Abstract
Study Objectives:
Short sleep duration (SSD) is common among deployed soldiers. The prevalence of SSD during redeployment, however, is unknown.
Design:
Cross-sectional study of a brigade combat team (n = 3152 US Army soldiers) surveyed 90–180 days after completing a 6–15 month deployment to Iraq as part of Operation Iraqi Freedom (OIF). Survey items targeted sleep habits and comorbid medical conditions. Multivariate logistic regression analyses were performed to calculate adjusted odds ratios of medical comorbidities associated with SSD.
Setting:
US Army Infantry Post.
Subjects:
All soldiers from a redeploying brigade combat team participated in a health assessment between 90 and 180 days upon return to Ft. Lewis from Iraq.
Interventions:
None.
Measurements and Results:
A total of 2738 (86.9%) soldiers answered questions regarding self-perceived sleep and were included in the analysis. Mean sleep duration was 5.8 ± 1.2 hours. Nineteen hundred fifty-nine (72%) slept ≤ 6 h, but only 16% reported a daytime nap or felt their job performance was affected due to lack of sleep. Short sleep was more common among soldiers who reported combat exposure. After controlling for combat exposure, short sleep duration (SSD) was associated with symptoms of depression, posttraumatic stress disorder, panic syndrome, and with high-risk health behaviors such as abuse of tobacco and alcohol products, and suicide attempts.
Conclusions:
SSD is common among redeployed soldiers. Soldiers who experienced combat are at increased risk for persistent SSD and comorbidities associated with SSD. Efforts to reestablish good sleep habits and aggressive evaluation of soldiers with persistent SSD following deployment may aid in the prevention and management of associated medical conditions.
Citation:
Luxton DD; Greenburg D; Ryan J; Niven A; Wheeler G; Mysliwiec V. Prevalence and impact of short sleep duration in redeployed OIF soldiers. SLEEP 2011;34(9):1189-1195.
Keywords: Short sleep duration (SSD), sleep quality, health, military, deployment, combat exposure
INTRODUCTION
Insufficient sleep, caused by short sleep duration (SSD), has been linked to a number of deleterious outcomes including impaired cognition, cardiovascular disease, and poor overall health.1–3 The Whitehall II Study,3 for example, indicated that obtaining < 7 h of sleep on a regular basis increases all-cause mortality from increases in cardiovascular deaths. Moreover, other epidemiologic studies have shown a link between sleep duration and diabetes risk,4 as well as body mass index and obesity.5 Although the putative mechanisms that link SSD to negative health outcomes are complex, it is clear that chronic inadequate sleep increases risk for a variety of health problems.
There are few published studies detailing sleep disturbances associated with war or traumatic events.6 A survey of 156 deployed US Air Force airmen living in austere conditions reported an average sleep duration of 6.5 h, with a sleep efficiency of 83%.7 Another large survey of deployed US Army soldiers reported an average duration of sleep of only 5.6 hours.8 The Millennium Cohort Study, a large survey of US military personnel, of whom 22% deployed, reported an average sleep duration of 6.5 h in non-deployed, currently deployed, and recently redeployed US service members.9 These studies demonstrate the association of SSD with deployment. No study to date has assessed post-deployment sleep duration and comorbid illnesses in a redeployed combat arms unit in which most soldiers have experienced combat exposure.
Given the high operational tempo since the start of the Global War on Terror in 2001, many service members have deployed to active theaters of operation multiple times. Poor sleep practices are common in theater and likely persist between deployments. This possibility may contribute to physical and occupational impairment, including chronic pain, fatigue, malaise, concentration or memory impairments, and accidents at work or while driving.10–12 The excess contribution of SSD to these impairments may negatively impact the time and resources spent to determine the etiology of these ailments. Service members returning from war may have persistence of learned poor sleep practices, circadian misalignment, and comorbid illnesses from their combat experiences that make adopting a normal sleep pattern upon return home difficult. Persistent SSD can potentially cause subtle cognitive and motor impairments even in otherwise high-functioning service members.
A number of studies have examined the association between sleep disturbances and posttraumatic stress disorder (PTSD).13 However, there may be a large population of service members with chronic insomnia or sleep deprivation experiencing functional impairments in daily living who do not meet the criteria for a psychiatric diagnosis. To our knowledge, there are no published studies evaluating sleep deprivation and insomnia in service members returning from war.
The aims of this study were to determine if combat exposure predicted short sleep duration after redeployment, identify the prevalence of SSD in redeployed soldiers, and examine the associations between SSD, medical comorbidities, and health risk factors. To accomplish these aims, we examined retrospective data from a single redeployed brigade combat team who completed deployments in support of Operation Iraqi Freedom (OIF) in 2007. This study used existing data and was approved by the Madigan Army Medical Center Department of Clinical Investigation. This research protocol was deemed to be exempt from informed consent.
METHODS
Overview
Data for this cross-sectional study was initially collected as part of the Health Risk Assessment II (HRAII) project initiated by the Department of Defense (DoD) to systematically screen all service members redeploying from combat environments for medical, spiritual, social, and emotional needs, as well as access to services to fulfill these needs.14 Service members complete the HRAII between 90 and 180 days after leaving the combat environment. The HRAII consists of 2 phases: a detailed computerized survey and in-person interviews with medical and behavioral health providers immediately afterward. Responses from the survey are used to facilitate these interviews.
The purpose of this project was to assess returning service member's sleep habits to include duration of sleep and symptoms of insufficient sleep. These items were incorporated into the computerized survey portion of the HRAII: How many hours of sleep do you get per night? 4 or less, 5 hours, 6 hours, 7 hours, 8 hours, 9 or more; and Does lack of sleep cause you to nap during the day or affect your job performance? Yes or no. Recently redeployed service members who answered both of these questions comprised the study population. Our institutional review board approved temporary modification of the HRAII at our local site to facilitate capturing data from a brigade combat team redeploying to Ft. Lewis, WA, which had been deployed in support of OIF during 2006 and 2007.
Instruments
Major depressive disorder
The HRAII incorporates many previously validated screening instruments to facilitate identification of mental health conditions. The Patient Health Questionnaire-9 (PHQ-9)15 was used to screen for major depression. The PHQ-9 is the Depression Scale of the Patient Health Questionnaire and consists of 9 items targeting the Diagnostic and Statistical Manual-IV (DSM-IV) diagnostic criteria for major depressive disorder. Items are rated on a 4-point scale (0 = Not at all; 1 = Several days; 2 = More than half the day; 3 = Nearly every day) and scores range from 0 to 27. Scores > 10 are indicative of moderate or greater depression severity with a sensitivity of 92% and specificity of 80% for major depressive disorder.16,17
PTSD
The Primary Care PTSD Screen (PC-PTSD)18 was used to screen for posttraumatic stress disorder (PTSD). The PC-PTSD is a 4-item (Yes/No) self-report screening instrument for PTSD that has sound psychometric properties for cutoff scores of 2 (sensitivity = 0.91, specificity = 0.72) and 3 (sensitivity = 0.78, specificity = 0.87) compared to diagnoses based on the Clinician Administered Scale for PTSD.19,20 Recent research also reported that the PC-PTSD demonstrated high diagnostic efficacy when compared against a standardized structured clinical interview in a population of combat deployed service members.21 Similar findings have been reported in other studies.22
Panic disorder
Five items from the Primary Care Evaluation of Mental Disorders (PRIME-MD)23 were used to screen for panic disorder. This brief, self-administered instrument has been shown to have a sensitivity of 81% and specificity of 99% for identifying panic disorder.24
Mild traumatic brain injury (mTBI)
The HRAII contains 10 items to screen for potential exposures to and consequences from blasts. For the purposes of this project, soldiers were defined as having mTBI if they answered affirmatively to at least one of the screening questions for an exposure and symptoms after the event. Items that evaluated for potential exposures include: While deployed, were you exposed to or near a blast, IED explosion, car bomb, suicide explosion, or exposed to any other event that caused a blow or jolt to your head? and While deployed, were you involved in a motor vehicle accident, a fall, a sports accident, or any other event that caused a blow to your head or that resulted in a neck whiplash? Post-exposure symptoms were assessed for with the following 3 questions: As a result of the event, were you unconscious for more than one minute? As a result of the event, were you dazed, “saw stars,” “bell rung,” or “lights knocked out,”? and At any time since the event have you had a seizure or convulsion?
Obesity
Soldiers were defined as obese if their body mass index (kg/m2) exceeded 30.
Health risk behaviors
Three high-risk health behaviors are screened for on the HRAII: alcohol abuse, tobacco abuse, and risk for suicide attempt. Three items from the HRAII were used to assess for alcohol abuse. Service members recorded the frequency with which they used alcohol over the past year (never drink, monthly or less, 2–4 times a month, 2–3 times a week, ≥ 4 times as week), number of drinks consumed in a typical setting (never drink, 1 or 2, 3 or 4, 5 or 6, 7, 8, 9, or ≥ 10), and if they used alcohol more than intended during the prior month. Alcohol abuse was defined as consumption of > 5 beverages on a typical setting or drinking more than intended on any occasion. Tobacco use was assessed through the item, Have you used tobacco in the past 6 months? Risk for future suicide attempts was assessed for using 2 items: (1) Do you feel like hurting yourself at this time? and (2) Have you ever attempted to kill yourself?
Combat exposure assessment
Four yes/no items were used to screen for combat exposures during the most recent deployment. Items asked the following: (1) During combat operations did you become wounded or injured? (2) During combat operations did you personally witness anyone being killed? (3) During combat operations did you see the bodies of dead Soldiers or civilians? (4) During combat operations did you kill others in combat? (or have reason to believe others were killed as a result of your actions?). Cumulative combat exposures were measured using the sum of these 4 screening items; thus scores can range from 0 to 4. Soldiers were categorized as having had combat exposure if they answered affirmatively to any of these questions.
Sleep characteristics
Sleep measures consisted of 2 items. The first question assessed sleep duration: How many hours of sleep do you get per night? 4 or less, 5, 6, 7, 8, 9 or more. Soldiers were defined as having short sleep duration (SSD) or very short sleep duration (VSSD) if they reported sleeping < 7 h or < 6 h, respectively. Insufficient sleep was defined as sleep duration < 7 h combined with an affirmative answer to the following question: Does lack of sleep cause you to nap during the day or affect your job performance? Yes or No.
Statistical Analyses
Data analysis was performed using Stata version 9.2.25 All statistical tests were 2-tailed, and significance set at P < 0.05. Potential differences in continuous and categorical variables were assessed using independent-samples t-tests and χ2 analysis, respectively. The medical comorbidities PTSD, depression, mTBI, obesity, and panic syndrome and the high-risk health behaviors abuse of tobacco, abuse of alcohol, and risk for suicide were selected a priori as outcome variables. Variables selected for inclusion in adjusted logistic regression model building included sleep duration (VSSD, SSD, normal), symptoms of insufficient sleep, age, sex, rank (enlisted, noncommissioned officer, commissioned or warrant officer), combat exposures, and number of deployments (1, 2, 3, ≥ 4) (see Reger et al.26 for similar modeling approach). The effect of including an interaction term between sleep duration (< 7 vs. ≥ 7 h nightly) and symptoms of insufficient sleep on fit of the model to the data was assessed using the likelihood-ratio test. We tested for potential colinearity (Pearson and Spearman correlation coefficients as appropriate) and avoided simultaneously modeling variables with correlation coefficients > 0.6. Model fit was assessed using the Hosmer-Lemeshow test.27 Variables included in final models were determined using the Goodness of Fit test from Hosmer and Lemeshow.
RESULTS
Of the 3152 respondents who took the survey, 89% (n = 2717) answered both items regarding sleep. Seventy-two percent were males in their 20s; ages ranged from 18 to 54 (mean 25.5; SD 5.6). The majority (93%) were enlisted soldiers, with the remaining 7% comprising commissioned and warrant officers. These demographic patterns are typical of combat arms units in the Army. Although all respondents in this study recently redeployed from Iraq, over half (55%) of the population had completed their second, third, or fourth deployment in support of the Global War on Terror (GWOT). The mean length of their most recent deployment was 398 days. Twenty-three percent (n = 628) of soldiers reported being wounded, injured, assaulted, or otherwise hurt during the deployment. Of those with injuries, 67% (n = 419) reported still being affected by the injuries sustained during combat operations at the time of the HRAII survey. Just over half (51%) of the soldiers in this study met criteria for one or more medical comorbidities.
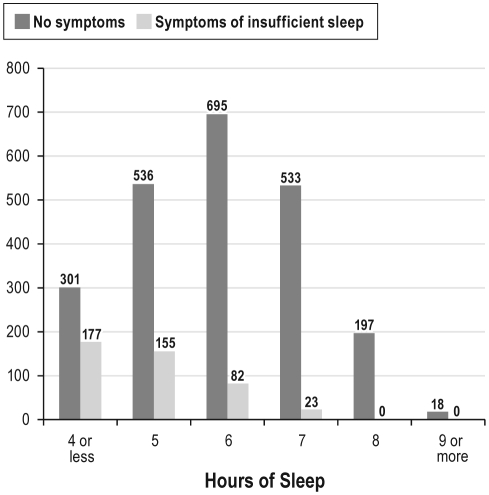
The breakdown of soldiers with and without symptoms of insufficient sleep based on hours of sleep are shown in Figure 1, and detailed characteristics of all respondents by sleep durations are presented in Table 1. Mean sleep duration was 5.8 ± 1.2 hours. Most (72%) soldiers reported short (43%) or very short (29%) sleep duration. Symptoms of insufficient sleep, as defined by the need to nap during the day or an influence on job performance, were reported by 16% (n = 444) of soldiers and were much more common among those with SSD (OR 2.9; 95% CI 1.9-4.5) or VSSD (OR 9.8; 95% CI 6.5–14.7) compared to those with normal sleep durations. Most soldiers (77%; n = 2,111) reported at least one combat exposure. Soldiers reporting combat exposures were much less likely to sleep > 6 h nightly (OR 0.44; 95% CI 0.38–0.54). The combat exposure with the strongest association with SSD and VSSD was being wounded or injured during combat operations. No difference in sleep duration was observed between sexes, ages, weights, or BMIs. Commissioned and warrant officers were more likely to have a normal sleep duration than either enlisted soldiers or noncommissioned officers (OR 1.5; 95% CI 1.2–2.2).
Figure 1.
Number of soldiers based on hours of sleep and presence of symptoms of insufficient sleep.
Table 1.
Characteristics of study population
| All subjects (n = 2717) | Very short sleepa (n = 1169) | Short sleepb (n = 777) | ≥ 7 hours of sleep (n = 771) | P-valuec | |
|---|---|---|---|---|---|
| Mean age (SD) | 25.6 (5.7) | 27.2 (5.9) | 27.0 (5.6) | 27.2 (5.5) | 0.14 |
| Sex | 0.08 | ||||
| Male | 2617 (96%) | 97% | 96% | 96% | |
| Female | 34 (4%) | 3% | 4% | 4% | |
| Average weight in pounds (SD) | 183 (36) | 185 (38) | 180 (35) | 182 (35) | 0.03 |
| Average BMI in kg/m2 (SD) | 26.3 (4.8) | 26.5 (5.0) | 26.1 (4.8) | 26.2 (4.4) | 0.10 |
| Rank | < 0.001 | ||||
| Junior enlisted | 1333 (49%) | 45% | 27% | 28% | |
| Noncommissioned officers | 1185 (44%) | 43% | 29% | 27% | |
| Warrant and commissioned officers | 198 (7%) | 27% | 35% | 38% | |
| Symptoms of insufficient sleep | 444 (16%) | 75% | 18% | 7% | < 0.001 |
| Any combat exposure | 2111 (78%) | 48% | 28% | 24% | < 0.001 |
| Killed | 1131 (42%) | 51% | 27% | 22% | < 0.001 |
| Wounded | 419 (15%) | 59% | 21% | 20% | < 0.001 |
| Saw killing | 1451 (53%) | 50% | 26% | 24% | < 0.001 |
| Saw dead bodies | 2054 (76%) | 48% | 28% | 24% | < 0.001 |
| Mean number of combat exposures (SD) | 0.78 (41%) | 0.86 (0.34) | 0.76 (0.43) | 0.68 (0.47) | < 0.001 |
| Mean number of GWOT deployments (SD) | 1.74 (0.90) | 1.80 (0.98) | 1.70 (0.84) | 1.69 (0.83) | 0.01 |
| Any medical comorbidity | 1387 (51%) | 55% | 25% | 19% | < 0.001 |
| PTSD | 422 (16%) | 75% | 17% | 8% | < 0.001 |
| Mild TBI | 940 (35%) | 57% | 24% | 19% | < 0.001 |
| Depression | 94 (4%) | 84% | 13% | 3% | < 0.001 |
| Panic syndrome | 86 (3%) | 73% | 20% | 7% | < 0.001 |
| Obesity | 471 (17%) | 50% | 28% | 23% | < 0.001 |
| Any high-risk health behaviors | 1790 (65%) | 48% | 27% | 24% | |
| Tobacco use | 1600 (59%) | 48% | 28% | 25% | < 0.001 |
| Alcohol use | 739 (27%) | 55% | 24% | 21% | < 0.001 |
| Suicide attempt | 70 (3%) | 70% | 20% | 10% | < 0.001 |
| None | 931 (34%) | 34% | 32% | 34% | < 0.001 |
Self reported < 6 h sleep duration.
Self reported < 7 h sleep duration.
Student's T-test was used for weight and BMI; Chi-square analysis was used for all other categorical variables.
The prevalence of medical comorbidities and high-risk behaviors varied by sleep duration group. Adjusted odds ratios (AOR) for prevalent medical comorbidities and high-risk behaviors are presented in Tables 2 and 3. Soldiers with VSSD were at increased risk for all conditions relative to those with either short or normal sleep duration. Symptoms of insufficient sleep independently predicted PTSD, depression, mTBI, panic syndrome, and suicide risk. Duration of most recent deployment, cumulative number of GWOT deployments, and the interaction term between sleep duration (< 7 vs. ≥ 7 h/night) and symptoms of insufficient sleep did not predict any of the outcomes of interest and were excluded from the final multivariable models.
Table 2.
Adjusted odds ratios and 95% confidence intervals measuring associations between predictor variables and medical conditions
| PTSD | Depression | Mild TBI | Panic syndrome | Obesity | |
|---|---|---|---|---|---|
| Very short sleep duration (< 6 h nightly) | 4.7 (3.2-6.9) | 11.4 (3.5-36.9) | 1.8 (1.4-2.3) | 3.9 (1.6-9.4) | 3.3 (1.3-8.9) |
| Short sleep duration (6 h nightly) | 1.9 (1.2-2.8) | 3.5 (1.0-12.6) | 1.2 (0.9-1.5) | 2.5 (1.0-6.4) | 2.1 (0.7-6.2) |
| Symptoms of insufficient sleep | 2.5 (2.0-3.3) | 3.4 (2.2-5.2) | 2.0 (1.5-2.6) | 3.0 (1.9-4.9) | 0.9 (0.4-1.9) |
| Age | 1.01 (0.99-1.04) | 1.02 (0.97-1.06) | 0.98 (0.97-1.00) | 1.01 (0.96-1.06) | 1.10 (1.05-1.20) |
| Female | 2.9 (1.6-5.4) | 2.0 (0.7-5.3) | 0.9 (0.5-1.7) | 1.9 (0.6-5.6) | 3.2 (1.0-9.7) |
| Junior enlisted (E1-E4)* | 1.6 (1.2-2.1) | 1.7 (1.0-2.8) | 0.9 (0.7-1.2) | 1.6 (0.9-2.7) | 3.4 (1.2-7.5) |
| Commissioned or warrant officers* | 0.9 (0.5-1.6) | 0.3 (0.03-1.9) | 0.5 (0.3-0.8) | 0.2 (0.03-1.8) | 0.8 (0.1-3.7) |
| Personally killed during combat operations | 1.5 (1.2-2.0) | 1.3 (0.8-2.3) | 1.7 (1.4-2.1) | 1.6 (0.9-2.9) | 1.2 (0.5-2.5) |
| Saw dead bodies during combat operations | 1.9 (1.4-2.6) | 1.0 (0.5-1.8) | 2.1 (1.6-2.6) | 0.9 (0.5-1.7) | 0.7 (0.3-1.7) |
| Personally witnessed someone die during combat operations | 1.9 (1.2-3.0) | 1.0 (0.5-1.9) | 5.0 (3.4-7.4) | 1.3 (0.6-2.9) | 1.2 (0.5-3.0) |
| Personally wounded or injured during combat operations | 2.1 (1.6-2.8) | 0.9 (0.5-1.6) | 5.1 (3.9-6.6) | 1.8 (1.1-2.9) | 2.5 (1.2-5.0) |
Compared to senior enlisted (E5-E9).
Table 3.
Adjusted odds ratios and 95% confidence intervals measuring associations between predictor variables and high risk behaviors
| Tobacco abuse | Alcohol abuse | Suicide risk | |
|---|---|---|---|
| Very short sleep duration (< 6 h nightly) | 1.5 (1.2-1.9) | 1.9 (1.5-2.4) | 3.8 (1.5-9.2) |
| Short sleep duration (6 h nightly) | 1.2 (1.0-1.5) | 1.1 (0.9-1.4) | 2.3 (0.9-6.0) |
| Symptoms of insufficient sleep | 1.0 (0.8-1.2) | 1.2 (1.0-1.5) | 2.4 (1.4-4.1) |
| Age | 0.96 (0.95-0.98) | 0.92 (0.90-0.94) | 1.05 (1.00-1.11) |
| Female | 0.4 (0.3-0.7) | 0.3 (0.2-0.7) | 0.5 (0.1-3.6) |
| Junior enlisted (E1-E4)* | 1.2 (1.0-1.4) | 1.0 (0.8-1.3) | 3.0 (1.6-5.6) |
| Commissioned or warrant officers* | 0.3 (0.2-0.4) | 0.2 (0.1-0.4) | — |
| Personally killed during combat operations | 1.3 (1.0-1.6) | 1.2 (1.0-1.5) | 2.2 (1.1-4.3) |
| Saw dead bodies during combat operations | 1.1 (0.8-1.3) | 1.0 (0.8-1.3) | 1.2 (0.6-2.5) |
| Personally witnessed someone die during combat operations | 1.4 (1.1-1.8) | 1.4 (1.1-1.8) | 0.5 (0.2-1.0) |
| Personally wounded or injured during combat operations | 1.0 (0.8-1.2) | 0.8 (0.7-1.1) | 0.7 (0.4-1.4) |
Compared to senior enlisted (E5-E9).
Symptoms of insufficient sleep were reported by 37% (n = 157) of soldiers who met screening criteria for PTSD. The strongest predictor of PTSD was sleep duration < 6 h/night (AOR 4.7; 95% CI 3.2–6.9). Depression was strongly associated with sleep duration (AOR 7.9; 95% CI 2.5–25.4) and symptoms of insufficient sleep (AOR 2.5; 95% CI 2.0–3.3). Mild traumatic brain injury was most strongly associated with any combat exposure (AOR 16.7; 95% CI 10.9–25.7) but also associated with VSSD (AOR 1.8; 95% CI 1.4–2.3) and symptoms of insufficient sleep (AOR 2.0; 95% CI 1.5–2.6). Panic syndrome was associated with VSSD (AOR 3.9; 95% CI 1.6–9.4) and symptoms of insufficient sleep (AOR 3.0; 95% CI 1.9–4.9). VSSD (AOR 3.3; 95% CI 1.3–8.9), but not SSD, predicted obesity and tobacco and alcohol abuse. Both VSSD (AOR 3.8; 95% CI 1.5–9.2) and symptoms of insufficient sleep (AOR 2.4; 95% CI 1.4–4.1) predicted suicidal ideation or having attempted suicide.
DISCUSSION
This is the first known study conducted with a redeployed combat arms unit comprised of OIF Service Members to show a link between sleep duration and post-deployment health outcomes. Our results show that SSD is common and persists in most redeployed soldiers at the 90- to 180-day time period. Respondents who reported combat exposures had an increased likelihood of SSD compared to soldiers without these experiences. Further, SSD was independently associated with a variety of common medical disorders following deployment and may be a contributing factor for these conditions.
The findings of this study are important because they provide evidence of increased risk among soldiers who experience sleep problems. These data also provide evidence of the importance of addressing sleep disturbances as a separate disorder upon redeployment. Short sleep duration, excessive sleepiness, and fatigue can lead to work-related accidents.28,29 Insufficient sleep is also associated with psychiatric symptoms and can exacerbate them. For instance, sleep duration and quality of sleep (how restful) is linked to both mood disorders30 and anxiety disorders, such as PTSD.31 There is also growing evidence that problems with sleep are associated with elevated risk for suicidal behaviors.32–34
Very short sleep duration was the strongest predictor of PTSD in our study, with 75% sleeping 6 hours or less. Similarly, the military personnel in the Millennium Cohort study with PTSD slept 6.11 hours per night, significantly less than the overall average of 6.5 hours.9 Further, in a study of Israelis exposed to rocket attacks, 37% of surveyed individuals had significant sleep disorders; this increased to 81% in individuals with probable PTSD.35 In our cohort the soldiers with PTSD did not report as high a percentage of insufficient sleep symptoms from their short sleep duration. This is potentially due to the ingrained military culture, in which sleep deprivation is an accepted, if not expected practice, versus the limitation of our question regarding insufficient sleep.
While our study did not assess hypertension, stroke, or other cardiovascular disorders (all of which are associated with SSD), we did assess obesity through self-reported height and weight, noting that obesity was associated with VSSD. There is an increased risk of obesity in individuals with SSD; however, prior studies as well as ours are limited due to multiple confounding factors and are unable to determine causality.36 There is growing evidence that sleep deprivation, disruption, and insomnia are associated with increased health care utilization.37,38 Efforts to reestablish good sleep practices and aggressive evaluation of soldiers with persistent SSD following deployment may aid in the prevention and management of a variety of health risks and potentially minimize long-term health care utilization.
The present study does have several limitations that are worth discussion. First, the measures used in the current study are self-report screening measures and are not clinician administered assessments. Thus, the data do not necessarily represent true diagnostic rates of symptoms or disorders. Further, it is also possible that self-reported sleep may not reflect actual sleep duration. This possibility is reflected by evidence that suggest that individuals are not accurate in determining the actual hours of sleep they obtain.39 Second, the data are also cross-sectional, and thus the direction of causality cannot be determined. Possible etiologies of the soldiers' SSD include persistence of learned poor sleep behaviors during deployment and insomnia from multiple potential etiologies. The etiology of SSD in the present sample, however, is unknown; it may be the case that symptoms from underlying medical or psychiatric illnesses cause sleep disturbances that result in SSD. Longitudinal tracking of sleep symptoms and health outcomes can help provide data on causality. Third, although the current sample was drawn from a large Army installation that represents a diverse cross-section of soldiers, it is possible that the results are not representative of the entire Army. It is also important to note that the sample analyzed consisted of cases that were deemed fit for duty at pre-deployment screening. It is possible that soldiers with high levels of health problems or psychiatric disorders participated in prior treatment or did not deploy. Finally, there is a significant difference between SSD and insomnia. Insomnia is characterized by the inability to sleep, as well as dissatisfaction with the quality of sleep.40 However, individuals who report SSD may not necessarily meet diagnostic criteria for insomnia. Nonetheless, 16.3% of the soldiers in our present sample reported a daytime nap or felt their job performance was affected due to lack of sleep. Additional research that examines true diagnostic rates of insomnia following deployment as well as longitudinal studies that examine the effects of chronic sleep problems on health risks among those serving in the current conflicts is required.
CONCLUSIONS
This study provides unique data on the prevalence of sleep problems and subsequent impairments among a large sample of post-deployed soldiers. In particular, this study provides important information on the risk of possible new-onset PTSD and concomitant sleep disorders, manifested by short sleep duration. Expanded screening for sleep disorders upon redeployment and a multidisciplinary approach that addresses both the sleep disorder and the symptoms of PTSD has the best potential of improved outcomes for these difficult-to-treat disorders. Overall, the results of this study point to the need for additional educational, behavioral, and clinical services for service members who have a very high prevalence of short sleep duration after deployment.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest. The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or reflecting the views of the Department of the Army or the Department of Defense.
ACKNOWLEDGMENTS
The authors thank Rick Barnhill for assistance with data abstraction.
REFERENCES
- 1.Wingard DL, Berkman LF. Mortality risk associated with sleeping patterns among adults. Sleep. 1983;6:102–7. doi: 10.1093/sleep/6.2.102. [DOI] [PubMed] [Google Scholar]
- 2.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 3.Ferrie JE, Shipley MJ, Cappuccio FP, et al. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep. 2007;30:1659–66. doi: 10.1093/sleep/30.12.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Sleep duration as a risk factor for diabetes incidence in a large US sample. Sleep. 2007;30:1667–73. doi: 10.1093/sleep/30.12.1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. 2005;28:1289–96. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- 6.Neylan TC, Marmar CR, Metzler TJ, et al. Sleep disturbances in the Vietnam generation: findings from a nationally representative sample of male Vietnam veterans. Am J Psychiatry. 1998;155:929–33. doi: 10.1176/ajp.155.7.929. [DOI] [PubMed] [Google Scholar]
- 7.Peterson AL, Goodie JL, Satterfield WA, Brim WL. Sleep disturbance during military deployment. Mil Med. 2008;173:230–5. doi: 10.7205/milmed.173.3.230. [DOI] [PubMed] [Google Scholar]
- 8.Office of the Surgeon Multi-National Force-Iraq and Office of the Surgeon General United States Army Medical Command; Mental Health Advisory Team (MHAT) V Operation Iraqi Freedom 06-08. [Google Scholar]
- 9.Seeling AD, Jacobson IG, Smith B, Tomoko I, et al. Sleep patterns before, during and after deployment to Iraq and Afghanistan. Sleep. 2010;33:1615–22. doi: 10.1093/sleep/33.12.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dinges DF, Pack F, Williams K, et al. Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4-5 hours per night. Sleep. 1997;20:267–77. [PubMed] [Google Scholar]
- 11.Morphy H, Dunn K, Lewis M, et al. Epidemiology of insomnia: a longitudinal study in a UK population. Sleep. 2007;30:274–80. [PubMed] [Google Scholar]
- 12.Belenky G, Wesenten NJ, Thorne DR, et al. Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: a sleep dose-response study. J Sleep Res. 2003;12:1–12. doi: 10.1046/j.1365-2869.2003.00337.x. [DOI] [PubMed] [Google Scholar]
- 13.Harvey AG, Jones C, Schmidt DA. Sleep and posttraumatic stress disorder: a review. Clin Psychol Rev. 2003;23:377–407. doi: 10.1016/s0272-7358(03)00032-1. [DOI] [PubMed] [Google Scholar]
- 14.ASD-Health Affairs Memorandum. SAB. 2005 [Google Scholar]
- 15.Spitzer R, Kroenke K, Williams JB. Validation and utility if the self-reported version of PRIME-MD. The PHQ Primary Care Study. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 16.Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002;32:1–7. [Google Scholar]
- 17.Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): a diagnostic meta-analysis. J Gen Intern Med. 2007;22:1596–602. doi: 10.1007/s11606-007-0333-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Prins A, Ouimette P, Kimerling R, et al. The primary care PTSD screen (PC-PTSD): development and operating characteristics. Primary Care Psychiatry. 2003;9:9–14. [Google Scholar]
- 19.Blake DD, Weathers FW, Nagy LM, et al. A clinical rating scale for assessing current and lifetime PTSD: The CAPS-1. The Behavior Therapist. 1990;18:187–8. [Google Scholar]
- 20.Ouimette P, Wade M, Prins A, Schohn M. Identifying PTSD in primary care: comparison of the Primary Care-PTSD screen (PC-PTSD) and the General Health Questionnaire-12 (GHQ) J Anxiety Disord. 2008;22:337–43. doi: 10.1016/j.janxdis.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 21.Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, Hoge CW. Validating the primary care posttraumatic stress disorder screen and the posttraumatic stress disorder checklist with soldiers returning from combat. J Consult Clin Psychol. 2008;76:272–81. doi: 10.1037/0022-006X.76.2.272. [DOI] [PubMed] [Google Scholar]
- 22.Gore KL, Engel CC, Freed MC, Liu X, Armstrong DW., 3rd Test of a single-item posttraumatic stress disorder screener in a military primary care setting. Gen Hosp Psychiatry. 2008;30:391–7. doi: 10.1016/j.genhosppsych.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 23.Spitzer RL, Williams JBW, Kroenke K, et al. Utility of new procedure for diagnosing mental disorders in primary care – the Prime-MD-1000 study. JAMA. 1994;272:1749–56. [PubMed] [Google Scholar]
- 24.Spitzer RL, Kroenke K, Williams JBW. Validation and utility of a self-report version of PRIME-MD. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 25.StataCorp. College Station, TX: StataCorp; 2005. Stata Statistical Software: Release 9. [Google Scholar]
- 26.Reger MA, Gahm GA, Swanson RD, Duma SJ. Association between number of deployments to Iraq and mental health screening outcomes in US Army soldiers. J Clin Psychiatry. 2009;70:1266–72. doi: 10.4088/JCP.08m04361. [DOI] [PubMed] [Google Scholar]
- 27.Hosmer D, Lemeshow S. Applied logistic regression. New York: John Wiley & Sons; 2000. [Google Scholar]
- 28.Åkerstedt T, Fredlund P, Gillberg M, Jansson B. A prospective study of fatal occupational accidents – relationship to sleeping difficulties and occupational factors. J Sleep Res. 2002;11:69–71. doi: 10.1046/j.1365-2869.2002.00287.x. [DOI] [PubMed] [Google Scholar]
- 29.Dinges DF. An overview of sleepiness and accidents. J Sleep Res. 2009;4:4–14. doi: 10.1111/j.1365-2869.1995.tb00220.x. [DOI] [PubMed] [Google Scholar]
- 30.Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. 1996;39:411–8. doi: 10.1016/0006-3223(95)00188-3. [DOI] [PubMed] [Google Scholar]
- 31.Ross RJ, Ball WA, Sullivan KA, Caroff SN. Sleep disturbance as the hallmark of posttraumatic stress disorder. Am J Psychiatry. 1989;146:697–707. doi: 10.1176/ajp.146.6.697. [DOI] [PubMed] [Google Scholar]
- 32.Agargun MY, Kara H, Solmaz M. Sleep disturbances and suicidal behavior in patients with major depression. J Clin Psychiatry. 1997;58:249–51. doi: 10.4088/jcp.v58n0602. [DOI] [PubMed] [Google Scholar]
- 33.Bernert RA, Joiner TE. Sleep disturbances and suicide risk: A review of the literature. Neuropsychiatr Dis Treat. 2007;3:735–43. doi: 10.2147/ndt.s1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krakow B, Artar A, Warner TD, et al. Sleep disorder, depression, and suicidality in female sexual assault survivors. Crisis. 2000;21:163–70. doi: 10.1027//0227-5910.21.4.163. [DOI] [PubMed] [Google Scholar]
- 35.Palmieri P, Chipman K, Canetti D, et al. Prevalence and correlates of sleep problems in adult Israeli Jews exposed to actual or threatened terrorist or rocket attacks. J Clin Sleep Med. 2010;6:557–64. [PMC free article] [PubMed] [Google Scholar]
- 36.Cappuccio F, Taggart F, Kandala N, et al. Meta-Analysis of short sleep duration and obesity in children and adults. Sleep. 2000;31:5619–626. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Simon GE, Von Korff M. Prevalence, burden and treatment of insomnia in primary care. Am J Psychiatry. 1997;154:1417–23. doi: 10.1176/ajp.154.10.1417. [DOI] [PubMed] [Google Scholar]
- 38.Kapur V, Redline S, Nieto J, Young TB, Newman AB, Henderson JA. The relationship between chronically disrupted sleep and healthcare use. Sleep. 2002;25:289–96. [PubMed] [Google Scholar]
- 39.Means MK, Edinger JD, Glenn DM, Fins AI. Accuracy of sleep perceptions among insomnia sufferers and normal sleepers. Sleep Med. 2003;4:285–96. doi: 10.1016/s1389-9457(03)00057-1. [DOI] [PubMed] [Google Scholar]
- 40.American Academy of Sleep Medicine. 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005. The international classification of sleep disorders: a diagnostic and coding manual. [Google Scholar]