ABSTRACT
Purpose: Rehabilitation costs for spinal-cord injury (SCI) are increasingly borne by Canada's private health system. Because of poor outcomes, payers are questioning the value of their expenditures, but there is a paucity of data informing analysis of rehabilitation costs and outcomes. This study evaluated the feasibility of using administrative claim file review to extract rehabilitation payment data and functional status for a sample of persons with work-related SCI.
Methods: Researchers reviewed 28 administrative e-claim files for persons who sustained a work-related SCI between 1996 and 2000. Payment data were extracted for physical therapy (PT), occupational therapy (OT), and psychology services. Functional Independence Measure (FIM) scores were targeted as a surrogate measure for functional outcome. Feasibility was tested using an existing approach for evaluating health services data.
Results: The process of administrative e-claim file review was not practical for extraction of the targeted data.
Conclusions: While administrative claim files contain some rehabilitation payment and outcome data, in their present form the data are not suitable to inform rehabilitation services research. A new strategy to standardize collection, recording, and sharing of data in the rehabilitation industry should be explored as a means of promoting best practices.
Key Words: occupational therapy, outcomes, outpatient, physical therapy, psychology, rehabilitation, spinal-cord injury
RÉSUMÉ
Objectif : Les coûts de la réadaptation à la suite d'une lésion à la moelle épinière sont de plus en plus pris en charge par le système de santé privé au Canada. En raison des faibles résultats obtenus, les payeurs s'interrogent sur la pertinence de cette dépense, mais il existe peu de données pour alimenter une réelle analyse des coûts et des résultats en réadaptation. Cette étude s'est penchée sur la faisabilité du recours à un examen des dossiers administratifs de réclamations pour l'extraction de données relatives aux sommes consacrées à la réadaptation et au statut fonctionnel des personnes ayant subi une lésion à la moelle épinière de nature professionnelle.
Méthode : Les chercheurs ont étudié 28 dossiers électroniques de réclamation de personnes ayant subi une lésion à la moelle épinière dans le cadre de leur travail entre 1996 et 2000. Des données sur le paiement ont été extraites pour les services de physiothérapie (PT), d'ergothérapie (OT) et de psychologie. Les mesures de l'indépendance fonctionnelle étaient visées et ont été utilisées comme mesure auxiliaire des résultats sur le plan fonctionnel. La faisabilité a été évaluée à l'aide d'une approche existante pour évaluer les données sur les services de santé.
Résultats : L'examen des dossiers administratifs électroniques de réclamations ne constitue pas une méthode pratique pour l'extraction des données visées par cette étude.
Conclusions : Malgré le fait que les dossiers administratifs de réclamation contiennent des données sur le paiement et les résultats de la réadaptation, ces données, dans leur forme actuelle, ne peuvent être utilisées pour la recherche sur les services de réadaptation. Une nouvelle stratégie visant à normaliser la collecte, la consignation et le partage des données dans l'industrie de la réadaptation devrait être envisagée comme moyen de favoriser des pratiques exemplaires.
Mots clés : ergothérapie, lésion à la moelle épinière, paiement, patient externe, physiothérapie, psychologie, réadaptation, résultats
INTRODUCTION
It has been estimated that in 2007, total health care costs (costs of hospital, medical supplies, practitioner support services, wheelchairs, personal assistance and home care, and vehicle modification) for traumatic spinal-cord injury (SCI) in Canada were almost $2 billion, in addition to the direct impact of lost wages associated with disability, estimated to exceed $184 million.1 In-patient care accounts for about 70% of total SCI health costs, while the remaining 30% is delivered through non-institutionalized care such as outpatient rehabilitation, funded in large part by private payers.2–4
A variety of health professionals, including physical therapists, occupational therapists, and psychologists, deliver rehabilitation in a variety of settings, and they are paid by a variety of payers.5 Much outpatient SCI rehabilitation takes place in the privately funded health system, where regulations for standard data recording and collection do not exist—a situation that is of concern to Canadian health researchers.6,7 Furthermore, care is often fragmented and lacks coordination.8,9 In Canada, as in other jurisdictions, pressure is growing to understand the relationship between rehabilitation, its costs, and its outcomes in order to support sound decision making and rationing of care.10,11
Little is known about the cost utility of outpatient physical therapy (PT), occupational therapy (OT), and psychology services in Canada. Nevertheless, persons with SCI routinely receive such services, particularly because of increasingly shorter lengths of stay for in-patient rehabilitation.12,13 There is some evidence that the cost of or the lack of funding for outpatient PT and OT services is a barrier to access to or satisfaction with health services for this population.14–16 There is also evidence from other jurisdictions that availability of PT, OT, and psychology services may promote recovery of motor and psychological function and, ultimately, translate into meaningful function and greater independence.17–24
Unlike the public health care sector, the private health care environment is characterized by multiple payers as well as multiple rehabilitation providers.4,25 Consequently, there is no single health database that captures private health interventions, costs, and outcomes. Administrative data does exist in the private health care sector, consisting of “claims filed with private or public payers, records maintained by managed care organizations (of visits, procedures, tests, etc.) or reports of hospitalization to state agencies.”26(p.164) There are known limitations to administrative data, related to the fact that such data are usually collected not to answer specific research questions but, rather, for billing and accounting purposes.27–32 On the other hand, administrative data have been used successfully to monitor service delivery and costs in some health programmes.33–38 A key advantage of administrative data over payment databases has been that they contain data from medical records, which some consider the gold standard for extraction of health, utilization, and outcome data.39
In the private health care environment, currently available data are not sufficient for payers to make informed decisions about rehabilitation services delivered to persons with SCI. For example, a therapist may prescribe treatment such as functional standing and walking programmes. Although such programmes have been shown in the literature to have beneficial health effects for patients with SCI,40 we do not have Canadian evidence to demonstrate their utility. Insurers may therefore refuse to pay for these interventions as a result of unfamiliarity with the interventions and their effectiveness. Some insurers may also exercise rationing. If there is a cap on the total amount of funding to which injured persons have access, the insurer may deny payment to preserve funds for future needs that the adjuster may consider more essential.a Rationing of health dollars by a payer may be subjective, or it may be based on predictions of future needs by treating health professionals or consultants. This time trade-off for services has not been investigated in SCI and is largely based on provider/payer opinions. As changes to payment mechanisms are considered by payers or governments, consideration must also be given to the possibility that such changes may alter the incentives of privately funded rehabilitation providers and thus, indirectly, the organization, availability, and accessibility of outpatient rehabilitation services. The consequences of such changes for Canada's outpatient rehabilitation environment are unknown, and this uncertainty underscores the need for research into outpatient rehabilitation, particularly for specific populations such as persons with SCI.
This study explores the feasibility of using administrative claim files as a data source for rehabilitation research. The SCI population was chosen for this research because SCI typically leads to significant rehabilitation costs and because, despite advances in acute medical and rehabilitative care, Canadians with SCI participate in the workforce in significantly smaller numbers than their counterparts without SCI,2,41 which makes the insights gained relevant to redesigning the vocational rehabilitation approach.
The objective of this study was to evaluate a process called e-claim file review. The evaluation was undertaken to determine whether the process is feasible for extracting meaningful payment data for PT, OT, and psychology services, as well as Functional Independence Measure (FIM) scores, from individual e-claim files compiled by the Workplace Safety and Insurance Board (WSIB) of Ontario.
METHODS
Sample
WSIB identified all claimants with work-related SCI that occurred in the 5-year period between January 1, 1996, and December 31, 2000. The sample consists of 28 SCI claims from a total of 506,956 WSIB lost-time claims for the same period.42,43 All claims had “aged” for at least 3 years, so that data could be collected from each e-claim file for the 3-year period after the onset of injury. This duration was chosen based on research suggesting that several years are required for patients to adjust to injury after SCI.44–49 Data extracted reflect an 8-year window from the earliest date of injury (April 1996) to December 2003, which marks 3 years after the latest date of injury (December 2000).
Inclusion criteria were as follows:
Traumatic SCI occurring in Ontario
Complete or incomplete tetraplegia or paraplegia
18 years or older at time of injury
At least 3 years post-injury at the time of data collection
SCI sustained between January 1, 1996, and December 31, 2000 (5-year period)
Claim paid by WSIB insurance for coverage of health expenses not paid by the public health system
Patient's care may have been, but was not necessarily managed as part of the WSIB Serious Injury Program
Exclusion criterion:
Prior upper motor neuron injury or degenerative condition
Data-Collection Procedure
In 1990, WSIB implemented an electronic claim file (e-claim file) system. An e-claim file was created for every injured worker eligible to make a claim. The e-claim file is comparable to a paper claim file, which contains records submitted to the payer by external parties, such as health professionals, and those generated by claims adjudicators or internal health consultants with WSIB. When paper documentation is submitted on behalf of an injured worker (claimant), the paper is scanned and converted to an image file, which is then stored as part of the e-claim file on the WSIB server. E-claim files are accessible electronically only to authorized persons.
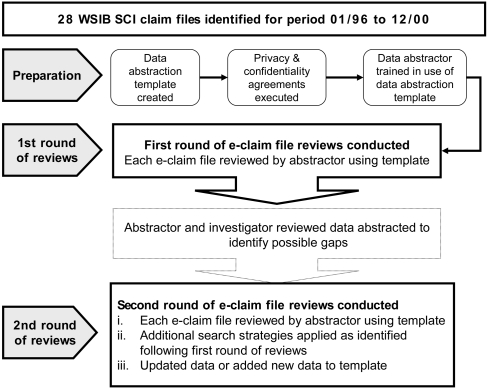
After appropriate confidentiality and privacy agreements had been executed and approval obtained from the University of Toronto Research Ethics Board, data extraction was carried out by an independent research assistant (abstractor) who had expertise with the WSIB e-claim file system and had previously worked as a serious injuryb claims adjuster. Data were extracted from each e-claim file for the 3-year period after the date of each subject's SCI. Figure 1 illustrates the flow of the e-claim file review process.
Figure 1.
Flow diagram of e-claim file review process
Note that in 2001, WSIB implemented a Provider Bill Approval System (PBAS) that permits health providers to submit invoices electronically to the WSIB Serious Injury Unit.50 There was no requirement for electronically submitted invoices to be included in the e-claim file, which means that not all such invoices will have been captured in the corresponding e-claim files; those not captured were obviously not reported by the abstractor. Unfortunately, data on the ratio of electronic versus paper submissions after 2001 are not available.
Data Extracted
Payment data have the potential to be useful in answering questions about the cost of health services; independence in personal care and other activities is a favourable outcome, and levels of independence drive health services usage and costs. The FIM, which assesses disability and caregiver burden associated with disability, is widely used as a functional assessment measure for SCI, including outpatient SCI rehabilitation research.16,51–54 At the time the e-claim files used in our study were compiled by WSIB, the FIM was routinely captured at time of discharge from publicly funded acute care and rehabilitation institutions;55 therefore, we anticipated that if the health record included a functional measure, it would most likely be the FIM. For these reasons, the FIM may be considered a surrogate measure for functional status for the purpose of examining SCI rehabilitation outcomes.
Method Used to Determine Feasibility
The feasibility of e-claim file review for data extraction was evaluated from a logistical perspective, as there was no standard procedure describing how administrative data in e-claim files should be extracted or recorded for analysis purposes. We evaluated the process of e-claim file review, as well as the data extracted, by adopting the approaches of Black et al.6 and Ardal et al.56 to describe the characteristics of quality data. Access and completeness were used as the criteria to evaluate the process of e-claim file review.
It was necessary to develop assumptions for the study, because there were no baseline data to determine typical usage patterns for outpatient rehabilitation services in the SCI population. Three factors informed the development of assumptions: (a) the administrative nature of the e-claim file, (b) the payment policies of WSIB, and (c) evidence in the SCI literature pertaining to rehabilitation services. Before data extraction began, the assumptions were reviewed for face validity by health researchers with expertise in SCI rehabilitation.
Access to the e-claim files and to payment data within e-claim files was evaluated using six sub-criteria—availability, accessibility, accommodation, affordability, acceptability, and adequacy—at both the file and the claim level (see Table 1).
Table 1.
Access Criteria and Questions to Evaluate Access to E-claim Files and Data within E-claim Files
| Evaluative Criteria | Black et al.6 | As Applied to E-claim File or to Data within E-claim File |
|---|---|---|
| 1. Availability |
|
|
| 2. Accessibility |
|
|
| 3. Accommodation |
|
|
| 4. Affordability |
|
|
| 5. Acceptability |
|
|
| 6. Adequacy |
|
|
Completeness of the payment data extracted was evaluated by comparing the predetermined assumptions for the PT, OT, and psychology payment data against the actual payment data extracted (see Table 2). It was assumed that outpatient PT and OT payment data would be present in all 28 e-claim files, but it was more difficult to make a similar assumption for outpatient psychology services. There is a substantial literature on the psychological sequelae of SCI, including depression and its influence on quality of life.17,20,22,57–59 We therefore assumed that psychology payment data would be found for at least 11% of the sample, reflecting the depression treatment rates reported in an able-bodied population.20
Table 2.
Assumptions Regarding Data-Extraction Frequencies for Payment Data by Neurological Level of Injury
| Payment Data |
Complete Tetraplegia n=2 |
Incomplete Tetraplegia n=7 |
Complete Paraplegia n=11 |
Incomplete Paraplegia n=8 |
Total n (%) |
|---|---|---|---|---|---|
| PT | 2 | 7 | 11 | 8 | 28 (100) |
| OT |
2 |
7 |
11 |
8 |
28 (100) |
| Psychology* | 3 | 3 (11%) | |||
The literature validated assumptions by level of injury for PT and OT services, but this was not possible for psychological services. The assumption regarding psychological services was based on presence of SCI and was not distinguished by level of injury.
As discussed above, collection of FIM data is mandated in Ontario for persons with SCI who receive care at publicly funded acute-care or rehabilitation hospitals with designated or specialized in-patient rehabilitation beds.13,41,60 Most persons with SCI transition from the public in-patient environment to the private outpatient health sector for treatment.2 Therefore, it was expected that FIM data might be communicated to private rehabilitation providers and/or payers to facilitate ongoing evaluation of functional status and burden of care, and particularly to justify payment for attendant care services. While we anticipated that FIM data would be retrievable from some e-claim files, we could not assume that it would be included in all files; therefore, no assumption was made with respect to the frequency of FIM data in the sample.
Once data were extracted, they were compared to the assumptions. Feasibility analysis was descriptive, and results are reported as frequency counts of extracted data against frequency counts of data assumed to be available for the SCI population.
RESULTS
The results are analyzed at three levels: access to e-claim files, access to payment data within each e-claim file, and completeness of payment data and FIM data.
It was feasible to access 28 of 28 e-claim files identified by WSIB for the 5-year time period (see Table 3).
Table 3.
Evaluation of Access to E-claim Files
| Criterion | Evaluation Rating |
|---|---|
| 1. Availability: | |
| Are researchers aware of existing e-claim files? | NE |
| Do the required e-claim files exist? | Y |
| Is it possible to use them for research? | Y |
| 2. Accessibility: | |
| Are the e-claim files physically convenient? | Y |
| 3. Accommodation: | |
| Are policies and procedures regarding access to e-claim files appropriate? | Y |
| Can the requirements be met in a timely fashion? | Y |
| 4. Affordability: | |
| Are costs to access e-claim files reasonable? | Y |
| 5. Acceptability: | |
| Do e-claim file custodians understand researcher needs? | NE |
| 6. Adequacy: | |
| Are e-claim files, as currently constructed, suitable for researcher needs? | Y |
Y=criterion met; N=criterion not met; NE=criterion not evaluated (not within scope of research)
Five of six evaluative criteria were met for access to payment data; however, the sixth criterion (adequacy) was not met, because data were not organized in a similar way across e-claim files (see Table 4).
Table 4.
Evaluation of Access to Data within E-claim Files
| Criterion | Evaluation Rating |
|---|---|
| 1. Availability: | |
| Are researchers aware of existing data? | NE |
| Do the required data exist? | Y |
| Is it possible to use them for research? | Y |
| 2. Accessibility: | |
| Are the data physically convenient? | Y |
| 3. Accommodation: | |
| Are policies and procedures regarding access to data appropriate? | Y |
| Can the requirements be met in a timely fashion? | Y |
| 4. Affordability: | |
| Are costs to access data reasonable? | Y |
| 5. Acceptability: | |
| Do data custodians understand researcher needs? | NE |
| 6. Adequacy: | |
| Are data, as currently constructed, suitable for researchers' needs? | N |
Y=criterion met; N=criterion not met; NE=criterion not evaluated (not within scope of research)
Neither the payment data nor the FIM data collected met the criterion for completeness. Of 28 e-claim files, 13 yielded no PT, OT, or psychology services payment data; within the 15 files in which payment data were found, PT services were the most frequent (10/28), followed by OT (7/28) and psychology (4/28). No FIM score data were extracted from any of the e-claim files. Data frequencies for psychology services met expectations, but frequencies for PT and OT did not. Table 5 summarizes the assumptions developed and compares them to the actual data yield for the data category. Of nine assumptions made about outpatient health services payments, only one was met. There did not appear to be a relationship between level of injury and frequency of payment data extracted; for example, payments recorded for OT, PT, and psychology were higher for persons with complete paraplegia than for persons with tetraplegia or incomplete paraplegia (see Table 6).
Table 5.
Data-Extraction Frequencies Compared to Assumptions for Payment Data
| Payment Data |
Complete Tetraplegia n=2 |
Incomplete Tetraplegia n=7 |
Complete Paraplegia n=11 |
Incomplete Paraplegia n=8 |
Total (%) n=28 |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| A | F | A | F | A | F | A | F | A* (%) | F (%) | |
| PT | 2 | 1 | 7 | 5 | 11 | 3 | 8 | 1 | 28 (100) | 10 (36) |
| OT |
2 |
0 |
7 |
1 |
11 |
3 |
8 |
3 |
28 (100) |
7 (25) |
| Psychology* | A=3, F=4 | 3 (11) | 4 (14) | |||||||
| FIM | No A, F=0 | No A | 0 | |||||||
A=assumption regarding frequency of payment data; F=actual frequency of payment data; No A=no assumption made
Psychology results were collapsed, as it was not possible to develop assumptions by level.
Table 6.
Mean Payment Data ($CAD) Extracted, by Level of Injury and Type of Service
| OT | PT | Psych | ||
|---|---|---|---|---|
| Complete tetraplegia n=2 |
Mean | 0 | 2,828 | 0 |
| Range | N/A | 0–5,655 | N/A | |
| Incomplete tetraplegia n=7 |
Mean | 0 | 352 | 96 |
| Range | N/A | 0–1,655 | 0–503 | |
| Complete paraplegia n=11 |
Mean | 786 | 4,200 | 4,870 |
| Range | 0–4,288 | 0–19,907 | 0–46,583 | |
| Incomplete paraplegia n=8 |
Mean | 45 | 2,081 | 10 |
| Range | 0–369 | 0–9,000 | 0–76 | |
| Total n=28 | Mean | 322 | 2,535 | 1,940 |
| Range | 0–4,288 | 0–19,907 | 0–46,583 |
OT=occupational therapy; PT=physical therapy; Psych=psychology; N/A=not applicable
DISCUSSION
The e-claim file review process permitted access to medical and rehabilitation documentation of the kind that may inform descriptive analysis of health interventions and outcome, as reported by Tierney and McDonald.39 While it was possible to access e-claim files and the data they contained, the data extracted using this process were considered incomplete, as they did not match the assumptions developed for payment data. For example, given the nature of SCI, it was expected that all e-claim files for persons with complete tetraplegia would yield payment data for OT and PT services;61,62 in fact, however, the two e-claim files for persons with complete tetraplegia yielded no evidence of OT payments, and only one yielded PT payment data. This finding is counterintuitive, since the records indicated that both persons had been discharged to live in the community after in-patient rehabilitation.
A number of factors may have influenced the success and failure of the e-claim file review process to permit extraction of the targeted data, including data requirements, data recording and sharing practices, and data linkages and alignment between health professionals and health payers.
The WSIB is empowered by legislation to obtain information from health organizations to inform the claims adjudication process.63 Such information may be obtained from both publicly funded and privately funded health sectors. Health records, such as hospital admission or discharge summaries, are routinely obtained; in this sample, such records were found in all e-claim files examined. In addition, standard claim forms are often used to collect information from health organizations that deliver outpatient health services. Using standard, condition-specific data requirements on claim forms is logical; the decision to do so, however, resides with the payer that requires the claim form and the organizations that control the intent and purpose of the form.
A lack of alignment in data-sharing practices between the public and private health systems may have contributed to the absence of FIM data in the e-claim files reviewed. While the use of standard claims forms by WSIB supported extraction of OT, PT, and psychology payment data, the standard claim form does not require submission of FIM data, even though these data are known to be collected routinely by publicly funded institutions. If payers do not require health care organizations to submit specific data, these organizations may lack stimulus or incentive to record such data or to share them with payers. In addition, publicly funded health care organizations may have defined practices for sharing of health data, and these practices may also be influenced by the requirements of the payer. The present study did not undertake to evaluate data-sharing practices in the public health sector; however, the data extracted during the project offer some insights. It is possible that when the WSIB requests data, in the form of health records, from a publicly funded organization, the request is broadly stated and does not specify a need to submit particular data such as FIM scores. Publicly funded health organizations are compelled by privacy laws to share only information that they are authorized by the claimant or by relevant laws to release. This may also limit the kinds and/or the quantity of data that such organizations routinely share with payers or other health providers. If WSIB and other payers do not specifically request certain data, it is understandable that those data may not be forthcoming from health organizations; however, this also reflects a lack of alignment of data standards across payers and along the continuum of care from public to private health systems. Privately funded rehabilitation is usually a continuation of care that began in the public health system; it is logical, therefore, to consider a move to align outcome measures across health sectors, whether public or private. Alignment of data-recording and data-sharing practices would also facilitate longitudinal research across health sectors.
Data-recording practices in the clinical setting may also influence the presence or absence of data in administrative claim files. Many of the health data contained in WSIB e-claim files were extracted from documentation submitted by health providers, and this documentation generally reflected the data collected in the clinical setting. Data collection in the clinical setting begins with the individual health provider who initiates assessment and treatment, and several factors may influence the process used, including (a) the needs of the injured person; (b) the health provider's need to be reimbursed for provision of care; and (c) the requirements of the payer. These three factors are inextricably linked. The health provider's ethical perspective likely places the needs of the injured person first, but, in the privately funded health system, taking the second and third factors into account is critical to achieving the first.
Many health facilities use condition-specific impairment measures to evaluate treatment interventions. But opportunities or incentives to link clinical impairment data (used to measure treatment effect) to outcomes such as employment are not always present. So, while data are collected in the clinical setting, the motivation to do so is often focused on evaluating the impairment and outcomes as they relate to treatment. Although these aspects are important, there is room to explore data collection that can support a broader evaluation of health outcomes related to activities and participation in societal roles.64
Privately funded rehabilitation providers in Ontario employ various business practices that may affect data recording and sharing. For example, health practices may operate as independent clinics or community-based practices, a small chain of several clinics operated by a single management, or a nationally managed chain of clinics spread across the country. Each of these organizations may be managed differently, have different treatment foci, and use different data-collection strategies. Consequently, although all of these organizations may treat persons with SCI, they may not collect or share the same types of data. The data they submit to WSIB, which ultimately reside in the e-claim file, may also reflect various data-collection practices in the privately funded health sector.
The concept of standardization of health data is not new. As delivery of outpatient rehabilitation shifts from the public to the private sector, private payers will want to improve the consistency and quality of data to permit monitoring of health services, costs, and outcomes. A growing number of health professions compete for reimbursement from limited public and private health dollars. Health professionals operating in a competitive marketplace may be motivated to collect standardized data to permit analysis of their practice's performance for comparison purposes, as well as to support best practices.
In the Canadian private rehabilitation sector, clinical practice guidelines (CPGs) have been promoted by health payers as a means of reducing variation in treatment and associated costs for certain conditions.65–67 Adoption of CPGs also has the potential to standardize collection of condition-specific data that can inform rehabilitation outcome research. Prior to implementing a CPG and related data standards, however, it would be important to engage researchers, health providers, and payers in the process to determine what might constitute an appropriate data set. There is some precedent for this approach. For example, WSIB has implemented programmes of care for acute low back pain and for upper-extremity and lower-extremity injuries, for which they consulted with worker and employer representatives as well as health professional organizations.67 In these programmes, standard outcome data are required, and mandatory fields exist on claim forms for the collection of these data. For uptake of a strategy to adopt CPGs in connection with standardized data collection, a well-defined analysis plan would need to be associated with the strategy, informing stakeholders of the potential impact of additional data-recording and data-collection efforts. Further, since collection of additional data may represent a new activity for some health professionals, consideration may need to be given to appropriate reimbursement for such activities. The issue of who will pay for effective production, recording, and management of data is likely one of several barriers to standard data practices that need to be addressed.
It appears that administrative review of WSIB e-claim files, in the absence of other data sources, holds extremely limited potential for outpatient rehabilitation data collection for the SCI population. The process should not be entirely dismissed, however, since it does provide some access to medical and rehabilitation documentation. Failure to locate all of the targeted data in this project may be related to a lack of rigour in the e-claim file review process itself, in SCI data requirements on the part of the payer, and/or in SCI data-recording and data-sharing practices in health organizations.
Finally, the rehabilitation needs of persons with SCI can be influenced by a large number of individual variables. Because of the highly individual analysis required for this population, any future attempt to use a similar process for data retrieval must consider that while demographic, injury, employability, and employment data can be accessed from e-claim files, outcome data such as FIM scores and payment data for services must be obtained from other sources, such as individual hospital records and the WSIB health services database.
It is critical that mechanisms be developed to ensure the existence of and access to standardized data in both the public and the private health care systems. While specific research questions will demand specific data, there is merit in defining minimum data sets that can inform desired health outcomes for a variety of conditions. Because of the extremely high cost of rehabilitation across the lifespan for persons with SCI, this is one condition for which consistent outcome data are important for longitudinal surveillance.
LIMITATIONS
This study evaluated a process of e-claim file review for gathering data from administrative claim files maintained by the WSIB. In spite of efforts to minimize abstractor error, the potential for some omissions or transcription errors remains. Such errors are unlikely, however, for a number of reasons. For example, results were consistently incomplete across all payment data; omissions were not restricted to one or two kinds of payment data, which suggests that other factors contributed to the incompleteness of the results. Validation of the process might have been achieved by comparing the extracted payment data with the WSIB aggregate database.
Because inter-abstractor and intra-abstractor reliability testing were not conducted, it is possible that data that existed in the e-claim file were not captured. The data abstractor was hired because he had extensive expertise and many years of experience with the WSIB e-claim file system; in addition, the cost of engaging another, similarly experienced data abstractor for the purpose of inter-abstractor reliability testing was financially prohibitive. Finally, the nature of the e-claim file, the privacy requirements of the payer, and the timing of the data extraction did not permit a second, blinded review of a single e-claim file at different time points for the purpose of intra-abstractor reliability testing.
Assumptions or expectations were developed to serve as a proxy for benchmarks for evaluative purposes. These were tied, where possible, to evidence from Canadian research. However, in the absence of robust Canadian data on use of and payment for outpatient SCI rehabilitation, the assumptions were also supported by evidence from the US literature, which may reflect health care payment levels and policies that differ from those in Canada.
Finally, a more comprehensive payment data set must be obtained through sources in addition to the e-claim file. For example, the new WSIB payment database, implemented in 2001, would enable researchers to access more comprehensive payment data.
CONCLUSIONS
One might dismiss the e-claim file review process as a method for outpatient rehabilitation data gathering. On the other hand, analysis of rehabilitation best practices in certain populations, such as persons with SCI, often requires a patient-specific approach, which may be well served by the details contained in medical and rehabilitation documentation. Given the absence of other viable methods for gathering such data, it is worth considering strategies to improve availability of SCI data through (a) standardization of data recorded by health providers and required by payers, (b) alignment of data practices in the public and private health sectors, and (c) approaches to improve the completeness of data compiled in administrative claim files by private health payers.
Standards to increase the usefulness of administrative claim files must benefit health researchers while not interfering with the primary needs of the data custodian, or payer, for benefits payment purposes. Creation of a minimum data set for outpatient SCI rehabilitation is paramount. Once standard data elements are agreed upon, payers can promote collection of these data by incorporating them into standard claim forms. Similarly, health professional organizations may promote collection and recording of standard data to inform outpatient SCI best practices. Alignment of SCI data practices and linkages between health sectors may also improve the consistency of data in administrative or clinical records, support longitudinal research across systems, and inform care.
With recent advances in technology, a universally accessible electronic health record integrating patient information from all sources into a single view is possible.68 Reintegration into family, community, the labour market, and society is challenging for persons with SCI; investment by stakeholders in implementing standardized collection of health data, including cost and payment data, is critical to inform both research that will improve our understanding of health services delivery and health policy development of care programmes that may improve health outcomes for individuals with SCI.
KEY MESSAGES
What Is Already Known on This Topic
Persons with spinal-cord injury (SCI) require rehabilitation goods and services in order to maximize their ability to reintegrate into the labour market and society at large. There is a trend toward more outpatient delivery of SCI rehabilitation and toward funding by private payers, including worker's compensation boards and automobile insurers. Health care costs for persons with SCI are significant, and return-to-work rates are low. There is little evidence to inform stakeholders about the cost or effectiveness of a growing number of rehabilitation interventions. Researchers need mechanisms to locate and collect data from the private health system in order to pursue SCI rehabilitation research. While administrative claim file review has been used with some success in rehabilitation research, a single method does not exist to permit researchers access to administrative claim file data held by the Canadian private health sector.
What This Study Adds
The process of administrative claim file review, applied to WSIB electronic claim files, has limited potential to inform SCI rehabilitation research. Implementation of standard data practices by privately funded health providers and alignment of data practices across the public and private health sectors would serve to improve the quality of data recorded in administrative claim files and, consequently, to improve the potential for SCI rehabilitation research using data from administrative claim files.
Many insurance plans limit the amount of funding available for medical and rehabilitation interventions. An insurer may have to balance the lifetime needs of a patient with SCI against the short-term benefits of a particular intervention. For example, in Ontario's first-party auto-insurance system, a maximum of $1,000,000 for medical and rehabilitation expenses and $1,000,000 for attendant care expenses is currently available for persons with SCI.
The category “serious injury” includes but is not limited to tetraplegia and paraplegia.
Riis R, Jaglal S, Boschen K, Walker J, Verrier M. Can administrative claim file review be used to gather physical therapy, occupational therapy, and psychology payment data and functional independence measure scores? implications for rehabilitation providers in the private health sector. Physiother Can. 2011;preprint. doi:10.3138/ptc.2010-25
References
- 1.Smetanin P, Kobak P. Life at risk: Analysis of traumatic SCI in Canada 2006 to 2036. Vancouver: Rick Hansen Foundation; 2007. [Google Scholar]
- 2.Canadian Paraplegic Association [CPA] Workforce participation survey of Canadians with spinal cord injury. Ottawa: The Association; 1996. [Google Scholar]
- 3.Johnson RL, Brooks CA, Whiteneck GG. Cost of traumatic spinal cord injury in a population-based registry. Spinal Cord. 1996;34:470–80. doi: 10.1038/sc.1996.81. [DOI] [PubMed] [Google Scholar]
- 4.Landry M, Williams P, Verrier M, Zakus D, Deber R. Shifting the public-private mix: a policy analysis of physical therapy funding in Ontario. Physiother Can. 2007;59:255–65. [Google Scholar]
- 5.Jongbloed L, Wendland T. The impact of reimbursement systems on occupational therapy practice in Canada and the United States of America. Can J Occup Ther. 2002;69(3):143–52. doi: 10.1177/000841740206900304. [DOI] [PubMed] [Google Scholar]
- 6.Black C, McGrail K, Fooks C, Baranek P, Maslove L. Data, data, everywhere…: improving access to population health and health services research data in Canada. Vancouver: Centre for Health Services and Policy Research and Canadian Policy Research Networks; 2005. [Google Scholar]
- 7.International Campaign for Cures of Spinal Cord Injury Paralysis [ICCP] Global summary of spinal cord injury, incidence and economic impact 2004. [cited 2004 Jan 9]. Available from: http://www.campaignforcure.org/globalsum.htm.
- 8.Verrier M, Walker J, Lawson N, McGillivray C, Ritchie K, Williams J. Health services needs for persons with spinal cord injury: consumer, provider and payer perspecitves. Toronto: Ontario Neurotrauma Foundation; 2001. [Google Scholar]
- 9.Insurance Bureau of Canada [IBC] Insurance Bureau of Canada report on industry issues: health care 2003. [cited 2003 Jul 21]. Available from: http://www.ibc.ca/templates/icc/icc1.cfm?CFID=392821&CFTOKEN=19509270&user_id=17&page=12020&template=17&resultat=0&order_num=&mot_recherche=&write=0&student_id=0&debut=0&curr_page=1.
- 10.McDaid D, Cookson R. Evaluating health care interventions in the European Union. Health Policy. 2003;63(2):133–9. doi: 10.1016/s0168-8510(02)00060-x. doi: 10.1016/S0168-8510(02)00060-X. [DOI] [PubMed] [Google Scholar]
- 11.McDaid D, Cookson R, Maynard A, et al. Evaluating health interventions in the 21st century: old and new challenges. Health Policy. 2003;63(2):117–20. doi: 10.1016/s0168-8510(02)00058-1. doi: 10.1016/S0168-8510(02)00058-1. [DOI] [PubMed] [Google Scholar]
- 12.Canadian Institute for Health Information [CIHI] The burden of neurologic injuries in Canada. Ottawa: Public Health Agency of Canada; 2006. [Google Scholar]
- 13.Canadian Institute for Health Information [CIHI] Inpatient rehabilitation in Canada 2005–2006. Ottawa: The Institute; 2006. [Google Scholar]
- 14.Beattie PF, Pinto MB, Nelson MK, Nelson R. Patient satisfaction with outpatient physical therapy: instrument validation. Phys Ther. 2002;82:557–65. [PubMed] [Google Scholar]
- 15.Eng JJ, Levins SM, Townson AF, Mah-Jones D, Bremner J, Huston G. Use of prolonged standing for individuals with spinal cord injuries. Phys Ther. 2001;81:1392–9. doi: 10.1093/ptj/81.8.1392. [DOI] [PubMed] [Google Scholar]
- 16.Lugo LH, Salinas F, Garcia HI. Out-patient rehabilitation programme for spinal cord injured patients: evaluation of the results on motor FIM score. Disabil Rehabil. 2007;29:873–81. doi: 10.1080/09638280701455494. doi: 10.1080/09638280701455494. [DOI] [PubMed] [Google Scholar]
- 17.Elliott TR, Frank RG. Depression following spinal cord injury. Arch Phys Med Rehabil. 1996;77:816–23. doi: 10.1016/s0003-9993(96)90263-4. doi: 10.1037//0090-5550.37.1.37. [DOI] [PubMed] [Google Scholar]
- 18.Boschen KA, Tonack M, Gargaro J. Long-term adjustment and community reintegration following spinal cord injury. Int J Rehabil Res. 2003;26(3):157–64. doi: 10.1097/00004356-200309000-00001. doi: 10.1097/00004356-200309000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Ditunno JF, Jr, Cohen ME, Hauck WW, Jackson AB, Sipski ML. Recovery of upper-extremity strength in complete and incomplete tetraplegia: a multicenter study. Arch Phys Med Rehabil. 2000;81:389–93. doi: 10.1053/mr.2000.3779. doi: 10.1053/mr.2000.3779. [DOI] [PubMed] [Google Scholar]
- 20.Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, Svenson LW, et al. Depression following traumatic spinal cord injury. Neuroepidemiology. 2005;25(2):55–61. doi: 10.1159/000086284. doi: 10.1159/000086284. [DOI] [PubMed] [Google Scholar]
- 21.Kennedy P, Rogers BA. Anxiety and depression after spinal cord injury: a longitudinal analysis. Arch Phys Med Rehabil. 2000;81:932–7. doi: 10.1053/apmr.2000.5580. doi: 10.1053/apmr.2000.5580. [DOI] [PubMed] [Google Scholar]
- 22.Krause JS, Kemp B, Coker J. Depression after spinal cord injury: relation to gender, ethnicity, aging, and socioeconomic indicators. Arch Phys Med Rehabil. 2000;81:1099–109. doi: 10.1053/apmr.2000.7167. doi: 10.1053/apmr.2000.7167. [DOI] [PubMed] [Google Scholar]
- 23.Murphy GC, Young AE, Brown DJ, King NJ. Explaining labor force status following spinal cord injury: the contribution of psychological variables. J Rehabil Med. 2003;35(6):276–83. doi: 10.1080/16501970310015209. doi: 10.1080/16501970310015209. [DOI] [PubMed] [Google Scholar]
- 24.Waters RL, Adkins RH, Yakura JS, Sie I. Motor and sensory recovery following complete tetraplegia. Arch Phys Med Rehabil. 1993;74:242–7. [PubMed] [Google Scholar]
- 25.Landry M, Jaglal S, Wodchis W, Cott CA. Forecasting demand for rehabilitation services across Ontario's continuum of care. Toronto: Toronto Rehabilitation Institute; 2006. [Google Scholar]
- 26.Garnick DW, Hendricks AM, Comstock CB. Measuring quality of care: fundamental information from administrative datasets. Int J Qual Health Care. 1994;6(2):163–77. doi: 10.1093/intqhc/6.2.163. [DOI] [PubMed] [Google Scholar]
- 27.Garnick DW, Hodgkin D, Horgan CM. Selecting data sources for substance abuse services research. J Subst Abuse Treat. 2002;22(1):11–22. doi: 10.1016/s0740-5472(01)00208-2. doi: 10.1016/S0740-5472(01)00208-2. [DOI] [PubMed] [Google Scholar]
- 28.Garnick DW, Horgan CM, Hendricks AM, Comstock C. Using health insurance claims data to analyze substance abuse charges and utilization. Med Care Res Rev. 1996;53:350–68. doi: 10.1177/107755879605300308. doi: 10.1177/107755879605300308. [DOI] [PubMed] [Google Scholar]
- 29.Iezzoni LI. Using administrative data to study persons with disabilities. Milbank Q. 2002;80:347–79. doi: 10.1111/1468-0009.t01-1-00007. doi: 10.1111/1468-0009.t01-1-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sorock GS, Ranney TA, Lehto MR. Motor vehicle crashes in roadway construction workzones: an analysis using narrative text from insurance claims. Accident Anal Prev. 1996;28(1):131–8. doi: 10.1016/0001-4575(95)00055-0. doi: 10.1016/0001-4575(95)00055-0. [DOI] [PubMed] [Google Scholar]
- 31.Stevens AJ, Raftery J, Roderick P. Can health technologies be assessed using routine data? Int J Technol Assess Health Care. 2005;21(1):96–103. doi: 10.1017/s0266462305050129. doi: 10.1017/S0266462305050129. [DOI] [PubMed] [Google Scholar]
- 32.Wunsch H, Harrison D, Rowan K. Health services research in critical care using administrative data. J Crit Care. 2005;20:264–9. doi: 10.1016/j.jcrc.2005.08.002. doi: 10.1016/j.jcrc.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 33.Sulzenko-Laurie B, Riis V, Grubisic E. A survey of injury claims data after introduction of injury care protocols in Alberta, Canada. J Occup Environ Med. 2010;52:450–5. doi: 10.1097/JOM.0b013e3181dbfa7d. doi: 10.1097/JOM.0b013e3181dbfa7d. [DOI] [PubMed] [Google Scholar]
- 34.Du Bois M, Donceel P, Debbaut B. Social insurance cost of standard discectomy and percutaneous nucleotomy: a retrospective study of 87 social insurance claim files of male blue collar workers. Acta Orthop Belg. 1998;64(2):144–9. [PubMed] [Google Scholar]
- 35.Foote SB, Virnig BA, Bockstedt L, Lomax Z. External review of health plan denials of mental health services: lessons from Minnesota. Adm Policy Ment Health. 2007;34(1):38–44. doi: 10.1007/s10488-006-0074-y. doi: 10.1007/s10488-006-0074-y. [DOI] [PubMed] [Google Scholar]
- 36.Webster BS, Verma S, Pransky GS. Outcomes of workers' compensation claimants with low back pain undergoing intradiscal electrothermal therapy. Spine. 2004;29:435–41. doi: 10.1097/01.brs.0000092376.41688.1a. doi: 10.1097/01.BRS.0000092376.41688.1A. [DOI] [PubMed] [Google Scholar]
- 37.Jones D, Switzer-McIntyre S. Falls from trucks: a descriptive study based on a workers compensation database. Work. 2003;20(3):179–84. [PubMed] [Google Scholar]
- 38.Manktelow RT, Binhammer P, Tomat LR, Bril V, Szalai JP. Carpal tunnel syndrome: cross-sectional and outcome study in Ontario workers. J Hand Surg-Am. 2004;29:307–17. doi: 10.1016/j.jhsa.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 39.Tierney WM, McDonald CJ. Practice databases and their uses in clinical research. Stat Med. 1991;10:541–57. doi: 10.1002/sim.4780100406. doi: 10.1002/sim.4780100406. [DOI] [PubMed] [Google Scholar]
- 40.Johnston T, Betz R, Smith B, Mulcahey MJ. Implanted functional electrical stimulation: an alternative for standing and walking in pediatric spinal cord injury. Spinal Cord. 2003;41(3):144–52. doi: 10.1038/sj.sc.3101392. doi: 10.1038/sj.sc.3101392. [DOI] [PubMed] [Google Scholar]
- 41.Canadian Institute of Health Information [CIHI] Life after traumatic spinal cord injury: from inpatient rehabilitation back to the community. Ottawa: The institute; 2006. [Google Scholar]
- 42.Workplace Safety and Insurance Board [WSIB] Statistical supplement to annual report. Toronto: The Board; 2005. [Google Scholar]
- 43.Workplace Safety and Insurance Board [WSIB] Statistical supplement to annual report. Toronto: The Board; 2006. [Google Scholar]
- 44.DeVivo MJ, Fine PR. Employment status of spinal cord injured patients 3 years after injury. Arch Phys Med Rehabil. 1982;63(5):200–3. [PubMed] [Google Scholar]
- 45.Jang Y, Wang YH, Wang JD. Return to work after spinal cord injury in Taiwan: the contribution of functional independence. Arch Phys Med Rehabil. 2005;86:681–6. doi: 10.1016/j.apmr.2004.10.025. doi: 10.1016/j.apmr.2004.10.025. [DOI] [PubMed] [Google Scholar]
- 46.Krause JS. Years to employment after spinal cord injury. Arch Phys Med Rehabil. 2003;84:1282–9. doi: 10.1016/s0003-9993(03)00265-x. doi: 10.1016/S0003-9993(03)00265-X. [DOI] [PubMed] [Google Scholar]
- 47.Lidal IB, Huynh TK, Biering-Sorensen F. Return to work following spinal cord injury: a review. Disabil Rehabil. 2007;29:1341–75. doi: 10.1080/09638280701320839. doi: 10.1080/09638280701320839. [DOI] [PubMed] [Google Scholar]
- 48.Tomassen P, Post M, van Asbeck F. Return to work after spinal cord injury. Spinal Cord. 2000;38:51–55. doi: 10.1038/sj.sc.3100948. [DOI] [PubMed] [Google Scholar]
- 49.Young AE, Webster B, Giunti G, Pransky G, Nesathurai S. Services provided following compensable work-related tetraplegia. Spinal Cord. 2004;42:248–60. doi: 10.1038/sj.sc.3101598. doi: 10.1038/sj.sc.3101598. [DOI] [PubMed] [Google Scholar]
- 50.Ianucci I. Conversation with: Viivi Riis (Department of Physical Therapy, University of Toronto) 2004. Feb 5, (Manager, Serious Injury Unit, WSIB)
- 51.Hamilton BB, Deutsch A, Russell C, Fiedler RC, Granger CV. Relation of disability costs to function: spinal cord injury. Arch Phys Med Rehabil. 1999;80:385–91. doi: 10.1016/s0003-9993(99)90274-5. doi: 10.1016/S0003-9993(99)90274-5. [DOI] [PubMed] [Google Scholar]
- 52.Stineman MG, Marino RJ, Deutsch A, Granger CV, Maislin G. A functional strategy for classifying patients after traumatic spinal cord injury. Spinal Cord. 1999;37:717–25. doi: 10.1038/sj.sc.3100914. doi: 10.1038/sj.sc.3100914. [DOI] [PubMed] [Google Scholar]
- 53.Hall KM, Cohen ME, Wright J, Call M, Werner P. Characteristics of the Functional Independence Measure in traumatic spinal cord injury. Arch Phys Med Rehabil. 1999;80:1471–6. doi: 10.1016/s0003-9993(99)90260-5. doi: 10.1016/S0003-9993(99)90260-5. [DOI] [PubMed] [Google Scholar]
- 54.Whiteneck G, Meade MA, Dijkers M, Tate DG, Bushnik T, Forchheimer MB. Environmental factors and their role in participation and life satisfaction after spinal cord injury. Arch Phys Med Rehabil. 2004;85:1793–803. doi: 10.1016/j.apmr.2004.04.024. doi: 10.1016/j.apmr.2004.04.024. [DOI] [PubMed] [Google Scholar]
- 55.Canadian Institute of Health Information [CIHI] Injury hospitalizations by nature of injury. Ottawa: The Institute; 2000. [Google Scholar]
- 56.Ardal S, Baigent L, Bains N, Hay C, Lee P, Loomer S. The health analyst's toolkit. Toronto: Health System Intelligence Project, Government of Ontario; 2006. [Google Scholar]
- 57.Eisenberg MG, Saltz CC. Quality of life among aging spinal cord injured persons: long term rehabilitation outcomes. Paraplegia. 1991;29:514–20. doi: 10.1038/sc.1991.74. [DOI] [PubMed] [Google Scholar]
- 58.Lundqvist C, Siosteen A, Blomstrand C, Lind B, Sullivan M. Spinal cord injuries: clinical, functional, and emotional status. Spine. 1991;16:78–83. [PubMed] [Google Scholar]
- 59.Siosteen A, Lundqvist C, Blomstrand C, Sullivan L, Sullivan M. The quality of life of three functional spinal cord injury subgroups in a Swedish community. Paraplegia. 1990;28:476–88. doi: 10.1038/sc.1990.64. [DOI] [PubMed] [Google Scholar]
- 60.Canadian Institute of Health Information [CIHI] The burden of neurological diseases, disorders and injuries in Canada. Ottawa: The Institute; 2007. [Google Scholar]
- 61.Canadian Spinal Research Organization [CASRO] The after and beyond spinal cord injury resource manual. Richmond Hill (ON): The Organization; 2005. [Google Scholar]
- 62.Lindsay L, Klebine P, Wells MJ. Understanding spinal cord injury and functional goals (Spinal Cord Injury InfoSheet #4) 2000. May, [cited 2007 Dec 15]. Available from: http://images.main.uab.edu/spinalcord/pdffiles/info-4.pdf.
- 63.Workplace Safety and Insurance Act. 1997. S. 23.
- 64.World Health Organization [WHO] Towards a common language for functioning, disability and health. Geneva: The Organization; 2002. [Google Scholar]
- 65.Rappolt SG. Clinical guidelines and the fate of medical autonomy in Ontario. Soc Sci Med. 1997;44:977–87. doi: 10.1016/s0277-9536(96)00223-7. doi: 10.1016/S0277-9536(96)00223-7. [DOI] [PubMed] [Google Scholar]
- 66.Morrison M. Outpatient rehabilitation outcomes: the cost-effectiveness challenge. J Rehabil Outcome Meas. 1997;1(2):43–7. [Google Scholar]
- 67.Workplace Safety and Insurance Board [WSIB] Programs of care. Toronto: The Board; 2007. [Google Scholar]
- 68.Szende A. A lifelong ehealth record. [updated 2001 Oct 1];Can Healthc Manager. 2001 55(6) Available from: http://www.chmonline.ca/issue/article.jsp?content=20011001_230095_9495. [Google Scholar]