Abstract
A 39-year-old Japanese man has been complaining of chest pain for 3 months and a CT revealed a huge tumour in the posterior mediastinum and retroperitoneum. The mediastinal tumour was continuous with the retroperitoneal one through the oesophageal hiatus and the lower oesophagus was completely surrounded by the tumour. MRI suggested lipogenic tumour. Resection of the tumour with oesophagectomy was performed through bilateral thoracotomy and laparotomy. Pathological examination revealed well-differentiated liposarcoma which was completely resected. The patient has been alive without recurrence for 14 months after surgery.
Background
Liposarcoma is a common soft tissue sarcoma which usually occurs in adults. The common sites of occurrence are the extremities, retroperitoneum and inguinal region. We have experienced a rare case of a giant liposarcoma located in the posterior mediastinum and retroperitoneum, surrounding the oesophagus. We successfully resected the tumour with an oesophagectomy through bilateral thoracotomy with a laparotomy. Here, we describe the feature of imaging studies of this rare tumour and demonstrate the operative procedures we undertook.
Case presentation
A 39-year-old Japanese man complained of chest pain for 3 months before admission. He had a good general condition and physical examination and laboratory data demonstrated no abnormality.
Investigations
CT of the thorax and abdomen revealed a huge tumour, 40×30×15 cm in size, in the posterior mediastinum and the retroperitoneum (figure 1). The mediastinal tumour was continuous with the retroperitoneal tumour through the oesophageal hiatus, and the lower oesophagus was completely surrounded by the tumour. The tumour contained areas of both fat and soft tissue density, and was scarcely enhanced with intravenous contrast medium. An 18F-fluorodeoxyglucose positron emission tomography (FDG-PET) revealed that small amount of FDG accumulated in the soft tissue density area. MRI demonstrated high intensity activity in the tumour by both T1-weighted and T2-weighted imaging, and there were many fibrous septa observed in the tumour (figure 2). These imaging studies indicated a lipogenic tumour and liposarcoma was highly suspected.
Figure 1.
A CT revealed a huge tumour located in the posterior mediastinum continuous to the retroperitoneum.
Figure 2.
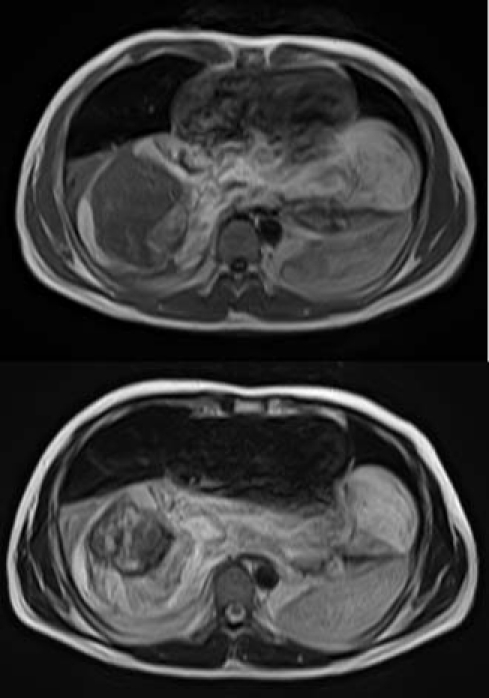
A MRI demonstrated low intensity tumour both in T1-weighted and T2-weighted images. A thick fibrous septa is observed in the tumour.
Treatment
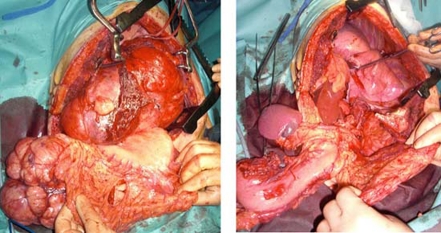
As a surgical resection was considered to be the only treatment to cure, surgery was performed. At first, under a general anaesthesia with the patient in a left lateral position, a right thoracotomy was undertaken through the fifth intercostal space. The tumour was located in the posterior mediastinum and adherent to the pleura, pericardium and oesophagus. The tumour was dissected sharply and bluntly from the surrounding organs. After the dissection was completed, the patient position was changed to a supine one and an upper midline skin incision was made for laparotomy. The tumour was located mainly in the retroperitoneum and adherent to the pancreas and mesocolon. The spleen, pancreas tail and descending colon were mobilised from the retroperitoneum, and the tumour was dissected from these organs. Finally, the patient was changed to a right hemi-lateral position, a left thoracotomy was made through the sixth intercostal space continuous to the laparotomy. The tumour was dissected from the left pleura and became free from the surrounding organs except the oesophagus, which ran through the tumour (figure 3A). At this point, it was decided to perform a combined resection of the oesophagus. A subtotal oesophagectomy was performed and the tumour was completely resected (figure 3B). As there was risk of local recurrence, a gastric conduit reconstruction was performed through the retrosternal route. Histopathologic examination revealed a well-differentiated liposarcoma (figure 4).
Figure 3.
(A,B) A complete removal of the tumour was achieved with combined resection of the oesophagus.
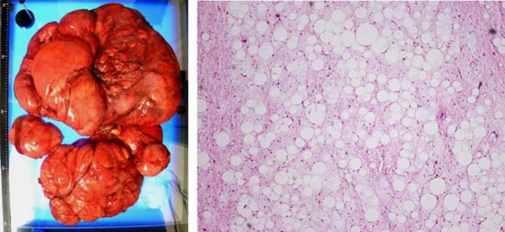
Figure 4.
Macroscopic and microscopic appearance of the resected tumour. Pathologic examination revealed well-differentiated liposarcoma (×100).
Outcome and follow-up
The postoperative course was uneventful and he was discharged on 18 postoperative day. At present, he has been alive without recurrence for 14 months.
Discussion
The incidence of sarcoma is relatively low, composing approximately 0.8% of all newly diagnosed malignancies. Of these sarcomas, liposarcoma accounts for approximately 20%, and 13% of them originate from the retroperitoneum. A mediastinal liposarcoma is extremely rare1 2 and there are few report of the mediastinal extension from the retroperitoneal liposarcoma. This is the first case report of liposarcoma which extended from the retroperitoneum to the mediastinum.
In most patients with liposarcoma, definite symptoms are lacking and the diagnosis is usually made by CT or MRI. Well-differentiated liposarcomas resemble lipomas, with attenuation (CT) and signal intensity (MRI) equal to those of fat. Fibrous septa may be thicker, more irregular, or more nodular than those seen in lipoma.3 In this case, both CT and MRI suggested a lipogenic tumour and thick fibrous septa was clearly observed in MRI.
Current recommendation in treatment for liposarcoma is en bloc removal if possible, as this is the only definitive treatment option.4 As well as the other soft tissue sarcomas, local control is critical and largely depends on the quality of surgery.5 In this case, we chose bilateral thoracotomy and laparotomy to approach the tumour, as it was the only method for en bloc removal of the tumour. Moreover, we performed oesophagectomy with the tumour resection, although it was a highly invasive surgery for the patient. As a result, a complete resection of the tumour was achieved. The patient is alive without disease at 14 months after surgery without any signs of recurrence.
Learning points.
-
▶
Mediastinal liposarcoma or mediastinal extension of the abdominal liposarcoma is extremely rare.
-
▶
Although a CT and a MRI are useful to diagnose lipogenic tumour, differential diagnosis of liposarcoma from lipoma is usually difficult.
-
▶
A complete resection of the tumour is the only treatment for cure.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Hsu JS, Kang WY, Liu GC, et al. Giant fibrolipoma in the mediastinum: an unusual case. Ann Thorac Surg 2005;80:e10–12 [DOI] [PubMed] [Google Scholar]
- 2.Lin YY, Su WF. Liposarcoma of the anterior mediastinum and neck. N Engl J Med 2010;363:864. [DOI] [PubMed] [Google Scholar]
- 3.Pereira JM, Sirlin CB, Pinto PS, et al. CT and MR imaging of extrahepatic fatty masses of the abdomen and pelvis: techniques, diagnosis, differential diagnosis, and pitfalls. Radiographics 2005;25:69–85 [DOI] [PubMed] [Google Scholar]
- 4.Wiedemann D, Schistek R, Gassner E, et al. Mediastinal liposarcoma. J Card Surg 2011;26:162–4 [DOI] [PubMed] [Google Scholar]
- 5.Stojadinovic A, Leung DH, Hoos A, et al. Analysis of the prognostic significance of microscopic margins in 2,084 localized primary adult soft tissue sarcomas. Ann Surg 2002;235:424–34 [DOI] [PMC free article] [PubMed] [Google Scholar]