INTRODUCTION
The adipose tissue is unique in its ability to expand and regress throughout life. In developed and developing countries, the overall adipose tissue expansion phase outpaces regression, resulting in an ever-expanding obese society. To shed the “extra pound”, a significant number of patients undergo surgeries to remove the unwanted fat. The resulting “medical wastes” are however potential therapeutic treasures for two reasons. One is that the adipose tissue is a rich source of multipotent mesenchymal cells called adipose-derived stem cells (ADSCs) 1,2; and the other is that the adipose extracellular matrix (ECM) can be fabricated into acellular scaffolds for tissue engineering 3–5. In regard to ADSCs, these cells have been shown to differentiate into Schwann cells that formed myelin sheath on axons 6 and have been used to seed nerve conduits for peripheral nerve repair 7–9. In addition, we have shown that ADSCs secrete neurotrophic factors that promote cavernous nerve (CN) regeneration 10,11. In regard to adipose ECM, the fabricated scaffolds have been shown to support adipogenic differentiation of ADSCs 5. In the present study we combined ADSC’s neuroregenerative potential and adipose ECM’s scaffold potential to construct nerve grafts for the repair of peripheral nerves, in this case, CN.
The CN innervate penile erectile tissue and are essential for erection. Due to their proximity to the prostate, bladder, and rectum, these nerves are often damaged during surgeries on these organs, resulting in erectile dysfunction (ED) 12–14. In particular, prostate cancer is the most prevalent malignancy in men and is often treated by radical prostatectomy, causing damage to the CN and subsequent ED 15. To repair the damaged CN, autologous nerve grafting with sural nerves has initially been shown to result in an erectile function recovery rate of 43% 16. However, the harvest of the sural nerves causes donor site morbidity and requires the collaborative support of plastic surgeons. On the other hand, the harvest of the genitofemoral nerves causes minimal morbidity and can be done by the urological surgeon. CN repair with genitofemoral nerve grafting has an erectile function recovery rate of approximately 50% 17,18. On an experimental basis, grafting with decellularized CN from donor rats has also been attempted 19. However, the clinical applicability of such a treatment procedure is rather low because of the need to harvest the CN from human volunteers or cadavers.
In the present study we processed lipectomized human and rat adipose tissues into acellular matrices, seeded the rat matrix with allogenic rat ADSCs, and grafted the seeded matrix into rats with transected CN. We observed variable but substantial recovery of erectile function following such grafting.
MATERIALS AND METHODS
Procurement of adipose tissues
Adipose tissue samples were obtained from patients during routine abdominoplasty following informed patient consent and according to the guidelines set by our institution’s Committee on Human Research. Rat adipose tissue was obtained from the epididymal fat pad of 2-month-old male Sprague-Dawley rats (Charles River Laboratories, Wilmington, MA). All animal care, treatments and procedures were approved by our Institutional Animal Care and Use Committee.
Decellularization of adipose tissue
The adipose tissue in a 50-ml conical tube was dipped into liquid nitrogen for 5 min and then immediately placed in a 37°C water bath for 10 min. After repeating this freeze-and-thaw step two more times, the tissue was centrifuged at 1500 rpm for 10 min at room temperature (RT). After removing the liquid fatty portion, the tissue was washed with 70% ethanol and PBS three times each. It was then incubated in 0.05% trypsin, 0.05% ethylenediaminetetraacetic acid, 20 ng/ml DNAse I, and 20 ng/ml RNAse for 4 h with slow rotation at RT. After washing with PBS twice, the tissue was incubated in 0.1% sodium dodecyl sulphate (SDS) for 12 h at RT. After washing with PBS three times, the tissue was incubated in 1% penicillin and streptomycin for 12 h at 4°C.
Preparation of acellular matrix
The decellularized tissue from above was further processed into various forms of acellular matrices as follows. In one example, the decellularized tissue was cut to ~0.5mm × 1mm × 8mm threads and dried for 12 h for the preparation of adipose tissue-derived acellular matrix thread (ADMT). In another example, the decellularized tissue was homogenized in PBS, placed into a 10-cm plastic dish, and dried for the preparation of adipose-derived acellular matrix sheet (ADMS). The resulting ADMT or ADMS was further UV-sterilized inside a tissue culture hood.
Seeding of acellular matrix thread with adipose-derived stem cells
ADMT was washed with PBS three times, dried at RT for 2 h, and placed in a 6-well cell culture dish. ADSCs were isolated as described previously 20. Approximately 1×104 ADSCs in 200 µl of DMEM was then evenly added to the ADMT. The culture dish was then placed in a humidified 37°C incubator with 5% CO2. Four h later, 3 ml of DMEM supplemented with 10% FBS was added to the ADMT, and the dish was returned to the incubator. At 24 h and 1 week, the seeded ADMT was stained with 1 µg/ml Calcein AM (Invitrogen, Carlsbad, CA) for 10 min at 37°C and examined with Nikon Eclipse E600 fluorescence microscope.
Subcutaneous transplantation of seeded matrix
Approximately 5×104 ADSCs were grown to 60% confluence and then labeled with 10 µM of EdU for 24 h as previously described 21. The cells were then washed three times with PBS and then seeded onto an allogenic ADMT by the above-described procedure. Forty-eight h later, the seeded ADMT was transplanted into an autologous host (from which the ADSC was isolated). The transplantation procedure was as follows. Under inhalant anesthesia, an incision was made in the lower abdomen to expose the subcutaneous space, into which the seeded ADMT was transplanted. Ten days later, the rat was sacrificed and the transplanted tissue examined by HE staining and microscopy. The transplanted ADMT was also retrieved and stained with an EdU detection cocktail that contained Alexa-594 (Invitrogen) and with 4',6-diamidino-2-phenylindole (DAPI, for nuclear staining, 1 µg/ml, Sigma-Aldrich). The stained matrix was examined with Nikon Eclipse E600 fluorescence microscope and photographed with Retiga 1300 Q-imaging camera.
Grafting of unseeded and seeded matrix in nerve injury rats
Thirty 2-month-old male Sprague-Dawley rats were randomized into three equal groups: Control, ADMT, and ADMT+ADSC. Under inhalant anesthesia, a midline incision was made in the lower abdomen and the periprostatic space containing the major pelvic ganglion (MPG) and the cavernous nerves (CN) were exposed. A 5-mm-long nerve segment, starting 5 mm distal from the origin of the CN at the MPG was isolated and resected. In the control group, the abdomen was then closed in layers without further treatment. In the treatment groups, either acellular ADMT, or ADMT/ADSC construct was microsurgically interposed and fixed against the prostatic capsule using 10-0 nylon sutures to bridge the nerve gap.
Determination of erectile function
Three months after CN injury with and without grafting, all rats were examined for erectile function by standard protocol 10. Under Ketamine-Midazolam anesthesia, the MPG and CN were exposed bilaterally via a midline laparotomy. A 23G butterfly needle was inserted into the proximal left corpus cavernosum, filled with 250 U/mL heparin solution and connected to a pressure transducer (Utah Medical Products, Midvale, UT, USA) for intracavernous pressure (ICP) measurement. The ICP was recorded at a rate of 10 samples/second using a computer with LabView 6.0 software (National Instruments, Austin, TX). A bipolar stainless-steel hook electrode was used to stimulate the origin of the CN at the MPG proximally from the nerve gap (in controls) or the interposed construct (in treatment groups). The electrode was connected to a signal generator (National Instruments) and custom-built constant-current amplifier generating monophasic rectangular pulses with stimulus parameters of 1.5 mA, 20 Hz, pulse width 0.2 ms, and duration 50 seconds. Three stimulations were conducted per side and the erection with the maximum increase in ICP was included for statistical analysis in each animal. For the calculation of ICP increase/mean arterial pressure (MAP) ratio, systemic blood pressure was recorded using a 23G butterfly needle inserted into the aorta at the level of the iliac bifurcation.
Immunohistochemical and immunofluorescence staining
Tissue samples were fixed in cold 2% formaldehyde and 0.002% saturated picric acid in 0.1 M phosphate buffer, pH 8.0, for 4 hours followed by overnight immersion in buffer containing 30% sucrose. The specimens were then embedded in OCT Compound (Sakura Finetec USA, Torrance, CA) and stored at −70 °C until use. Fixed frozen tissue specimens were cut at 7 microns, mounted onto SuperFrost-Plus charged slides (Fisher Scientific, Pittsburgh, PA) and air dried for 5 min. For immunostaining, the slides were placed in 0.3% H2O2/methanol for 10 min, washed twice in PBS for 5 min and incubated with 3% horse serum in PBS/0.3% Triton X-100 for 30 min at RT. After draining this solution, the slides were incubated at RT with anti-nNOS antibody (Santa Cruz Biotechnology, Santa Cruz, CA) or anti-S100 antibody (Leica Microsystems Inc., Bannockburn, IL) for 1.5 h. After rinses with PBS, the sections were incubated with FITC-conjugated secondary antibody (Jackson ImmunoResearch Laboratories, West Grove, PA). After rinses with PBS, the slides were incubated with freshly made EdU detection cocktail (Invitrogen) for 30 min at RT followed by staining with DAPI. The stained tissue was examined with Nikon Eclipse E600 fluorescence microscope and photographed with Retiga 1300 Q-imaging camera.
Statistical analysis
Data was analyzed with Prism 4 (GraphPad Software, Inc., San Diego, CA) using one-way ANOVA followed by Tukey-Kramer test for post-hoc comparisons. All data are reported as mean ± standard deviation. Significance was set at p<0.05.
RESULTS
Decellularization and molding
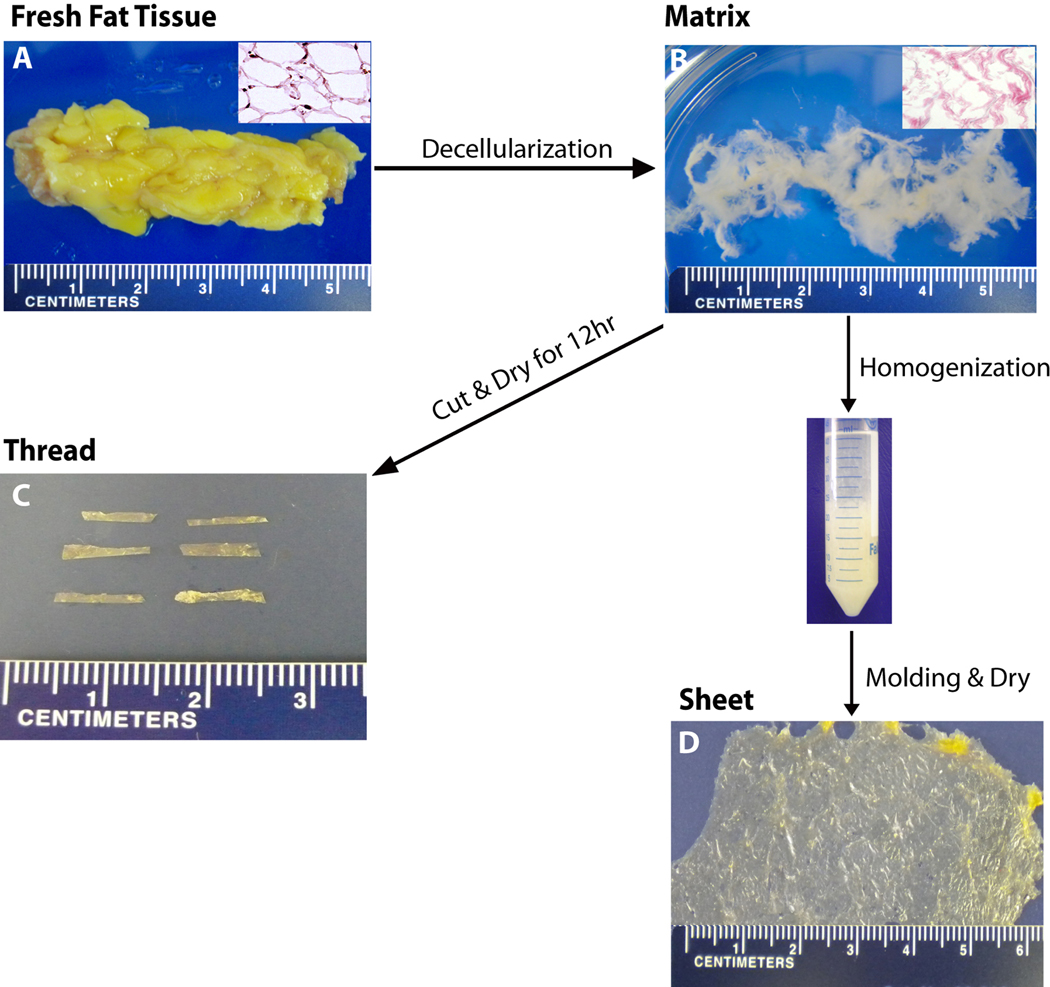
Decellularization was performed with adipose tissue isolated from both human and rat. Data shown in Fig. 1 are for a tissue sample obtained from a patient who underwent elective abdominoplasty. After a 5-day extraction procedure, the original tissue (Fig. 1A) was transformed into a loose matrix that was devoid of cells and cell debris (Fig. 1B). Qualitatively, the decellularized adipose tissue had similar dimensions and shape as the original tissue (Fig. 1A &B). Quantitatively, the matrix represented approximately 35% of the original tissue mass. After drying under ambient condition, the decellularized adipose tissue could be cut into various sizes and shapes, for example, threads (Fig. 1C). It could also be homogenized and then molded into various three-dimensional architectures, in this case, a sheet (Fig. 1D).
Fig. 1.
Decellularization and fabrication of adipose tissue. A human adipose tissue (A) was decellularized according to the protocol shown in Materials and Methods and transformed into an acellular matrix (B). Inserts in A and B are histological images of the adipose tissue before and after decellularization. The matrix in B was cut into threads as shown in C, or homogenized and then molded into a sheet as shown in D.
Seeding of matrix with ADSCs
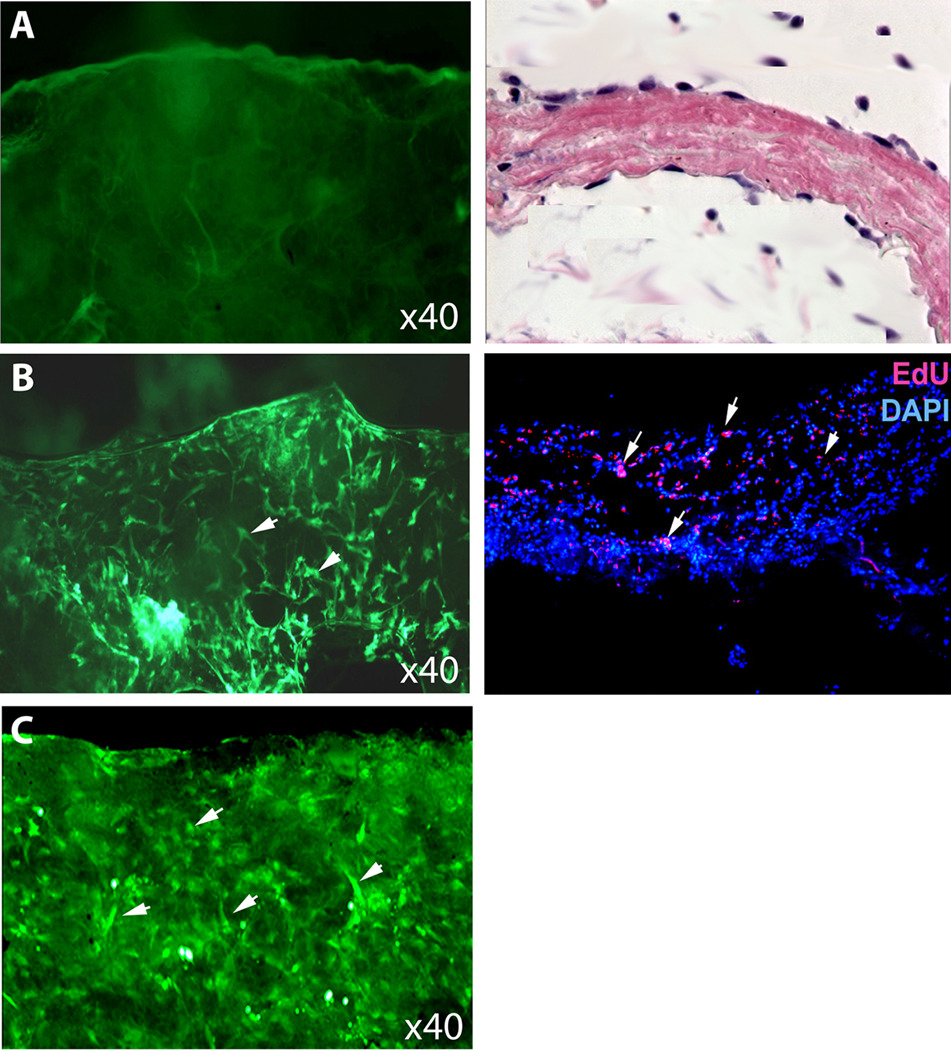
It has been shown that nerve conduits seeded with ADSCs produced better results than unseeded ones for peripheral nerve repair 7–9,22. We thus examined how well ADSCs could attach and grow on acellular adipose matrix, in this case, threads to be used as nerve conduits. We also considered that, for future clinical application, the most ideal matrix-based nerve conduit should combine allogenic matrix with autologous ADSCs. Thus, data shown in Fig. 2 are for a nerve conduit that will be grafted into a rat host, and it was constructed by seeding an allogenic matrix with autologous ADSCs. Twenty-four h after seeding, the autologous ADSCs adhered to the allogenic matrix and covered about 55% of the surface. One week later, the cells covered about 90% of the matrix surface (Fig. 2A–C). As a pre-grafting test, the seeded matrix was transplanted into the subcutaneous space of an allogenic host, and during a 10-day course, no sign of inflammatory reaction was observed. Furthermore, histological examination of the transplanted tissue showed that the matrix remained intact and was covered with a layer of cells (Fig. 2D). Thus, autologous ADSC-seeded allogenic adipose matrix was tolerated by the host and remained intact for an extended period of time in vivo.
Fig. 2.
Seeding with ADSC. A. The decellularized matrix was devoid of cells as indicated by calcein stain (green). B. Twenty-four h after seeding 55% of the surface was covered with ADSCs (arrowheads). C. One week after seeding 90% of the surface was covered with ADSCs (arrowheads). D. The seeded matrix was transplanted into subcutaneous space, which was examined by HE staining 10 days later. E. Another transplanted matrix was examined by EdU staining for the presence of seeded ADSCs (arrowheads) and by DAPI staining for cell nuclei.
Grafting of seeded and unseeded matrix
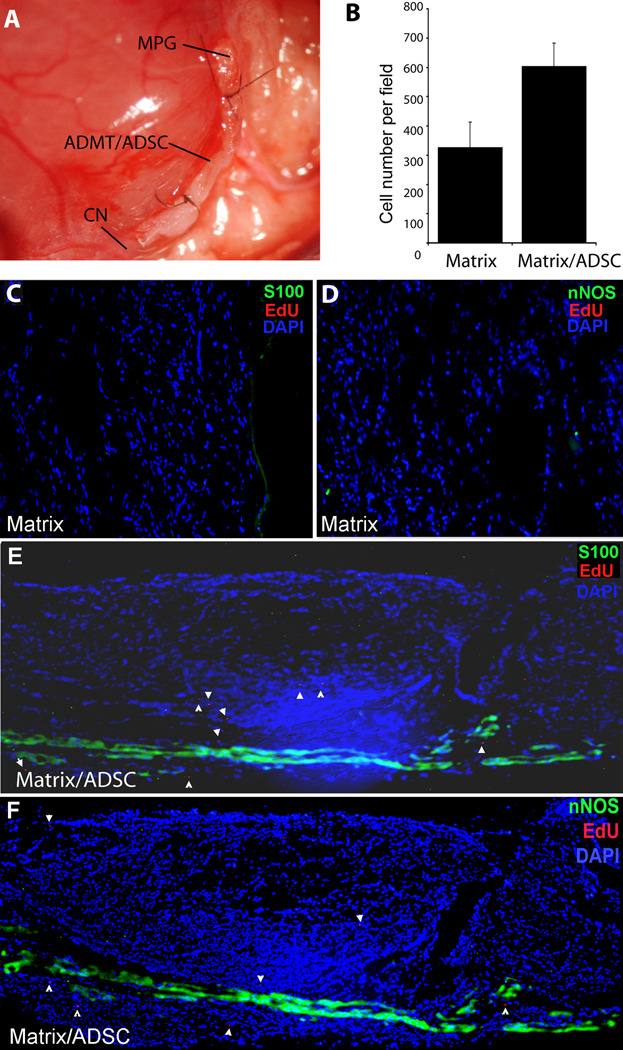
To simulate post-prostatectomy nerve injury, male rats underwent bilateral CN transection. These rats then received no graft, unseeded adipose matrix, or ADSC-seeded adipose matrix (Fig. 3A). Three months later, these rats were examined for erectile function and then sacrificed. Histological examination of the grafts showed that both unseeded and seeded matrices were covered with numerous cells (Fig. 3B–F). On average the cell density was nearly twice as high on seeded matrix as on unseeded matrix (Fig. 3B). S100, a general nerve marker, and nNOS, an erectile nerve-specific nerve marker, were both absent and present on the unseeded and seeded matrices, respectively (Fig. 3C–F). On the seeded matrices S100 and nNOS were expressed at various degrees but mostly co-localized near the MPG, indicating various degrees of CN axonal extension. One of the seeded matrices contained an S100/nNOS-positive nerve across its entire length, and several EdU-positive cells (ADSC) were found along this nerve fiber (Fig. 3E&F).
Fig. 3.
Grafting to repair cavernous nerve. Rats were subjected to cavernous nerve (CN) dissection and then grafted with ADMT or with ADSC-seeded ADMT. A. Seeded ADMT was grafted below the major pelvic ganglion (MPG). Three months after grafting, the matrices were examined by EdU staining for the presence of seeded ADSC, by DAPI staining for cell nuclei, and by immunostaining for S100 or nNOS expression. B. The number of cells was nearly twice as great on the seeded matrix as on the unseeded matrix. C. Unseeded matrix immunostained for S100. D. Unseeded matrix immunostained for nNOS. E. Seeded matrix immunostained for S100. F. Seeded matrix immunostained for nNOS. Note the presence of EdU-positive cells (arrowheads) along the nerve fiber.
Assessment of erectile function
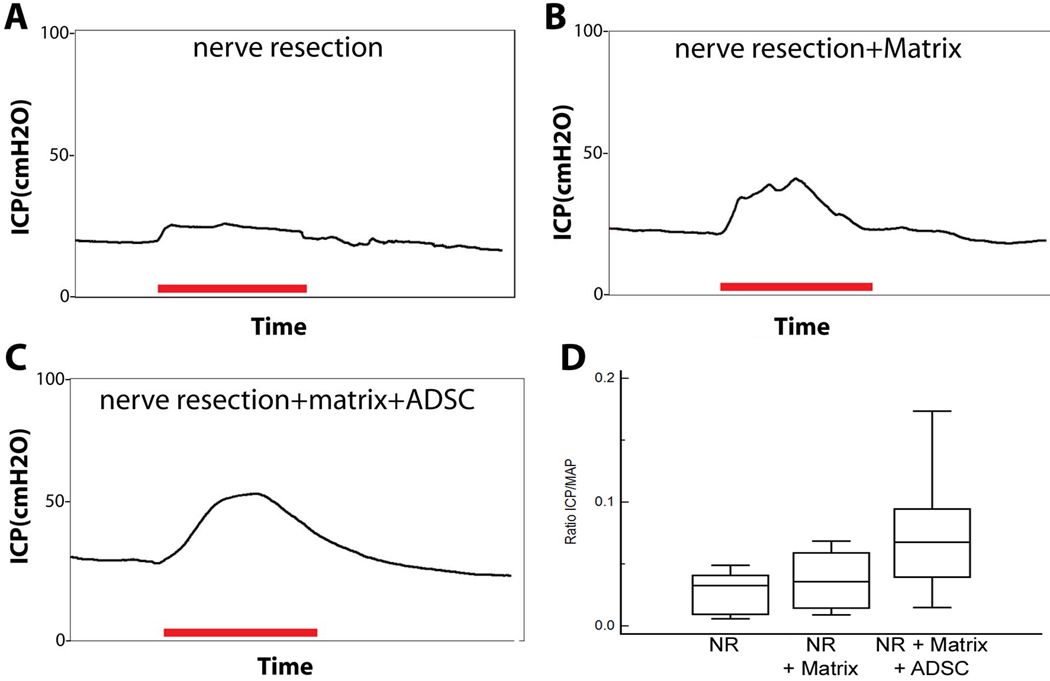
Erectile function of above-mentioned rats was assessed by measuring the intracorporal pressure (ICP) after electrostimulation of CN, which was normalized against mean arterial blood pressure (MAP). The results showed that the ADMT group had better erectile function than the control, and the ADMT+ADSC group was better than the ADMT group (Fig. 4). However, despite a clear trend toward functional recovery, especially in the ADMT+ADSC group, the difference (P=0.07 between ADMT+ADSC and control) did not reach statistical significance due to large variations.
Fig. 4.
Measurement of erectile function. Representative graphs of intracorporal pressure (ICP) are presented for rats with bilateral CN resection (A), bilateral CN resection and grafting with unseeded matrix (B), and bilateral CN resection and grafting with seeded matrix (C). The red bar indicates the duration of cavernous nerve stimulation (50 seconds). The ICP/MAP ratio was compared among the three groups of rats (D).
DISCUSSION
Autologous nerve grafting inevitably requires sacrificing a functional nerve; in addition, the procurement of such a graft often requires a secondary surgery and causes donor site morbidity. On the other hand, xenografting materials do not have these problems but carry the risks of host rejection and transmitting zoonotic diseases 23. Thus, allogenic grafts may have the best potential but still require careful considerations. For example, their procurement should not be harmful to the living donor or should be agreeable to the family of the deceased donor. However, these criteria are difficult to fulfill because few tissues possess graft-material quality and can be removed from a living person without causing harm. In addition, cultural confines may prevent the wide adoption of cadaveric tissues.
The adipose tissue is one of the rare tissues that can be partially removed from a living person without causing harm. Its superficial location makes it more accessible than most other tissues, and its removal is an intervention desired by many patients. As the volume of surgeries for obesity and post-weight-loss contouring continues to increase, adipose tissue is removed in an increasing rate. Thus, there is no doubt that there is an abundance of adipose tissue, and a recent study by Flynn 5 has demonstrated its potential as an acellular matrix for adipose tissue reconstruction. Specifically, scanning electron microscopic examination of the acellular adipose matrix identified regions of network-type collagen, consistent with the rich basement membrane component in adipose tissue. Thus, the decellularized adipose tissue appears to be an ideal material for tissue reconstruction.
The present study was initiated more than one year prior to the publication of the above-mentioned study by Flynn. Therefore, both the idea of developing an acellular adipose matrix and the formulation of the decellularization protocol were conceived independently. In fact, while Flynn’s decellularization protocol avoided using SDS, we did use SDS in our protocol. The reason why Flynn avoided SDS is that SDS has been found to alter the matrix architecture 24 and affect cellular repopulation of the matrix 25. However, as demonstrated in the present study, our matrix was repopulated by ADSCs in vitro and by host cells in vivo, and it remained intact 10 days and 3 months in the subcutaneous space and pelvic cavity, respectively. Therefore, our matrix was not only cytocompatible but also highly durable.
While we believe that adipose-derived matrix is an ideal grafting material for the repair of most peripheral nerves, we opted to test it for repairing CN because our lab is experienced in working with CN injury rat model. We hypothesized that the porous nature of the adipose-derived matrix in combination with ADSC’s neuroregenerative properties and ability to transdifferentiate into Schwann cells might result in increased neuroregeneration. The results showed that, 3 months after grafting, animals receiving implantation of ADSC-seeded matrices tended to have the best outcome. Histological examination of the grafts showed that the seeded matrices had more cells than the unseeded matrices, and the seeded matrices stained positive for S100, nNOS, and EdU while the unseeded matrices were negative for these markers. Marker expression level however varied considerably among the seeded matrices, and only one of them had a complete axonal in-growth. The presence of EdU-positive cells, which stained negative for S100, along the nerve fiber suggest that CN regeneration was encouraged by ADSC’s paracrine actions. In our recent study we have shown that ADSCs secrete CXCL5 cytokine that had neurotrophic effects on CN regeneration 11.
As to why large variations occurred in both the CN regeneration and erectile function recovery, one possibility is that the matrix lacked a directional canal that can guide axonal elongation toward the other side of the injured nerve. Thus, we believe that in future studies it is necessary to further fabricate the matrix into a tubular structure, which can then be seeded with autologous ADSCs prior to implantation for the repair of not just CN but other peripheral nerves as well. This plan appears feasible due to a recent study that successfully demonstrated the fabrication of adipose matrix into tubular scaffolds 4. Thus, while limited in success rate, the present study offers a proof of concept that can be further validated with new fabrication technologies.
CONCLUSION
Adipose tissue can be obtained in quantity and made into acellular matrices of various shapes and sizes. The matrix can be seeded with ADSC and used to bridge gaps in severed nerves. Grafting of the seeded matrix in a rat model of CN injury resulted in a substantial recovery of erectile function; however, further refinement of the matrix architecture is needed to improve the success rate.
ACKNOWLEDGMENTS
This study was supported by a grant from the department of defense (PC030775 to BK). MA has received research grants from the Belgische Vereniging voor Urologie, European Society of Surgical Oncology, Federico Foundation and Bayer Healthcare Belgium. MA is a fellow of the Research Foundation (FWO) Flanders.
REFERENCES
- 1.Lin CS, Xin ZC, Deng CH, et al. Defining adipose tissue-derived stem cells in tissue and in culture. Histol Histopathol. 2010;25:807–815. doi: 10.14670/HH-25.807. [DOI] [PubMed] [Google Scholar]
- 2.Zuk PA. The Adipose-derived stem cell: looking back and looking ahead. Mol Biol Cell. 2010;21:1783–1787. doi: 10.1091/mbc.E09-07-0589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown BN, Fruend JM, Li H, et al. Comparison of Three Methods for the Derivation of a Biologic Scaffold Composed of Adipose Tissue Extracellular Matrix. Tissue Eng Part C Methods. doi: 10.1089/ten.tec.2010.0342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choi JS, Yang HJ, Kim BS, et al. Fabrication of porous extracellular matrix scaffolds from human adipose tissue. Tissue Eng Part C Methods. 2010;16:387–396. doi: 10.1089/ten.TEC.2009.0276. [DOI] [PubMed] [Google Scholar]
- 5.Flynn LE. The use of decellularized adipose tissue to provide an inductive microenvironment for the adipogenic differentiation of human adipose-derived stem cells. Biomaterials. 2010;31:4715–4724. doi: 10.1016/j.biomaterials.2010.02.046. [DOI] [PubMed] [Google Scholar]
- 6.Chi GF, Kim MR, Kim DW, et al. Schwann cells differentiated from spheroid-forming cells of rat subcutaneous fat tissue myelinate axons in the spinal cord injury. Exp Neurol. 2010;222:304–317. doi: 10.1016/j.expneurol.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 7.Santiago LY, Clavijo-Alvarez J, Brayfield C, et al. Delivery of adipose-derived precursor cells for peripheral nerve repair. Cell Transplant. 2009;18:145–158. doi: 10.3727/096368909788341289. [DOI] [PubMed] [Google Scholar]
- 8.di Summa PG, Kingham PJ, Raffoul W, et al. Adipose-derived stem cells enhance peripheral nerve regeneration. J Plast Reconstr Aesthet Surg. 2010;63:1544–1552. doi: 10.1016/j.bjps.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Zhang Y, Luo H, Zhang Z, et al. A nerve graft constructed with xenogeneic acellular nerve matrix and autologous adipose-derived mesenchymal stem cells. Biomaterials. 2010;31:5312–5324. doi: 10.1016/j.biomaterials.2010.03.029. [DOI] [PubMed] [Google Scholar]
- 10.Albersen M, Fandel TM, Lin G, et al. Injections of Adipose Tissue-Derived Stem Cells and Stem Cell Lysate Improve Recovery of Erectile Function in a Rat Model of Cavernous Nerve Injury. J Sex Med. 2010 doi: 10.1111/j.1743-6109.2010.01875.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang H, Yang R, Wang Z, et al. Adipose Tissue-Derived Stem Cells Secrete CXCL5 Cytokine with Neurotrophic Effects on Cavernous Nerve Regeneration. J Sex Med. doi: 10.1111/j.1743-6109.2010.02128.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mulhall JP, Bella AJ, Briganti A, et al. Erectile function rehabilitation in the radical prostatectomy patient. J Sex Med. 2010;7:1687–1698. doi: 10.1111/j.1743-6109.2010.01804.x. [DOI] [PubMed] [Google Scholar]
- 13.Hekal IA, El-Bahnasawy MS, Mosbah A, et al. Recoverability of erectile function in post-radical cystectomy patients: subjective and objective evaluations. Eur Urol. 2009;55:275–283. doi: 10.1016/j.eururo.2008.06.072. [DOI] [PubMed] [Google Scholar]
- 14.Celentano V, Fabbrocile G, Luglio G, et al. Prospective study of sexual dysfunction in men with rectal cancer: feasibility and results of nerve sparing surgery. Int J Colorectal Dis. doi: 10.1007/s00384-010-0995-5. [DOI] [PubMed] [Google Scholar]
- 15.Mulhall JP. Defining and reporting erectile function outcomes after radical prostatectomy: challenges and misconceptions. J Urol. 2009;181:462–471. doi: 10.1016/j.juro.2008.10.047. [DOI] [PubMed] [Google Scholar]
- 16.Kim ED, Nath R, Slawin KM, et al. Bilateral nerve grafting during radical retropubic prostatectomy: extended follow-up. Urology. 2001;58:983–987. doi: 10.1016/s0090-4295(01)01403-0. [DOI] [PubMed] [Google Scholar]
- 17.Nelson BA, Chang SS, Cookson MS, et al. Morbidity and efficacy of genitofemoral nerve grafts with radical retropubic prostatectomy. Urology. 2006;67:789–792. doi: 10.1016/j.urology.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 18.Satkunasivam R, Appu S, Al-Azab R, et al. Recovery of erectile function after unilateral and bilateral cavernous nerve interposition grafting during radical pelvic surgery. J Urol. 2009;181:1258–1263. doi: 10.1016/j.juro.2008.10.153. [DOI] [PubMed] [Google Scholar]
- 19.Connolly SS, Yoo JJ, Abouheba M, et al. Cavernous nerve regeneration using acellular nerve grafts. World J Urol. 2008;26:333–339. doi: 10.1007/s00345-008-0283-y. [DOI] [PubMed] [Google Scholar]
- 20.Ning H, Lin G, Lue TF, et al. Neuron-like differentiation of adipose tissue-derived stromal cells and vascular smooth muscle cells. Differentiation. 2006;74:510–518. doi: 10.1111/j.1432-0436.2006.00081.x. [DOI] [PubMed] [Google Scholar]
- 21.Lin G, Huang YC, Shindel AW, et al. Labeling and tracking of mesenchymal stromal cells with EdU. Cytotherapy. 2009;11:864–873. doi: 10.3109/14653240903180084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tse KH, Sun M, Mantovani C, et al. In vitro evaluation of polyester-based scaffolds seeded with adipose derived stem cells for peripheral nerve regeneration. J Biomed Mater Res A. 2010 doi: 10.1002/jbm.a.32889. [DOI] [PubMed] [Google Scholar]
- 23.Takeuchi Y, Weiss RA. Xenotransplantation: reappraising the risk of retroviral zoonosis. Curr Opin Immunol. 2000;12:504–507. doi: 10.1016/s0952-7915(00)00128-x. [DOI] [PubMed] [Google Scholar]
- 24.Flynn L, Semple JL, Woodhouse KA. Decellularized placental matrices for adipose tissue engineering. J Biomed Mater Res A. 2006;79:359–369. doi: 10.1002/jbm.a.30762. [DOI] [PubMed] [Google Scholar]
- 25.Gratzer PF, Harrison RD, Woods T. Matrix alteration and not residual sodium dodecyl sulfate cytotoxicity affects the cellular repopulation of a decellularized matrix. Tissue Eng. 2006;12:2975–2983. doi: 10.1089/ten.2006.12.2975. [DOI] [PubMed] [Google Scholar]