Abstract
Background
Patients with locally advanced skin cancer often present an uncommon and unique treatment challenge. Surgical resection and reconstruction with an acceptable cosmetic outcome is difficult for larger lesions with deep infiltration into subcutaneous tissues. Radiation therapy has been shown to be an effective treatment modality for advanced non-melanoma skin cancers, with cure rates ranging 50-100%. In this case report, we discuss the efficacy and outcome of treatment using an advanced radiation therapy technique to a large T4 squamous cell carcinoma of the face.
Main observations
The patient responded favorably to the advanced radiation treatment course, and achieved a clinical complete response to therapy. No further intervention was required. Advanced radiation therapy techniques offered treatment advantages that resulted in greater tumor dose escalation and minimizing of patient morbidity.
Conclusions
Patients with advanced skin cancers of the head and neck should be considered for definitive radiation therapy using advanced treatment techniques. The use of definitive RT only for tumors deemed unresectable, or for inoperable patients at presentation deserves reconsideration. Further investigation is warranted.
Keywords: IMRT, Moh's surgery, skin cancer, squamous cell carcinoma
Introduction
Nonmelanoma skin cancers (NMSC) are the most common of all cancers, with over one million cases diagnosed annually in the United States.[1] Basal cell carcinoma accounts for approximately 80% of all NMSC, and the remainder is mostly squamous cell carcinoma.[2] The skin of the head and neck is the most common site of presentation, accounting for more than 80% of all NMSC.[3] Treatment options for NMSC include surgical resection, cryotherapy, electrocautery, Moh's surgery, and radiation therapy.[2] Each of these modalities carries a 90-95% cure rate when used appropriately as indicated by clinical history, tumor size, histology, and location.[2] While these modalities are very efficacious, treatment approaches must be carefully considered and individualized to achieve an acceptable cosmetic and functional patient outcome.[3]
Patients with locally advanced T3 and T4 NMSC often present an uncommon and unique treatment challenge.[4] Surgical resection and reconstruction with an acceptable cosmetic outcome is difficult for larger lesions with deep infiltration into subcutaneous tissues.[3] At initial presentation, many large and some relatively small skin lesions are more deeply infiltrating than clinically and / or radiographically perceived.[3] When performing Moh's surgery to remove these lesions, the surgeon is required to perform a more extensive resection requiring reconstruction. Large lesions that are determined radiographically and / or clinically to be intimately involved with critical structures or in close proximity to normal anatomic structures often are deemed unresectable at presentation. When attempted, cosmetic outcomes are sometimes unfavorable and often complete resection with negative margins is unachievable.
Radiation therapy has been shown to be an effective treatment modality for advanced NMSC, with cure rates ranging 50-100%.[5,6] Advantages of radiation therapy as opposed to surgery include: sparing the patients from the adverse cosmetic outcomes associated with extensive surgery, it is a safe treatment for patients determined to be poor operative candidates, and it offers patients relatively equivalent cure rates to surgery.[2,3]
In this case report, we discuss the efficacy and outcome of treatment with definitive radiation therapy to a large T4 squamous cell carcinoma of the face.
Case Report
An 88-year-old gentleman with a history of multiple skin cancers presented to his primary care physician for evaluation of a large malodorous mass with central necrosis present on the right side of his face. Figure 1 shows the patient at initial presentation. He reported that the mass had begun as a small pimple approximately 18 months prior, and slowly continued to enlarge to its measured size of 8 cm x 8 cm at presentation. He reported that the mass ruptured and began to rapidly expand in the 3-4 months prior to evaluation. Two other lesions on his right forehead were also noted at initial presentation. Biopsies were performed on all three lesions and the results showed basal cell carcinoma involving the two lesions on the forehead, and squamous cell carcinoma involving the cheek.
Figure 1.

Patient at initial presentation.
The patient was referred to dermatology with plans to consult head and neck surgery, and plastic / reconstructive surgery. Due to the patient's age and presence of multiple chronic medical conditions, he was determined to be a poor operative candidate. Furthermore, evaluation of the size of the lesion and the presence of squamous cell histology caused concern that complete resection with reconstruction would be very difficult. He was then referred to radiation oncology to consider palliative treatment.
The patient accepted radiation therapy treatment, and was treated with intensity modulated radiation therapy (IMRT) to the right cheek lesion. The two basal cell carcinomas on the forehead were treated with electron therapy. Treatment planning was carried out by using three dimensional CT reconstruction for advanced radiation planning techniques of the large T4 lesion, and by electron planning for the two basal cell carcinomas of the forehead.
The patient was treated using a simultaneous integrated boost planning technique. The outer contour (PTV1) covered the gross tumor volume and was treated to a total dose of 7425 cGy at 225 cGy per daily fraction. The inner contour (PTV2) covered the clinically determined high risk region which was estimated to be 2.0-3.0 cm for tumor microscopic local invasion, and was treated to a total dose 5940 cGy at 180 cGy per daily fraction. The treatment plan had to be modified during therapy due to tumor shrinkage after 25 fractions.
Treatment was administered with the use of a Varian linear accelerator (Varian Medical Systems, Palo Alto, California) using 6 MV photon beams. A thermoplastic mask was used for patient immobilization. Treatment planning with the use of five static coplanar beams was performed using Eclipse planning software. A 5 mm thick bolus was applied to the skin surface to allow better surface dose distribution to the superficial extent of the lesion. The contralateral parotid was held to a mean dose of 1020 cGy, all optic structures were held under 1100 cGy, and the mandible was held to a mean dose of 2500 cGy.
The two forehead basal cell carcinomas were treated with 6 MeV electrons to a total dose 6075 cGy at 225 cGy per daily fraction. Custom designed cutouts using cerrobend casting were used to design the treatment port. A 5 mm thick wet bolus was applied to both lesions daily for treatment.
In addition to radiation therapy, an aggressive wound debridement plan was initiated to facilitate sloughing and removal of necrotic tissue during treatment. Frequent and often daily nursing care was provided to assist in this process.
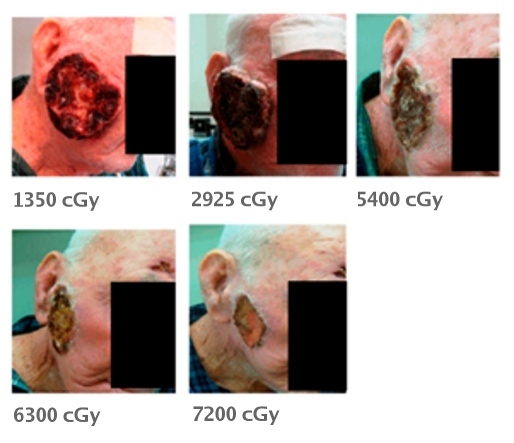
The patient responded favorably to the radiation treatment course and necrotic tissue debridement. Figure 2 illustrates the tumor response in correlation to treatment dose. The patient tolerated therapy well and did not require any treatment break for acute reaction complications. No infections or wound complications occurred.
Figure 2.
Tumor response of the lesion correlated with dose received.
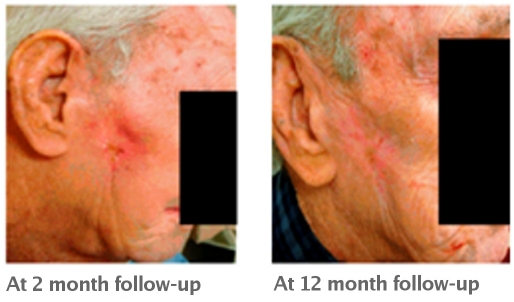
Figure 3 shows the patient at follow-up. The patient achieved a complete response of all lesions to definitive radiation therapy and has had complete resolution of acute treatment reactions. Long term complications are noted as some increased scarring over the lesion areas and hypopigmentation of the skin over the treatment areas. The patient has not experienced significant xerostomia, nor has he developed cataracts. The patient is now at 16 months follow-up without evidence of tumor recurrence.
Figure 3.
Patient at follow-up.
Discussion
Patients with locally advanced NMSC present a unique and challenging situation for achievement of optimal treatment outcomes. Treatment approaches must be individualized to each patient with consideration to patient age, tumor location, tumor histology, patient concerns for morbidity and cosmetic outcome, and likelihood of tumor control based on the modality selected. Therefore, a multidisciplinary effort for such patients is likely the best approach.
Radiation therapy and Moh's surgery with reconstruction are the preferred techniques for patients presenting with high risk features of recurrence or locally advanced disease. Previous reports have reviewed the use of radiation therapy versus surgery for carcinoma involving the face.[7,8] The outcomes of this study[7] showed a more favorable cosmesis and tumor control following surgery. Radiation techniques in this trial have been criticized as these patients were treated prior to the development of newer radiation techniques, and many patients received brachytherapy with high dose fractionation. High dose fractionation has been shown to cause more adverse long term cosmetic outcomes. Follow-up conclusions supported excellent local control outcomes for NMSC of the face with surgery or radiation therapy.[8] In regards to locally advanced NMSC of the face, previous reports showed that radiation therapy can achieve local control rates of approximately 53% at five years, and that primary untreated lesions fared better than recurrent lesions of either histology.[6,9] This report[9] also indicated that radiation therapy also allowed more normal tissue sparing when compared to surgery.
Despite the limited evidence in the literature pertaining to locally advanced, non-metastatic NMSC of the head and neck, the use of radiation therapy should be considered for all patient presentations. Newer radiation techniques including IMRT have been proven to allow greater dose escalation to tumor volumes with decreased normal tissue toxicity. As a result the therapeutic index will be further increased allowing improved local control rates while decreasing patient long term morbidity. As highlighted in this report, many patients due to tumor characteristics or comorbidities are unresectable, and if attempted would likely achieve a poor cosmetic outcome. Radiation therapy for this patient was an appropriate successful treatment approach and as such should be considered for other patients. Further research is needed to investigate the use of advanced radiation planning techniques such as IMRT in the treatment of advanced NMSC.
Conclusion
Patients with advanced NMSC of the head and neck should be considered for definitive radiation therapy. Advanced radiation therapy techniques offer greater dose escalation to tumor volumes while decreasing patient long term morbidity. As such, local control rates will likely be improved by the use of these advanced techniques and offer patients equivalent or superior disease control and less morbidity as opposed to surgery. The use of definitive RT only for tumors deemed unresectable, or for inoperable patients at presentation deserves reconsideration. Further investigation is warranted.
References
- Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin. 2009;59:225–249. doi: 10.3322/caac.20006. [DOI] [PubMed] [Google Scholar]
- Halperin EC, Perez CA, Brady LW. Perez and Brady's principles and practice of radiation oncology. 5th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008. [Google Scholar]
- Harrison LB, Sessions RB, Hong WK. Head and neck cancer: a multidisciplinary approach. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2009. [Google Scholar]
- Mendenhall WM, Parsons JT, Mendenhall NP, Million RR. T2-T4 carcinoma of the skin of the head and neck treated with radical irradiation. Int J Radiat Oncol Biol Phys. 1987;13:975–981. doi: 10.1016/0360-3016(87)90034-4. [DOI] [PubMed] [Google Scholar]
- Locke J, Karimpour S, Young G, Lockett MA, Perez CA. Radiotherapy for epithelial skin cancer. Int J Radiat Oncol Biol Phys. 2001;51:748–755. doi: 10.1016/s0360-3016(01)01656-x. [DOI] [PubMed] [Google Scholar]
- Al-Othman MO, Mendenhall WM, Amdur RJ. Radiotherapy alone for clinical T4 skin carcinoma of the head and neck with surgery reserved for salvage. Am J Otolaryngol. 2001;22:387–390. doi: 10.1053/ajot.2001.28083. [DOI] [PubMed] [Google Scholar]
- Leshin B, Yeatts P, Anscher M, Montano G, Dutton JJ. Management of periocular basal cell carcinoma: Mohs' micrographic surgery versus radiotherapy. Surv Ophthalmol. 1993;38:193–212. doi: 10.1016/0039-6257(93)90101-c. [DOI] [PubMed] [Google Scholar]
- Petit JY, Avril MF, Margulis A, Chassagne D, Gerbaulet A, Duvillard P, Auperin A, Rietjens M. Evaluation of cosmetic results of a randomized trial comparing surgery and radiotherapy in the treatment of basal cell carcinoma of the face. Plast Reconstr Surg. 2000;105:2544–2551. doi: 10.1097/00006534-200006000-00039. [DOI] [PubMed] [Google Scholar]
- Lee WR, Mendenhall WM, Parsons JT, Million RR. Radical radiotherapy for T4 carcinoma of the skin of the head and neck: a multivariate analysis. Head Neck. 1993;15:320–324. doi: 10.1002/hed.2880150409. [DOI] [PubMed] [Google Scholar]