Abstract
Background
Solitary and multiple glomus tumors are vascular tumors arising from glomus cells. These two forms have distinct clinical and histopathological features, suggesting that they might have a different pathogenesis. The multiple form is less frequent than the solitary form. Its diagnosis and treatment are more problematic and often delayed.
Main observation
We present the case of a 40-year-old patient, with a 20-year history of numerous non-tender disseminated blue papules. At the age of 30 years one of the lesions was excised and than regrew and became painful. The histological exam of the lesions was consistent with glomangioma, also known as glomus tumor. We performed surgical resection of the nodular and painful lesions.
Conclusion
The diagnosis of glomus tumor is easily suspected when the lesion is painful located in the subungual region. However, if the lesions are multiple and extradigitally located, the clinical diagnosis may be difficult and requires having in mind this differential diagnosis. Our case also shows that glomus tumors may regrow after excision in the same location.
Keywords: glomangioma, glomus tumors, multiple glomus tumors, glomuvenous malformation
Introduction
Multiple glomus tumors, also known as glomangiomas, are hamartomas arising from glomus cells.[1] These tumors are extremely rare, representing only 15% of all glomus tumors.[2] Although the solitary and multiple forms of glomus tumors are both characterized by the presence of glomus cells, they have many different clinical and histopathological features.
Most of the multiple glomus tumors are sporadic and only very rarely occur in families. It is suspected that a mutation in the gene located on chromosome 1p21-22 could be involved in development of glomus tumors.[3]
We report the case of a 40-year-old male with a long history of multiple glomus tumors.
Case Report
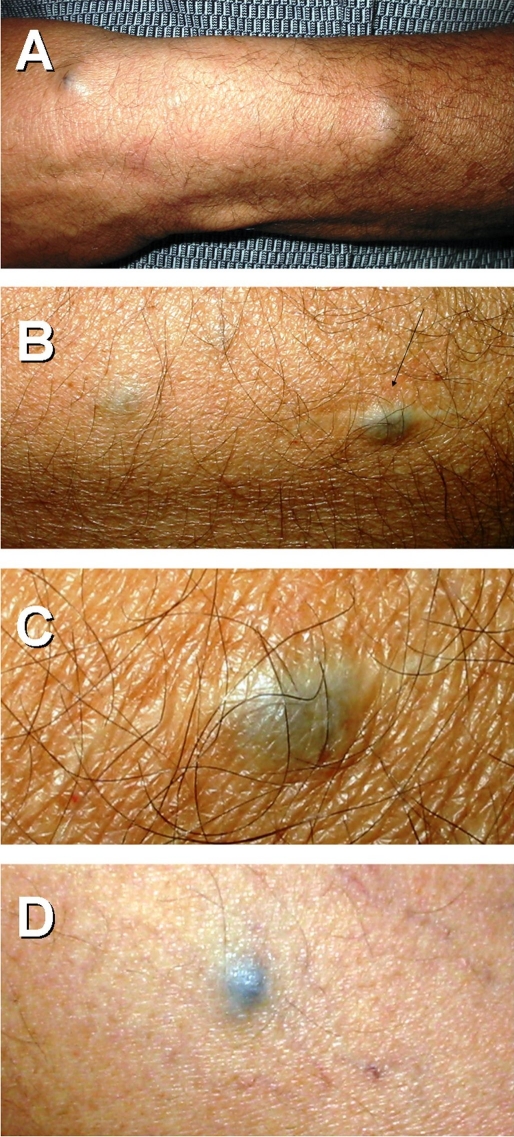
We present the case of a 40-year-old patient, with a 20-year history of numerous non-tender blue papules located on his arms, legs and trunk, and one soft, bluish painful subcutaneous nodule, 1 cm in diameter placed on the left forearm, near a post-surgical scar. [Fig. 1]. Ten years prior to present referral, this lesion was treated by local surgical excision, but after several years, a new painful one occurred in the same location. Over time other, small non-painful blue-red papules on the trunk and limbs that became darker in color with time. The patient's family history was negative for vascular malformations.
Figure 1.
Glomus tumors (blue nodules and soft papules) in different locations, one of them located in a surgical scar (arrow).
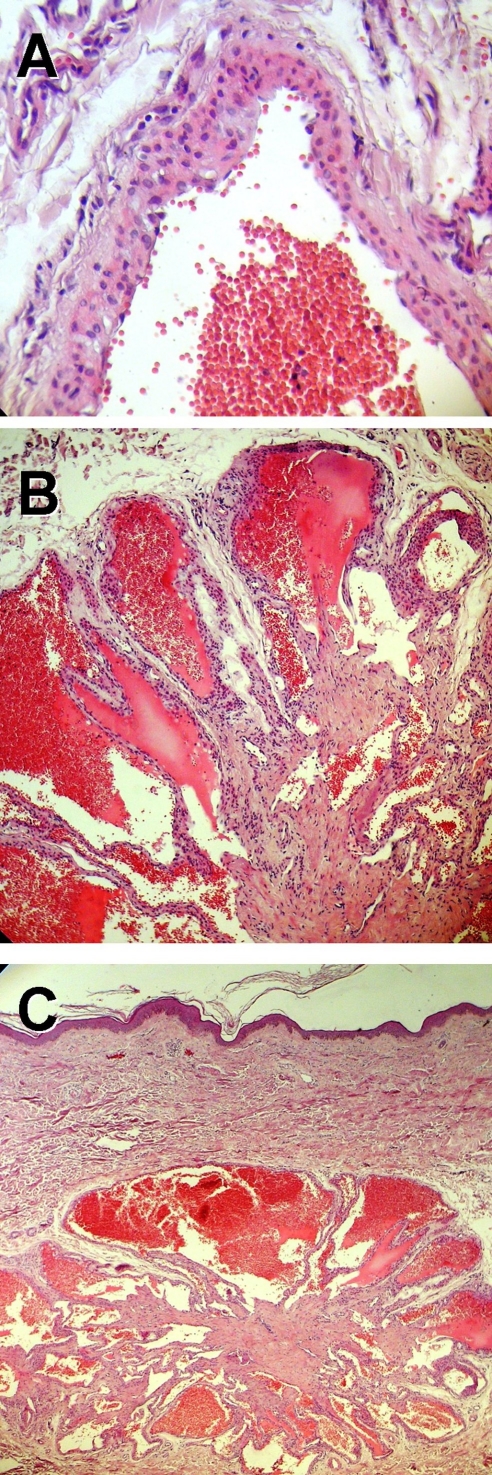
Histological exam showed large, irregularly shaped vascular spaces in dermis and subcutaneous tissue, filled with blood and surrounded by few layers of uniform glomus cells [Fig. 2], consistent with the diagnosis of glomus tumors.
Figure 2.
Histopathology images (H&E stain) show large, irregularly shaped vascular spaces in dermis and subcutaneous tissue filled with blood (A), large vascular spaces surrounded by few layers of uniform glomus cells (B and C).
Based on clinical and histological findings we established the diagnosis of multiple glomangiomas (glomus tumors). We performed surgical resection of the nodular and painful lesions. The patient will be evaluated periodically and the new painful lesions will be excised. Although extremely rare, atypical and malignant forms have been described.[4]
Discussion
Glomus tumor is a rare benign vascular lesion arising from the arterial segment of a specialized thermal regulatory apparatus called Sucquet-Hoyer canal. In the past, glomus tumors were considered to be a subtype of venous malformations, but it is now accepted that they are different entities with different origins. They are not actually true tumors, but malformations presented in the fetus due to a mutation of the glomulin gene. This is the reason why some authors prefer the name glomuvenous malformation.[5,6]
The abnormalities in arterio-venous anastomoses were first described in 1924 by Masson who called them glomus tumors.[7]
The origin of the glomus tumor is debated. Some of the authors consider that its origin is in preexisting normal glomus cells, this fact explaining why most of the tumors are localized on the extremities where the glomus apparatus is best expressed. However, occasionally, the glomus tumor is found at sites where physiologically there are no glomus bodies, these tumors being considered atypical or ectopic.[8] Cases of gastric,[9,10] pulmonary,[11] tracheal,[12,13] bone,[14–16] bowel,[17] intraneural,[18,19] neuromal,[18] fallopian tube,[21] and intravenous[22,23] glomus tumors have been described. These extradigital locations suggest that glomus tumors may arise from pluripotent mesenchimal cells or modified smooth muscle cells. This fact is also suggested by immunohistochemical studies which showed that glomus cells react positively to actin and vimentin, exactly like smooth muscle cells.
There are two major forms of glomus tumors: solitary and multiple. The solitary form is more frequently seen than the multiple form. It usually occurs in young adults in the form of a solitary, painful, red-blue tumor on the extremities with a predilection for subunghial sites. The multiple form, also known as multiple or infiltrating glomus tumor, is extremely rare, representing 10-20% of all glomus tumors[2] and is typically present in children. In some cases the disease may be inherited in an autosomal dominant pattern with incomplete penetrance and variable expressivity and involves mutations in the glomulin gene. The multiple glomus tumors vary from small bluish macules and papules to large nodules and plaques, ranging in number from few to hundreds of lesions. They have no predilection site. Usually, they are more compressible than the solitary lesions and less painful.
Besides the clinical examination and histology, other investigation methods, like conventional radiograph, ultrasound and magnetic resonance imaging (MRI), may be used to support the diagnosis. MRI is the most sensitive method and is used for defining the extent of the tumor and its relationship to other anatomical structures. This method is extremely useful for glomangiomas which are more extensive.
Histologically, there are three main variants described accordingly to the predominant component.[24]
solitary glomus tumor - usually encapsulated and has many glomus cells surrounding the vascular lumina and small vascular spaces. Glomus cells are round or polygonal cells with centrally placed round or ovoid nuclei and have scant eosinophilic cytoplasm.
glomangioma - has larger and more irregular vascular spaces coated by few layers of glomus cells and is less well circumscribed. This type is usually seen in multiple glomus tumors.[25]
glomangiomyoma - also contains multiple smooth muscle cells.[24]
The differential diagnosis includes all the painful tumors, blue nevus, malign melanoma and Kaposi disease. Besides those, glomangiomas must be distinguished from ordinary venous malformations that can be emptied by compression and that lack glomus cells by histological examination. Blue rubber bleb nevus syndrome is a familial disorder characterized by multiple venous malformations, cutaneously and systemically, such as in the gastrointestinal tract where they can cause bleeding.
If the lesions are asymptomatic and the patient is untroubled by their cosmetic appearance, there is no treatment required and only periodically evaluation is needed.
The treatment modalities reported are complete surgical excision, electrodessication, pulsed dye laser[24] and sclerotherapy using hypertonic saline[26] and sodium tetradecyl sulfate.[27] In case of multiple tumors, the therapeutic approach is more complicated due to their more extensive features.
In conclusion, multiple glomus tumors are rare benign vascular lesions more commonly seen in males and children. Although a hereditary predisposition has been suggested, only few familial cases have been reported. In our patient the family history was negative. This type of glomus tumors has an earlier age of onset than the solitary tumors, usually arising in children and adolescents. In our case the lesions occurred in adult life. There are only few reports of multiple glomus tumors developed later in life with one case reported in a 82-year-old women.[28]
Multiple glomus tumors are usually asymptomatic, but painful and painless lesions may be present in the same patient[25], as it is in our case. There are several hypotheses trying to explain this symptom. Pain may be triggered by trauma, pressure or temperature changes, as well as estrogen stimuli, because during premenstrual periods there is an increase of severity of pain. In some of the lesions, the histological exam revealed an increased number of mast cells and their degranulation may explain the occurrence of pain. However, not all tumors have this feature. In our case, there was only a sparse infiltrate with lymphocytes.
The diagnosis of glomus tumor is readily suspected if the lesion is painful and if it is in subungual region. On the contrary, if the lesions are multiple and extradigital located, the clinical diagnosis is much more problematic. Often the patients are seen by numerous consultants and the diagnosis is delayed. This explains why it is so important to have in mind this differential diagnosis in both, adolescents and adult persons.
Acknowledgments
The authors would like to thank Dr. Alice Rusu and Maria Grigore from "Scarlat Longhin" Clinical Hospital of Dermatology and Venerology for pathologic evaluation.
References
- Anakwenze OA, Parker WL, Schiefer TK, Inwards CY, Spinner RJ, Amadio PC. Clinical features of multiple glomus tumors. Dermatol Surg. 2008;34:884–890. doi: 10.1111/j.1524-4725.2008.34173.x. [DOI] [PubMed] [Google Scholar]
- North PE, Hull C, Kincannon J. Vascular Neoplasms and Neoplastic-like Proliferations In Dermatology Bolognia JL, Jorizzo JL, Rapini RP. Mosby; 2004. pp. 1835–1837. [Google Scholar]
- Irrthum A, Brouillard P, Enjolras O, Gibbs NF, Eichenfield LF, Olsen BR, Mulliken JB, Boon LM, Vikkula M. Linkage disequilibrium narrows locus for venous malformation with glomus cells (VMGLOM) to a single 1.48 Mbp YAC. Eur J Hum Genet. 2001;9:34–38. doi: 10.1038/sj.ejhg.5200576. [DOI] [PubMed] [Google Scholar]
- Brathwaite CD, Poppiti RJ Jr. Malignant glomus tumor. A case report of widespread metastases in a patient with multiple glomus body hamartomas. Am J Surg Pathol. 1996;20:233–238. doi: 10.1097/00000478-199602000-00012. [DOI] [PubMed] [Google Scholar]
- Mallory SB, Enjolras O, Boon LM, Rogers E, Berk DR, Blei F, Baselga E, Ros AM, Vikkula M. Congenital plaque-type glomuvenous malformations presenting in childhood. Arch Dermatol. 2006;142:892–896. doi: 10.1001/archderm.142.7.892. [DOI] [PubMed] [Google Scholar]
- Boon LM, Mulliken JB, Enjolras O, Vikkula M. Glomuvenous malformation (glomangioma) and venous malformation: distinct clinicopathologic and genetic entities. Arch Dermatol. 2004;140:971–976. doi: 10.1001/archderm.140.8.971. [DOI] [PubMed] [Google Scholar]
- Masson P. Le glomus neuromyoarteriel des region tactiles et ses tumeurs. Lyon Chirurgical. 1924;21:257–280. [Google Scholar]
- Schiefer TK, Parker WL, Anakwenze OA, Amadio PC, Inwards CY, Spinner RJ. Extradigital glomus tumors: a 20-year experience. Mayo Clin Proc. 2006;81:1337–1344. doi: 10.4065/81.10.1337. [DOI] [PubMed] [Google Scholar]
- Alempijevic T, Knezevic S, Knezevic D, Ostojic S, Stojakov D, Micev M, Tomic D, Krstic M. Gastric multicentric glomangioma: a case report of this rare cause of abdominal pain. Med Sci Monit. 2008;14:CS5–8. [PubMed] [Google Scholar]
- Urbańczyk K, Stachura J, Papla B, Karcz D, Matłok M. Gastric solid glomus tumor and multiple glomangiomyomas of the large bowel with intravascular spread, multifocal perivascular proliferations and liver involvement. Pol J Pathol. 2007;58:207–214. [PubMed] [Google Scholar]
- Dalfior D, Parisi A, Cannizzaro C, Bontempini L, Di Pace C, Menestrina F, Dalla Palma P, Barbareschi M. Pulmonary glomus tumor. Int J Surg Pathol. 2008;16:81–84. doi: 10.1177/1066896907304520. [DOI] [PubMed] [Google Scholar]
- Altinok T, Cakir E, Gulhan E, Tastepe I. Tracheal glomus tumor. J Thorac Cardiovasc Surg. 2006;132:201–202. doi: 10.1016/j.jtcvs.2006.03.032. [DOI] [PubMed] [Google Scholar]
- Haver KE, Hartnick CJ, Ryan DP, Shailam R, Mark EJ. Case records of the Massachusetts General Hospital. Case 10-2008. A 10-year-old girl with dyspnea on exertion. N Engl J Med. 2008;358:1382–1390. doi: 10.1056/NEJMcpc0800629. [DOI] [PubMed] [Google Scholar]
- Gombos Z, Fogt F, Zhang PJ. Intraosseous glomus tumor of the great toe: a case report with review of the literature. J Foot Ankle Surg. 2008;47:299–301. doi: 10.1053/j.jfas.2008.04.003. [DOI] [PubMed] [Google Scholar]
- Okada K, Ito K, Yamasoba T, Ishii M, Iwasaki S, Kaga K. Benign mass lesions deep inside the temporal bone: imaging diagnosis for proper management. Acta Otolaryngol Suppl. 2007;559:71–77. doi: 10.1080/03655230701597127. [DOI] [PubMed] [Google Scholar]
- Sunderraj S, al-Khalifa AA, Pal AK, Pim HP, Sabri SH. Primary intra-osseous glomus tumour. Histopathology. 1989;14:532–536. doi: 10.1111/j.1365-2559.1989.tb02191.x. [DOI] [PubMed] [Google Scholar]
- Ramos Macías A, Borkoski Barreiros S, Pérez Plasencia D, Lisner Contreras I, Armesto Fernández A, Cenjor Espanol C, Masgoret E. Glomus tumours of temporal bone origin. Study of 17 cases. Acta Otorrinolaringol Esp. 2007;58:358–361. [PubMed] [Google Scholar]
- Koibuchi H, Fujii Y, Taniguchi N. An unusual case of a glomus tumor developing in a subcutaneous vein of the wrist. J Clin Ultrasound. 2008;36:369–370. doi: 10.1002/jcu.20493. [DOI] [PubMed] [Google Scholar]
- Calonje E, Fletcher CD. Cutaneous intraneural glomus tumor. Am J Dermatopathol. 1995;17:395–398. doi: 10.1097/00000372-199508000-00016. [DOI] [PubMed] [Google Scholar]
- Polk P, Biggs PJ. Glomus tumor in neural tissue. Am J Dermatopathol. 1996;18:444. doi: 10.1097/00000372-199608000-00053. [DOI] [PubMed] [Google Scholar]
- Bartels LJ, Pennington J, Kamerer DB, Browarsky I. Primary fallopian canal glomus tumors. Otolaryngol Head Neck Surg. 1990;102:101–105. doi: 10.1177/019459989010200201. [DOI] [PubMed] [Google Scholar]
- Koibuchi H, Fujii Y, Taniguchi N. An unusual case of a glomus tumor developing in a subcutaneous vein of the wrist. J Clin Ultrasound. 2008;36:369–370. doi: 10.1002/jcu.20493. [DOI] [PubMed] [Google Scholar]
- Beham A, Fletcher CD. Intravascular glomus tumor: a previously undescribed phenomenon. Virchows Arch A Pathol Anat Histopathol. 1991;418:175–177. doi: 10.1007/BF01600294. [DOI] [PubMed] [Google Scholar]
- Antony FC, Cliff S, Cowley N. Complete pain relief following treatment of a glomangiomyoma with the pulsed dye laser. Clin Exp Dermatol. 2003;28:617–619. doi: 10.1046/j.1365-2230.2003.01403.x. [DOI] [PubMed] [Google Scholar]
- Carvalho VO, Taniguchi K, Giraldi S, Bertogna J, Marinoni LP, Fillus JN, Reis Filho JS. Congenital plaquelike glomus tumor in a child. Pediatr Dermatol. 2001;18:223–226. doi: 10.1046/j.1525-1470.2001.018003223.x. [DOI] [PubMed] [Google Scholar]
- Siegle RJ, Spencer DM, Davis LS. Hypertonic saline destruction of multiple glomus tumors. J Dermatol Surg Oncol. 1994;20:347–348. doi: 10.1111/j.1524-4725.1994.tb01636.x. [DOI] [PubMed] [Google Scholar]
- Gould EP. Sclerotherapy of multiple glomangiomata. J Dermatol Surg Oncol. 1991;17:351–352. doi: 10.1111/j.1524-4725.1991.tb01710.x. [DOI] [PubMed] [Google Scholar]
- Betti R, Palvarini M, Inselvini E, Crosti C. Multiple glomus tumors in an octuagenarian. J Eur Acad Dermatol Venereol. 1996;6:270–273. [Google Scholar]