Abstract
Background
Angiosarcoma is a malignant tumor of the blood vessels' endothelial lining. The tumor is very aggressive and tends to recur locally and metastasize to distant organs. Commonly, it is associated with different risk factors like lymphoedema, prior radiotherapy but rarely, it may also be associated with chronic venous ulceration.
Main observation
We present a patient with a chronic venous ulceration who developed angiosarcoma of the ulcerated leg with good outcome after treatment.
Conclusion
It is very important to follow patients with chronic wounds and recognize changes which may be life threatening. In addition to squamous cell carcinoma (Marjolin's tumor), which is most common, angiosarcoma can develop within a venous ulcer.
Keywords: angiosarcoma, CD31, pathology, skin, Ulex europaeus, ulcer
Introduction
Angiosarcoma is a malignant tumor of the blood vessels' endothelial lining. The tumor is very aggressive and tends to recur locally and metastasize to distant organs. Commonly, it is associated with different risk factors like lymphoedema, prior radiotherapy but rarely, it may also be associated with chronic venous ulceration. We present a patient with a chronic venous ulceration who developed angiosarcoma of the ulcerated leg with good outcome after treatment.
Case Report
A 59 year old Caucasian female of French-Canadian origin who is presented to our clinic in 2002 complaining of a left leg medial malleolus ulcer for few months duration. The problem started 10 years ago with recurrent bilateral leg ulcerations with periods of relapse and remission. She is known for morbid obesity, deep venous thrombosis in 1985, and a bilateral venous insufficiency.
The patient was treated with compression therapy and analgesics with good response. Over 3-4 weeks, red indurated plaques around the ulcer that extended proximally accompanied by severe pain, and increased ulcer size were noticed [Fig. 1]. Soft tissue infection (cellulitis) was suspected and antibiotic therapy was administered. No improvement was seen. Worsening of the pain, redness, and induration were observed.
Figure 1.
Red infiltrative plaques around the left leg medial malleolus ulcer extending proximally and distally.
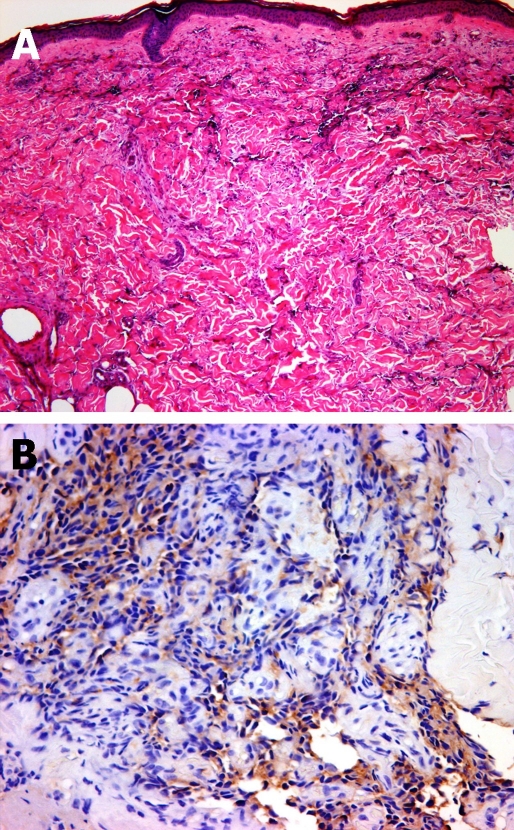
Two biopsies were obtained from the red plaques above and below the ulcer. A dermal infiltrative process with proliferations of pleomorphic cells with hyperchromatic nuclei residing in spaces between the collagen bundles were observed [Fig. 2A]. In addition, solid areas of similar cellular proliferations were noticed. These cells were stained positive for endothelial markers CD31, Ulex europaeus, and Factor VIII [Fig. 2B]. Based on these observations, angiosarcoma is diagnosed, that extensively infiltrating the dermis and superficial subcutaneous tissue.
Figure 2.
Infiltrative pleomorphic cells in between collagen bundles, forming spaces. H&E x5 (A) The cells stained positive with endothelial markers. Ulex europaeus x20 (B).
CT scans of the chest, abdomen, and pelvis showed illdefined lesions in the lungs, liver, and adrenals. These lesions were not typical of metastasis but further investigations were carried out to exclude metastatic disease.
Consequently, the patient underwent positron emission tomography (PET) scan, which showed diffuse soft tissue involvement of the left leg and distal area of the thigh. There were no metastases.
The patient was referred to the radiation oncology and orthopedic surgery departments for further treatment. The left lower extremity was amputated followed by radiation therapy. The patient had survived and is currently alive over 5 years after initial diagnosis without recurrence of the tumor.
Discussion
Angiosarcoma is a malignant tumor of the endothelial cells which accounts for 1% of all sarcomas.[1] It is a very aggressive tumor, which tends to recur locally and metastasize despite aggressive therapies. In contrast to other sarcomas, angiosarcoma has a predilection to skin and soft tissues especially the head and neck region.[2] It has been proposed that the unique anastomatic arrangement of vessels as well as the vascular density of the head and neck region, in combination with ultraviolet radiation are important factors for this predilection.
Rouhani et al have reviewed cutaneous soft tissue sarcoma in United States from 1992 through 2004 and have found that angiosarcoma incidence was highest among whites as compared to blacks.[3] In addition, the incidence rate of angiosarcoma was increasing in whites that was 0.5 per 1,000,000.[3] The risk factors for angiosarcoma[4] include: chronic pyothorax, exposure to environmental toxins and drugs (Thorotrast, insecticides containing AsO3, vinyl chloride, long-term anabolic steroid and estrogen therapy), previous radiotherapy, chronic lymphoedema (Stewart-Treves syndrome), morbid obesity,[5] and renal transplantation.[6,7]
Less commonly reported associations are pre-existing neoplasia (benign and malignant nerve sheath tumors, leiomyomas, plexiform neurofibromas, schwannomas, and malignant germ cell tumour), familial syndromes (Klippel-Trenaunay syndrome, Maffucci syndrome, neurofibromatosis, Aicardi syndrome, xeroderma pigmentosum, and hereditary retinoblastoma), and adjacent to foreign material (shrapnel, steel, plastic, Dacron, vascular graft material, surgical sponges, and bone wax).[8,9]
Chronic skin ulceration is a rare predisposing condition for angiosarcoma. Two cases of angiosarcoma involving a cutaneous ulcer were reported.[10,11] The first case report described a chronic ulcer that developed in a gumma scar which has been associated with lymphoedema for 20 years. The histopathology described in the report is not clearly stated.[10] On the other hand, the second reported case was a poorly differentiated angiosarcoma that developed in an ulcer that persisted for 15 years in the left lower leg. The lesion recurred following multiple radiation therapies. The patient died from metastasis a year after diagnosis.[11]
In our patient, no preceding lymphoedema, and preexisting lesions (prior to ulceration) was described. The age of the patient is younger than the previously reported cases and the duration between ulceration and the development of the tumor is shorter as compared to the reported patients. Moreover, the histopathological diagnosis is clear that was made earlier with good outcome after treatment. It is an unusual presentation of this aggressive neoplasm which has a higher incidence in the older age groups, commonly involving the head and neck region and the upper limb.
The Overall prognosis of angiosarcoma is poor, with a reported 5-year survival of 10% to 35%.[12] Higher reported 5-year survival of 45% was seen in the US study of cutaneous soft tissue sarcoma.[3] Poor prognostic factors include tumor diameter, depth of invasion, positive resection margins, metastases, and tumor recurrence.[13]
Treatment of cutaneous angiosarcoma represents a therapeutic challenge. As the disease is rare, the standard treatment has not been established yet. Radical surgical excision and radiotherapy is the mainstay of treatment but can be difficult because of the multifocal growth of the tumor and non-apparent transdermal spread.[14] Irradiation with high dose per fraction (30 Gy /10 fractions) has been suggested in one case report.[15]
The role of adjuvant chemotherapy is unclear. Different chemotherapeutic agents have been used that include: Doxorubicin,[16] systemic paclitaxel,[17] and subcutaneous interferon alfa-2a with oral 13-cis-retinoic acid.[18]
In conclusion, we presented a 59 years old woman with angiosarcoma of the skin in association with a chronic venous ulcer of the left medial malleolus. Early diagnosis and treatment by amputation and radiotherapy was associated with a favorable course.
It is crucial for healthcare providers to follow patients with chronic wounds and recognize changes which may be life threatening. When an ulcer does not respond to adequate medical and wound care, the potential for an underlying malignancy should be considered. Cutaneous malignancies that may masquerade as ulcers include nodulo- ulcerative basal cell carcinoma, squamous cell carcinoma, keratoacanthoma, nodular melanoma, tumor stage mycosis fungoides, lymphomatoid granulomatosis, lymphomatoid papulosis, angiosarcoma, and cutaneous metastases from internal malignancy.[19] Our case shows that in addition to the more commonly described squamous cell carcinoma (Marjolin's tumor), also angiosarcoma can develop within a venous ulceration.
References
- Abraham JA, Hornicek FJ, Kaufman AM, Harmon DC, Springfield DS, Raskin KA, Mankin HJ, Kirsch DG, Rosenberg AE, Nielsen GP, Desphpande V, Suit HD, DeLaney TF, Yoon SS. Treatment and outcome of 82 patients with angiosarcoma. Ann Surg Oncol. 2007;14:1953–1967. doi: 10.1245/s10434-006-9335-y. [DOI] [PubMed] [Google Scholar]
- Deyrup AT, McKenney JK, Tighiouart M, Folpe AL, Weiss SW. Sporadic cutaneous angiosarcomas: a proposal for risk stratification based on 69 cases. Am J Surg Pathol. 2008;32:72–77. doi: 10.1097/PAS.0b013e3180f633a3. [DOI] [PubMed] [Google Scholar]
- Rouhani P, Fletcher CD, Devesa SS, Toro JR. Cutaneous soft tissue sarcoma incidence patterns in the U.S.: an analysis of 12,114 cases. Cancer. 2008;113:616–627. doi: 10.1002/cncr.23571. [DOI] [PubMed] [Google Scholar]
- Abeloff MD. Clinical Oncology. Chapter 96, 3rd ed. Elsevier; 2004. [Google Scholar]
- Azam M, Saboorian H, Bieligk S, Smith T, Molberg K. Cutaneous angiosarcoma complicating morbid obesity. Arch Pathol Lab Med. 2001;125:531–533. doi: 10.5858/2001-125-0531-CACMO. [DOI] [PubMed] [Google Scholar]
- Ahmed I, Hamacher KL. Angiosarcoma in a chronically immunosuppressed renal transplant recipient: report of a case and review of the literature. Am J Dermatopathol. 2002;24:330–335. doi: 10.1097/00000372-200208000-00009. [DOI] [PubMed] [Google Scholar]
- Kibe Y, Kishimoto S, Katoh N, Yasuno H, Yasumura T, Oka T. Angiosarcoma of the scalp associated with renal transplantation. Br J Dermatol. 1997;136:752–756. [PubMed] [Google Scholar]
- Weiss SW, Goldblum JR. Malignant vascular tumors. In: Weiss SW, Goldblum JR, eds. Soft tissue tumors, 4th ed. St. Louis: Mosby; 2001. pp. 917–954. [Google Scholar]
- Calonje E, Fletcher CDM. Tumors of blood vessels and lymphatics. In: Fletcher CDM, ed. Diagnostic histopathology of tumors, 2nd ed. London: Churchill Livingstone; 2000. pp. 45–86. [Google Scholar]
- Kofler H, Pichler E, Romani N, Philadelphy H, Fritsch P. Hemangiosarcoma in chronic leg ulcer. Arch Dermatol. 1988;124:1080–1082. [PubMed] [Google Scholar]
- Al-Najjar AA, Harrington CI, Slater DN. Angiosarcoma: a complication of varicose leg ulceration. Acta Derm Venereol. 1986;66:167–170. [PubMed] [Google Scholar]
- Gkalpakiotis S, Arenberger P, Vohradnikova O, Arenbergerova M. Successful radiotherapy of facial angiosarcoma. Int J Dermatol. 2008;47:1190–1192. doi: 10.1111/j.1365-4632.2008.03813.x. [DOI] [PubMed] [Google Scholar]
- Morgan MB, Swann M, Somach S, Eng W, Smoller B. Cutaneous angiosarcoma: a case series with prognostic correlation. J Am Acad Dermatol. 2004;50:867–874. doi: 10.1016/j.jaad.2003.10.671. [DOI] [PubMed] [Google Scholar]
- Mark RJ, Poen JC, Tran LM, Fu YS, Juillard GF. Angiosarcoma. A report of 67 patients and a review of the literature. Cancer. 1996;77:2400–2406. doi: 10.1002/(SICI)1097-0142(19960601)77:11<2400::AID-CNCR32>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- Holloway CL, Turner AR, Dundas GS. Cutaneous angiosarcoma of the scalp: a case report of sustained complete response following liposomal Doxorubicin and radiation therapy. Sarcoma. 2005;9:29–31. doi: 10.1080/13577140500043948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bong AB, Bonnekoh B, Schön MP, Gollnick H. Treatment of scalp angiosarcoma by controlled perfusion of A. carotis externa with pegylated liposomal doxorubicin and intralesional application of pegylated interferon alfa. J Am Acad Dermatol. 2005;52:20–23. doi: 10.1016/j.jaad.2004.06.026. [DOI] [PubMed] [Google Scholar]
- Pestoni C, Paredes-Suarez C, Peteiro C, Toribio J. Early detection of cutaneous angiosarcoma of the face and scalp and treatment with placitaxel. J Eur Acad Dermatol Venereol. 2005;19:357–359. doi: 10.1111/j.1468-3083.2004.01139.x. [DOI] [PubMed] [Google Scholar]
- Spieth K, Gille J, Kaufmann R. Therapeutic efficacy of interferon alfa-2a and 13-cis-retinoic acid in recurrent angiosarcoma of the head. Arch Dermatol. 1999;135:1035–1037. doi: 10.1001/archderm.135.9.1035. [DOI] [PubMed] [Google Scholar]
- Perrotto J, Glick B. Lower extremity malignancies masquerading as ulcers. Ostomy Wound Manage. 2006;52:46–52. [PubMed] [Google Scholar]