ABSTRACT
BACKGROUND
Pay-for-performance programs could worsen health disparities if providers who care for disadvantaged patients face systematic barriers to providing high-quality care. Risk adjustment that includes sociodemographic factors could mitigate the financial incentive to avoid disadvantaged patients.
OBJECTIVE
To test for associations between quality of care and the composition of a physician’s patient panel.
DESIGN
Repeat cross-sectional analysis
PARTICIPANTS
Nationally representative sample of US primary care physicians responding to a panel telephone survey in 2000–2001 and 2004–2005
MAIN MEASURES
Quality of primary care as measured by provision of eight recommended preventive services (diabetic monitoring [hemoglobin A1c testing, eye examinations, cholesterol testing and urine protein analysis], cancer screening [screening colonoscopy/sigmoidoscopy and mammography], and vaccinations against influenza and pneumococcus) documented in Medicare claims data and the association between quality and the sociodemographic composition of physicians’ patient panels.
KEY RESULTS
Across eight quality measures, physicians’ quality of care was not consistently associated with the composition of their patient panel either in a single year or between time periods. For example, a substantial number (seven) of the eighteen significant associations seen between sociodemographic characteristics and the delivery of preventive services in the first time period were no longer seen in the second time period. Among sociodemographic characteristics, panel Medicaid eligibility was most consistently associated with differences in the delivery of preventive services between time points; among preventive services, the delivery of influenza vaccine was most likely to demonstrate disparities in both time points.
CONCLUSIONS
In a Medicare pay-for-performance program, a better understanding of the effect of effect of patient panel composition on physicians’ quality of care may be necessary before implementing routine statistical adjustment, since the association of quality and sociodemographic composition is small and inconsistent. In addition, we observed improvements between time periods among physicians with varying panel composition.
KEY WORDS: quality, disparities, payment incentives
INTRODUCTION
Physicians and policymakers have raised concerns that pay-for-performance programs could exacerbate health disparities.1 This concern stems from two observations. Research demonstrates that the care of poor or minority patients tends to be clustered among specific subsets of physicians, and that these patients on average receive lower quality care.2,3 If performance bonuses accrue disproportionately to physicians with higher quality scores on average, and these physicians are less likely to provide care to vulnerable populations, this could create a disparity of resources that will further widen the gap between physicians who care for many disadvantaged patients and their peers. Over the longer term, resource and bonus differences may also discourage physicians from caring for disadvantaged populations.4 Some evidence suggests that selected hospitals serving a disproportionate share of poor patients are able to improve care under a pay-for-performance system, but the same has not been shown for physician practices.5
One possible solution to this potential problem is to adjust performance measures and bonuses for the sociodemographic characteristics of a physician’s patient panel.1 Such adjustment for sociodemographic characteristics could "level the playing field" for physicians who disproportionately care for poor or minority patients, particularly because prior research suggests that some sociodemographic factors do also predict the level of practice resources.6,7 The approach would be particularly appropriate if limited resources are a sizable impediment to delivering high quality care to vulnerable populations. Under such a scenario, physicians who lack sufficient staff support, equipment, or ability to access specialists or diagnostic testing may need to work harder to meet their patients’ needs, which are also, on average, greater. If they are resource dependent, receiving fewer bonus payments would cause them to fall further behind in their performance.
The proposal to adjust performance bonuses for patient sociodemographics relies on two important assumptions: that the sociodemographics of the physicians’ patient panel is a reliable predictor of lack of practice resources, and that it is also a reliable marker of poor performance. If these related assumptions are incorrect, and instead patient panel sociodemographics do not reliably predict physician performance, adjusting for patient panel sociodemographics could spuriously reward a lower standard of care for poor and minority patients, which would paradoxically undermine the objective of reducing health disparities.
Recent studies have suggested that the observed link between sociodemographic characteristics of patients and care quality has attenuated over time.8–10 But some of these studies were conducted on insured populations in managed care plans, and others relied on older data. In order to inform policies in pay-for-performance approaches to equitably address health disparities, we used recent Medicare data to test the hypothesis that patient sociodemographics reliably predict providers’ performance as measured by their delivery of preventive services.
METHODS
Overview of Study Design
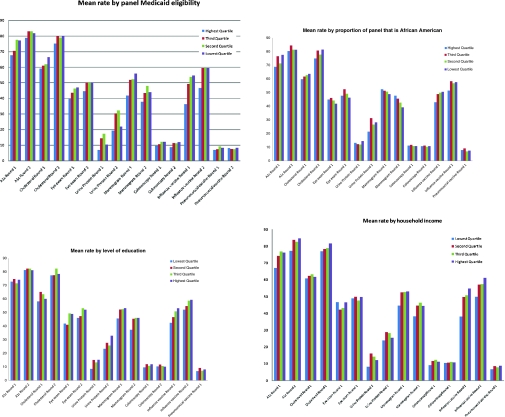
We identified a nationally representative sample of primary care physicians based on the Community Tracking Study (CTS) Physician Survey administered in 2000–2001 and 2004–2005. The two rounds of the CTS survey served as the basis for two time points of evaluation, which will be abbreviated as Round 1 and Round 2. For each round, primary care physicians' rates of delivery of preventive services to their patients who are covered by fee-for-service Medicare was evaluated by an analysis of Medicare claims (in 2000 for the Round 1 and in 2006 for the Round 2). We divided physicians into quartiles based on census tract geocoding of characteristics of their Medicare patients including the median household income, levels of educational attainment, the proportion of their Medicare patients who were also Medicaid-eligible, and the proportion of their patients who were black. Because two of the patient panel characteristics (household income and educational attainment) were obtained from the decennial census which was only conducted in 2000, complete patient panel data is only available for Round 1. For two of the sociodemographic measures we evaluated (educational attainment and household income), populations in the highest quartile were expected to be the least disadvantaged sociodemographically, while for the other two sociodemographic variables (proportion of patients who were black and proportion of patients who were Medicaid-eligible) the highest quartile were expected to be the most disadvantaged sociodemographically. For the purpose of consistency, data in each panel of Figure 1, which shows a graphic representation of provider performance by quartile, is arranged in order from most disadvantaged to least disadvantaged. We compared rates of delivery for each preventive service among physicians whose patients were more likely to be sociodemographically disadvantaged or black, versus for other physicians, in each round.
Figure 1.
Rates of service delivery, stratified by socioeconomic characteristics (2000 and 2006).
Sources of Data
The Community Tracking Study (CTS) Physician Survey is a periodic, nationally representative telephone survey of nonfederal US physicians conducted in 60 randomly selected metropolitan statistical areas and supplemented by a national sample. The survey included physicians who reported at least 20 hours per week of direct patient care in an office- or hospital-based practice, including Bureau of Primary Health Care sites. Residents and fellows and certain specialties such as pathology or anesthesiology were excluded; primary care physicians were oversampled. (Details of the survey have previously been published and are available at http://www.hschange.org/index.cgi?data=04) The third round of the survey, conducted in 2000–2001, had 12,389 completed interviews for a response rate of 59%; 40% of the respondents interviewed were primary care physicians. The fourth round, conducted in 2004–2005 and including the same panel of physicians as well as other, new respondents, had 6,628 completed interviews for a weighted response rate of 52%; 37% of the respondents interviewed were primary care physicians. We drew our analytic sample only from the roughly two-thirds of respondents from the 2000–2001 survey who were targeted for and re-interviewed in the 2004–2005 survey. This group included 1,008 primary care physicians, who represented our final study population. Physician data were linked to patient visit data from the 2000 and 2006 Medicare files using physician respondents’ Unique Physician Identification Number (UPIN). Details of the survey and the linkage method have been described elsewhere.11 Physicians were eligible for this study if they (1) reported their primary specialty as general internal medicine, geriatrics, general practice, or family practice in both 2000–2001 and 2004–2005; and (2) had in both 2000 and 2006 15 or more attributed Medicare beneficiaries who were eligible for a given preventive measure. Using established algorithms, the study attributed patients to the physician who billed for the plurality of their outpatient evaluation and management visits.
Beneficiary and Community Characteristics
Beneficiary characteristics were ascertained from Medicare files and included age as a continuous variable, sex, race/ethnicity (white, black, other; see Discussion section for a discussion of the reason for this categorization scheme), Medicaid dual-eligibility, and comorbidity based on the index described by Klabunde et al.12 Community variables were derived from U.S. Bureau of the Census data in the Area Resources File, and included median household income of residents aged 65 years and older in the beneficiary’s zip code (from the 2001 Census); percentage of adults aged 25 years and older in the beneficiary’s county who completed 12 or more years of schooling; and (in the model for delivery of screening mammography) the number of radiologists per 1,000 capita in the county. The four primary sociodemographic variables of interest were race, Medicaid eligibility, and local household income and educational attainment.
Physician and Practice Characteristics The same physicians responded to our survey in both rounds (although their patient panel may have changed from one round to the next). After determining that there was little difference between the 2000 and 2004 survey on the variables of interest, we characterized physicians by their self-report of the following characteristics in the earlier round of the survey (1) training, qualifications and number of years in practice; (2) practice setting and location; and (3) practice resources and incentives. Training and qualifications included physician self-reported primary specialty (general internal medicine or family practice/general practice); board certification in the primary specialty; and whether medical school education was completed in the United States and Canada, rather than in another country. Practice setting variables included practice type/size and location (urbanicity and census region). Practice resources and incentives included availability of electronic information systems to exchange clinical information, provide automated reminders for preventive services to clinicians, access treatment guidelines, or any combination of the three, as well as exposure to payment incentives for maintaining high patient satisfaction, meeting quality standards, or based on the results of profiling, or for any combination of the three. Also included was a measure of physicians’ agreement with the statement that standardized guidelines affect their practice.
Quality Measures of Preventive Service Delivery
We evaluated beneficiaries’ Medicare claims to determine eligibility for, and receipt of, eight recommended preventive services: diabetic monitoring (hemoglobin A1c testing, eye examinations, cholesterol testing and urine protein analysis), cancer screening (screening colonoscopy/sigmoidoscopy and mammography), and vaccinations (influenza and pneumococcal) during 2000 and again in 2006. These are all measures endorsed by the National Quality Forum or the Ambulatory Quality Alliance.13 Relevant claims codes and algorithms are included as Table 4 in the Appendix.
Statistical Analysis
The individual physician was the unit of analysis. We characterized each physician and his or her practice using data from the Physician Survey and calculated overall quality indicators (delivery of preventive services) to their attributed, eligible beneficiaries in 2000 and 2006. We calculated the rate at which individual physicians delivered each preventive service to eligible beneficiaries. We then grouped physicians into quartiles based on each sociodemographic element (community income, community level of education, patient panel Medicaid eligibility, and patient panel racial composition). We compared the performance of groups of physicians with different patient panel sociodemographic characteristics to one another, and between time periods. To test the statistical significance of the difference between different physician group quartiles on the delivery of recommended preventive services, we used the ANOVA test. This study was approved by the institutional review contractor for Mathematica Inc., the parent organization of the Center for Studying Health System Change.
Role of the Funding Source
This study was funded by the Robert Wood Johnson Foundation and the National Institutes of Health. Neither organization played any role in the design, conduct or reporting of this study.
RESULTS
Population Characteristics and Baseline Rates of Preventive Services Delivery
Table 1 describes the characteristics of physicians, practices and beneficiaries represented in the study population. Fewer than one in ten beneficiaries were black, and fewer than one in five were Medicaid-eligible. In both rounds of the survey most physicians worked in smaller practices; most were not exposed to performance incentives of any kind, and many did not have access to an electronic medical record. Table 2 shows the overall rates of receipt of each service in 2000 and 2006. Overall rates of delivery for most of the recommended preventive services increased between 2000 and 2006.
Table 1.
Provider and Patient Panel Characteristics
| Practice Characteristics (physician reported) | Percent of Physician Practices | |
|---|---|---|
| Practice location | Urban | 82 |
| Mixed | 8 | |
| Rural | 10 | |
| Practice type | Solo or 2-physician | 45 |
| 3-10 physicians | 20 | |
| 11-50 physicians | 6 | |
| >50 physicians | 3 | |
| Medical school | 3 | |
| Outpatient department/other | 21 | |
| Group/staff HMO | 2 | |
| Information technology | For reminders only | 6 |
| For exchanging clinical information only | 7 | |
| For treatment guidelines only | 22 | |
| For reminders AND clinical information | 2 | |
| For reminders AND treatment guidelines | 8 | |
| For clinical information AND treatment guidelines | 12 | |
| For all three functionalities | 10 | |
| Does not have/use IT | 32 | |
| Payment incentives | Based on patient satisfaction | 4 |
| Based on meeting quality standards | 2 | |
| Based on provider profiling | 1 | |
| Based on patient satisfaction AND quality standards | 6 | |
| Based on patient satisfaction AND provider profiling | 2 | |
| Based on quality standards AND provider profiling | 1 | |
| Based on all three | 3 | |
| Does not use payment incentives | 81 | |
| Community-level characteristics based on 2001 census (household income )and ARF (education), and practice demographics based on claims data (race, Medicaid eligibility) | ||
| Percent African American | 8 | |
| Percent Medicaid eligible | 18 | |
| Median household income | $48,361 | |
| Percent >25 years old with some education beyond high school | 81 | |
Table 2.
Delivery of Recommended Preventive Services in 2001 and 2006
| Eligible Physicians (15 or more eligible patients in both rounds) | Median patients per provider in Round 1 (IQR) | Median patient per provider in Round 2 (IQR) | Rate of delivery in Round 1 (%) | Rate of delivery in Round 2 (%) | Change in rate of preventive service delivery (95% CI) | |
|---|---|---|---|---|---|---|
| Hemoglobin A1c testing | 594 | 35 (29) | 46 (38) | 71.3 | 82.8 | +11.51 (10.81–12.20) |
| Cholesterol testing | 594 | 35 (29) | 46 (38) | 63.8 | 80.0 | +16.20 (15.47–16.94) |
| Eye examination | 594 | 35 (29) | 46(38) | 45.4 | 49.8 | +4.45 (3.64–5.27) |
| Urine protein testing | 594 | 35 (29) | 46 (38) | 10.8 | 25.0 | +14.12 (13.51–14.72) |
| Mammography | 697 | 39 (36) | 43(37) | 52.6 | 45.9 | –6.74 ((−7.49)–(−5.99)) |
| Colonoscopy/Sigmoidoscopy | 943 | 77 (86) | 90 (96) | 11.0 | 11.1 | 0.16 ((−0.14)–0.44) |
| Influenza Vaccine | 1008 | 95 (119) | 119(135) | 53.6 | 59.6 | +6.05 (5.67–6.42) |
| Pneumococcal Vaccine | 1008 | 95 (119) | 119 (135) | 8.1 | 8.2 | 0.07 ((−0.14)–0.28) |
Table 3.
Statistical Significance of the Variability in Performance of the Clinical Service Among Quartiles of Socioeconomic Status
| Income | Education | Race | Medicaid | |||||
|---|---|---|---|---|---|---|---|---|
| Round 1 | Round 2 | Round 1 | Round 2 | Round 1 | Round 2 | Round 1 | Round 2 | |
| A1c | 9.56* | 7.12* | 1.01 | 0.17 | 4.26* | 3.19 | 6.05* | 4.27* |
| Cholesterol | 0.9 | 0.52 | 1.12 | 0.84 | 0.21 | 1.26 | 2.7 | 2.09 |
| Eye examination | 2.73 | 1.68 | 6.61* | 6.71* | 3.5 | 4.91 | 10.62* | 10.95* |
| Urine Protein Testing | 3.48 | 1.17 | 4.95 | 5.84* | 4.31* | 3.02 | 4.45* | 3.71 |
| Mammography | 12.1* | 5.6* | 8.13* | 2.78 | 2.72 | 0.87 | 27.72* | 5.58* |
| Colonoscopy | 4.45* | 0.99 | 3.28 | 1.05 | 1.27 | 0.94 | 12.27* | 10.13* |
| Influenza Vaccine | 36.19* | 25.66* | 25.73* | 22.16* | 16.44* | 15.65* | 59.86* | 36.88* |
| Pneumococcal Vaccine | 8.36* | 0.28 | 2.82 | 2.91 | 3.31 | 0.28 | 6.75* | 0.93 |
*Values shown are the F test values for ANOVA tests comparing the performance of groups ofphysicians with different patient panel characteristics on the provision of recommendedpreventive measures at 2 different time points. Starred values represent F test values that aresignificant at p <0.01, indicating that a statistically significant difference was found. Forexample, physicians with higher- and lower-income patient panels performed significantlydifferently in their provision of influenza vaccine in both rounds; in the provision ofpneumococcal vaccine, however, significant differences were seen in the first round but not thesecond. In the provision of eye examinations to diabetics, no statistically significant differenceswere seen at either time point.
Relation Between Sociodemographic Factors and Delivery of Preventive Services
In 2000 we found a relationship between sociodemographic characteristics of physicians’ patient panels and preventive services delivery. For example, there appears to be a clear relationship between the community level of education and the percentage of that physician’s patients who received the influenza vaccine (Fig. 1).
Some of these relations were statistically significant, including that between Medicaid eligibility and all of the preventive measures other than cholesterol screening (Table 3). In 2006, there were fewer apparent or statistically significant relationships between patient panel make-up and rates of delivery for any of the services.
Table 3 shows how delivery of preventive services was associated with each sociodemographic factor. We observed variation for each preventive service. These variations were present with some sociodemographic characteristics but not others. In general, fewer associations were seen in 2006 than in 2000. Eleven associations seen in 2000 were seen again in 2006, although their magnitude changed. Seven associations seen in 2000 were no longer significant in 2006, and one appeared only in 2006.
Among the patient panel characteristics we studied, the percentage of Medicaid eligible patients was the characteristic most frequently associated with the quality indicators including seven of the eight preventive services in Round 1, and five of the eight services in Round 2. Local median income was associated with five of eight quality indicators in Round 1, and three of eight in Round 2. The racial composition of a physician's panel was associated with the delivery of three preventive services (A1c measurement, influenza vaccine and urine protein testing) in the first round, and only one (influenza vaccine) in the second.
Among individual preventive service measures, delivery of influenza vaccine was associated with all four sociodemographic characteristics in both rounds. Measurement of hemoglobin A1c and mammography were associated with three out of four characteristics in Round 1, and two out of four in Round 1. At the other end of the spectrum, delivery of pneumococcal vaccine was associated with two sociodemographic factors in the first round, and none in the second.
Overall, associations between sociodemographic factors and the delivery of preventive services did not appear to follow predictable patterns either at a single point in time or between time periods. With the exception of influenza vaccination, no preventive service was associated with every sociodemographic variable, and no sociodemographic variable was associated with every preventive service. While the majority of associations seen in the first round were present in the second round, a substantial number (seven out of 18) were no longer present. If the delivery of influenza vaccine, which appears to show an unusually strong association with sociodemographic factors, were removed from the analysis, more associations would be present in only one of the two time periods (7) than in both of them (6).
Discussion
Pay-for-performance models could widen disparities in the quality of care if they systematically penalize physicians who care for disadvantaged populations.14 Adjustment for the sociodemographic characteristics of a physician's patients could ameliorate this concern, but may have the unintended consequence of rewarding substandard care if sociodemographic factors are not consistently associated with physician performance.15 We examined rates of delivery of preventive services using common quality metrics for a large population of primary care physicians and found that associations between patient sociodemographics and performance were both inconsistent across different measures and unstable between time periods.
Specifically, of the four sociodemographic characteristics we evaluated, two (patient residential area-level household income and panel Medicaid eligibility) were more likely to be significantly associated with provider performance, but even these associations did not appear consistent across measures or between time periods. Patient-panel Medicaid eligibility is associated in our sample with the most disparities in care, and these disparities were most likely to persist. The racial make-up of a physician’s panel was associated with only two of eight preventive care measures in Round 1, and one in Round 2. A general pattern appeared to be present, with many of the associations seen in the first round of measurement no longer present in the second round of measurement. Our results mirror those of other research demonstrating inconsistent associations between sociodemographics and patient ratings of care.
Influenza vaccine is a notable exception to our findings. Unlike the other preventive measures examined, the delivery of influenza vaccine was associated with significant disparities in care across all sociodemographic measures and in both study periods. This is particularly remarkable given that, unlike some of the other preventive measures we studied, influenza vaccine is indicated for all Medicare beneficiaries. Previous studies have identified potential sources of disparities in the delivery of influenza vaccine, including access to care, patient preferences or concerns about vaccines, and patient initiation of a visit specifically for vaccination.16 Interestingly, delivery of pneumococcal vaccine, which is also indicated for all Medicare beneficiaries and presumably is influenced by similar barriers, was associated with only two associations in the first study period and none in the second study period, although the overall rate of service delivery was much lower. This further illustrates the challenge of predicting the relationship between sociodemographic factors and quality of care.
Among sociodemographic factors, the proportion of a provider’s patient panel that is Medicaid-eligible was most consistently associated with disparities in the provision of recommended preventive services. This may reflect that Medicaid-eligible patients have been found to have lower quality of care in other studies; they are also more likely to report poor health, which may increase the number of problems providers must address at each appointment and make it less likely that routine preventive services can be administered.17,18 However, it may also be related to some other aspect of the way Medicaid services are administered or reimbursed. In anticipation of possible expansions of Medicaid programs nationwide, the delivery of preventive care to Medicaid recipients may merit further study.
A number of providers in our sample were exposed to a variety of payment incentives for performance during the study period. Some of these incentives were linked to physician behaviors that would likely have influenced our results (for example, incentives for meeting quality targets) while others reflected physician behaviors that would be less likely to do so (for example, incentives for maintaining high levels of patient satisfaction). Adjusting for exposure to these incentives did not significantly affect the presence or absence of associations between providers’ patient panel sociodemographics and their delivery of recommended preventive measures. It is still possible that the providers who are currently unexposed to incentives would, in fact, change their behavior significantly under a Medicare pay for performance program in ways related to their patients’ sociodemographic status. However, studies in the United Kingdom evaluating the impact of national pay-for-performance programs have shown a limited or inconsistent effect on disparities.19,20
Limitations
Our results should be interpreted within the context of our study’s limitations. We considered only Medicare beneficiaries, whose health disparities may be attenuated compared with other age groups since they are all eligible for some level of health insurance coverage. We considered only measures of preventive care; sociodemographic disparities in the delivery of more resource-intensive services, such as recommended diagnostic testing or treatment may exhibit more consistency and stability. Although our analytic sample was drawn from a nationally representative survey respondent pool, only physicians who treated the required minimum number of eligible patients and participated in both rounds of the CTS survey were examined. Thus, our results may not generalize to the broader population of physicians. An optimal analysis of health disparities related to race and ethnicity would include multiple categories for race and ethnicity, reflecting the true diversity of the US population. Unfortunately, the ways in which race and ethnicity have historically been collected and categorized for Medicare claims data have led to researcher concerns that these data are not accurate for categories other than white and black.21 An analysis comparing race and ethnicity assignment in 1998–2001 Medicare Current Beneficiary Survey data with beneficiary self-report showed that Current Beneficiary Survey assignments were 96.5% sensitive for identifying White respondents and 95.6% sensitive for identifying Black respondents. However, sensitivities fell off rapidly for respondents identified as members of other racial and ethnic groups (54% for respondents identified as Asian and 35.7% for respondents identified as Hispanic, for example).22 Because of concerns that claims data would not accurately capture other categories, race and ethnicity are combined in our analysis and categorized as White, Black and Other. Some markers of patient sociodemographic status were drawn from outside sources such as the US Census and measured at the level of the area rather than the individual. However, previous research suggests that area-level sociodemographic variables are valid predictors of individual health status.23,24 Some services, such as influenza vaccination, may be delivered outside of physicians’ offices (e.g., by free vaccination vans), which may bias our results toward stronger associations between sociodemographics and service delivery as disadvantaged populations may be more reliant on these alternative sites of care. Lastly, a minority (19%) of the physicians in our sample were exposed to performance incentives during our initial study period, which makes it difficult to determine what would have happened in the absence of such incentives. However, we adjusted for exposure to incentives, and our findings were robust when we repeated our analyses excluding these physicians (data not shown).
We chose not to adjust for patients’ underlying health status, except to ensure that delivery of preventive services was measured only for the appropriate patients. For example, in measuring providers’ measurement of Hemoglobin A1c, we only considered patients who were known to have diabetes, but did not distinguish among diabetics who do and do not have comorbidities such as hypertension. While adjusting for patients’ comorbid illness is standard in many studies, we did not feel it was relevant to our research questions since none of these comorbidities would affect providers’ obligation to perform recommended services.
Despite these limitations, our study provides important insights into the potentially complex interplay between performance-based incentive programs and health disparities.
Our study raises concerns about the strategy of adjusting performance based on patient panel sociodemographics to mitigate the potential risk that pay-for-performance would worsen disparities. This could occur if adjustment for these factors had the unintended consequence of legitimizing differences in quality of care that many low-performing physicians can (and should) change, and thus lowering the average quality of care received by poor and minority patients. Unnecessary adjustment could let those who care for underserved populations perform at a lower level and still receive the same performance bonuses as other physicians who treat less disadvantaged patients but have higher levels of performance before adjustment. Our study also highlights the complexity of specifying an adjustment model. In our data, adjusters selected based on year 2000 data would not be relevant a few years later as the predictors of performance and the measures they are associated with shifted considerably.
Given the inconsistency of the relationships between patient panel sociodemographics and the quality of care delivered by individual physicians, adjusting performance scores for patient panel sociodemographics may not be routinely useful in a Medicare pay-for-performance program.
Acknowledgements
This study was funded by the National Institutes of Health and the Robert Wood Johnson Foundation.
Disclaimer This paper is based on work conducted before Dr. Pham joined the Center for Medicare & Medicaid Services (CMS), and does not reflect the policies or programs of CMS or of the Department of Health and Human Services.
Conflict of Interest None disclosed.
Appendix
Table 4.
| Preventive service | Eligibility criteria |
|---|---|
| Hemoglobin A1C CPT Code: 83036, 82985 2). Eye exam CPT Code: 92002 – 92014, 92225, 92250 ICD-9-CM Code: 95.02, 95.03, 95.11, V72.0 and V80.2 | Medicare Beneficiaries 65 years and older diagnosed with diabetes by ICD-9-CM Code 250–250.93. |
| Colonoscopy - Screening only CPT Code: 45355, 45378, G0105 ICD-9-CM Code: 45.22, 45.23, 45.42, 45.43 - Other CPT Code: 45379, 45380, 45382 – 45385 ICD-9-CM Code: 45.25, 45.41 2). Sigmoidoscopy - Screening only CPT Code: 45330, G0104 ICD-9-CM Code: 45.24, 48.22, 48.23, 48.36 - Other CPT Code: 45331 – 45334, 45337 – 45339 ICD-9-CM Code: 48.24, 48.26, 48.35 | 65 to 79 years old Exclude those with cancer diagnoses ICD-9-CM or V codes: 153–153.9, 154–154.8, V10.05, V10.06 |
| Screening mammography CPT Code: 76090 – 76092 ICD-9-CM Code: 87.37 | Women 65 to 74 years old Exclude those with cancer diagnoses ICD-9-CM or V codes: 174, 174.0 thru 174.6, 174.8, 174.9, V10.3 |
| Influenza vaccination CPT Code: 90658, G0008 ICD-9-CM Code: V04.8 | 65 and older |
| Pneumococcal vaccination CPT Code: 90732, G0009 ICD-9-CM Code: V03.82 | 65 and older |
| Prostate cancer screening CPT Code: G0107, 86316, 84153 | Male 65 and older exclude those with cancer diagnosis code: 185 |
| Cholesterol screening CPT Code: 80061, 83715, 83716, 83721, 82465, 83718, 84478, V81.0, V81.1, V81.2 | For diabetics only |
| Urine microalbumin screening CPT Code: 82042, 82043, 82044, or (84155, 84160, 84165, in combination with 81050). | For diabetics only |
References
- 1.Casalino L, Elster A. Will pay for performance and quality reporting Affect health care disparities? Health Aff. 2007;26:W405–W414. doi: 10.1377/hlthaff.26.3.w405. [DOI] [PubMed] [Google Scholar]
- 2.Smedley, B Stith Y and Nelson R, eds. Unequal treatment: confronting racial and ethnic disparities in health care. Washington DC: The National Academies Press; 2003 [PubMed]
- 3.Schneider EC, Zaslavsky A, Epstein A. Racial disparities in the quality of care for enrollees in Medicare managed care. JAMA. 2002;287:1288–1294. doi: 10.1001/jama.287.10.1288. [DOI] [PubMed] [Google Scholar]
- 4.Warner R. Does pay for performance steal from the poor and give to the rich? Ann Intern Med. 2010;153:340–341. doi: 10.7326/0003-4819-153-5-201009070-00010. [DOI] [PubMed] [Google Scholar]
- 5.Jha A, Orav E, Epstein A. The effect of financial incentives on hospitals that serve poor patients. Ann Intern Med. 2010;153:299–306. doi: 10.7326/0003-4819-153-5-201009070-00004. [DOI] [PubMed] [Google Scholar]
- 6.Bach P, Pham HH, Schrag D, Tate R, Hargraves JL. Primary care physicians who treat blacks and whites. New Engl J Med. 2004;351:575–584. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- 7.Hong C, Atlas S, Chang Y, Subramanian S, Ashburner J, Barry M, et al. Relationship between patient panel providers and primary care physician clinical performance rankings. JAMA. 2010;304:1107–1113. doi: 10.1001/jama.2010.1287. [DOI] [PubMed] [Google Scholar]
- 8.Trivedi A, Zaslavsky A, Schneider E, Ayanian J. Trends in the quality of care and racial disparities in managed care. New Engl J Med. 2005;353:692–700. doi: 10.1056/NEJMsa051207. [DOI] [PubMed] [Google Scholar]
- 9.Franks P, Fiscella K, Meldrum S. Racial disparities in the content of primary care visits. J Gen Intern Med. 2005;20:599–603. doi: 10.1007/s11606-005-0106-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gornick M. A decade of research on disparities in Medicare utilization: lessons for the health and health care of vulnerable men. Am J Public Health. 2008;98(Supp 1):753–759. doi: 10.2105/ajph.93.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pham HH, Schrag D, Hargraves JL, Bach PB. Delivery of preventive services to older adults by primary care physicians. JAMA. 2005;294:473–481. doi: 10.1001/jama.294.4.473. [DOI] [PubMed] [Google Scholar]
- 12.Kalbunde C, Potosky A, Legler J, Warren L. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53:1258–1267. doi: 10.1016/S0895-4356(00)00256-0. [DOI] [PubMed] [Google Scholar]
- 13.AQA Approved Quality Measures.http://www.aqaalliance.org/performancewg.htm, and NQF Endorsed Standards. http://qualityforum.org/Measures_List.aspx. Both viewed April 21, 2011.
- 14.Friedberg M, Safran D, Coltin K, Dresser M, Schneider E. Paying for performance in primary care: potential impact of practices and disparities. Health Aff. 2010;29(5):1–7. doi: 10.1377/hlthaff.2009.0985. [DOI] [PubMed] [Google Scholar]
- 15.Rosenthal M, Dudley R. Pay-for-performance: will the latest payment trend improve care? JAMA. 2007;297:740–744. doi: 10.1001/jama.297.7.740. [DOI] [PubMed] [Google Scholar]
- 16.Fiscella K. Commentary—anatomy of racial disparity in influenza vaccination. HSR: Health Services Research. 2005;40:539–550. doi: 10.1111/j.1475-6773.2005.0w372.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang J, Huang E, Drum M, Kirchhof A, Schlichting J, Schaefer C, et al. Insurance status and quality of diabetes care in community health centers. Am J Public Health. 2008;99:742–747. doi: 10.2105/AJPH.2007.125534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Broyles R, McAuley W, Baird-Holmes D. The medically vulnerable: their health risks, health status, and use of physician care. Journal of Health Care for the Poor and Underserved. 1999;10:186–200. doi: 10.1353/hpu.2010.0498. [DOI] [PubMed] [Google Scholar]
- 19.Millet C, Gray J, Wall M and Majeed A. Ethnic disparities in coronary heart disease management and pay for performance in the UK. J Gen Intern Med 24 (1): 8–13. [DOI] [PMC free article] [PubMed]
- 20.Millet C, Gray J, Saxena S, Netuveli G, Khunti K and Majeed A. Ethnic disparities and diabetes management and pay-for-performance in the UK: The Wandsworth Prospective Diabetes Study. PLoS Med 4(6): e191 [DOI] [PMC free article] [PubMed]
- 21.Lauderdale DS, Goldberg J. The expanded racial and ethnic codes in the Medicare data files: their completeness of coverage and accuracy. Am J Publ Health. 1996;86:712–716. doi: 10.2105/AJPH.86.5.712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Waldo DR. Accuracy and bias of race/ethnicity codes in the Medicare enrollment database. Health Care Financing Review Winter 2004–2005; 26: 61–71 [PMC free article] [PubMed]
- 23.Subramanian SV, Chen JT, Rekhopf DH, et al. Comparing individual- and area-based socioeconomic measures for the surveillance of health disparities: a multilevel analysis of Massachusetts births, 1989–1991. Am J Epidemiol. 2006;164:823–834. doi: 10.1093/aje/kwj313. [DOI] [PubMed] [Google Scholar]
- 24.Krieger N, Chen JT, Waterman PD, et al. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter? The Public Health Disparities Geocoding Project. Am J Epidemiol. 2002;156:471–482. doi: 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]