81 (84%) | 46 (79%) | 35 (92%) | 0.09 |
comparing subjects with CD4 counts above and below 200 at 2 months
This protocol was a non-interventional study to follow CD4 counts and outcomes with standard radiation and temozolomide. As a result, it did not specify the duration of post-radiation temozolomide which is commonly prescribed for six months or longer. The median time that patients on this multi-institutional study received temozolomide was 5.8 months (STD = ± 3 months). Only four patients (4%) continued on temozolomide for 11 months or more. Eighty-five of the 96 patients (89%) did not have second line chemotherapy during the 12 months they were followed on this study. Of the 11 patients who received salvage chemotherapy during the follow-up period, only two were treated with bevacizumab. Others received BCNU, CCNU, Gliadel wafers, imatinib, IL-13, bortezomib, tamoxifen, and/or a dendritic cell vaccine.
CD4 COUNTS OVER TIME
CD4 counts were reliably obtained from patients on this study. No deaths occurred during the first two months of therapy and all patients had a baseline CD4 count and one or more follow-up CD4 counts during the first three months after beginning radiation and temozolomide.
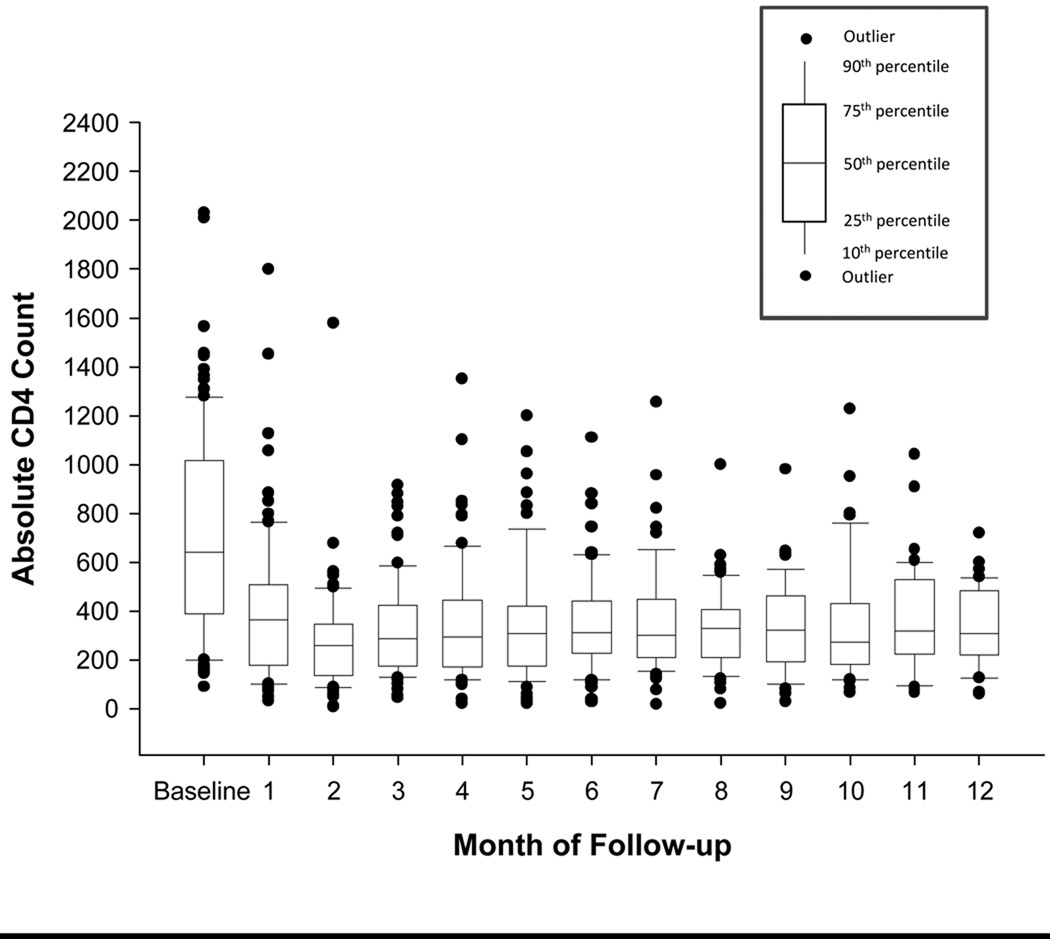
Serial CD4 count results are provided in Figure 1. The median CD4 count in these patients prior to initiating radiation and temozolomide was 664 cells/mm3 (range: 90 to 2010 cells/mm3). Two months after initiating radiation and temozolomide the median CD4 count was 255 cells/mm3 (range: 8–1580 cells/mm3) and subsequent CD4 counts remained persistently low during the 12 months of observation (Figures 1 and 2). The lowest CD4 counts were observed two months after beginning antineoplastic therapy when 70 patients (73% [95% CI: 63–82%]) had CD4 counts below 300 cells/mm3, and 38 (40% [95% CI: 30–50%]) had CD4 counts below 200 cells/mm3. Although there was a wide range of CD4 counts noted at baseline this variability was greatly reduced at two months (Figure 1).
Figure 1.
CD4 Count Trend over Time
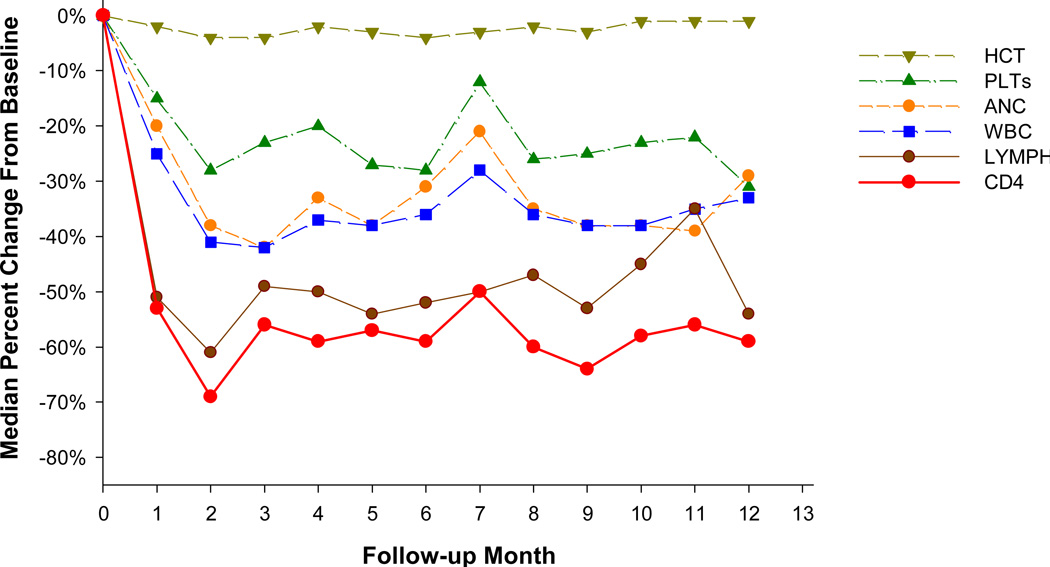
Figure 2.
Percent Decline in Hematologic Values over Time
Age, sex, KPS, extent of surgery, and time from surgery to treatment were not associated with a low post-treatment CD4 count (Table 1). Subjects who developed grade III–IV CD4 count depression had significantly lower CD4 counts (458 vs 887 cells/mm3, p = 0.0001) and total lymphocyte counts (1044 vs 1645 cells/mm3, p =0.001) prior to beginning radiation and temozolomide than those who did not. In addition, they were more likely to be on glucocorticoids (92% vs 76%, p = 0.04) prior to beginning radiation and temozolomide, have a diagnosis of glioblastoma (92% vs 79%, p=0.09), and have had a biopsy rather than resection (26% vs 16% p=0.19).
Two months after initiating radiation and temozolomide, the average absolute reduction in CD4 counts was 476 cells/mm3. The median percent reduction in CD4 counts at two months was 69% in all patients. Patients with baseline CD4 counts of >500 cells/mm3 fell by 72% while those with baseline CD4 counts of <500 cells/mm3 fell by 49%. The reduction in CD4 counts paralleled changes in total lymphocyte counts but was not related to changes in the white blood cell counts, neutrophil counts, platelet counts, or hematocrit (Figure 2). The percent of subjects who developed CD4 counts <200 cells/mm3 was similar in those receiving radiation and temozolomide alone or with the addition of talampanel, cilengitide, BSI, or poly ICLC (42% versus 31%, P=0.4).
INFECTION
A total of 40 subjects (41%) had a documented infection during the12 month study period. Infections were seen in 17 individuals (46%) with CD4 counts that fell below 200 cells/mm3 and in 23 (40%) with CD4 counts that remained above 200 cells/mm3 (p=0.54). Seven subjects developed pneumonia and one of these was diagnosed as PJP despite recommended PJP prophylaxis. Only two of the 81 deaths (2.5%) that occurred in the study population were due to infection, and these occurred in subjects who survived for 11 and 25 months. The median survival time of individuals with infection was 16.8 months (95% CI: 15.2 – 20.7 months) and of those without infection was 17.8 months (95% CI: 13.2 – 23.5 months). Also, time-to-first-infection was assessed as a time dependent covariate in a univariate and a multivariate proportional hazards model. After adjusting for baseline age, surgical procedure, histology, KPS, and CD4 counts (greater than or less than 200 cells/mm3), the adjusted hazard ratio for death attributed to infection was 1.16 (95% CI: 0.73–1.83; p=0.5, Table 2).
Table 2.
Associations between Patient Characteristics and Survival:
| Characteristic | Hazard Ratio (95% CI) | p-value |
|---|---|---|
| Univariable Association | ||
| Histology: GBM vs. other | 3.28 (1.50–7.17) | 0.003 |
| Biopsy vs. Craniotomy | 2.22 (1.31–3.78) | 0.003 |
| CD4 count at baseline: <500 vs. ≥500* | 2.07 (1.32–3.24) | 0.002 |
| CD4 count at 2 months: <200 vs. 200* | 1.99 (1.27–3.11) | 0.003 |
| KPS: 60–70 vs. 80–100 | 1.95 (0.78–4.87) | 0.15 |
| Age: ≥55 vs. <55 | 1.73 (1.08–2.77) | 0.02 |
| Anticonvulsant Use : yes vs. no | 1.47 (0.85–2.54) | 0.17 |
| Steroids Use: yes vs. no | 1.09 (0.60–1.98) | 0.78 |
| Infection ** | 1.04 (0.07–1.61) | 0.86 |
| Multivariable Association | ||
| Histology: GBM vs. other | 3.39 (1.43–8.02) | 0.006 |
| KPS: 60–70 vs. 80–100 | 3.18 (1.18–8.56) | 0.022 |
| Biopsy vs. Craniotomy | 2.30 (1.31–4.04) | 0.004 |
| CD4 count at 2 months: <200 vs. 200* | 1.66 (1.05–2.64) | 0.03 |
| Age: ≥55 vs. <55 | 1.37 (0.83–2.28) | 0.22 |
| Infection** | 1.16 (0.73–1.83) | 0.53 |
CD4 count at baseline is dichotomized at 500 (normal vs abnormal). CD4 count at 2 months is dichotomized at 200
Time dependent covariate (time-to-first-infection)
HOSPITALIZATIONS
Fifty-three of the 96 subjects (55%) were hospitalized during the year of observation. Hospitalizations were more frequent in subjects with CD4 counts <200 cells/mm3 at two months than in those with higher CD4 counts (73% versus 43%, p=0.003). Among those who required hospitalization, the median number of hospitalizations was two (range 1–6) for all CD4 counts, two for those with CD4 counts <200 at 2 months and one for those with higher CD4 counts (p=0.8). The reasons for hospitalization were highly variable and over 50 different admission diagnoses were recorded. Examples included additional surgery, thromboembolic disease, change in mental status or seizures, nausea/vomiting, peripheral edema, fatigue, weakness, pain management, glucose control, constipation, drug allergy, GI bleed, hematoma, meningitis, pneumonia, and spontaneous pneumothorax.
SURVIVAL
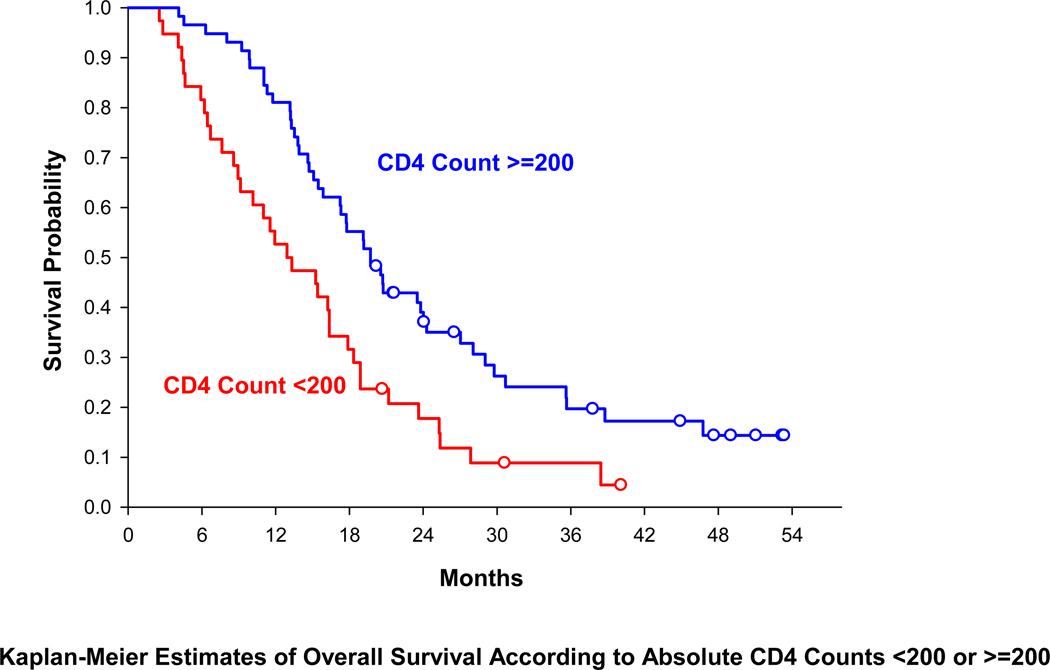
At the time of analysis, 81 of the 96 subjects had died. The overall median survival time was 17.3 months (95% CI: 14.6–19.7 months). The unadjusted and adjusted hazard ratios with respect to the factors associated with overall survival are listed in Table 2. As shown in Table 2, an analysis of the unadjusted hazard ratio for death identified previously known prognostic factors for patients with high grade gliomas: histology (GBM vs other high grade gliomas, p = 0.003), extent of surgery (biopsy vs craniotomy, p = 0.003), and age (≥55 vs <55, p = 0.02). Baseline CD4 counts (<500 vs ≥500, p=0.002) and CD4 counts at 2 months (<200 vs ≥200, p=0.003) were identified as related to survival. The median survival time in patients with CD4 counts <200 cells/mm3 at two months was 13.1 months (95% CI: 9.1–16.4) compared to 19.7 months (95% CI: 15.9–24.0) in subjects with higher CD4 counts (p=0.002, log-rank test). The relevant Kaplan Meier survival curves are presented in Figure 3 (hazard rate = 1.99, 95% CI: 1.27–3.1).
Figure 3.
Overall Survival by CD4 Count at 2 Months
Legend for Figure 3: Survival in patients with CD4 counts <200 cells/mm3 at two months was substantially different from those with higher CD4 counts as measured by median survival (13.1 months (95% CI: 9.1–16.4) versus to 19.7 months (95% CI: 15.9–24.0)), log rank test (p=0.002, log-rank test), or the adjusted hazard ratio for death (1.66 (p=0.03)).
A proportional hazards model was constructed to estimate the risk of death attributed to low CD4 count at two months while accounting for known baseline clinical prognostic factors (Table 2). Covariates entered into this model included those identified in the univariate analysis (histology, surgical procedure, age and baseline and two month CD4 counts) as well as KPS and infection. The adjusted hazard ratio for death for three known prognostic factors were confirmed in this model: histology (GBM vs other) = 3.39 (p = 0.006), surgical procedure (biopsy vs craniotomy) = 2.3 (p=0.004), and KPS (60–70 vs 80–100) = 3.18 (p=0.02). The adjusted hazard ratio for death attributable to baseline CD4 count (dichotomized at 500) was 1.29 (p=0.38). The corresponding hazard ratio attributable to CD4 count at 2 months (dichotomized at 200) was 1.66 (p=0.03) after two months of therapy. Further analysis revealed that survival was related to the CTC toxicity grades for CD4 counts at two months. The median survival of patients who developed Grade I (n=9), Grade II (n=49) and Grade III–IV (n=38) reductions in CD4 counts at two months were 23.8 months, 19.7 months, and 13.1 months respectively (p=0.009). A common hazard ratio for death with respect to the severity of the toxicity grade (per unit increase) was 1.7 (95% CI: 1.13 to 2.54, p=0.01) after adjusting for age, surgical procedure, histology, and KPS.
DISCUSSION
This is the first study to follow serial CD4 counts in patients with newly diagnosed high grade gliomas treated with radiation and temozolomide and to correlate the findings with clinical outcomes. Despite weeks of peri- and post-operative glucocorticoids, CD4 counts in these patients were usually within the normal range before radiation and temozolomide were started. This suggests that the disease itself is not associated with marked immunosuppression. These findings are consistent with a previous report of patients with newly diagnosed glioblastoma treated with radiation, glucocorticoids, but no chemotherapy.(12) In these patients CD4 counts began in the normal range but after six weeks of radiation 47% had CD4 counts <300 cells/mm3 and 26% had <200 cells/mm3. In the study reported in this manuscript where temozolomide was added to radiation and glucocorticoids, 73% of patients had <300 cells/mm3 and 40% had <200 CD4 cells/mm3 two months after initiating therapy. Patients with the lowest CD4 counts at two months were more likely to have begun radiation and temozolomide with lower total lymphocyte and CD4 counts. In most subjects, this Grade III–IV toxicity persisted for the full year of follow-up. Subjects with CD4 counts below 200 cells/mm3 two months after beginning radiation and temozolomide had significantly shorter survival than others after adjusting for known prognostic factors. Remarkably, the cause of death in these study subjects was early tumor progression and was unrelated to opportunistic infection.
The significant reduction in CD4 counts observed in this study is consistent with available information on the toxicities of the administered agents. Glucocorticoids are potent lympholytic agents and their use has been associated with PJP and other opportunistic infections.(18–21) Lymphocytes are also highly sensitive to the effects of radiation. Although radiation for high grade gliomas is delivered only to the affected region of the brain, modeling studies suggest that there is substantial exposure to circulating lymphocytes as blood flow to the brain is high and the radiation beam is on for approximately 30 minutes during the six weeks of therapy.(22) Finally, temozolomide administered to patients with melanoma as a single agent, without glucocorticoids or radiation, produces profound lymphopenia and a striking reduction in CD4 counts that lasts for months after temozolomide is discontinued.(15) Thus, it is plausible that the combined use of glucocorticoids, radiation, and temozolomide in patients with high grade gliomas results in significant and long lasting reductions in CD4 and total lymphocyte counts that can lead to clinically significant immunologic impairment.
Our findings that low CD4 counts at two months are independently associated with shorter survival are of special concern. Our initial hypothesis was that the addition of temozolomide would result in more highly immunosuppressed patients who would be at risk to develop severe opportunistic infections that might shorten their lives. However, we found that with appropriate PJP prophylaxis serious infections were not a significant cause of death. Instead, patients died early from progressive growth of their high grade gliomas. One potential explanation for this finding is that highly immunocompromised patients were poor prognosis patients with the largest post-operative tumor burden who required higher doses of glucocorticoids. Although this would be consistent with data in Table 1 showing that patients with lower CD4 counts at two months were older (60.9 vs 56.6 years) and more likely to have been biopsied than resected (26% vs 16%), these differences are not statistically significant. As noted in Table 1, patients with lower CD4 counts were more likely to be on glucocorticoids when beginning radiation and temozolomide (92% vs 79%, p=0.04). The extent to which CD4 count depletion is related to glucocorticoid dose is difficult to determine as steroid doses were changed frequently but recorded only every 2 months. However, the multivariable analysis which adjusts for significant prognostic variables demonstrates that the CD4 count at two months was independently associated with survival (Table 2).
An alternative explanation is that the severe immunosuppression noted in 40% of patients treated with this regimen compromises survival. It has long been thought that the immune system plays a significant role in controlling the growth of cancers. This is the basis for a large body of experimental work on tumor vaccines and other immunologic approaches designed to stimulate the immune system to “fight” the cancer. If stimulating the immune system can improve cancer outcomes, it is possible that immunosuppression could compromise the ability of the body to assist in tumor control. In fact, severe immunosuppression has been related to poor outcomes in patients with cancer. More rapid disease progression and shorter survival have been reported in patients with hematologic and solid tumor malignancies and a diminished immune response reflected by reduced total lymphocyte counts(23–26), lack of intra-tumoral lymphocytes at diagnosis (27–29), delayed or incomplete lymphocyte recovery following chemotherapy(30, 31) or autologous bone marrow transplantation.(32–35) Although the correlation of immune status and clinical outcome is well described, the precise biological mechanisms remain poorly defined.
The observations reported in this manuscript suggest that the immune status may play a significant role in survival in patients with high grade gliomas. Additional studies are required to confirm these findings. Our trial, which opened in 2004 as the first to explore the effects of radiation and temozolomide on CD4 counts and patient outcome, did not include detailed immunologic assessments and measurements of lymphocyte subtypes over time. However, now that the depth and duration of treatment-related immunosuppression and its potential relationship to survival have been described, future studies should investigate the immunological consequences of therapy in depth. This is a complex and controversial research topic. Our observations suggest that severe immunosuppression is associated with poor outcomes while other investigators have recently reported that that temozolomide treatment-related lymphopenia might enhance the results of immunotherapy in patients with glioblastoma.(36)
In addition, further studies should also explore if the association that we describe between treatment-induced immunosuppression and poor survival is also present in other systemic malignancies where patients are intensively treated with radiation and chemotherapy. A better understanding of the general consequences of treatment-related lymphopenia and immunosuppression are critical to improving the design and conduct of translational research and improving the outcomes of patients with malignancies.
STATEMENT OF TRANSLATIONAL RELEVANCE.
Patients with high grade gliomas routinely receive radiation, temozolomide, and glucocorticoids. Each of these treatment modalities has been associated with lymphopenia, immunosuppression, and opportunistic infections. CD4 counts were followed for one year in 96 patients with newly diagnosed high grade gliomas to: 1) quantify the degree and duration of treatment-related reductions in CD4 counts and 2) determine if low CD4 counts were associated with adverse outcomes. After two months of treatment, 40% of patients had CD4 counts <200 cells/mm3. These patients continued to have low CD4 counts for the full year of follow-up and died earlier from tumor progression. These findings raise concerns that severe treatment-related lymphopenia may compromise survival in patients with high grade gliomas and perhaps other cancers as well. Further studies of the consequences of treatment-related lymphopenia and immunosuppression could be important to the design and conduct of translational research and improving patient outcomes.
Acknowledgments
Funding : NIH grant # : UO1: CA-62475 New Approaches to Brain Tumor Therapy CNS Consortium (PI Grossman)
Footnotes
Conflict of Interest: None
References
- 1.Masur H. Prevention and treatment of pneumocystis pneumonia. N Engl J Med. 1992;327(26):1853–1860. doi: 10.1056/NEJM199212243272606. [DOI] [PubMed] [Google Scholar]
- 2.Masur H, Lane HC, Kovacs JA, Allegra CJ, Edman JC. NIH conference. pneumocystis pneumonia: From bench to clinic; Ann Intern Med; 1989. pp. 813–826. [DOI] [PubMed] [Google Scholar]
- 3.Arend SM, Kroon FP, van't Wout JW. Pneumocystis carinii pneumonia in patients without AIDS, 1980 through 1993. an analysis of 78 cases. Arch Intern Med. 1995;155(22):2436–2441. [PubMed] [Google Scholar]
- 4.Browne MJ, Hubbard SM, Longo DL, Fisher R, Wesley R, Ihde DC, et al. Excess prevalence of pneumocystis carinii pneumonia in patients treated for lymphoma with combination chemotherapy. Ann Intern Med. 1986;104(3):338–344. doi: 10.7326/0003-4819-104-3-338. [DOI] [PubMed] [Google Scholar]
- 5.Gluck T, Geerdes-Fenge HF, Straub RH, Raffenberg M, Lang B, Lode H, et al. Pneumocystis carinii pneumonia as a complication of immunosuppressive therapy. Infection. 2000;28(4):227–230. doi: 10.1007/s150100070041. [DOI] [PubMed] [Google Scholar]
- 6.Jacobs JL, Libby DM, Winters RA, Gelmont DM, Fried ED, Hartman BJ, et al. A cluster of pneumocystis carinii pneumonia in adults without predisposing illnesses. N Engl J Med. 1991;324(4):246–250. doi: 10.1056/NEJM199101243240407. [DOI] [PubMed] [Google Scholar]
- 7.Mansharamani NG, Balachandran D, Vernovsky I, Garland R, Koziel H. Peripheral blood CD4 + T-lymphocyte counts during pneumocystis carinii pneumonia in immunocompromised patients without HIV infection. Chest. 2000;118(3):712–720. doi: 10.1378/chest.118.3.712. [DOI] [PubMed] [Google Scholar]
- 8.Mansharamani NG, Garland R, Delaney D, Koziel H. Management and outcome patterns for adult pneumocystis carinii pneumonia, 1985 to 1995: Comparison of HIV-associated cases to other immunocompromised states. Chest. 2000;118(3):704–711. doi: 10.1378/chest.118.3.704. [DOI] [PubMed] [Google Scholar]
- 9.Seijo LML, GY Pneumocystis carinii pneumonia among patients without AIDS at a cancer hospital. Pulmonary Medicine. 2000;7(4):170–177. [Google Scholar]
- 10.Sepkowitz KA, Brown AE, Armstrong D. Pneumocystis carinii pneumonia without acquired immunodeficiency syndrome. more patients, same risk. Arch Intern Med. 1995;155(11):1125–1128. [PubMed] [Google Scholar]
- 11.Mahindra AK, Grossman SA. Pneumocystis carinii pneumonia in HIV negative patients with primary brain tumors. J Neurooncol. 2003;63(3):263–270. doi: 10.1023/a:1024217527650. [DOI] [PubMed] [Google Scholar]
- 12.Hughes MA, Parisi M, Grossman S, Kleinberg L. Primary brain tumors treated with steroids and radiotherapy: Low CD4 counts and risk of infection. Int J Radiat Oncol Biol Phys. 2005;62(5):1423–1426. doi: 10.1016/j.ijrobp.2004.12.085. [DOI] [PubMed] [Google Scholar]
- 13.Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987–996. doi: 10.1056/NEJMoa043330. [DOI] [PubMed] [Google Scholar]
- 14.Stupp R, Dietrich PY, Ostermann Kraljevic S, Pica A, Maillard I, Maeder P, et al. Promising survival for patients with newly diagnosed glioblastoma multiforme treated with concomitant radiation plus temozolomide followed by adjuvant temozolomide. J Clin Oncol. 2002;20(5):1375–1382. doi: 10.1200/JCO.2002.20.5.1375. [DOI] [PubMed] [Google Scholar]
- 15.Su YB, Sohn S, Krown SE, Livingston PO, Wolchok JD, Quinn C, et al. Selective CD4+ lymphopenia in melanoma patients treated with temozolomide: A toxicity with therapeutic implications. J Clin Oncol. 2004;22(4):610–616. doi: 10.1200/JCO.2004.07.060. [DOI] [PubMed] [Google Scholar]
- 16.Kaplan EL, Meir P. Nonparametric estimation from incomplete observations. 1958;53:457–481. [Google Scholar]
- 17.Cox DR. Regression models and life-tables. Journal of the Royal Statistical Society Series B. 1972;34:187–220. [Google Scholar]
- 18.Curtis JR, Westfall AO, Allison J, Bijlsma JW, Freeman A, George V, et al. Population-based assessment of adverse events associated with long-term glucocorticoid use. Arthritis Rheum. 2006;55(3):420–426. doi: 10.1002/art.21984. [DOI] [PubMed] [Google Scholar]
- 19.Franklin J, Lunt M, Bunn D, Symmons D, Silman A. Risk and predictors of infection leading to hospitalisation in a large primary-care-derived cohort of patients with inflammatory polyarthritis. Ann Rheum Dis. 2007;66(3):308–312. doi: 10.1136/ard.2006.057265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lichtenstein GR, Feagan BG, Cohen RD, Salzberg BA, Diamond RH, Chen DM, et al. Serious infections and mortality in association with therapies for crohn's disease: TREAT registry. Clin Gastroenterol Hepatol. 2006;4(5):621–630. doi: 10.1016/j.cgh.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 21.McDonough AK, Curtis JR, Saag KG. The epidemiology of glucocorticoid-associated adverse events. Curr Opin Rheumatol. 2008;20(2):131–137. doi: 10.1097/BOR.0b013e3282f51031. [DOI] [PubMed] [Google Scholar]
- 22.Kleinberg L, Grossman SA, Piantadosi S, Zeltzman M, Wharam M. The effects of sequential versus concurrent chemotherapy and radiotherapy on survival and toxicity in patients with newly diagnosed high-grade astrocytoma. Int J Radiat Oncol Biol Phys. 1999;44(3):535–543. doi: 10.1016/s0360-3016(99)00060-7. [DOI] [PubMed] [Google Scholar]
- 23.Lissoni P, Brivio F, Fumagalli L, Messina G, Ghezzi V, Frontini L, et al. Efficacy of cancer chemotherapy in relation to the pretreatment number of lymphocytes in patients with metastatic solid tumors. Int J Biol Markers. 2004;19(2):135–140. doi: 10.1177/172460080401900208. [DOI] [PubMed] [Google Scholar]
- 24.Siddiqui M, Ristow K, Markovic SN, Witzig TE, Habermann TM, Colgan JP, et al. Absolute lymphocyte count predicts overall survival in follicular lymphomas. Br J Haematol. 2006;134(6):596–601. doi: 10.1111/j.1365-2141.2006.06232.x. [DOI] [PubMed] [Google Scholar]
- 25.Ege H, Gertz MA, Markovic SN, Lacy MQ, Dispenzieri A, Hayman SR, et al. Prediction of survival using absolute lymphocyte count for newly diagnosed patients with multiple myeloma: A retrospective study. Br J Haematol. 2008;141(6):792–798. doi: 10.1111/j.1365-2141.2008.07123.x. [DOI] [PubMed] [Google Scholar]
- 26.De Angulo G, Yuen C, Palla SL, Anderson PM, Zweidler-McKay PA. Absolute lymphocyte count is a novel prognostic indicator in ALL and AML: Implications for risk stratification and future studies. Cancer. 2008;112(2):407–415. doi: 10.1002/cncr.23168. [DOI] [PubMed] [Google Scholar]
- 27.Zhang L, Conejo-Garcia JR, Katsaros D, Gimotty PA, Massobrio M, Regnani G, et al. Intratumoral T cells, recurrence, and survival in epithelial ovarian cancer. N Engl J Med. 2003;348(3):203–213. doi: 10.1056/NEJMoa020177. [DOI] [PubMed] [Google Scholar]
- 28.Pages F, Berger A, Camus M, Sanchez-Cabo F, Costes A, Molidor R, et al. Effector memory T cells, early metastasis, and survival in colorectal cancer. N Engl J Med. 2005;353(25):2654–2666. doi: 10.1056/NEJMoa051424. [DOI] [PubMed] [Google Scholar]
- 29.Camus M, Tosolini M, Mlecnik B, Pages F, Kirilovsky A, Berger A, et al. Coordination of intratumoral immune reaction and human colorectal cancer recurrence. Cancer Res. 2009;69(6):2685–2693. doi: 10.1158/0008-5472.CAN-08-2654. [DOI] [PubMed] [Google Scholar]
- 30.Behl D, Porrata LF, Markovic SN, Letendre L, Pruthi RK, Hook CC, et al. Absolute lymphocyte count recovery after induction chemotherapy predicts superior survival in acute myelogenous leukemia. Leukemia. 2006;20(1):29–34. doi: 10.1038/sj.leu.2404032. [DOI] [PubMed] [Google Scholar]
- 31.Porrata LF, Ristow K, Witzig TE, Tuinistra N, Habermann TM, Inwards DJ, et al. Absolute lymphocyte count predicts therapeutic efficacy and survival at the time of radioimmunotherapy in patients with relapsed follicular lymphomas. Leukemia. 2007;21(12):2554–2556. doi: 10.1038/sj.leu.2404819. [DOI] [PubMed] [Google Scholar]
- 32.Porrata LF, Gertz MA, Inwards DJ, Litzow MR, Lacy MQ, Tefferi A, et al. Early lymphocyte recovery predicts superior survival after autologous hematopoietic stem cell transplantation in multiple myeloma or non-hodgkin lymphoma. Blood. 2001;98(3):579–585. doi: 10.1182/blood.v98.3.579. [DOI] [PubMed] [Google Scholar]
- 33.Gordan LN, Sugrue MW, Lynch JW, Williams KD, Khan SA, Moreb JS. Correlation of early lymphocyte recovery and progression-free survival after autologous stem-cell transplant in patients with hodgkin's and non-hodgkin's lymphoma. Bone Marrow Transplant. 2003;31(11):1009–1013. doi: 10.1038/sj.bmt.1704050. [DOI] [PubMed] [Google Scholar]
- 34.Porrata LF, Litzow MR, Tefferi A, Letendre L, Kumar S, Geyer SM, et al. Early lymphocyte recovery is a predictive factor for prolonged survival after autologous hematopoietic stem cell transplantation for acute myelogenous leukemia. Leukemia. 2002;16(7):1311–1318. doi: 10.1038/sj.leu.2402503. [DOI] [PubMed] [Google Scholar]
- 35.Joao C, Porrata LF, Inwards DJ, Ansell SM, Micallef IN, Johnston PB, et al. Early lymphocyte recovery after autologous stem cell transplantation predicts superior survival in mantle-cell lymphoma. Bone Marrow Transplant. 2006;37(9):865–871. doi: 10.1038/sj.bmt.1705342. [DOI] [PubMed] [Google Scholar]
- 36.Sampson JH, Aldape KD, Archer GE, Coan A, Desjardins A, Friedman AH, et al. Greater chemotherapy-induced lymphopenia enhances tumor-specific immune responses that eliminate EGFRvIII-expressing tumor cells in patients with glioblastoma. Neuro Oncol. 2011;13(3):324–333. doi: 10.1093/neuonc/noq157. [DOI] [PMC free article] [PubMed] [Google Scholar]