Abstract
Aims
The current study was designed to re-examine the motivation matching hypothesis from Project MATCH using growth mixture modeling, an analytical technique that models variation in individual drinking patterns.
Design, setting and participants
Secondary data analyses of data from Project MATCH (n = 1726), a large multi-site alcoholism treatment-matching study.
Measurements
Percentage of drinking days was the primary outcome measure, assessed from 1 month to 12 months following treatment. Treatment assignment, alcohol dependence symptoms and baseline percentage of drinking days were included as covariates.
Findings
The results provided support for the motivation matching hypothesis in the out-patient sample and among females in the aftercare sample: the majority of individuals with lower baseline motivation had better outcomes if assigned to motivation enhancement treatment (MET) compared to those assigned to cognitive behavioral treatment (CBT). In the aftercare sample there was a moderating effect of gender and alcohol dependence severity, whereby males with lower baseline motivation and greater alcohol dependence drank more frequently if assigned to MET compared to those assigned to CBT.
Conclusions
Results from the current study lend partial support to the motivation-matching hypothesis and also demonstrated the importance of moderating influences on treatment matching effectiveness. Based upon these findings, individuals with low baseline motivation in out-patient settings and males with low levels of alcohol dependence or females in aftercare settings may benefit more from motivational enhancement techniques than from cognitive–behavioral techniques.
Keywords: Client–treatment-matching, cognitive–behavioral therapy, growth mixture modeling, motivation to change, motivational enhancement therapy, Project MATCH
INTRODUCTION
Motivation to change is often considered a central construct in the treatment of alcohol use disorders [1]. Motivational interviewing (MI) [2] and motivation enhancement therapy (MET) [3], which were designed specifically to increase motivation to change behavior, have been shown to be effective and efficacious in the treatment of both alcohol and drug use disorders (see [4]). Clients’ initial motivation to change alcohol-related behavior certainly informs delivery of MI and MET [4], and may then impact effectiveness. For example, in a randomized trial with problem drinkers, Heather and colleagues [5] found that MI was more effective in reducing alcohol consumption than behavior-change skills training for low-motivated clients. However, Maisto and colleagues’ [6] report contrasting effects in a randomized controlled trial (RCT) comparison of MET and brief advice with a similar alcohol-misusing population. Although reviews [7–9] consistently note post-intervention motivation as a robust predictor of change in alcohol-related behavior, the collective data from smaller, single-site studies remain equivocal as to whether MET or other adaptations of MI are differentially effective for clientele of varying pre-treatment motivation.
On strictly conceptual grounds it seems quite reasonable—if post-treatment motivation for change is a desired proximal outcome—that MET interventions that target a strengthening of client motivation via resolution of ambivalence about change might be more helpful than some alternatives for clients who arrive for treatment less eager to engage in services. Based upon this logic and prior research, the Project MATCH Research Group [10] originally proposed that clients with low baseline motivational readiness to change would have better outcomes if assigned to MET [3], compared to those assigned to cognitive–behavioral treatment (CBT), a treatment that was designed to teach clients specific skills such as coping behavior, examining thoughts and problem solving [11]. Project MATCH was a multi-site, randomized clinical alcohol treatment study designed to test a number of client attribute × treatment-matching hypotheses in both free-standing out-patient treatment and continuing care following a more intensive treatment episode. However, the Project MATCH Research Group [10,12] found minimal support for the motivation-matching hypothesis. Among the out-patient participants there was a significant motivation × treatment effect in the expected direction, but only at the 15-month follow-up: low-motivated MET clients had more days abstinent than low-motivated CBT clients [13]. Immediately following treatment the low-motivated clients assigned to CBT had significantly more days abstinent than the low-motivated clients assigned to MET. Among the highly motivated clients, there were no differences in drinking outcomes between MET and CBT clients at any time-points. For the continuing care (i.e. aftercare) sample, there was no significant motivation × by treatment interaction effect. The recently reported results from the UK Alcohol Treatment Trial [14], a multi-site study designed to test similar matching hypotheses to Project MATCH, also provided no support for a motivation × treatment-matching effect.
These null findings for the motivation-matching hypothesis may be explained partially by three factors: first, the manner in which the Project MATCH researchers defined ‘low’ versus ‘high’ motivation. To measure motivation the University of Rhode Island Change Assessment (URICA) [15] scores for each client were divided to create low, medium and high motivation subgroups [13]. To examine the impact of treatment on alcohol use at varying levels of motivation, clients in the medium subgroup were excluded from analyses, leaving only the lower and upper thirds to represent low and high motivation, respectively. However, excluding the middle third and using only the lower and upper third of cases substantially reduces statistical power [16]. Secondly, as discussed by the United Kingdom Alcohol Treatment Trial (UKATT) Research Team [14], it could be that in both Project MATCH and the UKATT trial the matching hypotheses were too simplistic and perhaps matching on client profiles that consist of more than one matching variable might be needed. For example, a recent review of predictors of alcohol treatment outcomes suggested that it is important to examine interactions between multiple client characteristics (e.g. gender and problem severity) in the prediction of outcomes [17]. It may be the case that a hypothesized matching variable could be meaningful for females, but not males (or the converse), as suggested by original inclusion of gender-matching hypotheses in Project MATCH. Consistent with this notion, Greenfield and colleagues [18] recently found a three-way interaction between psychiatric symptoms, time and treatment group (mixed-gender via women-only groups) in the prediction of substance use outcomes. Finally, both the Project MATCH and UKATT analytical techniques did not take advantage of the heterogeneity in post-treatment drinking patterns. When a behavior is highly heterogeneous (as drinking often is following treatment) it is often useful to characterize that heterogeneity in order to identify discrete patterns of growth. Not doing so can obscure important relationships, which can result in null findings [19]. Alluding to this issue in their discussion of the motivation matching findings, DiClemente and colleagues [13] stated: ‘we need to understand better the larger process of change for drinking behavior in order to be able to better promote movement through that change process’ (p. 220).
Gaining a better understanding of the process of drinking behavior change was the primary goal of two recent studies designed to re-examine two of the Project MATCH matching hypotheses by applying a novel analytical technique, growth mixture modeling (GMM), to the Project MATCH data [19,20]. Specifically, Witkiewitz and colleagues [19] found partial support for the self-efficacy matching hypothesis (individuals low in self-efficacy at baseline would have better outcomes if assigned to CBT compared to MET) in the prediction of percentage of drinking days among the out-patient MATCH sample. Wu & Witkiewitz [20] found partial support for the network support hypothesis [individuals with high network support for drinking would have better outcomes if assigned to 12-Step facilitation (TSF) compared to CBT or MET] in the prediction of drinking consequences in the out-patient MATCH sample.
The goals of the current study were to replicate the unconditional mixture models that were conducted with the Project MATCH out-patient sample [19] in the Project MATCH aftercare sample; and to use GMM to re-examine the Project MATCH motivation-matching hypothesis, which stated that clients low in motivational readiness to change at the beginning of treatment would have better outcomes if assigned to MET compared to CBT, whereas CBT would be better for clients who had higher motivational readiness to change prior to the start of treatment.
In addition, we considered two hypotheses that contained higher-order interactions. First, given recent analyses of the Project MATCH data that identified alcohol dependence as a significant predictor of drinking outcomes using a mixture modeling approach [21], we incorporated alcohol dependence as a predictor of outcomes. Informed by review of the Project MATCH monographs, we hypothesized that individuals with higher dependence severity would have worse drinking outcomes if assigned to MET [22]. Secondly, we were interested in testing whether outcome differences occurred by gender. Recent research has identified gender as a significant predictor of outcomes [17] and others have suggested the importance of examining complex relations between gender and treatment settings in the prediction of outcomes [18,23]. Specifically, we hypothesized that women would have better outcomes than men and that women with low motivation assigned to MET would have better outcomes than women with low motivation assigned to CBT. We did not have any specific hypotheses about outcome differences between men and women with respect to out-patient and aftercare treatment settings; however, given the findings of Greenfield et al. [18] we did examine potential interactions between gender, treatment setting and outcomes.
METHODS
Participants and procedures
Project MATCH recruited 1726 clients (952 out-patient and 774 aftercare) from 10 clinical research units across the United States. In the out-patient arm, participants were recruited from the community or out-patient treatment centers. In the aftercare arm, participants were recruited from intensive day hospital or in-patient treatment centers. Upon meeting the inclusion and exclusion criteria [10], participants were given an intake assessment and were then randomized to one of three treatments: (i) CBT [11], (ii) MET [3] or (iii) TSF [24]. All treatments were delivered over the course of 3 months. In the current study only the CBT (n = 567) and MET (n = 577) groups were included in the analyses. Table 1 displays characteristics for the MET and CBT participants. For more information on demographics, please refer to previous publications from Project MATCH [10,12,25] Follow-up assessments were conducted immediately post-treatment, 6, 9, 12 and 15 months after intake. Measures relevant to the current study are described below. For a comprehensive list of all assessments see Project MATCH [10,12].
Table 1.
Demographic characteristics, baseline motivation and drinking behavior.
| Out-patient sample (n = 617) |
Aftercare sample (n = 527) |
|||
|---|---|---|---|---|
| MET (n = 316) | CBT (n = 301) | MET (n = 261) | CBT (n = 266) | |
| n (% female) | 316 (25.6%) | 301 (27.9%) | 261 (18.0%) | 266 (24.1%) |
| URICA (SD) | 10.60 (1.60) | 10.44 (1.80) | 11.04 (1.65) | 11.10 (1.41) |
| Alcohol dependence | 5.75 (1.81) | 5.80 (1.96) | 6.89 (1.84) | 6.68 (2.01) |
| PDD baseline (SD) | 65% (29%) | 67% (29%) | 75% (28%) | 72% (30%) |
| PDD month 4 (SD) | 25% (30%) | 21% (30%) | 14% (27%) | 14% (27%) |
| PDD month 5 (SD) | 27% (33%) | 25% (33%) | 16% (29%) | 15% (29%) |
| PDD month 6 (SD) | 26% (32%) | 26% (32%) | 18% (30%) | 16% (30%) |
| PDD month 7 (SD) | 26% (31%) | 27% (32%) | 19% (31%) | 15% (28%) |
| PDD month 8 (SD) | 26% (32%) | 27% (34%) | 22% (35%) | 17% (31%) |
| PDD month 9 (SD) | 27% (33%) | 30% (34%) | 22% (34%) | 17% (30%) |
| PDD month 10 (SD) | 29% (35%) | 29% (34%) | 22% (34%) | 18% (30%) |
| PDD month 11 (SD) | 28% (35%) | 28% (35%) | 22% (35%) | 17% (30%) |
| PDD month 12 (SD) | 26% (34%) | 28% (34%) | 23% (35%) | 18% (32%) |
| PDD month 13 (SD) | 28% (35%) | 29% (35%) | 22% (36%) | 19% (32%) |
| PDD month 14 (SD) | 28% (35%) | 28% (35%) | 22% (35%) | 18% (31%) |
| PDD month 15 (SD) | 28% (35%) | 28% (35%) | 23% (35%) | 19% (32%) |
MET: motivational enhancement therapy; CBT: cognitive–behavioral therapy; URICA: University of Rhode Island Change Assessment; PDD: percentage of drinking days. All variables with standard deviation (SD) in parentheses are mean scores.
Measures
Drinking frequency
The criterion variable for the current study was percentage of drinking days (PDD) in all months following treatment, derived from the Form-90 instrument [26]. PDD is a reflection of percentage of days abstinent (PDA), which was one of the primary outcome measures in Project MATCH and the only outcome measure for which partial support was found of the motivation-matching hypothesis. PDA has also been identified as a measure of drinking frequency that is commonly employed [27]. Subtracting PDA from 100 to create PDD provided a zero point that represented the absence of drinking, which was necessary for the two-part modeling strategy described below. It is also important to note that because of the modeling strategy employed in the current study we did not perform any transformations of PDD, as was conducted in Project MATCH. As described below, the strategy used in the current study assumes non-normality of the dependent variable and thus does not require the dependent variables to be distributed normally. In Project MATCH self-reported drinking data were corroborated via collateral informants and biochemical measures [12]. Drinking frequency in the first month following treatment was used as the first time-point in the growth mixture models, described below. Baseline PDD was also included as a covariate in all analyses.
Motivation for change
The University of Rhode Island Change Assessment (URICA) [15] scores were used to assess motivation for change at intake. The URICA includes 28 items assessing a client’s motivation for change measured on a five-point scale (1 = strongly disagree to 5 = strongly agree). The 28 items were used to calculate a total readiness score (continuous measure) by summing together the average scores on contemplation, action and maintenance sub-scales and subtracting the average score on the pre-contemplation subscale. The total readiness score was used as the primary measure of motivation in Project MATCH and the current study. The reliability of the URICA readiness score was adequate (Cronbach’s α 0.75).
Alcohol dependence was defined as the number of current alcohol dependence symptoms (range 0–9), based on the Structured Clinical Interview for DSM disorders (SCID) [27] administered prior to treatment.
Statistical analyses
Growth mixture modeling (GMM) is an analytical strategy that takes into account individual variability in the process of change across time [28]. GMM is a type of finite mixture model, which is a statistical tool that can be used to approximate a ‘mixture’ of normal distributions from a non-normal distribution. In the case of GMM, non-normally distributed growth factors (i.e. intercept and slope) are approximated as multiple classes of continuous growth, such that common patterns of drinking trajectories could be estimated separately from dissimilar trajectories. Each ‘class’ of drinking trajectories is approximately normally distributed (a testable assumption), with its own mean growth and variation around the mean growth. Importantly, recent criticisms of GMM [29] and simulation studies [30,31] have indicated that using GMM to identify classes and then making direct inferences regarding the estimated classes can result in erroneous conclusions (for an overview see [32,33]). However, using GMM as a statistical tool for parsing heterogeneity and then returning to the whole population (rather than individual classes) when making inferences avoids many of the previously identified problems of the direct applications of GMM. This ‘indirect’ application of GMM simply identifies a number of latent trajectory classes and then evaluates expected values of trajectory intercepts, slopes or covariate effects mixed over classes, providing a single set of estimates using an average across the within-class predicted values.
GMM can also be extended to include covariates and can be used within a two-part framework for semi-continuous outcomes (an outcome that is characterized by a continuous distribution with a preponderance of values at one or more locations). Alcohol use is often semi-continuous immediately following treatment where most individuals are not drinking and other individuals are drinking some amount, which is distributed continuously across individuals. The two-part model (see [19,34]) includes a logistic growth model to derive estimates of drinking versus not across time and a continuous growth model that incorporates drinkers and non-drinkers to estimate the average alcohol use, if any, for all participants, across time [34].
The program Mplus version 5.21 [35] was used to estimate all models. Mplus utilizes full information maximum likelihood estimation under the assumption of missing at random (MAR) with robust standard errors (called the MLR estimator in Mplus), an accepted approach for handling missing data [21,36].
Data analyses can be summarized in two steps. First, a series of unconditional two-part growth mixture models were estimated in the aftercare sample in an attempt to replicate the out-patient three-class growth mixture model identified previously [19]. The relative fit of models with varying numbers of classes was assessed using the two most widely cited methods: the Bayesian information criterion (BIC) and the bootstrapped likelihood ratio test (BLRT) [29,37,38]. The BIC provides a measure of relative model fit (when comparing similar models) where smaller values of the BIC indicate a better-fitting model. The BLRT provides a significance test for the fit of a k − 1 class model against a k class model, with a significant P-value indicating that the null hypothesis of k − 1 classes should be rejected in favor of at least k classes [38].
PDD at months 4–15 (post-intake, 1–12 months post-treatment) were used as the observed indicators in the growth mixture model. Five continuous latent growth factors were estimated: three for the continuous growth process: (i) intercept (i.e. PDD following treatment), (ii) linear slope (i.e. linear rate of change after treatment), (iii) quadratic slope (i.e. non-linear rate of change after treatment); and two for the categorical growth process (i) intercept (i.e. drinking or not following treatment) and (ii) linear slope (i.e. rate of change in drinking or not). Individuals were allowed to vary on intercept and linear slope terms within each class. The variance of the quadratic slope was fixed at zero because negative variances were estimated in some iterations (indicating that the observed variance was near zero).
Secondly, the URICA scores at baseline were mean-centered and incorporated into a series of conditional two-part growth mixture models. The three covariates, baseline URICA scores, treatment assignment (CBT = 0 versus MET = 1) and the URICA × treatment assignment interaction, were added to the model systematically in order to evaluate model stability under different model specifications (e.g. predicting class membership, predicting growth parameters). The individual growth factors within each class (i.e. class-varying) were regressed on the three covariates of interest providing within-class predicted regression estimates. A mixed-effect estimate was then calculated by weighting the within-class predicted values by the probabilities of class membership (given the covariate effects) and then summing together the within-class weighted regression estimates to provide a single-population level estimate of the regression of the growth factors on the covariate effects. Baseline PDD and alcohol dependence were also included as covariates of within-class growth.
RESULTS
Unconditional models: replication of GMM with aftercare sample
In the current study the unconditional three-class two-part growth mixture model of drinking frequency provided the best balance of parsimony and model fit in the aftercare sample, replicating the findings from the out-patient sample reported by Witkiewitz et al. [19]. For drinking frequency the three classes were defined by evaluating the means of the class-specific growth factors. In the aftercare sample, class 1 (‘infrequent drinkers’) had a mean PDD intercept of 4% with a non-significant slope (P = 0.97), with approximately 72.0% of the sample (n ≈ 379) most probably classified in class 1. Class 2 (‘increasing frequency drinkers’ were comprised of approximately 12.5% of the sample, n ≈ 66) had a mean PDD intercept of 9% and a significantly positive slope of 18% (P < 0.001). An additional 15.5% of the sample (n ≈ 82) was most probably classified in class 3 (‘frequent drinkers’), which had a mean PDD intercept of 73% and a non-significant slope (P = 0.58). Average latent class probabilities showed a strong correspondence between latent class probabilities and most probably latent class membership (probabilities of correct classification were 0.89, 0.96 and 0.95 for classes 1–3, respectively).
Conditional models
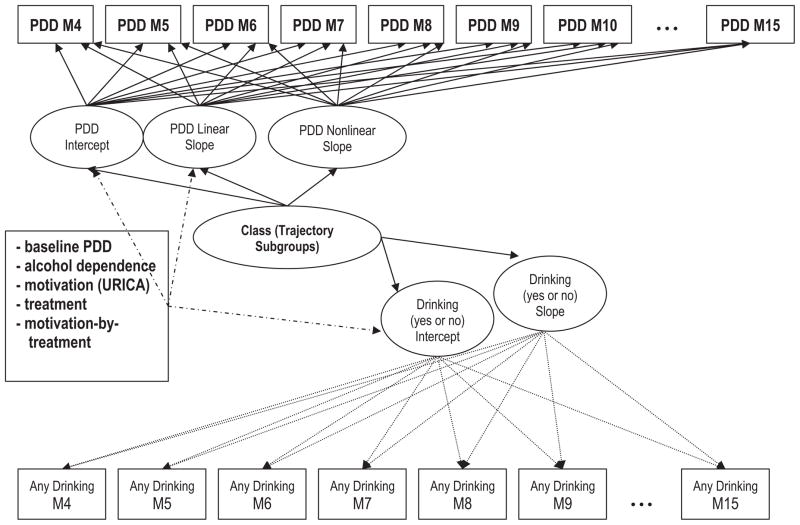
Next, the conditional model shown in Fig. 1 was estimated. For both out-patient and aftercare samples the class probabilities in both conditional models mirrored the estimates from the unconditional models, and classification quality did not change with the inclusion of covariates. As shown in Table 2, for the out-patient sample baseline PDD, treatment condition and the motivation × treatment interaction were significant predictors of the slope of drinking frequency, baseline PDD was also a significant predictor of the intercept, and both baseline PDD and number of alcohol dependence symptoms were related significantly to the intercept of any drinking. For the aftercare sample, baseline PDD and alcohol dependence symptoms were related significantly to the intercept of PDD, and no other covariate effects were significant.
Figure 1.
Hypothesized conditional two-part growth mixture model. PDD: percentage of days drinking; URICA: University of Rhode Island Change Assessment
Table 2.
Regression estimates (standard errors) for conditional growth mixture model.
| Out-patient B (SE) | Aftercare B (SE) | |
|---|---|---|
| Intercept on | ||
| PDD baseline | 0.41 (0.05)* | 0.18 (0.08)* |
| Alcohol dependence | 0.002 (0.01) | 0.03 (0.01)* |
| Motivation (URICA) | −0.01 (0.02) | 0.03 (0.03) |
| Treatment (CBT = 0, MET = 1) | 0.37 (0.21) | −0.11 (0.36) |
| Motivation × treatment | −0.03 (0.02) | 0.01 (0.03) |
| Slope on | ||
| PDD baseline | 0.02 (0.01)* | 0.003 (0.01) |
| Alcohol dependence | −0.001 (0.001) | 0.00 (0.001) |
| Motivation (URICA) | −0.002 (0.001) | −0.002 (0.003) |
| Treatment (CBT = 0, MET = 1) | −0.07 (0.02)* | 0.04 (0.04) |
| Motivation × treatment | 0.01 (0.002)* | −0.003 (0.003) |
| Any drinking intercept on | ||
| PDD baseline | 3.17 (0.68)* | 0.38 (0.79) |
| Alcohol dependence | −0.22 (0.10)* | 0.16 (0.11) |
| Motivation (URICA) | −0.24 (0.17) | 0.17 (0.21) |
| Treatment (CBT = 0, MET = 1) | 0.89 (2.32) | 3.79 (3.30) |
| Motivation × treatment | −0.05 (0.22) | −0.31 (0.30) |
Significant at α < 0.05. B: unstandardized regression coefficient; SE: standard error; MET: motivational enhancement therapy, CBT: cognitive–behavioral therapy; URICA: University of Rhode Island Change Assessment; PDD: percentage of drinking days.
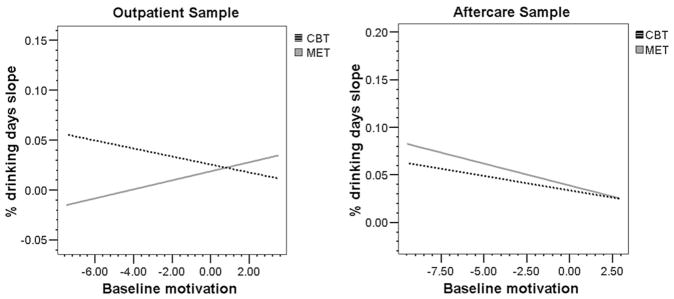
Motivation × treatment interaction
In the out-patient sample the motivation × treatment interaction effect was a significant predictor of the change in drinking frequency over time [B (SE) = 0.01 (0.002], P = 0.01 f2 = 0.02). As seen in Fig. 2a, individuals who were assigned randomly to MET with lower baseline motivation (below-average motivation) evinced less of an increase in the slope of drinking frequency compared to those assigned to CBT, supporting the Project MATCH matching hypothesis. The motivation × treatment interaction effect was not significant in the aftercare sample. As shown in Fig. 2b, individuals with low baseline motivation, regardless of treatment assignment, had greater increases in drinking frequency over time.
Figure 2.
Interaction between motivation and treatment assignment in predicting the slope of drinking frequency. CBT: cognitive–behavioural therapy; MET: motivational enhancement therapy
Within the context of using the indirect method of growth mixture modeling, the meaning of the significant motivation × treatment interaction effect in the out-patient sample can be interpreted as: across the population of individuals with low motivation to change at the initiation of out-patient alcohol treatment, those who received MET were likely to drink less frequently over time compared to those who received CBT. However, this effect needs to be evaluated in the context of the analysis, which essentially parses the heterogeneity of drinking outcomes into discrete classes of drinkers, estimates the effect of the motivation × treatment interaction within each class, and then combines across classes to create a summary estimate that can be generalized to a population. The interaction effect within each class is weighted by the size of each class and then pooled to make a population estimate, therefore the population estimates are determined predominantly by the estimated effect within the largest class (the ‘infrequent drinking’ class in the current sample). Further evaluation of the within-class effects indicated that the motivation-matching effect was a significant predictor of slope only within the infrequent drinking class. Thus, based on these analyses we can conclude that for the majority of individuals (69% of the out-patient sample, as reported in Witkiewitz et al. [19]) the motivation-matching hypothesis was supported, but it was not supported for all individuals in the sample.
Higher-order interactions
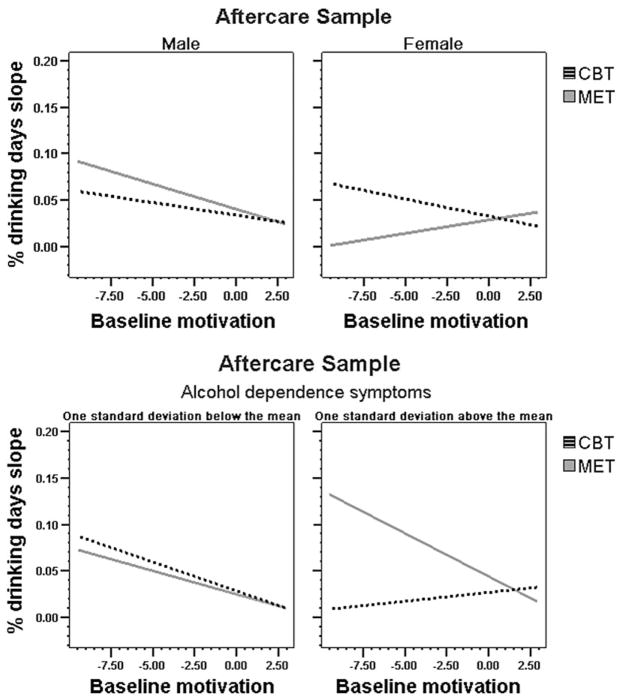
Previous Project MATCH analyses have identified discrepancies across results from the out-patient and aftercare samples in the relation between drinking outcomes and both alcohol dependence symptoms [39] and gender [40], so to further examine the disparity in the significance of the interaction effect across out-patient and aftercare samples we examined whether alcohol dependence and/or gender influenced the lack of an interaction effect in either sample. To evaluate this question we conducted moderation analyses with mean-centered alcohol dependence scores multiplied by mean-centered motivation and with gender multiplied by mean-centered motivation scores using the methods described by Aitken & West [41]. In order to probe the interaction for alcohol dependence we dichotomized alcohol dependence symptoms at 1 standard deviation (SD) below and above the mean of alcohol dependence symptoms within each treatment arm and then examined the relation between baseline motivation and model estimated individual drinking slopes at each level of alcohol dependence. The gender interaction was examined by looking at the relation between baseline motivation and treatment group and model-estimated individual drinking slopes by gender.
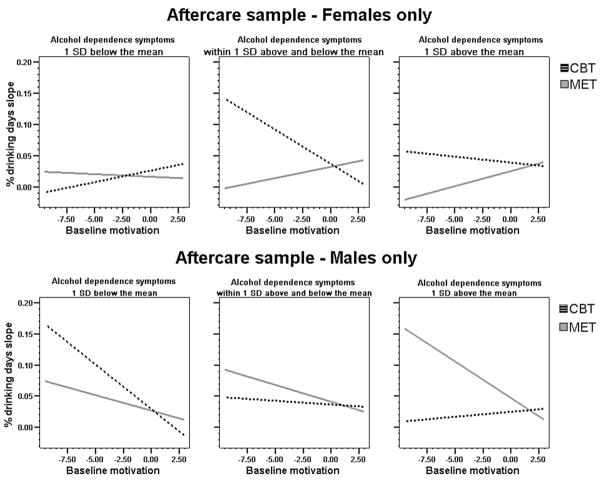
As shown in Fig. 3a, among the aftercare participants there was an interaction between motivation and treatment in predicting drinking slope in the hypothesized direction for females. However, the matching effect was in the opposite direction for individuals with an above-average number of alcohol dependence symptoms (Fig. 3b): highly alcohol-dependent individuals with lower baseline motivation assigned to MET evinced the greatest increase in drinking frequency over time. Finally, as shown in Fig. 4a and b, the Project MATCH matching hypothesis was supported among females, particularly among those females at higher levels of alcohol dependence (Fig. 4a), and a reverse interaction effect with alcohol dependence was found only among males with the highest number of alcohol dependence symptoms (Fig. 4b). Moderated regression analyses were then conducted to examine the significance of these effects. As shown in Table 3, the three-way alcohol dependence × treatment × motivation interaction was significant for males [B (SE) = −0.004 (0.002), P = 0.03, f2 = 0.03], but not for females [B (SE) = 0.004 (0.003), P = 0.18, f2 = 0.02] in the aftercare sample. The three-way interaction was not significant for the out-patient sample and neither alcohol dependence nor gender moderated the outcomes found in the out-patient sample.
Figure 3.
Interactions between gender, alcohol dependence symptoms, motivation and treatment assignment in the prediction of drinking frequency. CBT: cognitive–behavioural therapy; MET: motivational enhancement therapy
Figure 4.
Three-way interactions between gender, alcohol dependence symptoms, motivation and treatment assignment in the prediction of drinking frequency. CBT: cognitive–behavioural therapy; MET: motivational enhancement therapy
Table 3.
Moderated regression estimates (standard errors) for aftercare sample.
| Males B (SE) | Females B (SE) | |
|---|---|---|
| Baseline PDD | 0.02 (0.01)* | 0.01 (0.01) |
| Motivation | −0.002 (0.003) | −0.01 (0.004) |
| Treatment group | 0.06 (0.04) | −0.14 (0.07) |
| Motivation by treatment interaction | −0.01 (0.003) | 0.01 (0.01) |
| Alcohol dependence | −0.002 (0.002) | 0.003 (0.003) |
| Alcohol dependence by treatment interaction | 0.04 (0.02)* | −0.04 (0.03) |
| Alcohol dependence by motivation interaction | 0.002 (0.001) | −0.001 (0.001) |
| Alcohol dependence by motivation by treatment | −0.003 (0.002)* | 0.004 (0.003) |
Significant at α < 0.05. B: unstandardized regression coefficient; PDD: percentage of drinking days; SE: standard error.
Replication of findings across outcome measures
Although not reported here to conserve space, the analyses for the PDD outcome were replicated with the drinks per drinking day (DDD) outcome measure and with the Drinker Inventory of Consequences (DrInC) [42]. For both the DDD and DrInC models the effects were in the same direction as observed with the PDD outcome, indicating significant treatment × motivation interactions in the prediction of change over time for both DDD and DrInC scores in the out-patient sample. There was also a significant treatment × motivation interaction effect in the prediction of DrInC slope in the aftercare sample. The aftercare findings for the DDD outcome were consistent with the PDD outcome findings (significant interaction effects for females and males with low levels of alcohol dependence). Full results from these analyses are available from the first author.
DISCUSSION
Project MATCH has been criticized widely for failing to find support for the large majority of the matching hypotheses [43]. The current study found partial empirical support for the motivation matching hypotheses during the first year following treatment. The majority of out-patient participants with lower baseline motivation to change their drinking who were assigned to MET had better outcomes (less frequent drinking) over time compared to low-motivated participants assigned to CBT. Among aftercare participants there was not a significant matching effect for the total sample; however, low-motivated females and low-motivated males with below-average alcohol dependence (1 SD below the mean number of alcohol dependence symptoms for aftercare participants), who were assigned to MET, reported less frequent drinking over time, whereas those assigned to CBT reported more frequent drinking over time. Among males in the aftercare sample with above-average alcohol dependence (8.77 symptoms of dependence or greater), those with lower baseline motivation had significantly worse outcomes if assigned to MET compared to those with lower baseline motivation assigned to CBT.
It is important to point out some sampling differences between the out-patient and aftercare arms that might help to explain the disparate findings across treatment settings. In general, individuals in aftercare and male participants had significantly more alcohol dependence symptoms (out-patient versus aftercare: t(1142) = −8.91, P < 0.001; males versus females: t(1142) = 2.53, P = 0.01). Moreover, there were significant differences between dependence symptoms among males and females in the aftercare condition (t(525) = 2.89, P = 0.004), but not among males and females in the out-patient condition (t(615) = 0.19, P = 0.85). Thus, of all Project MATCH groups, males in aftercare had significantly more symptoms of dependence. These results are consistent with the original alcohol involvement-matching hypothesis: that individuals with high levels of alcohol dependence are less likely to benefit from a less intensive treatment (e.g. MET) and this might especially be the case for individuals with high levels of dependence and low levels of motivation to change.
Findings that help to identify client moderators of MET effectiveness—particularly those of a larger, multi-site trial such as Project MATCH—inform our notions of treatment-matching. Current findings may be particularly useful given inconsistent moderation effects of baseline client motivation reported previously in smaller, single-site studies [5,6,44]. The field continues to explore other potential moderators of MET effectiveness, including client-variables that might be expected to overlap with client motivation—such as whether one is/is not mandated to alcohol treatment, or has a high/low alcohol problem severity. In a meta-analytical review of the effectiveness of MI-based interventions for alcohol misuse, Vasilaki and colleagues [9] lend support to the moderating effects of these variables—concluding that MI-based interventions are most effective with those seeking alcohol treatment of their own accord, and/or with mild-to-moderate alcohol dependence. Although original Project MATCH analyses identified client anger as a predictor of differential effectiveness of MET [45], subsequent attempts to establish other client moderators of MI-based interventions have been less convincing. Basic demographic dimensions (e.g. age, gender) have generally not been robust or reliable predictors of outcome—with the noted exception of client ethnicity [8].
A key limitation of this secondary analysis project was an inability to examine specific mechanisms through which the motivation-matching effect may work. MET worked better for low-motivated clients, presumably because MET was designed to increase motivation to change, which then facilitates a change in drinking behavior. While Project MATCH did administer the URICA at the end of treatment, previous research [13] and our measurement invariance testing indicated that the responses to the URICA measure shifted over time, such that the end of treatment URICA scores and baseline URICA scores were not measuring the same construct. Thus, determining whether an increase in motivation from pre-treatment to end of treatment was the mechanism of change in the current study was not possible. Future studies could examine changes in motivation during the course of treatment and whether these changes mediate the relationship between treatment assignment and alcohol treatment outcomes. An additional limitation is the relatively small effect sizes, even for those effects that were statistically significant, as well as the large number of statistical tests. As described by Finney [46], these weaker higher-order interactions might not be very promising for identifying client–treatment matches, and focusing upon individual differences in responses to treatment via adaptive treatment designs [47] could yield better treatment outcomes.
The results of this study have two direct treatment implications. First, the majority of individuals seeking out-patient treatment who are not motivated to change their drinking behavior may benefit more from MET than CBT, because in the absence of motivation skills training could be premature [5]. Secondly, low-motivated males with higher levels of alcohol dependence in in-patient or aftercare settings might fare better with CBT. It may also be the case that MET and skills training need to be provided concurrently based on the evolving needs of the client. For example, MET could set the tone and provide the base for treatment, which could be supplemented by selective skills training when the client demonstrates skills deficits [48,49]. Current findings may also hold broader implications for those utilizing and evaluating MET-based interventions. By advancing understanding of with whom MET interventions are most effective, findings may inform ongoing efforts to identify mechanisms that contribute to client behavior change [50]. Identification of client and setting attributes that influence effectiveness of MET may also increase understanding of the specific therapeutic processes that distinguish it from other intervention approaches [51]. Finally, current findings that support the original treatment-matching hypotheses of Project MATCH may also inform decisions about whether and how MET delivery is tailored for specific client populations. Future research should continue to explore factors that may account for differential outcomes in evaluation of MET and other empirically supported approaches to intervention for substance-misusing clients.
Acknowledgments
This research was supported by National Institute of Alcohol Abuse and Alcoholism Grant RO3: AA016322-01 (Witkiewitz, Principal Investigator). We acknowledge Nadia Villarroel for assistance with preparation of this manuscript and Johnny Wu for his input on analyses and earlier versions of this manuscript.
Footnotes
Declarations of interest
None.
References
- 1.DiClemente CC, Bellino LE, Neavins TM. Motivation for change and alcoholism treatment. Alcohol Health Res World. 1999;23:86–92. [PMC free article] [PubMed] [Google Scholar]
- 2.Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2. New York: Guilford Press; 2002. [Google Scholar]
- 3.Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivation Enhancement Therapy Manual: A Clinical Research Guide for Therapists. Washington, DC: US Government Printing Office; 1992. [Google Scholar]
- 4.Miller WR, Wilbourne PL. Mesa grande: a methodological analysis of clinical trials of treatment for alcohol use disorders. Addiction. 2002;97:265–77. doi: 10.1046/j.1360-0443.2002.00019.x. [DOI] [PubMed] [Google Scholar]
- 5.Heather N, Rollnick S, Bell A, Richmond R. Effects of brief counseling among male heavy drinkers identified on general hospital wards. Drug Alcohol Rev. 1996;15:29–38. doi: 10.1080/09595239600185641. [DOI] [PubMed] [Google Scholar]
- 6.Maisto SA, Conigliaro J, McNeil M, Kraemer K, Conigliaro RL, Kelley ME. Effects of two types of brief intervention and readiness to change on alcohol use in hazardous drinkers. J Stud Alcohol. 2001;62:605–14. doi: 10.15288/jsa.2001.62.605. [DOI] [PubMed] [Google Scholar]
- 7.Dunn C, DeRoo L, Rivara FP. The use of brief interventions adapted from motivational interviewing across behavioral domains: a systematic review. Addiction. 2001;96:1725–42. doi: 10.1046/j.1360-0443.2001.961217253.x. [DOI] [PubMed] [Google Scholar]
- 8.Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- 9.Vasilaki EI, Hosier SG, Cox WM. The efficacy of motivational interviewing as a brief intervention for excessive drinking: a meta-analytic review. Alcohol Alcohol. 2006;41:328–55. doi: 10.1093/alcalc/agl016. [DOI] [PubMed] [Google Scholar]
- 10.Project MATCH Research Group. Rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcohol Clin Exp Res. 1993;17:1130–45. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- 11.Kadden R, Carroll KM, Donovan D, Cooney N, Monti P, Abrams D, et al. NIAAA Project MATCH Monograph Series, vol. 3, NIH Publication no. 94-3724. Bethesda, MD: Department of Health and Human Services; 1992. Cognitive-Behavioral Copings Skills Therapy Manual: A Clinical Research Guide for Therapists Treating Individuals with Alcohol Abuse and Dependence. [Google Scholar]
- 12.Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- 13.DiClemente CC, Carbonari J, Zweben A, Morrel T, Lee RE. Motivation hypothesis causal chain analysis. In: Longabaugh R, Wirtz PW, editors. Project MATCH: Hypotheses, Results, and Causal Chain Analyses, NIAAA Project MATCH Monograph Series, vol. 8, NIH Publication no. 01-4238. Bethesda, MD: Department of Health and Human Services; 2001. pp. 206–22. [Google Scholar]
- 14.United Kingdom Alcohol Treatment Trial (UKATT) Research Team. UK alcohol treatment trial: client-treatment matching effects. Addiction. 2008;103:228–38. doi: 10.1111/j.1360-0443.2007.02060.x. [DOI] [PubMed] [Google Scholar]
- 15.DiClemente CC, Hughes SO. Stages of change profiles in alcoholism treatment. J Subst Abuse. 1990;2:217–35. doi: 10.1016/s0899-3289(05)80057-4. [DOI] [PubMed] [Google Scholar]
- 16.Preacher KJ, Rucker DD, MacCallum RC, Nicewander WA. Use of extreme groups approach: a critical reexamination and new recommendations. Psychol Methods. 2005;10:178–92. doi: 10.1037/1082-989X.10.2.178. [DOI] [PubMed] [Google Scholar]
- 17.Adamson SJ, Sellman JD, Frampton CM. Patient predictors of alcohol treatment outcome: a systematic review. J Subst Abuse Treat. 2009;36:75–86. doi: 10.1016/j.jsat.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 18.Greenfield SF, Sharpe-Potter J, Lincoln MF, Popuch RE, Kuper L, Gallop RJ. High psychiatric symptom severity is a moderator of substance abuse treatment outcomes among women in single versus mixed gender group treatment. Am J Drug Alcohol Abuse. 2008;34:594–602. doi: 10.1080/00952990802304980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Witkiewitz K, van der Maas HJ, Hufford MR, Marlatt GA. Non-normality and divergence in post-treatment alcohol use: re-examining the Project MATCH data ‘another way’. J Abnorm Psychol. 2007;116:378–94. doi: 10.1037/0021-843X.116.2.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu J, Witkiewitz K. Network support for drinking: an application of multiple groups growth mixture modeling to examine client–treatment matching. J Stud Alcohol Drug. 2008;69:21–9. doi: 10.15288/jsad.2008.69.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Muthén L, Muthén B. Mplus User’s Guide: Statistical Analysis with Latent Variables. 4. Los Angeles, CA: Muthén & Muthén; 2007. [Google Scholar]
- 22.Rychtarik RG, Miller WR, Tonigan JS. The alcohol involvement matching hypothesis and findings. In: Longabaugh R, Wirtz PW, editors. Project MATCH Hypotheses: Results and Causal Chain Analyses, Project MATCH Monograph Series. Vol. 8. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2001. pp. 44–60. [Google Scholar]
- 23.Hensing G, Spak F. Introduction: gendering socio-cultural alcohol and drug research. Alcohol. 2009;44:602–6. doi: 10.1093/alcalc/agp073. [DOI] [PubMed] [Google Scholar]
- 24.Nowinski J, Baker S, Carroll K. NIAAA Project MATCH Monograph Series, vol. 1, NIH Publication no. 94-3722. Bethesda, MD: Department of Health and Human Services; 1992. Twelve Step Facilitation Manual: A Clinical Research Guide for Therapists Treating Individuals with Alcohol Abuse and Dependence. [Google Scholar]
- 25.Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: treatment main effects and matching effects on drinking during treatment. J Stud Alcohol. 1998;59:631–9. doi: 10.15288/jsa.1998.59.631. [DOI] [PubMed] [Google Scholar]
- 26.Miller WR, Del Boca FK. Measurement of drinking behavior using the Form 90 Family of Instruments. J Stud Alcohol. 1994;12:112–8. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- 27.Babor TF, Longabaugh R, Zweben A, Fuller RK, Stout RL, Anton RF, et al. Issues in the definition and measurement of drinking outcomes in alcoholism treatment research. J Stud Alcohol Suppl. 1994;12:101–11. doi: 10.15288/jsas.1994.s12.101. [DOI] [PubMed] [Google Scholar]
- 28.Spitzer RL, Williams JB. Structured Clinical Interview for DSM-III-R. Patient version. New York: New York State Psychiatric Institute; 1985. [Google Scholar]
- 29.Muthén BO. Latent variable analysis: growth mixture modeling and related techniques for longitudinal data. In: Kaplan D, editor. The Sage Handbook of Quantitative Methodology for the Social Sciences. Thousand Oaks, CA: Sage Publications; 2004. pp. 345–68. [Google Scholar]
- 30.Bauer DJ, Curran PJ. Distributional assumptions of growth mixture models: implications for over-extraction of latent trajectory classes. Psychol Methods. 2003a;8:338–63. doi: 10.1037/1082-989X.8.3.338. [DOI] [PubMed] [Google Scholar]
- 31.Bauer DJ, Curran PJ. Over-extracting latent trajectory classes: much ado about nothing? Psychol Methods. 2003b;8:384–93. doi: 10.1037/1082-989X.8.3.338. [DOI] [PubMed] [Google Scholar]
- 32.Hipp JR, Bauer DJ. Local solutions in the estimation of growth mixture models. Psychol Methods. 2006;11:36–53. doi: 10.1037/1082-989X.11.1.36. [DOI] [PubMed] [Google Scholar]
- 33.Bauer DJ. Observations on the use of growth mixture models in psychological research. Multivariate Behav Res. 2007;42:757–86. [Google Scholar]
- 34.Muthén B. Second-generation structural equation modeling with a combination of categorical and continuous latent variables: new opportunities for latent class/latent growth modeling. In: Collins LM, Sayer A, editors. New Methods for the Analysis of Change. Washington, DC: APA; 2001. pp. 291–322. [Google Scholar]
- 35.Olsen MK, Schafer JL. A two-part random effects model for semi-continuous longitudinal data. J Am Stat Assoc. 2001;96:730–45. [Google Scholar]
- 36.Little RJA, Rubin DB. Statistical Analysis with Missing Data. 2. New York: Wiley-Interscience; 2002. [Google Scholar]
- 37.Muthén B, Shedden K. Finite mixture modeling with mixture outcomes using the EM algorithm. Biometrics. 1999;55:463–9. doi: 10.1111/j.0006-341x.1999.00463.x. [DOI] [PubMed] [Google Scholar]
- 38.Nylund KL, Asparouhov T, Muthen B. Deciding on the number of classes in latent class analysis and growth mixture modeling. A Monte Carlo simulation study. Struct Equ Modeling. 2007;14:535–69. [Google Scholar]
- 39.Witkiewitz K. Lapses following alcohol treatment: modeling the falls from the wagon. J Stud Alcohol Drugs. 2008;69:594–604. doi: 10.15288/jsad.2008.69.594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Del Boca FK, Mattson ME. Project MATCH Monograph Series. Bethesda, MD: US Department of Health and Human Services; 2001. The Gender Matching Hypothesis. [Google Scholar]
- 41.Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- 42.Miller WR, Tonigan JS, Longabaugh R. The Drinker Inventory of Consequences (DrInC): An Instrument for Assessing Adverse Consequences of Alcohol Abuse. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. [Google Scholar]
- 43.Glaser FB. The unsinkable Project MATCH. Addiction. 1999;94:34–6. [PubMed] [Google Scholar]
- 44.Monti PM, Colby SM, Barnett NP, Spirito A, Rohsenow DJ. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. J Consult Clin Psych. 1999;67:989–94. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- 45.Project MATCH Research Group. Project MATCH secondary a priori hypotheses. Addiction. 1997b;92:1671–98. [PubMed] [Google Scholar]
- 46.Finney JW. Matching clients to psychosocial treatments: at the cusp of hope and evidence? Addiction. 2008;103:239–40. doi: 10.1111/j.1360-0443.2007.02117.x. [DOI] [PubMed] [Google Scholar]
- 47.McKay JR. Continuing care research: what we have learned and where we are going. J Subst Abuse Treat. 2009;36:131–45. doi: 10.1016/j.jsat.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Baer JS, Kivlahan DR, Donovan DM. Integrating skill training and motivational therapies: implications for the treatment of substance dependence. J Subst Abuse Treat. 1999;17:15–23. doi: 10.1016/s0740-5472(98)00072-5. [DOI] [PubMed] [Google Scholar]
- 49.Miller WR, et al., editors. Combine Monograph Series, Volume 1. Combined Behavioral Intervention Manual: A Clinical Research Guide for Therapists Treating People with Alcohol Abuse and Dependence. DHHS Publication No. (NIH): 04-5288. Bethesda, MD: 2004. [Google Scholar]
- 50.Apodaca TR, Longabaugh R. Mechanisms of change in motivational interviewing: a review and preliminary evaluation of the evidence. Addiction. 2009;104:705–15. doi: 10.1111/j.1360-0443.2009.02527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Miller WR, Rollnick S. Ten things that motivational interviewing is not. Behav Cogn Psychother. 2009;37:129–40. doi: 10.1017/S1352465809005128. [DOI] [PubMed] [Google Scholar]