Abstract
Objective
Negative affect is a significant predictor of alcohol relapse, and the relation between negative affect and drinking has been shown to be strongly mediated by alcohol craving. Thus, targeting craving during treatment could potentially attenuate the relation between negative affect and drinking.
Method
The current study is a secondary analysis of data from the COMBINE study, a randomized clinical trial that combined pharmacotherapy with behavioral intervention in the treatment of alcohol dependence. The goal of the current study was to examine whether a treatment module that targeted craving would predict changes in negative mood during the 16-week Combined Behavioral Intervention (CBI; n=776) and the relation between changes in mood, craving, and changes in heavy drinking during treatment and one year posttreatment.
Results
Changes in negative mood were significantly associated with changes in heavy drinking during treatment (f2=0.78). Participants (n=432) who received the craving module had significantly fewer heavy drinking days during treatment (d = 0.31) and receiving the module moderated the relation between negative mood and heavy drinking during treatment (f2=0.92) and one year posttreatment (f2=0.03). Moderating effects of the craving module were mediated by changes in craving during treatment. Within subject analyses indicated significant pre- to post-module reductions in negative mood. Additionally, post-module craving significantly mediated the association between negative mood and heavy drinking during treatment and posttreatment.
Conclusions
The craving module of CBI may weaken the relation between negative affect and heavy drinking by fostering greater decreases in craving during treatment.
Keywords: craving, negative mood, heavy drinking, urge surfing, behavioral intervention
Emotions play a major role in the development, maintenance and cessation of substance use disorders (Kassel, 2009). The strong association between negative affect and alcohol use disorders is apparent in the high rates of co-occurrence of alcohol use disorders and affective disorders (Davis, Uezato, Newell, & Frazier, 2008; Kushner, Abrams & Borchardt, 2000), and negative affect has been identified as one of the most significant predictors of alcohol lapses following treatment (Lowman et al., 1996, Marlatt & Gordon, 1985; Witkiewitz & Villarroel, 2009; Zywiak et al., 2006).
Several models have been proposed to explain the associations between negative affect, craving and drinking outcomes (Baker et al., 2004; Le Moal & Koob, 2007; Weiss, 2005). Koob and Le Moal (2001) proposed an allostatic neuroadaptive model of drug addiction, which highlights the chronic dysregulation of reward circuits and self-regulatory failures over the course of chronic drug dependence. The allostatic view maintains that continued alcohol or other drug use results in decreases in the reward value of the substance, which disturbs an individual’s self-regulatory set-point and therefore their ability to modulate dysphoric feelings in the absence of the substance. The combination of the cognitive component of craving (desire for the previous effects of a drug), withdrawal-induced negative affect, and a dysregulated reward system during abstinence leads to a greatly increased vulnerability to relapse (Koob, 2000).
Baker and colleagues (2004) proposed an affective model of drug motivation, where avoidance of negative affect during withdrawal is the primary motive for relapse to drug use. Previous negative reinforcement of unpleasant affective states via drug use provides the learning experience that substances ameliorate the unpleasant affective states inherent to virtually all withdrawal syndromes (Baker et al., 2004). Recently, McCarthy, Curtin, Piper, and Baker (2010) expanded the Baker et al. (2004) affective model to consider the importance of contextual influences (e.g., drug cues), awareness, and cognitive control in the interplay between negative-reinforcement learning, craving, and drug motivation. They contend that responses to distress and negative affect are the primary basis for continued drug use and conclude that treatment approaches should attempt to change the learned associations between affect and drug responses, as well as improve effortful coping.
Generally, learning-based models of negative affect and substance use disorders consider a negative emotional state to be a conditioned stimulus (CS) that can elicit conditioned drug responses (CR). Stasiewicz and Maisto (1993), however, proposed that the simple CS-CR model was not sufficient to explain associations between affect and substance use. The authors extended the learning based model to a two-factor model that considered negative affect to be a conditioned emotional response, highlighting that many substance users have learned the negative emotional response because of repeated pairings of an aversive neutral stimulus (e.g., fight with a spouse) with negative emotional responses (e.g., anger). The individual then learns that substance use can temporarily alleviate the negative emotional state, and repeated substance use in response to negative emotional states results in a conditioned avoidance response via operant conditioning. If the individual is abstinent and cannot use substances in response to negative emotional states, then craving will occur in response to the negative emotional state. Stasiewicz and Maisto (1993) focus on the implications of the two-factor model as part of cue exposure treatments. However, it could be proposed that, in general, behavioral treatments for substance use disorders need to focus on extinction of the craving response to negative emotional states.
Recent empirical work (Witkiewitz & Villarroel, 2009), which found a dynamic association between negative affective states and alcohol lapses following treatment, provided empirical support for the theories of McCarthy and colleagues (2010) and Stasiewicz and Maisto (1993), concluding that substance use treatments need to focus on changing an individual’s response to negative emotional states. Consistent with this idea, a recently developed intervention, mindfulness-based relapse prevention (MBRP; Bowen, Chawla, Collins, et al., 2009), designed to target client responses to emotional states and craving, has shown promise in disrupting the relations between negative affect, craving and substance use (Witkiewitz & Bowen, 2010). Individuals randomized to receive the eight-week MBRP intervention did not evince the strong, positive association between depression symptoms, craving and subsequent substance use observed in a treatment-as-usual control condition. Results suggested that participants in the MBRP treatment learned alternative responses to depressive symptoms, whereby these symptoms did not significantly predict craving, thus weakening the relation between negative affect, craving and relapse. Despite these promising results, a number of limitations of the MBRP study have been noted (Bowen et al., 2009; Witkiewitz & Bowen, 2010), including the brevity of the follow-up assessments (four months following intervention), small sample size, and the lack of measurement of emotional states and craving during the course of the intervention.
The current study was designed to follow-up on the findings from the Witkiewitz and Bowen (2010) study by evaluating whether a specific treatment component that focuses on skills for coping with craving and urges could produce similar effects. The Coping with Craving and Urges module was incorporated as a procedure in one of several treatment modules in the Combined Behavioral Intervention (CBI) developed for the COMBINE study (COMBINE Study Research Group, 2003; Miller et al., 2004). The COMBINE study (i.e., “Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence” COMBINE Study Research Group, 2006), was a multi-site randomized clinical trial evaluating the effectiveness of two pharmacotherapies (naltrexone [ReVia] and acamprosate [Campral]) with or without the behavioral internvention (CBI). A total of 1,383 participants were provided treatment for 16 weeks, and were followed for one year following treatment. Results from the COMBINE study indicated that CBI was effective in reducing heavy drinking following treatment with or without the provision of pharmacotherapy (Anton et al., 2006). Publications from the COMBINE study have found no differences between treatment groups on a variety of drinking outcomes (Donovan et al, 2008) and a variety of non-drinking outcomes including stress, physical and mental health, quality of life, psychiatric symptoms, or craving (LoCastro et al., 2009). To date, no published studies have examined the effectiveness of the different skills training modules of the CBI intervention. Also, no published studies have evaluated whether hypothesized mechanisms of change mediated the effectiveness of CBI or other treatment conditions of the COMBINE study.
The first goal of the current study was to examine the association between negative mood and frequency of heavy drinking during the course of the 16-week active treatment phase of the combined behavioral intervention for alcohol dependence (Anton et al., 2006). Based on prior research (Baker et al., 2004; Koob, 2000; Stasiewicz & Maisto, 1993), it was hypothesized that negative mood and frequency of heavy drinking would be strongly correlated during the course of treatment. The second aim was to examine whether receiving the Coping with Craving and Urges module moderated the relation between negative mood and drinking behavior. We were specifically interested in replicating the results from the Witkiewitz & Bowen (2010) study, in which the authors found that a treatment that targeted reactions to craving significantly attenuated the association between depressive symptoms and substance use. For the current study, it was hypothesized that receiving the Coping with Craving and Urges module would attenuate the association between negative mood and heavy drinking during and following treatment. The third aim was to determine whether this moderation effect was mediated by changes in craving. It was hypothesized that the reductions in the association between negative mood and heavy drinking following the Coping with Craving and Urges module could be explained by decreases in self-reported craving during treatment. A final goal was to determine whether the effects of the Coping with Craving and Urges module persisted up to one year following treatment.
Methods
The data for this study are from the COMBINE study (COMBINE Study Research Group, 2003), a multi-site randomized trial. Participants (N = 1,381) were recruited from 11 research sites and were randomized into nine treatment groups, described below. Treatment was provided for 16 weeks and participants were followed for one year following treatment.
Participants
The sample was recruited from inpatient and outpatient referrals at the study sites and throughout the community. Prior to baseline, 4,965 volunteers were screened by telephone to determine whether they met eligibility criteria. Participants were excluded if they were dependent on another drug besides alcohol, nicotine, or cannabis, had recently used opioids, had a serious mental illness or any medical condition that could disrupt study participation, had taken one of the study medications 30 days prior to baseline, or had taken medication that could raise the potential risks of participation in the study. To be included in the COMBINE study, subjects needed to have a minimum of 14 drinks (females) or 21 drinks (males) average per week over successive 30-days in the 90-day period prior to beginning abstinence. Additionally, participants needed to have two or more days of heavy drinking in the 90-day period with the last drink being within 21 days of enrollment. Heavy drinking days was defined as four drinks per day for females and five drinks per day for males. Subjects meeting eligibility criteria were then required to produce a breath alcohol level of zero before completing baseline assessments.
The current study focused on data from the 776 individuals who were randomly assigned to the Combined Behavioral Intervention (CBI) condition and had the opportunity to receive the craving module. Thus, those in the COMBINE study who received medications without CBI were excluded. All participants in the subsample of 776 CBI participants included in the current analyses had alcohol-use disorders and had been drinking 90 days prior but had been abstinent for at least 4 days prior to randomization. The subsample was 31% female and 69% male. Approximately 23% of the subsample self-identified as ethnic minorities. Participants identified as follows: 76.7% non-Hispanic white, 10.7% Hispanic American, 7.7% African American, and 4.1% Other. The mean age of the subsample was 44 years, 70% had at least 12 years of education, and 43% were married. Within treatment, 94% completed all drinking data, while one year posttreatment 82.3% completed the drinking data. The retention rates did not differ significantly between groups.
Procedures
Upon meeting inclusion and exclusion criteria, participants completed a baseline assessment and were randomly assigned to one of nine treatment groups, each falling into one of three broader categories. The Medical Management groups (n=607) included: Naltrexone, Acamprosate, Naltrexone + Acamprosate, and Placebo. The Medical Management with CBI groups (n=619) consisted of: Naltrexone + CBI, Acamprosate + CBI, Naltrexone + Acamprosate + CBI, and Placebo + CBI. The final group, CBI only (n=157), was included to examine the effects of CBI without medication or placebo (COMBINE Study Research Group, 2003; Weiss, et al. 2008).
Subjects received treatment for a total of 16 weeks. Participants receiving study medication were offered nine Medical Management visits during weeks 0, 1, 2, 4, 6, 8, 10, 12, and 16. Those who received CBI had a maximum of 20 sessions available to them over the 16 weeks. Participants were subsequently followed for 52 weeks post-treatment and seen at the site following treatment on weeks 10, 26, and 52 for assessments. Both study participants and researchers were blind to medication/placebo group assignments during treatment and throughout the one-year posttreatment assessment period.
CBI was a multiple phase treatment. In the first phase therapists used motivational interviewing techniques to build clients’ motivation for change. The second phase consisted of conducting a functional analyses and developing a treatment plan. In the third phase, CBI was individualized to each client’s situation and needs. Treatment procedures were drawn from a menu of nine cognitive-behavioral skills training modules and the selection of particular modules was based on the therapist’s discretion, the treatment plan, and the therapist’s assessment of the client’s personal needs and preferences. The nine skills training modules included: Assertion Skills Training, Communication Skill Training, Coping with Craving and Urges, Drink Refusal and Social Pressure Skill Training, Job Finding Training, Mood Management Training, Mutual Help Group Involvement, Social and Recreational Counseling, and Social Support for Sobriety.
The current study focused specifically on the Coping with Craving and Urges module, which was received by over half of CBI participants (n = 432). The Coping with Craving and Urges module incorporated several components, including a description of the rationale that experiences of urges and craving are predictable and can be controlled, an assessment of the particular cues or situations that elicit craving or urges, an urge-monitoring homework assignment, psychoeducation on strategies for coping with external triggers, and an urge surfing exercise to cope with internal triggers (such as negative mood). Urge surfing is a mindfulness-based technique used in mindfulness-based relapse prevention to teach clients how to “ride” urges through fluctuations in intensity without fighting or giving in to the urge. Specifically, clients are instructed to, “picture the urge as an ocean wave, and imagine yourself surfing, using your breath as the surfboard…Ride this wave through its peak and its decline, without being submerged or wiped out by its enormity” (Bowen, Chawla, & Marlatt, 2010). Of those who received the Coping with Craving and Urges module, 33% received the module once, 37% received the module two times, 18% received the module three times, 8% received the module four times, and 4% received the module six to eight times.
Measures
The primary outcome measures in the COMBINE study assessed drinking behavior by percent days abstinent and number of days to first heavy drinking period (Anton & Randall, 2005). Secondary outcome measures or covariates monitored included level of craving, presence of DSM-IV diagnosis of alcohol dependence, biological markers of heavy alcohol consumption, number of heavy drinking days, use of other drugs, self-efficacy, motivation or baseline readiness to change, social support/supportive significant other, family history of alcohol use, clinical composite outcome, emotional status, mood, stress, psychosocial functioning, and quality of life. Treatment process measures evaluated therapeutic alliance, process of change, and client satisfaction. A complete list of all assessments and schedule of assessments can be found in the previous COMBINE publication (COMBINE study Research Group, 2003).
Drinking Outcomes
The primary outcome measure in the current study was percent heavy drinking days with heavy drinking defined as four or more drinks per day for women, or five or more drinks per day for men. Using a calendar method, drinking was assessed for the prior 30 days at baseline and during the 16-week active treatment phase using the Timeline Follow-Back (Sobell & Sobell, 1996). The Form-90 interview (Miller & Del Boca, 1994) was used to assess drinking across the 12-months following treatment. In the current study, the primary drinking outcome measure was the percent heavy drinking days during the 16 weeks of treatment and at one year following treatment completion.
Negative Mood
The Profile of Mood States–Brief (POMS; McNair, Loor, & Droppleman, 1992) was administered at baseline, after the first two weeks of treatment, and every four weeks during the 16 weeks of treatment. Participants were queried as to how they were feeling during the past week using 30 adjectives describing feelings and moods (e.g., Tense, Angry, Annoyed, etc.), with ratings for each adjective ranging from 0 (not at all) to 4 (extremely). Ratings on the 30 items were combined into six mood subscales: Tension, Depression, Anger, Vigor, Fatigue, and Confusion. For the current study, the Tension, Depression, Anger and Fatigue subscales were included as indicators of a negative mood latent variable at each time point, described in detail below. The internal consistency reliability of the 30 items averaged α = 0.89 across all time points. Reliabilities for each of the subscales exceeded α = 0.70 at all time points.
Craving
The Obsessive Compulsive Drinking Scale (OCDS; Anton, Moak & Latham, 1995) is a 14-item self-report instrument assessing drinking-related thoughts, urges to drink, and the ability to resist thoughts and urges to drink. Items were rated on a five-point Likert-type scale, with lower ratings indicating less craving. A total score was calculated by summing 12 of the 14 items (the two items that assessed drinking quantity and frequency were not included). Reliability of the scale was greater than α = 0.90 at all time points.
Statistical Analyses
All models, described below, were estimated using Mplus version 5.21 (Muthen & Muthen, 2007). Considering the complex sampling design in the COMBINE study (participants recruited from 11 sites), all parameters were estimated using a weighted maximum likelihood function and all standard errors were computed using a sandwich estimator1 (the MLR estimator in Mplus). MLR provides the estimated variance-covariance matrix for the available data and therefore all available data were included in the models. Maximum likelihood is a preferred method for estimation when some data are missing, assuming the data are missing at random (Schafer & Graham, 2002). Attrition analyses revealed no significant differences on any study variables between those with missing data and those with complete data. Model fit of all models were evaluated by χ2 values, the Root Mean Square Error of Approximation (RMSEA; Browne & Cudeck, 1993), and the Comparative Fit Index (CFI; Bentler, 1990). Models with non-significant χ2, RMSEA less than 0.06 and CFI greater than 0.95 were considered a good fit to the observed data (Hu & Bentler, 1999).
Results
Descriptive statistics for all study variables are reported in Table 1. Statistics are provided both for all CBI participants, and separately for those CBI participants who did and did not receive the craving module. Independent samples t-tests were conducted to assess the significance of mean differences between craving module groups (received vs. not received). As seen in Table 1, individuals who received the craving module were drinking significantly less during treatment and had significantly lower negative mood scores (i.e., less negative mood) after week 4. Surprisingly, there were no differences between those receiving the craving module versus not receiving the craving module on self-reported craving.
Table 1.
Descriptive Statistics, Mean (Standard Deviation), for all Study Variables
| Variable | Total M (SD) | Craving module not received M (SD) | Craving module received M (SD) |
|---|---|---|---|
| PHD baseline | 65.48 (29.16) | 63.12 (29.96) | 67.37 (28.40) |
| PHD week 4 | 14.06 (23.70) | 16.50 (26.61) | 12.16 (20.98)* |
| PHD week 8 | 16.41 (26.88) | 21.52 (31.45) | 12.72 (22.35)* |
| PHD week 12 | 15.91 (26.91) | 21.14 (31.04) | 12.21 (22.88)* |
| PHD week 16 | 15.78 (28.01) | 21.16 (32.61) | 11.97 (23.53)* |
| PHD 1 year | 25.29 (34.09) | 25.39 (31.20) | 25.22 (33.34) |
| Craving baseline | 20.14 (7.42) | 20.04 (7.94) | 20.21 (6.89) |
| Craving week 1 | 11.78 (7.02) | 12.03 (7.28) | 12.45 (6.74) |
| Craving week 2 | 11.27 (7.15) | 11.09 (7.30) | 11.96 (6.97) |
| Craving week 4 | 10.75 (7.41) | 10.40 (7.92) | 11.24 (7.05) |
| Craving week 8 | 10.49 (7.36) | 9.93 (7.69) | 11.09 (6.94) |
| Craving week 12 | 9.43 (7.32) | 8.90 (7.99) | 9.94 (7.09) |
| Craving week 16 | 9.46 (7.55) | 9.06 (8.51) | 9.89 (7.20) |
| POMS week 0 | 0.28 (3.13) | 0.40 (3.20) | 0.18 (3.08) |
| POMS week 1 | −0.35 (2.92) | −0.13 (3.06) | −0.52 (2.79) |
| POMS week 2 | −0.58 (2.93) | −0.44 (2.98) | −0.69 (2.89) |
| POMS week 4 | −0.69 (3.11) | −0.36 (3.30) | −0.95 (2.93)* |
| POMS week 8 | −1.038 (3.12) | −0.77 (3.20) | −1.25 (3.04)* |
| POMS week 12 | −0.85 (3.30 | −0.56 (3.46) | −1.08 (3.15)* |
| POMS week 16 | −1.10 (3.29) | −0.68 (3.56) | −1.43 (3.03)* |
Note. n = 776; PHD = Percent heavy drinking days; POMS = Factor scores for Profile of Mood States latent variable at each assessment point;
Differences between craving module groups based on independent samples t-test p < 0.05
Preliminary analyses were conducted to determine baseline differences between those who did and did not receive the craving module on demographic measures (gender, race, income, age, years of education), family history of alcohol dependence, number of comorbid conditions, severity of alcohol dependence, baseline drinking, baseline readiness to change, baseline drinking related problems, working alliance, treatment history, percent of drinkers in the social network, baseline mood and baseline craving. Differences between module groups (those who did or did not receive the module) were identified for race (χ2 (1) = 15.13, p < 0.001), age (t (774) = −4.57, p < 0.001), years of education (t (760) = −3.60, p < 0.001), alcohol dependence severity (t (771) = 3.05, p = 0.002), baseline percent drinking days (t (774) = −2.72, p = 0.007), baseline drinks per drinking day (t (774) = 3.02, p = 0.003), and baseline drinking related problems (t (772) = 4.07, p < 0.001). Individuals who received the module were more likely to be White and non-Hispanic, older, and have more years of education. The individuals who received the module also reported lower baseline alcohol dependence severity, fewer drinks per drinking day and fewer drinking-related problems, yet they drank on a greater percentage of days. Measures that were significantly different between module groups were included as covariates in all analyses that included between-module group comparisons.
Preliminary Model Testing
Longitudinal confirmatory factor analysis (LCFA) was used to create a latent measure of negative mood at each time point and to evaluate the equivalence of the negative mood measure across time. At each time point the four POMS subscales, Depression, Tension, Anger and Fatigue, were used as indicators of a single negative mood latent factor. At all time-points the POMS negative mood factor provided an excellent fit to the data (e.g., Week 1: χ2 (2) = 0.28, p = 0.87; CFI = 1.00; RMSEA = 0.00; Week 16: χ2 (2) = 0.25, p = 088; CFI = 1.00; RMSEA = 0.00). We then examined whether the factor structure was metric invariant over time (Byrne, Shavelson, & Muthén, 1989) by comparing a model with all item loadings constrained to be equal at each time point to an unconstrained model with item loadings freely estimated at each time point. Both models provided an excellent fit to the data based on CFI = 0.995 and RMSEA = 0.01. The model with loadings constrained to equality did not fit significantly worse than the unconstrained model based on a χ2 difference test (Δχ2 (Δdf = 18) = 21.51, p = 0.25).
Latent growth curve modeling was used to examine the changes in negative mood, percent heavy drinking days, and craving scores across time. The negative mood model, including the POMS negative mood factor models at each time point, with a linear and quadratic slope, provided an excellent fit to the observed data based on the CFI = 0.98 and RMSEA = 0.03 (90% CI of RMSEA: 0.026-0.035). The slope of negative mood was significantly negative (linear slope B (SE) = −0.54 (0.13), p < 0.005) with a significantly positive quadratic effect (quadratic slope B (SE) = 0.06 (0.02), p = 0.01), suggesting a significant decrease in negative mood over the first several weeks of treatment with a slight increase in negative mood toward the end of treatment.
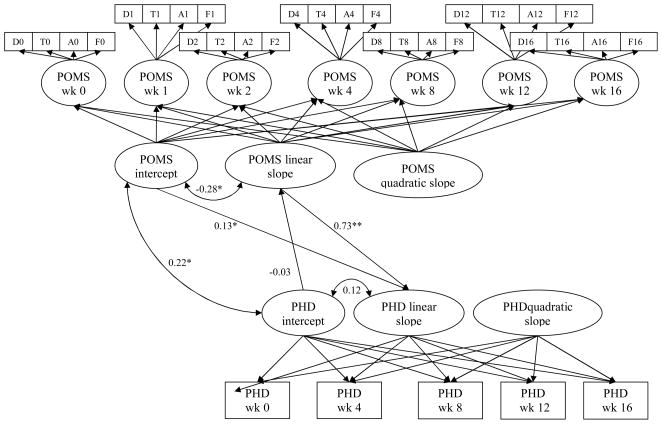
Parallel Process Latent Growth Curve Models
The parallel process latent growth curve model shown in Figure 1 was used to examine the associations between negative mood and heavy drinking across time during treatment, following the recommendations for testing parallel process models described by Cheong and colleagues (2003). Variances of the quadratic growth factors were constrained to zero for model convergence. The model provided a reasonable fit to the data based on CFI = 0.94 and RMSEA = 0.05 (90% CI 0.046–0.052). As seen in Figure 1, the linear change in percent heavy drinking days over time was significantly predicted by the intercept and linear slope growth factor of the negative mood latent factor (intercept: B (SE) = 0.20 (0.09), p = 0.04; slope: B (SE) = 5.78 (0.80), p < 0.001). The linear slope of negative mood was regressed on the percent heavy drinking days initial status; however, this association was not significant (p = 0.69). The covariance between the intercepts of negative mood and percent heavy drinking days, which represents the pre-treatment assessment, was significant (p = 0.004). Likewise, there was a strong negative covariance between the negative mood linear slope with the negative mood intercept (p < 0.005), indicating individuals with higher negative mood at baseline experienced greater decreases in negative mood over time.
Figure 1.
Unconditional multiple process latent growth curve model with standardized path coefficients (*p<0.05; **p<0.001). D = depressed, T = tense, A = anxious, F = frustrated; POMS = Profile of Mood States; PHD = percent heavy drinking days.
Together, these findings suggest that negative mood and the frequency of heavy drinking are significantly associated prior to the start of treatment and that changes in negative mood during the course of treatment significantly predict changes in the frequency of heavy drinking during treatment. Specifically, individuals with greater decreases in negative mood also engage in less frequent heavy drinking over time during treatment.
Between-Group Moderation Analyses
After establishing a strong relation between negative mood and heavy drinking, the second goal of the current study was to examine whether receiving the Coping with Craving and Urges module during the course of treatment moderated this relation. First, a binary variable was created to distinguish individuals who received the module at any point during treatment (n = 432), from those who never received the module (n = 344). This binary variable was then incorporated into the parallel process growth model, described above, as a moderator of the relation between the negative mood linear slope and the percent heavy drinking days linear slope. Specifically, an interaction term was created by multiplying each of the negative mood linear growth factors by the binary craving module variable (Aiken & West, 1991). Each interaction term was then entered into the parallel process growth model as a predictor of the percent heavy drinking days linear slope. An estimate of the moderation effect size, f2, was calculated as the proportion of variance explained by the interaction relative to the unexplained variance in the criterion (see Aiken & West, 1991).
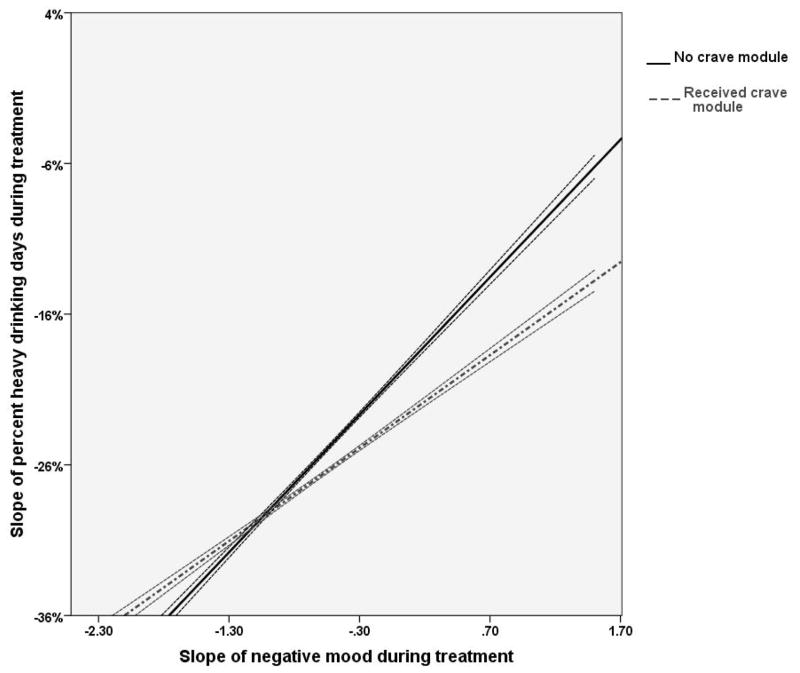
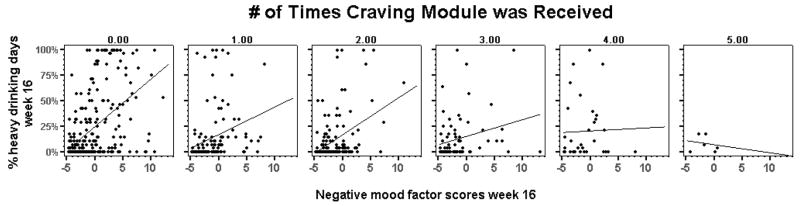
Results from the moderation analyses confirmed a significant interaction between the linear slope of negative mood and receiving the craving module in prediction of the percent heavy drinking days linear slope (B (SE) = −5.93 (1.61), p < 0.001), which indicated a large moderation effect (f2 = 0.92). As seen in Figure 2, the relation between changes in negative mood and changes in percent heavy drinking days was stronger for those who did not receive the craving module, as compared to those who did receive the module. Furthermore, an examination of the bivariate association between percent heavy drinking days and negative mood factor scores during the last week of treatment among those individuals who received the craving module more than once (n = 288) indicated a clear dose-response association (see Figure 3). The more times the craving module was received, the weaker the association between percent heavy drinking days and negative mood. Receiving the craving module did not moderate the relations between intercept of negative mood or the quadratic slope of negative mood and percent heavy drinking days slope.
Figure 2.
Moderating effect of craving module on relation between negative mood slope and percent heavy drinking slope, with 95% confidence bands.
Figure 3.
Dose-response effect of craving module on relation between negative mood (x-axis) and percent heavy drinking days (y-axis) during the last week of treatment (week 16).
Between-Group Mediation Analyses
Mediation modeling was then used to examine whether changes in self-reported craving during treatment mediated the moderating relation between negative mood slope and receiving the craving module in the prediction of percent heavy drinking days. This mediation of a moderator effect (see Fairchild & MacKinnon, 2009; Preacher, Rucker & Hayes, 2007) examined the negative mood-by-craving module interaction predicting percent heavy drinking days via changes in craving during the course of treatment. Although many variants of moderated-mediation or mediated-moderation can be tested, in this instance of mediated moderation the relation between changes in negative mood and percent heavy drinking days depend on the level of a moderating variable (receiving the craving module), and this relation is mediated by changes in craving (Morgan-Lopez & MacKinnon, 2006; Preacher et al. 2007). Models were estimated using maximum likelihood with 1000 bootstrap draws to obtain the 95% confidence interval for the indirect effect (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002).
Results from the mediated moderation model indicated the effect of changes in negative mood in the prediction of changes in percent heavy drinking days was conditional on the receipt of the craving module, and the moderating effects of receipt of the craving module was mediated by changes in self-reported craving over time (95% CI: −2.76 - −0.04). When change in craving was included in the model, the relation between negative mood linear slope and the linear slope of percent heavy drinking days was no longer significant (B (SE) = 2.10 (2.31), p = 0.36). As reported in Table 2, linear change in craving over time was also significantly predicted by receiving the craving module (individuals who received the module had less craving over time), linear slope of negative mood (greater change in negative mood positively associated with greater change in craving over time) and the interaction between receipt of the craving module and the negative mood slope (all ps < 0.01).
Table 2.
Regression Coefficients for Multiple Process Latent Growth Curve Model with Craving Intervention as a Mediator
| Criterion | Predictor | Unstandardized B (SD) |
|---|---|---|
| Linear slope PHD | Intercept negative mood | −0.005 (0.12) |
| Linear slope negative mood | 2.10 (2.31) | |
| Craving module received | −2.45 (0.59)* | |
| Negative mood by craving module interaction | −1.90 (0.83) | |
| Intercept craving | 0.31 (0.16) | |
| Linear slope craving | 5.92 (1.86)* | |
| Linear slope craving | Intercept negative mood | −0.01 (0.01) |
| Linear slope negative mood | 1.08 (0.15)* | |
| Craving module received | −0.16 (0.08)* | |
| Negative mood by craving module interaction | −0.24 (0.10)* | |
Note. PHD = percent heavy drinking days;
p < 0.01
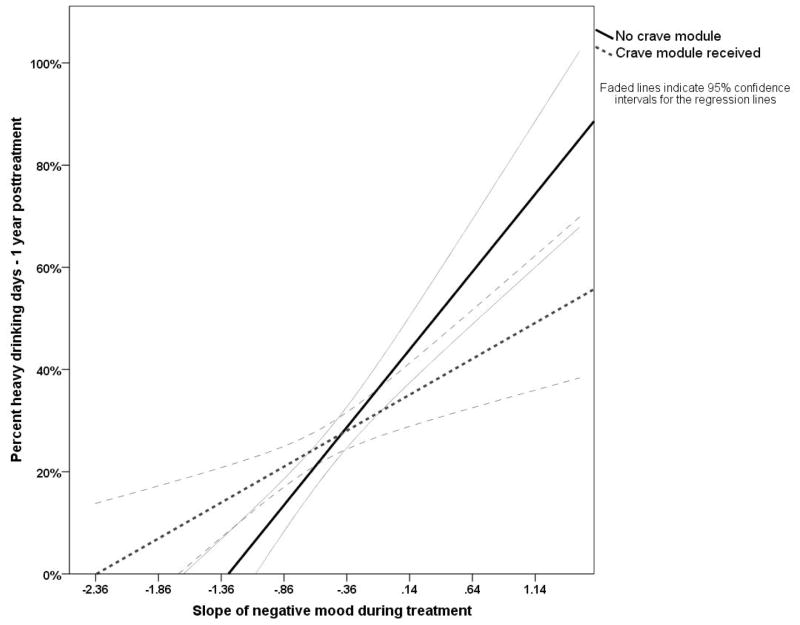
Between-Group Post-Treatment Outcomes
To examine whether the moderation and/or mediated moderation effects were still significant following treatment, percent heavy drinking days at one year following treatment was incorporated as the primary outcome measure in each of the models. Thus, one year posttreatment percent heavy drinking days was regressed on receiving the craving module, the craving-module-by-mood-slope interaction, and the during-treatment mood and craving scores. For the moderation analyses, results indicated that only age, the growth factors of negative mood the craving-module-by-mood-slope interaction effect remained significant predictors of one-year posttreatment percent heavy drinking days (Age: B (SE) = −0.01 (0.004), p = 0.004; Mood intercept: B (SE) = 0.10 (0.03), p = 0.002; Mood slope: B (SE) = 1.17 (0.19), p < 0.001; Interaction: B (SE) = −0.65 (0.27), p = 0.02), explaining 13% of the variance in percent heavy drinking days at the one-year follow-up, which constitutes a small effect (f2 = 0.03). Figure 4 provides the regression lines (and 95% confidence intervals) for the relation between negative mood and percent heavy drinking days by groups. As indicated by the dashed line, the association between negative mood and percent heavy drinking days was less strong among those who received the craving module, in comparison to those who did not receive the module (solid line). Likewise, the changes in self-reported craving during treatment significantly mediated the association between negative mood, receiving the craving module, and posttreatment percent heavy drinking days (B (SE) = −0.51 (0.13), p < 0.001; 95% CI of the indirect effect: −0.77, −0.25).
Figure 4.
Moderating effect of craving module on relation between negative mood and percent heavy drinking days one year following treatment, with 95% confidence bands for regression lines.
Within-Group Analyses
To examine the effect of the craving module on negative mood during the course of treatment among those who received the module, we calibrated the negative mood assessment points to the timing of the craving module. Most individuals (n = 361, 85% of those who received the module) had at least four assessments of mood prior to receiving the craving module for the first time. After the craving module was administered for the first time, most individuals (n = 339, 78%) had at least two assessments of mood and 57% of individuals (n = 245) had at least three assessments of mood. Table 3 provides a summary of the observed means averaged across assessments. There is a reduction in average mood scores for each of the POMS subscales from pre- to post-craving module. Pre- to post-differences in means were significant (p < 0.001) for anger, tension, and fatigue subscales based on paired samples t-tests.
Table 3.
Means (Standard Deviations) for all POMS scales pre- and post-craving module
| POMS Scale | Pre-module Mean (SD) | Post-module Mean (SD) |
|---|---|---|
| Depression | 3.52 (3.42) | 3.33 (3.52) |
| Anger | 3.31 (3.09) | 2.91 (3.13)** |
| Tension | 3.78 (2.90) | 3.28 (3.09)** |
| Fatigue | 4.33 (3.57) | 3.79 (3.63)** |
Note. n = 404.
Differences from pre- to post-module based on paired samples t-test p < 0.01.
Using the pre- and post-module mood assessments, we then estimated piecewise growth models to evaluate whether changes in negative mood factor scores from pre to post-craving module were related to percent heavy drinking days during treatment and posttreatment. Piecewise models were estimated with a single intercept and two linear slopes. The intercept was centered at the first assessment point following the craving module, which provided the opportunity to evaluate changes in negative mood from baseline to the first assessment after the module (slope 1), as well as changes in negative mood following the craving module (slope 2). The unconditional piecewise model (without covariates) provided an excellent fit to the observed data (CFI = 0.98; RMSEA = 0.03). The mean of slope 1 (Mean (SE) = −0.37 (0.05), p < 0.001) indicated significant reductions in negative mood from baseline to the assessment following the craving module. The mean of slope 2 (Mean (SE) = −0.12 (0.09), p = 0.19) was not significant.
Results from a model that incorporated percent heavy drinking days during treatment as a parallel process indicated that changes in percent heavy drinking days during treatment were significantly related to the level of negative mood at the first assessment following the module (B (SE) = 0.37 (0.11), p < 0.001), and changes in negative mood from baseline to following the craving module (B (SE) 5.07 (2.00), p = 0.01). Likewise, percent heavy drinking days at one year following treatment was significantly related to the level of negative mood at the first assessment following the module (B (SE) = 2.10 (0.95), p = 0.03). Thus, lower levels of negative mood following the craving module were associated with significantly fewer heavy drinking days during treatment and one year following treatment.
Finally, changes in craving following the craving module were incorporated as a mediator of these effects. The craving growth model was estimated in the same way as the negative mood growth model with craving assessment points calibrated to the timing of the craving module. The level of craving following the craving module significantly mediated the association between levels of negative mood and drinking outcomes during treatment (95% CI: 0.28, 0.98) and one year following treatment (95% CI: 1.05, 3.80).
Discussion
Negative mood has been identified as one of the key predictors of alcohol use disorders and alcohol relapse following treatment. The current study examined the association between negative mood and heavy drinking frequency during the course of treatment and provided additional support for a significant correlation of the two processes: decreases in negative mood are significantly associated with decreases in heavy drinking frequency. The current study also found that receiving the Coping with Craving and Urges module of the Combined Behavioral Intervention (CBI) moderated the relation between negative mood and heavy frequent drinking during treatment and one year following treatment, such that individuals who received the module evinced a weaker relation. Mediated moderation analyses further demonstrated that the interaction between the craving module and the relation between negative mood and frequent heavy drinking during treatment and one year following treatment could be explained by changes in self-reported craving during the course of treatment. Within subject analyses among individuals who received the craving module indicated significant reductions in negative mood from pre-module to the assessment point following the craving module. Negative mood following the craving module predicted changes in heavy drinking during treatment and percent heavy drinking days one year following treatment. Consistent with the results from the mediated moderation analyses, the effects of negative mood on drinking following the craving module were mediated by changes in craving following the craving module.
The results from the current study are consistent with neurobiological (Koob & Le Moal, 2001) and learning based (McCarthy et al., 2010; Stasiewicz & Maisto, 1993) models of substance abuse relapse, which contend that negative emotional responses to environmental stimuli during abstinence are associated with craving responses, which predict an increased probability of relapse. Several empirical studies have found strong associations between negative mood and alcohol lapses (e.g., Lowman et al., 1996, Zywiak et al., 2006) and negative mood inductions have been shown to trigger craving responses (e.g., Maude-Criffin & Tiffany, 1996; see Tiffany, 2010 for a review). Based on the theoretical models, previous empirical research, and the results from the current study, it appears that targeting craving in response to negative emotional states can help reduce the risk of heavy drinking episodes following treatment for alcohol dependence.
The current findings also replicated and the extended the findings from a previous study (Witkiewitz & Bowen, 2010), which found that mindfulness-based relapse prevention, an intervention that also targets craving responses to negative affect, moderated the relations between end-of-treatment depression symptoms and both craving two months posttreatment and substance use at a four-month follow-up. The current study differs from Witkiewitz and Bowen (2010) in several respects. The current sample size was much larger (n=776 vs. n=168 in the Witkiewitz & Bowen study); the follow-up was longer (12-months vs. 4 months); the measures were different (Witkiewitz & Bowen only had one measure of depressive symptoms); and the participants in the current study were more geographically diverse and represented a different population than those in the Witkiewitz and Bowen study (e.g., all participants were recruited from a single treatment agency, 19% were polysubstance dependent, many were court-mandated and/or homeless, majority were below poverty line). Despite these differences, the results from the two studies were very similar, suggesting a robust common mechanism.
Limitations
The current study had several limitations. Most importantly, lack of random assignment to the craving module greatly limits our interpretation of the findings. To address this limitation, we co-varied all predictors that differentiated those who did and did not receive the module in all between group analyses, thus statistically controlling for differences between groups on all available measures. However, other client characteristics (as well as therapist characteristics) not measured in the COMBINE study could have influenced the therapists’ choice of who did and did not receive the module, and these unmeasured characteristics could also explain the differences observed in the current study. In addition, the current study focused exclusively on the total OCDS score, whereas future research could examine whether there are differential effects of the craving module on specific dimensions of craving. A further limitation is presented by the multi-component structure of the craving module which, in addition to urge surfing, included a rationale of urges and cravings, assessment of eliciting cues or situations, urge-monitoring assignments, and psychoeducation. It is therefore not possible to isolate which components of the craving module were most effective in moderating the relation between negative affect and drinking. Finally, all of the measures of mood, craving and drinking frequency were self-report. Physiological or behavioral indicators of mood, craving and drinking would greatly enhance our confidence in these findings.
Conclusions
Negative mood has often been considered a strong predictor of alcohol relapse. The current study provides empirical support for the Coping with Craving and Urges module (received as part of a combined behavioral intervention) as an intervention that targets responses to negative mood. Specifically, this module reduced the impact of negative mood on heavy drinking days. Furthermore, the current results indicate that change in craving, the primary target in the craving module, was a potential mechanism by which the relation between negative mood and heavy drinking frequency was altered. The treatment of comorbid mood and alcohol use disorders using behavioral approaches has received some support (see Carroll, 2004 for a review); however large scale studies and dismantling studies have not been conducted. The current study offers preliminary support for the inclusion of the Coping with Craving and Urges module into behavioral interventions for alcohol dependence and comorbid mood disorders.
Acknowledgments
This research was supported by National Institute on Alcohol Abuse and Alcoholism grant R21AA017137 (Witkiewitz, PI). The authors thank members of the COMBINE Study Research Group for their assistance in facilitating access to COMBINE study data.
Footnotes
Given the lack of substantive reasons for differences across sites as well as low intraclass correlations (ICCs) that indicated minimal effects of site (all ICCs below 0.015), we did not use a multilevel modeling framework and instead used a sandwich estimator to adjust the standard errors of model estimates for the minimal influence of treatment site.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp
Contributor Information
Katie Witkiewitz, Department of Psychology, Washington State University.
Sarah Bowen, Department of Psychology, University of Washington.
Dennis M. Donovan, Alcohol and Drug Abuse Institute and Department of Psychiatry and Behavioral Sciences, University of Washington
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA US: Sage Publications, Inc; 1991. [Google Scholar]
- Anton RF, Moak DH, Latham PK. The Obsessive Compulsive Drinking Scale: A new method of assessing outcome in alcoholism treatment studies. Archives of General Psychiatry. 1996;53:225–231. doi: 10.1001/archpsyc.1996.01830030047008. [DOI] [PubMed] [Google Scholar]
- Anton RF, O'Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, et al. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA. 2006;295:2003–2017. doi: 10.1001/jama.295.17.2003. [DOI] [PubMed] [Google Scholar]
- Anton RE, Randall CL. Measurement and choice of drinking outcome variables in the COMBINE Study. Journal of Studies on Alcohol Suppl. 2005;(15):104–109. 192–103. doi: 10.15288/jsas.2005.s15.104. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bowen S, Chawla N, Collins S, Witkiewitz K, Hsu S, Grow J, et al. Mindfulness-based relapse prevention for substance use disorders: A pilot efficacy trial. Substance Abuse. 2009;30:295–305. doi: 10.1080/08897070903250084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Chawla N, Marlatt GA. Mindfulness-Based Relapse Prevention. New York, NY: Guilford; 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing Structural Equation Models. Beverly Hills, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Byrne BM, Shavelson RJ, Muthén B. Testing for the equivalence of factor covariance and mean structures: The issue of partial measurement invariance. Psychological Bulletin. 1989;105:456–466. [Google Scholar]
- Carroll KM. Behavioral therapies for co-occurring substance use and mood disorders. Biological Psychiatry. 2004;56:778–784. doi: 10.1016/j.biopsych.2004.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COMBINE Study Research Group. Testing combined pharmacotherapies and behavioral interventions in alcohol dependence: rationale and methods. Alcoholism Clinical and Experimental Research. 2003;27:1107–1122. doi: 10.1097/00000374-200307000-00011. [DOI] [PubMed] [Google Scholar]
- Davis L, Uezato A, Newell JM, Frazier E. Major depression and comorbid substance use disorders. Current Opinion in Psychiatry. 2008;21:14–18. doi: 10.1097/YCO.0b013e3282f32408. [DOI] [PubMed] [Google Scholar]
- Fairchild AJ, MacKinnon DP. A general model for testing mediation and moderation effects. Prevention Science. 2009;10:87–99. doi: 10.1007/s11121-008-0109-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- Kassel JD. Substance Abuse and Emotion. American Psychological Association; 2009. [Google Scholar]
- Koob GF. Neurobiology of addiction. Toward the development of new therapies. Annals of the New York Academy of Sciences. 2000;909:170–185. doi: 10.1111/j.1749-6632.2000.tb06682.x. [DOI] [PubMed] [Google Scholar]
- Koob GF, Le Moal M. Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacology. 2001;24(2):97–129. doi: 10.1016/S0893-133X(00)00195-0. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Abrams K, Borchardt C. The relationship between anxiety disorders and alcohol use disorders: a review of major perspectives and findings. Clinical Psychology Review. 2000;20:149–171. doi: 10.1016/s0272-7358(99)00027-6. [DOI] [PubMed] [Google Scholar]
- Le Moal M, Koob GF. Drug addiction: pathways to the disease and pathophysiological perspectives. European Neuropsychopharmacology. 2007;17:377–393. doi: 10.1016/j.euroneuro.2006.10.006. [DOI] [PubMed] [Google Scholar]
- LoCastro J, Youngblood MA, Cisler R, Mattson MM, Zweben A, Anton R. Alcohol treatment effects on secondary non-drinking outcomes and quality of life: The COMBINE Study. Journal of Studies on Drugs and Alcohol. 2009;70:186–196. doi: 10.15288/jsad.2009.70.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowman C, Allen J, Stout RL. Replication and extension of Marlatt's taxonomy of relapse precipitants: overview of procedures and results. The Relapse Research Group. Addiction. 1996;91(Suppl):S51–71. [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA, Gordon JR. Relapse Prevention. New York, NY: Guilford; 1985. [Google Scholar]
- Maude-Griffin PM, Tiffany ST. Production of smoking urges through imagery: The impact of affect and smoking abstinence. Experimental and Clinical Psychopharmacology. 1996;4:198–208. [Google Scholar]
- McCarthy DE, Curtin JJ, Piper ME, Baker TB. Negative reinforcement: Possible clinical implications of an integrated model. In: Kassel JD, editor. Substance Abuse and Emotion. Washington DC: American Psychological Association; 2010. pp. 15–42. [Google Scholar]
- McNair DM, Lorr M, Droppleman LF. POMS: Profile of Mood States. North Tonawanda, NY: Multi-Health Systems Inc; 1992. [Google Scholar]
- Miller WR, Del Boca FK. Measurement of drinking behavior using the Form 90 family of instruments. Journal of Studies on Alcohol Suppl. 1994;12:112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Morgan-Lopez AA, MacKinnon DP. Demonstration and evaluation of a method for assessing mediated moderation. Behavioral Research Methods. 2006;38:77–87. doi: 10.3758/bf03192752. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus (Version 5) Los Angeles: Muthén & Muthén; 2007. [Google Scholar]
- Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research. 2007;42:185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Alcohol Timeline Followback Users’ Manual. Toronto, Canada: Addiction Research Foundation; 1995. [Google Scholar]
- Stasiewicz PR, Maisto SA. Two-factor avoidance theory: The role of negative effect in the maintenance of substance use in substance use disorder. Behavior Therapy. 1993;24:337–356. [Google Scholar]
- Tiffany ST. Drug craving and affect. In: Kassel JD, editor. Substance Abuse and Emotion. Washington DC: American Psychological Association; 2010. pp. 83–108. [Google Scholar]
- Weiss F. Neurobiology of craving, conditioned reward and relapse. Current Opinions Pharmacology. 2005;5:9–19. doi: 10.1016/j.coph.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Weiss RD, O'Malley SS, Hosking JD, Locastro JS, Swift R COMBINE Study Research Group. Do patients with alcohol dependence respond to placebo? Results from the COMBINE Study. Journal of Studies on Alcohol and Drugs. 2008;69:878–84. doi: 10.15288/jsad.2008.69.878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S. Substance use following mindfulness-based relapse prevention: A moderated-mediation model of depression, craving and post-treatment substance use. Journal of Consulting and Clinical Psychology. 2010;78:362–374. doi: 10.1037/a0019172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Villarroel NA. Dynamic association between negative affect and alcohol lapses following alcohol treatment. Journal of Consulting and Clinical Psychology. 2009;77:633–644. doi: 10.1037/a0015647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zywiak WH, Stout RL, Trefry WB, Glasser I, Connors GJ, Maisto SA, et al. Alcohol relapse repetition, gender, and predictive validity. Journal of Substance Abuse Treatment. 2006;30:349–353. doi: 10.1016/j.jsat.2006.03.004. [DOI] [PubMed] [Google Scholar]