Abstract
Background
Erythema multiforme is a cutaneous reaction that has only rarely been described in varicella zoster virus infection.
Main observations
We describe a 76-year old immunocompetent male patient with thoracic herpes zoster. While treated with oral brivudin he developed a widespread cutaneous erythema multiforme. The lesions completely cleared with two weeks with systemic corticosteroids.
Conclusion
Varicella zoster infections are possible triggers of erythema multiforme and this is the oldest patient reported with such an association. Brivudin itself has not been reported to induce erythema multiforme and is an unlikely cause of disease in our patient.
Keywords: brivudin, drug reaction, erythema multiforme, varicella zoster virus, virus diseases
Introduction
Erythema multiforme is a skin condition considered to be a hypersensitivity reaction to infections or drugs. It consists of a polymorphous eruption of macules, papules, and characteristic "target" lesions that are symmetrically distributed with a propensity for the distal extremities. There is minimal mucosal involvement.
Histopathologic characteristics include a lymphocytic infiltrate at the dermal-epidermal junction and around dermal blood vessels, dermal edema, epidermal keratinocyte necrosis, and subepidermal bullae formation. Inflammatory infiltrates of EM have a high density of cell infiltrate rich in T-lymphocytes.
The incidence of EM has been estimated to be between 0.01 and 1%. EM usually is not associated with any mortality. Most cases are self-limited and resolve without sequelae in 2-4 weeks. EM affects males more often than females, with a ratio ranging from 3:2 to 2:1. All ages are affected, with a peak incidence in the second through fourth decades of life. This condition is rare in persons younger than 3 years and older than 50 years. The onset is sudden with rapidly progressive, symmetrical, and cutaneous and / or mucocutaneous lesions, with concentric colour changes in some or all lesions. Pruritus is generally absent. The major causative factors are herpes simplex (HSV) infection and drugs.[1]
A patient with EM associated with herpes zoster virus (VZV) infection will be described.
Case Report
A 76-year old imunocompentent male developed herpes zoster thoracicus. The patient had no history of other diseases (also no HSV infection) or medications. He was treated with oral 125 mg brivudin (Zostex®) once daily for 7 days according to German guidelines for herpes zoster treatment.[2]
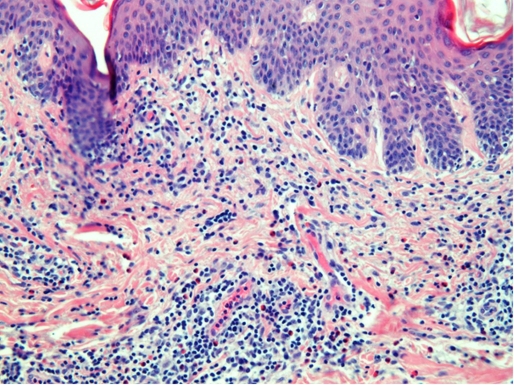
During this period herpes zoster improved but a multiform, partly vesiculous, non-pruritic exanthematous rash developed [Figs. 1 and 2]. There was no mucosal involvement. We took a skin biopsy that revealed the typical histopathologic findings of EM [Fig. 3], with high density lymphocytic infiltrates and epidermal necrosis of the basal layer.
Figure 1.
Herpes zoster thoracicus with multiform erythematous lesions.
Figure 2.
Erythema multiforme: detail shows targetoid lesions with some vesiculation.
Figure 3.
Histopathology of multiform erythema showing with high density lymphocytic infiltrates and epidermal necrosis of the basal layer (HE, x20).
Because of the widespread cutaneous lesions we started corticosteroid therapy, beginning with 100 mg prednisolone intravenously per day. The dosage was tapered down after partial response and the application was switched to oral tablets. EM showed a complete clearing within two weeks.
Discussion
Varicella zoster -associated EM is a rare occasion. In recent years 7 patients including two children have been described. [3,4,5] Some cases had vesicobullous EM lesions. At least in one patient anti-viral therapy with acyclovir might have been responsible for EM eruption.[5] Only three adult patients have been identified with herpes zoster followed by EM [Table 1].
Table 1. Overview of published cases of herpes zoster-associated erythema multiforme.
| Patient | Age (years) | Zoster type | Zoster treatment | Mucous membranes | Conjunctivitis | Bullae | Delay in days after zoster | Reference |
|---|---|---|---|---|---|---|---|---|
| Caucasian male | 35 | thoracic | oral acyclovir | + | + | + | 10 | 3 |
| Caucasian male | 22 | thoracic | oral acyclovir | + | - | + | 14 | 3 |
| Caucasian female | 20 | thoracic | oral acyclovir | - | - | + | 14 | 3 |
| Japanese male | 49 | cervical | intravenous acyclovir | - | - | + | 14 | 5 |
| Caucasian male | 76 | thoracic | oral brivudin | - | - | + | 6 | present |
It has been suggested that soluble factors of T-cells may be responsible for epidermal detachment and vesicobullous eruptions in both viral lesions and EM. Identified factors involved in pathophysiology of EM-lesions are perforin, thymus- and activation-regulated chemokine (TARC), IL-12 and soluble Fas - ligand among others.[6,7]
Remarkable that our patient: 1) does not belong to the preferred age group of zoster-induced erythema multiforme and 2) no other case treated with brivudin has yet been described. This drug may me theoretically the inducing factor for EM, however the course of EM in our patient suggests a closer relationship to virus-induced immune alterations than to antiviral drug use.[8] Although mild cases do not need treatment, we decided in this particular patient to use systemic corticosteroids because of widespread cutaneous involvement.
In conclusion, varicella-zoster virus infections have to be considered as possible trigger of erythema multiforme eruptions.
References
- Lamoreux MR, Sternbach MR, Hsu WT. Erythema multiforme. Am Fam Physician. 2006;74:1883–1888. [PubMed] [Google Scholar]
- Gross G, Schöfer H, Wassilew S, Friese K, Timm A, Guthoff R, Pau HW, Malin JP, Wutzler P, Doerr HW. Herpes zoster guideline of the German Dermatology Society (DDG) J Clin Virol. 2003;26:277–289. doi: 10.1016/s1386-6532(03)00005-2. [DOI] [PubMed] [Google Scholar]
- Weisman K, Petersen CS, Blichmann CW, Nielsen NH, Hultberg BM. Bullous erythema multiforme following herpes zoster and varicella-zoster virus infection. J Eur Acad Dermatol Venereol. 1998;11:147–150. doi: 10.1111/j.1468-3083.1998.tb00768.x. [DOI] [PubMed] [Google Scholar]
- Prais D, Grisuru-Soen G, Barzilai A, Amir J. Varicella zoster virus infection associated with erythema multiforme in children. Infection. 2001;29:37–39. doi: 10.1007/s15010-001-0003-7. [DOI] [PubMed] [Google Scholar]
- Onishi I, Kishimoto S. Erythema multiforme after resolution of herpes zoster by acyclovir. Eur J Dermatol. 2002;12:370–372. [PubMed] [Google Scholar]
- Sayama K, Watanabe Y, Tohyama M, Miki Y. Localization of perforin in viral vesicles and erythema multiforme. Dermatology. 1994;188:305–309. doi: 10.1159/000247172. [DOI] [PubMed] [Google Scholar]
- Quaglino P, Caproni M, Antiga E, Del Bianco E, Osella-Abate S, Savoia P, Frezzolini A, Schena D, Marzano A, Volpi W, De Simone C, Parodi A, Fabbri P, Bernengo MG. Serum levels of the Th1 promoter IL-12 and the Th2 chemokine TARC are elevated in erythema multiforme and Stevens-Johnson syndrome/toxic epidermal necrolysis and correlate with soluble Fas ligand expression. An immunoenzymatic study from the Italian Group of Immunopathology. Dermatology. 2007;214:296–304. doi: 10.1159/000100880. [DOI] [PubMed] [Google Scholar]
- Keam SJ, Chapman TM, Figgitt DP. Brivudin (bromovinyl deoxyuridine) Drugs. 2004;64:2091–2097. doi: 10.2165/00003495-200464180-00011. [DOI] [PubMed] [Google Scholar]