Abstract
Background
Pyoderma gangrenosum is a rare inflammatory disease of unknown etiology and a poorly understood pathogenesis. Its clinical presentation is variable and a large percentage of cases are associated with inflammatory bowel diseases. Peristomal pyoderma gangrenosum represents a variant of the diseases, occurring in patients with colostomy. Multiple cases demonstrate efficacy of infliximab and other anti-TNF-alpha drugs in treatment of pyoderma gangrenosum.
Main observations
A 47-year-old male with ulcerative colitis and proctocolectomy with ileal pouch reconstruction protected by ileostomy in the course of diseases received infliximab therapy together with azathioprine for his inflammatory bowel diseases. Six months after initiation of infliximab therapy the patient developed multiple pyoderma gangrenosum lesions on the trunk, abdomen, genitalia, gluteus, extremities, left preauricular region and peristomal area. After systemic corticosteroid therapy, combined with topical tacrolimus, the lesions slowly improved. Seven months later, during ongoing infliximab therapy, the patient developed a sepsis with fatal outcome.
Conclusion
Constant trauma generated by colostomy may be a contributing factor to the development and persistence of pyoderma gangrenosum. It may be hypothesized that this patient developed pyoderma gangrenosum despite infliximab or that pyoderma gangrenosum may represent a rare adverse effect of the drug.
Keywords: adverse effects, biological products, inflammatory bowel diseases infliximab, pyoderma gangrenosum, stoma, ulcerative colitis
Introduction
Pyoderma gangrenosum (PG) is a rare inflammatory disease of unknown etiology and a poorly understood pathogenesis.[1] Its clinical presentation is variable and a large percentage of cases are associated with inflammatory bowel diseases.[1–5] Several case report and studies of short series demonstrated the efficacy anti-tumor necrosis factor therapy in pyoderma gangrenosum.[6] We report the case of a patient with ulcerative colitis who developed PG during therapy with infliximab.
Case Report
A 47-year-old hispanic male with a history of ulcerative colitis. He had evidence of high grade dysplasia, requiring proctocolectomy with ileal pouch reconstruction protected by ileostomy. The patient developed an abdominal collection with suprapubic skin drainage that recurred two times. He was treated with antibiotics and percutaneous drainage guidesd by tomography.
He continued presenting manifestations of pouchitis, demonstrated by rectosigmoidoscopy, and a perianal fistulae of difficult management, having multiple local infections needing medical and surgical treatment.
Because of the resistance to medical and surgical treatments, infliximab was started (3 doses of 5 mg/kg, at 0, 2 and 6 weeks, followed by 5 mg/kg every 8 wks) together with azathioprine, obtaining a good response of the intestinal symptoms. During infliximab therapy, six months after the first dose, the patient developed multiple erythemato- violaceous lesions that became ulcerated. Painful ulcers, with an erythemato-violaceous border and a seropurulent base were present on the trunk, abdomen, genitalia, gluteus, extremities, left preauricular region and peristomal area. Despite multiple antibiotic treatments there was no improvement. New lesions continued to appear [Fig. 1 and 2]. Patients never reported arthralgia or fever associated with dermatologic lesions.
Figure 1.
Peristomal pyoderma gangrenosum.
Figure 2.
Ulcer with irregular violaceous border on left preauricular region with partial scarring.
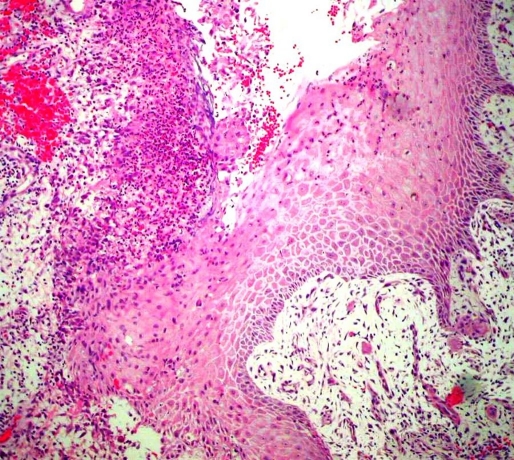
Biopsy showed an ulcerated epidermis with a dense cell infiltrate; compose of giant cells, plasmatic cells and lymphocytes, as well as neutrophils abscesses. These changes were non-diagnostic but raised the possibility of a pyoderma gangrenosum [Fig. 3].
Figure 3.
Histopathology of a lesion. Skin with ulceration, giant cells, plasmatic cells and lymphocytes, as well as neutrophils abscesses.
Aerobic, anaerobic and fungal cultures were negative.
The patient had normal baseline chest radiography before infliximab therapy. Chest radiography was not repeated thereafter.
Methylprednisolone was administered at a dose of 100 mg IV tbd, for 5 days. At day three oral prednisolone was initiated at 1 mg/kg/d and topical tacrolimus 0,1% twice a day was introduced. Slow improvement of the ulcers, except the peristomal lesion, was observed.
The patient was discharged with topical tacrolimus 0,1% bid and oral prednisolone (1mg/kg/day). Two months later the skin ulcers continue to improve and prednisolone was tapered 5 mg per week until was discontinued. Infliximab therapy was continued. After an observation period of 7 months the patient developed a fatal sepsis.
Discussion
Pyoderma gangrenosum (PG), is a rare inflammatory disease of unknown etiology.[1–4] Although in about 40% of cases a systemic disease is not detectable (idiopathic PG), more than half of cases are associated with systemic disease, especially inflammatory bowel disease, either ulcerative colitis or Crohn disease.[5] Other diseases that have been associated with pyoderma gangrenosum are: rheumatoid arthritis, seronegative polyarthritis, myelocytic leukaemias, hairy cell leukaemia, myelofibrosis, myeloid metaplasia; monoclonal gamopathy. Rarely reported associations include spondylitis, osteoarthritis, psoriatic arthritis, chronic active hepatitis, hepatitis C viral infection, primary bliary cirrhosis, myeloma, polycythemia rubra vera, paroxysmal nocturnal haemoglobinuria, lymphomas, systemic lupus erythematosus; C7 complement deficiency, hypogammalgobulinaemia, hyperimmunoglobulin E syndrome. HIV infection, sarcoidosis, Takayasu's arteritis, hidradenitis suppurativa, acne conglobata, solid tumours and chronic obstructive pulmonary disease iatrogenic immunesuppression, malignancy, Grave's disease or primary antiphospholipid syndrome.[4–7]
Cutaneous lesions of PG are classified according to their morphology (ulcerative, bullous, pustular and vegetant). Even though one variant predominates, some patients could present with more than one type (frequently pustular and ulcerative PG).[1–4] Frequently, clinical presentation of PG is variable and does not have a histological pathognomonic finding.[3,4]
Peristomal PG could be considered a variant of PG, found around colostomies. This variant was first described by O'Loughlin and Perry, as characterized by multiple sterile pustules surrounded by an erythematous halo and accompanied by with fever and arthralgias.[8] Since then, multiple cases have been reported.[2,9–11] Lyon et al estimated that the incidence of peristomal PG is 0.6% among all patients will colostomies.[10] Poritz et al[11] observed that peristomal PG occurs an average of 18.4+/-7.5 months after stoma creation. The majority of cases reported have occurred in patients with inflammatory bowel disease, particularly Crohn's disease, probably because these patients require more frequently colostomies.[11] This variant of pyoderma gangrenosum, in addition to pain and discomfort related to ulceration, impairs patient's social live due to related to weakened adhesion of the stomal appliance and leakage of faeces. In our case peristomal pyoderma gangrenosum was accompanied by widespread lesion in various locations.
There are no unified guidelines for an uniformly effective treatment for pyoderma gangrenosum.[11,12] Drugs being used in therapy of pyoderma gangrenosum include systemic corticosteroids, and immunosuppressive drugs, such as cyclosporine, azathioprine, cyclophosphamide, chlorambucil, cyclosporin, tacrolimus, mycophenolate mofetil, methotrexate and cyclophosphamide or intravenous immunoglobulins. Pyoderma gangrenosum can respond to sulfones (sulfasalazine or dapsone), clofazimine, and wide spectrum antiobiotics, including minocycline and rifampicin.[11,12]
Recently anti-TNF-alpha biological drugs have widened the therapeutic options for several diseases, including inflammatory bowel disease, rheumatoid arthritis, psoriatic arthritis and psoriasis. There are several case reports and randomized trials demonstrating a favorable response to anti-TNF-alpha drugs infliximab[12-18] etanercept[19–22] and adalimumab[23–26] used in pyoderma gangrenosum, associated with inflammatory bowel diseases or applied offlabel in idiopatic PG.
Although there is generally a good response to therapy in general and particularly to anti-TNF-alpha biological drugs in most cases of pyoderma gangrenosum,[12] peristomal PG remains difficult to treat. Poritz et al[11] carried out a retrospective study (1997-2007), identifying 16 patients with peristomal PG, of whom 6 received infliximab, being effective just in two of them. Single case reports of favorable course of persomal PG treated with another anti-TNF-alpha drug, adalimumab, were published in 2009.[23,24]
In our case infliximab therapy was applied for inflammainflammatory bowel disease. Development of pyoderma gangrenosum six moths after therapy introduction must be considered a paradox reaction. Lesions had a wide distribution, including trunk, abdomen, genitalia, gluteus, extremities, left preauricular region and peristomal area. The presence of peristomal PG in this patient may contribute to the general observation that this a variant of PG, which requires an individual therapeutic approach.
In these patients, constant trauma generated by the colostomy may be a contributing factor to the development and persistence of pyoderma gangrenosum. The best PG treatment in these cases would be the closure of the colostomy, yet this is not always possible. Thus, peristomal PG, usually do not show a good response to therapy.[11]
It may be hypothesized that in our patient the development of pyoderma gangrenosum despite infliximab therapy may reflect the severity of the intestinal disease, or the opposite, and less probable, it is an adverse effect of the drug.
More data are needed to determine the efficacy and safety of these anti-TNF-alpha agents, especially in patients with a colostomy.
References
- Powell FC, Hacket CH. Pyoderma gangrenosum, in Fitzpatrick's. Dermatology in General Medicine. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ (eds) New York: McGraw Hill; 2008. pp. 296–302. [Google Scholar]
- Ruocco E, Sangiuliano S, Gravina AG, Miranda A, Nicoletti G. Pyoderma gangrenosum: an updated review. J Eur Acad Dermatol Venereol. 2009;23:1008–1017. doi: 10.1111/j.1468-3083.2009.03199.x. [DOI] [PubMed] [Google Scholar]
- Wollina U. Pyoderma gangrenosum - a review. Orphanet J Rare Dis. 2007;2:19. doi: 10.1186/1750-1172-2-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callen JP, Jackson JM. Pyoderma gangrenosum: an update. Rheum Dis Clin North Am. 2007;33:787–802. doi: 10.1016/j.rdc.2007.07.016. [DOI] [PubMed] [Google Scholar]
- Feliciani C, De Simone C, Amerio P. Dermatological signs during inflammatory bowel diseases. Eur Rev Med Pharmacol Sci. 2009;13 Suppl 1:15–21. [PubMed] [Google Scholar]
- Reguiaï Z, Grange F. The role of anti-tumor necrosis factor-alpha therapy in Pyoderma gangrenosum associated with inflammatory bowel disease. Am J Clin Dermatol. 2007;8:67–77. doi: 10.2165/00128071-200708020-00002. [DOI] [PubMed] [Google Scholar]
- Masatlioğlu SP, Göktay F, Mansur AT, Akkaya AD, Güneş P. Systemic lupus erythematosus presenting as pyoderma gangrenosum in two cases. Rheumatol Int. 2009;29:837–840. doi: 10.1007/s00296-008-0791-5. [DOI] [PubMed] [Google Scholar]
- O'Loughlin S, Perry HO. A diffuse pustular eruption associated with ulcerative colitis. Arch Dermatol. 1978;114:1061–1064. [PubMed] [Google Scholar]
- McGarity WC, Robertson DB, McKeown PP, Amerson JR, Darden WA. Pyoderma gangrenosum at the parastomal site in patients with Crohn's disease. Arch Surg. 1984;119:1186–1188. doi: 10.1001/archsurg.1984.01390220064014. [DOI] [PubMed] [Google Scholar]
- Lyon CC, Smith AJ, Beck MH, Wong GA, Griffiths CE. Parastomal pyoderma gangrenosum: clinical features and management. J Am Acad Dermatol. 2000;42:992–1002. [PubMed] [Google Scholar]
- Poritz LS, Lebo MA, Bobb AD, Ardell CM, Koltun WA. Management of peristomal pyoderma gangrenosum. J Am Coll Surg. 2008;206:311–315. doi: 10.1016/j.jamcollsurg.2007.07.023. [DOI] [PubMed] [Google Scholar]
- Reichrath J, Bens G, Bonowitz A, Tilgen W. Treatment recommendations for pyoderma gangrenosum: an evidence-based review of the literature based on more than 350 patients. J Am Acad Dermatol. 2005;53:273–283. doi: 10.1016/j.jaad.2004.10.006. [DOI] [PubMed] [Google Scholar]
- Swale VJ, Saha M, Kapur N, Hoffbrand AV, Rustin MH. Pyoderma gangrenosum outside the context of inflammatory bowel disease treated successfully with infliximab. Clin Exp Dermatol. 2005;30:134–136. doi: 10.1111/j.1365-2230.2004.01681.x. [DOI] [PubMed] [Google Scholar]
- Singh M, Andrew SM, Lear JT. Infliximab as a treatment for recalcitrant pyoderma gangrenosum. Clin Exp Dermatol. 2004;29:196–197. doi: 10.1111/j.1365-2230.2004.01470.x. [DOI] [PubMed] [Google Scholar]
- Brooklyn TN, Dunnill MG, Shetty A, Bowden JJ, Williams JD, Griffiths CE, Forbes A, Greenwood R, Probert CS. Infliximab for the treatment of pyoderma gangrenosum: a randomised, double blind, placebo controlled trial. Gut. 2006;55:505–509. doi: 10.1136/gut.2005.074815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajan N, Das S, Taylor A, Abinun M, Spencer D, Carmichael A. Idiopathic infantile pyoderma gangrenosum with stridor responsive to infliximab. Pediatr Dermatol. 2009;26:65–69. doi: 10.1111/j.1525-1470.2008.00825.x. [DOI] [PubMed] [Google Scholar]
- Marzano AV, Tourlaki A, Alessi E, Caputo R. Widespread idiopathic pyoderma gangrenosum evolved from ulcerative to vegetative type: a 10-year history with a recent response to infliximab. Clin Exp Dermatol. 2008;33:156–159. doi: 10.1111/j.1365-2230.2007.02607.x. [DOI] [PubMed] [Google Scholar]
- Juillerat P, Christen-Zäch S, Troillet FX, Gallot-Lavallée S, Pannizzon RG, Michetti P. Infliximab for the treatment of disseminated pyoderma gangrenosum associated with ulcerative colitis. Case report and literature review. Dermatology. 2007;215:245–251. doi: 10.1159/000106584. [DOI] [PubMed] [Google Scholar]
- McGowan JW 4th, Johnson CA, Lynn A. Treatment of pyoderma gangrenosum with etanercept. J Drugs Dermatol. 2004;3:441–444. [PubMed] [Google Scholar]
- Rogge FJ, Pacifico M, Kang N. Treatment of pyoderma gangrenosum with the anti-TNFalpha drug - Etanercept. J Plast Reconstr Aesthet Surg. 2008;61:431–433. doi: 10.1016/j.bjps.2006.11.011. [DOI] [PubMed] [Google Scholar]
- Charles CA, Leon A, Banta MR, Kirsner RS. Etanercept for the treatment of refractory pyoderma gangrenosum: a brief series. Int J Dermatol. 2007;46:1095–1099. doi: 10.1111/j.1365-4632.2007.03286.x. [DOI] [PubMed] [Google Scholar]
- Ducharme E, Weinberg JM. Etanercept. Expert Opin Biol Ther. 2008;8:491–502. doi: 10.1517/14712598.8.4.491. [DOI] [PubMed] [Google Scholar]
- Hubbard VG, Friedmann AC, Goldsmith P. Systemic pyoderma gangrenosum responding to infliximab and adalimumab. Br J Dermatol. 2005;152:1059–1061. doi: 10.1111/j.1365-2133.2005.06467.x. [DOI] [PubMed] [Google Scholar]
- Traczewski P, Rudnicka L. Adalimumab in dermatology. Br J Clin Pharmacol. 2008;66:618–625. doi: 10.1111/j.1365-2125.2008.03263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zold E, Nagy A, Devenyi K, Zeher M, Barta Z. Successful use of adalimumab for treating fistulizing Crohn's disease with pyoderma gangrenosum: Two birds with one stone. World J Gastroenterol. 2009;15:2293–2295. doi: 10.3748/wjg.15.2293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkhouri N, Hupertz V, Mahajan L. Adalimumab treatment for peristomal pyoderma gangrenosum associated with Crohn's disease. Inflamm Bowel Dis. 2009;15:803–806. doi: 10.1002/ibd.20748. [DOI] [PubMed] [Google Scholar]