Abstract
Background
Psoriasis is a frequently occurring disorder with a chronic and relapsing course. Common sites of involvement are the extremities, trunk, scalp and nails. The disease may occasionally involve genitalia and the anus. Although cutaneous lesions are generally sufficiently distinct to make a diagnosis, diagnostic difficulties can be found in cases of unusual involvement.
Main observations
We report a 38-year-old man who presented scaling and cracking of the lips without intraoral involvement as a first manifestation of psoriasis. Three years later he developed erythematous plaques with desquamation on fingers, characteristic of psoriasis.
Conclusion
Psoriasis should be considered in the differential diagnosis of chronic or recurrent labial lesions.
Keywords: cheilitis, diagnosis, lips, oral mucosa, psoriasis
Introduction
Psoriasis is a frequently occurring disorder with a chronic and relapsing course, which affects both sexes equally. Psoriasis is more prevalent in caucasians with fifty percent of cases appearing before the second decade of life. Common sites of involvement are the extremities, trunk, scalp and nails. The disease may occasionally involve genitalia and the anus. Although cutaneous lesions are generally sufficiently distinct to make a diagnosis, diagnostic difficulties can be found in cases of unusual involvement. We report a 38-year-old man who presented psoriasis of the lips without intraoral involvement as a first manifestation of psoriasis.
Case Report
A 38-year-old man presented with a 3-year history of scaling and cracking of the lips. The lesions eventually involved both lips completely, but the surrounding skin remained uninvolved during this period. It was associated with discomfort, aggravated by lip microinjuries and intake of citrus fruits. The patient was receiving treatment in the form of ointment base without any improvement. There was no personal or family history of psoriasis or any other dermatological conditions, and no history of smoking. He was working as a construction worker.
Dermatological examination revealed diffuse mild erythema, adherent silvery scales and fissuring on upper lip, extending beyond the vermillion border. The upper lip was slightly swollen [Fig. 1A]. The remaining oral mucosa and surrounding skin appeared normal. His clinical course was quite chronic with exacerbations and spontaneous remissions. He denied any history of contact with lipstick, topical antibiotics or other cosmetics. Moreover, there were erythematous plaques with desquamation on some fingers of the hands that had been present for about 4 months [Fig. 2]. The remaining skin, hair and mucous membranes were spared.
Figure 1.
Erythema and scaling of the lips, extending beyond vermillion border before (A) and after (B) treatment.
Figure 2.
Erythematous plaques with desquamation on some fingers of the hands.
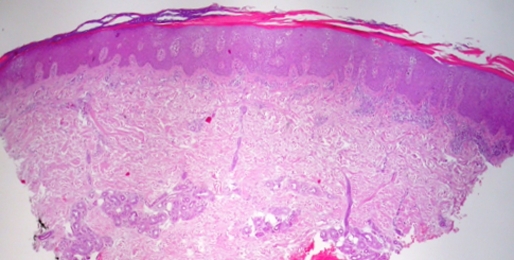
Routine laboratory examinations were normal. Patch test with the GEIDAC standard series (by True Test, Mekos Laboratories ApS, Hillerad, Denmark) was negative. Serological tests were negative. Incisional biopsy was taken from the second finger of the left hand and it revealed epithelial hyperplasia, elongation of rete ridges and compact hyperkeratosis. The epithelium was thin over the connective tissue papillae and there was mild lymphocytic infiltrate noted in the upper dermis [Fig. 3]. The features indicated psoriasis. The patient gave no consent to a biopsy from the lip.
Figure 3.
Epithelial hyperplasia, elongation of rete ridges and compact hyperkeratosis. The epithelium was thin over the connective tissue papillae and there was mild lymphocytic infiltrate noted in the upper dermis. (HE, X 40).
An emolient cream and a momethasone fuorate 0.1% ointment once daily for 14 days was prescribed. The lesions on the lips cleared by the end of the second week and topical steroid treatment was stopped [Fig. 1B]. The lesions on the fingers also improved with this treatment.
During the follow-up, the patient presented several exacerbations of skin lesions coexisting with labial lesions that had good response to calcipotriene.
Discussion
Perioral psoriasis without intraoral involvement has been rarely reported in the literature, there have only been six reported cases, five with associated skin lesions[1–7] [Table 1]. Mild trauma or cheilitis can lead to psoriatic lesions on the lips, especially in a genetically predisposed individual. It runs a chronic course and is associated with moderate to severe discomfort especially in daily activities, such as eating and mastication[1].
Table 1.
| Sex | Age (years) | Clinical features on the lips | Skin lesions (yes/no) | Remaining oral mucosa | Treatment on the lips | Response tothe treatment | |
|---|---|---|---|---|---|---|---|
| Rahman et al1 | woman | 20 | Scaly white lesions for 2 years | Yes | Not involved | triamcinolone acetonide ointment | effective |
| Tosti et al2 | woman | 24 | Cheilitis for 1 year | No | Not involved | corticoisteroid cream | effective |
| Yamamoto et al3 | man | 65 | Silver scales | Yes | Not involved | vitamin D3 ointment | ineffective |
| Migliari et al4 | man | 13 | Erosions, fissures, yellowish scales for 4 years | No | Involved | vitamin A derivates and topical steroids | ineffective |
| Ülker et al5 | woman | 45 | Desquamation for 5 years | Yes | Not involved | metotrexate | effective |
| Ersoy-Evans et al6 | woman | 19 | Fissuring and cracking for 8 years | Yes | Not involved | fluticasone propionate 0.005% ointment | effective |
| Baz et al7 | woman | 22 | Scaling and cracking for 5 years | Yes | Not involved | mometasone fuorate 0.1% ointment | effective |
| our case | man | 38 | Scaling and cracking for 3 years | Yes | Not involved | mometasone fuorate 0.1% ointment and calcipotriene | effective |
Brenner et al[8] reported a case with lip psoriasis, which was triggered by protunding teeth. Their case did not clear with any type of dermatological treatments including topical corticosteroids and calcipotriol, however, the lesions on the lips completely resolved after replacement of the protruding teeth by a non-irritating prosthesis.
Psoriasis of the lips can be the sole presentation of psoriasis, preceding the appearance of typical psoriasis lesions by several years. Actinic dermatitis, cheilitis, chronic candidiasis, chronic eczema and leucoplakia can all be confused with perioral psoriasis. Reiter's syndrome, histologically similar to psoriasis must be excluded. In this case it was excluded as the patient had none of the other triad of symptoms associated with this syndrome.
Psoriasis of the lips, although rare, does occur and the diagnosis is best made when the clinical course of the oral lesions parallels that of skin lesions and is supported by histological examination[4,7]. Some additional criteria for the diagnosis of oral psoriasis such as a positive family history and human leucocyte antigen (HLA) typing have also been considered important in supporting a diagnosis of oral psoriasis. Some features such as the chronicity and clinical appearance of the lesions characterized by silvery scales also suggested a diagnosis of isolated lip psoriasis.
Therefore, in a long-standing eczema-like eruption occurring on the lips, psoriasis should be suspected in the differential diagnosis and a biopsy should be taken in case no response to treatment occurs. Dermoscopy may provide significant additional information in patients who do not give consent to invasive diagnostic techniques.
Our case is interesting, as it indicates that psoriasis can manifest with sole involvement of the lips for a long time. Therefore, psoriasis should be considered in the differential diagnosis of chronic or recurrent, treatment-resistant labial lesions, even in the absence of accompanying skin lesions or a positive family history.
References
- Rahman MA, Fikree M. Perioral psoriasis. J Eur Acad Dermatol Venereol. 2000;14:521–522. doi: 10.1046/j.1468-3083.2000.00170-7.x. [DOI] [PubMed] [Google Scholar]
- Tosti A, Misciali C, Cameli N, Vincenzi C. Guess what! Psoriasis of the lips. Eur J Dermatol. 2001;11:589–590. [PubMed] [Google Scholar]
- Yamamoto T, Nishioka K. Oral psoriasis in a patient with hepatitis C virus infection. Eur J Dermatol. 2002;12:75–76. [PubMed] [Google Scholar]
- Migliari DA, Penha SS, Marques MM, Matthews RW. Considerations on the diagnosis of oral psoriasis: a case report. Med Oral. 2004;9:300–303. [PubMed] [Google Scholar]
- Gül U, Kiliç A, Gönül M, Soylu S, Bilgili S, Han O. Psoriasis of the lips: an unusual localization. Int J Dermatol. 2006;45:1381–1382. doi: 10.1111/j.1365-4632.2006.03117.x. [DOI] [PubMed] [Google Scholar]
- Ersoy-Evans S, Nuralina L, Erkin G, Ozkaya O. Psoriasis of the lips: a rare entity. J Eur Acad Dermatol Venereol. 2007;21:142–143. doi: 10.1111/j.1468-3083.2006.01824.x. [DOI] [PubMed] [Google Scholar]
- Baz K, Yazici AC, Usta A, Ikizoglu G, Apa DD. Isolated lip involvement in psoriasis. Clin Exp Dermatol. 2007;32:578–579. doi: 10.1111/j.1365-2230.2007.02445.x. [DOI] [PubMed] [Google Scholar]
- Brenner S, Lipitz R, Llie B, Krakowski A. Psoriasis of the lips: the unusual Köbner phenomenon caused by protruding upper teeth. Dermatologica. 1982;164:413–416. doi: 10.1159/000250128. [DOI] [PubMed] [Google Scholar]